Abstract
The Southeastern region of the United States is known as the “Stroke Belt” because of the excess stroke mortality in this region as compared to the rest of the country. However, whether a similar geographic variation in heart failure mortality exists is unknown. Using the CDC WONDER’s publicly-available compressed mortality data files and the 2000 United States population as the standard, we estimated age-adjusted heart failure and stroke mortality rates per 100,000 for individuals of all ages, both sexes and all races during 1979–1998 in the United States, and mapped them at the state level. The age-adjusted heart failure mortality rate for the six contiguous Southeastern states (Alabama, Arkansas, Mississippi, Oklahoma, Louisiana, and Georgia) was 31.0/100,000, which was 69% higher than the national rate of 18.3/100,000. This geographic disparity was similar among African Americans (32.9/100,000 in the Southeast versus 21.7/100,000 nationally) and whites (30.8/100,000 in the Southeast versus 18.1/100,000 nationally). These findings suggest that in addition to the “Stroke Belt”, the Southeastern region of the United States may also be burdened by a “Heart Failure Belt”. To better understand the causes of the excess stroke mortality in the “Stroke Belt”, the National Institutes of Health has funded the REasons for Geographic and Racial Differences in Stroke (REGARDS) study (N=30,239, over half from the Southeastern region), which provide a unique opportunity to study the underlying causes of excess heart failure mortality in the “Heart Failure Belt”.
Keywords: heart failure, mortality, southeastern states
The Southeastern region of the US has the highest stroke mortality rate and is often referred to as the “Stroke Belt” of the country.1, 2 However, whether a similar geographic variation in heart failure mortality exists remains unknown. Several studies have reported that the rate of heart failure hospitalization is the highest in the Southeastern region of the country.3, 4 The purpose of the current study is to examine if heart failure mortality is also the highest in the Southeastern region of the United States.
Methods
We used publicly available compressed mortality data files from the Center for Disease Control and Prevention (CDC) Wide-ranging Online Data for Epidemiologic Research (WONDER) website (http://wonder.cdc.gov/) for the current study. The CDC WONDER contains county-level national mortality data from all 50 states and the District of Columbia but excludes deaths occurring abroad and those of foreign residents occurring in the United States. Data on death were obtained from the death certificates and the causes of death were determined by the conditions listed by physicians as the cause of death on the death certificate. Data on population estimates are based on U.S. Census Bureau estimates at national, state, and county levels, and were available for Census Regions and Divisions.
Death due to heart failure was determined based on International Classification of Diseases, Ninth Revision (ICD-9) codes 428.0, 428.1 and 428.9, and death due to stroke was defined by ICD-9 codes 430–438. Using the 2000 United States population as the standard population, we estimated age-adjusted mortality rates per 100,000 persons for heart failure and stroke in the United States for all ages, both sexes and all races during 1979–1998, and mapped those rates at the state level. We then repeated our estimation of age-adjusted mortality rates for heart failure in the United States separately for African Americans and whites, and mapped those rates at the state level. We further estimated age-adjusted mortality rates for heart failure for all ages, both sexes and all races during 1979–1998 in the six contiguous Southeastern states of Georgia, Alabama, Mississippi, Louisiana, Arkansas and Oklahoma, and mapped those rates at the state level. Finally, we estimated age-adjusted mortality rates for heart failure for all ages, both sexes and all races during 1979–1998 in Alabama, the state with the highest heart failure mortality rate, and mapped those rates at the county level.
Results
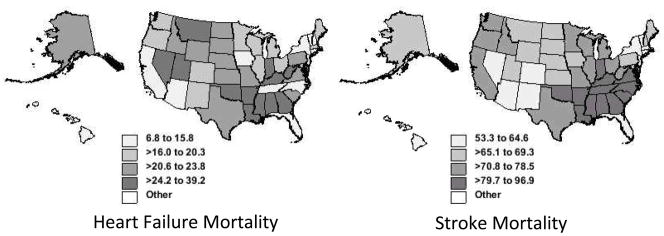
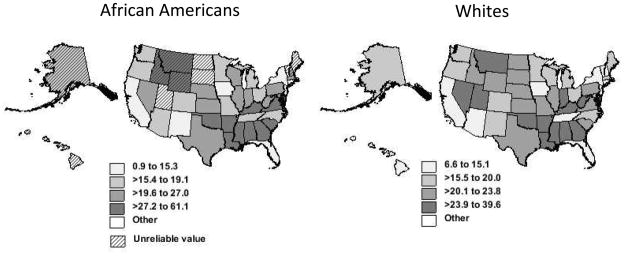
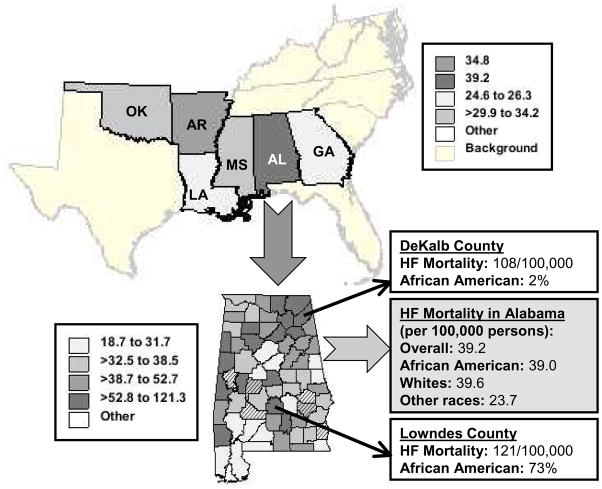
Similar to stroke mortality, heart failure mortality also varied by region, and was the highest in the Southeastern region of the United States (Figure 1). Six of the contiguous Southeastern states were among the nine states with the highest heart failure mortality rates: Alabama (39.2/100,000), Arkansas (34.8/100,000), Mississippi (34.2/100,000), Oklahoma (29.9/100,000), Louisiana (26.3/100,000), and Georgia (24.6/100,000). Compared to the national age-adjusted heart failure mortality rate of 18.3/100,000, the corresponding overall rate for these six Southeastern states was 31.0/100,000, representing an excess 69% heart failure mortality. The regional variation in the age-adjusted heart failure mortality rates was similar for African Americans and whites (Figure 2). Among African Americans, the age-adjusted heart failure mortality rate for the six contiguous Southeastern states was 32.9/100,000, which was 52% higher than the national rate of 21.7/100,000. Among whites, the age-adjusted heart failure mortality rate for the six contiguous Southeastern states was 30.8/100,000, which was 70% higher than the national rate of 18.1/100,000. In Alabama, while one of the two counties with the highest heart failure mortality rate was predominantly white, the other was predominantly African American (Figure 3).
Figure 1.
Age-adjusted rate for mortality (per 100,000 persons) due to heart failure (left panel) and stroke (right panel) in the United States (1979–1998) by states, data for all ages, both sexes and all races
Figure 2.
Age-adjusted rate for mortality (per 100,000 persons) due to heart failure among African Americans (left panel) and whites (right panel) in the United States (1979–1998) by states, data for all ages and both sexes
Figure 3.
Age-adjusted heart failure (HF) mortality rates for all ages from the 6 southeastern US states with the highest mortality rates (1979–1998) and at county levels in Alabama (the state with the highest rate)
Discussion
The findings from the current analysis suggest that there was wide regional variation in heart failure mortality in the United States, with the highest rate in the Southeastern region. This is very similar to the regional variation in stroke mortality that is also the highest in the Southeastern region of the country and often referred to as the “Stroke Belt” of the country. Taken together with the highest heart failure hospitalization in the Southeastern region of the United States,3, 4 the findings of the current study suggest that the Southeastern region may be burdened by a “Heart Failure Belt”.
Although the presence of the Stroke Belt has been long known, little is known about its causes and hypotheses abound. To better understand the regional variations in stroke mortality, the National Institute of Neurological Disorders and Stroke (NINDS) has funded the REasons for Geographic and Racial Differences in Stroke (REGARDS) study.5 Preliminary findings from REGARDS suggest that the incidence of stroke may be higher in the stroke belt region of the country (unpublished data), a finding that was also demonstrated in National Health and Nutrition Examination Survey (NHANES I) Epidemiologic Followup Study (1971–1987),6 this in part explains the higher stroke mortality.7 However, findings from REGARDS indicate that hypertension awareness and treatment in the Stroke Belt may not be substantially different from those in the rest of the country suggesting that the causes of an increased incidence of stroke in Stroke Belt may be complex and may not be fully explained by regional variation in traditional risk factors.8 The role of non-traditional risk factors and whether there is regional variation in stroke case fatality are currently being studied in REGARDS.
To the best of our knowledge, the presence of a possible Heart Failure Belt in the Southeastern United States is largely unknown. Far lesser is known about the potential causes of the excess heart failure mortality in the Southeastern United States. Large prospective national population studies with strong representation from the Southeastern United States are needed to understand the underlying causes of excess heart failure mortality in this region. REGARDS has enrolled 30,239 participants 45 years or older from the 48 contiguous states between January 2003 and October 2007.6 Because over half of the REGARDS participants are from the Southeastern region of the United States and because there is a robust similarity between regional variations in stroke and heart failure mortality, REGARDS provides a unique opportunity to study the causes of excess heart failure mortality in the Southeastern United States .
Several limitations of our study need to be acknowledged. Because sudden cardiac death and death from progressive HF are the two major modes of death in heart failure, misclassification and underestimation of heart failure mortality rate are possible. Also, the analysis is based on mortality due to heart failure as a primary cause and thus underestimates the total burden of death in all heart failure patients. However, these are likely to be random for all regions of the country and may not confound the regional differences observed in our study. In conclusion, findings from the current analysis demonstrate a profound regional disparity in heart failure mortality in the United States and provide evidence for the existence of a Heart Failure Belt, similar to the Stroke Belt, in the Southeastern region of the United States, where heart failure mortality is the highest in the nation.
Acknowledgments
Funding/Support: Dr. Ahmed is supported by the National Institutes of Health through grants (R01-HL085561 and R01-HL097047) from the National Heart, Lung, and Blood Institute (NHLBI) and a generous gift from Ms. Jean B. Morris of Birmingham, Alabama
Footnotes
Conflict of Interest Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Borhani NO. Changes and Geographic Distribution of Mortality from Cerebrovascular Disease. Am J Public Health Nations Health. 1965;55:673–681. doi: 10.2105/ajph.55.5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howard G. Why do we have a stroke belt in the southeastern United States? A review of unlikely and uninvestigated potential causes. Am J Med Sci. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Zhang W, Watanabe-Galloway S. Ten-year secular trends for congestive heart failure hospitalizations: an analysis of regional differences in the United States. Congest Heart Fail. 2008;14:266–271. doi: 10.1111/j.1751-7133.2008.00009.x. [DOI] [PubMed] [Google Scholar]
- 4.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 5.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 6.Gillum RF, Ingram DD. Relation between residence in the southeast region of the United States and stroke incidence. The NHANES I Epidemiologic Followup Study. Am J Epidemiol. 1996;144:665–73. doi: 10.1093/oxfordjournals.aje.a008979. [DOI] [PubMed] [Google Scholar]
- 7.Cushman M, Cantrell RA, McClure LA, Howard G, Prineas RJ, Moy CS, Temple EM, Howard VJ. Estimated 10-year stroke risk by region and race in the United States: geographic and racial differences in stroke risk. Ann Neurol. 2008;64:507–513. doi: 10.1002/ana.21493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howard G, Prineas R, Moy C, Cushman M, Kellum M, Temple E, Graham A, Howard V. Racial and geographic differences in awareness, treatment, and control of hypertension: the REasons for Geographic And Racial Differences in Stroke study. Stroke. 2006;37:1171–1178. doi: 10.1161/01.STR.0000217222.09978.ce. [DOI] [PubMed] [Google Scholar]