Abstract
Multiple sclerosis (MS) is associated with significant economic burden and high rates of unemployment. This investigation evaluated patient and disease characteristics associated with work loss and work initiation using the NARCOMS patient registry. Patient and disease characteristics associated with transitions to unemployment or employment were evaluated cross-sectionally and prospectively over the course of two assessment periods (mean interval of 1.56 ± 0.93 years). Eligible participants included 8,867 patients for the cross-sectional component, and 8,122 for longitudinal analyses. At Time 1 and Time 2 56–58 % of MS patients were not employed. At Time 1, unemployed participants more likely to have a progressive disease course, had a longer symptom duration, greater levels of disability as measured by the PDDS, and greater functional limitations across all domains of the performance scales (p < 0.0001 for all). At Time 2, increasing MS symptoms in the past 6 months increased the odds of becoming unemployed. In addition, specific problems in mobility, hand function, fatigue, and cognitive performance domains were associated with increased odds of becoming unemployed. Less severe problems in similar areas, including mobility, hand function, and cognitive functioning were also predictive of work initiation among patients not employed. MS is associated with high rates of unemployment. Specific physical and mental health limitations confer risk of employment cessation over time, as well as the likelihood of employment initiation. This study has implications for rehabilitation interventions to target specific MS related limitations that place patients at greatest risk for work status changes.
Keywords: multiple sclerosis, disability, employment, rehabilitation
Introduction
Multiple sclerosis (MS) is a chronic neurological condition affecting young adults during critical years of work life. It is well known that MS is associated with a heavy economic burden coupled with a decreased ability to remain in the work force. The loss of employment brings detrimental consequences to patients and families with respect to short-term and long-term economic, psychosocial and healthcare utilization domains [27].
Previous studies of employment and work loss in MS cite unemployment rates ranging from 24–80 % [5, 6, 13, 16, 17, 19, 21, 28, 30, 31, 35–37, 40]. These studies have found that patients are less likely to be employed when they exhibit global markers of disease severity including physician disability ratings (e.g. the Expanded Disability Status Scale (EDSS)) [6, 7, 12, 15, 20, 22, 29]. In addition, unemployment has been associated with decreased ambulation and mobility in relation to changes in work status [3, 11], longer disease duration [2, 4], and a progressive disease course [17, 41]. Specific symptoms such as fatigue [10, 11, 40], perceived levels of cognitive dysfunction [9], and poorer performance on neuropsychological tests have also been associated with employment problems in MS [3, 34, 40]. Specific patient demographic characteristics are often associated with employment loss in MS, including older age and lower educational attainment [3, 6, 22]. Some studies have reported women are at greater risk for work loss [9, 22], but some have also found men to be at increased risk for work loss [6].
While there is a growing literature on factors associated with employment status in patients with MS, there are also a number of shortcomings in this literature. Most studies to date have been cross sectional, as opposed to predictive. In addition, research has focused exclusively on patients leaving the workforce with virtually no attention to the possibility that patients re-enter the workforce. MS is a condition that predominantly affects women, particularly those of childbearing age. Therefore, work status in MS may be a dynamic process and there are likely transitions both out of, but also into the workforce. The purpose of this investigation was to evaluate patient and disease characteristics as temporal predictors of work cessation and re-entry into the work force. This investigation was conducted as a secondary data analysis of self-reported data from the North American Research Committee on Multiple Sclerosis (NAR-COMS) patient registry.
Methods
NARCOMS MS Patient Registry and selection criteria
Beginning in 1996, the Consortium of MS Centers in collaboration with Yale University initiated the NARCOMS MS Patient Registry. The overarching goal of this registry was to facilitate clinical and epidemiological research in MS [42]. The NARCOMS registry is a patient driven database, with self-reported information collected semi-annually through the internet or through mail survey forms.
The inclusion criterion to participate in NARCOMS is a diagnosis of MS. Data collected include demographic information, healthcare insurance status, MS related medical history, the use of disease modifying therapies for MS, symptomatic therapies, and healthcare service utilization.
For the purposes of this study, NARCOMS registry patients were selected based on two criteria. Patients less than 64 were included to exclude people who are not working due to retiring. Patients also had to have available employment data for two subsequent time periods.
Disability measurement
Patient Determined Disease Steps (PDDS)
The PDDS is an 8-level measure of disability (0 = normal to 8 = bed-ridden) that, like the analog provider administered EDSS [20], is predominantly influenced by gait and ambulation disturbances. The PDDS correlates highly with the EDSS (spearman r = 0.93) [39].
Performance scales
The performance scales reflect disability in specific functional domains: mobility, hand function, fatigue, vision, cognitive, sensory, pain, bladder function, and spasticity [39]. Disability is rated by the participants on a scale of 0 (normal) to 5 (total disability) for each of the domains except mobility, which ranges from 0 to 6.
Statistical analyses
Analyses were conducted with the use of the Intercooled STATA statistical package version 8.2 (StataCorp, LP, College Station, TX). Group comparisons were conducted using t-test or chi-square for continuous and categorical variables, respectively. Multivariate logistic regressions were conducted to determine the contribution of each predictor variable on the change from employed to unemployed status between the two time-points as well as the change from unemployed to employed. In order to determine the strength of the intercorrelations among related predictors, Multicollinearity was assessed for each logistic regression model using the collin function in STATA. The commonly utilized variance inflation factor (VIF) and Tolerance techniques were utilized to detect predictor variables that were highly intercorrelated, creating redundancy in predictors and subsequent proportion of variance accounted for. Variables were dropped if the VIF was greater or equal to 10 or the Tolerance was less than 0.1.
Results
Demographics, disease status, and disability characteristics across employment status groups
The selection criteria resulted in a sample of 8,867 NAR-COMS registry participants. These participants were very similar across demographic characteristics compared to previous investigations utilizing larger subsets of NARCOMS participants [14, 25, 26, 43]. For the entire subgroup, the mean age was 47.60 ± 8.59, participants were 75 % female, and 93 % Caucasian.
Group comparisons using t-tests or chi-square statistics for continuous and categorical variables, respectively, among demographic characteristics across employment status (Table 1), revealed that when compared to participants reporting unemployment, employed participants were younger (p < 0.0001), more likely to be female (p < 0.001), more likely to be Caucasian (p < 0.0001), and had greater levels of educational attainment (p < 0.0001).
Table 1.
Demographic and patient characteristics of NARCOMS participants
| Cohort (N = 8867) | Employed (N = 3881) | Unemployed (N = 4986) | |
|---|---|---|---|
| Age | 47.60 ± 8.59 | 45.02 ± 8.29 | 49.62 ± 8.28* |
| Female (%) | 73.9 | 75.9 | 72.3* |
| Caucasian (%) | 92.6 | 93.9 | 91.5* |
| Education | |||
| % < College degree | 57.8 | 48.1 | 65.4* |
| % College degree and postgraduate | 42.2 | 51.9 | 34.6* |
| MS Worsened in previous 6 months (%) | 53.0 | 38.2 | 62.6* |
| Duration of MS symptoms (years) | 18.09 ± 10.12 | 15.27 ± 9.26 | 20.33 ± 10.22* |
| PDDSa median (Q25, Q75) | 3 (1,5) | 2 (0,3) | 4 (3,6)* |
| Performance scales | |||
| Mobility median (Q25, Q75) | 3 (1,4) | 1 (0,3) | 4 (2,5)* |
| Hand function median (Q25, Q75) | 1 (1,2) | 1 (0,2) | 2 (1,3)* |
| Vision median (Q25, Q75) | 1 (0,2) | 1 (0,2) | 1 (0,2)* |
| Fatigue median (Q25, Q75) | 3 (2,4) | 2 (1,3) | 3 (2,4)* |
| Cognitive median (Q25, Q75) | 1 (1,2) | 1 (0,2) | 2 (1,3)* |
| Bladder/bowel median (Q25, Q75) | 2 (1,3) | 1 (0,2) | 2 (1,3)* |
| Sensory median (Q25, Q75) | 1 (1,3) | 1 (1,2) | 2 (1,3)* |
| Spasticity median (Q25, Q75) | 1 (1,3) | 1 (0,2) | 2 (1,3)* |
| Pain median (Q25, Q75) | 1 (1,3) | 1 (0,2) | 2 (1,3)* |
PDDS Patient Determined Disease Steps
t-test (continuous variables) or chi-square (dichotomous variables) p < 0.0001
Group comparisons of patient and disease characteristics across groups indicate that a greater proportion of unemployed patients report worsening of symptoms in the past 6 months (Table 1). In addition, unemployed participants had a significantly higher PDDS (p<0.0001), and greater reported disability across all functional domains on the performance scales (p < 0.0001 for all).
Employment status from Times 1 and 2
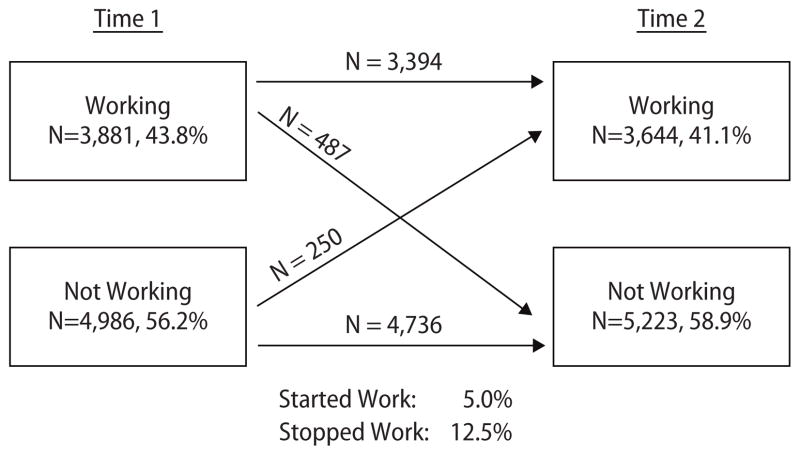
Transitions in employment status are displayed in Fig. 1. Time 1 reflects the first assessment period with employment data reported, and Time 2 reflects the next subsequent period with employment data reported (mean lag = 1.56 ± 0.53 years). At Time 1, 43.8 % of participants were employed, decreasing to 41.1 % at Time 2. From Time 1 to Time 2 487 (12.5 % of those working; 6 % of entire sample) stopped working, while 250 (5.0 % of those not working; 3 % of entire sample) began working.
Fig. 1.
Employment status in time 1 and time 2
Predictors of work loss between Times 1 and 2
Logistic regression analyses (Table 2) were conducted using all of the above demographic, patient and disease characteristics, and disability status as predictors of work loss between Time 1 and Time 2 among patients who were employed at Time 1. None of the predictors met thresholds for multicollinearity and were retained in the model. Educational attainment and age emerged as the only demographic characteristics that were significantly predictive of employment loss at Time 2, with greater levels of education being protective against work loss (OR 0.63, CI 0.51–0.77, p < 0.0001) and older age predicting work loss (OR 1.02, CI 1.01–1.03, p < 0.01). Other demographic predictors including ethnicity and gender were not significantly predictive of work loss.
Table 2.
Results of logistic regression: predictors of transitions out of the work force
| Outcome: work cessation at Time 2 | Demographic model (N = 3,624) |
Full model (N = 3,624) |
||||
|---|---|---|---|---|---|---|
| OR | 95 % CI | p-value | OR | 95 % CI | p-value | |
| Time lag Time 1 to Time 2 | 1.04 | 0.93–1.16 | 0.51 | 1.03 | 0.92–1.15 | 0.60 |
| Age | 1.02 | 1.01–1.03 | < 0.01 | 1.01 | 1.00–1.03 | 0.20 |
| Female | 0.85 | 0.68–1.07 | 0.18 | 1.00 | 0.79–1.27 | 1.00 |
| Not Caucasian | 1.27 | 0.85–1.90 | 0.25 | 1.13 | 0.74–1.74 | 0.57 |
| College/post-graduate degree | 0.63 | 0.51–0.77 | < 0.0001 | 0.68 | 0.55–0.84 | < 0.0001 |
| % MS worsened in previous 6 months | 1.01 | 0.99–1.02 | 0.08 | 1.41 | 1.11–1.79 | < 0.01 |
| Duration of MS symptoms (years) | 1.00 | 0.99–1.01 | 0.77 | |||
| Patient Determined Disease Steps | 0.97 | 0.86–1.09 | 0.57 | |||
| Performance scales | ||||||
| Mobility | 1.20 | 1.04–1.37 | < 0.05 | |||
| Hand function | 1.25 | 1.12–1.40 | < 0.0001 | |||
| Vision | 1.00 | 0.89–1.11 | 0.97 | |||
| Fatigue | 1.18 | 1.06–1.32 | < 0.01 | |||
| Cognitive | 1.15 | 1.04–1.29 | < 0.05 | |||
| Bladder/bowel | 1.09 | 0.98–1.21 | 0.11 | |||
| Sensory | 0.98 | 0.88–1.10 | 0.79 | |||
| Spasticity | 0.94 | 0.85–1.05 | 0.30 | |||
| Pain | 1.01 | 0.91–1.11 | 0.92 | |||
After accounting for demographic variables, patient and disease characteristics, PDDS, and performance scales were entered into the logistic regression model. Reported worsening of symptoms over the past 6 months was significantly predictive of employment loss (OR 1.41, CI 1.11–1.79, p < 0.01). Disease course and symptoms duration were not significantly predictive of employment loss. In addition, the PDDS also did not significantly predict work loss. Four of the performance scales evaluating specific symptoms were significantly predictive of work loss including mobility problems (OR 1.20. CI 1.04–1.37, p < 0.05), hand function problems (OR 1.25, CI 1.12–1.40, p < 0.0001), fatigue (OR 1.18, CI 1.06–1.32, p < 0.01), and cognitive problems (OR 1.15, CI 1.04–1.29, p < 0.05). Problems with vision bladder or bowel, sensory functioning, spasticity, and pain were not significantly predictive of employment loss.
Predictors of work initiation between Times 1 and 2
Logistic regression analyses (Table 3) were conducted using all of the above demographic, patient and disease characteristics, and disability status as predictors of work initiation between Time 1 and Time 2 among patients who were not employed at Time 1. None of the variables met thresholds for multicollinearity and were retained in the model. Age and educational attainment emerged as demographic characteristics significantly predictive of employment initiation at Time 2, with greater levels of education being predictive of work initiation (for educational level College or Post-graduate degree OR 2.38, CI 1.80–3.13, p < 0.0001); and younger aged individuals more likely to initiate work (OR 0.93, CI 0.91–0.95, p < 0.0001). Other demographic predictors, including ethnicity and gender, were not significantly predictive of work initiation.
Table 3.
Results of logistic regression: predictors of transitions into of the work force
| Outcome: work initiation at Time 2 | Demographic model (N = 4,498) |
Full model (N = 4,498) |
||||
|---|---|---|---|---|---|---|
| OR | 95 % CI | p-value | OR | 95 % CI | p-value | |
| Time lag Time 1 to Time 2 | 0.92 | 0.79–1.06 | 0.22 | 0.93 | 0.80–1.08 | 0.33 |
| Age | 0.93 | 0.91–0.95 | < 0.0001 | 0.94 | 0.92–0.96 | < 0.0001 |
| Female | 1.22 | 0.87–1.72 | 0.25 | 0.81 | 0.57–1.16 | 0.26 |
| Not Caucasian | 0.68 | 0.40–1.18 | 0.17 | 0.74 | 0.43–1.30 | 0.17 |
| College/post-graduate degree | 2.38 | 1.80–3.13 | < 0.0001 | 1.96 | 1.46–2.59 | < 0.0001 |
| % MS worsened in previous 6 months | 0.99 | 0.97–1.01 | 0.29 | 1.04 | 0.75–1.43 | 0.83 |
| Duration of MS symptoms (years) | 1.01 | 0.99–1.03 | 0.49 | |||
| Patient Determined Disease Steps | 0.91 | 0.79–1.05 | 0.19 | |||
| Performance scales | ||||||
| Mobility | 0.82 | 0.69–0.98 | < 0.05 | |||
| Hand function | 0.83 | 0.71–0.97 | < 0.05 | |||
| Vision | 1.03 | 0.89–1.19 | 0.68 | |||
| Fatigue | 0.98 | 0.86–1.13 | 0.81 | |||
| Cognitive | 0.83 | 0.71–0.96 | < 0.05 | |||
| Bladder/bowel | 1.09 | 0.95–1.25 | 0.22 | |||
| Sensory | 1.00 | 0.86–1.16 | 0.99 | |||
| Spasticity | 0.90 | 0.77–1.04 | 0.15 | |||
| Pain | 1.02 | 0.89–1.15 | 0.82 | |||
After accounting for demographic variables, patient and disease characteristics, PDDS, and performance scales were entered into the logistic regression model. Disease course, worsening symptoms, and PDDS did not predict initiation of work. Three of the performance scales evaluating specific symptoms were significantly predictive of work initiation including reduced mobility problems (OR 0.82, CI 0.69–0.98, p < 0.05), reduced hand function problems (OR 0.83 CI 0.71–0.97, p < 0.05), and reduced cognitive problems (OR 0.83, CI 0.71–0.96, p < 0.05). Problems with fatigue, vision, bladder or bowel, sensory functioning, spasticity, and pain were not significantly predictive of employment initiation.
Discussion
The purpose of this investigation was to evaluate employment status and predictors of transitions into and out of the work force in a large cohort of persons with MS. The cross-sectional analyses were largely consistent with previous work. Unemployment rates of 56–58 % were consistent with other studies, although these do vary considerably from 24 to 80 % [5, 6, 13, 16, 17, 19, 21, 28, 30, 31, 35–37, 40]. Our associations between demographic variables (increased age, decreased education, and non-white ethnicity) and MS-related factors (worsening of symptoms, greater disability as measured by the PDDS, and increased disability in all performance domains including mobility, hand function, vision, fatigue, cognitive, bladder/bowel, sensory, spasticity, pain and depression) were also consistent with existing cross-sectional studies [3, 6, 22, 31, 40].
Unlike previous work, this study examined both exit and entry into the workforce. Over the course of two sequential NARCOMS assessment time points, fluctuations were observed both into and out of the workforce; however, twice the number of patients left the workforce (6 % of the entire sample) than entered the workforce (3 %). This finding suggests that employment status is a dynamic process in which patients leave and possibly re-enter the work force. We therefore examined predictors of both of these transitions.
A number of demographic and disease characteristics predicted subsequent loss of employment. Similar to many studies, low educational attainment is associated with increased risk of subsequent work loss, which is generally interpreted in terms of the protective attributes of greater education [8, 32]. Specific disease characteristics were also predictive of employment loss, including mobility, hand function, fatigue and perceived cognitive impairment. The impact of hand function on employment likely reflects the universal occupational demands on hands across labor domains. The impact of fatigue on employment is very consistent with other studies [10, 11]. The impact of perceived cognitive impairment is also consistent with other studies in MS [9]. While correlations between perceptions of cognitive dysfunction and performance on objective cognitive measures vary [18, 23, 24], studies of employment in MS that include neuropsychological testing yield very similar findings [3, 34, 40]. Finally, mobility was predictive of employment loss, which remains consistent with previous work [3, 11].
Similar to previous studies, global measures of disability, in this case the PDDS were associated with unemployment status (e.g., the EDSS) [1, 6, 7, 12, 22, 31, 40]. However, the PDDS was not predictive of work loss over time. This suggests that although global indices of functioning can discriminate between patients who are employed and not employed, more specificity in the assessment of MS symptoms and their impact is required to predict the future loss of employment.
Many of the factors predicting re-entry to the work place mirror those that predict loss of employment including greater levels of educational attainment predict re-entry and younger age. The specific MS related problems that were significantly predictive of re-entry into the workforce included fewer mobility problems, fewer hand function problems and less perceived cognitive difficulties. Unlike loss of employment, patient reported fatigue was not significantly associated with obtaining employment. These results suggest that not only are these symptoms predictive of work cessation, but decreased problems in these areas are associated with work initiation. Also similar to the analysis on predictors of employment loss, overall measures of disability did not predict which patients entered the work force. This again suggests that predicting entry into the work force requires greater specificity.
A number of limitations in this study must be mentioned. First, employment data and longitudinal follow-up were not available on the full NARCOMS sample. While employment data were not collected for some of the sample, some patients did not complete the employment items, and others were lost to follow-up, which may attenuate the generalizability of our findings. However, the subsample of over 8,000 subjects with all complete data represents one of the largest studies to date evaluating employment status in MS. In addition, the interval between Time 1 and 2 is relatively short, and perhaps future studies may prospectively evaluate employment transitions over a longer period of time (e.g., 5 years, 10 years). Another limitation of these analyses is that the cause of employment loss or attainment is unknown. While this prevents us from making finer distinctions (e.g., disability, early retirement, leaving to care for children, choosing not to work, termination for performance failure), this does not invalidate the findings from the longitudinal analyses. Additionally, the NARCOMS dataset has many of the limitations of such registries. As volunteers, they may differ from patients who do not volunteer. In addition, registry data are all self-report and accuracy of clinical information is not verified against medical records. However, previous studies utilizing NARCOMS data suggest that diagnosis status, disability status, and clinical characteristics are similar to large cohort studies of MS patients with available clinical and medical record data [17, 33].
Changes in labor force participation and other employment characteristics other than unemployment status are not captured in these analyses. There is evidence for both quantitative and qualitative changes in the work life of MS patients that are not captured in this investigation. For example, there is evidence that patients with MS experience inhibition in overall career development [38]. Additionally, prior to leaving the work force, many patients first experience MS-related changes including a decrease in the number of hours worked, changes in job characteristics, and the need to decrease job related demands [40]. Future studies characterizing such changes in work force participation are warranted.
In conclusion, these data suggest that close to 60 % of this NARCOMS registry cohort, aged 64 or under at a mean age of 47, are unemployed. Over an average period of 18 months, 6 % percent of the sample (12.5 % of employed sample) became unemployed and 3 % (5 % of those not working) gained employment. Twice the number of registry participants appears to be leaving the workforce compared to those entering. As expected, patients with worsening symptoms are particularly at risk for future employment loss. One important implication of this investigation is that employment should be considered a dynamic process. While some patients may simply leave work permanently, others may experience a period of time in which they cease working, and then subsequently resume. Understanding the factors related to leaving and re-entering the workforce is critical to improving our ability to intervene on behalf of patients.
The second important point is the observation that specific symptoms predict employment loss, better than general estimates of disability. These findings have implications for the improvement of functional domains within both the work and rehabilitation setting. First, employers could provide accommodations to address specific limitations including increased flexibility in work hours and breaks during regular intervals for MS patients with fatigue. Ergonomic solutions to support hand limitations and reduced demands on ambulation could also be beneficial for specific physical limitations. In addition, cognitive dysfunction and fatigue can be addressed in the occupational therapy or rehabilitation setting with specific skills training, improving coping mechanisms, compensatory strategies, or cognitive rehabilitation. This investigation suggests that patients with improved functioning in these domains are more likely to maintain employment or even initiate employment.
Early work cessation or reduction of involvement in the labor force can cause considerable difficulties for persons with MS across economic, health insurance status, and psychosocial domains. MS related symptoms and limitations should be considered in tandem with workplace demands and job characteristics in order to promote maintenance of employment.
Acknowledgments
The authors would like to gratefully acknowledge the following funding sources: NIH R01-HD043323 and K08MH072724 as well as the National Multiple Sclerosis Society FG1481-A-1. We would also like to thank Ed Yelin PhD for guidance in the preparation of this manuscript.
Contributor Information
Laura J. Julian, Email: laura.julian@ucsf.edu, Suite 270, 3333 California Street, 94143-0920 San Francisco, CA, USA, Tel.: +1-415/502-4587, Fax: +1-415/476-9030.
Lea Vella, Veterans Administration Medical Center, San Francisco, CA, USA.
Tim Vollmer, Barrow Neurological Institute, Phoenix, AZ, USA.
Olympia Hadjimichael, Yale University School of Medicine, New Haven, CT, USA.
David C. Mohr, Northwestern University.
References
- 1.Ariel M, Sara D. Health-related quality of life in multiple sclerosis: the impact of disability, gender and employment status. Qual Life Res. 2006;15:259–271. doi: 10.1007/s11136-005-0891-6. [DOI] [PubMed] [Google Scholar]
- 2.Bauer HJ, Firnhaber W, Winkler W. Prognostic criteria in multiple sclerosis. Ann N Y Acad Sci. 1965;122:542–551. doi: 10.1111/j.1749-6632.1965.tb20234.x. [DOI] [PubMed] [Google Scholar]
- 3.Beatty W, Blanco C, Wilbanks S, Paul R, Hames K. Demographic, clinical and cognitive characteristics of multiple sclerosis patients who continue to work. J Neurol Rehabil. 1995;9:167–173. [Google Scholar]
- 4.Beatty WW, Blanco CR, Wilbanks BS, Paul RH, Hames BA. Demographic, clinical, and cognitive characteristics of multiple sclerosis patients who continue to work. J Neurol Rehabil. 1995;9:167–173. [Google Scholar]
- 5.Beatty WW, Blanco CR, Wilbanks SL, Paul RH, Hames KA. Demographic, clinical, and cognitive characteristics of multiple sclerosis patients who continue to work. J Neurol Rehabil. 1995;9:167–173. [Google Scholar]
- 6.Busche KD, Fisk JD, Murray TJ, Metz LM. Short term predictors of unemployment in multiple sclerosis patients. Can J Neurol Sci. 2003;30:137–142. doi: 10.1017/s0317167100053403. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Burden of Illness Group. Burden of illness of multiple sclerosis: part II: quality of life. Can J Neurol Sci. 1998;25:31–38. [PubMed] [Google Scholar]
- 8.de Croon EM, Sluiter JK, Nijssen TF, Dijkmans BAC, Lankhorst GJ, Frings-Dresen MHW. Predictive factors of work disability in rheumatoid arthritis: a systematic literature review. Ann Rheum Dis. 2004;63:1362–1367. doi: 10.1136/ard.2003.020115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edgley K, Sullivan M, Dehoux E. A survey of multiple sclerosis: determinants of employment status. Can J Rehabil. 1991;4:127–132. [Google Scholar]
- 10.Freal JE, Kraft GH, Coryell JK. Symptomatic fatigue in multiple sclerosis. Arch Phys Med Rehabil. 1984;65:135–138. [PubMed] [Google Scholar]
- 11.Genevie L, Kallos JE, Struening EL. Job retention among people with MS. J Neurol Rehabil. 1987;1:131–135. [Google Scholar]
- 12.Grima DT, Torrance GW, Francis G, Rice G, Rosner AJ, Lafortune L. Cost and health related quality of life consequences of multiple sclerosis. Mult Scler. 2000;6:91–98. doi: 10.1177/135245850000600207. [DOI] [PubMed] [Google Scholar]
- 13.Gronning M, Hannisdal E, Mellgren SI. Multivariate analyses of factors associated with unemployment in people with multiple sclerosis. J Neurol Neurosurg Psychiatry. 1990;53:388–390. doi: 10.1136/jnnp.53.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadjimichael O, Kerns RD, Rizzo MA, Cutter G, Vollmer T. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007;127(1–2):35–41. doi: 10.1016/j.pain.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Hammond SR, McLeod JG, Macaskill P, English DR. Multiple sclerosis in Australia: socioeconomic factors. J Neurol Neurosurg Psychiatry. 1996;61:311–313. doi: 10.1136/jnnp.61.3.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson MF, Quaal C, Reeves MA. Effects of multiple sclerosis on occupational and career patterns. Axone. 1991;13:16–17. 20–12. [PubMed] [Google Scholar]
- 17.Jacobs LD, Wende KE, Brownscheidle CM, Apatoff B, Coyle PK, Goodman A, Gottesman MH, Granger CV, Greenberg SJ, Herbert J, Krupp L, Lava NS, Mihai C, Miller AE, Perel A, Smith CR, Snyder DH. A profile of multiple sclerosis: the New York State Multiple Sclerosis Consortium. Mult Scler. 1999;5:369–376. doi: 10.1177/135245859900500511. [DOI] [PubMed] [Google Scholar]
- 18.Julian L, Merluzzi NM, Mohr DC. The relationship among depression, subjective cognitive impairment, and neuropsychological performance in multiple sclerosis. Mult Scler. 2007;13:81–86. doi: 10.1177/1352458506070255. [DOI] [PubMed] [Google Scholar]
- 19.Kornblith AB, La Rocca NG, Baum HM. Employment in individuals with multiple sclerosis. Int J Rehabil Res. 1986;9:155–165. doi: 10.1097/00004356-198606000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 21.Larocca N, Kalb R, Scheinberg L, Kendall P. Factors associated with unemployment of patients with multiple sclerosis. J Chronic Dis. 1985;38:203–210. doi: 10.1016/0021-9681(85)90093-1. [DOI] [PubMed] [Google Scholar]
- 22.LaRocca N, Kalb R, Scheinberg L, Kendall P. Factors associated with unemployment of patients with multiple sclerosis. J Chronic Dis. 1985;38:203–210. doi: 10.1016/0021-9681(85)90093-1. [DOI] [PubMed] [Google Scholar]
- 23.Lovera J, Bagert B, Smoot KH, Wild K, Frank R, Bogardus K, Oken BS, Whitham RH, Bourdette DN. Correlations of Perceived Deficits Questionnaire of Multiple Sclerosis Quality of Life Inventory with Beck Depression Inventory and neuropsychological tests. J Rehabil Res Dev. 2006;43:73–82. doi: 10.1682/jrrd.2004.09.0118. [DOI] [PubMed] [Google Scholar]
- 24.Marrie RA, Chelune GJ, Miller DM, Cohen JA. Subjective cognitive complaints relate to mild impairment of cognition in multiple sclerosis. Mult Scler. 2005;11:69–75. doi: 10.1191/1352458505ms1110oa. [DOI] [PubMed] [Google Scholar]
- 25.Marrie RA, Cutter G, Tyry T, Hadjimichael O, Campagnolo D, Vollmer T. Changes in the ascertainment of multiple sclerosis. Neurology. 2005;65:1066–1070. doi: 10.1212/01.wnl.0000178891.20579.64. [DOI] [PubMed] [Google Scholar]
- 26.Marrie RA, Cutter G, Tyry T, Vollmer T, Campagnolo D. Does multiple sclerosis-associated disability differ between races? Neurology. 2006;66:1235–1240. doi: 10.1212/01.wnl.0000208505.81912.82. [DOI] [PubMed] [Google Scholar]
- 27.McCabe MP, De Judicibus M. Multiple sclerosis and economic well-being: role of health, age, and duration of illness. J Clin Psychol Med Settings. 2003;10:139–147. [Google Scholar]
- 28.Midgard R, Riise T, Nyland H. Impairment, disability, and handicap in multiple sclerosis. A cross-sectional study in an incident cohort in More and Romsdal County, Norway. J Neurol. 1996;243:337–344. doi: 10.1007/BF00868408. [DOI] [PubMed] [Google Scholar]
- 29.Miller DM, Rudick RA, Cutter G, Baier M, Fischer JS. Clinical significance of the multiple sclerosis functional composite: relationship to patient-reported quality of life. Arch Neurol. 2000;57:1319–1324. doi: 10.1001/archneur.57.9.1319. [DOI] [PubMed] [Google Scholar]
- 30.Mitchell JN. Multiple sclerosis and the prospects for employment. J Soc Occup Med. 1981;31:134–138. doi: 10.1093/occmed/31.4.134. [DOI] [PubMed] [Google Scholar]
- 31.O’Connor RJ, Cano SJ, Ramio i Torrenta L, Thompson AJ, Playford ED. Factors influencing work retention for people with multiple sclerosis: cross-sectional studies using qualitative and quantitative methods. J Neurol. 2005;252:892–896. doi: 10.1007/s00415-005-0765-4. [DOI] [PubMed] [Google Scholar]
- 32.Patricia AF, Usha S. Employment and Disability: Evidence from the 1996 Medical Expenditures Panel Survey. J Occupational Rehabil. 2004;14:1–11. doi: 10.1023/b:joor.0000015007.46881.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Preiningerova J, Hadjimichael O, Vollmer T, Rizzo MA. Validation of patient-reported disease descriptors in the NARCOMS patient registry. International Journal of MS Care. 2003;5:126. (serial online) [Google Scholar]
- 34.Rao SM, Leo GJ, Ellington L, Nauertz T, Bernardin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. II. Impact on employment and social functioning. Neurology. 1991;41:692–696. doi: 10.1212/wnl.41.5.692. (see comments) [DOI] [PubMed] [Google Scholar]
- 35.Rodriguez M, Siva A, Ward J, Stolp-Smith K, O’Brien P, Kurland L. Impairment, disability, and handicap in multiple sclerosis: a population-based study in Olmsted County, Minnesota. Neurology. 1994;44:28–33. doi: 10.1212/wnl.44.1.28. [DOI] [PubMed] [Google Scholar]
- 36.Rozin R, Schiff Y, Kahana E, Soffer D. Vocational status of multiple sclerosis patients in Israel. Arch Phys Med Rehabil. 1975;56:300–304. [PubMed] [Google Scholar]
- 37.Rune M, Trond R, Harald N. Impairment, disability and handicap in multiple sclerosis A cross-sectional study in an incident cohort in Møre and Romsdal County, Norway. J Neurol. 1996;243:337–344. doi: 10.1007/BF00868408. [DOI] [PubMed] [Google Scholar]
- 38.Salomone PR, O’Connell KR. The impact of disability on career development of people with multiple sclerosis. Journal of Career Development. 1988;25(1):65–81. [Google Scholar]
- 39.Schwartz CE, Vollmer T, Lee H. Reliability and validity of two self-report measures of impairment and disability for MS. North American Research Consortium on Multiple Sclerosis Outcomes Study Group. Neurology. 1999;52:63–70. doi: 10.1212/wnl.52.1.63. [DOI] [PubMed] [Google Scholar]
- 40.Smith MM, Arnett PA. Factors related to employment status changes in individuals with multiple sclerosis. Mult Scler. 2005;11:602–609. doi: 10.1191/1352458505ms1204oa. [DOI] [PubMed] [Google Scholar]
- 41.Verdier-Taillefer MH, Sazdovitch V, Borgel F, Cesaro P, Kurtz A, Millet MF, Roullet E, Marteau R. Occupational environment as risk factor for unemployment in multiple sclerosis. Acta Neurol Scand. 1995;92:59–62. doi: 10.1111/j.1600-0404.1995.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 42.Vollmer T, Ni W, Stanton S, Hadjimichael O. The NARCOMS Patient Registry: a resource for investigators. Int J MS Care. 1999 (serial online) [Google Scholar]
- 43.Vollmer TL, Hadjimichael O, Preiningerova J, Ni W, Buenconsejo J. Disability and treatment patterns of multiple sclerosis patients in United States: a comparison of veterans and nonveterans. J Rehabil Res Dev. 2002;39:163–174. [PubMed] [Google Scholar]