Abstract
Aims/Hypothesis
The FinnDiane Study has reported that mortality in type 1 diabetes is not increased over a 7-yr follow-up in the absence of renal disease (RD). Using the Pittsburgh Epidemiology of Diabetes Complications (EDC) Study population (n=658) of childhood-onset type 1 diabetes (age<17 yrs), we sought to replicate and expand these findings to a 20-yr follow-up (as of 1/1/2008) and examine cause of death by renal status.
Methods
At baseline (1986–1988), mean age and duration of diabetes were 28 and 19 yrs, respectively. RD was defined as an albumin excretion rate ≥20 μg/min from multiple samples and grouped as microalbuminuria (MA, 20–200 μg/min), overt nephropathy (ON, >200 μg/min), or end stage renal disease (ESRD, dialysis or renal transplantation).
Results
At baseline, 311 (47.3%) individuals had RD (MA 21.3%, ON 22.2%, and ESRD 3.8%). During a median 20 yr follow-up, there were 152 deaths (23.1%). Mortality was 6.2 (95% CI, 5.2–7.2) times higher than expected, with standardized mortality ratios (SMRs) of 2.0 (1.2–2.8) for normoalbuminuria (NA); 6.4 (4.4–8.4) for MA; 12.5 (9.5–15.4) for ON; and 29.8 (16.8–42.9) for ESRD. Excluding those (n=64) with NA who later progressed to RD, no significant excess mortality was observed in the remaining NA group (1.2, 0.5–1.9), whose deaths were largely unrelated to diabetes.
Conclusion/Interpretation
These data confirm the importance of RD, including persistent microalbuminuria, as a marker of mortality risk and suggest that type 1 diabetes patients without renal disease achieve long-term survival comparable to the general population.
Keywords: type 1 diabetes, microalbuminuria, overt nephropathy, end stage renal disease, renal disease, mortality
Introduction
Many previous studies have documented that individuals with type 1 diabetes have an increased age-adjusted mortality risk of death compared to the general population.[1, 2] This excess mortality risk in large part results from the development of chronic complications, particularly renal disease (RD).[3–7] Furthermore, a recent article by Groop et al. (FinnDiane Study) reports that while 7-year mortality in type 1 diabetes patients increases in a step-wise manner by degree of albuminuria at baseline, individuals with normoalbuminuria have an equivalent mortality to that of the general age- and sex-matched Finnish population.[8]
Despite these landmark FinnDiane findings, four salient questions remain unanswered. First, it is unknown whether the FinnDiane findings are unique to the Finnish population and its medical system. Second, as the analysis by Groop et al. covered a median follow-up of only 7 years, whether these findings will also apply over a longer time span is unknown. Similarly, the contemporary long-term mortality of individuals with persistent normoalbuminuria is not well documented. Finally, it is not known whether, as would be predicted by these findings, type 1 diabetes individuals with normoalbuminuria die only from non-diabetes-related causes. Using 20 years of follow-up data from a well-characterized hospital-based cohort of individuals with type 1 diabetes living near Pittsburgh, Pennsylvania, USA, we thus sought to replicate the FinnDiane findings and answer these questions.
Methods
Study population
The Pittsburgh Epidemiology of Diabetes Complications (EDC) Study has previously been described in detail.[9, 10] The EDC population has been shown to be epidemiologically representative of the type 1 diabetes population in Allegheny County, Pennsylvania.[11] Briefly, Pittsburgh EDC Study participants (n=658), who were diagnosed with childhood-onset (age<17 yrs) type 1 diabetes between 1950 and 1980 (and seen at Children’s Hospital of Pittsburgh within 1 year of diagnosis), were first evaluated for EDC between 1986 and 1988, when mean age and diabetes duration were 28 (±7.9) and 19 (±7.5) yrs, respectively. Participants have been followed biennially by survey and for the first 10 years and again at 18 years by examination. Study protocols were approved by the University of Pittsburgh Institutional Review Board, and all participants provided written informed consent.
Clinical Evaluation and Procedures
EDC participants completed surveys regarding medical history and demographic information prior to their clinical examination. Blood pressure was measured according to the Hypertension Detection and Follow-Up Program protocol with a random-zero sphygmomanometer after a 5-min rest. An ever smoker was defined as a person who had smoked ≥100 cigarettes over their lifetime.
Fasting blood samples were taken to measure glycosylated hemoglobin (HbA1), lipids, and lipoproteins. For analysis purposes, original HbA1 values were converted to Diabetes Complications and Control Trial (DCCT)-aligned HbA1c using the following regression equation derived from duplicate assays: DCCT HbA1c = 0.14 + 0.83(EDC HbA1). Total cholesterol and triacylglycerol was measured enzymatically, and HDL cholesterol was determined after a heparin and manganese chloride precipitation method.[12] White blood cell counts were obtained with a Coulter Counter (model S-plus IV, Beckman-Coulter, Fullerton, CA) and fibrinogen using a biuret colorimetric procedure and a clotting method.
Height and weight were measured for body mass index (BMI, in kg/m2), and waist and hip circumferences were measured at least twice and averaged to calculate waist-to-hip ratio (WHR). Insulin sensitivity was estimated using a regression equation for glucose disposal rate (eGDR) derived from hyperinsulinemic-euglycemic clamp studies, as previously described.[13]
Serum and urinary albumin were measured by immunonephelometry,[14] and creatinine was assayed using an Ectachem 400 Analyzer (Eastman Kodak, Rochester, NY). Estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease (MDRD) equation.[15] Baseline renal damage status was defined on the basis of urinary albumin excretion rates (AER) in at least two of three timed urine collections as <20 μg/min – normoalbuminuria (NA), 20–200 μg/min – microalbuminuria (MA), or >200 μg/min – overt nephropathy (ON). End stage renal disease (ESRD) was defined as renal failure or transplantation. Progression to renal disease during follow-up was defined as confirmed MA in two consecutive EDC cycles, or any ON or ESRD. Overall, 53 (8.1%) participants did not, after the baseline examination, provide any updated renal examination data, 38 of whom had NA at baseline.
Macrovascular disease was defined as myocardial infarction, stroke, coronary or peripheral revascularization, angiographic stenosis ≥50%, carotid surgery, or amputation of an ischemic limb, confirmed by hospital records. Proliferative retinopathy was assessed using stereoscopic fundus photographs of fields 1, 2, and 4 with a Zeiss camera, read by the University of Wisconsin-Madison Fundus Photography Reading Center and classified based on the modified Arlie House system.[16] For participants refusing fundus photographs (n=43), proliferative retinopathy was defined as receiving laser phototherapy for proliferative retinopathy.
Mortality data
Vital status was determined as of January 1, 2008. Deaths were also identified via searches in both the Social Security Death Index and the National Death Index. Vital status could not be ascertained for 16 (2.4%) participants. To confirm each death, death certificates were obtained and as many of the following as possible: 1) pertinent medical records; 2) autopsy/coroner’s reports; and 3) interview with next-of-kin regarding the circumstances surrounding the death. The underlying cause of death, and rank order for all contributing causes, for each decedent was determined by an M.D. Mortality Classification Committee using all available data based on standardized procedures.[17]
Statistical analysis
Each variable’s distributional characteristics were assessed for normality. Student’s t-test and one-way ANOVA were used to compare normally distributed variables between groups, while Mann-Whitney U and Kruskal-Wallis tests were used for non-normally distributed variables, adjusting for multiple comparisons using the Bonferroni correction. The χ2 (or Fisher’s exact) test was used to compare categorical variables between groups, as appropriate. Significant univariate measures and other variables known to be associated with mortality were made available in multivariable Cox proportional hazards regression models using backward selection. As age and diabetes duration are highly correlated in this cohort (r=0.85), only duration was made available to multivariable models. The proportional hazards assumption was assessed visually and verified by testing time-dependent interaction variables. Survival plots by baseline albuminuria status, macrovascular disease status, and proliferative retinopathy status were produced based on these multivariable models. The effect of progression to RD on mortality was assessed as a time-varying covariate in a diabetes duration-adjusted Cox model for study participants with normoalbuminuria at baseline. With this method, participants were treated as normoalbuminuric until the examination when progression to RD occurred and then considered as having RD thereafter.
Expected mortality was estimated using the person-years method based on general population life tables for Allegheny County, Pennsylvania.[18] Age-, sex-, and race-adjusted standardized mortality ratios (SMRs) were calculated as the observed divided by the expected number of deaths in each age, sex, and race category. Mortality rates were compared using rate ratio (RR) analyses and calculating 95% CIs.[19]
Hazard ratios (HR) for continuous variables are reported per increase of 1 SD. Statistical significance was considered as p < 0.05. Analyses were completed using either SPSS 17.0 (SPSS, Chicago, IL) or SAS 9.1 (SAS Institute, Cary, NC). For comparability purposes, analyses, complication groupings, and covariates reflect those in reference 8 (Groop et al.), along with further covariates made available for modeling based on univariate analyses in this report, as described.
Results
Baseline characteristics by degree of renal disease and function
At baseline, approximately half the population had NA, while half had varying levels of RD (MA 21.3%, ON 22.2%, and ESRD 3.8%) (Table 1). Compared to individuals with NA, those with RD were significantly older and had longer duration of diabetes, greater waist-to-hip ratio, and adverse cardiovascular (SBP, DBP, non-HDL cholesterol, HDL cholesterol, triacylglycerol) and inflammatory (WBC, fibrinogen) risk profiles, which worsened in a linear fashion with severity of RD. No differences in RD status were seen by sex or race. Those with RD also had a higher prevalence of diabetes-related complications, such as proliferative retinopathy and macrovascular disease, which increased with greater renal damage. Similar trends were seen when the cohort was stratified by renal function measures (data not shown).
Table 1.
Characteristics of the Pittsburgh EDC population by baseline renal damage categories
| Variables | NA (AER<20) | MA (AER=20–200) | ON (AER>200) | ESRD |
|---|---|---|---|---|
| N (%) | 347 (52.7) | 140 (21.3) | 146 (22.2) | 25 (3.8) |
| Male sex | 162 (46.7) | 76 (54.3) | 79 (54.1) | 16 (64.0) |
| Black race | 7 (2.0) | 3 (2.1) | 3 (2.1) | 2 (8.0) |
| Age (years)d | 25.3±7.7 | 28.6±7.9b | 30.9±6.2b | 36.1±5.8b |
| Diabetes Duration (years)d | 17.0±7.1 | 20.5±7.3b | 22.6±6.6b | 26.8±5.3b |
| Body Mass Index (kg/m2) | 23.2±3.2 | 23.9±3.6 | 23.9±3.0 | 23.7±3.1 |
| Waist-to-Hip Ratiod | 0.81±0.06 | 0.84±0.07b | 0.84±0.08b | 0.90±0.07b |
| Insulin dose (IU kg−1 day−1) | 0.80±0.23 | 0.79±0.25 | 0.75±0.25 | 0.82±0.41 |
| HbA1c (%) | 8.56±1.39 | 9.15±1.71b | 8.92±1.60 | 8.96±1.44 |
| eGDR (mg kg−1 min−1)d | 8.56±1.33 | 7.45±1.79b | 6.63±2.17b | 4.70±1.72b |
| Serum Creatinine(μmol/L)d | 70.7 (53.0–88.4) | 79.6 (61.9–97.2)a | 88.4 (70.7–123.8)b | 194.5 (123.8–455.3)b |
| MDRD eGFR (ml min−1 1.73 m−2)d | 111.9±44.3 | 101.2±36.8a | 75.3±40.2b | 32.8±22.6b |
| Systolic BP (mmHg)d | 108.1±10.6 | 112.4±12.9b | 124.0±16.7b | 139.8±30.3b |
| Diastolic BP (mmHg)d | 69.0±8.1 | 73.1±10.5b | 80.2±11.9b | 84.3±15.9b |
| BP Medication Use | 5 (1.5) | 10 (7.6)a | 42 (30.2)b | 10 (40.0)b |
| Pulse (bpm) | 76.6±9.3 | 80.1±9.9b | 81.4±10.0b | 75.4±13.0 |
| Total-C (mmol/L)d | 4.58±0.84 | 5.05±0.99b | 5.62±1.30b | 5.84±1.26b |
| Non-HDL-C (mmol/L)d | 3.15±0.83 | 3.66±0.96b | 4.27±1.33b | 4.61±1.24b |
| HDL-C (mmol/L)c | 1.43±0.31 | 1.37±0.31 | 1.35±0.34a | 1.23±0.38a |
| Triacylglycerol (mmol/L)d | 0.81 (0.62–1.10) | 0.99 (0.77–1.50)b | 1.18 (0.85–1.87)b | 1.93 (1.44–3.10)b |
| WBC count (×109/L)d | 5.8 (5.0–7.0) | 6.5 (5.5–8.0)b | 6.9 (5.8–8.4)b | 7.6 (6.0–9.2)b |
| Fibrinogen (μmol/L)d | 7.4 (6.2–8.8) | 8.2 (7.1–9.8)b | 9.4 (7.8–11.6)b | 9.1 (7.9–11.0)b |
| Proliferative retinopathy | 46 (13.5) | 44 (32.4)b | 91 (62.8)b | 23 (92.0)b |
| Macrovascular disease | 20 (5.8) | 16 (11.4) | 21 (14.4)a | 11 (44.0)b |
| Ever Smoker | 105 (31.3) | 58 (43.3)a | 71 (48.6)b | 14 (56.0)a |
Data presented as either n (%) or mean ± SD or median (IQR).
Comparison to participants with normoalbuminuria:
p<0.05,
p<0.001.
significant linear trend, p<0.05,
significant linear trend, p<0.001
Abbreviations: Epidemiology of Diabetes Complications, EDC; normoalbuminuria, NA; microalbuminuria, MA; overt nephropathy, ON; end stage renal disease, ESRD; albumin excretion rate, AER; estimated glucose disposal rate, eGDR; Modification of Diet in Renal Disease, MDRD; estimated glomerular filtration rate, eGFR; blood pressure, BP; total cholesterol, Total-C; high density lipoprotein cholesterol, HDL-C; white blood cell, WBC.
Mortality trends
The median follow-up time was 20.1 yrs (range 0.2–21.7 yrs). Of 658 participants, 152 (23.1%) died giving an overall mortality of 1.3 / 100 person-years (Table 2). Although mortality did not significantly differ by sex or race, mortality significantly increased with greater albumin excretion rate.
Table 2.
Mortality rates in type 1 diabetes participants by sex, race, and baseline renal damage categories
| n (%) | Median FUT (yrs) | Total FUT (yrs) | Deaths n (%) | Mortality rate (95% CI) (per 100 person-yrs) | |
|---|---|---|---|---|---|
| Overall | 658 | 20.1 | 11,870 | 152 (23.1) | 1.3 (1.1, 1.5) |
| Sex | |||||
| Males | 333 (50.6) | 20.0 | 5,922 | 85 (26.2) | 1.4 (1.1, 1.7) |
| Females | 325 (49.4) | 20.2 | 5,948 | 67 (21.1) | 1.1 (0.9, 1.4) |
| Race | |||||
| White | 643 (97.7) | 20.1 | 11,610 | 147 (22.9) | 1.3 (1.1, 1.5) |
| Black | 15 (2.3) | 20.2 | 260 | 5 (33.3) | 1.9 (0.2, 3.6) |
| AER | |||||
| Normoalbuminuria | 347 (52.7) | 20.4 | 6,851 | 24 (7.1) | 0.3 (0.2, 0.5) |
| Microalbuminuria | 140 (21.3) | 20.1 | 2,510 | 39 (28.1) | 1.6 (1.1, 2.0)a |
| Overt nephropathy | 146 (22.2) | 19.0 | 2,275 | 69 (47.3) | 3.0 (2.3, 3.8)a,b |
| ESRD | 25 (3.8) | 8.6 | 234 | 20 (80.0) | 8.6 (4.8, 12.3)a,b,c |
p<0.001 for rate ratio compared to:
normoalbuminuria;
microalbuminuria;
overt nephropathy.
Abbreviations: follow-up time, FUT; albuminuria excretion rate, AER; end stage renal disease, ESRD.
Association between renal disease and 10-yr or 20-yr mortality
To approximately replicate the recently published FinnDiane results, we calculated 10-year specific hazard ratios and SMRs according to baseline RD status (Table 3). The risk of death in individuals with NA at baseline was not significantly greater than that in the local age and sex-matched general population (SMR 1.3, 95% CI 0.2–2.5); however, mortality increased step-wise with increasing renal damage, as did the SMR relative to the local general population.
Table 3.
10- and 20-year mortality risk and standardized mortality ratios in EDC participants with type 1 diabetes categorized by renal damage status at baseline, before after adjustment for other risk factors.
| 10-year follow-up |
||||||
|---|---|---|---|---|---|---|
| Unadjusted HR | 95% CI | Adjusted HRa | 95% CI | Adjusted SMRb | 95% CI | |
| AER Category | ||||||
| Normoalbuminuria (Ref) | 1.0 | --- | 1.0 | --- | 1.3 | (0.2, 2.5) |
| Microalbuminuria | 6.8 | (2.4, 19.1) | 3.5 | (1.1, 11.4) | 6.6 | (3.0, 10.1) |
| Overt nephropathy | 16.3 | (6.4, 42.0) | 5.2 | (1.6, 16.1) | 14.2 | (9.2, 19.2) |
| ESRD | 68.6 | (25.1, 187.6) | 28.8 | (8.7, 95.9) | 38.9 | (19.8, 57.9) |
| 20-year follow-up |
||||||
|---|---|---|---|---|---|---|
| Unadjusted HR | 95% CI | Adjusted HRa | 95% CI | Adjusted SMRb | 95% CI | |
| AER Category | ||||||
| Normoalbuminuria (Ref) | 1.0 | --- | 1.0 | --- | 2.0 | (1.2, 2.8) |
| Microalbuminuria | 4.5 | (2.7, 7.5) | 2.4 | (1.4, 4.3) | 6.4 | (4.4, 8.4) |
| Overt nephropathy | 9.3 | (5.8, 14.6) | 4.0 | (2.3, 7.0) | 12.5 | (9.5, 15.4) |
| ESRD | 28.9 | (15.9, 52.6) | 9.0 | (4.3, 18.7) | 29.8 | (16.8, 42.9) |
Variables available to the model: duration of diabetes, sex, race, WHR, HbA1c, SBP, DBP, BP medication use, HDL-c, non-HDL-c, WBC count, estimated GFR, presence of macrovascular disease, presence of proliferative retinopathy, and ever smoker.
Adjusted for age, race, and sex
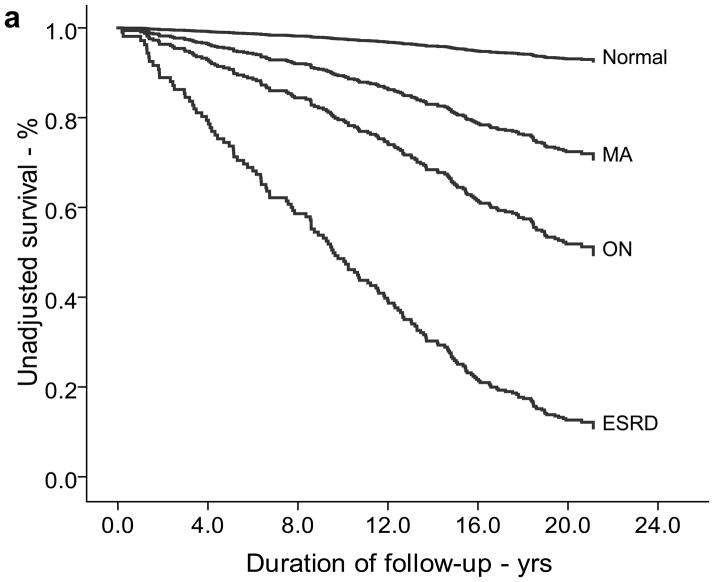
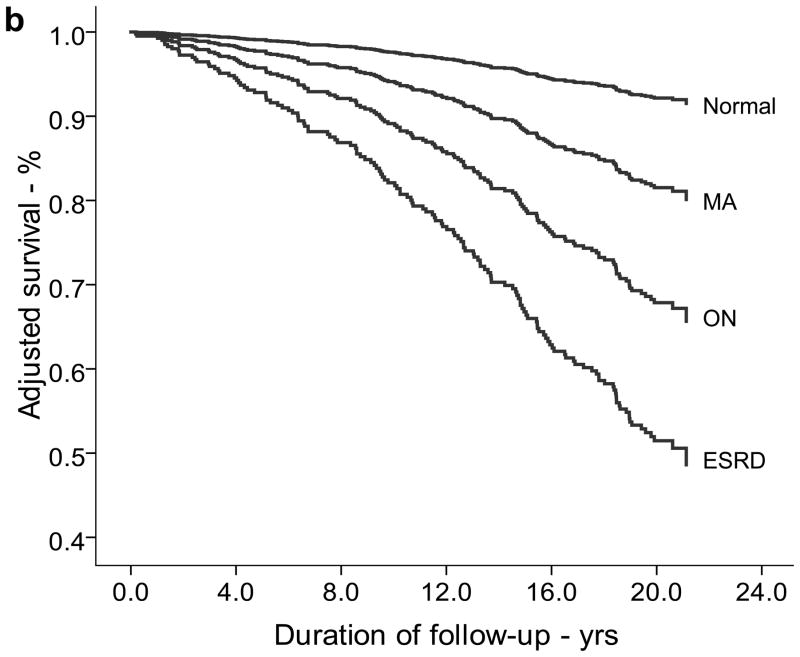
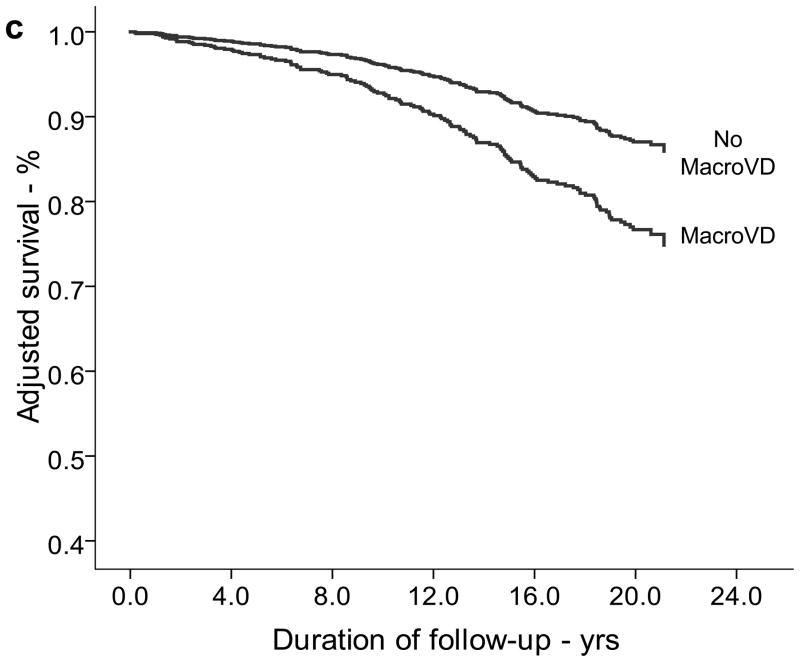
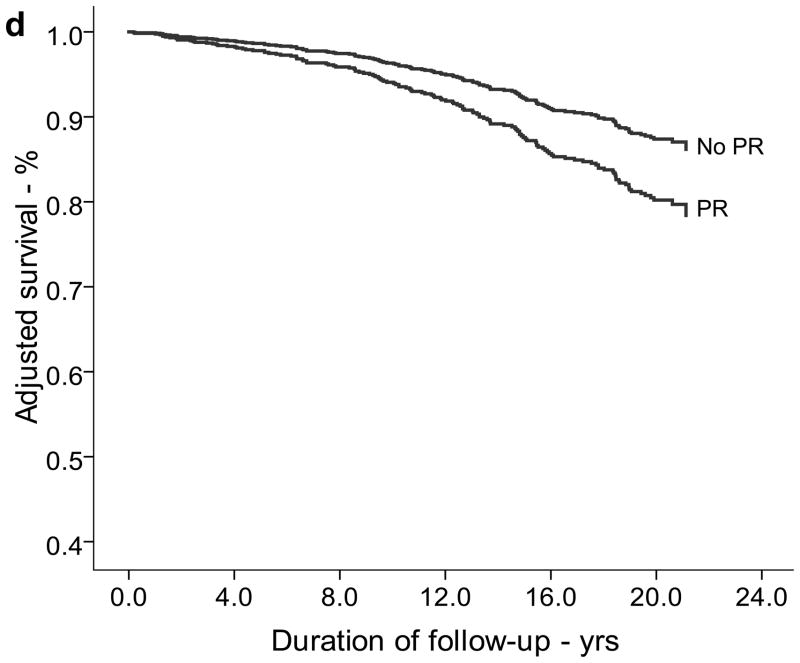
Twenty-year survival curves generated using multivariable Cox-regression analysis are illustrated by baseline stages of RD, macrovascular disease, or proliferative retinopathy (Figure 1). As can be seen, renal disease categories showed the greatest impact on survival. Survival curves did not differ when stratified by sex or after excluding individuals with ESRD (data not shown). Compared to those with NA at baseline, individuals with MA, ON, or ESRD had 20-year mortality risks that were 2.4 (95% CI 1.4–4.3), 4.0 (2.3–7.0), or 9.0 (4.3–18.7) times higher, respectively (Table 3). Other significant predictors of 20-year mortality that remained in the multivariable model included male sex (HR 1.7, 95% CI 1.1–2.6), longer diabetes duration (1.4, 1.1–1.7), greater WHR (1.5, 1.2–1.9), higher HbA1c level (1.3, 1.1–1.6), higher SBP (1.2, 1.0 – 1.4), positive smoking history (1.9, 1.3–2.7), MDRD eGFR<60 ml min−1 1.73 m−2 (1.8, 1.1–2.9), and presence of macrovascular disease (1.9, 1.3–2.9). Other significant predictors of mortality at the 10-year follow-up did not dramatically differ from those at 20 years, except that baseline non-HDL cholesterol replaced HbA1c level in the model (data not shown). Compared to the age and sex-matched general population, individuals with NA had twice as many deaths as would have been expected in the general population over 20 years of follow-up (SMR 2.0, 95% CI 1.2–2.8). The SMRs increase steadily for individuals with increasingly severe RD, e.g., MA 6.4 (4.4–8.4); ON 12.5 (9.5–15.4); and ESRD 29.8 (16.8–42.9).
Figure 1.
Survival plots based on Cox-adjusted analysis of EDC participants stratified for the presence and severity of albuminuria, both unadjusted (a) and adjusted (b), the presence of macrovascular disease (c), and the presence of proliferative retinopathy (d) at baseline. Panels b–d are adjusted for duration of diabetes, sex, race, WHR, HbA1c, SBP, renal function (eGFR-MDRD), ever smoker, and the other complications not being presented (i.e., macrovascular disease, proliferative retinopathy, and/or renal damage). Other variables available to the model but not selected include: DBP, BP medication use, HDL and non-HDL cholesterol, and WBC count. Panel d not adjusted for renal damage status (albuminuria category)
Mortality in participants with normoalbuminuria
We conducted a subgroup analysis of individuals with NA at baseline to determine how many progressed to RD during the study period, and if progression to RD could explain their two-fold increased mortality over the longer (20-yr) follow-up period. Of the 347 individuals with NA at baseline, 64 (18.4%) progressed to RD (MA, n=33; ON, n=22; ESRD, n=9) over a median follow-up of 17.9 years. For those who remained free of RD, the median follow-up time was 18.2 yrs.
In the baseline NA group, 13 (4.6%) individuals of those who remained free of RD (n=283) died during the 20 year period compared to 11 (17.2%) of those who progressed to RD (type 1 diabetes duration-adjusted hazards ratio from time-varying Cox model = 4.3, 95% CI 1.6–12.1). After exclusion of the 64 individuals with NA at baseline who progressed to RD, the adjusted 20-year age and sex-matched SMR for the NA group fell from 2.0 to 1.2 (95% CI 0.5–1.9).
Comparison of cause of death by renal disease status
We also compared the primary cause of death in those who consistently had NA to those with baseline NA who later developed RD during follow-up (Table 4). Those with RD had a longer duration of diabetes (p<0.05) and in 93% of cases, their death was primarily attributed to a diabetes-related cause. In contrast, only 54% of deaths in the NA group were diabetes related (p=0.001). Of these seven diabetes-related deaths in the NA group, two were due to hypoglycemia (one complicated by alcohol abuse), four due to cardiac disease, and one due to pneumonia (complicated by tobacco abuse and asthma).
Table 4.
Primary cause of death of Pittsburgh EDC study participants by most recent renal damage category.
| Variables | Normoalbuminuria | Any Renal Damage |
|---|---|---|
| N (%) | 284 (43.2) | 374 (56.8) |
| Overall Deaths (%) | 13 (4.6) | 139 (37.2) |
| Mean Diabetes Duration at Death | 30.3 ± 8.9 | 35.3 ± 8.0a |
| Cause of Deathb | ||
| Acute diabetes complicationsc | 2 (15.4) | 16 (11.5) |
| Chronic diabetes complicationsd | 5 (38.5) | 113 (81.3) |
| Non-diabetes related causese | 6 (46.2) | 9 (6.5) |
| Unknown | 0 (0.0) | 1 (0.7) |
p≤0.05;
p≤0.001
Includes deaths from hypoglycemia and diabetic ketoacidosis
Includes deaths from cardiovascular, renal, infectious, and other diabetes-related causes (e.g., diabetic gangrene, brain damage secondary to diabetes)
Includes deaths from accident, suicide, and other non-diabetes-related causes (e.g., multiple sclerosis, gastrointestinal bleeding)
Discussion
Our results confirm and expand, with longer follow-up, previously published findings by the FinnDiane group[8] demonstrating that in the absence of renal disease, individuals with type 1 diabetes experience mortality rates similar to those in the general population. Thus, although the risk of death among participants with normoalbuminuria at study entry was twice the risk of death in the age- and sex-matched general population after 20 years of follow-up, restricting analyses to individuals maintaining normoalbuminuria throughout the duration of the study produced mortality rates not dissimilar to those in the general population. Correspondingly, a much greater proportion of deaths was due to non-diabetes related causes among deceased who had remained normoalbuminuric, whereas individuals with renal disease died primarily from acute and chronic diabetes complications.
It has long been known that the development of overt nephropathy in type 1 diabetes bears excess mortality risk,[17] although the importance of microalbuminuria has been less clear, both because of its often transient nature and also because its sensitivity in identifying those at risk of progressive renal function loss in diabetes has been questioned.[20–22] Nevertheless, we have previously shown that although moderately decreased estimated renal function (e.g., glomerular filtration rate) can occur in type 1 diabetes in the absence of preceding or concurrent albuminuria, this event is rare, particularly when the Cockcroft-Gault formula is used as opposed to the Modification of Diet in Renal Disease (MDRD) study formula to estimate renal function.[23] Moreover, the importance of microalbuminuria was further emphasized in a recent analysis of risk factors for major outcomes of type 1 diabetes, comprising the aggregate of coronary artery disease, renal failure and diabetes-related death, where it emerged as the single best predictor from all individual measures studied, including HbA1.[24] In the present report, the presence of albuminuria at study entry was associated with an increased risk of mortality during follow-up. Indeed, mortality risk increased linearly with worsening of albuminuria, reaching, among those with ESRD, 30 times the mortality observed in the age- and sex-matched general population.
Considerable focus has been placed on the search for potential mechanisms linking renal disease with excess mortality in diabetes and a large body of literature has addressed the association between renal and cardiovascular disease. However, although renal damage (albuminuria) is a risk factor for cardiovascular outcomes, whether this relationship can be attributed to abnormalities caused by renal disease leading to atherosclerosis, or simply worsening of known cardiovascular risk factors is unclear.[24] In addition, a further potential mechanism may reflect the “common soil” hypothesis, i.e. both renal and cardiovascular states result from the same predisposing factor. In fact, insulin resistance has been proposed as one such factor underlying both renal and cardiovascular complications,[25, 26] and thus, could potentially explain much of the link between renal and cardiovascular outcomes. Nonetheless, we have previously shown that overt nephropathy is a strong independent risk factor for incident “hard” CAD events (but not total CAD), even after allowing for standard risk factors including lipid and blood pressure levels as well as a measure of insulin resistance.[25]
Of particular note is the finding that the vast majority of deaths in the renal disease group (93%) were related to diabetes, whereas nearly half of the deaths in those without renal disease were clearly not associated with diabetes at all. It should be stressed that these cause of death classifications were made before these analyses were conceived and performed and thus no potential bias exists. However, half the deaths in the normoalbuminuric group appear to be diabetes related (i.e., acute and chronic diabetes complications). We thus cannot totally exclude a minor increased mortality risk in the absence of renal disease, although any such increase is likely to be very small. Interestingly, two of the seven “diabetes-related” deaths in the NA group had significant concomitant conditions (alcohol abuse and asthma).
Although these results, along with the recently published findings from the FinnDiane study,[8] are encouraging and suggest that prevention of kidney disease virtually eliminates the excess mortality associated with this diabetes type, analyses of complication rates over time within the EDC study demonstrate that still much work has to be done in preventing renal disease. For while ESRD has declined dramatically and a declining trend in the incidence of overt nephropathy was also noted, this latter improvement was lost with longer follow-up, suggesting that advanced renal disease incidence is merely being delayed, not prevented.[27] In addition, CAD event rates have also not shown a fall after 30 years of follow-up,[27] although a recent comparative analysis of the DCCT and EDC cohorts suggest that intensive therapy may reduce 30 year cardiovascular disease incidence.[28] Considerable effort should then be aimed at the control of modifiable risk factors, including hyperglycemia, dyslipidemia, and hypertension.
The EDC study has several strengths for evaluating the relationship between renal disease and mortality, including its prospective design with biennial examinations to assess albuminuria status, its long-term follow-up to ascertain mortality, and its detailed classification of cause of death, including death certificates, autopsy and hospital records and review by an expert committee, using a standardized protocol to determine the primary cause of death and to rank contributory causes.[17] Ascertainment of numerous relevant demographic and clinical variables also allowed us to incorporate these into our analysis to minimize confounding. The longitudinal nature of the data also allows the assessment of the effect of progression from normoalbuminuria to renal disease on mortality. Renal disease classifications were based on multiple samples (and confirmed by persistence or progression at the next examination) using identical protocols throughout the study period. Our data are remarkably consistent with those previously published from the FinnDiane study, thus strengthening the overall validity, particularly given the different socioeconomic and healthcare backgrounds from which both cohorts derive.[8, 29, 30]
However, this study is not without limitations. Our cohort is hospital-based; however, a comparison of the EDC population with the Allegheny County type 1 diabetes registry found the EDC cohort to be epidemiologically representative of the local type 1 diabetes population.[11] Also, the EDC population consists of individuals with long-standing diabetes. Thus, these data partially reflect outdated diabetes management and care, and may not be generalizable to individuals recently diagnosed with type 1 diabetes, whose experience may more closely resemble that of the DCCT intensive therapy cohort, as recently described.[28]
In conclusion, our results demonstrate that in long-term follow-up, renal disease, including persistent microalbuminuria, is a key determinant of long-term excess mortality in type 1 diabetes, but that individuals with type 1 diabetes who avoid renal disease appear to achieve long-term mortality similar to, or only marginally higher, than seen in the general population. These results and those of the FinnDiane study should help focus attention on the identification of those at risk of microalbuminuria[31] and the development of appropriate prevention strategies.
Acknowledgments
The Pittsburgh EDC Study was supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (R01-DK034818). AMS was supported by a training grant from the National Institute of Diabetes and Digestive and Kidney Diseases (F30-DK082137). The authors also acknowledge the long term help of the EDC participants, and Jason Sanders (University of Pittsburgh, Pittsburgh, PA) for assistance with manuscript preparation.
Abbreviations
- AER
albumin excretion rate
- BP
blood pressure
- EDC
Epidemiology of Diabetes Complications
- eGDR
estimated glucose disposal rate
- eGFR
estimated glomerular filtration rate
- ESRD
end stage renal disease
- HDL-c
high density lipoprotein cholesterol
- MA
microalbuminuria
- MDRD
Modification of Diet in Renal Disease
- NA
normoalbuminuria
- ON
overt nephropathy
- SMR
standardized mortality ratio
Footnotes
Conflict of Interest Statement
We have no conflicts of interest to disclose.
Author Contributions
TJO had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: TJO, AMS, RGM, TC. Acquisition of data: RGM, AMS. Analysis and interpretation of the data: TJO, AMS, RGM, TC. Drafting the manuscript: AMS, RGM, TC. Critical review of the manuscript for important intellectual content: TJO, AMS, RGM, TC. Statistical analysis: AMS, RGM. Obtained funding: TJO. Administrative, technical, or material support: TJO, RGM, TC. Study supervision: TJO.
References
- 1.Asao K, Sarti C, Forsen T, et al. Long-term mortality in nationwide cohorts of childhood-onset type 1 diabetes in Japan and Finland. Diabetes Care. 2003;26:2037–2042. doi: 10.2337/diacare.26.7.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nishimura R, LaPorte RE, Dorman JS, Tajima N, Becker D, Orchard TJ. Mortality trends in type 1 diabetes. The Allegheny County (Pennsylvania) Registry 1965–1999. Diabetes Care. 2001;24:823–827. doi: 10.2337/diacare.24.5.823. [DOI] [PubMed] [Google Scholar]
- 3.Rossing P, Hougaard P, Borch-Johnsen K, Parving HH. Predictors of mortality in insulin dependent diabetes: 10 year observational follow up study. BMJ. 1996;313:779–784. doi: 10.1136/bmj.313.7060.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Messent JW, Elliott TG, Hill RD, Jarrett RJ, Keen H, Viberti GC. Prognostic significance of microalbuminuria in insulin-dependent diabetes mellitus: a twenty-three year follow-up study. Kidney Int. 1992;41:836–839. doi: 10.1038/ki.1992.128. [DOI] [PubMed] [Google Scholar]
- 5.Forsblom CM, Groop PH, Ekstrand A, Groop LC. Predictive value of microalbuminuria in patients with insulin-dependent diabetes of long duration. BMJ. 1992;305:1051–1053. doi: 10.1136/bmj.305.6861.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hovind P, Tarnow L, Rossing K, et al. Decreasing incidence of severe diabetic microangiopathy in type 1 diabetes. Diabetes Care. 2003;26:1258–1264. doi: 10.2337/diacare.26.4.1258. [DOI] [PubMed] [Google Scholar]
- 8.Groop PH, Thomas MC, Moran JL, et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes. 2009;58:1651–1658. doi: 10.2337/db08-1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Orchard TJ, Dorman JS, Maser RE, et al. Factors associated with avoidance of severe complications after 25 yr of IDDM. Pittsburgh Epidemiology of Diabetes Complications Study I. Diabetes Care. 1990;13:741–747. doi: 10.2337/diacare.13.7.741. [DOI] [PubMed] [Google Scholar]
- 10.Orchard TJ, Dorman JS, Maser RE, et al. Prevalence of complications in IDDM by sex and duration. Pittsburgh Epidemiology of Diabetes Complications Study II. Diabetes. 1990;39:1116–1124. doi: 10.2337/diab.39.9.1116. [DOI] [PubMed] [Google Scholar]
- 11.Wagener DK, Sacks JM, LaPorte RE, Macgregor JM. The Pittsburgh study of insulin-dependent diabetes mellitus. Risk for diabetes among relatives of IDDM. Diabetes. 1982;31:136–144. doi: 10.2337/diab.31.2.136. [DOI] [PubMed] [Google Scholar]
- 12.Warnick GR, Albers JJ. Heparin--Mn2+ quantitation of high-density-lipoprotein cholesterol: an ultrafiltration procedure for lipemic samples. Clin Chem. 1978;24:900–904. [PubMed] [Google Scholar]
- 13.Williams KV, Erbey JR, Becker D, Arslanian S, Orchard TJ. Can clinical factors estimate insulin resistance in type 1 diabetes? Diabetes. 2000;49:626–632. doi: 10.2337/diabetes.49.4.626. [DOI] [PubMed] [Google Scholar]
- 14.Ellis D, Coonrod BA, Dorman JS, et al. Choice of urine sample predictive of microalbuminuria in patients with insulin-dependent diabetes mellitus. Am J Kidney Dis. 1989;13:321–328. doi: 10.1016/s0272-6386(89)80039-3. [DOI] [PubMed] [Google Scholar]
- 15.Levey AS, Coresh J, Greene T, et al. Expressing the Modification of Diet in Renal Disease Study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2007;53:766–772. doi: 10.1373/clinchem.2006.077180. [DOI] [PubMed] [Google Scholar]
- 16.Early Treatment of Diabetic Retinopathy Study Coordinating Center: Manual of Operations. University of Maryland School of Medicine; Baltimore, MD: 1980. [Google Scholar]
- 17.International evaluation of cause-specific mortality and IDDM. Diabetes Epidemiology Research International Mortality Study Group. Diabetes Care. 1991;14:55–60. doi: 10.2337/diacare.14.1.55. [DOI] [PubMed] [Google Scholar]
- 18.Epidemiologic Query and Mapping System (EpiQMS). Bureau of Health Statistics, Pennsylvania Department of Health. [accessed March 17, 2010]; Available from http://app2.health.state.pa.us/epiqms.
- 19.Armstrong BG. Comparing standardized mortality ratios. Ann Epidemiol. 1995;5:60–64. doi: 10.1016/1047-2797(94)00032-o. [DOI] [PubMed] [Google Scholar]
- 20.Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR. Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes. 2006;55:1832–1839. doi: 10.2337/db05-1620. [DOI] [PubMed] [Google Scholar]
- 21.Kramer HJ, Nguyen QD, Curhan G, Hsu CY. Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA. 2003;289:3273–3277. doi: 10.1001/jama.289.24.3273. [DOI] [PubMed] [Google Scholar]
- 22.Molitch ME, Steffes M, Sun W, et al. The Development and Progression of Renal Insufficiency with and without Albuminuria in Adults with Type 1 Diabetes Mellitus in the Diabetes Control and Complications Trial (DCCT) and Epidemiology of Diabetes Interventions and Complications (EDIC) Study. Diabetes Care. 2010 doi: 10.2337/dc09-1098. ePub 4/24/2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costacou T, Ellis D, Fried L, Orchard TJ. Sequence of progression of albuminuria and decreased GFR in persons with type 1 diabetes: a cohort study. Am J Kidney Dis. 2007;50:721–732. doi: 10.1053/j.ajkd.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Pambianco G, Costacou T, Orchard TJ. The prediction of major outcomes of type 1 diabetes: a 12-year prospective evaluation of three separate definitions of the metabolic syndrome and their components and estimated glucose disposal rate: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes Care. 2007;30:1248–1254. doi: 10.2337/dc06-2053. [DOI] [PubMed] [Google Scholar]
- 25.Orchard TJ, Olson JC, Erbey JR, et al. Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care. 2003;26:1374–1379. doi: 10.2337/diacare.26.5.1374. [DOI] [PubMed] [Google Scholar]
- 26.Orchard TJ, Chang YF, Ferrell RE, Petro N, Ellis DE. Nephropathy in type 1 diabetes: a manifestation of insulin resistance and multiple genetic susceptibilities? Further evidence from the Pittsburgh Epidemiology of Diabetes Complication Study. Kidney Int. 2002;62:963–970. doi: 10.1046/j.1523-1755.2002.00507.x. [DOI] [PubMed] [Google Scholar]
- 27.Pambianco G, Costacou T, Ellis D, Becker DJ, Klein R, Orchard TJ. The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes. 2006;55:1463–1469. doi: 10.2337/db05-1423. [DOI] [PubMed] [Google Scholar]
- 28.Nathan DM, Zinman B, Cleary PA, et al. Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983–2005) Arch Intern Med. 2009;169:1307–1316. doi: 10.1001/archinternmed.2009.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arun CS, Stoddart J, Mackin P, MacLeod JM, New JP, Marshall SM. Significance of microalbuminuria in long-duration type 1 diabetes. Diabetes Care. 2003;26:2144–2149. doi: 10.2337/diacare.26.7.2144. [DOI] [PubMed] [Google Scholar]
- 30.Allen KV, Walker JD. Microalbuminuria and mortality in long-duration type 1 diabetes. Diabetes Care. 2003;26:2389–2391. doi: 10.2337/diacare.26.8.2389. [DOI] [PubMed] [Google Scholar]
- 31.Vergouwe Y, Soedamah-Muthu SS, Zgibor J, et al. Progression to microalbuminuria in type 1 diabetes: development and validation of a prediction rule. Diabetologia. 2010;53:254–262. doi: 10.1007/s00125-009-1585-3. [DOI] [PMC free article] [PubMed] [Google Scholar]