Abstract
Objective
To measure physicians’ experiences with opioid-related adverse events and their perceived level of confidence in their opioid prescribing skills and practices.
Design
Mailed survey.
Setting
The province of Ontario.
Participants
A total of 1000 primary care physicians randomly selected from the College of Physicians and Surgeons of Ontario registration database.
Main outcome measures
Opioid-related adverse events and concerns (eg, number of patients, type of opioid, cause of the event or concern); physicians’ confidence, comfort, and satisfaction with opioid prescribing; physicians’ opinions on strategies to optimize their prescribing; and physicians’ perspectives of their interactions with pharmacists and nurses.
Results
The response rate was close to 66%, for a total of 658 participants. Almost all respondents reported prescribing opioids for chronic pain in the past 3 months. Eighty-six percent of respondents reported being confident in their prescribing of opioids, but 42% of respondents indicated that at least 1 patient had experienced an adverse event related to opioids in the past year, usually involving oxycodone, and 16.3% of respondents did not know if their patients had experienced any opioid-related adverse events. The most commonly cited factors leading to adverse events were that the patient took more than prescribed, the prescribed dose was too high, or the patient took alcohol or sedating drugs with the opioids. Most physicians had concerns about the opioid use of 1 or more of their patients; concerns included running out of opioids early, minimal access to pain and addiction treatment, and addiction and overdose. The reported number of physicians’ patients taking opioids was positively associated with their confidence and comfort levels in opioid prescribing and negatively associated with their belief that many patients become addicted to opioids.
Conclusion
Most physicians have encountered opioid-related adverse events. Comprehensive strategies are required to promote safe prescribing of opioids, including guidelines and comprehensive office-system materials.
Résumé
Objectif
Évaluer les cas d’effets indésirables liés aux opiacés qu’ont connus les médecins ainsi que la confiance qu’ils estiment avoir en leur habileté et leur façon de prescrire les opiacés.
Type d’étude
Enquête postale.
Contexte
La province d’Ontario.
Participants
Un total de 1000 médecins de première ligne choisis au hasard à partir de la base de données des inscriptions au Collège des médecins et chirurgiens de l’Ontario.
Principaux paramètres à l’étude
Effets indésirables et inquiétudes liés aux opiacés (c.-à-d. nombre de patients, type d’opiacé, cause de l’effet indésirable ou de l’inquiétude); confiance, confort et satisfaction des médecins par rapport à la prescription d’opiacés; leur opinion sur des stratégies pour optimiser leur façon de prescrire; et vision des médecins concernant leurs interactions avec les pharmaciens et les infirmières.
Résultats
Il y a eu 685 participants, pour un taux de réponse de près de 66 %. Presque tous les participants ont déclaré avoir prescrit des opiacés pour des douleurs chroniques au cours des 3 derniers mois. Parmi eux, 86 % se disaient confiants dans leur façon de prescrire les opiacés, mais 42 % indiquaient qu’au moins 1 de leurs patients avait eu un effet indésirable lié aux opiacés au cours de la dernière année, généralement avec l’oxycodone, et 16,3 % des répondants ignoraient si leurs patients avaient eu des effets indésirables liés aux opiacés. Les causes d’effets indésirables les plus souvent mentionnées étaient que le patient prenait plus du médicament que ce qui était prescrit, que la dose prescrite était trop élevée, ou que le patient prenait de l’alcool ou des sédatifs avec les opiacés. La plupart des médecins étaient inquiets de la consommation d’opiacés d’au moins un de leurs patients; les causes d’inquiétudes comprenaient le fait de manquer d’opiacés trop rapidement, l’accès insuffisant aux traitements de la douleur et de la dépendance, et la dépendance et la surdose. Le nombre de patients d’un médecin qui prenaient des opiacés était directement relié aux niveaux de confiance et de confort du médecin dans la prescription d’opiacés, et inversement relié à sa crainte que plusieurs patients développent une dépendance.
Conclusion
La plupart des médecins ont fait face à des effets indésirables liés aux opiacés. Des stratégies globales doivent être instaurées pour favoriser une prescription d’opiacés sécuritaire, incluant des directives et de la documentation pour le bureau.
Opioid prescribing in Canada has increased dramatically in the past 10 years, accompanied by a marked increase in prescription opioid misuse and addiction. A national study1 found that most people who inject opioids in Canada are now injecting prescription opioids such as morphine (54%) and hydromorphone (50%) rather than street-derived heroin (42%). North America has seen a dramatic increase in visits to the emergency department, hospitalizations, and deaths from prescription opioid overdose.2–7
Previous surveys of North American physicians have documented varying levels of comfort and confidence in prescribing opioids. Both American and Canadian surveys found that primary care physicians were concerned that opioid prescribing would cause or contribute to addiction.8–11 To our knowledge, however, previous surveys have not attempted to measure the type, frequency, and causes of opioid-related adverse events, factors contributing to adverse events, or physicians’ specific concerns about patients taking opioids. A more nuanced understanding of these events and concerns could help in planning educational interventions. For example, if physicians are concerned that their opioid prescriptions are contributing to overdose or addiction, then educational events should focus on strategies to mitigate these risks, such as careful dose titration, prescribing cautions with benzodiazepines, and methadone or buprenorphine treatment of opioid addiction.12–14
This survey was part of a larger research project designed to develop and evaluate an interprofessional education program to improve the safety of opioid use in community settings. The first phase of this research was to conduct a needs assessment survey for physicians, pharmacists, and nurses. Here we report the findings of the assessment of physician needs. The objectives of the assessment were to categorize opioid-related adverse events (eg, by number of patients, type of opioid, cause of the event), the number of patients for whom physicians had concerns, and the nature of physicians’ concerns. We also wanted to measure physicians’ confidence, comfort, and satisfaction with opioid prescribing, their opinions on strategies to optimize their prescribing, and their interactions with pharmacists and nurses.
METHODS
Questionnaire design
The questionnaire (which is available on CFPlus*) asked about physicians’ confidence, comfort, satisfaction, and expectations of a positive outcome when prescribing opioids for chronic pain. The questions were based on attitudinal questions that are frequently used in surveys about physician attitudes and practices.9,15–20 Research suggests that these attitudes are associated with physicians’ willingness to prescribe opioids.10,11,16,21 The questionnaire was pretested on 10 family medicine residents at St Joseph’s Health Centre in Toronto, Ont. A fax-back method was adopted, using a modified Dillman procedure.22 A total of 2 reminders were sent to the physicians invited to participate.
Sample selection
One thousand physicians were randomly selected from the College of Physicians and Surgeons of Ontario (CPSO) registration database. Criteria for inclusion in the random selection pool included having an active, independent practice licence; having a primary practice address in Ontario; having Certification with the College of Family Physicians of Canada or being registered as a general practitioner; and indicating on the annual CPSO membership renewal survey that 40% of the practice comprised general or family practice activities, with or without active or admitting hospital privileges. These selection criteria were established to ensure that only family physicians or general practitioners with primary care practices were included in the sample, as opposed to those with focused practices (eg, psychotherapy or sports medicine).
Ethics
To protect the anonymity of the respondents, all contact with physicians was made by the CPSO, the list of physicians contacted was not released to the research team by the CPSO, and the survey responses were returned directly to the research team with no physician identifiers. Ethics approval was granted by the Centre for Addiction and Mental Health Ethics Review Board. The study was funded by the Canadian Patient Safety Institute.
Analysis
Descriptive analyses of the survey results are reported. Simple measures of association, such as rank order correlation testing (using the Spearman rank correlation coefficient [ρ]), were used to determine the relationships between volume of patients with chronic pain and opioid prescribing beliefs and behaviour as well as the relationship between physician confidence in their prescribing skills and their concerns about patient safety.
RESULTS
Respondent demographics
From the 1000 sample physicians who were sent the questionnaire, 658 (65.8%) responded. Respondent ages ranged from 27 to 83 years, with a mean age of 52.2 years. Years in practice ranged from 1 to 61 years, with a mean of 26.8 years in practice. Age and years in practice were highly correlated (ρ = 0.95, P < .001). Male physicians represented 65.7% of the respondent population. Male physicians were significantly older than female physicians (54.9 years vs 46.8 years, P < .001). Most (79.4%) respondents practised in larger urban centres with populations of more than 30 000 people.
The respondent population was comparable in age and sex distribution to that found in the total sample population of 1000 physicians, minimizing our concern of nonresponse bias. The mean age of physicians in the sample population was 50.0 years compared with 52.2 years in the respondent population. Women made up 36.5% of the sample population, whereas 34.3% of respondents were women. Compared with the 2007 average Ontario physician population, the respondent population was slightly older (52.2 years compared with 51.2 years) and had a marginally higher proportion of female physicians (34.3% compared with 32.1%).23 Compared with the overall population of Canadian family physicians, the respondents were slightly older (mean age 52.2 years vs 49.3 years across Canada) and comprised fewer women than are found nationally (34.3% female respondents vs 41.8% female physicians across Canada).24 The respondent population was comparable to the national population with respect to the urban-rural distribution.25
Opioid prescribing volume
Of the 658 participating physicians, 651 responded to questions about their opioid prescribing volume in the past 3 months. Almost all physicians reported prescribing opioids within the past 3 months (95.4%). The median numerical range of patients receiving prescriptions was 6 to 10 (26.4%); 36.4% of respondents had prescribed opioids to 11 or more patients. Reasons for not prescribing opioids in the past 3 months included choosing not to provide this service (n = 6), having no patients with chronic pain (n = 9), being concerned about opioid misuse and addiction (n = 9), and having a licence restriction (n = 1). No physicians cited uncertainty about the efficacy of opioids as a reason for not prescribing them.
Comfort, confidence, efficacy, and concerns
Physicians’ levels of comfort and confidence in their prescribing skills are reported in Table 1. Briefly, 75.1% and 86.4% of the respondents indicated that they strongly or somewhat agreed with the statements “I am comfortable prescribing opioids for pain” and “I am confident in my clinical skills in prescribing opioids,” respectively. A large proportion of respondents somewhat or strongly agreed that “many patients experience substantial relief with opioids” and “many patients function better with opioids” (92.1% and 86.3%, respectively); 57.2% agreed that “many patients become addicted to opioids.” Physicians who strongly or somewhat agreed that their patients might become addicted to opioids were significantly older (t = −3.107, P = .002) than those who disagreed.
Table 1.
Physicians’ levels of comfort and confidence with prescribing opioids
| STATEMENT | NO. OF RESPONDENTS | STRONGLY AGREE, % | SOMEWHAT AGREE, % | SOMEWHAT DISAGREE, % | STRONGLY DISAGREE, % |
|---|---|---|---|---|---|
| I am comfortable prescribing opioids for chronic pain | 643 | 24.7 | 50.4 | 17.7 | 7.2 |
| I am confident in my clinical skills in prescribing opioids | 639 | 30.7 | 55.7 | 11.1 | 2.5 |
| Many pain patients experience substantial pain relief with opioids | 638 | 40.8 | 51.3 | 6.7 | 1.3 |
| Many pain patients function better with opioids | 633 | 35.9 | 50.4 | 10.4 | 3.3 |
| Many pain patients become addicted to opioids | 631 | 23.8 | 33.4 | 30.9 | 11.9 |
| I find it satisfying to prescribe opioids to pain patients | 630 | 7.1 | 36.7 | 37.9 | 18.3 |
Adverse events and patient concerns
Of the 640 physicians responding to questions about adverse events, 42.0% indicated that no patients had had adverse events in the past year; 9.7% had 1 patient, 12.5% had 2 patients, 6.9% had 3 patients, and 12.7% had 4 or more patients who had had opioid-related adverse events in the past year; and 16.3% did not know whether any patients had experienced adverse events. The opioid most commonly cited as being involved in the most recent adverse event was oxycodone (n = 93), followed by codeine (n = 41) and morphine (n = 39). The most commonly cited factor believed to contribute to the adverse event was that the “patient took more than prescribed” (n = 88), followed by “prescribed dose was too high” (n = 48) and “patient took alcohol or sedating drugs along with opioids” (n = 39). Other factors included patient misunderstanding about dosing (n = 24) and the patient not contacting the physician about symptoms (n =32). Further details are presented in Table 2.
Table 2.
Factors contributing to adverse events due to opioids: N = 268.*
| FACTOR | N |
|---|---|
| Patient took more than prescribed | 88 |
| Prescribed dose was too high | 48 |
| Patient took alcohol or sedating drugs along with opioids | 39 |
| Patients did not contact the physician or pharmacist about symptoms | 32 |
| Patient or caregiver misunderstanding about dosing | 24 |
| Patient injected, crushed, or snorted the tablet | 12 |
| Loss of tolerance following a period of noncompliance | 9 |
| Physician, pharmacist, or nurse did not take into account that the patient was at high risk of overdose (eg, elderly) | 8 |
| Lack of communication between physician and pharmacist or nurse | 6 |
| Physician, pharmacist, or nurse involved did not recognize seriousness of symptoms | 5 |
| Patient refused to go to the emergency department | 1 |
| Dispensing error | 1 |
Some physicians indicated more than 1 factor.
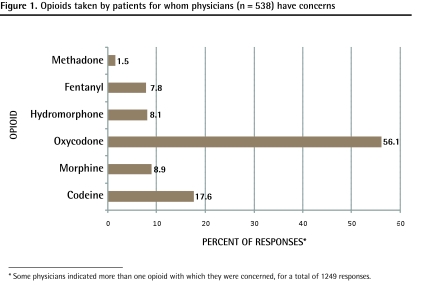
Approximately 15% of physicians had no current concerns about the opioid use of any of their patients, while 84.9% (550 of the 648 who responded to this question) were concerned about at least 1 patient. Of the doctors who were concerned, most (47.9%) were concerned about 1 to 3 patients. Of those patients, more than half (56.1%) were prescribed oxycodone (Figure 1).
Figure 1.
Opioids taken by patients for whom physicians (n = 538) have concerns
* Some physicians indicated more than one opioid with which they were concerned, for a total of 1249 responses.
With respect to opioid prescribing, respondents were most concerned about patients running out of medication early, demanding fit-in appointments, or losing prescriptions, with 71.0% indicating that they were either somewhat or very concerned (Table 3). Many respondents (70.5%) indicated that they were somewhat or very concerned about causing an addiction by prescribing opioids, and many were concerned about the lack of addiction treatment resources (59.4%) and specialized pain clinics (69.7%). Other frequent concerns were patients taking high doses (59.4%), disagreements with patients (57.6%), and overdose (44.0%). One-third (36.7%) of respondents were somewhat or very concerned about getting into trouble with regulatory authorities.
Table 3.
Level of concern about negative opioid prescribing outcomes
| OUTCOME | NO. OF RESPONDENTS | NOT AT ALL CONCERNED, % | A LITTLE CONCERNED, % | SOMEWHAT CONCERNED, % | VERY CONCERNED, % |
|---|---|---|---|---|---|
| Patient addiction | 641 | 4.1 | 25.4 | 32.1 | 38.4 |
| Getting into trouble with the CPSO | 632 | 32.0 | 31.3 | 23.4 | 13.3 |
| Patient noncompliance | 622 | 19.6 | 31.7 | 32.5 | 16.2 |
| Patients running out early, demanding fit-in appointments, or losing prescriptions | 634 | 9.6 | 19.4 | 26.2 | 44.8 |
| Overdose | 639 | 15.8 | 40.2 | 25.2 | 18.8 |
| Lack of addiction treatment resources | 637 | 15.7 | 25.0 | 33.0 | 26.4 |
| Lack of specialized pain clinics | 637 | 12.6 | 17.7 | 27.5 | 42.2 |
| Disagreements with patients about opioids | 640 | 11.7 | 30.6 | 35.6 | 22.0 |
| Patients getting high doses | 636 | 11.5 | 29.1 | 31.4 | 28.0 |
CPSO—College of Physicians and Surgeons of Ontario.
Education and resources
More than half of respondents (n = 360, 54.7%) indicated that they had participated in educational events on opioids for treatment of chronic non-malignant pain in the previous year. Of those who did participate in educational activities, 62.2% participated in pharmaceutical-sponsored dinners or workshops, 51.7% read journal articles, 44.7% attended presentations at conferences or hospitals, 20.3% read pharmaceutical publications, and 11.1% participated in some other educational activity.
Most respondents rated the following strategies as very or somewhat helpful in managing opioid therapy (Table 4): access to a provincial database of patients’ prescriptions (77.5%); guidelines for management of high-risk patients (86.6%); office materials, such as patient information (76.2%); a quick-reference pocket guide (71.0%); and CPSO guidelines on opioid prescribing (75.5%).
Table 4.
Rating of strategies to help manage chronic pain patients taking opioids
| STRATEGY | NO. OF RESPONDENTS | NOT AT ALL HELPFUL, % | SLIGHTLY HELPFUL, % | SOMEWHAT HELPFUL, % | VERY HELPFUL, % |
|---|---|---|---|---|---|
| Toll-free help line | 596 | 23.8 | 23.5 | 31.0 | 21.6 |
| Quick-reference pocket guide on opioid prescribing | 613 | 8.8 | 20.2 | 37.4 | 33.6 |
| One-day course on opioid prescribing | 612 | 7.7 | 20.6 | 41.7 | 30.1 |
| Access to provincial database of patients’ prescriptions | 613 | 8.6 | 13.9 | 25.0 | 52.5 |
| Online prescribing course | 605 | 20.5 | 28.9 | 32.6 | 18.0 |
| CPSO guidelines on opioid prescribing | 621 | 5.0 | 19.5 | 42.5 | 33.0 |
| Guidelines for management of high-risk patients | 618 | 2.3 | 11.2 | 39.2 | 47.4 |
| Office materials, such as treatment agreements and patient information | 615 | 5.4 | 18.4 | 39.0 | 37.2 |
| Website with clinical information | 608 | 12.5 | 25.2 | 38.2 | 24.2 |
| Physician mentor who can be contacted by telephone or e-mail | 614 | 15.8 | 28.2 | 31.9 | 24.1 |
CPSO—College of Physicians and Surgeons of Ontario.
Interprofessional interactions
Most responding physicians (73.9%) indicated that they had interacted with pharmacists in the past year regarding opioid therapy and prescriptions. In contrast, only 36.2% reported interacting with nurses about opioid therapy. The most frequent contacts between physicians and pharmacists involved verification of, or changes to, prescription wording, with 59.1% and 58.3% of respondents indicating that this occurred sometimes or frequently (Table 5). Almost all respondents (97.0%) indicated that pharmacists adequately answered their questions or addressed concerns regarding opioids. In addition, 86.8% of respondents indicated that pharmacists were knowledgeable about opioids and 84.2% agreed that they were not difficult to reach directly. The overall responses regarding nurse-physician interactions were positively skewed—28.8% of respondents indicated that nurses sometimes or frequently pressed them to prescribe benzodiazepines or analgesics for patients to keep them calm or quiet (Table 5); 17.2% of respondents indicated that they sometimes or frequently disagreed when nurses thought a patient displayed drug-seeking behaviour or was difficult; and 16.0% of respondents indicated that they sometimes or frequently felt that a nurse’s assessment of intoxication, withdrawal, or pain was inaccurate.
Table 5.
Nature of interprofessional encounters regarding prescription opioids in the past 3 months
| NATURE OF ENCOUNTER | NO. OF RESPONDENTS | NOT AT ALL, % | SOMETIMES, % | FREQUENTLY, % |
|---|---|---|---|---|
| Pharmacists | ||||
| • Pharmacist was difficult to reach directly by telephone | 494 | 84.2 | 13.4 | 2.4 |
| • Pharmacist challenged a prescription I felt was appropriate | 493 | 75.9 | 23.3 | 0.8 |
| • Pharmacist made a recommendation to a patient that I thought was inappropriate; then the patient wanted me to prescribe what the pharmacist had suggested | 493 | 78.7 | 19.7 | 1.6 |
| • Pharmacist requested a change in the wording of the prescription | 499 | 41.7 | 51.9 | 6.4 |
| • Pharmacist paged or called for minor issues or nonemergencies | 491 | 62.1 | 33.8 | 4.1 |
| • Pharmacist called to verify something that was already stated on the prescription | 494 | 40.9 | 52.6 | 6.5 |
| • Pharmacist dispensed opioid earlier than the time stated on the prescription | 491 | 88.4 | 10.8 | 0.8 |
| • Pharmacist dispensed medication without a prescription when the physician could not be reached | 494 | 93.9 | 5.9 | 0.2 |
| • Pharmacist did not adequately answer my question or address my concern about opioids | 494 | 97.0 | 3.0 | 0 |
| • Pharmacist did not seem very knowledgeable about opioids | 492 | 86.8 | 12.0 | 1.2 |
| Nurses | ||||
| • Nurse was uncomfortable administering the opioids that I prescribed | 389 | 84.6 | 14.7 | 0.8 |
| • Nurse disagreed with my prescription or medical order | 359 | 91.3 | 8.5 | 0.3 |
| • Nurse felt that the patient was displaying drug-seeking behaviour or was difficult and I did not necessarily agree | 390 | 82.8 | 16.9 | 0.3 |
| • Nurse pressured me to prescribe something to keep the patient calm or quiet, such as benzodiazepines or painkillers | 388 | 71.1 | 26.0 | 2.8 |
| • I did not think that the nurse’s assessment of opioid intoxication, withdrawal, or pain was accurate | 387 | 84.0 | 14.0 | 2.0 |
Opioid prescribing beliefs and behaviour
As the number of pain patients per physician increased, so did the number of patients with adverse events reported in the past year (ρ = 0.546, P < .001). Spearman correlation coefficients indicated that the number of pain patients a physician saw who were prescribed opioids was positively associated with their levels of comfort and satisfaction with opioid prescribing and negatively associated with the belief that many patients become addicted to opioids (comfort: ρ = 0.29, P < .001; satisfaction: ρ = 0.162, P < .001; addiction: ρ = −0.11, P = .008). In addition, increasing numbers of pain patients were associated with higher levels of confidence in opioid prescribing skills (ρ = 0.14, P < .001) and a stronger belief that many patients experience substantial pain relief (ρ = 0.18, P < .001) and better function with opioids (ρ = 0.25, P < .001).
Confidence and comfort with prescribing skills
Physicians who indicated that they somewhat or strongly agreed that they were confident (P = .016) and comfortable (P = .024) with respect to opioid prescribing were significantly younger than those who indicated that they somewhat or strongly disagreed with that statement. Generally speaking, physicians who were comfortable and confident in their prescribing skills were less likely to be concerned about patients getting addicted, getting into trouble with the regulatory authorities, overdoses, lack of resources, disagreements with patients, or patients getting overly high doses (Table 6). The more comfortable physicians were with prescribing opioids, the less helpful they felt a 1-day course on prescribing opioids (ρ = −0.082, P = .045), a toll-free number (ρ = −0.09, P = .031), or CPSO guidelines (ρ = −0.137, P = .001) would be. Similar patterns of correlation were found between improvement of education strategies and increasing physician confidence in their prescribing skills. However, the more confident physicians were in their prescribing skills, the more likely they were to indicate that access to provincial patient prescription databases would be helpful (ρ = 0.088, P = .031).
Table 6.
Physicians’ comfort and confidence with prescribing in relation to potential patient concerns: N=658.
| CONCERN | COMFORTABLE WITH PRESCRIBING | CONFIDENCE IN PRESCRIBING SKILLS | ||
|---|---|---|---|---|
| SPEARMAN ρ | PVALUE | SPEARMAN ρ | PVALUE | |
| Getting patient addicted | −0.381 | < .001 | −0.223 | < .001 |
| Getting into trouble with the CPSO | −0.163 | < .001 | −0.202 | < .001 |
| Noncompliance (eg, missed appointments) | −0.013* | .748* | −0.043* | .288* |
| Running out early, demanding fit-in appointments, losing prescriptions | −0.111 | .006 | −0.099 | .015 |
| Overdose | −0.190 | < .001 | −0.144 | < .001 |
| Lack of addiction treatment resources | −0.162 | < .001 | −0.153 | < .001 |
| Lack of specialized pain clinics | −0.079* | .061* | −0.167 | < .001 |
| Disagreements with patients about opioids | −0.287 | < .001 | −0.203 | < .001 |
| Patients getting high doses | −0.323 | < .001 | −0.213 | < .001 |
CPSO—College of Physicians and Surgeons of Ontario.
Results are not significant.
DISCUSSION
To our knowledge this survey is the first to attempt to quantify physicians’ estimates of the number of patients prescribed opioids for whom they have concerns and the number of opioid-related adverse events their patients experience. These estimates are disturbingly high and suggest an urgent need for educational intervention.
While recognizing the important role of opioids in chronic pain management, respondents were concerned that their prescribing could inadvertently contribute to their patients’ risk of overdose and addiction. Recent evidence suggests that these concerns are legitimate (ie, both medically prescribed and diverted or “street” opioids are involved in overdoses and addiction). For example, among 1095 patients in the Ontario Drug Benefit Program who died of opioid overdose, 56% had received opioid prescriptions within 4 weeks of their deaths.6 Chronic pain patients taking opioids have a dose-related risk of overdose; those taking more than 100 mg of morphine or its equivalent per day have a 9-fold increased risk relative to those taking 20 mg or less (1.8% vs 0.2% annual overdose rate).12 Among opioid-addicted patients admitted to a treatment facility in Toronto, 37% received their opioids primarily from physician prescriptions, 26% from both prescriptions and the street, and only 21% entirely from the street.7 In a national US study of 1408 patients entering treatment for opioid abuse, 79% of male and 85% of female patients were first exposed to opioids through prescriptions for pain relief.26 Safe opioid prescribing will minimize these risks. It will also limit the supply of diverted opioids; the total amount of diverted opioids is directly related to the total amount of prescribed opioids.27
We acknowledge limitations to our study. The survey asked about chronic pain, without excluding cancer or palliative pain; different opioid prescribing protocols apply to palliative patients. The study did not ask respondents about their interest in learning more about specific clinical topics, such as the use of addiction screening tools. Also, it would have been helpful to measure the frequency of urine drug screening and other clinical practices for identifying and managing opioid misuse. Future studies should seek to validate the reliability of perceived levels of confidence in opioid prescribing with actual practice patterns. A qualitative study will be helpful in characterizing more fully physicians’ perspectives of both their concerns and the adverse events the patients experienced.
It is concerning that the respondents’ most common source of education was the pharmaceutical industry. Our survey indicates that physicians would be very receptive to unbiased and evidence-based guidelines and office materials. The response rate for the survey was unusually high for physicians (65.8%), attesting to their interest in this topic. The respondents clearly stated what they needed to prescribe opioids more safely. A provincial prescribing database would help physicians identify and manage patients who misuse opioids. Guidelines and office materials can assist physicians with specific clinical protocols such as opioid titration, the use of treatment agreements and urine drug screening, tapering of benzodiazepines and opioids, and the prevention of overdose in patients at risk of opioid toxicity.
Given the concerns elicited from this survey, as well as emerging evidence of serious public health harms due to opioids, medical organizations must undertake initiatives to promote safe and appropriate opioid prescribing. Some might worry that this will further discourage physicians from prescribing opioids; however, contrary to previous surveys,10 our survey found little evidence of physician reluctance to prescribe opioids. Only 4.6% of respondents had not prescribed opioids for chronic pain within the past 3 months, and most physicians were confident in their prescribing and believed that opioids had an important role to play in chronic pain management.
Furthermore, evidence suggests that education on opioid prescribing and misuse does not discourage physicians from prescribing opioids. A controlled trial and a pre-post study demonstrated that education on managing opioid prescribing and opioid addiction actually increased physicians’ confidence and comfort in opioid prescribing.28,29 Our survey results showed that the number of patients for whom the physicians had prescribed opioids in the past year was positively associated with their confidence and comfort level in prescribing and negatively associated with their concern about addiction.
Conclusion
Most physicians have encountered opioid-related adverse events, including opioid intoxication and misuse. Comprehensive educational strategies are required to promote safe prescribing of opioids. The strategies should emphasize the clinical skills required to identify, prevent, and manage opioid overdose, misuse, and addiction.
EDITOR’S KEY POINTS
Opioid prescribing has increased dramatically throughout North America, accompanied by increases in opioid overdose, misuse, and addiction.
Physicians’ estimates of the number of patients prescribed opioids for whom they have concerns and the number of opioid-related adverse events their patients experience are disturbingly high and suggest an urgent need for educational intervention.
Physician comfort with prescribing opioids is positively associated with how many of their patients are taking opioids and negatively associated with their level of concern over opioid prescribing; however, the number of patients prescribed opioids was also positively associated with the number of patients experiencing adverse events.
Currently, the biggest source of opioid education is the pharmaceutical industry; this survey shows that physicians would be very receptive to unbiased and evidence-based guidelines and office materials, such as treatment agreements, to ensure safe opioid prescribing, increase confidence and comfort with prescribing, and minimize associated risks.
POINTS DE REPÈRE DU RÉDACTEUR
Il y a eu une augmentation dramatique de la prescription d’opiacés en Amérique du Nord, avec une augmentation parallèle des cas de surdose, d’abus et de dépendance aux opiacés.
Le nombre de patients qui reçoivent des opiacés et dont le médecin s’inquiète, et le nombre d’effets indésirables liés aux opiacés observés chez leurs patients atteignent des niveaux préoccupants et révèlent un urgent besoin de formation.
Le niveau de confort d’un médecin dans sa prescription d’opiacés est en relation directe avec le nombre de ses patients qui en reçoivent et en relation inverse avec leur niveau d’inquiétude concernant la prescription d’opiacés : toutefois, le nombre de patients à qui des opiacés étaient prescrits était aussi en relation directe avec nombre de patients ayant eu des effets indésirables.
À l’heure actuelle, la principale source d’information sur les opiacés est l’industrie pharmaceutique; cette enquête démontre que les médecins seraient très réceptifs à des directives impartiales fondées sur des preuves et à de la documentation pour le bureau, comme des ententes de traitement, pour s’assurer de prescrire les opiacés de façon sécuritaire, augmenter leur niveau de confiance et de confort avec ces prescriptions et minimiser les risques associés.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
The survey questionnaire is available at www.cfp.ca. Go to the full text of this article online, then click on cFPlus in the menu at the top right-hand side of the page.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Fischer B, Rehm J, Patra J, Cruz MF. Changes in illicit opioid use across Canada. CMAJ. 2006;175(11):1385. doi: 10.1503/cmaj.060729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drummer OH. Recent trends in narcotic deaths. Ther Drug Monit. 2005;27(6):738–40. doi: 10.1097/01.ftd.0000179853.16846.a9. [DOI] [PubMed] [Google Scholar]
- 3.Mueller MR, Shah NG, Landen MG. Unintentional prescription drug overdose deaths in New Mexico, 1994–2003. Am J Prev Med. 2006;30(5):423–9. doi: 10.1016/j.amepre.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Cicero TJ, Inciardi JA, Muñoz A. Trends in abuse of Oxycontin and other opioid analgesics in the United States: 2002–2004. J Pain. 2005;6(10):662–72. doi: 10.1016/j.jpain.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81(2):103–7. doi: 10.1016/j.drugalcdep.2005.05.009. Epub 2005 Jul 14. [DOI] [PubMed] [Google Scholar]
- 6.Dhalla IA, Mamdani MM, Sivilotti ML, Kopp A, Qureshi O, Juurlink DN. Prescribing of opioid analgesics and related mortality before and after the introduction of long-acting oxycodone. CMAJ. 2009;181(12):891–6. doi: 10.1503/cmaj.090784. Epub 2009 Dec 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sproule B, Brands B, Li S, Catz-Biro L. Changing patterns in opioid addiction: characterizing users of oxycodone and other opioids. Can Fam Physician. 2009;55:68-9.e1–5. Available from: www.cfp.ca/cgi/reprint/55/1/68. Accessed 2011 Feb 7. [PMC free article] [PubMed] [Google Scholar]
- 8.Boulanger A, Clark AJ, Squire P, Cui E, Horbay GL. Chronic pain in Canada: have we improved our management of chronic noncancer pain? Pain Res Manag. 2007;12(1):39–47. doi: 10.1155/2007/762180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobscha SK, Corson K, Flores JA, Tansill EC, Gerrity MS. Veterans affairs primary care clinicians’ attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med. 2008;9(5):564–71. doi: 10.1111/j.1526-4637.2007.00330.x. [DOI] [PubMed] [Google Scholar]
- 10.Morley-Forster PK, Clark AJ, Speechley M, Moulin DE. Attitudes toward opioid use for chronic pain: a Canadian physician survey. Pain Res Manag. 2003;8(4):189–94. doi: 10.1155/2003/184247. [DOI] [PubMed] [Google Scholar]
- 11.Hutchinson K, Moreland AM, de C Williams AC, Weinman J, Horne R. Exploring beliefs and practice of opioid prescribing for persistent non-cancer pain by general practitioners. Eur J Pain. 2007;11(1):93–8. doi: 10.1016/j.ejpain.2006.01.003. Epub 2006 Feb 17. [DOI] [PubMed] [Google Scholar]
- 12.Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cone EJ, Fant RV, Rohay JM, Caplan YH, Ballina M, Reder RF, et al. Oxycodone involvement in drug abuse deaths. II. Evidence for toxic multiple drug-drug interactions. J Anal Toxicol. 2004;28(4):217–25. doi: 10.1093/jat/28.4.217. Corrected and republished in: J Anal Toxicol 2004;28(7):616–24. [DOI] [PubMed] [Google Scholar]
- 14.Caplehorn JR, Dalton MS, Haldar F, Petrenas AM, Nisbet JG. Methadone maintenance and addicts’ risk of fatal heroin overdose. Subst Use Misuse. 1996;31(2):177–96. doi: 10.3109/10826089609045806. [DOI] [PubMed] [Google Scholar]
- 15.Green CR, Wheeler JR, LaPorte F, Marchant B, Guerrero E. How well is chronic pain managed? Who does it well? Pain Med. 2002;3(1):56–65. doi: 10.1046/j.1526-4637.2002.02003.x. [DOI] [PubMed] [Google Scholar]
- 16.Nwokeji ED, Rascati KL, Brown CM, Eisenberg A. Influences of attitudes on family physicians’ willingness to prescribe long-acting opioid analgesics for patients with chronic nonmalignant pain. Clin Ther. 2007;29(Suppl):2589–602. doi: 10.1016/j.clinthera.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Scanlon MN, Chugh U. Exploring physicians’ comfort level with opioids for chronic noncancer pain. Pain Res Manag. 2004;9(4):195–201. doi: 10.1155/2004/290250. [DOI] [PubMed] [Google Scholar]
- 18.Rohman ME, Cleary PD, Warburg M, Delbanco TL, Aronson MD. The response of primary care physicians to problem drinkers. Am J Drug Alcohol Abuse. 1987;13(1–2):199–209. doi: 10.3109/00952998709001509. [DOI] [PubMed] [Google Scholar]
- 19.Lefebvre LG, Ordean A, Midmer D, Kahan M, Tolomiczenko G. Physicians’ knowledge of alcohol, tobacco and folic acid in pregnancy. Subst Abus. 2007;28(1):3–9. doi: 10.1300/J465v28n01_02. [DOI] [PubMed] [Google Scholar]
- 20.Kahan M, Wilson L, Liu E, Borsoi D, Brewster JM, Sobell LC, et al. Family medicine residents’ beliefs, attitudes and performance with problem drinkers: a survey and simulated patient study. Subst Abus. 2004;25(1):43–51. doi: 10.1300/J465v25n01_07. [DOI] [PubMed] [Google Scholar]
- 21.Potter M, Schafer S, Gonzalez-Mendez E, Gjeltema K, Lopez A, Wu J, et al. Opioids for chronic nonmalignant pain. Attitudes and practices of primary care physicians in the UCSF/Stanford collaborative research network. University of California, San Francisco. J Fam Pract. 2001;50(2):145–51. [PubMed] [Google Scholar]
- 22.Dillman DA. Mail and Internet surveys: the tailored design method. 2nd ed. New York, NY: John Wiley Co; 2000. [Google Scholar]
- 23.College of Physicians and Surgeons of Ontario . Reaping the rewards—striving for sustainability. 2007 registration statistics and survey findings. Toronto, ON: College and Physicians and Surgeons of Ontario; 2008. Available from: www.cpso.on.ca/uploadedFiles/policies/positions/resourceinitiative/Reaping%20the%20Rewards%20Survey_07.pdf. Accessed 2011 Jan 26. [Google Scholar]
- 24.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada . National physician survey: 2007 results. Mississauga, ON: College of Family Physicians of Canada; 2007. Available from: www.nationalphysiciansurvey.ca/nps/2007_Survey/2007results-e.asp. Accessed 2011 Jan 26. [Google Scholar]
- 25.Canadian Institute for Health Information . Distribution and internal migration of Canada’s physician workforce. Ottawa, ON: Canadian Institute for Health Information; 2007. Available from: http://secure.cihi.ca/cihiweb/products/2007_phys_EN_web.pdf. Accessed 2011 Jan 26. [Google Scholar]
- 26.Cicero TJ, Lynskey M, Todorov A, Inciardi JA, Surratt HL. Co-morbid pain and psychopathology in males and females admitted to treatment for opioid analgesic abuse. Pain. 2008;139(1):127–35. doi: 10.1016/j.pain.2008.03.021. Epub 2008 May 1. [DOI] [PubMed] [Google Scholar]
- 27.Dasgupta N, Kramer ED, Zalman MA, Carino S, Jr, Smith MY, Haddox JD, et al. Association between non-medical and prescriptive usage of opioids. Drug Alcohol Depend. 2006;82(2):135–42. doi: 10.1016/j.drugalcdep.2005.08.019. Epub 2005 Oct 19. [DOI] [PubMed] [Google Scholar]
- 28.Midmer D, Kahan M, Marlow B. Effects of a distance learning program on physicians’ opioid- and benzodiazepine-prescribing skills. J Contin Educ Health Prof. 2006;26(4):294–301. doi: 10.1002/chp.82. [DOI] [PubMed] [Google Scholar]
- 29.Roth CS, Burgess DJ. Changing residents’ beliefs and concerns about treating chronic noncancer pain with opioids: evaluation of a pilot workshop. Pain Med. 2008;9(7):890–2. doi: 10.1111/j.1526-4637.2008.00458.x. [DOI] [PubMed] [Google Scholar]