Abstract
PURPOSE Patient-centered care is widely acknowledged as a core value in family medicine. In this systematic review, we aimed to identify and compare instruments, subscales, or items assessing patients’ perceptions of patient-centered care in family medicine.
METHODS We conducted a systematic literature review using the MEDLINE, Embase, and Cochrane databases covering 1980 through April 2009, with a specific search strategy for each database. The search strategy was supplemented with searching by hand and expert suggestions. We looked for articles meeting all of the following criteria: (1) describing self-administered instruments measuring patient perceptions of patient-centered care; (2) reporting quantitative or psychometric results of development or validation; (3) being relevant to an ambulatory family medicine context. The quality of each article retained was assessed using a modified version of the Standards for Reporting of Diagnostic Accuracy. Instrument’ items were mapped to dimensions of a patient-centered care conceptual framework.
RESULTS Of the 3,045 articles identified, 90 were examined in detail, and 26, covering 13 instruments, met our inclusion criteria. Two instruments (5 articles) were dedicated to patient-centered care: the Patient Perception of Patient-Centeredness and the Consultation Care Measure, and 11 instruments (21 articles) included relevant subscales or items.
CONCLUSIONS The 2 instruments dedicated to patient-centered care address key dimensions but are visit-based, limiting their applicability for the study of care processes over time, such as chronic illness management. Relevant items from the 11 other instruments provide partial coverage of the concept, but these instruments were not designed to provide a specific assessment of patient-centered care.
Keywords: Patient-centered care; questionnaires, instruments; systematic review; family medicine
INTRODUCTION
In the 1950s American humanistic psychologist Carl R. Rogers developed the concept of client-centered therapy.1–3 This approach was promoted in the medical field by psychoanalyst Michael Balint, who introduced the term “patient-centered medicine.” 4,5 A number of authors compared traditional medical approaches with patient-centered care. Today, patient-centered care is widely acknowledged as a core value in family medicine.6–8 It has been associated with positive outcomes: reduction of malpractice complaints and improvements in physician satisfaction, consultation time, patients’ emotional state, and medication adherence.9,10 Patient-centered care may also increase patient satisfaction and empowerment, as well as reduce symptom severity, use of health care resources, and health care costs.11
Although many authors refer to the patient-centered care concept, definitions often differ.10,12–19 The model developed by Stewart et al10 is most frequently cited in family medicine.11,14,20 It proposes 6 dimensions: exploring both the disease and the illness experience, understanding the whole person, finding common ground, incorporating prevention and health promotion, enhancing the patient-doctor relationship, and being realistic. Mead and Bower14 reviewed the conceptual and empirical literature to develop a model of the various aspects of the doctor-patient relationship encompassed by the concept of patient-centered care. They identified the following dimensions: biopsychosocial perspective, patient-as-person, sharing power and responsibility, therapeutic alliance, and doctor-as-person.
A clear conceptual framework is an essential first step for measurement. In the absence of a clear consensual model in the literature, we decided to keep the 4 dimensions common to Stewart et al and Mead and Bower’s review: (1) disease and illness experience (patient-as-person in Mead and Bower’s model), (2) whole person (biopsychosocial perspective), (3) common ground (sharing power and responsibility), and (4) patient-doctor relationship (therapeutic alliance). Figure 1▶ represents the patient-centered care framework used as the conceptual basis in our review.
Figure 1.
Conceptual framework of patient-centered care (PCC).
Various methodological approaches have been taken in designing instruments to measure patient-centered care, the 2 most predominant being direct observation of the clinical encounter (structured objective checklist) and self-assessment of the patient’s or the physician’s experience of the encounter.21 Many studies have shown that measures of the patients’ perceptions are more successful at predicting outcomes than either observation or physicians’ perceptions.9–11,22 Experts also claim that patient-administered questionnaires are the best way to measure patient-centered care attributes of primary health care.23 In this study, we aimed to identify and compare instruments, subscales, or items assessing patients’ perceptions of patient-centered care in family medicine.
METHODS
Our review process was based on important domains and elements identified by the Agency for Healthcare Rersearch and Quality for systematic reviews.24
Inclusion Criteria
We looked for articles meeting all of the following criteria: (1) describing self-administered instruments measuring at least 2 dimensions of the conceptual framework of patient-centered care, (2) reporting quantitative or psychometric results of development or validation, and (3) being relevant to the context of ambulatory family medicine.
Search Strategy and Article Selection
We conducted an electronic literature search of the MEDLINE (1980–), Embase (1980–), and Cochrane (1991–) databases for English and French articles published between 1980 and April 2009. An information specialist developed and ran specific strategies for each database (Supplemental Appendix 1, available online at http://www.annfammed.org/cgi/content/full/9/2/155/DC1). The following MeSH terms and key words were used: “patient-centered care” and its linguistic variations, “questionnaire,” “process assessment (health care),” “quality assurance, health care,” “psychometrics,” “validation studies,” “reproducibility of results,” “factor analysis, statistical,” “outcome and process assessment (health care),” and “outcome assessment (health care).” To broaden the scope of our research, we also applied the following search strategy to the same databases using “patient-centered care” and its linguistic variations, “family practice,” “primary health care,” “primary medical care,” and “primary care.”
We also examined reference lists for additional relevant articles (searching by hand). In addition, we consulted experts to identify articles describing instruments, including subscales or items that assess dimensions of patient-centered care.
All search results were transferred to a reference database (Refworks), and duplicates were eliminated. Titles and abstracts were read by one team member (M.L.) to exclude articles that were not eligible. We excluded references clearly not meeting our inclusion criteria and retained all other references for complete reading. If there was any doubt, the full article was retrieved and read to apply selection criteria. Two authors (M.L., M.E.P.) independently appraised the full text of the retrieved articles to identify any that were potentially eligible. Articles meeting all inclusion criteria were retained for quality assessment and data extraction. Discrepancies between the 2 reviewers were resolved by team consensus.
Assessment of Study Quality
We assessed study quality with a modified version of the Standards for Reporting of Diagnostic Accuracy STARD (Supplemental Appendix 2, available online at http://www.annfammed.org/cgi/content/full/9/2/155/DC1).25–27 The STARD is a result of the Consolidated Standards of Reporting Trials (CONSORT) initiative,28 and has been adopted by many leading biomedical and psychology journals.29 Using the modified 15-item scale,30 2 researchers (M.L., M.E.P.) independently determined a global quality score for each article. Scores were compared, and consensus was reached. Studies were excluded if the quality score was less than 8 of a maximum score of 15.
Data Extraction
The following data were extracted for each instrument: development procedures and conceptual base, quality score, description of the instrument (number of dimensions and items), response scale, and psychometric properties when available (internal consistency, test-retest fidelity, and predictive validity).31 Data extraction was performed independently by 2 members of the team (M.L., M.E.P.), and disagreements were resolved by consensus.
Instrument subscales or items were mapped to dimensions of our patient-centered care conceptual framework. Our initial intention was to map only at the subscale level, but we realized that an item-level analysis was required, because certain sub-scales contained items that mapped with more than one dimension of the consensual framework and because we found scales without any subscales.
RESULTS
Articles Included in the Review
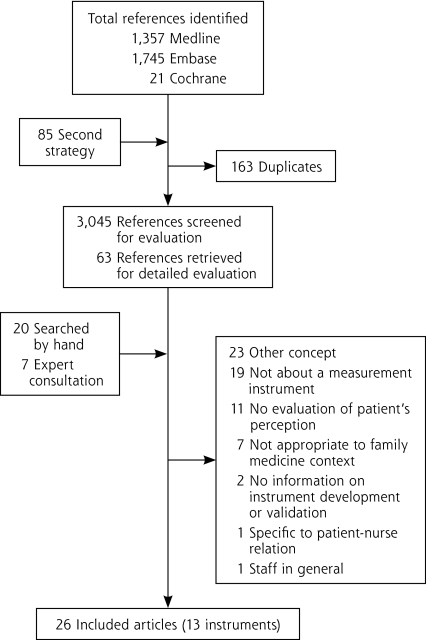
The search strategies identified 3,208 references, of which 3,045 were unique after removing duplicates. Most of these references were excluded as clearly not meeting our inclusion criteria by reading the abstract. Sixty-three articles were retained to be read completely; 20 additional references were identified by a hand search, and 7 were included as a result of experts’ suggestions. Of these 90 articles, 64 were excluded: 23 addressed a concept other than patient-centered care and did not measure at least 2 dimensions of the conceptual framework32–54; 11 reported on instruments assessing physicians’ or nurses’ perceptions55–65; 19 did not deal with quantitative instruments21–22,66–82; 7 were not relevant to an ambulatory family medicine context (6 in an inpatient context83–88 and 1 in specialty medicine89); 1 measured relations between the patient and the nurse specifically79; 1 described an instrument designed to evaluate staff (very general questions)90; and 2 did not provide sufficient information on the development and validation of the instrument.91,92 A final sample of 26 articles (Table 1▶) was retained for data extraction as outlined in the selection process shown in Figure 2▶.
Table 1.
Instruments Covered by the 21 Articles Included in the Review
| Instrument | Authors | Country | Year | Quality Scorea |
|---|---|---|---|---|
| Patient Perception of Patient-Centeredness (PPPC) | Stewart et al9 | Canada | 2000 | 8 (11)b |
| Mallinger et al93 | United States | 2005 | 13 | |
| Consultation Care Measure (CCM) | Little et al11 | United Kingdom | 2001 | 11 |
| Little et al94 | United Kingdom | 2001b | 10 | |
| Smith et al95 | United Kingdom | 2007 | 11 | |
| Patient Reactions Assessment (PRA) | Galassi et al96 | United States | 1992 | 8 |
| Perceived Involvement in Care Scale (PICS) | Lerman et al97 | United States | 1995 | 12 |
| Loh et al98 | United States | 2007 | 11 | |
| Component of Primary Care Instrument (CPCI) | Flocke99 | United States | 1997 | 14 |
| Flocke et al100 | United States | 1998 | 11 | |
| Flocke et al101 | United States | 1999 | 11 | |
| Medical Communication Competence Scale (MCCS) | Cegala et al102 | United States | 1998 | 10 |
| Primary Care Assessment Survey (PCAS) | Safran et al103 | United States | 1998 | 12 |
| Safran et al104 | United States | 2006 | 12 | |
| Duberstein et al105 | United States | 2007 | 9 | |
| Interpersonal Processes of Care (IPC) | Stewart et al106 | United States | 1999 | 10 |
| Stewart et al107 | United States | 2007 | 14 | |
| General Practice Assessment Survey (GPAS) | Ramsay et al108 | United Kingdom | 2000 | 13 |
| Jayasinghe et al109 | Australia | 2008 | 12 | |
| Patient Perception of Quality (PPQ) | Haddad et al110 | Canada | 2000 | 12 |
| Primary Care Assessment Tool-Adult (PCAT–A) | Shi et al111 | United States | 2001 | 12 |
| Haggerty et al112 | Canada | 2008 | 11 | |
| Consultation and Relational Empathy (CARE) | Mercer et al113 | United Kingdom | 2004 | 12 |
| Mercer et al114 | United Kingdom | 2005 | 12 | |
| Mercer et al115 | United Kingdom | 2008 | 11 | |
| Instrument on Doctor-Patient Communication Skills (IDPCS) | Campbell et al116 | Canada | 2007 | 12 |
a Maximum score is 15.
b Evaluation of an unpublished paper on PPPC (Stewart et al, 2004, available from authors on request), combined with the initial assessment of the study quality of the main article.
Figure 2.
Number of references identified through the stages of the systematic review.
The quality scores of the final sample ranged from 8 to 14 of 15; all articles were retained for the review.
Instruments Dedicated to Patient-Centered Care
Five articles covering 2 instruments were included (Table 2▶): the Patient Perception of Patient-Centeredness (PPPC)9,93 and the Consultation Care Measure (CCM).11,94,95
Table 2.
Characteristics of Instruments Measuring Patient-Centered Care
| Instrument | Origin | Conceptual Base | Description | Subscale (Items) |
|---|---|---|---|---|
| Patient Perception of Patient-Centeredness (PPPC) | Existing literature and empirical studies on the doctor-patient relationship and the Stewart et al model | Stewart et al model | 14 Items, 4-point Likert scale (completely to not at all) | No subscale (14/14, α= .71) |
| Consultation Care Measure (CCM) | Existing literature and empirical studies on the doctor-patient relationship, the Stewart et al model, and patient interviews | Stewart et al model | 21 Items, 4-point Likert scale (very strongly agree to neutral/disagree) | Communication and partnership (11/11, α = .96), personal relationship (3/3, α= .89), health promotion (2/2, α = .87), positive and clear approach to problem (3/3, α= .84) and interest in effect on life (2/2, α= .89) |
| Patient Reactions Assessment (PRA) | Existing instruments, existing literature and empirical studies on the physician-patient relationship, interviews with patients and caregivers, and clinical experiences of the research team | Dimensions of the physician-patient medical relationship | 15 Items, 7-point Likert scale (very strongly disagree to very strongly agree) | Patient information index (2/5, α = .87), patient communication index (1/5, α=.91) and patient affective index (5/5, α=.90) Excluded: Patient information index (3/5) and patient communication (4/5) |
| Perceived Involvement in Care Scale (PICS) | Existing literature and empirical studies on patient participation in medical care, observations of the principal researcher, expert consultations | Dimensions of patient participation | 13 Items, dichotomous scale (yes/no) | Doctor facilitation (5/5, α=.60–.73) Excluded: Patient information (4/4) and patient decision making (4/4) |
| Component of Primary Care Instrument (CPCI) | Interim report by the Institute of Medicine (IOM) in 1994 defining primary care and its components | IOM’s definition of primary care and dimensions of primary care | 52 Items, 6-point Likert scale (strongly disagree to strongly agree) | Accumulated knowledge (7/7, α = .88), interpersonal communication (6/6, α=.75), advocacy (2/9, α=.88), family context(2/3, α = .82) and community context (2/2, α not available) Excluded: Comprehensive care (6/6), preference for regular physician (4/4), coordination of care (6/6), family context (1/3), duration of relationship (2/2) and continuity (3/3) |
| Medical Communication Competence Scale (MCCS) | Existing literature and empirical studies on doctor-patient communication | Dimensions of medical communication | 40 Items (patient’s version), 7-point Likert scale strongly agree to strongly disagree) | No subscale (24/40, α = .79 for information giving, α = .76 for information seeking, α = .85 for information verifying, and α =.92 for socioemotional communication) Excluded: Patients’ self-competence items (16/40) |
| Primary Care Assessment Survey (PCAS) | Interim report by the Institute of Medicine (IOM) in 1994 defining primary care and its components | IOM’s definition of primary care | 51 Items, 6-point Likert scale (very poor to excellent) | Contextual knowledge of patient (5/5, α=.92), communication (6/6, α=.95), interpersonal treatment (4/5, α = .95) and trust (5/8, α=.86) Excluded: Organizational access (6/6), financial access (2/2), longitudinal continuity (1/1) and visit-based continuity (2/2), preventive counseling (7/7), integration (6/6), interpersonal treatment (1/5), thoroughness of physical examination (1/1), trust (3/8), screener items (2/2) |
| Interpersonal Processes of Care (IPC) | Focus group, existing literature and empirical studies on the doctor-patient relationship and the quality of care, Stewart et al model and cognitive interviews | Dimensions of interpersonal care processes | 29 Items, 5-point Likert scale (never to always) | Hurried communication (5/5, α = .65), elicited concerns, responded (3/3, α=.80), explained results, medication (4/4, α = .81), patient-centered decision-making (3/3, α = .75) and compassionate, respectful (5/5, α=.71) Excluded: Discrimination (4/4) and disrespectful office staff (5/5) |
| General Practice Assessment Survey (GPAS) | PCAS | Dimensions of primary care | 30 Items, 6-point Likert scale (very poor to excellent) | Communication (2/4, α = .90), interpersonal care (3/3, α=.93), trust (2/4, α=.69) and knowledge of patient (3/3, α=.91) Excluded: Accessibility (8/8), technical care (5/5), communication (2/4), trust (2/4) and nursing care (3/3) |
| Patient Perception of Quality (PPQ) | Existing instruments, existing literature and empirical studies on quality of care, patient interviews and expert consultations | Dimensions of quality of care | 22 Items, 5-point Likert scale (negative to positive) | Interpersonal aspects of care (5/5, α = .91) and technical aspects of care (5/12, α=.91) Excluded: Technical aspects of care (7/12) and outcomes of care (5/5) |
| Priamry Care Assessment Tool– Adult (PCAT–A) | Primary Care Assessment Tool–Child, expert consultations | Dimensions of primary care | 74 Items, 4-point Likert scale (definitely not to definitely) | Ongoing care (12/20, α=.92) Excluded: First-contact accessibility (4/4), first contact utilization (3/3), ongoing care (8/20) coordination of services (8/8), comprehensiveness services available (21/21), comprehensive service received (13/13) and community orientation (5/5) |
| Colsultation and Relational Empathy (CARE) | Existing literature and empirical studies on empathy and in-depth qualitative work on patient’s views on holistic care | Dimensions of empathy | 10 Items, 5-point Likert scale (poor to excellent) | No subscale (10/10, α=.92) |
| Instrument on Doctor-Patient Communication Skills (IDPCS) | Existing instruments (PPPC and Core Competency of Interpersonal and Communication Skills), revised conceptual framework adapted from the Calgary–Cambridge guide and expert consultations | The Stewart et al model and communication theories | 19 items, 5-point Likert scale (strongly disagree to strongly agree) | No subscale (19/19, α=.69) |
Patient Perception of Patient-Centeredness
The PPPC,9,93 which was developed in Canada, is based on empirical studies of the doctor-patient relationship and Stewart et al’s model.10 It measures patient perceptions of patient-centered care during the last visit with a family physician. The instrument has 14 items using a 4-point Likert scale from completely to not at all, and no subscales. Cronbach’s α reliability for the global score was .71. The PPPC showed significant correlations with better recovery from discomfort, alleviation of concerns, and better emotional health 2 months after the initial visit, and with use of fewer diagnostic tests and referrals.9 Patients’ perception of patient-centered behaviors was strongly associated with patients’ satisfaction with information.93
The PPPC measures 3 of the 4 dimensions of the conceptual framework (Table 3▶): disease and illness experience (4 items), whole person (1 item), and common ground (9 items).
Table 3.
Patient-Centered Care Measurement Instruments Included in the Review
|
Number of Items Assessing Conceptual Framework Dimension |
||||
|---|---|---|---|---|
| Instrument | Disease and Illness Experience | Whole Person | Common Ground | Patient-Doctor Relationship |
| Patient Perception of Patient-Centeredness | 4 | 1 | 9 | 0 |
| Consultation Care Measure | 6 | 2 | 9 | 1 |
| Patient Reactions Assessment | 0 | 0 | 2 | 6 |
| Perceived Involvement in Care Scale | 2 | 0 | 3 | 0 |
| Component of Primary Care Instrument | 5 | 5 | 3 | 6 |
| Medical Communication Competence Scale | 0 | 0 | 18 | 6 |
| Primary Care Assessment Survey | 4 | 1 | 4 | 12 |
| Interpersonal Processes of Care | 4 | 0 | 8 | 8 |
| General Practice Assessment Survey | 2 | 1 | 2 | 5 |
| Patient Perception of Quality | 0 | 1 | 4 | 5 |
| Primary Care Assessment Tool–Adult | 4 | 4 | 2 | 2 |
| Consultation and Relational Empathy | 2 | 1 | 2 | 5 |
| Instrument on Doctor-Patient Communication Skills | 2 | 0 | 10 | 3 |
Consultation Care Measure
The CCM,11,94,95 which was developed in Great Britain, is based on empirical studies of the doctor-patient relationship, Stewart et al’s model, and patient interviews. It also measures patients’ perceptions of patient-centered care during the last visit with a family physician. The instrument has 5 subscales: communication and partnership (11 items), personal relationship (3 items), health promotion (2 items), positive and clear approach to the problem (3 items), and interest in effect on life (2 items), for a total of 21 items using a 4-point Likert scale ranging from very strongly agree to neutral/disagree.
Cronbach’s α reliability ranged from .84 for the positive and clear approach to problem subscale, to .96 for the communication and partnership subscale. Satisfaction was related to communication and partnership and positive approach. Enablement was more significantly related with interest in effect on life, health promotion, and positive approach. Positive approach was associated with reduced symptom burden at 1 month. Referrals were fewer if patients felt they had a personal relationship with their doctor.11
The CCM assesses all the conceptual dimensions (Table 3▶): disease and illness experience (6 items), whole person (2 items), common ground (9 items), and patient-doctor relationship (1 item).
Both instruments are based on Stewart et al’s model and measure patients’ perceptions of patient-centered care during the last visit with a family physician with a similar length of administration. The CCM has better Cronbach’s α reliability for each subscale than the overall PPPC. Both instruments show that a higher level of patient-centered care is associated with better health outcomes in the short term. The PPPC does not assess patient-doctor relationship, whereas only 1 item of CCM assesses this dimension.
Patient-Centered Care Dimensions in Other Instruments
Included were 21 articles validating 11 instruments. These instruments are the Patient Reactions Assessment (PRA),96 the Perceived Involvement in Care Scale (PICS),97,98 the Components of Primary Care Instrument (CPCI),99–101 the Medical Communication Competence Scale (MCCS),102 the Primary Care Assessment Survey (PCAS),103–105 the Interpersonal Processes of Care (IPC),106,107 the General Practice Assessment Survey (GPAS),108,109 the Patient Perception of Quality (PPQ),110 the Primary Care Assessment Tool–Adult Edition (PCAT–A),111,112 the Consultation and Relational Empathy (CARE),113–115 and the Instrument on Doctor-Patient Communication Skills (IDPCS).116
Table 2▶ displays all of these instruments: name of the instrument as given by the developer, development procedures and conceptual base, description of the instrument (number of dimensions and items), response scale, included subscales with Cronbach α coefficients, and excluded subscales. Supplemental Appendix 3, available online at http://www.annfammed.org/cgi/content/full/9/2/155/DC1, displays the subscales and items of instruments measuring patient-centered care. The majority contain subscales except for the MCCS, CARE, and the IDPCS. Seven assess physician care over time (PRA, CPCI, PCAS, IPC, GPAS, PPQ, and PCAT–A). The number of items ranges from 10 (CARE) to 74 (PCAT–A). Other psychometric properties are presented in Supplemental Appendix 4, available online at http://www.annfammed.org/cgi/content/full/9/2/155/DC1. They all use a Likert scale except for the PICS (yes/no answer). Quality scores ranged from 8 to 14 out of a possible 15 (Table 1▶).
All of these instruments assess, at least partially, the “common ground,” “disease and illness experience” (except the PRA, MCCS, and PPQ), and “patient-doctor relationship” (except the PICS) dimensions (Table 3▶). Only 6 instruments (CPCI, PCAS, GPAS, PPQ, PCAT–A, and CARE) measure the “whole-person” dimension. The CPCI, the PCAS, the GPAS, the PCAT–A, and the CARE assess, at least partially, all dimensions of the conceptual framework.
DISCUSSION
Although patient-centered care has been defined in various ways by different authors, we identified, in this review, instruments that address 2 or more dimensions of a conceptual framework consisting of 4 core dimensions that are common to 2 conceptual models in family medicine.10,14
If clinicians, researchers, or decision makers are interested in instruments specifically dedicated to measure patient-centered care, our review identified 2 instruments, the PPPC and the CCM, both of which showed that higher levels of patient-centered care were associated with better health outcomes in the short term.9,11 Length of administration is similar for both of them. The CCM briefly evaluates the patient-doctor relationship (1 item) whereas the PPPC does not measure this dimension.
For clinicians, researchers, or decision makers interested in a broader scope of health care delivery, our review identified 11 instruments that also address dimensions of patient-centered care. Although all but the PRA, PICS, and MCCS address at least 3 of the dimensions in our conceptual framework, it is important to note that they reflect how the dimension of patient-centered care relates to another construct, such as comprehensiveness, continuity, or respectfulness. These subscales were not designed to provide an assessment of patient-centered care as such; nonetheless, 1 instrument may be selected over another based on the extent to which patient-centered care is represented as a component of other attributes.
One core element of patient-centered care10,14,117 is an ongoing relationship with the family physician. It implies that it is probably best assessed by evaluating patient-centered care over time rather than during a single visit,10 as do both dedicated instruments identified (PPPC9,93 and CCM11,94,95). A measure over time may be particularly relevant for patients suffering from chronic diseases, which by definition require ongoing management for years or decades.6,9,93 The development of longitudinal measures (evaluating, for example, the last 6 or 12 months) of the PPPC and CCM instruments could evaluate losses or gains in precision and validity. Inspiration could be derived from 7 of the 11 instruments measuring other concepts that assess the dynamics between physician and patient for a prolonged period.
To date, the patient-centered care concept and measurement instruments in family medicine mainly refer to the approach and behavior of family physicians during the care process. Measures of patient-centered care have always been relevant to family medicine at a clinical level to reflect the concordance of practice with one of its core values. It is becoming increasingly important, however, as an organizing principle for change in health services delivery at a systems level. In the United States,117,118 and more recently in Canada,119 the patient-centered medical home has been the organizing framework for recent reforms of the health system and specifically of primary care. Within this approach, patient-centered care is part of a broad organization of health care delivery and is measured by such practice indicators as enhanced access procedures, the use of information systems to create disease registries and evaluate quality of care, care coordination within and across health care teams, processes to engage the patient in health promotion and prevention, and regular surveys of patients’ experience. Within this framework, assessment of the patient-centered clinical encounter is only one component of evaluating patient-centered care in family medicine.120,121
We do not think that there is an inherent contradiction between clinical-level and systems-level patient-centered care. Based on the seminal work by Stewart et al10 and Little et al,11 however, we contend that whatever structural and payment reforms may be implemented, ultimately the patient needs to perceive that his or her individual needs and circumstances are at the heart of the clinical care he or she receives, hence the importance of identifying appropriate measurement instruments.
As valid measures of perceptions of patient-centered care are applied within the patient-centered medical home organizing framework, we will be better able to determine how systems-level dimensions, such as accessibility and coordination of care, fit and whether they should be considered in a patient-centered care model. Additionally, qualitative interviews with primary care patients could help refine the conceptual model empirically to better understand which dimensions are really patient-centered, are most meaningful for the patients, and may have an impact on long-term outcomes.
Limitations of the Study
One of the main limitations of a systematic review is the potential omission of relevant articles, as well as any unpublished material. Our search strategy relied on key words assigned by authors and may have missed instruments that are relevant to patient-centered care but were not identified. Even so, our search strategy was adapted for different databases, was developed in collaboration with an information specialist, and enabled an exhaustive literature review. Moreover, we identified further articles through searching by hand and consultation with experts. In addition, we decided to focus on instruments relevant to ambulatory family medicine, because we were interested in this particular context. We acknowledge, however, that other instruments have been designed to measure patient-centered care in other contexts (nursing, medical specialty, hospital setting). Examination of these instruments was beyond the scope of the article.
Because patient-centered care is a multidimensional concept, we decided to include instruments measuring at least 2 dimensions of the conceptual framework. This decision led to the exclusion of instruments measuring only 1 dimension, such as shared decision-making, for example.
If clinicians, researchers, or decision makers are interested in instruments dedicated to measuring patient-centered care, our review identified 2 visit-based instruments, the PPPC and the CCM, both of which showed that higher levels of patient-centered care were associated with better health outcomes in the short term. For people interested in a broader scope of health care delivery, we identified 11 instruments that address at least 3 dimensions in our conceptual framework (except for the PRA, PICS, and MCCS). Because these instruments were not designed to provide a specific assessment of patient-centered care, convergent validity of patient-centered care instruments and sub-scales or items of other instruments could be examined.
Acknowledgments
The authors would like to thank Dr Marie-Dominique Beaulieu, Professor, Department of Family Medicine, Université de Montréal, Canada, for her comments and suggestions on the first version of the article; Dr Moira Stewart, Director and Professor, Centre for Studies in Family Medicine and Thames Valley Family Practice Research Unit, University of Western Ontario, Canada; Dr Paul Little, Professor, Faculty of Medicine, University of Southampton, Great Britain; Dr Peter Bower, Researcher, National Primary Care Research and Development Centre, University of Manchester, Great Britain; Dr Ronald Epstein, Director, Rochester Center to Improve Communication in Health Care, and Professor, Department of Family Medicine and Psychiatry, University of Rochester, United States, for their contribution as external experts.
Conflicts of interest: authors report none.
Funding support: This research received financial support from the Canadian Health Services Research Foundation (CHSRF) through the Research, Exchange and Impact for System Support (REISS) Competition.
REFERENCES
- 1.Rogers CR. Psychometrics tests and client-centered counseling. Educ Psychol Meas. 1946;6:139–144. [Google Scholar]
- 2.Rogers CR. Significant aspects of client-centered therapy. Am Psychol. 1946;1(10):415–422. [DOI] [PubMed] [Google Scholar]
- 3.Rogers CR. Client-centered psychotherapy. Sci Am. 1952;187:1–7. [Google Scholar]
- 4.Balint M, Hunt J, Joyce D, Marinker M, Woodcock J. Treatment or Diagnosis: A Study of Repeat Prescriptions in General Practice. Philadelphia, PA: JB Lippincott; 1970.
- 5.Balint M. The Doctor, His Patient and the Illness. London: Pitman Medical; 1957.
- 6.WHO. World Health Organization. The Innovative Care for Chronic Condition (ICCC). http://www.who.int/diabetesactiononline/about/ICCC/en/index.html. Accessed Sep 10, 2010.
- 7.WHO. World Health Organization. Former les personnels de santé du XXe siècle: le défi des maladies chroniques. http://www.who.int/chp/knowledge/publications/workforce_report_fre.pdf. Accessed Sep 10, 2010.
- 8.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511–544. [PubMed] [Google Scholar]
- 9.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 10.Stewart M, Brown JB, Weston WW, Freeman TR. Patient-Centred Medicine: Transforming the Clinical Method. 2nd ed. United Kingdom: Radcliffe Medical Press; 2003.
- 11.Little P, Everitt H, Williamson I, et al. Observational study of effect of patient centredness and positive approach on outcomes of general practice consultations. BMJ. 2001;323(7318):908–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA. 1996;275(2):152–156.8531314 [Google Scholar]
- 13.Winefield HR, Murrell TG, Clifford JV, Farmer EA. The usefulness of distinguishing different types of general practice consultation, or are needed skills always the same? Fam Pract. 1995;12(4):402–407. [DOI] [PubMed] [Google Scholar]
- 14.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–1110. [DOI] [PubMed] [Google Scholar]
- 15.Balint E. The possibilities of patient-centered medicine. J R Coll Gen Pract. 1969;17(82):269–276. [PMC free article] [PubMed] [Google Scholar]
- 16.Byrne P, Long B. Doctor Talking to Patients. London: HMSO; 1976.
- 17.McWhinney I. The need for a transformed clinical method. In: Stewart M, Roter D, eds. Communicating With Medical Patients. London: Sage Publications; 1989. p.
- 18.Grol R, de Maeseneer J, Whitfield M, Mokkink H. Disease-centred versus patient-centred attitudes: comparison of general practitioners in Belgium, Britain and The Netherlands. Fam Pract. 1990; 7(2):100–103. [DOI] [PubMed] [Google Scholar]
- 19.Lipkin M Jr, Quill TE, Napodano RJ. The medical interview: a core curriculum for residencies in internal medicine. Ann Intern Med. 1984;100(2):277–284. [DOI] [PubMed] [Google Scholar]
- 20.Gilmore KA, Hargie O. Quality issues in the treatment of depression in general practice. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2000;13(1):34–41. [DOI] [PubMed] [Google Scholar]
- 21.Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005;61(7):1516–1528. [DOI] [PubMed] [Google Scholar]
- 22.Henbest RJ, Stewart M. Patient-centredness in the consultation. 2: Does it really make a difference? Fam Pract. 1990;7(1):28–33. [DOI] [PubMed] [Google Scholar]
- 23.Haggerty J, Burge F, Lévesque JF, et al. Operational definitions of attributes of primary health care: consensus among Canadian experts. Ann Fam Med. 2007;5(4):336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. Systems to rate the strength of scientific evidence. http://archive.ahrq.gov/clinic/epcsums/strengthsum.htm. Accessed Sep 10, 2010.
- 25.Bossuyt PM, Reitsma JB; Standards for Reporting of Diagnostic Accuracy. The STARD initiative. Lancet. 2003;361(9351):71. [DOI] [PubMed] [Google Scholar]
- 26.Bossuyt PM, Reitsma JB, Bruns DE, et al.; Standards for Reporting of Diagnostic Accuracy. The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Intern Med. 2003;138(1):W1–W12. [DOI] [PubMed] [Google Scholar]
- 27.Meyer GJ. Guidelines for reporting information in studies of diagnostic test accuracy: the STARD initiative. J Pers Assess. 2003;81(3): 191–193. [DOI] [PubMed] [Google Scholar]
- 28.Altman DG, Schulz KF, Moher D, et al.; CONSORT GROUP (Consolidated Standards of Reporting Trials). The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134(8):663–694. [DOI] [PubMed] [Google Scholar]
- 29.Streiner DL, Norman GR. Health Measurement Scale: A Pratical Guide to the Development and Use. 4th ed. Oxford: Oxford University Press; 2008.
- 30.Hudon C, St-Cyr Tribble D, Legare F, Bravo G, Fortin M, Almirall J. Assessing enablement in clinical practice: a systematic review of available instrument. J Eval Clin Pract. 2010; 16(6):1301–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McDowell I. Measuring Health. A Guide to Rating Scales and Questionnaires. 3rd ed. New York, NY: Oxfort University Press; 2006.
- 32.Haughney J, Cotton P, Rosen JP, Rosen JP, Morrison K, Price D. The use of a modification of the Patient Enablement Instrument in asthma. Prim Care Respir J. 2007;16(2):89–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hansson L, Björkman T, Priebe S. Are important patient-rated outcomes in community mental health care explained by only one factor? Acta Psychiatr Scand. 2007;116(2):113–118. [DOI] [PubMed] [Google Scholar]
- 34.Myklebust M, Pradhan EK, Gorenflo D. An integrative medicine patient care model and evaluation of its outcomes: the University of Michigan experience. J Altern Complement Med. 2008;14(7):821–826. [DOI] [PubMed] [Google Scholar]
- 35.McLean M, Armstrong D. Eliciting patients’ concerns: a randomised controlled trial of different approaches by the doctor. Br J Gen Pract. 2004;54(506):663–666. [PMC free article] [PubMed] [Google Scholar]
- 36.Chao J. Continuity of care: incorporating patient perceptions. Fam Med. 1998;20(5):333–337. [PubMed] [Google Scholar]
- 37.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–1651. [DOI] [PubMed] [Google Scholar]
- 38.Williams GC, Rodin GC, Ryan RM, Grolnick WS, Deci EL. Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychol. 1998;17(3):269–276. [DOI] [PubMed] [Google Scholar]
- 39.Howie JGR, Heaney DJ, Maxwell M. Quality, core values and the general practice consultation: issues of definition, measurement and delivery. Fam Pract. 2004;21(4):458–468. [DOI] [PubMed] [Google Scholar]
- 40.Howie JGR, Heaney DJ, Maxwell M, Walker JJ, Freeman GK. Developing a ‘consultation quality index’ (CQI) for use in general practice. Fam Pract. 2000;17(6):455–461. [DOI] [PubMed] [Google Scholar]
- 41.Hoy E. Measuring patient experiences of care. Bull Am Coll Surg. 2008;93(5):13–16. [PubMed] [Google Scholar]
- 42.Jung HP, Wensing M, de Wilt A, Olesen F, Grol R. Comparison of patients’ preferences and evaluations regarding aspects of general practice care. Fam Pract. 2000;17(3):236–242. [DOI] [PubMed] [Google Scholar]
- 43.Kleeberg UR, Tews JT, Ruprecht T, Höing M, Kuhlmann A, Runge C. Patient satisfaction and quality of life in cancer outpatients: results of the PASQOC study. Support Care Cancer. 2005;13(5):303–310. [DOI] [PubMed] [Google Scholar]
- 44.Mercer SW, Howie JG. CQI-2—a new measure of holistic interpersonal care in primary care consultations. Br J Gen Pract. 2006; 56(525):262–268. [PMC free article] [PubMed] [Google Scholar]
- 45.Neumann M, Wirtz M, Bollschweiler E, et al. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns. 2007;69(1–3):63–75. [DOI] [PubMed] [Google Scholar]
- 46.Pawlikowska TR, Nowak PR, Szumilo-Grzesik W, Walker JJ. Primary care reform: a pilot study to test the evaluative potential of the Patient Enablement Instrument in Poland. Fam Pract. 2002;19(2):197–201. [DOI] [PubMed] [Google Scholar]
- 47.Suhonen R, Välimäki M, Katajisto J. Developing and testing an instrument for the measurement of individual care. J Adv Nurs. 2000;32(5):1253–1263. [DOI] [PubMed] [Google Scholar]
- 48.Suhonen R, Välimäki M, Katajisto J. Individualized care in a Finnish healthcare organization. J Clin Nurs. 2000;9(2):218–227. [DOI] [PubMed] [Google Scholar]
- 49.Suhonen R, Välimäki M, Katajisto J, Leino-Kilpi H. Provision of individualised care improves hospital patient outcomes: an explanatory model using LISREL. Int J Nurs Stud. 2007;44(2):197–207. [DOI] [PubMed] [Google Scholar]
- 50.Swaine BR, Dutil E, Demers L, Gervais M. Evaluating clients’ perceptions of the quality of head injury rehabilitation services: development and validation of a questionnaire. Brain Inj. 2003;17(7):575–587. [DOI] [PubMed] [Google Scholar]
- 51.Carr AJ, Higginson IJ. Are quality of life measures patient centred? BMJ. 2001;322(7298):1357–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fiscella K, Franks P, Srinivasan M, Kravitz RL, Epstein RM. Ratings of physician communication by real and standardized patients. Ann Fam Med. 2007;5(2):151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martin LR, DiMatteo MR, Lepper HS. Facilitation of patient involvement in care: development and validation of a scale. Behav Med. 2001;27(3):111–120. [DOI] [PubMed] [Google Scholar]
- 54.Egede LE, Ellis C. Development and testing of the multi-dimensional trust in health care systems scale. J Gen Intern Med. 2008;23(6): 808–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tsimtsiou Z, Kerasidou O, Efstathiou N, Papaharitou S, Hatzimouratidis K, Hatzichristou D. Medical students’ attitudes toward patient-centred care: a longitudinal survey. Med Educ. 2007;41(2):146–153. [DOI] [PubMed] [Google Scholar]
- 56.Batenburg V, Smal JA. Does a communication course influence medical students’ attitudes? Med Teach. 1997;19(4):263–269. [Google Scholar]
- 57.Batenburg V, Smal JA, Lodder A, de Melker RA. Are professional attitudes related to gender and medical specialty? Med Educ. 1999;33(7):489–492. [DOI] [PubMed] [Google Scholar]
- 58.Cockburn J, Killer D, Campbell E, Sanson-Fisher RW. Measuring general practitioners’ attitudes towards medical care. Fam Pract. 1987;4(3):192–199. [DOI] [PubMed] [Google Scholar]
- 59.Haidet P, Kelly PA, Chou C; Communication, Cirriculum, and Culture Study Group. Characterizing the patient-centeredness of hidden curricula in medical schools: development and validation of a new measure. Acad Med. 2005;80(1):44–50. [DOI] [PubMed] [Google Scholar]
- 60.Jenkins M. Doctors’ understanding of their consultations in terms of doctor/patient centredness. Educ Gen Pract. 2000;11(1):36–45. [Google Scholar]
- 61.Krupat E, Bell RA, Kravitz RL, Thom D, Azari R. When physicians and patients think alike: patient-centered beliefs and their impact on satisfaction and trust. J Fam Pract. 2001;50(12):1057–1062. [PubMed] [Google Scholar]
- 62.O’Keefe M, Roberton D, Sawyer M, Baghurst P. Medical student interviewing: a randomized trial of patient-centredness and clinical competence. Fam Pract. 2003;20(2):213–219. [DOI] [PubMed] [Google Scholar]
- 63.Rolfe G. Some factors associated with change in patient-centredness of student nurses during the Common Foundation Programme in Nursing. Int J Nurs Stud. 1994;31(5):421–436. [DOI] [PubMed] [Google Scholar]
- 64.Rolfe G. The Patient-Centredness Multi-Choice Questionnaire: developing an instrument for the measurement of patient-centredness in student nurses. J Adv Nurs. 1993;18(1):120–126. [DOI] [PubMed] [Google Scholar]
- 65.Haidet P, Dains JE, Paterniti DA, Chang T, Tseng E, Rogers JC. Medical students’ attitudes toward patient-centered care and standardized patients’ perceptions of humanism: a link between attitudes and outcomes. Acad Med. 2001;76(10)(Suppl):S42–S44. [DOI] [PubMed] [Google Scholar]
- 66.Cegala D, Socha McGeen D, McNeilis K. Components of patients’ and doctors’ perceptions of communication competence during a primary care medical interview. Health Commun. 1996;8(1):1–27. [Google Scholar]
- 67.Minnick A, Roberts MJ, Young WB, Kleinpell RM, Micek W. An analysis of posthospitalization telephone survey data. Nurs Res. 1995;44(6):371–375. [PubMed] [Google Scholar]
- 68.Michie S, Miles J, Weinman J. Patient-centredness in chronic illness: what is it and does it matter? Patient Educ Couns. 2003; 51(3):197–206. [DOI] [PubMed] [Google Scholar]
- 69.Kinnersley P, Stott N, Peters TJ, Harvey I. The patient-centredness of consultations and outcome in primary care. Br J Gen Pract. 1999;49(446):711–716. [PMC free article] [PubMed] [Google Scholar]
- 70.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002; 48(1):51–61. [DOI] [PubMed] [Google Scholar]
- 71.Graugaard PK, Holgersen K, Finset A. Communicating with alexithymic and non-alexithymic patients: an experimental study of the effect of psychosocial communication and empathy on patient satisfaction. Psychother Psychosom. 2004;73(2):92–100. [DOI] [PubMed] [Google Scholar]
- 72.Henbest RJ, Stewart MA. Patient-centredness in the consultation. 1: A method for measurement. Fam Pract. 1989;6(4):249–253. [DOI] [PubMed] [Google Scholar]
- 73.Laerum E, Steine S, Finckenhagen M, Finset A. The final version of the Patient Perspective Survey (PPS): a new tool to improve consultation outcome and patient participation in general practice patients with complex health problems. Doctors’ and patients’ evaluation and guidelines for clinical use. Fam Pract. 2002;19(3):264–271. [DOI] [PubMed] [Google Scholar]
- 74.Laerum E, Steine S, Finset A, Lundevall S. Complex health problems in general practice: do we need an instrument for consultation improvement and patient involvement? Theoretical foundation, development and user evaluation of the Patient Perspective Survey (PPS). Fam Pract. 1998;15(2):172–181. [DOI] [PubMed] [Google Scholar]
- 75.Sisler JJ, Brown JB, Stewart M. Family physicians’ roles in cancer care. Survey of patients on a provincial cancer registry. Can Fam Physician. 2004;50:889–896. [PMC free article] [PubMed] [Google Scholar]
- 76.Zandbelt LC, Smets EM, Oort FJ, Godfried MH, de Haes HC. Medical specialists’ patient-centered communication and patient-reported outcomes. Med Care. 2007;45(4):330–339. [DOI] [PubMed] [Google Scholar]
- 77.Shields CG, Franks P, Fiscella K, Meldrum S, Epstein RM. Rochester Participatory Decision-Making scale (RPDA): reliability and validity. Ann Fam Med. 2005;3(5):436–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wright J. Developing a tool to assess person-centred continence care. Nurs Older People. 2006;18(6):23–28. [PubMed] [Google Scholar]
- 79.Bethel S, Ridder J. Evaluating nursing practice: satisfaction at what cost? Nurs Manage. 1994;25(9):41–43, 46–48. [PubMed] [Google Scholar]
- 80.Ong LML, Visser MRM, Lammes FB, de Haes JCJM. Doctor-patient communication and cancer patients’ quality of life and satisfaction. Patient Educ Couns. 2000;41(2):145–156. [DOI] [PubMed] [Google Scholar]
- 81.Cassell EJ. Teaching the fundamentals of primary care: a point of view. Milbank Q. 1995;73(3):373–405. [PubMed] [Google Scholar]
- 82.Cegala DJ, Gade C, Lenzmeier Broz S, McClure L. Physicians’ and patients’ perceptions of patients’ communication competence in a primary care medical interview. Health Commun. 2004;16(3):289–304. [DOI] [PubMed] [Google Scholar]
- 83.Edvardsson D, Sandman PO, Rasmussen B. Swedish language Person-centred Climate Questionnaire - patient version: construction and psychometric evaluation. J Adv Nurs. 2008;63(3):302–309. [DOI] [PubMed] [Google Scholar]
- 84.Ryan ME, Collins FJ, Dowd JB, Pierce PK. Measuring patient satisfaction: a case study. J Nurs Care Qual. 1995;9(2):44–53. [DOI] [PubMed] [Google Scholar]
- 85.Wilde B, Larsson G, Larsson M, Starrin B. Quality of care. Development of a patient-centred questionnaire based on a grounded theory model. Scand J Caring Sci. 1994;8(1):39–48. [DOI] [PubMed] [Google Scholar]
- 86.Gesell SB, Wolosin RJ. Inpatients’ ratings of care in 5 common clinical conditions. Qual Manag Health Care. 2004;13(4):222–227. [DOI] [PubMed] [Google Scholar]
- 87.Picker Foundation. Eight dimensions of patient-centered care. http://www.nrcpicker.com/Measurement/Understanding%20PCC/Pages/DimensionsofPatient-CenteredCare.aspx. Accessed Sep 10, 2010.
- 88.Laschinger HS, Hall LM, Pedersen C, Almost J. A psychometric analysis of the patient satisfaction with nursing care quality questionnaire: an actionable approach to measuring patient satisfaction. J Nurs Care Qual. 2005;20(3):220–230. [DOI] [PubMed] [Google Scholar]
- 89.Poochikian-Sarkissian S, Wennberg RA, Sidani S. Examining the relationship between patient-centred care and outcomes on a neuroscience unit: a pilot project. Can J Neurosci Nurs. 2008;30(2):14–19. [PubMed] [Google Scholar]
- 90.Hiidenhovi H, Laippala P, Nojonen K. Development of a patient-orientated instrument to measure service quality in outpatient departments. J Adv Nurs. 2001;34(5):696–705. [DOI] [PubMed] [Google Scholar]
- 91.Dirkzwager AJ, Verhaak PF. Patients with persistent medically unexplained symptoms in general practice: characteristics and quality of care. BMC Fam Pract. 2007;8(33):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Flach SD, McCoy KD, Vaughn TE, Ward MM, Bootsmiller BJ, Doebbeling BN. Does patient-centered care improve provision of preventive services? J Gen Intern Med. 2004;19(10):1019–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mallinger JB, Griggs JJ, Shields CG. Patient-centered care and breast cancer survivors’ satisfaction with information. Patient Educ Couns. 2005;57(3):342–349. [DOI] [PubMed] [Google Scholar]
- 94.Little P, Everitt H, Williamson I, et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ. 2001;322(7284):468–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Smith F, Orrell M. Does the patient-centred approach help identify the needs of older people attending primary care? Age Ageing. 2007;36(6):628–631. [DOI] [PubMed] [Google Scholar]
- 96.Galassi JP, Ware W, Schanberg R. The Patient Reactions Assessment: a brief measure of the quality of the patient-provider medical relationship. Psychol Assess. 1992;4(3):346–351. [Google Scholar]
- 97.Lerman CE, Brody DS, Caputo GC, Smith DG, Lazaro CG, Wolfson HG. Patients’ Perceived Involvement in Care Scale: relationship to attitudes about illness and medical care. J Gen Intern Med. 1990;5(1):29–33. [DOI] [PubMed] [Google Scholar]
- 98.Loh A, Simon D, Wills CE, Kriston L, Niebling W, Härter M. The effects of a shared decision-making intervention in primary care of depression: a cluster-randomized controlled trial. Patient Educ Couns. 2007;67(3):324–332. [DOI] [PubMed] [Google Scholar]
- 99.Flocke SA. Measuring attributes of primary care: development of a new instrument. J Fam Pract. 1997;45(1):64–74. [PubMed] [Google Scholar]
- 100.Flocke SA, Stange KC, Zyzanski SJ. The association of attributes of primary care with the delivery of clinical preventive services. Med Care. 1998;36(8)(Suppl):AS21–AS30. [DOI] [PubMed] [Google Scholar]
- 101.Flocke SA, Orzano AJ, Selinger HA, et al.; Ambulatory Sentinel Practice Network. Does managed care restrictiveness affect the perceived quality of primary care? A report from ASPN. J Fam Pract. 1999;48(10):762–768. [PubMed] [Google Scholar]
- 102.Cegala DJ, Coleman MT, Turner JW. The development and partial assessment of the medical communication competence scale. Health Commun. 1998;10(3):261–288. [DOI] [PubMed] [Google Scholar]
- 103.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36(5):728–739. [DOI] [PubMed] [Google Scholar]
- 104.Safran DG, Karp M, Coltin K, et al. Measuring patients’ experiences with individual primary care physicians. Results of a statewide demonstration project. J Gen Intern Med. 2006;21(1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Duberstein P, Meldrum S, Fiscella K, Shields CG, Epstein RM. Influences on patients’ ratings of physicians: Physicians demographics and personality. Patient Educ Couns. 2007;65(2):270–274. [DOI] [PubMed] [Google Scholar]
- 106.Stewart AL, Nápoles-Springer A, Pérez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77(3):305–339, 274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Stewart AL, Nápoles-Springer AM, Gregorich SE, Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv Res. 2007;42(3 Pt 1)(3, Part I):1235–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ramsay J, Campbell JL, Schroter S, Green J, Roland M. The General Practice Assessment Survey (GPAS): tests of data quality and measurement properties. Fam Pract. 2000;17(5):372–379. [DOI] [PubMed] [Google Scholar]
- 109.Jayasinghe UW, Proudfoot J, Holton C, et al. Chronically ill Australians’ satisfaction with accessibility and patient-centredness. Int J Qual Health Care. 2008;20(2):105–114. [DOI] [PubMed] [Google Scholar]
- 110.Haddad S, Potvin L, Roberge D, Pineault R, Remondin M. Patient perception of quality following a visit to a doctor in a primary care unit. Fam Pract. 2000;17(1):21–29. [DOI] [PubMed] [Google Scholar]
- 111.Shi L, Starfield B, Xu J. Validating the adult primary care assessment tool. J Fam Pract. 2001;50(2):161–175. [Google Scholar]
- 112.Haggerty JL, Pineault R, Beaulieu MD, et al. Practice features associated with patient-reported accessibility, continuity, and coordination of primary health care. Ann Fam Med. 2008;6(2):116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mercer SW, Maxwell M, Heaney D, Watt GC. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21(6):699–705. [DOI] [PubMed] [Google Scholar]
- 114.Mercer SW, McConnachie A, Maxwell M, Heaney D, Watt GC. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam Pract. 2005;22(3):328–334. [DOI] [PubMed] [Google Scholar]
- 115.Mercer SW, Neumann M, Wirtz M, Fitzpatrick B, Vojt G. General practitioner empathy, patient enablement, and patient-reported outcomes in primary care in an area of high socio-economic deprivation in Scotland—a pilot prospective study using structural equation modeling. Patient Educ Couns. 2008;73(2):240–245. [DOI] [PubMed] [Google Scholar]
- 116.Campbell C, Lockyer J, Laidlaw T, Macleod H. Assessment of a matched-pair instrument to examine doctor-patient communication skills in practising doctors. Med Educ. 2007;41(2):123–129. [DOI] [PubMed] [Google Scholar]
- 117.Patient-Centered Primary Care Collaborative. Joint principles of the Patient-Centered Medical Home. http://www.pcpcc.net/content/joint-principles-patient-centered-medical-home. Accessed Sep 10, 2010.
- 118.AAFP News Now. Medical home concept gains prominence thanks to Academy’s efforts. Ann Fam Med. 2007;5(4):378–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Patient-centered primary care in Canada. http://www.cfpc.ca/local/files/Communications/Health%20Policy/Bring%20it%20on%20Home%20FINAL%20ENGLISH.pdf. Accessed Sep 15, 2010.
- 120.American Academy of Family Physicians. Patient-Centered Medical Home. http://www.aafp.org/online/en/home/membership/initiatives/pcmh.html. Accessed Sep 10, 2010.
- 121.Audet AM, Davis K, Schoenbaum SC. Adoption of patient-centered care practices by physicians: results from a national survey. Arch Intern Med. 2006;166(7):754–759. [DOI] [PubMed] [Google Scholar]