Abstract
Biological scaffolds composed of extracellular matrix (ECM) have been shown to be resistant to deliberate bacterial contamination in preclinical in vivo studies. The present study evaluated the degradation products resulting from the acid digestion of ECM scaffolds for antibacterial effects against clinical strains of Staphylococcus aureus and Escherichia coli. The ECM scaffolds were derived from porcine urinary bladder (UBM-ECM) and liver (L-ECM). These biological scaffolds were digested with acid at high temperatures, fractionated using ammonium sulfate precipitation, and tested for antibacterial activity in a standardized in vitro assay. Degradation products from both UBM-ECM and L-ECM demonstrated antibacterial activity against both S. aureus and E. coli. Specific ammonium sulfate fractions that showed antimicrobial activity varied for the 2 different ECM scaffold types. The results of this study suggest that several different low-molecular-weight peptides with antibacterial activity exist within ECM and that these peptides may help explain the resistance to bacterial infection provided by such biological scaffolds.
INTRODUCTION
Biological scaffolds composed of extracellular matrix (ECM) have been successfully used as templates for the constructive remodeling of numerous tissues in preclinical studies and human clinical applications.1–12 Such biological scaffolds have been surprisingly resistant to bacterial infection,13–16 even in clinical applications that are at high risk for bacterial contamination.17–20 Generally, naturally occurring biomaterials such as those composed of purified collagen or intact ECM are more resistant to bacterial infection than synthetic biomaterials.13–16, 21
Porcine-derived ECM composed of small intestinal sub-mucosa (SIS) has been successfully used as a resorbable biological scaffold for tissue-engineering applications in more than 500,000 human patients and has shown resistance to deliberate bacterial infection in preclinical studies.13–16 The antibacterial activity associated with the SIS-ECM is not a property of the intact ECM itself,22 but rather of the degradation products of the ECM.23 In vitro studies have shown that acid/heat-digested SIS-ECM and acid/heat-digested urinary bladder submucosa (UBS)-ECM possess antibacterial activity against gram-positive S. aureus and gram-negative E. coli. The greatest antibacterial activity appears to be present in degradation peptides between 5 and 16 kDa.23
The objective of the present study was to determine whether antimicrobial activity similar to that found in SIS-ECM and UBS-ECM is detectable in the degradation products of ECM scaffolds derived from the liver (L-ECM) and superficial layers (tunica propria and basement membrane) of the porcine urinary bladder (UBM-ECM). These ECM materials have been studied as biological scaffolds for tissue engineering/regenerative medicine applications, and the presence of such activity within these materials could have significant clinical applications.
MATERIALS AND METHODS
Preparation of ECM powders
Porcine urinary bladders and livers were harvested from market-weight pigs (~110–130 kg) immediately after euthanasia. UBM-ECM was prepared as previously described.24–26 In brief, connective and adipose tissue were removed from the serosal surface of the bladder, and the tunica serosa, tunica muscularis externa, tunica submucosa, and most of the tunica muscularis mucosa were mechanically removed. The luminal urothelial cells of the tunica mucosa were dissociated by soaking in a 1.0-N saline solution, leaving a biomaterial composed of only the basement membrane and the subjacent tunica propria of the tunica mucosa and the resident cell population of those 2 layers.
L-ECM was prepared by slicing lobes of porcine liver to 5-mm sections, then rinsing the slices in deionized water with agitation on an orbital shaker for a total of three 30-min rinses. Slices were then placed on a polypropylene mesh and subjected to uniform pressure to burst the hepatocytes. The tissue slices were returned to a flask and submerged in 0.02% trypsin/0.05% ethylenediaminetetraacetic acid for 1 h at 37°C, agitated at room temperature in 3% (v/v) Triton X-100 for 1 h and then in 4% (w/v) deoxycholic acid for 1 h. Tissue slices were rinsed with deionized water and massaged between each treatment step.26
Both types of ECM were decellularized using treatment with 0.1% peracetic acid/4% ethanol for 2 h and rinsed with phosphate buffered saline (PBS) and deionized water. Complete decellularization was confirmed using 4′-6-diamidino-2-phenylindole nuclear staining and hematoxylin and eosin staining. The ECMs were then lyophilized in sheet form and frozen. The frozen sheets were comminuted into a particulate form using a Waring commercial blender and Wiley Mill with a #60 mesh screen.25
Degradation of ECM
ECM was digested using mild acid and heat. Adapting a previously described procedure,23 lyophilized, particulate ECM was hydrated by placing 10 mg dry weight of ECM in 140 mL of 1× PBS with protease inhibitors (5 mM benzamide, 1 mM phenylmethanesulfonyl fluoride (PMSF), and 10 mM N-ethylmaleimide) and stirring for 1 to 2 h, then filtering with vacuum through Whatman #42 filter paper in a Buchner funnel. The retentate material, which remained hydrated, was collected and suspended in 110 mL of 0.5-N acetic acid. The suspension was transferred to a stirred, glass-lined autoclave reactor (Autoclave Engineers, Erie, PA), heated to 120°C over 55 min, and held at 120°C for 30 min with constant stirring. The suspension was then cooled to 60°C in 2 to 4 min and then to room temperature in 15 to 20 min. The acid-digested suspension was then removed from the autoclave reactor and filtered in series, through cheesecloth, Fischer P8 filter paper, and Whatman #42 filter paper, with the use of vacuum for the last 2 filtration steps. The filtrate material was collected and snap frozen on dry ice and ethanol at an angle to maximize surface area. Samples were lyophilized, yielding a dry ECM digest that could withstand long-term storage.
Ammonium sulfate precipitation of ECM digests
The lyophilized ECM digest was resuspended in 0.1 M sodium phosphate/0.15 M sodium chloride, pH 6.8, with 2 mM PMSF (re-suspension buffer) at 200 mg dry sample mass per mL. The sample was rocked at room temperature for 45 min to re-suspend, centrifuged at 12,000 rpm for 1 h, and finally filtered through a 0.45-μm syringe filter. A bicinchoninic acid assay (Pierce Biotechnology, Rockford, IL) was performed to estimate protein concentration of the suspension. The suspension was then diluted with re-suspension buffer to a concentration of 10 mg protein per mL. Ammonium sulfate was added to the suspension to saturation percentages of 10%, 20%, 30%, 40%, 50%, 60%, 70%, 80%, and 100%. The saturation percentage was slowly increased 10% daily with constant stirring at 4°C to avoid localized precipitation of proteins. At each percentage mark, the solution was centrifuged at 12,000 rpm, resulting in the formation of a firm pellet. The supernatant was removed from the tubes and stored at 4°C overnight. Two mM of fresh PMSF was added the following morning before adding additional salt. The precipitated pellets were resuspended in resuspension buffer, snap frozen, and stored at −80°C. Samples of the supernatants and resuspended pellets were desalted, concentrated, and pH neutralized using Microcon YM-3 centrifugal filter devices, with a 3-kD molecular-weight cutoff (Millipore, Billerica, MA). Desalted samples were snap frozen and stored at −80°C for further analysis.
Antimicrobial assay
Tryptic soy agar plates were streaked with Staphylococcus aureus (American Type Culture Collection 29213, wound isolate) and Escherichia coli (American Type Culture Collection 25922, clinical isolate), and an isolated colony from each was used to inoculate 10 mL of tryptic soy broth. The bacteria were grown in suspension overnight in a 37°C shaker. The bacteria were then diluted to 5×105 CFU/mL,23 and 150 μL of bacterial suspension were added to each well of a 96-well microplate; 16.5 μL of each sample to be tested for antibacterial activity was added to the bacterial suspension. Samples tested include desalted UBM-ECM or L-ECM digest ammonium sulfate fractions, a one-third dilution of each fraction, a negative control of media alone, and positive controls of antibiotics (vancomycin for S. aureus and tetracycline for E. coli). Each sample was tested in duplicate. The bacterial growth in each well was monitored over the course of 24 h using absorbance readings at 570 nm with a BioRad 680 microplate reader. Statistical significance of the absorbance values between samples was determined using the paired t-test. The absorbance reading of each UBM-ECM or L-ECM fraction was compared with the negative control of media alone for each time point.
RESULTS
Degradation products from UBM-ECM and L-ECM demonstrated antibacterial activity against S. aureus and E. coli. All UBM-ECM and L-ECM digest desalted ammonium sulfate pellets and supernatants were tested for antibacterial activity. Those fractions demonstrating statistically significant inhibition of bacterial growth are shown in Figs. 1, 2, and 3. The most potent antibacterial activity was present in the UBM-ECM pellet precipitated at 60% ammonium sulfate saturation. This sample effectively inhibited S. aureus growth for 24 h (Fig. 1). This same sample also effectively inhibited E. coli growth for 9 h (Fig. 2). The L-ECM digest precipitated with 60% ammonium sulfate showed strong antibacterial activity against E. coli and S. aureus (Figs. 1 and 2). Furthermore, the L-ECM pellet that precipitated at 40% ammonium sulfate saturation showed the greatest activity of all samples tested against S. aureus, inhibiting growth for the full 24 h of the assay (Fig. 1). These results suggest that there are multiple antibacterial molecules present in ECM degradation products and that differences exist between antimicrobial peptides present in L-ECM and UBM-ECM.
FIG. 1.
Effect of porcine urinary bladder (UBM-ECM) and liver (L-ECM) extracellular matrix digest ammonium sulfate fractions on Staphylococcus aureus growth. All absorbance values were statistically significant compared with the negative control of media with p <0.05 except L-ECM digest 40% pellet at 2 h; L-ECM digest 60% pellet at 2 and 3 h; UBM-ECM digest 20% pellet at 4, 5, 21, and 24 h; and UBM-ECM digest 60% pellet at 1 and 2 h.
FIG. 2.
Effect of porcine urinary bladder (UBM-ECM) and liver (L-ECM) extracellular matrix digest ammonium sulfate fractions on Escherichia coli growth. All absorbance values were statistically significant compared with the negative control of media with p <0.05 except L-ECM digest 40% pellet at 0–4, 13, 23, and 24 h; L-ECM digest 60% pellet at 0–2, 23, and 24 h; UBM-ECM digest 20% pellet at all time points; and UBM-ECM digest 60% pellet at 0, 1, 5, 21, and 24 h.
FIG. 3.
Effect of diluted porcine urinary bladder (UBM-ECM) and liver (L-ECM) extracellular matrix digest ammonium sulfate fractions on Staphylococcus aureus growth. All absorbance values were statistically significant compared with the negative control of media with p <0.05 except L-ECM digest 40% pellet at 1, 2, and 23 h; L-ECM digest 60% pellet at 0–3, and 8–24 h; UBM-ECM digest 20% pellet at 0–2, 4, and 24 h; and UBM-ECM digest 60% pellet at 0, 1, and 4 h.
The ECM digest samples that were diluted one-third showed antibacterial activity only against S. aureus (Fig. 3). The diluted samples of the UBM-ECM digest 60% ammonium sulfate pellet and L-ECM 40% ammonium sulfate pellet were equally as effective at inhibiting bacterial growth as the undiluted samples at the same ammonium sulfate saturation. The diluted L-ECM digest at 60% ammonium sulfate concentration pellet also demonstrated a small amount of antibacterial activity against S. aureus. The UBM-ECM digest pellet that precipitated at 20% ammonium sulfate saturation, which had no measurable antibacterial activity when undiluted, strongly inhibited S. aureus growth when diluted one-third (Fig. 3).
Absorbance readings at t = 0 varied because of the opacity of some samples when added to the bacterial suspension. Some samples contained precipitates that dissolved after incubation with the bacterial suspension. Within a few hours of incubation, these samples no longer appeared to be opaque upon visual inspection; this observation was supported using absorbance readings. After 24 h, the appearance of wells containing samples that demonstrated a strong antibacterial effect showed a striking difference from wells in which bacterial proliferation occurred (Fig. 4).
FIG. 4.
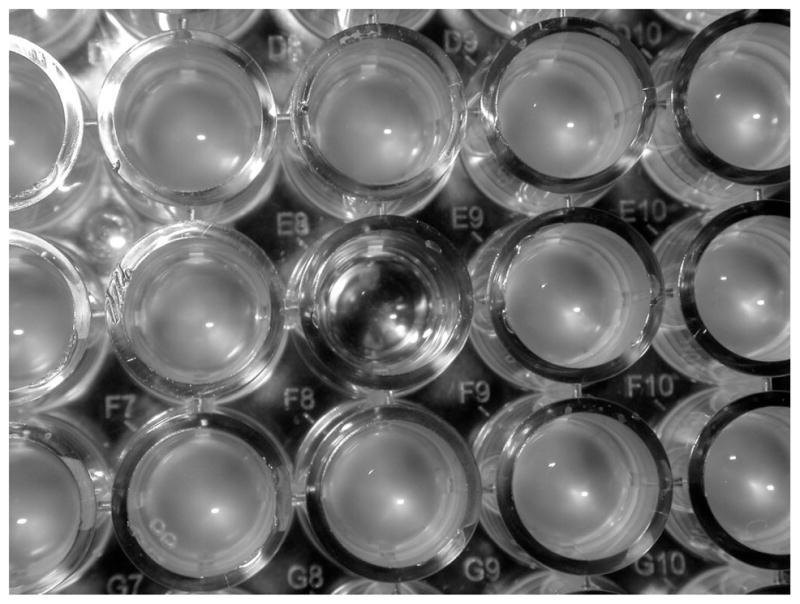
Appearance of microplate containing Staphylococcus aureus after 24-h incubation at 378C. The clear well, E8, contains liver extracellular matrix (L-ECM) digest 40% ammonium sulfate pellet. The surrounding samples did not exhibit strong antibacterial activity.
A preliminary characterization of UBM-ECM and L-ECM fractions that showed antibacterial activity included determination of protein concentration using bicinchoninic acid assay. The UBM-ECM pellets that precipitated at 60% and 20% ammonium sulfate saturation had protein concentrations of approximately 80 mg protein/mL and 90 mg protein/mL, respectively. The L-ECM pellets that precipitated at 40% and 60% ammonium sulfate saturation had protein concentrations of approximately 50 mg protein/mL and 10 mg protein/mL, respectively. SDS-PAGE was performed to estimate the molecular weight of the UBM-ECM fractions that demonstrated antibacterial activity, with an approximate molecular weight range of 7 to 15 kDa.
DISCUSSION
The present study demonstrates that the degradation products of UBM-ECM and L-ECM scaffold materials possess antibacterial activity against S. aureus and E. coli. Urinary bladder–derived ECM has been used in numerous regenerative medicine applications, including bladder regeneration, urethral repair, and esophageal repair.12,27,28 Liver-derived ECM has also been evaluated as a biological scaffold for use in regenerative medicine.29
The antimicrobial peptides present in the degradation products of UBM-ECM and L-ECM were released using acid/heat digestion and fractionated using ammonium sulfate precipitation. Ammonium sulfate precipitation of the degraded ECM resulted in fractions that showed variable degrees of antibacterial activity against S. aureus and E. coli. Certain fractions showed greater antibacterial activity at lower concentrations of total protein. These observations suggest that each ammonium sulfate fraction contains a complex mixture of proteins. This mixture may include antimicrobial peptides as well as inhibitors of those peptides, the combination of which cause a net effect of antibacterial activity when present in specific concentrations. The full spectrum of antimicrobial activity of these low-molecular-weight peptides has not been determined, including their efficacy against anaerobic bacteria.
Certain ammonium sulfate–precipitated fractions from both ECMs maintained strong antibacterial activity against gram-positive S. aureus for a longer period of time than against gram-negative E. coli. Although the antibacterial activity against S. aureus persisted for the full 24 h of the assay, the antibacterial activity against E. coli declined as the antibacterial peptides present in the digest fractions lost activity or were stoichiometrically overwhelmed by the bacteria. The short-term antibacterial effects of ECM degradation products may be particularly beneficial in preventing an implant infection by providing immediate protection while the host inflammatory cell response and humoral immune response become activated. In addition, because the ECM bioscaffold is subjected to progressive degradation in vivo and is remodeled by host tissues, antimicrobial peptides may continue to be released, providing a sustained antibacterial effect.
Degradation of the ECM is one of the earliest events after tissue injury. ECM degrades rapidly and is completely resorbed within 90 days.30–32 Degradation products of ECM derived from several tissues have previously shown biological properties such as antimicrobial, chemotactic, and angiogenic activity.23,33,34 The methods used in the present study to digest the ECM cause cleavage of inactive parent molecules and the production of bioactive fragment molecules. The degradation products of several types of collagen, fibronectin, and laminin are known to produce fragment molecules with angiogenic, antiangiogenic, and chemotactic properties.34,35–39 The present study suggests that antimicrobial activity can be added to the list of bioactive properties that result from ECM degradation. The harsh in vitro methods used in the present study may or may not relate to the degradation of ECM bioscaffolds that occurs in vivo. It seems improbable that the acid/heat digestion of different types of ECM would by chance produce bioactive peptides that are not created by physiological degradation processes. It remains to be shown, however, that in vivo degradation mechanisms generate the same types of bioactive peptides.
Naturally occurring antimicrobial peptides (AMPs) that play key roles in innate immunity have been isolated from plants (thionins), several insect orders (cecropins), amphibians (magainins), and mammals (defensins). Most AMPs have certain common features, including small size (12–100 amino acid residues), polycationic charge, amphipathic structure, and a common mechanism for killing bacteria, which involves direct electrostatic interaction with microbial cell membranes, followed by physical disruption of the membrane.40 Most AMPs are produced as part of the innate immune defense system and stored in the granules of cells involved in immune response. AMPs are synthesized as propeptides that are activated by proteolytic cleavage, releasing the active antimicrobial peptide, which may have microbicidal effects against gram-negative bacteria, gram-positive bacteria, yeast, and enveloped viruses.40,41
At least 18 AMPs, with a broad range of antimicrobial activity, have been identified from various porcine cells and tissues.40,42–44 The upper portion of porcine small intestine, when immersed in boiling water, frozen, and extracted with cold 0.5 M acetic acid,45 has been shown to possess several AMPs.42–44 Using this method, a cecropin-like AMP with activity against E. coli and other gram-negative bacteria was the first porcine AMP to be purified and identified, in 1989.42 Since then, additional porcine AMPs have been isolated from the small intestine,43,44 as well as from polymorphonuclear leukocytes and lymphocytes.40 It may not be surprising then that in vitro and in vivo antimicrobial activity was found in the SIS-ECM biological scaffold.13–16,23 One porcine defensin, pBD-1, was cloned and found to be expressed by the epithelia of the gastrointestinal and respiratory tracts as well as in urinary bladder, liver, skin, kidney, lymph node, and others.46
Naturally occurring AMPs that have been identified from porcine sources generally have molecular weights of less than 10kD,40 which coincides with the 5- to 16-kD molecular-weight range of the fraction of SIS-ECM and UBS-ECM extracts that possess antimicrobial activity.23 The present study shows that the UBM-ECM and L-ECM antibacterial peptides also exist within this molecular weight range, based on sodium dodecyl sulfate polyacrylamide gel electrophoresis analysis (not shown). However it is unknown whether the ECM-derived antibacterial peptides are the same as any of the already identified porcine AMPs or represent novel AMPs. Further purification, isolation, and identification of these antimicrobial peptides from ECM degradation products will better elucidate the mechanism by which they are produced and their in vivo functionality.
Antibacterial activity has now been shown in 4 different types of non—chemically cross-linked ECMs, suggesting that this biological activity may be a common feature of all ECMs. The findings of the present study lend support to the use of ECM biological scaffolds for regenerative medicine applications, particularly for use in sites with high potential for bacterial contamination.
References
- 1.Badylak SF, Lantz GC, Coffey A, Geddes LA. Small intestinal submucosa as a large diameter vascular graft in the dog. J Surg Res. 1989;47:74. doi: 10.1016/0022-4804(89)90050-4. [DOI] [PubMed] [Google Scholar]
- 2.Badylak SF, Tullius R, Kokini K, Shelbourne KD, Klootwyk T, Voytik SL, Kraine MR, Simmons C. The use of xenogeneic small intestinal submucosa as a biomaterial for Achilles tendon repair in a dog model. J Biomed Mater Res. 1995;29:977. doi: 10.1002/jbm.820290809. [DOI] [PubMed] [Google Scholar]
- 3.Badylak SF, Meurling S, Chen M, Spievack A, Simmons-Byrd A. Resorbable bioscaffold for esophageal repair in a dog model. J Pediatr Surg. 2000;35:1097. doi: 10.1053/jpsu.2000.7834. [DOI] [PubMed] [Google Scholar]
- 4.Badylak SF, Obermiller J, Geddes L, Matheny R. Extracellular matrix for myocardial repair. Heart Surg Forum. 2003;6:E20. doi: 10.1532/hsf.917. [DOI] [PubMed] [Google Scholar]
- 5.Vaught JD, Kropp BP, Sawyer BD, Rippy MK, Badylak SF, Shannon HE, Thor KB. Detrusor regeneration in the rat using porcine small intestinal submucosal grafts: functional innervation and receptor expression. J Urol. 1996;155:374. [PubMed] [Google Scholar]
- 6.Kropp BP, Rippy MK, Badylak SF, Adams MC, Keating MA, Rink RC, Thor KB. Regenerative urinary bladder augmentation using small intestinal submucosa: urodynamic and histopathologic assessment in long-term canine bladder augmentations. J Urol. 1996;155:2098. doi: 10.1016/s0022-5347(01)66117-2. [DOI] [PubMed] [Google Scholar]
- 7.Kropp BP, Eppley BL, Prevel CD, Rippy MK, Harruff RC, Badylak SF, Adams MC, Rink RC, Keating MA. Experimental assessment of small intestinal submucosa as a bladder wall substitute. Urology. 1995;46:396. doi: 10.1016/S0090-4295(99)80227-1. [DOI] [PubMed] [Google Scholar]
- 8.Dahms SE, Piechota HJ, Nunes L, Dahiya R, Lue TF, Tanagho EA. Free ureteral replacement in rats: regeneration of ureteral wall components in the acellular matrix graft. Urology. 1997;50:818. doi: 10.1016/S0090-4295(97)00391-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Atala A. Experimental and clinical experience with tissue engineering techniques for urethral reconstruction. Urol Clin North Am. 2002;29:485. doi: 10.1016/s0094-0143(02)00033-2. [DOI] [PubMed] [Google Scholar]
- 10.Dejardin LM, Arnoczky SP, Clarke RB. Use of small intestinal submucosal implants for regeneration of large fascial defects: an experimental study in dogs. J Biomed Mater Res. 1999;46:203. doi: 10.1002/(sici)1097-4636(199908)46:2<203::aid-jbm9>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 11.Badylak SF. Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol. 2004;12:367. doi: 10.1016/j.trim.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 12.Badylak SF, Vorp DA, Spievack AR, Simmons-Byrd A, Hanke J, Freytes DO, Thapa A, Gilbert TW, Nieponice A. Esophageal reconstruction with ECM and muscle tissue in a dog model. J Surg Res. 2005;128:87. doi: 10.1016/j.jss.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Badylak SF, Wu CC, Bible M, McPherson E. Host protection against deliberate bacterial contamination of an extracellular matrix bioscaffold versus Dacron™ mesh in a dog model of orthopedic soft tissue repair. J Biomed Mater Res B Appl Biomater. 2003;67:648. doi: 10.1002/jbm.b.10062. [DOI] [PubMed] [Google Scholar]
- 14.Badylak SF, Coffey AC, Lantz GC, Tacker WA, Geddes LA. Comparison of the resistance to infection of intestinal submucosa arterial autografts versus polytetrafluoroethylene arterial prostheses in a dog model. J Vasc Surg. 1994;19:465. doi: 10.1016/s0741-5214(94)70073-7. [DOI] [PubMed] [Google Scholar]
- 15.Shell DH, 4th, Croce MA, Cagiannos C, Jernigan TW, Edwards N, Fabian TC. Comparison of small-intestinal submucosa and expanded polytetrafluoroethylene as a vascular conduit in the presence of gram-positive contamination. Ann Surg. 2005;241:995. doi: 10.1097/01.sla.0000165186.79097.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jernigan TW, Croce MA, Cagiannos C, Shell DH, Handorf CR, Fabian TC. Small intestinal submucosa for vascular reconstruction in the presence of gastrointestinal contamination. Ann Surg. 2004;239:733. doi: 10.1097/01.sla.0000124447.30808.c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruiz CE, Iemura M, Medie S, Varga P, Van Alstine WG, Mack S, Deligio A, Fearnot N, Beier UH, Pavcnik D, Hijazi ZM, Kiupel M. Transcatheter placement of a low-profile biodegradable pulmonary valve made of small intestinal submucosa: A long-term study in a swine model. J Thorac Cardiovasc Surg. 2005:130–477. doi: 10.1016/j.jtcvs.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Kim BS, Baez CE, Atala A. Biomaterials for tissue engineering. World J Urol. 2000;18:2. doi: 10.1007/s003450050002. [DOI] [PubMed] [Google Scholar]
- 19.Mantovani F, Trinchieri A, Castelnuovo C, Romano AL, Pisani E. Reconstructive urethroplasty using porcine acellular matrix. Eur Urol. 2003;44:600. doi: 10.1016/s0302-2838(03)00212-4. [DOI] [PubMed] [Google Scholar]
- 20.Kim MS, Hong KD, Shin HW, Kim SH, Kim SH, Lee MS, Jang WY, Khang G, Lee HB. Preparation of porcine small intestinal submucosa sponge and their application as a wound dressing in full-thickness skin defect of rat. Int J Biol Macromol. 2005;36:54. doi: 10.1016/j.ijbiomac.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Carlson GA, Dragoo JL, Samimi B, Bruckner DA, Bernard GW, Hedrick M, Benhaim P. Bacteriostatic properties of biomatrices against common orthopaedic pathogens. Biochem Biophys Res Commun. 2004;321:472. doi: 10.1016/j.bbrc.2004.06.165. [DOI] [PubMed] [Google Scholar]
- 22.Holtom PD, Shinar Z, Benna J, Patzakis MJ. Porcine small intestine submucosa does not show antimicrobial properties. Clin Orthop Relat Res. 2004;427:18. doi: 10.1097/01.blo.0000143573.03645.b4. [DOI] [PubMed] [Google Scholar]
- 23.Sarikaya A, Record R, Wu C, Tullius B, Badylak S, Ladisch M. Antimicrobial activity associated with extracellular matrices. Tissue Eng. 2002;8:63. doi: 10.1089/107632702753503063. [DOI] [PubMed] [Google Scholar]
- 24.Freytes DO, Tullius RS, Badylak SF. The effect of storage upon material properties of lyophilized porcine extracellular matrix derived from the urinary bladder. J Biomed Mater Res B Appl Biomater. 2005 Dec 19; doi: 10.1002/jbm.b.30491. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Gilbert TW, Stolz DB, Biancaniello F, Simmons-Byrd A, Badylak SF. Production and characterization of ECM powder: implications for tissue engineering applications. Biomaterials. 2005;26:1431. doi: 10.1016/j.biomaterials.2004.04.042. [DOI] [PubMed] [Google Scholar]
- 26.Brown B, Lindberg K, Reing J, Beer Stolz D, Badylak SF. The basement membrane component of biologic scaffolds derived from extracellular matrix. Tissue Eng. 2006;12:519. doi: 10.1089/ten.2006.12.519. [DOI] [PubMed] [Google Scholar]
- 27.Piechota HJ, Gleason CA, Dahms SE, Dahiya R, Nunes LS, Lue TF, Tanagho EA. Bladder acellular matrix graft: in vivo functional properties of the regenerated rat bladder. Urol Res. 1999;27:206. doi: 10.1007/s002400050111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sievert KD, Bakircioglu ME, Nunes L, Tu R, Dahiya R, Tanagho EA. Homologous acellular matrix graft for urethral reconstruction in the rabbit: histological and functional evaluation. J Urol. 2000;163:1958. [PubMed] [Google Scholar]
- 29.Lin P, Chan WC, Badylak SF, Bhatia SN. Assessing porcine liver-derived biomatrix for hepatic tissue engineering. Tissue Eng. 2004;10:1046. doi: 10.1089/ten.2004.10.1046. [DOI] [PubMed] [Google Scholar]
- 30.Badylak SF, Kropp B, McPherson T, Liang H, Snyder PW. Small intestinal submucosa: a rapidly resorbed bioscaffold for augmentation cystoplasty in a dog model. Tissue Eng. 1998;4:379. doi: 10.1089/ten.1998.4.379. [DOI] [PubMed] [Google Scholar]
- 31.Record RD, Hillegonds D, Simmons C, Tullius R, Rickey FA, Elmore D, Badylak SF. In vivo degradation of 14C-labeled small intestinal submucosa (SIS) when used for urinary bladder repair. Biomaterials. 2001;22:2653. doi: 10.1016/s0142-9612(01)00007-2. [DOI] [PubMed] [Google Scholar]
- 32.Gilbert TW, Stewart-Akers AM, Simmons-Byrd A, Badylak SF. Degradation and remodeling of small intestinal submucosa in canine Achilles tendon repair. JBJS—Am. doi: 10.2106/JBJS.E.00742. (submitted) [DOI] [PubMed] [Google Scholar]
- 33.Li F, Li W, Johnson S, Ingram D, Yoder M, Badylak S. Low-molecular-weight peptides derived from extracellular matrix as chemoattractants for primary endothelial cells. Endothelium. 2004;11:199. doi: 10.1080/10623320490512390. [DOI] [PubMed] [Google Scholar]
- 34.Haviv F, Bradley MF, Kalvin DM, Schneider AJ, Davidson DJ, Majest SM, McKay LM, Haskell CJ, Bell RL, Nguyen B, Marsh KC, Surber BW, Uchic JT, Ferrero J, Wang YC, Leal J, Record RD, Hodde J, Badylak SF, Lesniewski RR, Henkin J. Thrombospondin-1 mimetic peptide inhibitors of angiogenesis and tumor growth: design, synthesis, and optimization of pharmacokinetics and biological activities. J Med Chem. 2005;48:2838. doi: 10.1021/jm0401560. [DOI] [PubMed] [Google Scholar]
- 35.Cornelius LA, Nehring LC, Harding E, Bolanowski M, Welgus HG, Kobayashi DK, Pierce RA, Shapiro SD. Matrix metalloproteinases generate angiostatin: effects on neovascularization. J Immunol. 1998;161:6845. [PubMed] [Google Scholar]
- 36.Mott JD, Werb Z. Regulation of matrix biology by matrix metalloproteinases. Curr Opin Cell Biol. 2004;16:558. doi: 10.1016/j.ceb.2004.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schenk S, Quaranta V. Tales from the crypt[ic] sites of the extracellular matrix. Trends Cell Biol. 2003;13:366. doi: 10.1016/s0962-8924(03)00129-6. [DOI] [PubMed] [Google Scholar]
- 38.Ortega N, Werb Z. New functional roles for non-collagenous domains of basement membrane collagens. J Cell Sci. 2002;115:4201. doi: 10.1242/jcs.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.O’Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS, Flynn E, Birkhead JR, Olsen BR, Folkman J. Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell. 1997;88:277. doi: 10.1016/s0092-8674(00)81848-6. [DOI] [PubMed] [Google Scholar]
- 40.Zhang G, Ross CH, Blecha F. Porcine antimicrobial peptides: New prospects for ancient molecules of host defense. Vet Res. 2000;31:277. doi: 10.1051/vetres:2000121. [DOI] [PubMed] [Google Scholar]
- 41.Carretero M, Del Rio M, Garcia M, Escamez MJ, Mirones I, Rivas L, Balague C, Jorcano JL, Larcher F. A cutaneous gene therapy approach to treat infection through keratinocyte-targeted overexpression of antimicrobial peptides. FASEB J. 2004;18:1931. doi: 10.1096/fj.04-1515fje. [DOI] [PubMed] [Google Scholar]
- 42.Lee JY, Boman A, Chuanxin S, Andersson M, Jornvall H, Mutt V, Boman HG. Antibacterial peptides from pig intestine: isolation of a mammalian cecropin. Proc Natl Acad Sci U S A. 1989;86:9159. doi: 10.1073/pnas.86.23.9159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agerberth B, Lee JY, Bergman T, Carlquist M, Boman HG, Mutt V, Jornvall H. Amino acid sequence of PR-39. Isolation from pig intestine of a new member of the family of proline-arginine-rich antibacterial peptides. Eur J Biochem. 1991;202:849. doi: 10.1111/j.1432-1033.1991.tb16442.x. [DOI] [PubMed] [Google Scholar]
- 44.Agerberth B, Boman A, Andersson M, Jornvall H, Mutt V, Boman HG. Isolation of three antibacterial peptides from pig intestine: gastric inhibitory polypeptide(7–42), diazepam-binding inhibitor(32–86), and a novel factor, peptide 3910. Eur J Biochem. 1993;216:623. doi: 10.1111/j.1432-1033.1993.tb18182.x. [DOI] [PubMed] [Google Scholar]
- 45.Chen ZW, Agerberth B, Gell K, Andersson M, Mutt V, Ostenson CG, Efendic S, Barros-Soderling J, Persson B, Jornvall H. Isolation and characterization of porcine diazepam-binding inhibitor, a polypeptide not only of cerebral occurrence but also common in intestinal tissues and with effects on regulation of insulin release. Eur J Biochem. 1988;174:239. doi: 10.1111/j.1432-1033.1988.tb14088.x. [DOI] [PubMed] [Google Scholar]
- 46.Zhang G, Wu H, Shi J, Ganz T, Ross CR, Blecha F. Molecular cloning and tissue expression of porcine beta-defensin-1. FEBS Lett. 1998;424:37. doi: 10.1016/s0014-5793(98)00134-3. [DOI] [PubMed] [Google Scholar]





