Abstract
Objective
To examine whether variation in prescribing at the level of the individual physician is associated with opioid-related mortality.
Design
A population-based cross-sectional analysis linking prescription data with records from the Office of the Chief Coroner.
Setting
The province of Ontario.
Participants
Family physicians in Ontario and Ontarians aged 15 to 64 who were eligible for prescription drug coverage under the Ontario Public Drug Program.
Main outcome measures
Variation in family physicians’ opioid prescribing and opioid-related mortality among their patients.
Results
The 20% of family physicians (n = 1978) who prescribed opioids most frequently issued opioid prescriptions 55 times more often than the 20% who prescribed opioids least frequently. Family physicians in the uppermost quintile also wrote the final opioid prescription before death for 62.7% of public drug plan beneficiaries whose deaths were related to opioids. Physician characteristics associated with greater opioid prescribing were male sex (P = .003), older age (P < .001), and a greater number of years in practice (P < .001).
Conclusion
Opioid prescribing varies remarkably among family physicians, and opioid-related deaths are concentrated among patients treated by physicians who prescribe opioids frequently. Strategies to reduce opioid-related harm should include efforts focusing on family physicians who prescribe opioids frequently.
Résumé
Objectif
Vérifier si le fait pour un médecin donné de faire plus ou moins de prescriptions d’opiacés est associé au nombre de décès lié aux opiacés.
Type d‘étude
Analyse transversale de nature démographique sur le lien entre les données relatives aux ordonnances et les registres du bureau du coroner en chef.
Contexte
La province d’Ontario.
Participants
Médecins de famille d’Ontario et patients ontariens entre 15 et 64 ans qui étaient admissibles au programme de médicaments d’ordonnance conformément à l’Ontario Public Drug Program.
Principaux paramètres à l’étude
Variations, chez les médecins de famille, dans la prescription d’opiacés et les décès reliés aux opiacés parmi leurs patients.
Résultats
Parmi les médecins de famille, les 20 % (n = 1978) qui prescrivaient des opiacés le plus fréquemment en prescrivaient 55 fois plus souvent que les 20 % qui en prescrivaient le moins souvent. Les médecins qui faisaient le plus de prescriptions avaient aussi fait la dernière prescription précédant la mort pour 62,7 % des bénéficiaires du programme public de médicaments dont la mort était reliée aux opiacés. Les caractéristiques des médecins qui faisaient le plus de prescriptions d’opiacés étaient les suivantes : sexe masculin (P = ,003), plus âgés (P < ,001) et plus grand nombre d’années de pratique (P < ,001).
Conclusion
La prescription d’opiacés varie beaucoup entre les médecins de famille, et les décès reliés aux opiacés sont concentrés parmi les patients traités par les médecins qui prescrivent plus souvent des opiacés. Les stratégies pour réduire les dangers associés aux opiacés devraient cibler principalement les médecins qui prescrivent fréquemment des opiacés.
Opioid prescribing and opioid-related mortality have increased dramatically over the past 20 years,1,2 coincident with an increased acceptance of opioids for the treatment of chronic nonmalignant pain.3,4 Along with the contemporaneous increases in opioid prescribing and opioid-related harm, there has also been evidence of considerable regional variation in opioid-related mortality.2 A recent study also indicated that overdose is more common among patients who are prescribed higher daily doses of opioids.5
Whether variation in prescribing at the level of the individual family physician is associated with opioid-related mortality remains unknown. High rates of opioid prescribing might not be associated with a proportionate increase in opioid-related deaths if “high-volume” physicians tend to prescribe opioids more carefully. Conversely, increased opioid prescribing could result in greater opioid-related harm if prescribing quality is unrelated to volume and deaths are proportionate to the number of prescriptions. To investigate this issue, we examined variations in opioid prescribing and opioid-related mortality in Ontario.
METHODS
We performed a population-based cross-sectional analysis among Ontarians aged 15 to 64 on January 1, 2006, who were eligible for prescription drug coverage under the Ontario Public Drug Program, a population in which the prevalence of opioid prescribing is high and in which high-dose prescribing (eg, 200 mg/d of morphine or equivalent) is common.6
We categorized physicians into quintiles according to the rate of their opioid prescribing in 2006. To determine the opioid-prescribing rate for each physician, we divided the number of opioid prescriptions dispensed to public drug plan beneficiaries by the number of public drug plan beneficiaries aged 15 to 64 treated by each physician. We excluded methadone because it is prescribed primarily for opioid addiction rather than pain. We included all opioids prescribed by physicians whose field of practice was either “general practice” or “family practice” in the physician database of the Institute for Clinical Evaluative Sciences. We excluded physicians who practised outpatient palliative care.
We also examined the records of the Office of the Chief Coroner of Ontario to identify deaths related to opioid use.1 The coroner, a licensed physician, ascertains the cause of all deaths that are either sudden and unexpected or unnatural. A postmortem examination, generally including detailed toxicologic testing, is conducted under the authority of the coroner when necessary to determine the cause or manner of death. From these records, we extracted detailed data about deaths in which opioids appeared to play a contributory role. A single abstractor collected data using an encrypted computer database. For each case, the cause and manner of death and the results of toxicologic analysis (including the concentration and specimen type for positive opioid and alcohol results) were recorded. Deaths were deemed to be opioid-related if that was the opinion of the investigating coroner. In almost all instances, this determination was made for 1 of 2 reasons: the toxicologic analysis revealed opioid concentrations sufficiently high to cause death, or the coroner determined that a combination of drugs (including at least 1 opioid present at a clinically significant concentration) collectively resulted in death. If another drug (eg, a cyclic antidepressant) was present at a concentration high enough to cause death and 1 or more opioids were present at levels that could be associated with therapeutic use, the death was not deemed to be related to opioid use. If the abstractor was uncertain whether a death was related to opioid use or not, the file was reviewed by 1 or more physician coinvestigators until consensus was achieved.
For each patient with an opioid-related death in 2006 who received at least 1 prescription for an opioid in the year before death, the final antemortem opioid prescription was assigned to the volume quintile of the prescribing family physician.
To test the hypothesis that the number of deaths increased across prescribing-volume quintiles, we performed a Cochran-Armitage test for trend. We also used bivariate regression to see if particular physician characteristics were associated with higher volumes of opioid prescribing.
This study was approved by the Research Ethics Board of the Sunnybrook Health Sciences Centre in Toronto.
RESULTS
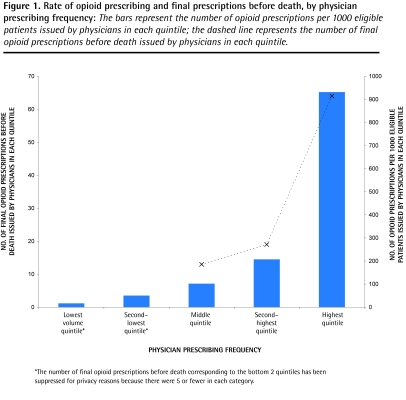
We found marked variation in opioid prescribing. Family physicians in the uppermost quintile (n = 1 978) had an average opioid-prescribing rate of 931.5 per 1000 eligible patients during the study year, while physicians in the lowermost quintile (n = 1 977) had an average opioid prescription rate of 16.7 per 1000 eligible patients (Figure 1). Therefore, physicians in the uppermost quintile had an opioid-prescribing rate 55 times higher than physicians in the lowermost quintile. Although there was an increase in the opioid-prescribing rate between each quintile, the largest increase—a 4.5-fold increase in prescribing rates—was evident between the top 2 quintiles. In bivariate analyses, physician characteristics associated with greater opioid prescribing were male sex (P = .003), older age (P < .001), and a greater number of years in practice (P < .001) (Table 1). The number of patients in a physician’s practice who were eligible for public drug plan coverage was not associated with a higher volume of prescribing (P = .48).
Figure 1.
Rate of opioid prescribing and final prescriptions before death, by physician prescribing frequency: The bars represent the number of opioid prescriptions per 1000 eligible patients issued by physicians in each quintile; the dashed line represents the number of final opioid prescriptions before death issued by physicians in each quintile.
*The number of final opioid prescriptions before death corresponding to the bottom 2 quintiles has been suppressed for privacy reasons because there were 5 or fewer in each category.
Table 1.
Physician characteristics across physician prescribing quintiles: Male sex (P = .003), older age (P < .001), and a greater number of years in practice (P < .001) were associated with greater opioid prescribing.
| CHARACTERISTIC | LOWEST VOLUME QUINTILE (N = 1977) | SECOND-LOWEST VOLUME QUINTILE (N = 1978) | MIDDLE QUINTILE (N = 1980) | SECOND-HIGHEST VOLUME QUINTILE (N = 1979) | HIGHEST VOLUME QUINTILE (N = 1978) |
|---|---|---|---|---|---|
| Male sex, % | 58 | 65 | 66 | 68 | 71 |
| Mean age, y | 48.4 | 47.0 | 47.1 | 49.0 | 50.5 |
| Mean no. of years in practice | 22.8 | 21.4 | 21.5 | 23.4 | 24.9 |
| Mean no. of patients eligible for public drug plan coverage | 343 | 374 | 404 | 433 | 424 |
Among the 408 individuals aged 15 to 64 whose deaths were related to opioids in 2006, 166 (40.7%) received at least 1 publicly funded opioid prescription in the year before death. Of these, 102 (61.4%) received their final prescription before death from family physicians. Family physicians in the highest-prescribing quintile issued the final prescription before death to 64 (62.7%) of these 102 individuals. The number of opioid-related deaths increased across prescribing-volume quintiles (P < .001).
DISCUSSION
Our results demonstrate that some family physicians prescribe opioids far more frequently than others, and that physicians who prescribe opioids more frequently are also more likely to issue the final prescription before a patient’s death.
Previous research has demonstrated temporal, geographic, and dose-related associations between opioid prescribing and mortality.1,5,7 Our findings illustrate an association between prescribing volume at the level of the individual physician and opioid-related mortality. Therefore, several lines of evidence suggest that increased opioid prescribing is associated with increased opioid-related mortality. Although the causal mechanism is likely to be complex, one important factor might simply be that more patients are placed at risk when more opioid prescriptions are written.
As opposed to other prescription drugs for which variation in prescribing exists, opioids are controlled substances with adverse effects including addiction and death. Moreover, the evidence base for opioid use in chronic nonmalignant pain is underdeveloped,8 and guidelines do not clearly indicate who should receive opioids and who should not.4 Reductions in opioid prescribing might therefore reduce opioid-related mortality without adversely affecting the quality of patient care. Although some risk factors for opioid-related death have been elucidated, most deaths are accidental and cannot be easily predicted.
Limitations
Some limitations of our study should be noted. Most important, the number of opioid-related deaths was too small to examine variation at the individual physician level, and it is possible that some high-volume opioid prescribers prescribe opioids in a manner that is associated with a very low risk of opioid-related harm. Second, our results might not be generalizable to other health care settings, particularly those in which care is comprehensive and coordinated and the average daily dose of opioids is relatively low.5 Third, we were only able to study publicly funded prescriptions, as we did not have access to records of prescription drugs that were obtained through private insurance or out-of-pocket payment. Fourth, we were unable to assess the appropriateness of individual prescriptions. Finally, we likely underestimated the number of opioid-related deaths because some deaths, particularly those that occur in the elderly, might not be the subject of detailed coroners’ investigations.
Conclusion
Opioid-related deaths are increasing and are now more common than deaths from HIV in North America.2,9 Our findings suggest that opioid-related deaths are concentrated among patients whose opioids are prescribed by a minority of physicians. Targeting high-volume prescribers, perhaps through “academic detailing”10 or focused regulatory intervention (eg, registration, audit, and monitoring for adherence to guidelines)11 might therefore help to reduce opioid-related mortality.
Our findings also suggest that family physicians might be able to reduce the risk of opioid-related harm by writing fewer opioid prescriptions. Achieving this goal will likely involve re-examining the appropriateness of prescribing for individual patients in light of the limited evidence for the utility of opioids in chronic nonmalignant pain.
Acknowledgments
We thank Greg Teitelbaum for assisting with data collection.
EDITOR’S KEY POINTS
Deaths involving prescription opioids are increasing in the United States and Canada, but whether variation in prescribing at the level of the individual physician is associated with opioid-related mortality remains unknown. High rates of opioid prescribing might not be associated with a proportionate increase in opioid-related deaths if “high-volume” physicians tend to prescribe opioids more carefully. Conversely, increased opioid prescribing could result in greater opioid-related harm if prescribing quality is unrelated to volume and deaths are proportionate to the number of prescriptions.
Results of this study demonstrate that some family physicians prescribe opioids far more frequently than others, and that physicians who prescribe opioids more frequently are also more likely to issue the final prescription before a patient’s death.
The findings also suggest that family physicians might be able to reduce the risk of opioid-related harm by writing fewer opioid prescriptions. Achieving this goal will likely involve re-examining the appropriateness of prescribing for individual patients in light of the limited evidence for the utility of opioids in chronic nonmalignant pain.
POINTS DE REPÈRE DU RÉDACTEUR
On observe une augmentation des décès liés à la prescription d’opiacés aux États-Unis et au Canada, mais on ignore s’il existe une relation entre le niveau de prescription d’un médecin donné et les décès liés aux opiacés. Le fait de faire beaucoup d’ordonnances d’opiacés pourrait ne pas entraîner une augmentation proportionnelle des décès liés aux opiacés si les médecins qui en prescrivent beaucoup le faisaient plus prudemment. À l’inverse, une augmentation des prescriptions d’opiacés pourrait causer plus d’effets nocifs liés aux opiacés s’il n’y avait pas de relation entre la qualité des ordonnances et leur nombre, les décès étant alors proportionnels au nombre d’ordonnances..
Les résultats de cette étude montrent que certains médecins de famille prescrivent des opiacés beaucoup plus souvent que d’autres, et que ces médecins sont beaucoup plus susceptibles d’avoir été les auteurs de l’ultime ordonnance ayant précédé le décès d’un patient.
Ces observations suggèrent aussi que le médecin pourrait être en mesure de réduire le risque de conséquences négatives liées aux opiacés s’il faisait moins de ce type d’ordonnances. Pour atteindre cet objectif, il faudra vraisemblablement se demander s’il est vraiment opportun de prescrire des opiacés à certains patients, compte tenu du peu de preuves concernant l’utilité de ces médicaments dans le traitement de la douleur chronique non cancéreuse.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Competing interests
None declared
Contributors
All authors contributed to the concept and design of the study; data analysis and interpretation; and preparing the manuscript for submission.
References
- 1.Dhalla IA, Mamdani MM, Sivilotti ML, Kopp A, Qureshi O, Juurlink DN. Prescribing of opioid analgesics and related mortality before and after the introduction of long-acting oxycodone. CMAJ. 2009;181(12):891–6. doi: 10.1503/cmaj.090784. Epub 2009 Dec 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warner M, Chen LH, Makuc DM. Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006. Atlanta, GA: Centres for Disease Control and Prevention; 2009. Available from: www.cdc.gov/nchs/data/databriefs/db22.htm. Accessed 2010 Nov 11. [PubMed] [Google Scholar]
- 3.Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;349(20):1943–53. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- 4.Furlan AD, Reardon R, Weppler C, National Opioid Use Guideline Group Opioids for chronic noncancer pain: a new Canadian practice guideline. CMAJ. 2010;182(9):923–30. doi: 10.1503/cmaj.100187. Epub 2010 May 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, Sullivan MD, et al. Opioid prescriptions for chronic pain and overdose. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gomes T, Mamdani MM, Dhalla IA, Mailis-Gagnon A, Paterson JM, Juurlink DN. Trends in opioid use and dosing among socio-economically disadvantaged patients. Open Med. 2011;5(1):13–22. [PMC free article] [PubMed] [Google Scholar]
- 7.Paulozzi LJ, Ryan GW. Opioid analgesics and rates of fatal drug poisoning in the United States. Am J Prev Med. 2006;31(6):506–11. doi: 10.1016/j.amepre.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Chapman CR, Lipschitz DL, Angst MS, Chou R, Denisco RC, Donaldson GW, et al. Opioid pharmacotherapy for chronic non-cancer pain in the United States: a research guideline for developing an evidence-base. J Pain. 2010;11(9):807–29. doi: 10.1016/j.jpain.2010.02.019. Epub 2010 Apr 28. [DOI] [PubMed] [Google Scholar]
- 9.Division of Vital Statistics, US Department of Health and Human Services . Deaths: final data for 2007. Atlanta, GA: Centres for Disease Control and Prevention; 2009. Available from: www.cdc.gov/NCHS/data/nvsr/nvsr58/nvsr58_19.pdf. Accessed 2010 Nov 11. [Google Scholar]
- 10.Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263(4):549–56. [PubMed] [Google Scholar]
- 11.Meier B. Move to restrict pain killers puts onus on doctors. New York Times. 2010. Jul 29, Sect. B:1. Available from: www.nytimes.com/2010/07/29/business/29pain.html?_r=1&hp. Accessed 2010 Aug 4.