Abstract
Objective
Little is known about racial/ethnic differences in the receipt of treatment for major depression among adolescents. This study examines differences in mental health service use among non-Hispanic white, black, Hispanic, and Asian adolescents who experienced an episode of major depression.
Method
Five years of data (2004–2008) were pooled from the National Survey on Drug Use and Health to derive a nationally representative sample of 7,704 adolescents (age 12–17) diagnosed with major depression in the past year. Racial/ethnic differences were estimated with weighted probit regressions across several measures of mental health service use controlling for demographics and health status. Additional models assessed whether family income and health insurance status accounted for these differences.
Results
The adjusted percentages of blacks (32%), Hispanics (31%), and Asians (19%) who received any treatment for major depression were significantly lower than among non-Hispanic whites (40%; p<0.001). Black, Hispanic, and Asian adolescents were also significantly less likely than non-Hispanic whites to receive prescription medication for major depression, to receive treatment for major depression from a mental health specialist or medical provider, and to receive any mental health treatment in an outpatient setting (p<0.01). These differences persisted after adjusting for family income and insurance status.
Conclusion
Results indicated low rates of mental health treatment for major depression among all adolescents. Improving access to mental health care for adolescents will also require attention to racial/ethnic subgroups at highest risk for nonreceipt of services.
Keywords: Race, ethnicity, mental health services, depression
Introduction
The onset of major depression is common during adolescence1 and associated with substantial short and long-term health, developmental, and social consequences.2, 3 Although highly effective treatments are available,4 major depression commonly goes untreated.5 It is therefore a central clinical and public health priority to identify the groups most at risk for nonreceipt of care.
In adults, one of the most important predictors of failure to receive care for depression is race/ethnicity – with members of racial/ethnic minority groups being 30% (African Americans) to 50% (Asians) less likely to receive any mental health treatment compared to non-Latino whites.6 However, less is known about racial/ethnic differences in the receipt of treatment for depression among adolescents. Although the existing literature has indicated that racial/ethnic minorities may be less likely to receive services than non-Hispanic whites,7–10 these studies have been limited by sample size constraints for assessing differences in service use across multiple racial/ethnic groups, lack of population-based survey measures to identify those with clinical depression, and/or little information about the treatment that was received for depression. Thus, further research is needed with samples that are nationally representative and with sufficient power to detect differences in service use across multiple racial/ethnic groups identified with clinical depression.
This study examines differences in mental health treatment across four racial/ethnic groups of adolescents with major depression (i.e. non-Hispanic whites, blacks, Hispanics, and Asians) using a large, nationally representative sample. In addition to having sufficient statistical power to make comparisons across these four groups, this study adds to existing literature by characterizing racial/ethnic differences in service use with multiple outcome measures including the receipt of any treatment for major depression, the use of prescription medication for major depression, the receipt of treatment for major depression across provider types, and the use of mental health services across inpatient, outpatient, and school settings.
Method
Data
Five years of data (2004–2008) are pooled from the National Survey of Drug Use and Health (NSDUH), an annual, nationally-representative, cross-sectional survey that is sponsored by the Substance Abuse and Mental Health Services Administration. NSDUH samples non-institutionalized individuals ages 12 and older in the U.S. civilian population from all 50 states and the District of Columbia in multiple stages. The survey was administered in English and Spanish. Our study uses data from the adolescent component (ages 12–17), which includes a series of questions to assess major depressive episodes (MDE) experienced in the previous year, information about mental health services utilization, health insurance status, and socio-demographic characteristics. Given the lack of private identifiers in this publically available dataset, the Emory IRB determined that the study did not meet the criteria for "Human Subjects Research" and that review was not necessary.
Study Sample
Our analytic sample is derived from the sub-sample of adolescents who experienced an episode of MDE in the previous year. Past year MDE was assessed with an adolescent depression module administered using computer-assisted interviewing (CAI) instrumentation. This module was adapted from the depression section of the National Comorbidity Survey-Adolescent,11 which is based on a modified version of the World Health Organization Composite International Diagnostic Interview-Short Form (CIDI-SF).12 For MDE, research has reported good psychometric concordance between the CIDI-SF and the full CIDI.12 Furthermore, research has indicated a high concordance between the full CIDI and independent clinical diagnoses in the adolescent population13 as well as in a U.S. sample of English- and Spanish-speaking Latinos.14
Of the 90,855 adolescents who participated in the NSDUH between 2004 and 2008, 7,704 (8.5%) experienced MDE in the past year. When examining the prevalence of MDE (unweighted) by race/ethnicity, 8.7% of non-Hispanic whites experienced MDE in the past year, compared to 8.4% of Hispanics, 7.4% of Asians, and 7.3% of blacks.
Measures
Treatment for Major Depression
After answering questions about MDE symptoms, adolescents were asked if in the past 12 months they talked to a medical doctor or other professional about these problems or if they received prescription medication for these problems. Two dichotomous measures assessed whether the adolescent received the following in the past year: (1) any MDE treatment from a mental health professional and/or medical professional and (2) any prescription medication for MDE. Two additional indicators assessed whether the adolescent received MDE treatment from: (1) a mental health professional (i.e. psychologist, psychiatrist, social worker, counselor, and/or other mental health professional), and a (2) a medical professional (i.e. general practitioner, family doctor, other medical doctor, nurse, occupational therapist, and/or other health professional).
Receipt of Mental Health Treatment Across Settings
NSDUH also provides information about past year mental health care use across settings irrespective of the specific mental health problem for which the adolescent sought treatment. Three indicators assess whether the adolescent: (1) had an inpatient stay for a mental health problem in a hospital and/or a residential treatment center, (2) received any outpatient treatment for a mental health problem at a clinic, day treatment center, therapist’s office, physician’s office, and/or home residence, and (3) received counseling from an individual (e.g. teacher and/or counselor) at school for a mental health problem. An additional measure was created for the total number of mental health outpatient visits during the past year and analyzed in supplemental analyses.
Race/Ethnicity
Race/ethnicity was reported as five mutually exclusive categories: non-Hispanic white, black, Hispanic, Asian, and other race/ethnicity. Other race/ethnicity comprises non-Hispanics who reported more than one racial background as well as groups with cell sizes that were too small for statistical analyses (e.g. Native Americans).
Socio-demographic and Health Status Measures
Prior research has indicated that age, gender, family status, income, and health insurance are important determinants of mental health care use among youth.15–17 These socio-demographic characteristics were assessed with a continuous measure of age in years (12–17), an indicator for females, an indicator for family status identifying adolescents who live with two parents versus those who do not, a categorical measure of family income (<$20K, $20K–$50K, $50K–$75K, >$75K), and a categorical measure of insurance status (any private insurance, public coverage, no insurance, and insurance status unknown). Lastly, although school enrollment may differ across racial/ethnic groups and facilitate MH service use, this measure is not included because 98% of the sample with MDE attends school.
To adjust for differences in underlying mental health status, analyses included an indicator for whether adolescents reported that their depressive symptoms resulted in severe or very severe impairment (versus no, mild, or moderate impairment) in at least one of four life domains: chores at home, school or work, family relationships, or social life. Additionally, because alcohol and drug use are correlated with depression,18 two indicators measured alcohol abuse/dependence and illicit drug abuse/dependence based on a series of questions designed to measure substance abuse and dependence according to DSM-IV criteria.11 Lastly, general health status, which is correlated with depression,19 was assessed with a self-reported measure of fair or poor health status (versus good, very good, or excellent).
Analysis
We estimated pooled weighted probit regressions and negative binomial regression models with the “svy” procedure in Stata to account for the complex survey design elements in NSDUH.20 Sampling weights adjusted for differential probabilities of sampling selection, non-response bias, and non-coverage bias. All models included year fixed effects. Risk differences for each minority racial/ethnic group were estimated at the weighted mean values of the control variables. The risk differences can be interpreted as the predicted difference in the percentage of adolescents in a racial/ethnic minority group with a positive value on the outcome variable compared to non-Hispanic whites, holding the covariates constant at their mean value. Individuals with missing values on study variables are excluded to yield two primary analytic samples: 7,618 adolescents for models examining racial/ethnic differences in measures of MDE treatment and 7,598 adolescents for models examining differences in mental health service use across settings.
According to the Institute of Medicine’s (IOM) report Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare, a health care disparity is defined as, “differences in the quality of healthcare that are not due to access-related factors or clinical needs, preferences, and appropriateness of intervention.”21 However, previous studies implementing this definition to examine mental health care disparities among the adult population have contended that “access-related factors” such as socioeconomic status (SES) and health insurance status should not be accounted for when estimating the total disparity in service use, but may be included in subsequent models to assess the degree to which they mediate the disparity.6, 22 Although we do not explicitly examine differences in mental health care quality, we estimate our models in a manner that is consistent with this general approach by first adjusting for differences in demographics (i.e. age, gender, family status) and mental health status and further adjusting for family income and insurance status in a subsequent model.
Additional analyses assessed the robustness of findings when including measures of population density (as a proxy for access to medical and mental health professionals)23 and language of interview (i.e. Spanish vs. English). Although all five years of NSDUH data contain a measure of population density, these measures differ across years; consequently, the creation of a single measure for use in the pooled data must be interpreted with caution.
Results
Among adolescents with MDE, only 38% received any MDE treatment, 17% took prescription medication for MDE, 30% received MDE treatment from a mental health specialist, and 11% received MDE treatment from a medical provider (Table 1). When examining measures of past year mental health treatment across settings, 5% had an inpatient stay, 36% had an outpatient visit, and 25% received counseling in a school setting. When comparing these measures across racial/ethnic groups using Wald tests, results indicate that Blacks, Hispanics, and Asians are significantly less likely than non-Hispanic Whites to receive any MDE treatment (p<0.01), use prescription medication for MDE (p<0.001), receive MDE treatment from a mental health specialist (p<0.01), receive MDE treatment from a medical professional (p<0.001), and have a mental health visit in an outpatient setting (p<0.001). Blacks, Hispanics, and Asians also have lower family incomes (p<0.001) and are less likely to have private health insurance (p<0.05) than non-Hispanic Whites.
Table 1.
Weighted descriptive statistics for pooled sample of U.S. adolescents with past year major depression (2004–2008)
| Total (N=7,618) |
Non-Hisp. Whites (N=4,758) |
Blacks (N=898) |
Hispanics (N=1,230) |
Asians (N=193) |
Other (N=539) |
|
|---|---|---|---|---|---|---|
| %/ Mean (SE) |
%/ Mean (SE) |
%/ Mean (SE) |
%/ Mean (SE) |
%/ Mean (SE) |
%/ Mean (SE) |
|
| Outcome Variables | ||||||
| Treatment for Major Depression | ||||||
| Any treatment | 38.1 | 41.3 | 33.9*** | 32.7*** | 23.2** | 39.3 |
| Any prescription medication | 16.6 | 21.2 | 7.1*** | 9.5*** | 3.6*** | 17.6 |
| Any treatment from MH professional | 29.7 | 32.4 | 26.1** | 25.7*** | 14.1*** | 31.1 |
| Any treatment from medical professional | 11.4 | 13.4 | 7.3*** | 8.6*** | 2.3*** | 12.9 |
| Past Year MH Treatment | ||||||
| Any Inpatient Stay a | 5.3 | 5.1 | 6.1 | 4.4 | 6.3 | 9.9 † |
| Any Outpatient Visita | 36.2 | 40.4 | 28.1*** | 29.2*** | 21.6*** | 40.7 |
| Number of Outpatient Visits for those with ≤1 visitb | 14.2(0.5) | 14.8(0.6) | 12.6(1.4) | 11.7(1.1)* | 13.5(4.4) | 17.0(2.4) |
| Any Counseling in Schoola | 24.6 | 25.4 | 26.7 | 21.6* | 16.4** | 25.6 |
| Explanatory Variables | ||||||
| Demographics | ||||||
| Age | 15.1(0.02) | 15.1(0.03) | 14.9(0.1)** | 15.1(0.1) | 15.0(0.1) | 14.9(0.1)** |
| Female | 72.5 | 72.4 | 72.3 | 73.4 | 72.0 | 71.0 |
| Lives with two parents | 65.3 | 69.3 | 41.7*** | 66.1 | 84.5*** | 54.1** |
| Need for Mental Health Services | ||||||
| Severe MDE Impairment | 69.8 | 71.5 | 65.9** | 67.6 | 61.0* | 73.9 |
| Illicit Drug Abuse/Dependence | 13.8 | 15.0 | 10.1** | 13.3 | 5.8*** | 15.8 |
| Alcohol Abuse/Dependence | 13.1 | 14.6 | 6.9*** | 13.1 | 4.8*** | 16.6 |
| Fair/Poor Health | 6.5 | 6.0 | 7.2 | 7.1 | 7.2 | 8.4 |
| Family Income | ||||||
| Income <20K | 16.6 | 10.4 | 36.0*** | 23.6*** | 19.0 | 19.4** |
| Income 20–50K | 35.1 | 31.2 | 39.5*** | 44.4*** | 41.9 | 36.5 |
| Income 50–75K | 18.4 | 20.4 | 12.6*** | 14.7*** | 19.2 | 21.9 |
| Income >75K | 29.9 | 38.0 | 11.9*** | 17.3*** | 19.8*** | 22.2*** |
| Insurance Status | ||||||
| Private Insurance | 65.9 | 75.7 | 46.6*** | 47.2*** | 60.9* | 55.4*** |
| Public Insurance | 24.8 | 17.2 | 44.9*** | 36.2*** | 23.3 | 34.7*** |
| Uninsured | 7.5 | 5.7 | 5.9 | 15.6*** | 7.2 | 6.0 |
| Insurance Status Unknown | 1.8 | 1.4 | 2.6 | 1.0 | 8.6 | 3.9† |
Note: P values reflect results from Wald Tests to compare measures between each racial/ethnic minority group and rnon-Hispanic Whites. MDE=Major Depressive Episode; MH = Mental Health.
Total sample size N=7,598.
Total sample size N=2,555.
p<0.05,
p<0.01,
p<0.001
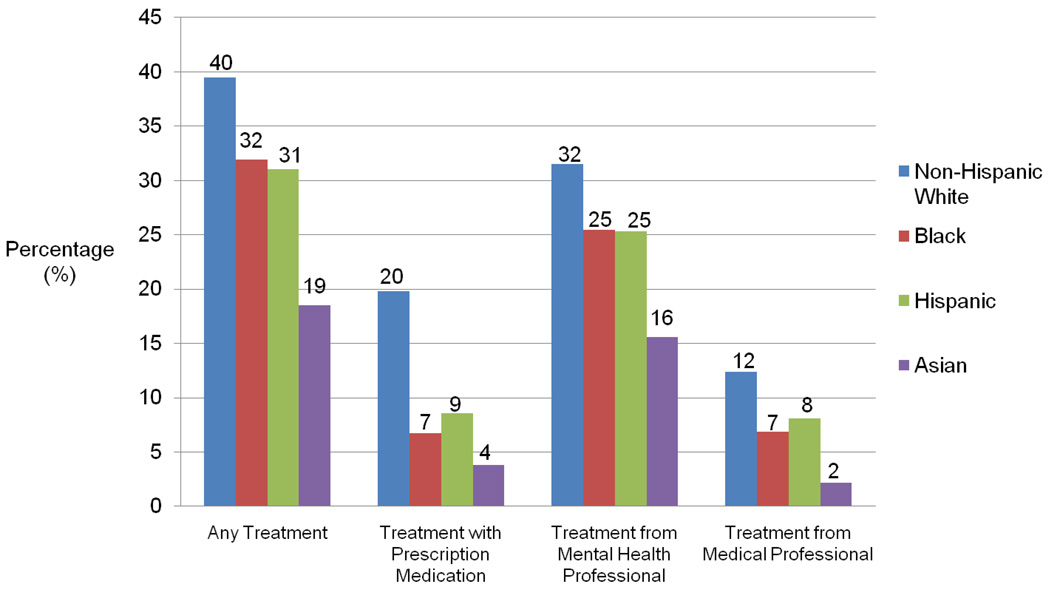
Controlling for demographics and health status (Table 2, Model 1), the absolute percentage of racial/ethnic minorities who received any MDE treatment is between 7.6 (Blacks: 95% CI=−12.3%, −3.0%) and 21.0 percentage points lower (Asians: 95% CI= −29.1%, −12.9%) than among non-Hispanic Whites. In other words, the adjusted percentages of those who received any MDE treatment are 31.9% for blacks, 31.0% for Hispanics, and 18.5% for Asians, compared to 39.5% for non-Hispanic whites. These adjusted percentages for each racial/ethnic group are depicted graphically in Figure 1, where the height difference between the bars corresponds to the adjusted risk differences estimated in this model. After including family income and insurance status, these risk differences are slightly reduced for each group but remain statistically significant (Table 2, Model 2).
Table 2.
Racial/ethnic differences in the receipt of any treatment and prescription medication for major depression among U.S. adolescents
| Any MDE Treatment | Received Prescription Medication for MDEa |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | |
| Blackb | −7.6 | (−12.3, −3.0) | −7.2 | (−11.8, −2.5) | −13.2 | (−15.8, −10.5) | −12.8 | (−15.5, −10.1) |
| Hispanicb | −8.5 | (−12.6, −4.4) | −7.6 | (−11.8, −3.5) | −11.2 | (−13.9, −8.6) | −10.8 | (−13.6, −8.0) |
| Asianb | −21.0 | (−29.1, −12.9) | −19.8 | (−27.9, −11.8) | −16.0 | (−19.3, −12.7) | −15.3 | (−18.8, −11.8) |
| Other Raceb | −2.6 | (−9.6, 4.4) | −2.4 | (−9.4, 4.6) | −3.7 | (−9.3, 1.9) | −3.3 | (−9.0, 2.4) |
| Age (12–17) | 0.6 | (−0.5, 1.7) | 0.6 | (−0.5, 1.7) | 1.9 | (1.1, 2.8) | 1.9 | (1.1, 2.8) |
| Female | 2.6 | (−0.6, 5.9) | 2.7 | (−0.6, 5.9) | −1.8 | (−4.3, 0.6) | −1.8 | (−4.2, 0.6) |
| Lives w/ 2 parents (1=yes) | −6.6 | (−10.0, −3.2) | −7.8 | (−11.3, −4.3) | −2.6 | (−5.4, 0.2) | −3.6 | (−6.6, −0.6) |
| Severe MDE Impairment (1=yes) | 17.2 | (14.0, 20.3) | 17.0 | (13.9, 20.1) | 12.0 | (9.3, 14.7) | 11.8 | (9.1, 14.5) |
| Illicit Drug Abuse/Dependence (1=yes) | 7.9 | (2.6, 13.2) | 7.8 | (2.5, 13.1) | 10.9 | (6.2, 15.6) | 10.7 | (6.0, 15.3) |
| Alcohol Abuse/ Dependence (1=yes) | 6.6 | (1.0, 12.2) | 6.5 | (0.9, 12.1) | 1.3 | (−3.2, 5.7) | 1.1 | (−3.2, 5.5) |
| Fair/Poor Health (1=yes) | 8.3 | (2.5, 14.1) | 8.6 | (2.8, 14.4) | 7.5 | (2.9, 12.1) | 7.9 | (3.4, 12.4) |
| Income 20–50Kc | 1.6 | (−3.8, 7.1) | 0.4 | (−3.4, 4.2) | ||||
| Income 50–75Kc | 4.0 | (−1.7, 9.7) | 2.4 | (−1.8, 6.6) | ||||
| Income >75Kc | 5.6 | (−0.8, 12.1) | 4.9 | (0.4, 9.4) | ||||
| Private Insuranced | 6.7 | (0.1, 13.3) | 1.7 | (−3.5, 7.0) | ||||
| Public Insuranced | 10.4 | (3.3, 17.5) | 4.6 | (−1.7, 11.0) | ||||
| Insurance Unknownd | −4.1 | (−19.3, 11.2) | −11.2 | (−19.6, −2.8) | ||||
Note: N=7,618; All models include year fixed effects. MDE = Major Depressive Episode;
Risk differences for racial/ethnic categories estimated at the mean value of covariates Omitted Reference Categories:
Non-Hispanic Whites;
Family income <20K;
Uninsured
Figure 1.
Adjusted percentage of U.S. adolescents who received treatment for major depression by race/ethnicity. Note: N=7,618. Results from multivariate probit models adjusting for age, gender, family status, depression-related impairment, substance abuse/dependence, and self-rated health
Results examining racial/ethnic differences in the use of prescription medication yield a similar pattern (Table 2, Model 3). Among racial/ethnic minorities, the absolute percentage of adolescents who use prescription medication for MDE is between 11.2 (Hispanics: 95% CI=−13.9%, −8.6%) and 16.0 percentage points lower (Asians: 95% CI= −19.3%, −12.7%) relative to non-Hispanic Whites. Consequently, the adjusted percentages of adolescents who received prescription medication for MDE are 19.8% for non-Hispanic whites, 6.7% for blacks, 8.6% for Hispanics, and 3.8% for Asians (Figure 1). As before, the inclusion of family income and insurance status slightly accounts for these differences, but the findings remain statistically significant (Model 4).
Blacks, Hispanics, and Asians are also significantly less likely than non-Hispanic whites to receive MDE treatment from a mental health professional or a medical provider (Table 3: Model 1, Model 3). Once again, the risk differences are largest for Asians. The adjusted percentage of non-Hispanic whites with MDE who received treatment from a mental health professional and a medical provider are 31.5% and 12.4%, respectively, compared to only 15.6% (RD=−16.0, 95% CI=−23.2%,−8.7%) and 2.2% (RD=−10.2, 95% CI=−12.8%,−7.5%) of Asians with MDE (Figure 1). Although the inclusion of family income and insurance status slightly reduces these differences, they remain statistically significant (Model 2, Model 4).
Table 3.
Racial/ethnic differences in the receipt of treatment for major depression across provider types among U.S. adolescents
| Saw/Talked to a Mental Health Professional for MDE |
Saw/Talked to a Medical Professional for MDE |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | |
| Blackb | −6.0 | (−10.3, −1.8) | −5.0 | (−9.2, −0.7) | −5.4 | (−7.5, −3.4) | −5.7 | (−7.6, −3.8) |
| Hispanicb | −6.2 | (−10.0, −2.5) | −4.9 | (−8.8, −1.0) | −4.3 | (−6.9, −1.7) | −4.3 | (−7.0, −1.5) |
| Asianb | −16.0 | (−23.2, −8.7) | −14.6 | (−21.7, −7.5) | −10.2 | (−12.8, −7.5) | −10.1 | (−12.7, −7.5) |
| Other Raceb | −2.3 | (−8.4, 3.8) | −1.8 | (−7.8, 4.2) | −0.4 | (−5.1, 4.2) | −0.8 | (−5.4, 3.7) |
| Age (12–17) | 0.5 | (−0.5, 1.5) | 0.5 | (−0.5, 1.5) | 1.4 | (0.8, 2.0) | 1.5 | (0.9, 2.1) |
| Female | 5.2 | (2.0, 8.3) | 5.3 | (2.1, 8.4) | 2.6 | (0.5, 4.8) | 2.6 | (0.4, 4.7) |
| Lives w/ 2 parents (1=yes) | −5.1 | (−8.4, −1.7) | −6.8 | (−10.3, −3.2) | −1.1 | (−3.0, 0.8) | −1.2 | (−3.4, 1.0) |
| Severe MDE Impairment (1=yes) | 16.2 | (13.5, 19.0) | 16.1 | (13.4, 18.7) | 8.9 | (6.3, 11.5) | 8.8 | (6.3, 11.4) |
| Illicit Drug Abuse/Dependence (1=yes) | 3.6 | (−1.0, 8.2) | 3.6 | (−0.9, 8.1) | 3.7 | (0.2, 7.2) | 3.6 | (0.2, 7.1) |
| Alcohol Abuse/ Dependence (1=yes) | 6.4 | (1.4, 11.3) | 6.2 | (1.3, 11.1) | −0.5 | (−3.5, 2.5) | −0.4 | (−3.5, 2.6) |
| Fair/Poor Health (1=yes) | 7.0 | (2.2, 11.9) | 7.3 | (2.5, 12.2) | 3.1 | (−0.9, 7.2) | 3.1 | (−1.0, 7.2) |
| Income 20–50Kc | 3.2 | (−2.1, 8.5) | −1.0 | (−4.4, 2.4) | ||||
| Income 50–75Kc | 5.7 | (−0.3, 11.7) | 1.8 | (−2.0, 5.7) | ||||
| Income >75Kc | 6.7 | (0.5, 12.9) | 0.9 | (−3.2, 4.9) | ||||
| Private Insuranced | 7.2 | (0.7, 13.6) | 4.9 | (1.2, 8.7) | ||||
| Public Insuranced | 9.1 | (2.4, 15.7) | 9.6 | (4.0, 15.3) | ||||
| Insurance Unknownd | −1.5 | (−15.8, 12.9) | 5.6 | (−6.2, 17.3) | ||||
Note: N=7,618; All models include year fixed effects. MDE=Major Depressive Episode;
Risk differences for racial/ethnic categories estimated at the mean value of covariates Omitted Reference Categories:
Non-Hispanic Whites;
Family income <20K;
Uninsured
Results examining racial/ethnic differences in past year mental health treatment across settings among adolescents with MDE, irrespective of the problem that was treated, are presented in Table 4. Although there are no racial/ethnic differences in the likelihood of having an inpatient stay, there are significant differences in the likelihood of having an outpatient visit and receiving counseling in a school setting. Findings from Model 3 indicate that 39.7% (model based prediction not shown) of non-Hispanic whites received an outpatient mental health visit during the year, compared to only 27.9% of blacks (RD=−11.7%, 95% CI=−15.8%, −7.6%), 28.7% of Hispanics (RD=−11.0%, 95% CI=−14.9%,−7.0%), and 23.1% of Asians (RD=−16.5%, 95% CI=−25.5%,−7.5%). These differences are slightly reduced, but remain significant, after accounting for family income and insurance status (Model 4). Lastly, results from Model 5 show that the percentage of Hispanics (RD= −3.7%; 95% CI= −7.1%, −0.2%) and Asians (RD= −7.6%; 95% CI= −13.7%, −1.5%) who received counseling in a school setting is significantly lower than among non-Hispanic whites (24.5%; Model based prediction not shown).
Table 4.
Racial/ethnic differences in the receipt of past-year mental health treatment across settings among U.S. adolescents with major depression
| Any Inpatient Visit for Mental Health Problem |
Any Outpatient Visit for Mental Health Problem |
Any Counseling in School for Mental Health Problem |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |||||||
| RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | RD(%)a | 95% CI | |
| Blackb | 0.8 | (−1.3, 3.0) | 0.0 | (−2.0, 2.0) | −11.7 | (−15.8,−7.6) | −9.7 | (−13.8, −5.7) | 1.7 | (−2.3, 5.6) | 1.4 | (−2.6, 5.5) |
| Hispanicb | −0.4 | (−2.2, 1.4) | −0.9 | (−2.4, 0.7) | −11.0 | (−14.9, −7.0) | −8.8 | (−13.2, −4.5) | −3.7 | (−7.1, −0.2) | −4.4 | (−7.8, −0.9) |
| Asianb | 3.1 | (−3.0, 9.2) | 3.1 | (−2.7, 8.8) | −16.5 | (−25.5,−7.5) | −14.5 | (−23.8, −5.2) | −7.6 | (−13.7, −1.5) | −7.7 | (−13.8, −1.7) |
| Other Raceb | 3.4 | (−0.3, 7.1) | 2.8 | (−0.7, 6.3) | −0.9 | (−8.2, 6.5) | 0.2 | (−7.0, 7.4) | −0.8 | (−6.5, 4.8) | −1.0 | (−6.5, 4.5) |
| Age (12–17) | −0.4 | (−0.7, 0.0) | −0.3 | (−0.7, 0.1) | −0.4 | (−1.4, 0.6) | −0.5 | (−1.5, 0.5) | −2.5 | (−3.4, −1.7) | −2.5 | (−3.4, −1.7) |
| Female | 0.4 | (−0.7, 1.5) | 0.4 | (−0.8, 1.5) | 6.6 | (3.7, 9.6) | 6.7 | (3.8, 9.7) | 7.8 | (5.3, 10.3) | 7.9 | (5.3, 10.4) |
| Lives w/ 2 parents (1=yes) | −2.1 | (−3.4, −0.9) | −1.6 | (−3.1, −0.2) | −2.2 | (−5.7, 1.3) | −5.0 | (−8.7, −1.4) | −0.9 | (−3.3, 1.6) | −0.4 | (−3.2, 2.5) |
| Severe MDE Impairment (1=yes) | 3.5 | (2.1, 5.0) | 3.5 | (2.0, 5.1) | 18.5 | (14.8, 22.2) | 18.3 | (14.7, 22.0) | 12.2 | (9.4, 15.1) | 12.4 | (9.5, 15.2) |
| Illicit Drug Abuse/ Dependence (1=yes) | 3.7 | (1.5, 5.8) | 3.7 | (1.5, 5.8) | 12.6 | (7.7, 17.5) | 12.6 | (7.8, 17.5) | 4.2 | (−0.5, 8.9) | 4.2 | (−0.5, 8.9) |
| Alcohol Abuse/ Dependence (1=yes) | 2.7 | (0.7, 4.6) | 2.8 | (0.8, 4.7) | 3.7 | (−1.1, 8.5) | 3.4 | (−1.3, 8.1) | 0.7 | (−3.7, 5.2) | 0.8 | (−3.7, 5.3) |
| Fair/Poor Health (1=yes) | 2.1 | (0.1, 4.0) | 2.0 | (0.1, 4.0) | 9.3 | (2.4, 16.1) | 9.9 | (2.9, 16.9) | 6.4 | (2.2, 10.7) | 6.4 | (2.1, 10.8) |
| Income 20–50Kc | −0.7 | (−2.3, 0.8) | 3.0 | (−2.3, 8.3) | 0.9 | (−3.4, 5.2) | ||||||
| Income 50–75Kc | −1.2 | (−2.9, 0.6) | 6.9 | (0.9, 12.9) | 0.0 | (−4.8, 4.8) | ||||||
| Income >75Kc | −1.0 | (−3.0, 1.0) | 9.4 | (3.2, 15.7) | −0.8 | (−5.9, 4.3) | ||||||
| Private Insuranced | 2.2 | (0.5, 3.9) | 5.0 | (−2.2, 12.2) | −4.1 | (−10.3, 2.0) | ||||||
| Public Insuranced | 5.1 | (2.2, 8.0) | 4.3 | (−1.9, 10.5) | −3.5 | (−8.7, 1.7) | ||||||
| Insurance Unknownd | −3.3 | (−4.9, −1.7) | −2.2 | (−16.8, 12.4) | −6.9 | (−14.7, 0.9) | ||||||
Note: N=7,598; All models include year fixed effects. MDE = Major Depressive Episode.
Risk differences for racial/ethnic categories estimated at the mean value of covariates. Omitted Reference Categories:
Non-Hispanic Whites;
Family income <20K;
Uninsured
Supplemental analyses further explored racial/ethnic differences in the number of outpatient visits among those who received any outpatient treatment. Among adolescents who received any outpatient visit, results from a negative binomial regression model indicated that Hispanics have approximately 2.8 fewer visits per year (95% CI = −5.0, −0.6) than non-Hispanic whites, who have approximately 13.6 visits per year. This difference was slightly reduced to 2.5 fewer visits among Hispanics after adjusting for family income and insurance status. Blacks and Asians, however, did not differ significantly from non-Hispanic whites in their number of outpatient visits. Lastly, supplemental models that also included language of interview and population density were virtually unchanged across all outcome measures.
Discussion
Findings from this nationally-representative sample revealed high rates of unmet need for mental health treatment among all adolescents with MDE and sizeable racial/ethnic differences in service use before and after adjusting for demographics and health status. The adjusted percentage of non-Hispanic whites who received any MDE treatment was 40%, compared to 32% among blacks, 31% among Hispanics, and 19% among Asians. Black, Hispanic, and Asian adolescents were also significantly less likely than non-Hispanic whites to receive MDE treatment from mental health professionals, to receive MDE treatment from medical providers, and to have any mental health outpatient visits, with Asians exhibiting the lowest rate of service use on each measure.
When examining racial/ethnic differences in the receipt of mental health outpatient treatment, it is notable that although black, Hispanic, and Asian adolescents were significantly less likely than non-Hispanic whites to receive any outpatient services, only Hispanics had significantly fewer outpatient visits than non-Hispanic whites among those who received services. This pattern of findings highlights the importance of implementing programs to address the barriers that exist to entering the mental health care treatment system for racial/ethnic minorities. Research has demonstrated that mental health care quality improvement programs in primary care settings may improve care among youth with depression, but may also have the benefit of reducing disparities in care for vulnerable racial/ethnic subpopulations.24
The adjustment for socioeconomic status and health insurance status accounts for only a small portion of the estimated differences in MDE treatment measures and outpatient utilization across racial/ethnic groups. Consequently, our results suggest that other factors are predominantly driving these differences. While stigma likely plays a large role in the low rates of service use among all adolescents,25, 26 it may also account for the differences in service utilization across racial/ethnic groups27 – especially for Asians.28, 29 In many Asian cultures, seeking help for problems outside of the family is a source of shame.30 Navigational barriers such as limited English proficiency could also explain a portion of the lower rates of service use among racial/ethnic minorities, especially among Hispanics and Asians.31 Even though supplemental analyses adjusting for language of interview (English versus Spanish) did not account for any of the difference in service use observed for Hispanic adolescents, it is possible that unmeasured differences in the English proficiency of the parents could account for part of the observed differences in service utilization.
Unlike treatment in outpatient settings, we did not find any significant racial/ethnic differences in the receipt of inpatient treatment. It may be that there is less discretion on the part of both patients and providers in the decision to pursue inpatient treatment once a mental health condition reaches the severity and acuity to require hospitalization. This finding is consistent with research documenting that disparities are likely to be particularly prominent under conditions of higher clinical uncertainty.32
The American Academy of Child and Adolescent Psychiatry (AACAP) recommends that antidepressants should be considered for adolescents who have severe, psychotherapy-resistant depression.4 More than 20% of non-Hispanic white adolescents reported using prescription medication for major depression, compared to 4% to 9% of Asians, blacks, and Hispanics. Because NSDUH does not provide sufficient detail to determine whether the use of prescription medication was consistent with AACAP guidelines for each individual, it is unclear whether these patterns are indicative of worse access to treatment by minorities, overutilization of medication by non-Hispanic whites, or both. However, racial/ethnic differences remained significant in supplemental analyses in which separate regressions were estimated for: (1) adolescents who reported having severe or very severe role impairment due to MDE, and (2) for adolescents who did not (not shown). Results from these supplemental models suggest that the overall racial/ethnic differences in prescription drug use may represent greater overutilization by whites as well as underutilization by racial/ethnic minorities.
We found that Asians and Hispanics with MDE are less likely than non-Hispanic whites to receive school-based counseling. However, results from a previous study using data from the National Longitudinal Study of Adolescent Health (Add Health) did not find racial/ethnic differences in the receipt of school-based counseling among adolescents with high depressive symptoms.9 One possible explanation is that there may be important differences in the composition of the racial/ethnic subgroups that comprise Hispanics and Asians in each dataset, although it is not possible to make a direct comparison because this information is not available in the public-use NSDUH files. For example, because Cubans and Puerto Ricans were oversampled in Add Health,33 they likely comprise a larger percentage of the Hispanic population in Add Health than in NSDUH. Future research should collect data that allows for comparisons across subgroups among the Hispanic and Asian adolescent populations.
Notably, one-fourth of all adolescents with MDE received school-based counseling, and the relative size of the difference in service use for Asians and Hispanics compared to non-Hispanic whites is smaller in school settings than in outpatient settings. Furthermore, blacks do not differ in their likelihood of receiving school-based counseling relative to non-Hispanic whites. Considered altogether, these findings suggest that greater investment in school-based mental health services could be one mechanism for reducing levels of unmet need for mental health services among all adolescents as well as racial/ethnic disparities in treatment. For example, the provision of mental health services through school-based health centers (SBHCs) has been shown to increase mental health care utilization among low-income adolescent populations across multiple racial/ethnic groups.34 Moreover, racial/ethnic minorities are as likely, if not more likely, to use SBCH services than non-Hispanic whites.35, 36
Along with these significant findings, it important to acknowledge several limitations in this study. First, causality cannot be established because the data are cross sectional. Second, although there may be important subgroup differences in service use within the racial/ethnic groups that were examined, it is not possible to disaggregate these groups any further due to both small cell sizes (e.g. Native Americans and Alaskan Natives) and lack of information about the country/region of origin for Hispanics and Asians. Third, because NSDUH was only conducted in English and Spanish, there may be other non-English speaking populations that are not represented in the sample. Fourth, several constructs such as family status and health status are assessed with proxy measures that may be imprecise. Lastly, the NSDUH public use files do not contain information about several mechanisms that could further explain these racial/ethnic differences in service use including nativity, immigration status, knowledge and stigma concerning mental health treatment, and geographic access to providers.
Notwithstanding these limitations, this study documents low rates of mental health service use among all adolescents with major depression and significantly lower rates among each racial/ethnic minority group that was examined. Investment in quality improvement programs implemented in primary care settings as well as school-based mental health services may reduce unmet need for mental health services among all adolescents with major depression as well as reduce the sizeable differences in service use across racial/ethnic groups. Future research should seek to collect the necessary data to examine subgroup differences and elucidate the distinct pathways that account for racial/ethnic disparities in use of services.
Acknowledgments
This work was supported by a National Institute of Mental Health grant (5K24MH07586703).
The authors are grateful for the helpful comments and suggestions by Neetu Chawla and Michelle Ko at the UCLA School of Public Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Cummings and Druss report have no biomedical financial interests or potential conflicts of interest.
References
- 1.SAMHSA. The NSDUH Report: Major Depressive Episode and Treatment among Adolescents. Rockville, MD: 2009. [Google Scholar]
- 2.Fergusson D, Woodward L. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59(3):225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 3.Weissman MM, Wolk S, Goldstein RB, et al. Depressed adolescents grown up. Jama. 1999 May 12;281(18):1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- 4.Birmaher B, Brent DA, Benson RS. Summary of the practice parameters for the assessment and treatment of children and adolescents with depressive disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1998 Nov;37(11):1234–1238. doi: 10.1097/00004583-199811000-00029. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7(1):3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 6.Alegria M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008 Nov;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olfson M, Gameroff MJ, Marcus SC, Waslick BD. Outpatient treatment of child and adolescent depression in the United States. Arch Gen Psychiatry. 2003 Dec;60(12):1236–1242. doi: 10.1001/archpsyc.60.12.1236. [DOI] [PubMed] [Google Scholar]
- 8.Wu P, Hoven CW, Cohen P, et al. Factors associated with use of mental health services for depression by children and adolescents. Psychiatr Serv. 2001 Feb;52(2):189–195. doi: 10.1176/appi.ps.52.2.189. [DOI] [PubMed] [Google Scholar]
- 9.Cummings JR, Ponce NA, Mays VM. Comparing Racial/Ethnic Differences in Mental Health Service Use Among High-Need Subpopulations Across Clinical and School-Based Settings. Journal of Adolescent Health. 2010;46(6):603–606. doi: 10.1016/j.jadohealth.2009.11.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexandre PK, Martins SS, Richard P. Disparities in adequate mental health care for pastyear major depressive episodes among Caucasian and Hispanic youths. Psychiatr Serv. 2009 Oct;60(10):1365–1371. doi: 10.1176/ps.2009.60.10.1365. [DOI] [PubMed] [Google Scholar]
- 11.SAMHSA. National Survey on Drug Use and Health Codebook. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration; 2008. [Google Scholar]
- 12.Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SD) International Journal of Methods in Psychiatric Research. 1998;7(4):171–185. [Google Scholar]
- 13.Kessler RC, Avenevoli S, Green J, et al. National comorbidity survey replication adolescent supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry. 2009 Apr;48(4):386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alegria M, Shrout PE, Torres M, et al. Lessons learned from the clinical reappraisal study of the Composite International Diagnostic Interview with Latinos. Int J Methods Psychiatr Res. 2009 Jun;18(2):84–95. doi: 10.1002/mpr.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexandre PK, Stephens RM, Laris AS, Dowling K, Rely K. Predictors of Outpatient Mental Health Service Use by American Youth. Psychol Serv. 2008 Aug 1;5(3):251–261. doi: 10.1037/1541-1559.5.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glied S, Bowen Garrett A, Hoven C, et al. Child outpatient mental health service use: why doesn't insurance matter? J Ment Health Policy Econ. 1998 Dec 1;1(4):173–187. doi: 10.1002/(sici)1099-176x(199812)1:4<173::aid-mhp23>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 17.Zimmerman FJ. Social and economic determinants of disparities in professional helpseeking for child mental health problems: evidence from a national sample. Health Serv Res. 2005 Oct;40(5 Pt 1):1514–1533. doi: 10.1111/j.1475-6773.2005.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deykin EY, Levy JC, Wells V. Adolescent depression, alcohol and drug abuse. Am J Public Health. 1987 Feb;77(2):178–182. doi: 10.2105/ajph.77.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rohde P, Lewinsohn PM, Seeley JR. Are adolescents changed by an episode of major depression? J Am Acad Child Adolesc Psychiatry. 1994 Nov–Dec;33(9):1289–1298. doi: 10.1097/00004583-199411000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Stata Statistical Software: Release 10.0 [computer program] College Station, TX: Stata Corporation LP; 2007. [Google Scholar]
- 21.Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington D.C.: Institute of Medicine; 2003. [PubMed] [Google Scholar]
- 22.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv Res. 2006 Oct;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas CR, Holzer CE., 3rd The continuing shortage of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry. 2006 Sep;45(9):1023–1031. doi: 10.1097/01.chi.0000225353.16831.5d. [DOI] [PubMed] [Google Scholar]
- 24.Ngo VK, Asarnow JR, Lange J, et al. Outcomes for youths from racial-ethnic minority groups in a quality improvement intervention for depression treatment. Psychiatr Serv. 2009 Oct;60(10):1357–1364. doi: 10.1176/appi.ps.60.10.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meredith LS, Stein BD, Paddock SM, et al. Perceived barriers to treatment for adolescent depression. Med Care. 2009 Jun;47(6):677–685. doi: 10.1097/MLR.0b013e318190d46b. [DOI] [PubMed] [Google Scholar]
- 26.Corrigan PW, Lurie BD, Goldman HH, Slopen N, Medasani K, Phelan S. How adolescents perceive the stigma of mental illness and alcohol abuse. Psychiatr Serv. 2005 May;56(5):544–550. doi: 10.1176/appi.ps.56.5.544. [DOI] [PubMed] [Google Scholar]
- 27.United States Department of Health and Human Services. Washington D.C.: U.S. Government Printing Office; Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. 2001 [PubMed]
- 28.Walker JS, Coleman D, Lee J, Squire PN, Friesen BJ. Children's stigmatization of childhood depression and ADHD: magnitude and demographic variation in a national sample. J Am Acad Child Adolesc Psychiatry. 2008 Aug;47(8):912–920. doi: 10.1097/CHI.0b013e318179961a. [DOI] [PubMed] [Google Scholar]
- 29.Georg Hsu LK, Wan YM, Chang H, Summergrad P, Tsang BY, Chen H. Stigma of depression is more severe in Chinese Americans than Caucasian Americans. Psychiatry. 2008 Fall;71(3):210–218. doi: 10.1521/psyc.2008.71.3.210. [DOI] [PubMed] [Google Scholar]
- 30.Cauce AM, Domenech-Rodriguez M, Paradise M, et al. Cultural and contextual influences in mental health help seeking: a focus on ethnic minority youth. J Consult Clin Psychol. 2002 Feb;70(1):44–55. doi: 10.1037//0022-006x.70.1.44. [DOI] [PubMed] [Google Scholar]
- 31.Sentell T, Shumway M, Snowden L. Access to mental health treatment by English language proficiency and race/ethnicity. J Gen Intern Med. 2007 Nov;22 Suppl 2:289–293. doi: 10.1007/s11606-007-0345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Balsa AI, Seiler N, McGuire TG, Bloche MG. Clinical Uncertainty and Healthcare Disparities. American Journal of Law & Medicine. 2003;29:203–219. [PubMed] [Google Scholar]
- 33.Harris KM, Halpern CT, Entzel P, Tabor J, Bearman PS, Udry JR. The National Longitudinal Study of Adolescent Health Research Design. [Accessed September 12, 2010];2008 http://www.cpc.unc.edu/projects/addhealth/design/wave1.
- 34.Juszczak L, Melinkovich P, Kaplan D. Use of health and mental health services by adolescents across multiple delivery sites. Journal of Adolescent Health. 2003 Jun;32(6 Suppl):108–118. doi: 10.1016/s1054-139x(03)00073-9. [DOI] [PubMed] [Google Scholar]
- 35.Walter HJ, Vaughan RD, Armstrong B, Krakoff RY, Tiezzi L, McCarthy JF. School-based health care for urban minority junior high school students. Arch Pediatr Adolesc Med. 1995 Nov;149(11):1221–1225. doi: 10.1001/archpedi.1995.02170240039006. [DOI] [PubMed] [Google Scholar]
- 36.Anglin TM, Naylor KE, Kaplan DW. Comprehensive school-based health care: high school students' use of medical, mental health, and substance abuse services. Pediatrics. 1996 Mar;97(3):318–330. [PubMed] [Google Scholar]