Abstract
Saliva provides a useful and non-invasive alternative to blood for many biomedical diagnostic assays. The level of the hormone cortisol in blood and saliva is related to the level of stress. We present here the development of a portable surface plasmon resonance (SPR) biosensor system for detection of cortisol in saliva. Cortisol-specific monoclonal antibodies were used to develop a competition assay with a 6-channel portable SPR biosensor designed in our laboratory. The detection limit of cortisol in laboratory buffers was 0.36 ng/ml (1.0 nM). An in-line filter based on diffusion through a hollow fiber hydrophilic membrane served to separate small molecules from the complex macromolecular matrix of saliva prior to introduction to the sensor surface. The filtering flow cell provided in-line separation of small molecules from salivary mucins and other large molecules with only a 29% reduction of signal compared with direct flow of the same concentration of analyte over the sensor surface. A standard curve for detection of cortisol in saliva was generated with a detection limit of 1.0 ng/ml (3.6 nM), sufficiently sensitive for clinical use. The system will also be useful for a wide range of applications where small molecular weight analytes are found in complex matrices.
INTRODUCTION
The steroid hormone cortisol is required for the regulation of blood pressure, cardiovascular function and many metabolic activities. The body regulates cortisol levels by controlling cortisol secretion and production based on levels in the bloodstream.1 An excess of cortisol leads to Cushing’s syndrome with symptoms that include obesity, fatigue as well as skin and bone fragility.2 A deficiency in cortisol leads to Addison’s disease with symptoms including weight loss, fatigue and darkening of skin folds and scars.3 Normal serum levels of cortisol vary on a diurnal cycle from 30 to 140 ng/ml (100 to 500 nM), peaking in early morning.4 Cortisol levels increase in response to physical stresses such as injury and illness as well as psychological stresses including depression and fatigue.5 Measuring serum cortisol levels has become an important diagnostic indicator of overall stress as well as disease state of patients.
Analysis of cortisol in saliva is a useful alternative to the standard method of measuring serum cortisol levels for several reasons. First, serum cortisol measurements include the cortisol bound to transport proteins and albumin while the fraction of free cortisol is thought to be more biologically active.6 Also, levels of salivary cortisol have been shown to correlate well with levels of unbound serum cortisol 7,8, however, overall levels of cortisol in saliva are up to 100-fold lower than in serum.9 Morning salivary cortisol levels range from 1 to 8 ng/ml (3.5 to 27 nM) in healthy adults.9 Finally, methods used for collecting blood may create stress and result in misleading cortisol values.10,11 It is also difficult to collect serum samples over the course of a whole day, while collecting saliva is easy and the samples remain useful for analysis for up to one week following collection.12 Methods for determining salivary cortisol provide an opportunity to increase ease and accuracy in detecting disease or stress level.
Several commercial kits use competitive enzyme-linked immunosorbant assay (cELISA) technology to measure cortisol in saliva, including kits available from Salimetrics (State College, PA) and Orion Diagnostica (Espoo, Finland). The cELISA methods provide accurate and reproducible results, but require several hours for analysis. Other immunoassays have been used to measure salivary cortisol levels including time-resolved fluoroimmunoassay13, rapid quantitative immuno-detection using a lateral flow assay14 and luminescence immunoassays.15,16 These immunoassays also take considerable time or lack quantifiable results. One protocol for detecting salivary cortisol uses liquid chromatography-tandem mass spectrometry but requires a slow cortisol extraction step.17 A near real-time method for detection of cortisol in saliva with little sample preparation has not yet been reported.
Surface plasmon resonance (SPR) detection of cortisol provides a method for rapid measurement of cortisol in saliva. SPR technology measures the changes in refractive index (RI) near the sensor surface in response to molecular interactions. Specific receptor molecules can be immobilized onto the gold sensor surface for detecting target analytes in solution. Binding of targets to the receptors results in measurable changes in RI. Binding of large target analytes such as proteins, viruses, spores and microbes to specific antibodies immobilized on the gold surface is easily monitored in near real time. Due to the significant change in RI occurring when these analytes are bound, labels or amplifying reagents are unnecessary for many SPR applications. A general review of SPR can be found in a book edited by Davies (1996).18 Small organic molecules such as cortisol require different methods for detection since direct binding of small targets to receptor molecules does not result in large changes in RI. As a result, competition or displacement assays are used to detect small analytes at clinically relevant levels. Competition assays are based on the inhibition of antibody binding to immobilized target by free analyte in solution. The SPR competition assay has been used to successfully detect small molecules including the herbicide atrazine19, the pesticides fenitrothion20, DDT, chlorpyrifos and carbaryl21, the pesticide metabolite paraoxon22, the antiepileptic drug phenytoin23, the hormones thyroxine24 and estradiol25, and the shellfish toxin domoic acid.26,27
Here, we report the detection of cortisol in saliva using a portable SPR biosensor and competition-based assays combined with a specially designed flow cell that reduces non-specific binding by retaining large molecules in the sample but delivering small molecular weight analytes to the sensor surface.
EXPERIMENTAL SECTION
Surface plasmon resonance sensor preparation
The gold surfaces of Texas Instruments (TI) Spreetatm 2000 sensor chips (available from ICx Nomadics, Oklahoma City, OK) were sequentially washed with 10% nitric acid for 10 minutes, 95% ethanol for 15 seconds and then distilled water for 15 seconds. Next, 100 μg/ml cortisol-conjugated bovine serum albumin (BSA) (Fitzgerald, Concord, MA) was incubated on the gold surface for 1 hour. After washing with phosphate-buffered saline (PBS), the sensor surfaces were coated with 0.1% casein in PBS for 30 minutes. Following a final wash with PBS, the sensors were coated with a storage reagent containing 2.5% trehalose and 2.5% dextran (average MW 500,000) buffered with 10 mM Tris, pH 8.0 and air dried. Surface-bound reagents are stable for at least a year under these conditions.27 Reference sensors were prepared as above using BSA.
The SPR biosensor
The 6-channel SPR biosensor used in these experiments contained two three-channel TI Spreetatm 2000 sensing chips and has been described previously.27–30 For the initial competition experiments, samples were introduced sequentially through the injection port into the sample loop and allowed to flow under positive pressure at a flow rate of 25 μl/min. over the two sensor surfaces. The temperature of the sensors was maintained at 23 ± 0.01°C. Data were transmitted to a laptop computer and analyzed using TI Multispr software version 10.82.
Analysis of cortisol by competition assay
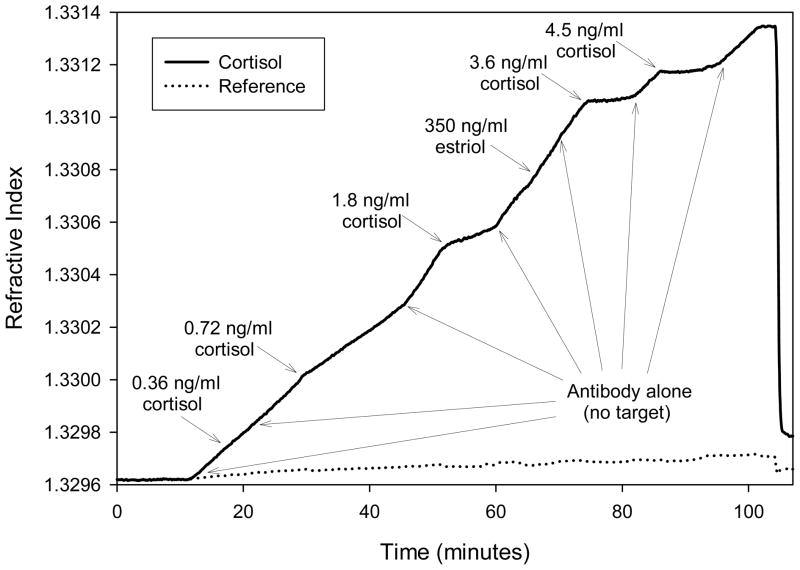
After placing the cortisol-conjugate and reference coated Spreetatm 2000 sensors and into the biosensor system, the sensors were calibrated for RI by exposing the sensor surfaces to aqueous solutions of known RI as described previously.31 PBS was flowed over the sensors to generate a baseline. PBS containing 1:15,000 diluted mouse monoclonal anti-cortisol antibodies (clone XM210 AbCam, Cambridge, UK, 1 mg/ml stock) was flowed over the sensor surfaces for 5 minutes to establish an initial rate of antibody binding. Next, sequential additions of antibodies mixed with known concentrations of cortisol (Sigma, St. Louis, MO), alternating with cortisol-free antibody samples were flowed over the sensors for 5 to 10 minutes (Figure 1). Introduction of the structurally similar steroid hormone estriol mixed with anti-cortisol antibody and then introduced to the sensors demonstrated the specificity of the cortisol antibodies (Figure 1). Cortisol solutions of known concentration were used to generate a standard curve (Figure 2). The sensors were regenerated by desorbing bound antibodies with a 5 minute low pH wash of 100 mM glycine, pH 2.2.
Figure 1.
SPR competition assay for cortisol. The SPR biosensor surfaces were coated with either cortisol-conjugated BSA, or BSA (reference channels). Mouse monoclonal anti-cortisol antibodies were introduced to the sensors at time = 12 minutes. Alternating pretreated samples with varying concentrations of cortisol were pulsed through the flow system. Reduction in binding slopes during antibody binding to the cortisol-conjugated BSA surface was used to measure cortisol. At time = 102 minutes, the sensors were washed with buffer alone, and then sensor surfaces were regenerated (at time = 104 minutes) using 100 mM glycine, pH 2.2. The data from 3 sensor channels were averaged for both the cortisol and reference measurements.
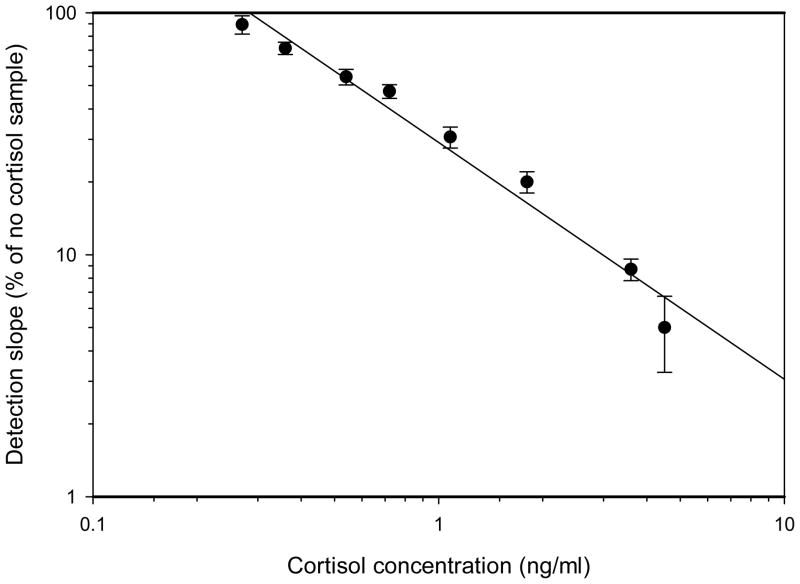
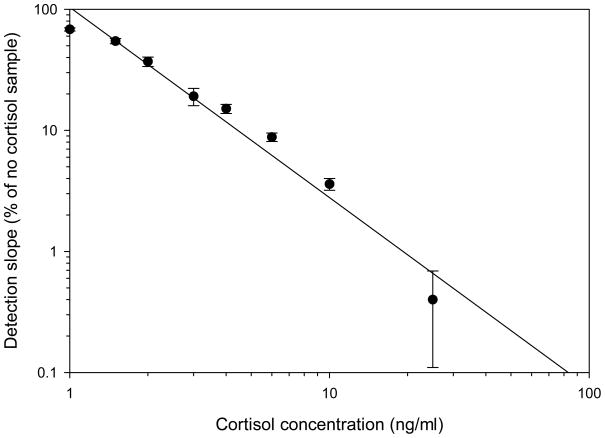
Figure 2.
Standard curve for cortisol detection in laboratory buffer. A log-log plot shows competition data for detection of cortisol in PBS. Error bars represent standard deviations for experiments run in triplicate.
Detection of cortisol in saliva using an in-line filtering flow cell
Collection of saliva was performed using human subjects authorized protocol 02-5536-EA03. Saliva was collected from 7 healthy adults. Volunteers were asked to rinse their mouths and saliva was collected by placing Salivettes (Sarstedt, Newton, NC) into their mouths for 10 minutes. The Salivettes were used according to manufacturer’s instructions. The saliva samples were pooled and frozen in 1 ml aliquots for later use.
A cortisol antibody affinity column was used to generate saliva depleted of endogenous cortisol. Anti-cortisol monoclonal antibodies (0.4 mg) (XM210) were first dialyzed against 1 liter of PBS. The antibodies were then attached to 1 ml of column matrix using an AminoLink Plus immobilization kit (Pierce, Rockford, IL) following the manufacturers instructions. Next, 10 ml saliva was flowed through the cortisol affinity column. The column was regenerated by washing with 100 mM glycine, pH 2.2, equilibrating with PBS and the pooled saliva column flow through was passed through the cortisol affinity column a second time. Cortisol concentrations in the saliva as well as in the column flow through fractions were measured using a Salivary Cortisol Enzyme Immunoassay Kit (Salimetrics, State College, PA) to ensure that all cortisol was removed.
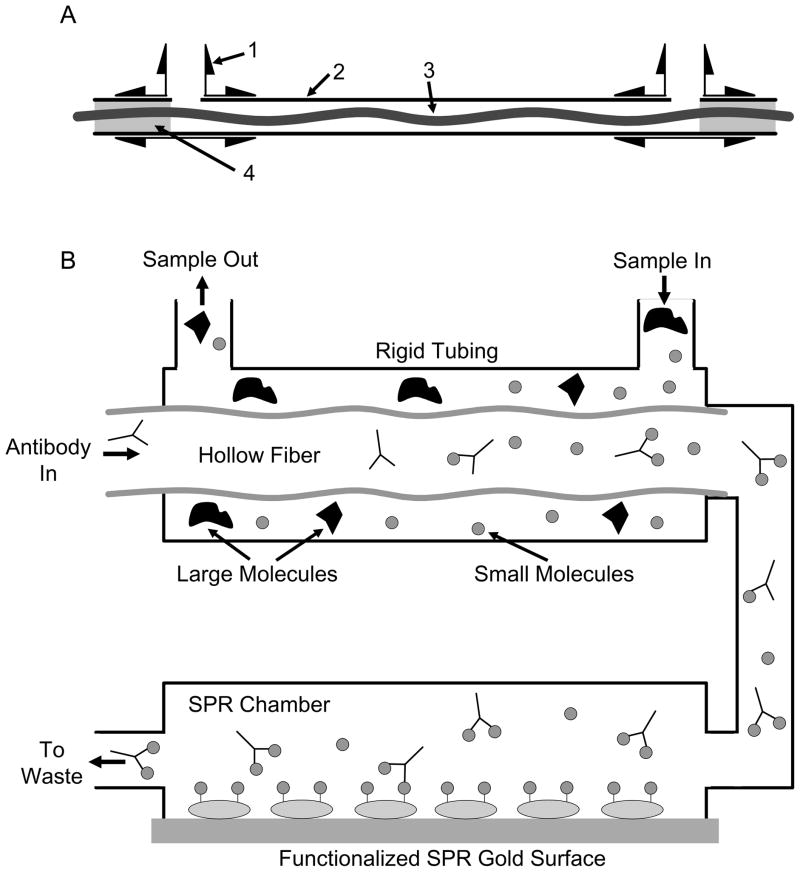
Cortisol-depleted saliva was diluted 1:2 in PBS containing 0.1% Tween-20 (PBST) and spiked with known concentrations of cortisol. PBST containing cortisol antibodies (1:15,000 dilution) was flowed through the fiber at a rate of 25 μl/min. Simultaneously, diluted saliva solutions spiked with varying concentrations of cortisol was flowed outside the fiber at a rate of 50 μl/min. The solution flowing inside the fiber was then flowed over the sensor surface (Figure 3).
Figure 3.
External, in-line filtering flow cell which directs flow into the SPR system. (A) Construction of the in-line filtering flow cell required sliding a 1.6 mm Tee connector (1) (#T210-1, Valve Plastics, Fort Collins, CO) over the ends of 0.75 inner diameter PEEK tube (2) (#1533, Upchurch Scientific, Oak Harbor, WA) followed by drilling a hole into the PEEK tube to allow sample flow, then sealing the peek tube to the tee with urethane adhesive (Lord Corp., Cary, NC). A hydrophilic hollow fiber (3) (Minntech, Minneapolis, MN) with a molecular weight cutoff of 20,000 Da was inserted into the PEEK tube and both ends were sealed with urethane adhesive (4). Following sealing of the hollow fiber into the PEEK tube, the ends of the hollow fiber were cut flush with the tee preserving the opening to the hollow fiber. (B) Salivary samples were diluted 1:2 with buffer and flowed through tubing external to the hollow fiber. The antibody solution was flowed counter current through the hydrophilic hollow fiber and then through the SPR biosensor system. Diffusion may also be aided by bulk-flow across the hollow fiber wall controlled by a pressure differential created by higher flow rates outside the hollow fiber. (Not drawn to scale)
Data analysis
Standard curves and cortisol competition values were generated from the raw data collected using the TI Multispr program. The RI versus time slope values for reference channels were averaged and subtracted from the cortisol channel RI versus time slope values to compensate for changes in RI due to bulk solution RI changes and nonspecific binding to the gold sensor surfaces. Next, the initial slope of RI change versus time was calculated for each addition of antibody without cortisol and antibody with cortisol in samples. The initial slopes for each sample were converted to a percentage of the cortisol-free samples by comparing slopes of samples containing cortisol to the average slopes of the cortisol-free samples detected immediately preceding and following injection of each sample. All samples were analyzed in triplicate and standard deviations were calculated.
RESULTS AND DISCUSSION
Detection of cortisol by SPR competition assay
Competition assays were performed by flowing a constant concentration (67 ng/ml) of monoclonal anti-cortisol antibody over the sensors. Periodic pulses of known amounts of cortisol were added to the antibodies. Each TI Spreetatm 2000 sensor contains 3 sensor channels. The 3 channels of one biosensor chip were coated with cortisol-conjugated BSA while the 3 channels of the reference chip were coated with BSA. Data were collected and displayed as RI versus time (Figure 1). A standard curve for the cortisol competition assay was generated by subtracting the reference channel data from the cortisol channel data, and comparing the change in slope for samples with cortisol to the slope for cortisol-free samples. The reference channels were used to compensate for bulk RI changes, minor temperature fluctuations and non-specific binding to the sensor surfaces. The standard curve is based on experiments performed in triplicate and is presented as a log-log plot (Figure 2).
Design of an in-line filtered flow cell
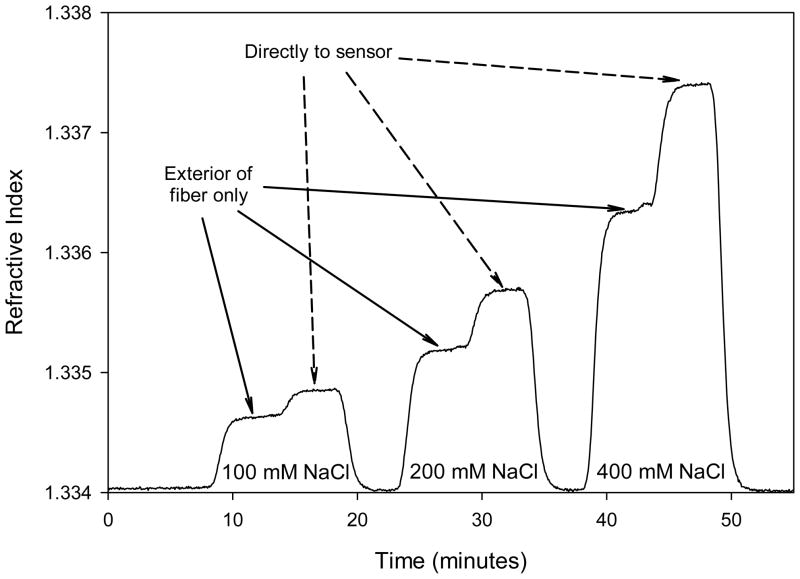
Detection of small molecules in complex matrices, like saliva, requires pretreatment for optimal sensitivity. A flow cell was developed that can eliminate contact between complex matrices such as saliva and the SPR sensor surface. A 10 cm long hydrophilic hollow fiber (Minntech, Minneapolis, MN) with a molecular weight cutoff of 20,000 Da was used to create the in-line filtering flow cell. The fiber was enclosed within a 0.75 mm inner diameter PEEK tube (Upchurch Scientific, Oak Harbor, WA) by sliding the hollow fiber into the PEEK tube and sealing the ends with urethane adhesive (Lord Corp., Cary, NC). Manufacture of the in-line filtering flow cell was simple and inexpensive. Flowing an analyte collection stream outside the hollow fiber, countercurrent to the flow of sample, allowed the diffusion of the small molecular weight components of saliva to the flow to the sensor surface and prevented the large molecular weight components such as the mucins and other large molecular weight components common in saliva samples from contacting the sensor surface (Figure 3). The in-line filtering flow cell allowed diffusion of small molecular weight analytes between the sample stream and the sensor flow stream. Diffusion was also aided by bulk-flow across the hollow fiber generated by a pressure differential created by an external flow rate of 50 μl/min. and an internal hollow fiber flow rate at 25 μl/min. Molecules that were small enough to flow through the wall of the fiber passed freely between the two liquids while larger molecules and particulates were restricted. The compound flow cell was tested using 100–400 mM NaCl (MW 58.44 Da) solutions to follow small molecule diffusion across the hollow fiber wall. NaCl has a strong effect on the RI detected by the sensors (Figure 4). The signal generated by flowing NaCl through the exterior of the hollow fiber and measuring the NaCl diffused through the fiber resulted in a 29% reduction in RI signal when compared to flowing NaCl directly over the sensor surface.
Figure 4.
Small molecule diffusion across the external, in-line filtering flow cell hollow fiber. PBS buffer solutions containing varying quantities (shown) of NaCl were flowed through the tubing external to the hollow fiber followed after 5 minutes with NaCl solution flowing directly over the sensor surface. The plateaus in signal RI represent the diffusion of NaCl at equilibrium for each condition. For external NaCl conditions, any NaCl that diffused into the hollow fiber resulted in an increase in RI on the SPR sensor. Flowing NaCl directly through the hollow fiber onto the sensor surface demonstrated the maximum RI change produced from each NaCl concentration.
Detection of cortisol in buffer and saliva using the in-line filtering flow cell
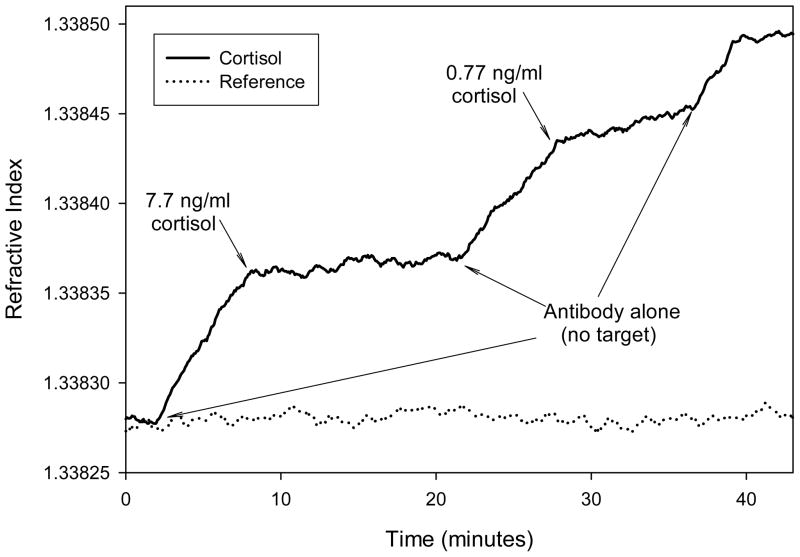
The in-line filtering flow cell system was used for detection of cortisol in saliva. PBST was used as the buffer both inside and outside the hollow fiber. Antibody was flowed through the hollow fiber at a flow rate of 25 μl/min. while known concentrations of cortisol were flowed outside the fiber at flow rates of 50 μl/min. Figure 5 shows a sensorgram generated using two concentrations of cortisol (7.7 and 0.77 ng/ml).
Figure 5.
Detection of cortisol in laboratory buffer using the external, in-line filtering flow cell. Alternating flow through the external PEEK tube of buffer containing no cortisol (2, 22 and 36 minutes) with buffer containing 7.7 ng/ml cortisol (28 nM) (8 minutes) or 0.77 ng/ml cortisol (2.8 nM) (28 minutes) demonstrated the detection of cortisol from the hollow fiber flow containing 1:15,000 diluted anti-cortisol antibody.
Saliva was collected from 7 adults and pooled to create a source of saliva for these experiments. The pooled saliva contained 1.8 ± 0.2 ng/ml cortisol as determined using a salivary cortosol detection kit (Salimetrics). Given the sensitivity of the SPR biosensor using laboratory buffers, cortisol-depleted saliva was needed to examine the sensitivity of the SPR system in saliva. The pooled saliva sample was depleted of cortisol as described in the methods. After one pass through the column, the cortisol level was 0.20 ± 0.05 ng/ml. Following a second pass through the column the cortisol level was 0.05 ± 0.05 ng/ml cortisol. Protein levels in the cortisol-depleted saliva were 90% of the initial sample.
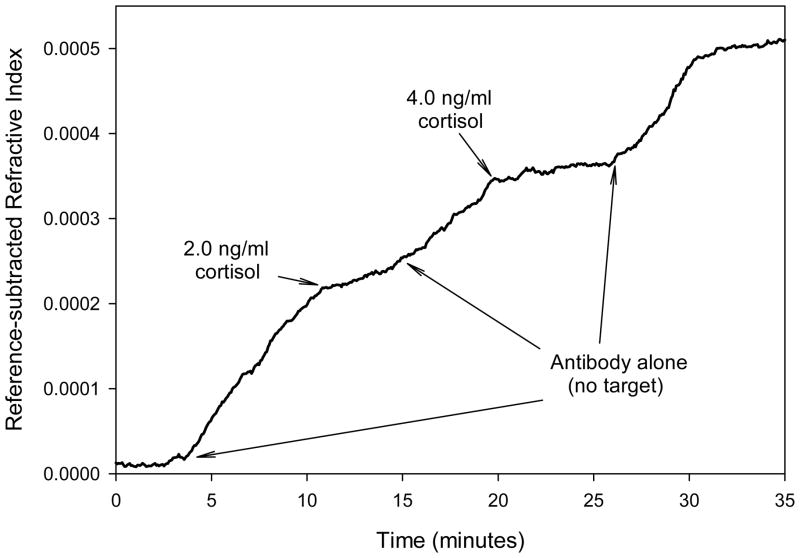
Cortisol-depleted saliva was diluted 1:2 with PBST and flowed outside the hollow fiber while antibodies were flowed counter current through the hollow fiber of the in-line filtering flow cell. Sensorgrams were generated by flowing saliva samples spiked with known quantities of cortisol through the exterior of the hollow fiber. A typical sensorgram for two concentrations of cortisol is shown in Figure 6. A standard curve for the salivary cortisol competition assay was generated by subtracting the reference channel data from the cortisol channel data, and comparing the changes in slopes for samples with cortisol to the slopes for cortisol-free samples (Figure 7). Cortisol was detected in saliva at concentrations as low as 1.0 ng/ml. The assay had a useful detection range between 1.5 and 10 ng/ml (5.4 and 36 nM). For these experiments, the concentration of antibody was selected to give optimal sensitivity in the low range of detection. For use with clinical samples, the high-end detection range can be extended by increasing the concentration of antibody. Future experiments will also explore increased sensitivity at the low end of detection by attaching antibodies to colloidal particles that significantly increase the change in RI per antibody molecule (data not shown).
Figure 6.
Example of a sensorgram for detection of cortisol in saliva using the external in-line filtering flow cell. Alternating flow through the external PEEK tube of 1:2 diluted cortisol-depleted saliva containing no cortisol (4, 15 and 26 minutes) or containing 2.0 ng/ml cortisol (10 minutes) or 4.0 ng/ml cortisol (20 minutes) demonstrated detection of cortisol from the hollow fiber flow containing 1:15,000 diluted anti-cortisol antibody.
Figure 7.
Standard curve for cortisol detection in saliva. The log-log plot shows competition data for detection of cortisol in PBS. Error bars represent standard deviations for experiments run in triplicate.
CONCLUSIONS
We report here a rapid assay for measuring cortisol levels in saliva. The small, portable SPR biosensor used for measurements of cortisol will allow for analysis in the field as well as in emergency rooms and provides results in less than 10 minutes. Levels of cortisol in blood and saliva can be measured and used as an indicator of stress. While measurements of cortisol in saliva are as much as 100X lower than in blood, it is thought that salivary cortisol and free cortisol in blood correlate more closely with stress than does total blood cortisol.6 Also, collecting blood may induce stress and alter the measurement while saliva collection is stress-free. The collection of saliva does not require trained medical skills and can, therefore, simplify collection of samples at numerous times.
The in-line filtering flow cell described here will be useful for detecting many other small molecular weight analytes in complex matrices. Detection of cortisol in a complex matrix such as saliva has been simplified by the addition of the external in-line filtering flow cell that allows for diffusion and bulk flow of small molecular weight analytes into the sensor feed stream while excluding particulates and larger organic molecules that can cause an increase in background signal. The external in-line filtering flow cell can be easily adapted for use in other SPR devices as well many other diagnostic biosensors with upstream processing capabilities.
Acknowledgments
This work was supported in part by NIH/NIDCR Grants 1-UO1DE14971 and NIEHS/NSF P50 ES012762;OCE-0434087, the Department of Defense and by Grant 66-0618 from the Center for Process Analytical Chemistry, University of Washington.
References
- 1.White PC, Curnow KM, Pascoe L. Endocr Rev. 1994;15:421–38. doi: 10.1210/edrv-15-4-421. [DOI] [PubMed] [Google Scholar]
- 2.Raff H, Findling JW. Ann Intern Med. 2003;138:980–91. doi: 10.7326/0003-4819-138-12-200306170-00010. [DOI] [PubMed] [Google Scholar]
- 3.Higazi AR, Ata AH. J Egypt Med Assoc. 1958;41:71–84. [PubMed] [Google Scholar]
- 4.Knutsson U, Dahlgren J, Marcus C, Rosberg S, Bronnegard M, Stierna P, Albertsson-Wikland K. J Clin Endocrinol Metab. 1997;82:536–540. doi: 10.1210/jcem.82.2.3769. [DOI] [PubMed] [Google Scholar]
- 5.al’Absi M, Arnett DK. Biomed Pharmacother. 2000;54:234–244. doi: 10.1016/S0753-3322(00)80065-7. [DOI] [PubMed] [Google Scholar]
- 6.Mendel CM. Endocr Rev. 1989;10:232–274. doi: 10.1210/edrv-10-3-232. [DOI] [PubMed] [Google Scholar]
- 7.Vining RF, McGinley RA. J Steroid Biochem. 1987;27:81–94. doi: 10.1016/0022-4731(87)90297-4. [DOI] [PubMed] [Google Scholar]
- 8.Gozansky WS, Lynn JS, Laudenslagar ML, Kohrt WM. Clin Endocrinol (Oxf) 2005;63:336–341. doi: 10.1111/j.1365-2265.2005.02349.x. [DOI] [PubMed] [Google Scholar]
- 9.Aardal E, Holm AC. Eur J Clin Chem Clin Biochem. 1995;33:927–932. doi: 10.1515/cclm.1995.33.12.927. [DOI] [PubMed] [Google Scholar]
- 10.Meeran K, Hattersley A, Mould G, Bloom SR. British J Clin Practice. 1993;47:246–247. [PubMed] [Google Scholar]
- 11.Kirschbaum C, Hellhammer DH. In: Encyclopedia of Stress. Fink G, editor. Vol. 3. Academic Press; San Diego: 2000. pp. 379–383. [Google Scholar]
- 12.Garde AH, Hansen AM. Scand J Clin Lab Invest. 2005;65:433–436. doi: 10.1080/00365510510025773. [DOI] [PubMed] [Google Scholar]
- 13.Hoferl M, Krist S, Buchbauer G. Arch Pharm Chem Life Sci. 2005;338:493–497. doi: 10.1002/ardp.200500116. [DOI] [PubMed] [Google Scholar]
- 14.Leung W, Chan P, Bosgoed F, Lehmann K, Renneberg I, Lehmann M, Renneberg R. J Immunol Methods. 2003;281:109–18. doi: 10.1016/j.jim.2003.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Westermann J, Demir A, Herbst V. Clin Lab. 2004;50:11–24. [PubMed] [Google Scholar]
- 16.Mirasoli M, Deo SK, Lewis JC, Roda A, Daunert S. Anal Biochem. 2002;306:204–211. doi: 10.1006/abio.2002.5695. [DOI] [PubMed] [Google Scholar]
- 17.Jonsson BA, Malmberg B, Amilon A, Helene Garde A, Orbaek P. J Chromatogr B Analyt Technol Biomed Life Sci. 2003;784:63–68. doi: 10.1016/s1570-0232(02)00753-5. [DOI] [PubMed] [Google Scholar]
- 18.Davies J, editor. Surface Analytical Techniques for Probing Biomaterial Processes. CRC Press; New York: 1996. [Google Scholar]
- 19.Minunni M, Mascini M. Anal Lett. 1993;26:1441–1460. [Google Scholar]
- 20.Kaufman BM, Clower M. J AOAC Int. 1995;78:1079–1090. [PubMed] [Google Scholar]
- 21.Mauriz E, Calle A, Manclús JJ, Montoya A, Lechuga LM. Anal Bioanal Chem. 2007;387:1449–1458. doi: 10.1007/s00216-006-0800-z. [DOI] [PubMed] [Google Scholar]
- 22.Lin TJ, Huang KT, Liu CY. Biosensors and Bioelectronics. 2006;22:513–518. doi: 10.1016/j.bios.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Fu E, Chinowsky T, Nelson K, Johnston K, Edwards T, Helton K, Grow M, Miller JW, Yager P. Ann N Y Acad Sci. 2007;1098:335–344. doi: 10.1196/annals.1384.026. [DOI] [PubMed] [Google Scholar]
- 24.Adamczyk M, Johnson DD, Mattingly PG, Moore JA, Pan Y. Bioconjug Chem. 1998;9:23–32. doi: 10.1021/bc9701353. [DOI] [PubMed] [Google Scholar]
- 25.Miyashita M, Shimada T, Miyagawa H, Akamatsu M. Anal Bioanal Chem. 2005;381:667–673. doi: 10.1007/s00216-004-2952-z. [DOI] [PubMed] [Google Scholar]
- 26.Traynor IM, Plumpton L, Fodey TL, Higgins C, Elliott CT. J AOAC Int. 2006;89:868–872. [PubMed] [Google Scholar]
- 27.Stevens RC, Soelberg SD, Eberhart BTL, Spencer S, Wekell JC, Chinowsky TM, Trainer VL, Furlong CE. Harmful Algae. 2007;6:166–17. [Google Scholar]
- 28.Chinowsky TM, Quinn JG, Bartholomew DU, Kaiser R, Elkind JL. Sens Actuators B. 2003;91:266–274. [Google Scholar]
- 29.Melendez J, Carr R, Bartholomew DU, Kukanskis K, Elkind J, Yee S, Furlong C, Woodbury R. Sens Actuators B. 1996;35:212–216. [Google Scholar]
- 30.Furlong CE, Stevens RC, Soelberg SD, Yee N, Geiss G, Katze MG, Near S, Yee S, Chinowsky T. In: Proceedings of a Conference, held at Imperial College, London, 20–21 April 2005. Winder C, editor. University of New South Wales; Sydney: 2005. pp. 255–270. [Google Scholar]
- 31.Naimushin AN, Soelberg SD, Nguyen DK, Dunlap L, Bartholomew D, Elkind J, Melendez J, Furlong CE. Biosens Bioelectron. 2002;17:573–584. doi: 10.1016/s0956-5663(02)00014-3. [DOI] [PubMed] [Google Scholar]