Abstract
In clinical trials of adoptive T-cell therapy, the persistence of transferred cells correlates with therapeutic efficacy. However, properties of human T cells that enable their persistence in vivo are poorly understood, and model systems that enable investigation of the fate of human effector T cells (TE) have not been described. Here, we analyzed the engraftment of adoptively transferred human cytomegalovirus pp65-specific CD8+ TE cells derived from purified CD45RO+CD62L+ central memory (TCM) or CD45RO+CD62L− effector memory (TEM) precursors in an immunodeficient mouse model. The engraftment of TCM-derived effector cells (TCM/E) was dependent on human interleukin-15, and superior in magnitude and duration to TEM-derived effector cells (TEM/E). T-cell receptor Vβ analysis of persisting cells demonstrated that CD8+ TCM/E engraftment was polyclonal, suggesting that the ability to engraft is a general feature of TCM/E. CD8+ TEM/E proliferated extensively after transfer but underwent rapid apoptosis. In contrast, TCM/E were less prone to apoptosis and established a persistent reservoir of functional T cells in vivo characterized by higher CD28 expression. These studies predict that human CD8+ effector T cells derived from TCM precursors may be preferred for adoptive therapy based on superior engraftment fitness.
Introduction
Durable reconstitution of immunity to viral pathogens by the adoptive transfer of virus-specific effector T cells (TE) can be reproducibly achieved in a variety of clinical settings.1,2 The adoptive transfer of Epstein-Barr virus (EBV)-specific T cells to target EBV-associated malignancies also leads to persistent engraftment of transferred T cells and tumor regressions.3 The persistence of transferred tumor-reactive T cells, either isolated from the blood or tumor infiltrate, has been less consistent, even if the host undergoes lymphodepleting chemotherapy before T-cell transfer and receives interleukin-2 (IL-2) after T-cell transfer.4 In T-cell therapy of viruses, the TE cells are typically derived from virus-specific memory T cells isolated from immune donors; however, studies in which virus-specific T-cell clones or gene-marked polyclonal T-cell lines have been adoptively transferred have shown that not all TE cells derived from memory precursors are capable of durable engraftment.5,6 It is now possible to engineer any T cell to be tumor-reactive through the introduction of genes that encode T-cell receptors or chimeric antigen receptors that are specific for tumor antigens. Thus, defining characteristics of T cells that predict their persistence after adoptive transfer has important implications for future applications of T-cell therapy for cancer.
The repertoire of memory T cells in mice and humans is heterogeneous with respect to phenotype and function.7,8 Conventionally, CD8+ memory T cells are divided into effector memory T cells (TEM), which are prevalent in the blood and peripheral tissues and are capable of rapid effector function after engaging antigen; and central memory T cells (TCM), which express CD62L and CCR7 and, as a consequence, reside predominantly in lymph nodes where they are capable of extensive proliferation and differentiation on antigen reencounter. Thus, it is conceivable that the cell-intrinsic programming of these distinct memory T-cell subtypes may dictate divergent fates of their derived effector cells, including the ability to survive in vivo after adoptive transfer. We recently demonstrated a clear dichotomy in the engraftment potential of TCM- and TEM-derived CD8+ cytotoxic T lymphocyte clones using a nonhuman primate model system in cynomolgus macaques that closely recapitulates the cell culture methods used in clinical T-cell therapy trials.5 Virus-specific effector cytotoxic T lymphocytes derived from TCM, but not TEM, established persistent, functional T-cell immunity after adoptive transfer to lymphoreplete healthy macaques. Remarkably, an infusion of TE cells derived from a single TCM restored pools of both TCM and TEM in vivo that mounted a recall response to subsequent viral antigen challenge.5 A more recent study in which TE clones were derived from TCM or TEM elicited by prior vaccination and adoptively transferred to rhesus macaques did not observe a consistent difference in engraftment, with both subsets displaying poor persistence in the peripheral blood.9
Here we investigated the relative engraftment fitness of human CD8+ cytomegalovirus (CMV)-specific TE cells derived from CD62L+ and CD62L− memory T-cell precursors using methods for ex vivo activation and expansion that are used commonly in clinical trials. To assess engraftment, we developed a NOD/Scid IL-2RγC null (NOG) mouse model in which human IL-15, a nonredundant cytokine that is essential for CD8+ memory cell survival,10–12 was produced at low levels. Our data demonstrate that human TE derived from TCM precursors have superior engraftment compared with TE derived from TEM, and provide superior antitumor activity. The engraftment of TCM-derived TE cells is polyclonal, suggesting that the cell-intrinsic characteristics that enable survival are a general property conferred by their TCM origin. These findings suggest that the prospective isolation of TCM for subsequent use in antiviral and antitumor adoptive therapy would yield cell products with superior engraftment fitness and therapeutic activity.
Methods
Flow cytometry
Human peripheral blood mononuclear cells (PBMCs) and T cells were analyzed by flow cytometry after staining with fluorochrome-conjugated monoclonal antibodies (mAbs) to CD4, CD8, CD62L, CD45RO, CD127, CD28, CD45, CD3, perforin, granzyme A, Ki-67, interferon-γ (IFN-γ), CD122 (IL-2Rβ), CD132 (IL-2Rγ; BD Biosciences), and CCR7, and IL-15Rα (R&D Systems). Phycoerythrin (PE)-conjugated CMV pp65 (NLVPMVATV)–HLA-A2*0201 iTAg MHC tetramer, PE-conjugated multiallele negative tetramer, and the IOTestBeta Mark TCR V β Repertoire Kit (representing ∼ 70% of normal TCR Vβ repertoire) were obtained from Beckman Coulter. Isotype-matched mAbs served as controls. Carboxyfluorescein diacetate succinimidyl ester (CFSE) was purchased from Invitrogen. CaspScreen Flow Cytometric Apoptosis Detection Kit with D2R substrate was purchased from BioVision. All mAbs, tetramers, and CFSE were used according to the manufacturer's instructions. Data acquisition was performed on a FACSCalibur (BD Biosciences) using FCS Express, Version 3 software (De Novo Software).
DNA constructs and lentiviral vector
The HygroR-pp65_pEK plasmid contains the hygromycin resistance gene derived from pMG (Invivogen) and the full-length CMV Pp65 gene (gift from Dr John Zaia, City of Hope National Medical Center), fused by polymerase chain reaction and ligated into the mammalian expression vector pEK, which originated from pcDNA3.1(+; Invitrogen), and in which the CMV promoter and the ampicillin gene were replaced by the human elongation factor 1α promoter derived from pMG. Pp65–2A-eGFP-ffluc_epHIV7 contains the full-length CMV Pp65 gene, the 2A peptide sequence, an enhanced Gfp gene (Clontech), and the firefly luciferase gene (Invivogen) within the epHIV7 lentiviral vector, which was generated from the pHIV7 vector (gift from Jiing-Kuan Yee, COHNMC) that had its CMV promoter replaced with elongation factor 1α promoter.
The GFP-IMPDH2dm-2A-IL-15_pcDNA3.1(+) plasmid contains a fusion of the Gfp gene, which confers fluorescence, and the human inosine monophosphate dehydrogenase II (T3331, S351Y) gene, which confers resistance to mycophenolic acid, followed by the 2A self-cleaving peptide sequence13 and a human recombinant IL-15 gene. OKT3–2A-Hygro_pEK contains the antihuman-CD3ϵ immunoglobulin gene (gift from Andrew Raubitschek, COHNMC), the 2A peptide sequence, and the hygromycin resistance gene within the pEK vector. All construct and construction-associated polymerase chain reaction primer sequences are available on request.
Generation of CMV-specific antigen-presenting cells and T cells
Human PBMCs were isolated by density gradient centrifugation over Ficoll-Paque (Pharmacia Biotech) from heparinized peripheral blood obtained from healthy, HLA-A2+ CMV-immune volunteer donors. HLA-A2 positivity was determined based on screening a PBMC sample with a PE-conjugated anti-HLA-A2 antibody BB7.2 (BioLegend). The protocol and consent forms were approved by the COHNMC Internal Review Board.
To generate antigen-presenting cells that express CMV pp65 (vAPCs), PBMCs were resuspended in nucleofection solution using the Human T cell Nucleofector kit (Amaxa), and 5 × 107 cells were aliquoted into 0.2-cm cuvettes containing 10 μg HygroR-pp65_pEK (or pmaxGFP, Amaxa; as a transfection control) in a final volume of 100 μL/cuvette. The cells were electroporated using the Amaxa Nucleofector I, program U-14, after which cells were allowed to recover for 6 hours at 37°C, and then γ-irradiated to a dose of 1200 cGy. For separation of TCM and TEM subsets, PBMCs were washed, labeled with fluorochrome-conjugated anti-CD45RO and anti-CD62L antibodies, and CD62L+CD45RO+ TCM and CD62L−CD45RO+ TEM cells were sort-purified using a MoFlo MLS (Dako Cytomation). To generate CMV-specific T cells, the sort-purified TCM or TEM were then stimulated with autologous irradiated vAPCs in the presence of 5 U/mL IL-2 (Chiron) at a 4:1 (responder/stimulator) ratio once a week for 3 weeks, in RPMI 1640 supplemented with 2mM l-glutamine, 25mM N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid, 100 U/mL penicillin, 0.1 mg/mL streptomycin, and 10% human serum (CM). After enrichment by antigen stimulation, the CMV pp65-specific T cells were expanded using a rapid expansion method (REM) by which 106 T cells were stimulated with 30 ng/mL anti-CD3ϵ (OKT3; Ortho Biotech), 5 × 107 γ-irradiated PBMCs (3500 cGy), and 107 γ-irradiated lymphoblastoid cell lines (LCLs, 8000 cGy) in 50-mL culture media.14 Cultures were then supplemented with 50 U/mL IL-2 and 10 ng/mL rhIL-15 (CellGenix) every 48 hours for 14 days, after which a second REM stimulation with IL-2/IL-15 was performed for another 14 days before in vitro analysis and adoptive transfer.
EBV-transformed LCLs were made from PBMCs as previously described.15 LCLs that expressed OKT3 (LCL-OKT3) were derived by suspending allogeneic LCLs in nucleofection solution using the Amaxa Nucleofector kit T, adding the OKT3–2A-Hygromycin_pEK plasmid (5 μg plasmid/107 cells), and electroporating the LCLs using the Amaxa Nucleofector I, program T-20. Stable transfectants were obtained by growing the transfected LCLs in CM containing 0.4 mg/mL hygromycin. To generate LCL-pp65, autologous LCLs (auto-LCLs) were transduced with lentiviral vector pp65–2A-eGFP-ffluc_epHIV7 at a multiplicity of infection of 20 in the presence of 5 μg/mL polybrene in 500 μL CM. The initial transduction efficiency was 48.5% as assessed by GFP expression, and the LCL-pp65 were subsequently purified to more than 98% purity by sorting GFP+ cells.
NS0-IL-15 cells were generated by transfecting the mouse myeloma line NS0 (gift from Andrew Raubitschek, COHNMC) with GFP-IMPDH2dm-2A-IL-15_pcDNA3.1. NS0 cells were resuspended in nucleofection solution using the Amaxa Nucleofector kit T, 5 μg of plasmid DNA was added to 5 × 106 cells, and the cells were electroporated using the Amaxa Nucleofector I, program T-27. The transfected cells were grown in Dulbecco modified Eagle medium (Irvine Scientific) supplemented with 10% fetal calf serum, 25mM HEPES, and 2mM l-glutamine in the presence of 6μM mycophenolic acid, and screened for human IL-15 transgene expression by cytometric bead array with a Bio-Plex assay (Bio-Rad Laboratories).
Cytokine production assays
T cells (105) were cocultured overnight in 96-well tissue culture plates with 105 of LCL-OKT3, auto-LCL-pp65, auto-LCLs, or auto-LCLs that had been pulsed (2 hours at 37°C in CM) with 10 μg/mL of either the HLA-A2-restricted pp65 peptide (NLVPMVATV) or an HLA-A2-restricted control peptide (VLQELNVTV16; City of Hope DNA/RNA Peptide Synthesis Facility). Supernatants were harvested 18 hours after stimulation and analyzed by cytometric bead array using the Bio-Plex Human Cytokine 17-Plex Panel (Bio-Rad Laboratories) according to the manufacturer's instructions.
Cytotoxicity assays
Four-hour 51Cr release assays were performed as previously described17 using the indicated effector cells and 51Cr-labeled target cells.
Proliferation assays
Proliferation of TCM/E and TEM/E (5 × 104) was determined on incubation with different concentrations of rhIL-15 in 200 μL CM. After 48 hours, 50 μCi/mL [3H]-thymidine was added, and then T cells were harvested the next day (PHD Harvester, Brandel). [3H]-Thymidine incorporation was measured with a liquid scintillation LS 6500 counter (Beckman Coulter) using a standard [3H]-thymidine incorporation assay.
Xenograft models
All mouse experiments were approved by the COH Institute Animal Care and Use Committee. Six- to 10-week old NOD/Scid IL-2RγC null (NOG) mice were injected intravenously on day 0 with 107 TCM/E or TEM/E cells. Irradiated (8000 cGy) NS0-IL-15 cells (1.5 × 107) were administered intraperitoneally 3 times a week starting on day 0 to provide a systemic supply of human IL-15 in vivo. Peripheral blood was harvested by retro-orbital bleeding, and leukocytes were analyzed by flow cytometry to monitor human T-cell engraftment. Where indicated, 107 irradiated (8000 cGy) or 2.5 × 106 nonirradiated LCL-pp65 cells were injected intravenously, and luciferase activity was measured by Xenogen imaging as previously described.18
D2R assay
Caspase activity was determined with CaspSCREEN Flow Cytometric Apoptosis detection Kit according to the manufacturer's instructions. Briefly, aliquots of harvested cells from recipient mice were washed with phosphate-buffered saline twice and resuspended in 0.3 mL D2R incubation buffer; 3 μL of 1M dithiothreitol, 1 μL of D2R reagent, and 5 μL peridinin chlorophyll protein-conjugated anti-huCD45 mAb and then incubated in the dark for 20 minutes at 37°C. Flow cytometric analysis was performed on CD45+-gated cells using the FL-1 channel for D2R cleavage-associated fluorescence.
Results
Frequency of CD8+ TCM and TEM in healthy donor peripheral blood
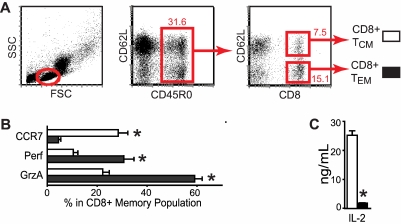
Human CD45RO+ memory T cells can be segregated into TCM and TEM based on differential expression of CD62L.8 Using multiparameter flow cytometry, we analyzed blood samples from 11 healthy donors to determine the proportions of CD45RO+ CD8+ TCM and TEM cells (Figure 1A; Table 1). Using forward and side scatter profiles to gate on lymphocytes, we found that CD45RO+ CD8+ cells in the blood have a predominantly CD62L− TEM phenotype, with CD8+ TCM accounting, on average, for only 5.1% of total lymphocytes. Consistent with previous reports on human memory T-cell heterogeneity, we observed that CD8+CD45RO+CD62L+ TCM more frequently, but not uniformally, coexpressed CCR7 compared with their CD8+ TEM counterparts (P < .05).7,19,20 Conversely, CD8+CD45RO+CD62L− TEM more frequently expressed perforin and granzyme A (P < .05) than CD8+CD45RO+CD62L+ TCM (Figure 1B).
Figure 1.
Frequency of CD8+ T-cell memory subsets in human peripheral blood. (A) Flow cytometric analysis of PBMCs from 4 different human donors gated on the lymphoid population by forward and side scatter (left panel) and analyzed for CD45RO, CD62L, and CD8 expression. CD45RO+ lymphocytes were then gated for CD8+CD62L+ TCM and CD8+CD62L− TEM (middle and right panels) and analyzed by multicolor flow cytometry with anti-CCR7, anti-perforin, or anti-granzyme A mAbs (B). Percentage of cells in each gate (red) is indicated, and mean percentage of the CD8+ TCM or TEM cells that were CCR7, perforin, or granzyme A positive (± SE; n = 3 donors) is indicated. *P < .05, CD8+ TCM versus TEM cells (unpaired Student t test). (C) Cytokine production profiles of the freshly isolated CD8+ TCM and TEM. Supernatants were collected after overnight coincubation with LCL-OKT3, and cytokine levels (mean ± SE of triplicate wells) were determined as described in “Cytokine production assays.” *P < .0001, cytokine levels of CD8+ TCM versus TEM cells (unpaired Student t test).
Table 1.
Percentage of lymphocytes from human PBMCs that are CD8+ TCM
| Donor | CD8+ TCM,* % | CD8+ TCM/TEM |
|---|---|---|
| 1 | 3.1 | 0.4 |
| 2 | 2.8 | 0.4 |
| 3 | 7.9 | 0.4 |
| 4 | 8.7 | 0.6 |
| 5 | 2.0 | 0.5 |
| 6 | 4.3 | 0.5 |
| 7 | 3.1 | 0.4 |
| 8 | 5.7 | 2.1 |
| 9 | 7.7 | 0.8 |
| 10 | 5.6 | 1.1 |
| 11 | 5.6 | 0.8 |
| Mean (SE) | 5.1 (0.6) | 0.7 (0.2) |
Values are percentages in lymphocyte gate based on forward scatter versus side scatter.
We then fluorescence-activated cell sorter-purified CD8+ cells from the TCM and TEM fractions to greater than 90% purity (supplemental Figure 1, available on the Blood Web site; see the Supplemental Materials link at the top of the online article) and assayed their direct effector function in vitro using OKT3 to provide a T-cell receptor (TCR) signal. Direct lysis of target cells expressing OKT3 was similar in CD8+ TCM and CD8+ TEM (36% lysis; data not shown), but OKT3 stimulation elicited significantly greater IL-2 production by CD8+ TCM cells compared with their TEM counterparts (P < .0001; Figure 1C).
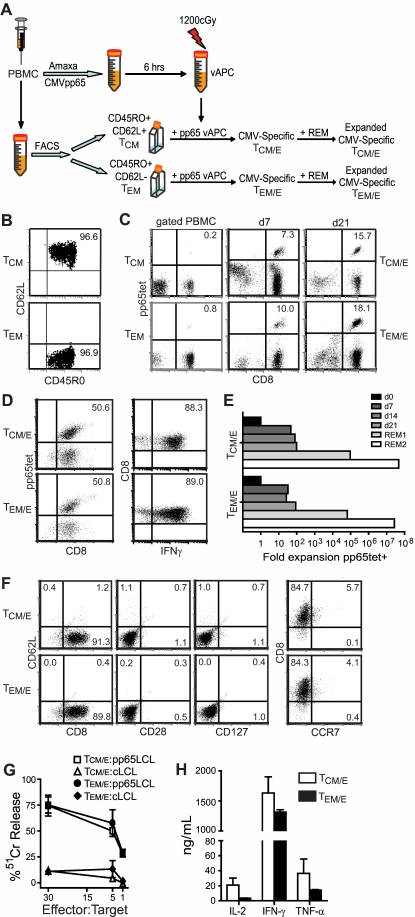
Differentiated TE cells derived from TCM and TEM are similar in phenotype and function in vitro
We chose CMV pp65 as a model antigen based in part on clinical experience with adoptive therapy targeting this antigen. We generated CMV pp65-specific TE lines from sort-purified TCM (TCM/E) or TEM (TEM/E) by stimulating the T cells weekly for 3 weeks with autologous irradiated PBMCs that were transfected with a full-length pp65 transgene as antigen-presenting cells (vAPCs; Figure 2A-B; supplemental Figure 2). The resulting polyclonal T-cell lines were enriched for pp65-specific T cells as determined by staining with an HLA A2/pp65 tetramer (Figure 2C) and were then expanded using anti-CD3 mAb and irradiated feeder cells. After 2 rounds of expansion, the majority (∼ 90%) of the CD8+ T cells secrete IFN-γ in response to overnight stimulation with antigen, with 50% of the CD8+ T cells staining positive for the HLA-A2/pp65 tetramer, which represents specificity to a single epitope of pp65 (Figure 2D). The expansion of pp65-specific T cells after stimulation with vAPCs and with anti-CD3 mAbs and feeders was equivalent for cells derived from TCM or TEM, with each culture expanding to cell numbers that approximated or exceeded clinical cell doses (> 109 cells; Figure 2E). Cultures derived from CD45RO+CD62L+ TCM or CD45RO+CD62L− TEM precursors exhibited an identical CD8+ TE phenotype (CD62L−, CD127−, CCR7−, and CD28−; Figure 2F) and equivalent cytolytic activity (Figure 2G). Cytokine secretion after engaging pp65-expressing target cells tended to be higher from TCM/E than TEM/E, but this was not statistically significant (Figure 2H).
Figure 2.
TE cells derived from TCM and TEM in vitro are similar in phenotype and function. (A) Schematic of methods for deriving CMV-specific TCM/E and TEM/E. Purified TCM, TEM, and pp65-expressing vAPCs were generated from the same CMV-seropositive donor's PBMCs. (B) CD45RO and CD62L staining of TCM (top) and TEM (bottom) after sorting from PBMCs. (C) CD8 and pp65-tetramer staining of gated PBMCs (left panels) and of CMV-specific TCM/E and TEM/E at day 7 (middle panels) and 21 (right panels) after stimulation with vAPCs. Histogram quadrants are based on staining with isotype and negative tetramer controls, and percentage of double-positive cells is indicated. (D) pp65 tetramer and intracellular IFN-γ staining of TCM/E and TEM/E before infusion, after overnight coincubation with LCL-pp65. (E) Fold expansion of pp65-tetramer+ cells was determined by multiplying the total number of cells by the percentage pp65tet+ (determined as shown in panel C) found at days 0, 7, 14, and 21 of vAPC stimulation and 14 days after the first and second anti-CD3 (REM) stimulations; these values were then normalized to the input cell number (day 0). (F) Expression of CD62L, CD127, CD28, CCR7, and CD8 on the TCM/E and TEM/E cell products. (G) Cytotoxic activity of TCM/E and TEM/E cell products against auto-LCLs loaded with either an HLA-A2-restricted control peptide (cLCL) or CMV pp65 peptide (pp65LCL). Mean percentage of 51Cr release (± SD) of triplicate wells is depicted. (H) Cytokine production by TCM/E and TEM/E. Supernatants were collected after coincubating T cells overnight with CMV pp65 peptide-loaded auto-LCLs, and mean (± SD of triplicate wells) cytokine levels were determined using cytometric bead array.
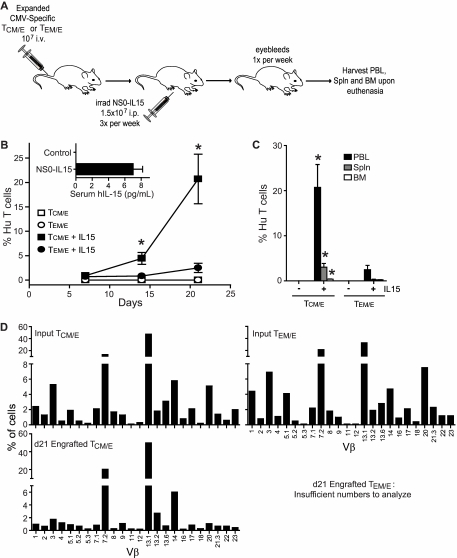
Engraftment of CMV-specific TCM/E in huIL-15 NOG mice is greater than that of TEM/E
We next examined the ability of human pp65-specific CD8+ TCM/E and TEM/E cells to persist after intravenous injection into NOG mice (Figure 3A). Because IL-15 is required for maintenance of memory T cells, we generated a murine NS0 cell line that constitutively secretes human IL-15 and developed an intraperitoneal dosing regimen of irradiated NS0-IL-15 cells that provided steady-state serum levels of human IL-15 in the range of 6 to 8 pg/mL (Figure 3B inset). To determine whether IL-15 was required for T-cell engraftment, we inoculated NOG mice intravenously with human TCM/E or TEM/E alone or with IL-15-producing NS0 cells. Mice inoculated with TCM/E or TEM/E alone did not exhibit sustained engraftment of human T cells. However, both TCM/E and TEM/E engrafted in mice that received NS0 cells that produced human IL-15, although the engraftment of TCM/E was markedly superior to that of TEM/E (20% vs 3% of circulating cells 21 days after adoptive transfer, P < .05; Figure 3B). The engraftment of TCM/E in spleen and bone marrow was also significantly higher than TEM/E in mice that received NS0-IL-15 cells (P < .05; Figure 3C).
Figure 3.
IL-15-dependent engraftment of CMV-specific TCM/E cells in NOG mice is greater than that of TEM/E. (A) Schematic of the experiment. (B) Mean percentage (± SE) of human T cells (CD45+ CD8+) in peripheral blood lymphocytes (PBLs) of mice engrafted with TCM/E (squares) or TEM/E (circles) was determined by flow cytometry (n = 5). *P < .05, TCM/E versus TEM/E cell engraftment in the presence of NS0-IL-15 cells (unpaired Student t test). (Inset) Mean levels of human IL-15 (± SE) in day 7 serum of NOG mice that had received 3 intraperitoneal injections of 1.5 × 107 irradiated NS0-IL-15 cells (n = 6) or in control mice (n = 10). (C) Mean percentage of human T cells (CD45+ CD8+) plus or minus SE in mouse PBL, bone marrow, and spleen at day 21. *P < .05, TCM/E cell engraftment in each organ versus that of TEM/E in the presence of NS0-IL-15 cells. (D) TCR Vβ repertoire of the CMV-specific TCM/E and TEM/E before (Input) and after (d21) engraftment. Percentage of CD3+ cells (Input) or CD45+ CD3+ cells (d21) that were positive for the indicated TCR Vβ genes was determined by flow cytometry.
To examine the possibility that the superior engraftment of TCM/E reflected the preferential expansion or survival of one or a few cells in the polyclonal culture, or that the failure of TEM/E to engraft was the result of limited diversity in the infused population, we performed TCR Vβ analysis on an aliquot of the input TCM/E and TEM/E and on aliquots of human T cells present in mice engrafted 21 days previously with TCM/E (Figure 3D). The in vivo analysis could not be performed in mice that received TEM/E because there were too few cells for analysis. The TCR repertoire was diverse in both TCM/E and TEM/E cultures with similar expansions of individual Vβ clonotypes, a result that excluded limited diversity of TEM/E as an explanation for poor engraftment. Moreover, the TCR Vβ diversity of the T cells that persisted in mice that received TCM/E was remarkably similar to that of the input population, indicating that engraftment fitness is a general feature of CD8+ TCM/E. To ensure that our results are not unique to CMV-specific cells, we also generated EBV-specific TCM/E and TEM/E to examine their engraftment potential (supplemental Figure 3A). After 3 stimulations using an EBV-transformed autologous lymphoblastoid cell line (auto-LCL), 73% and 75%, respectively, of viral-specific TCM/E and TEM/E are CD8+ (data not shown). Both EBV-specific TCM/E and TEM/E showed 70% cytotoxic activity against autologous, but not allogeneic, LCLs at a 30:1 effector/target ratio (supplemental Figure 3B). On adoptive transfer, these CD8+ TCM/E again showed enhanced engraftment fitness compared with their TEM/E counterparts (P < .05; supplemental Figure 3C).
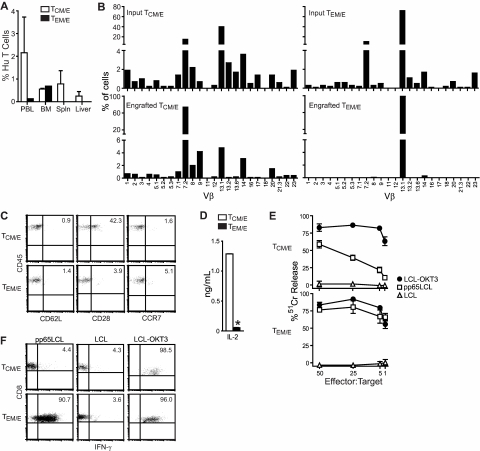
Human CD8+ TCM/E persist long-term in huIL-15 NOG mice and reacquire attributes of their TCM precursors
We followed a cohort of NOG mice that continued to receive injections of NS0-IL-15 cells for 100 days to determine the duration that CD8+ pp65-specific TCM/E and TEM/E would persist after adoptive transfer in response to IL-15. The engraftment of the CD8+ TCM/E in the blood remained steady at approximately 2% of mononuclear cells, whereas TEM/E remained at or below the level of detection (Figure 4A). Mice engrafted with TCM/E also had significant populations of human T cells in the spleen and bone marrow, whereas TEM/E were only detected in the bone marrow.
Figure 4.
Human CD8+ TCM/E persist long-term (100 days) in huIL-15 NOG mice and remain functional. TCM/E and TEM/E (107) were injected intravenously at day 0, and irradiated NS0-IL-15 cells (1.5 × 107) were administered 3 times a week starting at day 0, until mice were killed at day 100. (A) Mean percentage of human CD45+CD8+ cells (± SE) in mouse PBL, bone marrow, and spleen at day 100 was determined by flow cytometry (n = 5). (B) TCR Vβ repertoire of the input and long-term engrafted TCM/E and TEM/E. Bone marrow was pooled from mice, and human CD45+ cells were sorted and expanded by stimulation with anti-CD3. The percentage of CD3+ cells positive for the indicated TCR Vβ genes was determined by flow cytometry. (C) Bone marrow harvested at day 100 from mice engrafted with TCM/E and TEM/E was analyzed by flow cytometry for expression of human CD45, CD62L, CCR7, and CD28. Gating was based on staining with isotype control mAb, and the percentage of double-positive cells is indicated. (D) IL-2 production from CD45+ T cells derived from day 100 bone marrow of mice engrafted with TCM/E and TEM/E. Supernatants were collected after T cells were coincubated overnight with LCL-pp65, and IL-2 levels were determined using cytometric bead array. (E) Cytotoxic activity of human T cells derived from day 100 bone marrow of mice engrafted with TCM/E and TEM/E, and stimulated with anti-CD3 mAb. Target cells included OKT3-expressing LCLs, auto-LCLs or LCL-pp65. Mean percentage of 51Cr release (± SD) of triplicate wells. (F) Intracellular IFN-γ staining of human T cells derived from day 100 bone marrow of mice engrafted with TCM/E and TEM/E and coincubated overnight with LCL-pp65, LCL-OKT3, or auto-LCLs.
To enable analysis of diversity and phenotype of the long-term engrafted populations, we pooled bone marrow harvested from 5 mice in each cohort, sorted human T cells based on expression of CD45 using an AutoMACS (Milteny Biotec), and expanded the sort-purified T cells in vitro for analysis. Similar to that observed in short-term engraftment experiments, T cells present in the bone marrow of mice engrafted with TCM/E displayed a broad TCR Vβ usage, whereas mice engrafted with TEM/E had only low levels of T cells that consisted of a single TCR clonotype (Vβ 13.1; Figure 4B). Although the phenotype and function of TCM/E and TEM/E were similar before infusion (Figure 2D-H), the T cells that persisted long-term in mice given TCM/E were 40% CD28+ compared with 4% CD28+ in mice given TEM/E (Figure 4C). On pp65 antigen stimulation, the TCM/E that persisted in vivo secreted 1.3 ng/mL IL-2, whereas TEM/E secreted only 0.05 ng/mL (P < .0001; Figure 4D). The persistent TCM/E displayed lower antigen-specific cytolytic activity and IFN-γ production compared with TEM/E (Figure 4E-F). Together, these data show that TE cells derived from TCM have a uniform capacity to persist long-term after infusion and to reacquire attributes of their TCM precursors, whereas the engraftment of TEM/E is poor and limited to a small subset of cells that retain immediate effector function.
Adoptively transferred CD8+ TEM/E exhibit both greater proliferation and cell death than CD8+ TCM/E in huIL-15 NOG mice
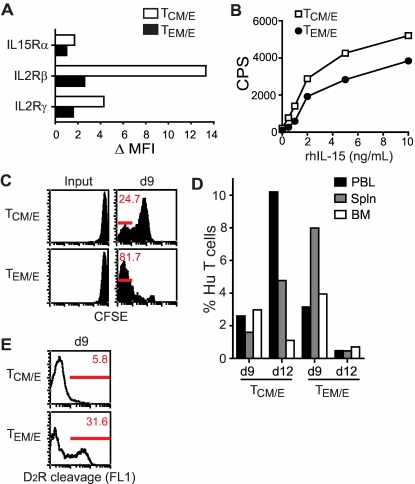
A potential mechanism by which the in vivo engraftment of TCM/E in NOG mice given irradiated NS0-IL-15 may be superior to TEM/E was that TCM/E may be more responsive to IL-15. Thus, we examined the cell surface expression of IL-15Rα, IL-2Rβ, and IL-2Rγ on CMV-specific TCM/E and TEM/E before infusion. Similar to the results we observed with T-cell clones derived from each memory subset in nonhuman primates,5 it was found that TCM/E expressed higher levels of surface IL-15Rα, IL-2Rβ, and IL-2Rγ (Figure 5A). This also conferred on TCM/E a slightly enhanced proliferative response when cultured in soluble IL-15 compared with TEM/E (Figure 5B). These results suggested that TCM/E might proliferate more vigorously in response to IL-15 in vivo. However, when we inoculated subsequent cohorts of huIL-15 NOG mice with TCM/E and TEM/E that were labeled with CFSE before in vivo administration, we observed greater proliferation of TEM/E in the first 9 days after adoptive transfer as indicated by the percentage of cells that diluted CFSE (ie, 81% for TEM/E and 25% for TCM/E, respectively; Figure 5C). Yet as in previous experiments, TCM/E again exhibited superior persistence in the blood, spleen, and bone marrow compared with TEM/E (Figure 5D).
Figure 5.
Differential cytokine receptor expression, IL-15–mediated proliferation, and caspase activity of TCM/E and TEM/E. (A) IL-15Rα, IL-2Rβ, or IL-2Rγ expression by TCM/E and TEM/E. Mean fluorescence intensity was normalized to that of isotype control staining in each case to determine ΔMFI. (B) Proliferation of TCM/E and TEM/E was determined after 48-hour incubation with different concentrations of rhIL-15 using a standard [3H]-thymidine incorporation assay. (C-D) CFSE-labeled TCM/E and TEM/E (107) were injected intravenously into mice at day 0, and irradiated NS0-IL-15 cells (1.5 × 107) were administered 3 times a week starting at day 0, until mice were killed at either day 9 or day 12. (C) CFSE profiles of the input and engrafted TCM/E and TEM/E in day 9 PBL was assessed by flow cytometry. Percentage of CFSE-diluted cells that fall within the first log are indicated. (D) Engraftment of the CD45+ human T cells in the PBL, bone marrow, and spleen was assessed on days 9 and 12 by flow cytometry. (E) FL-1 profiles of CD45+ human T cells in the PBL were assessed on day 9 as a readout for cleavage of the caspase substrate D2R. The percentage of cells with cleaved D2R is depicted.
The finding that TEM/E proliferated more vigorously than TCM/E in vivo, but were present in lower numbers (ie, at day 12), suggested that these cells may undergo more rapid cell death. To evaluate this possibility, D2R cleavage was used as a measure of caspase activity and a surrogate for apoptosis. We found that 31.6% of TEM/E but only 5.8% of TCM/E were positive for activated caspase activity at day 9 after infusion (Figure 5E). We also found that the percentage of CD28+ cells markedly increased within the in vivo engrafted TCM/E population compared with the TCM/E before infusion (16% ± 2% vs 1%), whereas the percentage of CD28+ TEM/E remained the same (1%). These results are consistent with superior survival of CD8+ TCM/E in huIL-15 NOG mice resulting from less cell death rather than increased proliferation.
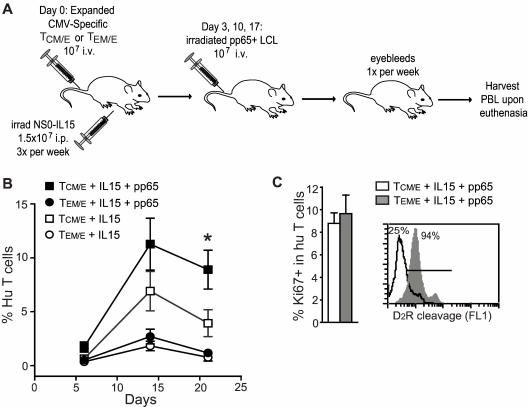
Adoptively transferred CD8+ TCM/E proliferate and exhibit superior protective immunity after in vivo antigen challenge
We next evaluated the ability of CMV-specific T cells engrafted in the huIL-15 NOG mice to respond to antigen challenge. CD8+ TCM/E and TEM/E were transferred into cohorts of 12 mice each and then irradiated auto-LCLs that were transduced to express CMV-pp65 were administered to half of the mice in each cohort on days 3, 10, and 17 after T-cell transfer (Figure 6A). Mice that received CD8+ TCM/E and antigen challenge exhibited significantly higher levels of human T-cell engraftment in the blood at days 14 and 21 than mice that received CD8+ TCM/E alone (P < .05). As before, the engraftment of CD8 TEM/E was significantly lower than that of TCM/E and was not augmented by antigen challenge (P > .05; Figure 6B). In this experiment, we assessed proliferation by staining human T cells harvested from mice for Ki-67 expression and found that nearly equivalent fractions (9%) of TCM/E and TEM/E were Ki-67 positive at this time point (Figure 6C). However, similar to the results in mice that did not receive antigen stimulation, 94% of the engrafted TEM/E were positive for activated caspase activity compared with 25% of the engrafted TCM/E, consistent with a higher propensity of the TEM/E to undergo apoptosis.
Figure 6.
Adoptively transferred CMV-specific CD8+ TCM/E exhibit a better response to antigen challenge in vivo than TEM/E. (A) Schematic of in vivo antigenic stimulation of engrafted CMV-specific TCM/E and TEM/E. (B) Engraftment of CMV-specific TCM/E (squares) or TEM/E (circles) was carried out with (black) or without (white) administration of irradiated CMV pp65-expressing LCLs at days 3, 10, and17; and mean percentage (± SE) of human T cells (CD45+ CD8+) in mouse PBL was determined by flow cytometry (n = 6). *P < .05, engraftment of TCM/E alone versus pp65-driven TCM/E engraftment (unpaired Student t test). (C) On euthanasia at day 28, PBLs were harvested and analyzed by flow cytometry for percentage of Ki-67+ cells in the human T-cell population (left) and for the ability of CD45+ human T cells to cleave the caspase substrate D2R (right).
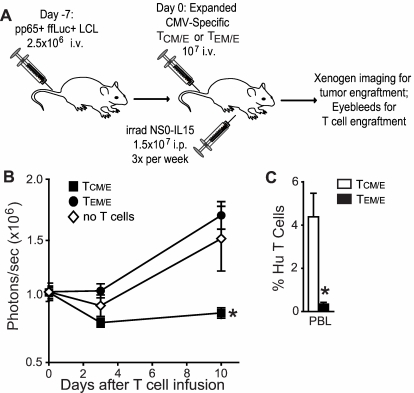
The higher levels of engraftment and superior response to antigen stimulation in vivo achieved with infusions of TCM/E suggested that this subset would have superior therapeutic activity. To evaluate this, we designed an experiment to assess the ability of transferred CMV-specific TE cells derived from either TCM or TEM to protect against the lethal outgrowth of auto-LCLs transduced to express both CMV-pp65 and firefly luciferase (ffLuc, a reporter for biophotonic imaging of tumor growth). In this experiment, pp65+ffLuc+ LCLs were inoculated intravenously into NOG mice and allowed to engraft for one week, after which the mice were either untreated or treated with a single infusion of either CMV-specific CD8+ TCM/E or TEM/E with irradiated NS0-IL-15 support (Figure 7A). Tumors progressed in mice receiving TEM/E at a rate similar to untreated control mice over a 10-day observation period, whereas administration of TCM/E caused a significant reduction in tumor growth (P < .05; Figure 7B). The superior antitumor response mediated by TCM/E correlated with significantly higher levels of engraftment (4.3% TCM/E vs 0.3% TEM/E; P < .05; Figure 7C).
Figure 7.
Adoptively transferred CMV-specific CD8+ TCM/E exhibit superior protection from tumor challenge. (A) Schematic of the in vivo tumor challenge experiment. (B) Engraftment of pp65+ ffLuc+ LCL in animals treated with or without CMV-specific TCM/E or TEM/E was determined by Xenogen imaging; and mean (± SE) of total flux levels of luciferase activity are shown for each group (n = 5). *P < .05, animals treated with TCM/E versus either untreated or TEM/E-treated animals (analysis of variance). (C) Mean percentage (± SE) of human CD45+CD8+ cells in day 10 mouse PBL was determined by flow cytometry. *P < .05, TCM/E versus TEM/E engraftment (unpaired Student t test).
Discussion
We have developed a NOG mouse model for studying the ability of human effector T cells derived from distinct memory T-cell subsets to establish persistent engraftment and respond to subsequent antigen stimulation. A unique feature of this model was the introduction of irradiated NS0 cells transfected to express human IL-15, which provided serum levels of IL-15 similar to those reported in normal humans. IL-15 has been shown to be essential for maintenance of memory T cells and enabled us to establish durable engraftment of antigen-specific human T cells in NOG mice after the infusion of differentiated TE cells.
A key finding of our study was that human antigen-specific CD8+ TE cells derived from TCM exhibit superior engraftment in hu-IL-15 NOG mice compared with TE cells derived from TEM. This result is in agreement with a study in nonhuman primates,5 in which we found that antigen-specific CD8+ T-cell clones derived from TCM, but not TEM, were capable of engrafting long-term and reverting to the memory T-cell pool. Our experiments in huIL-15 NOG mice extend the primate experiment in several ways. First, we used polyclonal T cells and included a comparison of the TCR Vβ repertoire of the input cells with that of persistently engrafted cells. This analysis demonstrated retention of a broad TCR repertoire in the human TCM/E cells that persisted long-term, suggesting that engraftment fitness is a general trait common to all TE cells derived from TCM, and not attributable to only a subset of these cells. The rare T cells that persisted from TEM/E were derived from a very restricted clonotype, consistent with the lack of engraftment being a general trait of TE cells derived from TEM. Second, we show that transfer of TCM/E provides superior protection from a tumor challenge, which was not possible in the nonhuman primate model. Finally, our study is the first, to our knowledge, to show that providing human IL-15 is sufficient to support the long-term persistence (> 3 months) of functional human virus-specific T cells in NOG mice.
In the studies in which TCM/E clones were transferred to nonhuman primates, a subset of the T cells that persisted long-term reexpressed surface markers of TCM, including CD62L and CCR7, and occupied memory cell niches in the lymph nodes and bone marrow.5 The human T cells that persisted long-term in huIL-15 NOG mice after the infusion of TCM/E did not reacquire expression of CD62L and CCR7. However, we did observe that a major fraction of the TCM/E that persisted in huIL-15 NOG mice highly expressed CD28 in vivo and were capable of autocrine IL-2 secretion in response to antigen stimulation. The persisting TCM/E were also capable of expanding in vivo more robustly in response to antigen reexposure and mediating superior protection from a lethal challenge with CMV-pp65+ tumor cells. This suggests that the huIL-15 NOG mouse model does not provide human T cells with all of the signals or niches required for the acquisition of CD62L and CCR7 but does provide sufficient cues for TCM/E to revert to resting functional memory T cells.
The observation that TCM/E exhibit superior engraftment potential has obvious implications for human adoptive T-cell therapy, yet the basis for the profound differences in the fate of TE cells is not completely understood. In the nonhuman primate studies, CD8+ TCM/E clones were found to express higher levels of IL-15 receptor chains and exhibited superior survival in vitro in response to IL-15 compared with TEM/E and less apoptosis in vivo. Our data comparing the fate of human TCM/E and TEM/E in vivo confirm a requirement for IL-15 for in vivo survival of transferred human T cells. Transferred TEM/E proliferate more in vivo than TCM/E in response to IL-15 but exhibit higher levels of caspase activation and cell death, consistent with a different cellular response to IL-15 as a potential mechanism that contributes to their poor survival. However, it is probable that additional cell-intrinsic properties dictate the capacity of TE cells to revert to the memory pool. This model also provides an opportunity to study other human cytokines, including inhibitory cytokines such as IL-10 for their effect on T-cell persistence and function.
Much of our current understanding of memory T-cell lineage fate decisions is derived from studies in mice and has focused on the transition of TE cells derived from the naive T-cell pool to the TCM and TEM subsets.6,21,22 Our work with human and nonhuman primate TE cells derived from the TCM and TEM subsets suggests that the initial lineage fate choice imparts cell-intrinsic programming that is retained through subsequent rounds of TE differentiation and influences the differential engraftment fitness after adoptive transfer. Recently, Araki et al described histone methylation as a transcriptional regulatory mechanism that is differentially maintained in human CD8+ central and effector memory subsets.23 Our data are consistent with an epigenetic programming mechanism that is retained on memory cell differentiation ex vivo to effector cells. Ongoing studies in the laboratory are evaluating broader epigenetic mechanisms, including genome-wide analysis of DNA methylation and the evaluation of ex vivo epigenetic modification of T cells to program a broader repertoire of effector cells for engraftment fitness.
We have focused on memory cells as a reservoir of antigen-specific precursor cells for adoptive therapy, but the extent to which human naive cells can be programmed in vitro for downstream therapeutic applications remains to be determined. Studies in murine models have suggested that TE cells derived from naive T cells may have a superior ability to persist in vivo compared with TCM, providing the culture duration before adoptive transfer is very short.24 However, these experiments were performed with T cells from a TCR transgenic mouse and would be difficult to easily translate to humans. Our studies in humans and nonhuman primates demonstrate that long-term culture of TCM/E cells is not an impediment to effective T-cell transfer, suggesting that the cell-intrinsic qualities that dictate engraftment are more permanently established in TCM/E than in TE cells derived from naive T cells. Pharmacologic manipulation of WNT signaling during culturing of murine naive T cells or manipulation of mammalian target of rapamycin signaling during the induction of an effector response from naive T cells in vivo may promote the acquisition of T-cell memory.25,26 It will be of interest to determine whether these findings can be extrapolated to human T cells. Achieving reproducible high level engraftment of human antigen-specific T cells in clinical trials of adoptive therapy for cancer has been a formidable obstacle; this is in contrast to the trials in which virus-specific TE generated from healthy immune donors were transferred to recipients to reconstitute viral immunity after allogeneic hematopoietic stem cell transplantation.1,27,28 To date, no cancer adoptive therapy clinical trial has used the transfer of effector cells from a defined population of precursor cells, whether they be naive, central memory, or effector memory in origin. Our studies and others show that CD8+ TCM are present in low frequency in the blood, constituting only 2% to 8% of peripheral blood T cells, and it is likely that this pool contains very rare T cells specific for tumor-associated antigens. Thus, adoptive T-cell therapy for cancer may need to use gene transfer to endow TCM or other subsets with tumor reactivity, such as could be accomplished by the introduction of genes encoding tumor-specific T-cell receptors or chimeric antigen receptors.29,30 Our group has therefore focused on developing methods to purify human T-cell subsets, including polyclonal and virus-specific TCM for the generation of tumor reactive TE via subsequent genetic modification using viral vectors. This will enable the incorporation of defined precursor cells into clinical trials designed to determine which subsets of T cells will provide superior in vivo persistence and therapeutic efficacy.
Supplementary Material
Acknowledgments
The authors thank Julie R. Ostberg for assistance in generating the manuscript.
This work was supported by the National Institutes of Health (grants P50 CA107399, P01 CA030206, R01 CA136551, R01 CA114536, and AI053193) and the Lymphoma Research Foundation.
Footnotes
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: X.W. designed and performed research, collected, analyzed, and interpreted data, and cowrote the manuscript; C.B. designed research, contributed analytic tools, analyzed and interpreted data, and cowrote the manuscript; C.W.W. performed research and collected data; S.J.F. analyzed and interpreted data; and S.R.R. and M.C.J. designed research, analyzed and interpreted data, and cowrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Michael C. Jensen, Center for Immunity and Immunotherapies, Division of Hematology and Oncology, Seattle Children's Research Institute, 1900 Ninth Ave, Seattle, WA 98101; e-mail: michael.jensen@seattlechildrens.org.
References
- 1.Mackinnon S, Thomson K, Verfuerth S, Peggs K, Lowdell M. Adoptive cellular therapy for cytomegalovirus infection following allogeneic stem cell transplantation using virus-specific T cells. Blood Cells Mol Dis. 2008;40(1):63–67. doi: 10.1016/j.bcmd.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Walter EA, Greenberg PD, Gilbert MJ, et al. Reconstitution of cellular immunity against cytomegalovirus in recipients of allogeneic bone marrow by transfer of T-cell clones from the donor. N Engl J Med. 1995;333(16):1038–1044. doi: 10.1056/NEJM199510193331603. [DOI] [PubMed] [Google Scholar]
- 3.Gottschalk S, Heslop HE, Rooney CM. Adoptive immunotherapy for EBV-associated malignancies. Leuk Lymphoma. 2005;46(1):1–10. doi: 10.1080/10428190400002202. [DOI] [PubMed] [Google Scholar]
- 4.Heemskerk B, Liu K, Dudley ME, et al. Adoptive cell therapy for patients with melanoma, using tumor-infiltrating lymphocytes genetically engineered to secrete interleukin-2. Hum Gene Ther. 2008;19(5):496–510. doi: 10.1089/hum.2007.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berger C, Jensen MC, Lansdorp PM, Gough M, Elliott C, Riddell SR. Adoptive transfer of effector CD8 T cells derived from central memory cells establishes persistent T cell memory in primates. J Clin Invest. 2008;118(1):294–305. doi: 10.1172/JCI32103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wherry EJ, Teichgraber V, Becker TC, et al. Lineage relationship and protective immunity of memory CD8 T-cell subsets. Nat Immunol. 2003;4(3):225–234. doi: 10.1038/ni889. [DOI] [PubMed] [Google Scholar]
- 7.Sallusto F, Geginat J, Lanzavecchia A. Central memory and effector memory T-cell subsets: function, generation, and maintenance. Annu Rev Immunol. 2004;22:745–763. doi: 10.1146/annurev.immunol.22.012703.104702. [DOI] [PubMed] [Google Scholar]
- 8.Farber DL, Ahmadzadeh M. Dissecting the complexity of the memory T cell response. Immunol Res. 2002;25(3):247–259. doi: 10.1385/IR:25:3:247. [DOI] [PubMed] [Google Scholar]
- 9.Minang JT, Trivett MT, Bolton DL, et al. Distribution, persistence, and efficacy of adoptively transferred central and effector memory-derived autologous simian immunodeficiency virus-specific CD8+ T cell clones in rhesus macaques during acute infection. J Immunol. 2010;184(1):315–326. doi: 10.4049/jimmunol.0902410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandau MM, Kohlmeier JE, Woodland DL, Jameson SC. IL-15 regulates both quantitative and qualitative features of the memory CD8 T cell pool. J Immunol. 2010;184(1):35–44. doi: 10.4049/jimmunol.0803355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kokaji AI, Hockley DL, Kane KP. IL-15 transpresentation augments CD8+ T cell activation and is required for optimal recall responses by central memory CD8+ T cells. J Immunol. 2008;180(7):4391–4401. doi: 10.4049/jimmunol.180.7.4391. [DOI] [PubMed] [Google Scholar]
- 12.Daudt L, Maccario R, Locatelli F, et al. Interleukin-15 favors the expansion of central memory CD8+ T cells in ex vivo generated, antileukemia human cytotoxic T lymphocyte lines. J Immunother. 2008;31(4):385–393. doi: 10.1097/CJI.0b013e31816b1092. [DOI] [PubMed] [Google Scholar]
- 13.Donnelly ML, Hughes LE, Luke G, et al. The ‘cleavage’ activities of foot-and-mouth disease virus 2A site-directed mutants and naturally occurring ‘2A-like’ sequences. J Gen Virol. 2001;82(5):1027–1041. doi: 10.1099/0022-1317-82-5-1027. [DOI] [PubMed] [Google Scholar]
- 14.Crossland KD, Lee VK, Chen W, Riddell SR, Greenberg PD, Cheever MA. T cells from tumor-immune mice nonspecifically expanded in vitro with anti-CD3 plus IL-2 retain specific function in vitro and can eradicate disseminated leukemia in vivo. J Immunol. 1991;146(12):4414–4420. [PubMed] [Google Scholar]
- 15.Pelloquin F, Lamelin JP, Lenoir GM. Human B lymphocytes immortalization by Epstein-Barr virus in the presence of cyclosporin A. In Vitro Cell Dev Biol. 1986;22(12):689–694. doi: 10.1007/BF02621085. [DOI] [PubMed] [Google Scholar]
- 16.Molldrem JJ, Lee PP, Wang C, Champlin RE, Davis MM. A PR1-human leukocyte antigen-A2 tetramer can be used to isolate low-frequency cytotoxic T lymphocytes from healthy donors that selectively lyse chronic myelogenous leukemia. Cancer Res. 1999;59(11):2675–2681. [PubMed] [Google Scholar]
- 17.Stastny MJ, Brown CE, Ruel C, Jensen MC. Medulloblastomas expressing IL-13Ralpha2 are targets for IL-13-zetakine+ cytolytic T cells. J Pediatr Hematol Oncol. 2007;29(10):669–677. doi: 10.1097/MPH.0b013e3181468c68. [DOI] [PubMed] [Google Scholar]
- 18.Kahlon KS, Brown C, Cooper LJ, Raubitschek A, Forman SJ, Jensen MC. Specific recognition and killing of glioblastoma multiforme by interleukin 13-zetakine redirected cytolytic T cells. Cancer Res. 2004;64(24):9160–9166. doi: 10.1158/0008-5472.CAN-04-0454. [DOI] [PubMed] [Google Scholar]
- 19.Sallusto F, Lenig D, Forster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401(6754):708–712. doi: 10.1038/44385. [DOI] [PubMed] [Google Scholar]
- 20.Lanzavecchia A, Sallusto F. Understanding the generation and function of memory T-cell subsets. Curr Opin Immunol. 2005;17(3):326–332. doi: 10.1016/j.coi.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Kaech SM, Wherry EJ. Heterogeneity and cell-fate decisions in effector and memory CD8+ T cell differentiation during viral infection. Immunity. 2007;27(3):393–405. doi: 10.1016/j.immuni.2007.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wherry EJ, Barber DL, Kaech SM, Blattman JN, Ahmed R. Antigen-independent memory CD8 T cells do not develop during chronic viral infection. Proc Natl Acad Sci U S A. 2004;101(45):16004–16009. doi: 10.1073/pnas.0407192101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Araki Y, Wang Z, Zang C, et al. Genome-wide analysis of histone methylation reveals chromatin state-based regulation of gene transcription and function of memory CD8+ T cells. Immunity. 2009;30(6):912–925. doi: 10.1016/j.immuni.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hinrichs CS, Borman ZA, Cassard L, et al. Adoptively transferred effector cells derived from naive rather than central memory CD8+ T cells mediate superior antitumor immunity. Proc Natl Acad Sci U S A. 2009;106(41):17469–17474. doi: 10.1073/pnas.0907448106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Araki K, Turner AP, Shaffer VO, et al. mTOR regulates memory CD8 T-cell differentiation. Nature. 2009;460(7251):108–112. doi: 10.1038/nature08155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gattinoni L, Zhong XS, Palmer DC, et al. Wnt signaling arrests effector T cell differentiation and generates CD8+ memory stem cells. Nat Med. 2009;15(7):808–813. doi: 10.1038/nm.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoffmann T, Russell C, Vindelov L. Generation of EBV-specific CTLs suitable for adoptive immunotherapy of EBV-associated lymphoproliferative disease following allogeneic transplantation. APMIS. 2002;110(2):148–157. doi: 10.1034/j.1600-0463.2002.100205.x. [DOI] [PubMed] [Google Scholar]
- 28.Greenberg PD, Reusser P, Goodrich JM, Riddell SR. Development of a treatment regimen for human cytomegalovirus (CMV) infection in bone marrow transplantation recipients by adoptive transfer of donor-derived CMV-specific T cell clones expanded in vitro. Ann N Y Acad Sci. 1991;636:184–195. doi: 10.1111/j.1749-6632.1991.tb33450.x. [DOI] [PubMed] [Google Scholar]
- 29.Kershaw MH, Teng MW, Smyth MJ, Darcy PK. Supernatural T cells: genetic modification of T cells for cancer therapy. Nat Rev Immunol. 2005;5(12):928–940. doi: 10.1038/nri1729. [DOI] [PubMed] [Google Scholar]
- 30.June CH, Blazar BR, Riley JL. Engineering lymphocyte subsets: tools, trials and tribulations. Nat Rev Immunol. 2009;9(10):704–716. doi: 10.1038/nri2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.