Because acute cough has a different range of causes in children younger than 15 years of age than it does in adults, children should be assessed and treated differently.1 In general, there are fewer randomized controlled trials in children than in adults, so the evidence is less bountiful, and an important aspect of treating children is paying attention to parental concerns and expectations.
One Tuesday morning in the clinic, Mrs Jones brings her 4-year-old daughter, Jenny, in to see you. Jenny has had a cough for about 4 days; she might have been feverish at the beginning of the illness, but she is not feverish now. She has a runny nose, and Mrs Jones says she was pulling at her ears yesterday. Her cough sounded dry and barky; she was not short of breath and her colour was always normal. Jenny has been at home for 3 days, missing day care. Jenny’s medical record shows that at the age of 3 months, she was hospitalized for treatment of bronchiolitis. She has twice been treated for otitis media and has received hydrocortisone cream for infantile eczema. Mrs Jones says that when they were away on holiday 2 years ago, a GP in another town gave Jenny antibiotics for pneumonia. Jenny has had no other hospital admissions or surgical procedures.
Epidemiology and population at risk
Cough is the most common pediatric problem managed by FPs, and it is more common in preschool children than in older children.2 Two out of 3 children aged between 0 and 4 years visit their FPs at least once a year with acute respiratory infections, and up to three-quarters of them will have coughs.3,4 Most coughs are caused by acute viral infections, and 7% to 12% of coughs are due to asthma; all other causes are rare.5 In Australia 11.4% of child coughs were due to asthma, and only 1.2% were caused by pneumonia6; in Dutch general practice, only 1.9% of coughs were due to pneumonia.7 With the exception of 0.3% due to whooping cough, all other coughs were the result of acute viral infections. Most coughs in children are caused by undifferentiated acute respiratory tract infections—a cough that does not conform to any clear diagnostic syndrome such as croup, whooping cough, pneumonia, or bronchiolitis.8
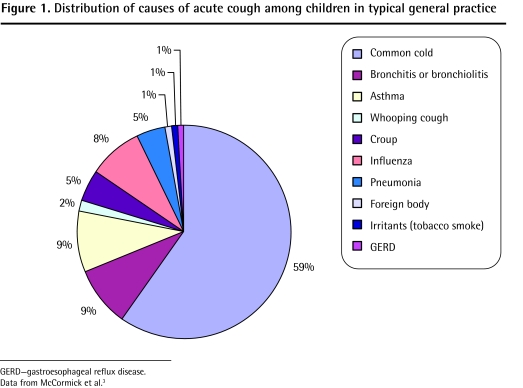
As with adults, children’s cough, whether described as a symptom of “upper respiratory tract infection” or “acute bronchitis,” is the most frequently managed acute presentation in primary care. These 2 diagnoses represent at least 75% of all coughs seen. Of the other causes, asthma is the most common; other, potentially dangerous, causes are much less common (Figure 1).3
Figure 1.
Distribution of causes of acute cough among children in typical general practice
GERD—gastroesophageal reflux disease.
Data from McCormick et al.3
As Jenny is an otherwise healthy child and is not taking any respiratory medicines, it is probable that her cough is due to an acute viral infection, probably picked up in the day-care centre; her mother’s description of a “barky” cough makes you wonder whether she might have croup.
Before you examine her, you consider what else it could be.
What else could it be?
Figure 13 shows that, overwhelmingly, acute coughs in children are due to acute viral infections (common colds, acute bronchitis, croup, and influenza). Although there is usually no need to be concerned with the chronic respiratory and cardiac conditions that affect some adults, acute cough can be indicative of conditions that the physician should not miss, such as asthma, bronchiolitis, whooping cough, pneumonia, and foreign body aspiration. A brief focused history will usually give information about such conditions.
Alarm symptoms
If there were an epidemic at the day-care centre, Mrs Jones would have been informed. Jenny’s immunization record will influence the chances of whooping cough or Haemophilus influenzae infection. A sudden history of choking will point to aspiration of a foreign body or exposure to toxic irritants. Mrs Jones should know if Jenny has been exposed to any irritants. What time of year is it? Peak incidence of infective cough is January to March; epidemics of croup tend to occur in autumn and bronchiolitis in winter.
Alarm signs
The child will look ill (with pneumonia or influenza) or be short of breath with tachypnea (with asthma or foreign body aspiration). The child will be working hard to breathe, perhaps with chest retractions. There might be a high fever (with pneumonia, but some children can run sudden high fevers with otherwise innocuous viral infections).
Jenny looks quite well to you. She is not running a fever and she is not short of breath. Her respiratory rate is 20 breaths/min; her pulse is 96 beats/min; and her temperature is 37.4°C. She has a runny nose, but her ears and throat are unremarkable. Her chest is clear. During the 15 minutes she is in your office, she coughs only once; the cough is dry and barky, but not spasmodic; the child barely seems to notice it, although Mrs Jones jumps. No alarm symptoms or signs are present.
Mrs Jones says Jenny has received pertussis, Haemophilus, and influenza vaccines, according to the schedules. Jenny is too old to have bronchiolitis. Mrs Jones admits to smoking 15 cigarettes per day at home.
You make a presumptive diagnosis of mild croup, following a viral upper respiratory tract infection, which is now recovering.
How sure of the diagnosis are you?
Most childhood respiratory tract infections are diagnosed based on history and examination alone. This is true for croup, which is associated with the same micro-organisms as the common cold. The barking cough of croup and the paroxysms of whooping cough are classic and easy to recognize,9 as is the wheeze in infants with bronchiolitis. Knowledge of the child’s vaccination status can help; clearly whooping cough and influenza are less common in children who have been immunized against these illnesses.
Much about the diagnosis of acute bronchitis in children is uncertain. A chart review of children in the United States with cough showed that GPs were more likely to diagnose acute bronchitis if there was sputum production (odds ratio [OR] = 25), rales or rhonchi on examination (OR = 12), or a past history of lower respiratory tract infection (OR = 3); the presence of fever and the duration of illness were not associated with the diagnosis.10
Unfortunately, there is little good quantitative evidence that will enable practitioners to estimate the likelihood of serious illness, in numerical ways, as there is for adults with acute cough.
Both doctors and parents worry that a coughing child might have pneumonia. Several studies have developed ways to rule out pneumonia: in the absence of tachypnea and chest retractions,11 if the respiratory rate is normal, auscultation is clear, and the child is not working hard to breathe, findings from chest radiographs are unlikely to be positive for pneumonia.12
If you are worried that the child might get sicker, you can teach the parents to observe for fast breathing, chest retractions, and wheezing as danger signs.13
You have decided that there are no symptoms or signs that point to a serious respiratory illness and you decide that Jenny can be safely treated at home. You advise Mrs Jones of this, and that a chest x-ray scan is not needed. You tell Mrs Jones that complete and speedy recovery is to be expected, but that a small proportion of children develop complications.
Is it likely to get worse?
Up to 12% of children with cough experience complications,14 and although the complications are usually mild and easily treated, some children do become very sick. Otitis media is the most common complication, followed by rash, diarrhea, and vomiting; only 5% of cases progress to bronchitis or pneumonia. Unfortunately, there is a paucity of information regarding the predictive value of signs and symptoms in children with cough.
The only study in primary care that looks at this is British15; only the presence of fever and chest signs were independently associated with complications (although presence of asthma and tachypnea initially produced high ORs, their 95% confidence intervals crossed 1.0). While children with neither fever nor chest signs had a posttest probability of complications of only 6%, for children with chest signs it was 18%, with fever it was 28%, and when both fever and chest signs were present the posttest probability was 40% (Table 1).15
Table 1.
Odds ratios for predicting complications after acute childhood cough
| SIGNS AND SYMPTOMS | POSITIVE ODDS RATIO | NEGATIVE ODDS RATIO |
|---|---|---|
| Added chest signs | 2.78 | 1.0 |
| Fever | 4.65 | 1.0 |
| Tachypnea | 3.80 | 1.0 |
| Attends day care | 1.0 | NA |
| Illness severity | 1.34 | NA |
| Lives with smoker | 1.0 | NA |
| Social deprivation | 1.0 | NA |
| Known to have asthma | 2.90 | NA |
NA—not applicable.
Data from Hay et al.15
Croup is a self-limiting illness. Only about 4% of children with croup need to be hospitalized, and only 1 in 4500 children with croup gets ill enough to require intubation.16
You tell Mrs Jones that it is very unlikely that Jenny will get worse or have any complications. If Jenny does get worse, she can come back to see you without making an appointment.
How long will the cough last?
Most children with croup are only mildly ill, and their croupy symptoms resolve within 48 hours. The cough might persist, however. Both clinicians and parents tend to underestimate how long acute cough in children will take to completely resolve. Prospective cohort studies have found that not until 10 days after onset have 50% of children with coughs recovered, and 10% of children are still coughing at 25 days.17
You tell Mrs Jones that the cough might be gone in a week, but that it would not be unusual for it to last for 2 to 3 weeks longer.
What does the parent expect?
As an FP you will also rely on your knowledge of the mother’s consulting patterns for the child’s past illnesses. A British study18 of mothers who consulted their FPs because their children had been coughing found that one of the main concerns mothers had was that their children were going to die because of choking on phlegm or vomit; they were also worried about asthma and crib death. Some mothers also worried that their children would develop long-term chest damage. Mothers themselves had been affected by sleep deprivation because of their worries about their children. First-time mothers and mothers with lower levels of education are more likely to consult their physicians.19
Several studies have found that if the parent expects to receive an antibiotic prescription, or the physician believes that the parent expects one, there is an increased likelihood that such a prescription will be written; this effect is second only to the presence of added respiratory sounds as a predictor of antibiotic prescription.20 On the other hand, if the parent thinks the child has a viral respiratory tract infection, the child is only half as likely to receive antibiotics.
You ask Mrs Jones what she was expecting would be the diagnosis and treatment for Jenny’s cough.
She says she was worried that Jenny might be developing pneumonia again; she is very relieved to hear that there is no sign of this. She understands that croupy coughs usually sound worse than they really are, and that a 4-year-old is in no real danger. She doesn’t really know what the treatment for croup is, but she remembers Jenny has taken antibiotics 3 times before.
Deciding on the best treatment
Evidence-based guidelines have shown that there are no effective medications to either cure or relieve the symptoms of acute cough in children.1,9 Once the FP has confidently excluded the rarer and more serious conditions for which therapy is effective, explanation is required for the parent.
Antibiotics have no effect on viral infections; indeed they might cause side effects that are more distressing than the cough. Most parents will not be too concerned about increasing antibiotic resistance; however, most should be told that antibiotics are at least as likely to cause side effects as they are to produce improvement in their children. They should also be told that serious adverse events and accidental poisonings have been recorded in children from exposures to over-the-counter medications.21
There is good evidence that oral corticosteroids are an effective treatment for moderate to severe croup22,23; they reduce symptom severity, illness duration, and return visits to the doctor. Unfortunately, all the corticosteroid trials have been done in hospital wards or children’s hospital emergency departments; it is not certain whether steroids would be of clinically significant benefit for the milder types of croup seen and managed entirely by GPs.
Mrs Jones accepts your explanation that an antibiotic is not needed for self-limiting croup. She understands that it is too late in the illness for steroid therapy. She mentions that she has already been giving Jenny a children’s cough syrup twice a day and at bedtime. You explain that the cough syrup is probably having no effect; she agrees that it doesn’t seem to be working. You mention that her second-hand smoke might be exacerbating the cough; she agrees to smoke outside while Jenny is ill.
When should I bring my child back?
There is little need for most children with acute cough to be seen more than once. However, FPs know that some parents will need to be seen for further reassurance. Most parents will need to be told to return if the cough does not improve in a certain time (which is longer than most parents think). All parents should be told, or should understand, that they can come back any time if they observe or fear their children are getting worse.
You tell Mrs Jones that Jenny will almost certainly continue to get better. Knowing her anxieties, you agree to check Jenny again in 3 days to judge whether she is fit enough to resume day care.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
Competing interests
None declared
References
- 1.Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):1S–23S. doi: 10.1378/chest.129.1_suppl.1S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morrell DC. Symptom interpretation in general practice. J R Coll Gen Pract. 1972;22(118):297–309. [PMC free article] [PubMed] [Google Scholar]
- 3.McCormick A, Fleming D, Charlton J. Morbidity statistics from general practice—fourth National Morbidity Survey, 1991–92. London, UK: HMSO, Office for National Statistics; 1995. [Google Scholar]
- 4.Hope-Simpson RE, Miller DL. The definition of acute respiratory illnesses in general practice. Postgrad Med J. 1973;49(577):763–70. doi: 10.1136/pgmj.49.577.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayres JG, Noah ND, Fleming DM. Incidence of episodes of acute asthma and acute bronchitis in general practice 1976–87. Br J Gen Pract. 1993;43(374):361–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Meza RA, Bridges-Webb C, Sayer GP, Miles DA, Traynor V, Neary S. The management of acute bronchitis in general practice: results from the Australian Morbidity and Treatment Survey, 1990–1991. Aust Fam Physician. 1994;23(8):1550–3. [PubMed] [Google Scholar]
- 7.Verheij TJ, Kaptein AA, Mulder JD. Acue bronchitis: aetiology, symptoms and treatment. Fam Pract. 1989;6(1):66–9. doi: 10.1093/fampra/6.1.66. [DOI] [PubMed] [Google Scholar]
- 8.Davy T, Dick PT, Munk P. Self-reported prescribing of antibiotics for children with undifferentiated acute respiratory tract infections with cough. Pediatr Infect Dis J. 1998;17(6):457–62. doi: 10.1097/00006454-199806000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Chang AB, Landau LI, Van Asperen PP, Glascow NJ, Robertson CF, Marchant JM, et al. Cough in children: definitions and clinical evaluation. Med J Aust. 2006;184(8):398–403. doi: 10.5694/j.1326-5377.2006.tb00290.x. [DOI] [PubMed] [Google Scholar]
- 10.Vinson DC. Acute bronchitis in children: a clinical definition. Fam Pract Res J. 1991;11(1):75–81. [PubMed] [Google Scholar]
- 11.Shamo’on H, Hawamdah A, Haddadin R, Jmeian S. Detection of pneumonia among children under six years by clinical examination. East Mediterr Health J. 2004;10(4–5):482–7. [PubMed] [Google Scholar]
- 12.Margolis P, Gadomski A. The rational clinical examination. Does this child have pneumonia? JAMA. 1998;279(4):308–13. doi: 10.1001/jama.279.4.308. [DOI] [PubMed] [Google Scholar]
- 13.Gadomski AM, Aref GH, Hassanian F, el Ghandour S, el-Mougi M, Harrison LH, et al. Caretaker recognition of respiratory signs in children: correlation with physical examination signs, x-ray diagnosis and pulse oximetry. Int J Epidemiol. 1993;22(6):1166–73. doi: 10.1093/ije/22.6.1166. [DOI] [PubMed] [Google Scholar]
- 14.Hay AD, Wilson AD. The natural history of acute cough in children aged 0 to 4 years in primary care: a systematic review. Br J Gen Pract. 2002;52(478):401–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Hay AD, Fahey T, Peters TJ, Wilson A. Predicting complications from acute cough in pre-school children in primary care: a prospective cohort study. Br J Gen Pract. 2004;54(498):9–14. [PMC free article] [PubMed] [Google Scholar]
- 16.Marx A, Török TJ, Holman RC, Clarke MJ, Anderson LJ. Pediatric hospitalization for croup (laryngotracheobronchitis): biennial increases with human parainfluenza virus 1 epidemics. J Infect Dis. 1997;176(6):1423–7. doi: 10.1086/514137. [DOI] [PubMed] [Google Scholar]
- 17.Hay AD, Wilson A, Fahey T, Peters TJ. The duration of acute cough in pre-school children: a prospective cohort study. Fam Pract. 2003;20(6):696–705. doi: 10.1093/fampra/cmg613. [DOI] [PubMed] [Google Scholar]
- 18.Cornford CS, Morgan M, Ridsdale L. Why do mothers consult when their children cough? Fam Pract. 1993;10(2):193–6. doi: 10.1093/fampra/10.2.193. [DOI] [PubMed] [Google Scholar]
- 19.Dewey CR, Hawkins NS. The relationship between the treatment of cough during early infancy and the maternal education level, age and number of other children in the household. ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. Child Care Health Dev. 1998;24(3):217–27. doi: 10.1046/j.1365-2214.1998.00067.x. [DOI] [PubMed] [Google Scholar]
- 20.Vinson DC, Lutz LJ. The effect of parental expectations on treatment of children with cough: a report from ASPN. J Fam Pract. 1993;37(1):23–7. [PubMed] [Google Scholar]
- 21.Gunn VL, Taha SH, Liebelt EL, Serwint JR. Toxicity of over-the-counter cough and cold medicines. Pediatrics. 2001;108(3):E52. doi: 10.1542/peds.108.3.e52. [DOI] [PubMed] [Google Scholar]
- 22.Kairys SW, Olmstead EM, O’Connor GT. Steroid treatment of laryngotracheitis: a meta-analysis of the evidence from randomised trials. Pediatrics. 1989;83(5):683–93. [PubMed] [Google Scholar]
- 23.Ausejo M, Saentz A, Pham B, Moher D, Chalmers TC, Kellner JD, et al. The effectiveness of glucocorticoids in treating croup: a meta analysis. West J Med. 1999;171(4):227–32. [PMC free article] [PubMed] [Google Scholar]