Abstract
Dental implantology has emerged as a practical alternative to traditional prosthodontics. Since the beginning, placement of implant in the bone to achieve a prosthetic solution that fulfils biologic, aesthetic and biomechanical requirements has been a challenge. In the past, implant site and inclination were dictated by residual bone quality. The desire for predictable prosthesis led to the development of prosthetically guided implantology. This concept establishes the correct implant position during the diagnostic stage according to planned definitive restoration. In prosthetically guided implantology where ideal placement of implant is determined by the definitive restoration, use of radiographic and surgical stent in conjunction with dental CT scan can play an important role. A stent is an appliance used for radiographic evaluation during treatment planning for implant placement and during surgical procedures to locate optimal implant placement site. The stent with dental CT scan enables the dental team to identify specific sites of prospective implant surgery and hence determines the optimal position and angulation of implant relative to occlusal load. Aided by stent the surgeon can avoid undesirable implant site preparation and minimize unnecessary osteotomy, resulting in favorable design of prosthesis, reduced surgical trauma, reduced surgical time and increased patient comfort. This case report is an insight into the method of fabrication of simple and cost effective stent for implant placement and its advantages over the other techniques of stent fabrication.
Keywords: Diagnostic stent, Surgical stent, CT scan, Dental implant
Introduction
Despite significant advances in devices and techniques, placing dental implants in a correct position still remains a challenge. Diagnostic casts, probing depths and panoramic radiography can lead to unpredictable results as they do not give three-dimensional (3-D) radiographic information required for correct positioning and orientation of implant [1]. Moreover, predictable implant supported prosthesis also requires a determination of final prosthesis in treatment planning stage. Thus for a successful implant supported prosthesis the Prosthodontist should plan the implant position in accordance with accurate mesiodistal and buccolingual location, angulation with residual bone and correct implant orientation. To achieve these objectives surgical guide (stent) with radiopaque marker in conjunction with dental CT scan imaging should be used. The purpose of stent is to preview the definitive restoration and its relationship to adjacent structures, to communicate the restoration planned by the Prosthodontist to the surgeon, to reduce osteotomy and to locate healing screws at the time of second stage surgery [2].
Case Report
A 30 year old male patient was referred to the department of Prosthodontics for the management of missing 46 and 47. A complete radiographic examination was carried out to corelate with the clinical findings and quality of bone (Fig. 1). The diagnostic impressions were made and casts were articulated to plan for fixed implant supported restoration.
Fig. 1.
Preoperative panoramic view
Treatment Planning
It was decided to prosthetically rehabilitate this patient with implant supported crowns to replace missing teeth.
Clinical and Laboratory Procedures
Diagnostic impressions were made with irreversible hydrocolloid impression material (Vignette-chromatic, Dentsply India) and poured.
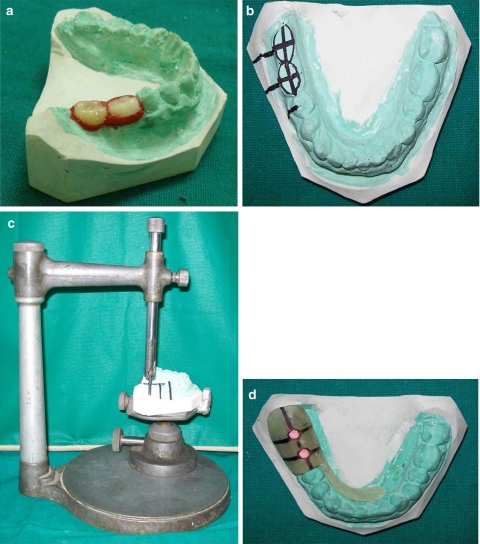
Casts were articulated and wax up was done (Fig. 2a).
Cast with wax up was duplicated.
The occlusal two third of the prosthesis was trimmed on the duplicated cast. To provide accurate implant positioning, the location of the access holes both mesiodistally and buccolingually was determined (Fig. 2b). The desired mesiodistal angulation of the implants along the buccal side of the cast was delineated, and a reference axis with tracing was established. Dental surveyor was used to transfer lines on buccal aspect to achieve relative parallelism between implants (Fig. 2c).
With an autopolymerizing acrylic resin (Rapid Repair, Pyrex polymer, India), stent was fabricated as a flat plane over the trimmed teeth and implant position was transferred on it.
A channel through the predetermined mesiodistal and buccolingual centre of the stent was made and filled with gutta percha marker (Fig. 2d).
The stent was placed in the patient mouth and dental CT scan images (Spiral CT scan, Wipro GE, Germany) of the implant site were obtained.
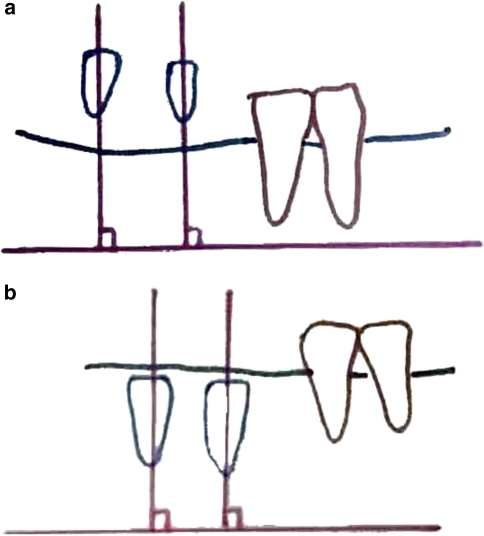
Analysis of dental CT scan images was done using denta scan software and making tracings of images in cross sectional, axial and panoramic view where gutta percha rods were visible for determining three-dimensional position of the implant (Fig. 3a–c; Table 1).
Because the angulation of the gutta percha rod represented the ideal angulation of the implants, this angulation was compared with the available bone to determine the best angulation for the implant.
This information was transferred to stent by removing the gutta percha from channels and thus the diagnostic stent was converted to surgical stent and was used for implant placement (Fig. 4).
Dental CT scan images of the jaw were taken again with the implant in place. Cross sectional, axial and panoramic sections were selected again at the implant site to record the final achieved position of implant (Fig. 5a–c; Table 2).
A comparison of the achieved implant position and ideal implant position (with the help of stent and dental CT scan) was done to evaluate the efficacy of stent in determining the position and orientation of implant (Table 3).
Fig. 2.
a Cast with wax up. b Location of access hole. c Parallelism with surveyor. d Channel filled with gutta percha marker
Fig. 3.
a Preoperative Trans axial image. b Preoperative cross sectional images. c Preoperative panoramic image (with gutta percha marker)
Table 1.
Preoperative planned position of implants (1) and (2) in different views
| Planned implants position in relation to adjacent structures (Trans axial view) | ||
|---|---|---|
| Distance from buccal cortical plate | 3.7 mm (1) | 3.2 mm (2) |
| Distance from lingual cortical plate | 3.3 mm (1) | 2.9 mm (2) |
| Distance from adjacent tooth | 4.0 mm | |
| Inter-implant distance | 6.1 mm | |
| Planned implant position in relation to buccolingual angulation (cross sectional view) | |
|---|---|
| Implant | Angle between long axis of bone and that of implant |
| (1) | 10° |
| (2) | 9° |
| Planned implant position in relation to mesiodistal parallelism (panoramic image) | |
|---|---|
| Implant | Angle between long axis of implant and flat plane |
| (1) | 91° |
| (2) | 90° |
| 3 (tooth no. 45) | 89° |
Fig. 4.
Surgical stent
Fig. 5.
a Post operative Trans axial image. b Post operative cross sectional images. c Post operative panoramic image (with implant in place)
Table 2.
Postoperative achieved position of implants (1) and (2) in different views
| Achieved implant position in relation to adjacent structures (Trans axial view) | ||
|---|---|---|
| Distance from buccal cortical plate | 2.6 mm (1) | 2.4 mm (2) |
| Distance from lingual cortical plate | 2.0 mm (1) | 2.2 mm (2) |
| Distance from adjacent tooth | 3.8 mm | |
| Inter-implant distance | 3.2 mm | |
| Achieved implant position in relation to buccolingual angulation (cross sectional view) | |
|---|---|
| Implant | Angle between long axis of bone and that of implant |
| (1) | 9° |
| (2) | 7° |
| Achieved implant position in relation to mesiodistal parallelism (panoramic view) | |
|---|---|
| Implant | Angle between long axis of implant and flat plane |
| (1) | 91° |
| (2) | 88° |
| 3 (tooth no.45) | 89° |
Table 3.
Comparison of ideal and achieved implant distance and angulation
| Ideal | Achieved | ||
|---|---|---|---|
| Implant (1) | Implant (2) | ||
| Implant and buccal cortical plate | >0.5 mm/1 mm | 2.6 mm | 2.4 mm |
| Implant and lingual cortical plate | >0.5 mm/1 mm | 2.0 mm | 2.2 mm |
| Implant and adjacent tooth | ≥1.5 mm | 3.8 mm | |
| Inter implant distance | ≥3 mm | 3.2 mm | |
| Implant (1) | Implant (2) | |
|---|---|---|
| Mesiodistal relative parallelism | 91° | 88° |
| Buccolingual relative parallelism | 9° | 7° |
| Angle between planned prosthesis and residual bone trajectory (should be <20°) | 9° | 7° |
Discussion
For a successful implant supported definitive restoration the implant must be placed at a correct and pre-planned position and angulation. The mesiodistal placement of the implant should aid in preservation of papilla and provide an esthetic implant restoration profile [3]. The implant should be placed at least 1.5 mm from the adjacent teeth with a minimum 3 mm interimplant distance. The distance of implant from buccal and lingual cortical plates should be greater than 0.5 mm. In the buccolingual plane the angle between the implant trajectory and residual bone trajectory should be less than 20° to prevent unfavorable bending moment [1, 4, 5]. In multiple implant situations non parallel implant placement is the primary cause of non axial loading and subsequent failure [6].
To achieve the above mentioned objectives use of stent has been suggested. It has been well documented in literature that the implants placed using stents are more accurately positioned than those without the stent [7, 8]. Ever since the introduction of stents in implant dentistry various designs have been suggested. The relative advantages and disadvantages of some of them have been listed in Table 4. Following the principles of stent design we decided to use a simplified and comprehensive dual purpose (diagnostic and surgical) stent made of acrylic resin and gutta percha marker with few modifications in its design. The stent was used in conjunction with three dimensional CT scan imaging and implant position was analysed using denta scan software.
Table 4.
Different types of stent
| Types of stent | Advantage | Disadvantage |
|---|---|---|
| 1. Clear vaccuform stent | Simple and quick to fabricate | Too much flexibility in positioning of implant and less accurate |
| 2. Self cure acrylic stent with lead strips | Simple to fabricate | Only an imaging stent (diagnostic) and not a surgical stent |
| 3. Self cure acrylic with metal sleeves and disks | Most accurate | Expensive, metal tubes and disks do not provide any flexibility during placement procedures(allows only single size of drill to pass through) |
| 4. Self cure acrylic with channel filled with gutta percha | Acceptable accuracy, easy to fabricate and inexpensive | Not as accurate as metal sleeves and disks |
The introductory stent designs in the mid and late 90’s were either diagnostic or surgical and focused on determining the correlation of implant site with surrounding vital structures [9–12].They did not help in determining the relative parallelism between adjacent multiple implants [13, 14]. The most recent ones though being very accurate are expensive and require extensive laboratory set up for their fabrication [1, 15–17].
The stent used in our case is cost effective and easy to fabricate. It provides adequate accuracy as well in terms of implant position and angulation. It stands out from other techniques that it helps to determine relative parallelism between adjacent implants. In our technique we have achieved this objective by using dental surveyor (Fig. 2c) and making preoperative (with stent in place) and post operative tracings (with implant in place) of the CT scan images (Fig. 6).
Fig. 6.
a Preoperative tracings (with gutta percha marker) of the CT scan images. b Post operative tracings (with implant in place) of the CT scan images
Akca et al. suggested a method to fabricate stent with a 4 mm flat plate to achieve mesiodistal parallel placement of multiple implants but this stent could not determine the buccolingual orientation of implant [18]. Our design enables the dentist to achieve both mesiodistal and buccolingual parallelism with a single stent. Moreover as demonstrated by an in vitro study by Choi et al., a 4 mm channel length is not sufficient to control implant angulation [19]. Hence we decided to make the stent of the height two thirds the occlusogingival height of the proposed restoration so as to achieve 6–8 mm length of drill channel.
Another stent design for the multiple implant placements was proposed by Tsuchida et al., where they used an acrylic resin stent with silicone markers [20]. In their design the buccal/lingual half of the stent was removed at the time of surgery to provide adequate visualization of the site. This can lead to compromised control of implant drill as it can deviate towards the unsupported site. In our stent the drill channel is supported from all side in occlusal two thirds of stent. The facial lower third of the stent can be removed at the time of surgery to provide visualization and irrigation of the implant site.
Another advantage of our stent is that the drill size can be enlarged according to the increasing size of sequential drills. The acrylic resin channel can be enlarged easily without shredding plastic or metal. A RCP (ridge crest preparation) guide fabricated by Shotwell et al. also permits this but it is only a surgical stent and is unsupported on the buccal side [21].
Gutta percha radioopaque marker has property of thermoplasticity and is easy to compact in the drill channel [9]. It does not produce artefacts as metal markers do and can be easily removed while conversion of stent from diagnostic to surgical use.
As the values indicate in the Tables 1, 2 and 3 we could achieve an accurate position and angulation of implant. Hence the use of dual purpose radiographic and surgical stent should be employed for treatment planning and placement of dental implants.
References
- 1.Almong DM, Torrado E, Meitner SW. Fabrication of imaging and surgical guides for dental implants. J Prosthet Dent. 2001;85:504–508. doi: 10.1067/mpr.2001.115388. [DOI] [PubMed] [Google Scholar]
- 2.Garber DA. The esthetic dental implant: letting restoration be the guide. J Am Dent Assoc. 1995;126:319–325. doi: 10.14219/jada.archive.1995.0175. [DOI] [PubMed] [Google Scholar]
- 3.Lazzara RJ. Effect of implant position on implant restoration design. J Esthet Dent. 1993;5:265–269. doi: 10.1111/j.1708-8240.1993.tb00791.x. [DOI] [PubMed] [Google Scholar]
- 4.Horiuchi M, Ichikawa T, Kanitani H, et al. Pilot-hole preparation for proper implant positioning and the enhancement of bone formation. J Oral Implantol. 1995;21:318–324. [PubMed] [Google Scholar]
- 5.Almog DM, Onufrak JM, Hebel K, et al. Comparison between planned prosthetic trajectory and residual bone trajectory using surgical guides and tomography—a pilot study. J Oral Implantol. 1995;21:275–280. [PubMed] [Google Scholar]
- 6.Taylor TD, Agar JR, Voigiatzi Implant prosthodontics: current perspective and future directions. Int J Maxillofac Implants. 2000;15:66–75. [PubMed] [Google Scholar]
- 7.Engelman MJ, Sorenson JA, Moy P. Optimum Placement of Osseointegrated implants. J Prosthet Dent. 1988;59:467–473. doi: 10.1016/0022-3913(88)90044-3. [DOI] [PubMed] [Google Scholar]
- 8.Modica F, Fava C, Benech A, et al. Radiologic-prosthetic planning of the surgical phase of the treatment of edentulism by osseointegrated implants: an in vitro study. J Prosthet Dent. 1991;65:541–546. doi: 10.1016/0022-3913(91)90297-A. [DOI] [PubMed] [Google Scholar]
- 9.Pesun IJ, Gardner FM. Fabrication of a guide for radiographic evaluation and surgical placement of implants. J Prosthet Dent. 1995;73:548–552. doi: 10.1016/S0022-3913(05)80114-3. [DOI] [PubMed] [Google Scholar]
- 10.Stellino G, Morgano SM, Imbelloni A. A dual-purpose, implant stent made from a provisional fixed partial denture. J Prosthet Dent. 1995;74:212–214. doi: 10.1016/S0022-3913(05)80191-X. [DOI] [PubMed] [Google Scholar]
- 11.Sethi A. Precise site location for implants using CT scans: a technical note. Int J Oral Maxillofac Implants. 1993;8:433–438. [PubMed] [Google Scholar]
- 12.Basten CH. The use of radiopaque templates for predictable implant placement. Quintessence Int. 1995;26:609–612. [PubMed] [Google Scholar]
- 13.Takeshita F, Suetsugu T. Accurate presurical determination for implant placement by using computerized tomography scan. J Prosthet Dent. 1996;76:590–591. doi: 10.1016/S0022-3913(96)90434-5. [DOI] [PubMed] [Google Scholar]
- 14.Takeshita F, Tokoshima T, Suetsugu A stent for presurgical evaluation of implant placement. J Prosthet Dent. 1997;77:36–38. doi: 10.1016/S0022-3913(97)70204-X. [DOI] [PubMed] [Google Scholar]
- 15.Meitner SW, Tallents RH. Surgical Templates for prosthetically guided implant placement. J Prosthet Dent. 2004;92:569–574. doi: 10.1016/j.prosdent.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 16.Atsu SS. A Surgical guide for dental implant placement in edentulous posterior regions. J Prosthet Dent. 2006;96:129–133. doi: 10.1016/j.prosdent.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Stumpel LJ. Cast based guided implant placement: a novel technique. J Prosthet Dent. 2008;100:61–69. doi: 10.1016/S0022-3913(08)60140-7. [DOI] [PubMed] [Google Scholar]
- 18.Akca k, Iplikcioglu H, Cehreli MC. A surgical guide for accurate mesiodistal paralleling of implants in the posterior edentulous mandible. J Prosthet Dent. 2002;87:233–235. doi: 10.1067/mpr.2002.120900. [DOI] [PubMed] [Google Scholar]
- 19.Choi M, Romberg Elaine, Driscoll Effect of varied dimensions of surgical guides on implant angulations. J Prosthet Dent. 2004;92:463–469. doi: 10.1016/j.prosdent.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 20.Tsuchida F, Hosoi T, Imanaka M, Kobayashi K. A technique for making a diagnostic and surgical template. J Prosthet Dent. 2004;91:395–397. doi: 10.1016/j.prosdent.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 21.Shotwell JL, Billy EJ, Wang HL, Oh TJ. Implant surgical guide fabrication for partially edentulous patients. J Prosthet Dent. 2005;93:294–297. doi: 10.1016/j.prosdent.2004.12.013. [DOI] [PubMed] [Google Scholar]