Abstract
CONTEXT
Although numerous studies have examined the role of latent variables in the structure of comorbidity among mental disorders, none has examined their role in the development of comorbidity.
OBJECTIVE
To study the role of latent variables in the development of comorbidity among 18 lifetime DSM-IV disorders in the WHO World Mental Health (WMH) surveys.
SETTING/PARTICIPANTS
Nationally or regionally representative community surveys in 14 countries with a total of 21,229 respondents.
MAIN OUTCOME MEASURES
First onset of 18 lifetime DSM-IV anxiety, mood, behavior, and substance disorders assessed retrospectively in the WHO Composite International Diagnostic Interview (CIDI).
RESULTS
Separate internalizing (anxiety and mood disorders) and externalizing (behavior and substance disorders) factors were found in exploratory factor analysis of lifetime disorders. Consistently significant positive time-lagged associations were found in survival analyses for virtually all temporally primary lifetime disorders predicting subsequent onset of other disorders. Within-domain (i.e., internalizing or externalizing) associations were generally stronger than between-domain associations. The vast majority of time-lagged associations were explained by a model that assumed the existence of mediating latent internalizing and externalizing variables. Specific phobia and obsessive-compulsive disorder (internalizing) and hyperactivity disorder and oppositional-defiant disorder (externalizing) were the most important predictors. A small number of residual associations remained significant after controlling the latent variables.
CONCLUSIONS
The good fit of the latent variable model suggests that common causal pathways account for most of the comorbidity among the disorders considered here. These common pathways should be the focus of future research on the development of comorbidity, although several important pair-wise associations that cannot be accounted for by latent variables also exist that warrant further focused study.
Comorbidity is the norm among common mental disorders, as more than 50% of people with a mental disorder in a given year meet criteria for multiple disorders.1, 2 The structure of this comorbidity has been the subject of considerable interest. Beginning with an influential paper by Krueger,3 numerous researchers have documented that bivariate associations among hierarchy-free anxiety, mood, behavior, and substance disorders can be accounted for by correlated latent predispositions to internalizing and externalizing disorders with division of internalizing disorders into secondary dimensions of fear (e.g., panic, phobia) and distress (e.g., major depressive episode, generalized anxiety disorder).4–9
These results have been used to argue for a reorganization of the classification of mental disorders in the DSM and ICD diagnostic systems.10–13 However, additional work is needed to evaluate the empirical support for such a reorganization, as the framework has only recently been expanded to include additional forms of psychopathology, such as psychotic experiences.14 Moreover, additional research on the stability of the structure across socio-demographic variables (e.g., age, sex, education) would be informative.
These results have also been used occasionally to investigate whether risk factors for individual disorders are more accurately conceptualized as risk factors for the latent dimensions underlying these disorders. Kramer and colleagues,15 for example, found that observed gender differences in several internalizing and externalizing disorders became statistically insignificant when controls were included for latent internalizing-externalizing dimensions. Such evidence can be valuable in distinguishing between specific and nonspecific risk factors. The use of latent variable models in this way is only in its infancy. One obvious application is to the development of comorbidity itself. In particular, while the cross-sectional structure of comorbidity has been examined in a number of studies, we are unaware of attempts to investigate the role of latent dimensions in accounting for the development of comorbidity.
Although several studies used longitudinal data to determine whether the structure of internalizing and externalizing disorders is stable over time,9, 16, 17 none investigated whether this structure accounts for the associations between temporally primary disorders and subsequent first onset of comorbid disorders. A number of other longitudinal studies examined temporal progression18, 19 or sequencing20–23 between earlier and later mental disorders, documenting strong persistence of individual disorders over time and significant predictive associations between some but not other temporally primary and later disorders. For example, Fergusson and colleagues18 found that childhood conduct disorder but not ADHD predicted subsequent substance disorders. None of these studies, though, investigated whether associations of earlier disorders with onset of later disorders were mediated by latent variables.
Analysis of the latter sort could be useful in identifying potentially modifiable risk pathways by focusing attention on subsets of disorders with especially strong predictive associations that could subsequently be examined in more focused analyses.24, 25 For example, clinical studies finding childhood impulse-control problems in a subset of patients with early-onset OCD26, 27 and finding that impulse-control disorders continue to feature prominently in some cases of adult OCD28, 29 have created interest in the importance of inhibitory dyscontrol in the pathogenesis of OCD.30 However, the role of putative neurobiological markers of such dyscontrol in accounting for the associations of impulse-control disorders with subsequent OCD remains unstudied. The documentation in epidemiological data of special associations between a cluster of early-onset impulse-control disorders and subsequent OCD could help spur such research by suggesting that more focused prospective neurobiological studies of this cluster beginning in childhood might yield important information about an important OCD subtype.
The current report proposes a novel approach to investigate the role of latent variables in the development of comorbidity. We begin with a conventional survival analysis of epidemiological data collected in 14 countries in the World Health Organization (WHO) World Mental Health (WMH) Survey Initiative31 to study associations between earlier lifetime disorders and the subsequent first onset of later disorders. We then elaborate these survival models using a new latent modeling approach to examine the extent to which the associations among observed disorders can be accounted for by the mediating effects of latent internalizing and externalizing variables.
METHODS AND MATERIALS
Samples
The 14 WMH countries include seven classified by the World Bank as developed (Belgium, France, Germany, Italy, the Netherlands, Spain, USA) and seven developing (Brazil, Colombia, India, Lebanon, Mexico, Peoples’ Republic of China [PRC], Romania). (Table 1) Surveys were carried out in multi-stage clustered area probability household samples representative of specific regions within countries (Brazil, Colombia, India, Mexico, PRC) or entire countries (the remaining countries). Respondents were interviewed face-to-face by trained lay interviewers who explained the purposes of the survey and made clear that participation was voluntary and that responses would be treated as confidential and obtained informed consent prior to beginning interviews. These recruitment and consent procedures were approved by the local Human Subjects committee that monitored the study in each country. A total of 61,292 respondents were interviewed. Country-specific response rates ranged from 45.9% (France) to 98.6% (India). The weighted (by sample size) average response rate was 71.1%.
Table 1.
World Mental Health (WMH) survey sample characteristics
| Country | Survey1 | Sample design | Field Dates | Age Range | Sample Size | Response Rate4 | ||
|---|---|---|---|---|---|---|---|---|
| Part I | Part II | Part II and Age 18–443 | ||||||
| I. Developed | ||||||||
| Belgium | ESEMeD | Stratified multistage clustered probability sample of individuals residing in households from the national register of Belgium residents. NR | 2001–2 | 18+ | 2,419 | 1,043 | 486 | 50.6 |
| France | ESEMeD | Stratified multistage clustered sample of working telephone numbers merged with a reverse directory (for listed numbers). Initial recruitment was by telephone, with supplemental in-person recruitment in households with listed numbers. NR | 2001–2 | 18+ | 2,894 | 1,436 | 727 | 45.9 |
| Germany | ESEMeD | Stratified multistage clustered probability sample of individuals from community resident registries. NR | 2002–3 | 18+ | 3,555 | 1,323 | 621 | 57.8 |
| Italy | ESEMeD | Stratified multistage clustered probability sample of individuals from municipality resident registries. NR | 2001–2 | 18+ | 4,712 | 1,779 | 853 | 71.3 |
| Netherlands | ESEMeD | Stratified multistage clustered probability sample of individuals residing in households that are listed in municipal postal registries. NR | 2002–3 | 18+ | 2,372 | 1,094 | 516 | 56.4 |
| Spain | ESEMeD | Stratified multistage clustered area probability sample of household residents. NR | 2001–2 | 18+ | 5,473 | 2,121 | 960 | 78.6 |
| United States | NCS-R | Stratified multistage clustered area probability sample of household residents. NR | 2002–3 | 18+ | 9,282 | 5,692 | 3,197 | 70.9 |
| Total | 30,707 | 14,488 | 7,360 | 63.8 | ||||
| II. Developing | ||||||||
| Brazil | São Paulo Megacity | Stratified multistage clustered area probability sample of household residents in the São Paulo metropolitan area. | 2004–7 | 18+ | 5,037 | 2,942 | 1,824 | 81.3 |
| Colombia | NSMH | Stratified multistage clustered area probability sample of household residents in all urban areas of the country (approximately 73% of the total national population) | 2003 | 18–65 | 4,426 | 2,381 | 1,731 | 87.7 |
| India | WMHI | Stratified multistage clustered area probability sample of household residents in Pondicherry region. NR | 2003–5 | 18+ | 2,992 | 1,373 | 825 | 98.6 |
| Lebanon | LEBANON | Stratified multistage clustered area probability sample of household residents. NR | 2002–3 | 18+ | 2,857 | 1,031 | 595 | 70.0 |
| Mexico | M-NCS | Stratified multistage clustered area probability sample of household residents in all urban areas of the country (approximately 75% of the total national population). | 2001–2 | 18–65 | 5,782 | 2,362 | 1,736 | 76.6 |
| PRC | Shenzhen | Stratified multistage clustered area probability sample of household residents and temporary residents in the Shenzhen area. | 2006–7 | 18+ | 7,134 | 7,1343 | 6,2183 | 80.0 |
| Romania | RMHS | Stratified multistage clustered area probability sample of household residents. NR | 2005–6 | 18+ | 2,357 | 2,357 | 940 | 70.9 |
| Total | 30,585 | 19,580 | 13,686 | 80.2 | ||||
| III. Total | 61,292 | 34,068 | 21,229 | 71.1 | ||||
ESEMeD (The European Study Of The Epidemiology Of Mental Disorders); NCS-R (The US National Comorbidity Survey Replication); NSMH (The Colombian National Study of Mental Health); WMHI (World Mental Health India); LEBANON (Lebanese Evaluation of the Burden of Ailments and Needs of the Nation); M-NCS (The Mexico National Comorbidity Survey); RMHS (Romania Mental Health Survey);
Most WMH surveys are based on stratified multistage clustered area probability household samples in which samples of areas equivalent to counties or municipalities in the US were selected in the first stage followed by one or more subsequent stages of geographic sampling (e.g., towns within counties, blocks within towns, households within blocks) to arrive at a sample of households, in each of which a listing of household members was created and one or two people were selected from this listing to be interviewed. No substitution was allowed when the originally sampled household resident could not be interviewed. These household samples were selected from Census area data in all countries other than France (where telephone directories were used to select households) and the Netherlands (where postal registries were used to select households). Several WMH surveys (Belgium, Germany, Italy) used municipal resident registries to select respondents without listing households. 10 of the 14 surveys are based on nationally representative (NR) household samples. The others are representative of particular cities (Brazil, India) or the urbanized areas of the countryt (Colombia, Mexico).
In Shenzhen, all respondents received the Part II interview and all respondents between ages of 18 and 44 were used in the current analysis.
The response rate is calculated as the ratio of the number of households in which an interview was completed to the number of households originally sampled, excluding from the denominator households known not to be eligible either because of being vacant at the time of initial contact or because the residents were unable to speak the designated languages of the survey.
The interview was divided into two parts. Part I assessed core disorders and was completed by all respondents. Part II assessed additional disorders and numerous correlates and was completed by 100% of respondents who met criteria for any Part I disorder plus a probability subsample of other Part I respondents. Based on a concern about recall bias, disorders defined as beginning in childhood (attention-deficit/hyperactivity disorder, conduct disorder, oppositional defiant disorder, separation anxiety disorder) were assessed only among respondents in the age range 18–44. This Part II 18–44 subsample, which ranges between 486 (Belgium) and 6,218 (PRC) and totals 21,229 respondents across countries, is the sample used in the current report. The Part I samples were weighted to adjust for differential probabilities of selection and residual discrepancies between sample and Census on socio-demographic and geographic variables. The Part II samples were additionally weighted to adjust for under-sampling of Part I respondents without Part I disorders. A more detailed discussion of WMH sampling and weighting is presented elsewhere.32
Diagnostic assessment
Diagnoses were based on Version 3.0 of the WHO Composite International Diagnostic Interview (CIDI),33 a fully-structured lay-administered interview that generates diagnoses according to both ICD-10 and DSM-IV criteria. DSM-IV criteria are used here. Translation and back translation followed standard WHO procedures.34 The seven-day interviewer training program was standardized across countries. Training culminated in an examination that had to be passed before the interviewer could begin production data collection. A more detailed discussion of WMH training and quality control is presented elsewhere.35
The 18 lifetime diagnoses include mood disorders (bipolar I–II or sub-threshold disorder, major depressive episode/dysthymia), anxiety disorders (agoraphobia with or without panic disorder, generalized anxiety disorder [GAD], obsessive-compulsive disorder [OCD], panic disorder with or without agoraphobia, post-traumatic stress disorder [PTSD], separation anxiety disorder, social phobia, specific phobia), behavior disorders (attention-deficit disorder [AD], hyperactivity disorder [HD], conduct disorder with covert symptoms [CD1; e.g., lying, shoplifting], conduct disorder with overt symptoms [CD2; e.g., bullying, being physically cruel to people], intermittent explosive disorder [IED], oppositional-defiant disorder [ODD]), and substance disorders (alcohol and drug abuse with or without dependence).
As detailed elsewhere,36 blinded clinical reappraisal interviews found generally good concordance between DSM-IV diagnoses based on the CIDI and those based on the Structured Clinical Interview for DSM-IV.37 Organic exclusions but not diagnostic hierarchy rules were used in making diagnoses. The CIDI included retrospective disorder age-of-onset reports based on a special question sequence that has been shown experimentally to improve recall accuracy.38 Respondents were asked to date their age when they first had the full syndrome for each disorder, not the first symptom of the disorder.
Analysis methods
Exploratory principal axis tetrachoric factor analysis with promax rotation was used to examine bivariate comorbidity. Clear internalizing (10 disorders) and externalizing (8 disorders) dimensions were found, but no evidence for a third factor that distinguished fear from distress disorders. Discrete-time survival analysis39 with person-year the unit of analysis and a logistic link function40 was then used to study associations of temporally primary lifetime disorders with subsequent first onset of later disorders. Each model predicted first onset of one of the 18 DSM-IV/CIDI disorders from information about prior lifetime occurrence of the other 17 disorders (18×17 = 306 pair-wise associations), which were treated as time-varying covariates, controlling for respondent age, sex, and country. Retrospective age-of-onset reports were used to define the predictor disorders as time-varying and to define age-of-onset of the outcome disorders.
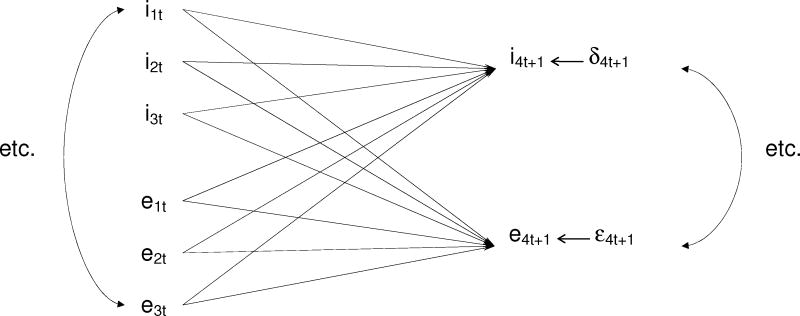
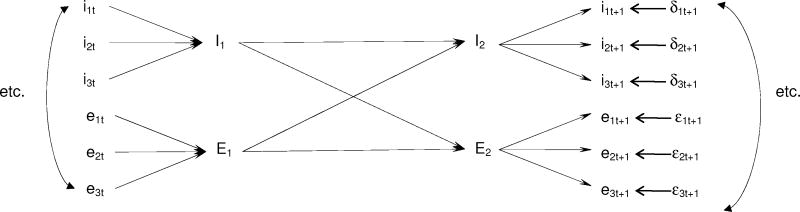
We then estimated a latent variable model that constrained the coefficients in the observed variable models to be mediated by hypothesized continuous time-varying latent internalizing and externalizing variables. The coefficients in the observed variable model were constrained in the sense that this model included 306 coefficients (Figure 1a), whereas the latent variable model used only 36 independent coefficients to reproduce these same associations (Figure 1b): 10 coefficients (one of which was non-independent because the 10 coefficients together perfectly predict the time t latent variable) for the time t lifetime internalizing disorders predicting the time t latent internalizing variable; 8 coefficients (one of which was non-independent because the 8 coefficients together perfectly predict the time t latent variable) for the time t lifetime externalizing disorders predicting the time t latent externalizing variable; 4 coefficients (two of which were non-independent because the pair of time t latent variables perfectly predict each of the two time t+1 latent variables) for the time t latent internalizing and externalizing variables predicting the time t+1 latent internalizing and externalizing variables; 10 coefficients for the time t+1 latent internalizing variable predicting first onsets of the 10 time t+1 internalizing disorders; and 8 coefficients for the time t+1 latent externalizing variable predicting first onsets of the 8 time t+1 externalizing disorders.
Figure 1.
Figure 1a. Schematic of the multivariate observed variable model1
1Only three observed lifetime time t internalizing disorders (e.g., i1t represents internalizing disorder 1 at time t) and externalizing disorders along with only one observed internalizing and one observed externalizing disorder at time t+1 are shown to simplify the presentation, but there were 10 observed lifetime internalizing and 8 observed externalizing disorders in the actual survival model at each time point. First onset of each of these 18 disorders between times t and t+1 was predicted by prior lifetime history of the other 17 disorders as of time t. Estimation was made in 18 separate survival equations, each with 17 predictors for prior history of the other disorders, for a total of 306 (18×17) pair-wise time-lagged associations between earlier and later mental disorders. The 17 predictor disorders were treated as time-varying covariates in a discrete-time (person-year) survival framework. Controls were also included for respondent age at interview, sex, person-year, and country.
Figure 1b. Schematic of the multivariate latent variable model1
1Only three observed lifetime time t internalizing disorders (e.g., i1t represents internalizing disorder 1 at time t) and externalizing disorders and only three disorders of each set at time t+1 are shown to simplify the presentation, but there were 10 observed lifetime internalizing and 8 observed externalizing disorders in the actual survival model. First onset of each of these 18 disorders between times t and t+1 was predicted by latent internalizing or latent externalizing variables at time t+1. These latent variables, in turn, were predicted by lifetime history of latent internalizing and externalizing variables as of time t. These time t latent variables, finally, were predicted by lifetime history of observed internalizing or externalizing variables as of time t. Estimation was carried out using a three-part iterative procedure. See the text for more details. A total of 36 independent associations were estimated, 270 fewer than in the model for associations among observed disorders. As in the earlier observed variable model, the predictor disorders were treated as time-varying covariates in a discrete-time (person-year) survival framework and controls were included for respondent age at interview, sex, person-year, and country.
In interpreting the latent variable results, it is useful to note that the latent variables are actually weighted (by ORs of disorders predicting latent variables) composites of all predictor disorders. The assumption that a single weighted composite can represent the effects of all predictor disorders is equivalent to assuming that the ratios of the ORs across predictors are constant across outcomes. These constraints are the key features of the model. The standard covariance structure analysis programs used in previous studies of the structure of comorbidity could not be used to impose these constraints, as discrete-time survival analysis is based on a person-year data array that varies in size across the outcomes. An iterative maximum-likelihood (ML) method implemented in a SAS macro was consequently written to estimate the coefficients.41 This procedure sequentially estimated the coefficients in the three parts of the model (time t observed variables predicting time t latent variables, time t latent variables predicting time t+1 latent variables, time t+1 latent variables predicting time t+1 observed variables), each time holding constant the coefficients in the other two parts of the model to their values in the previous iteration, until estimates converged.
Once estimated, a likelihood-ratioχ2 test was used to compare the fit of the latent variable model and the observed variable model with 270 (306-36) degrees of freedom. As described below, the latent variable model provided a better fit. We also investigated whether any of the 306 pair-wise associations remained significant after controlling for the latent variables. Simple pair-wise tests were inappropriate for here because separate .05-level tests would generate more than a dozen false positives out of 306 tests. The Bonferroni method and its extensions deal with this problem,42 but these are low-power tests that make it difficult to detect all but the largest true associations.43 We consequently used an internal sub-sampling strategy to pinpoint pair-wise associations for further investigation by estimating observed variable survival models controlling for the latent variables in subsets of person-years. Rather than use random subsamples, which would simply have produced patterns determined by the rules of random sampling, we focused on meaningfully different subsamples defined by four independent life course stages (childhood: ages 4–12; adolescence: ages 13–19; young adulthood: ages 20–29; middle adulthood: ages 30–44) and considering a given pair-wise association substantively significant only if it was statistically significant at the .05 level both in the total sample and in at least two independent sub-samples with consistent sign patterns and odds-ratios (exponentiated survival coefficients) either greater than or equal to 2.0 or less than or equal to 0.5. As the WMH data are both clustered and weighted, the design-based method of jackknife repeated replications (JRR)44 was used to calculate standard errors and assess statistical significance. A SAS macro was used for this purpose.41
RESULTS
Exploratory factor analysis
Exploratory factor analysis of the 18 lifetime DSM-IV/CIDI disorders was carried out separately in developed and developing countries. Only two meaningful factors were found, with unrotated eigenvalues of 8.0 and 1.8 (developed) and 6.6 and 2.3 (developing). Promax rotated factor loadings (standardized partial regression coefficients) showed the factors correspond to internalizing and externalizing dimensions. (Table 2) All the mood and anxiety disorders other than bipolar disorder (BPD) loaded clearly on the internalizing factor (.43–.87 standardized regression coefficients). All the behavior and substance disorders other than IED loaded clearly on the externalizing factor (.51–.94 standardized regression coefficients). BPD cross-loaded in developed countries (.31–.37) and IED in developing countries (.30–.48). However, country-level analyses found that BPD generally loaded more strongly on the internalizing factor and IED on the externalizing factor, leading us to classifying them with these dimensions in further analyses. (Detailed results are not reported, but are available on request.) Separate factor analysis of only the internalizing disorders found no reliable secondary distinction between fear and other distress disorders (unrotated eigenvalues of 4.8 and 1.0 in developed countries and 4.3 and 1.3 in developing countries).
Table 2.
Prevalence and rotated (promax) factor pattern (standardized regression coefficients) of lifetime DSM-IV/CIDI disorders separately in developed and developing WMH countries1
| Estimated lifetime prevalence | Standardized regression coefficients | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Developed | Developing | Total | Developed | Developing | Total | |||||||
| % | (SD) | % | (SD) | % | (SD) | I | II | I | II | I | II | |
| I. Internalizing disorders | ||||||||||||
| Agoraphobia2 | 1.8 | 13.0 | 1.0 | 9.9 | 1.3 | 11.0 | .87 | −.11 | .74 | −.16 | .82 | −.14 |
| Bipolar I–II disorder | 4.4 | 22.9 | 2.0 | 15.1 | 2.8 | 18.3 | .37 | .31 | .54 | .20 | .46 | .27 |
| Generalized anxiety disorder | 4.9 | 22.0 | 1.4 | 12.5 | 2.6 | 16.8 | .67 | .04 | .72 | −.02 | .69 | .05 |
| Major depressive episode/dysthymia | 17.5 | 40.9 | 9.4 | 33.1 | 12.0 | 36.5 | .72 | .07 | .69 | .09 | .71 | .09 |
| Obsessive-compulsive disorder | 6.9 | 29.7 | 5.8 | 32.6 | 6.2 | 31.7 | .51 | .12 | .71 | −.17 | .63 | −.04 |
| Panic disorder3 | 3.4 | 16.6 | 0.7 | 8.0 | 1.6 | 11.8 | .65 | .10 | .51 | .17 | .60 | .17 |
| Post-traumatic stress disorder | 4.4 | 25.4 | 1.6 | 14.8 | 2.6 | 19.5 | .57 | .18 | .43 | .18 | .52 | .21 |
| Separation anxiety disorder | 5.8 | 25.3 | 5.5 | 24.2 | 5.6 | 24.6 | .54 | .20 | .47 | .14 | .50 | .15 |
| Social phobia | 7.7 | 30.4 | 2.6 | 18.5 | 4.3 | 23.7 | .72 | .09 | .74 | −.04 | .71 | .09 |
| Specific phobia | 10.4 | 35.4 | 7.1 | 32.3 | 8.2 | 33.3 | .75 | −.13 | .78 | −.16 | .79 | −.16 |
| II. Externalizing disorders | ||||||||||||
| Attention-deficit disorder | 3.4 | 23.5 | 0.8 | 9.5 | 1.6 | 15.8 | .30 | .51 | .36 | .57 | .31 | .55 |
| Hyperactivity disorder | 2.7 | 19.7 | 0.6 | 8.4 | 1.3 | 13.7 | .19 | .58 | .32 | .60 | .22 | .61 |
| Conduct disorder (Overt)4 | 1.6 | 15.3 | 0.8 | 9.2 | 1.1 | 11.6 | −.09 | .94 | −.03 | .90 | −.08 | .93 |
| Conduct disorder (Covert)5 | 4.5 | 31.1 | 1.8 | 15.6 | 2.7 | 22.1 | −.04 | .90 | .05 | .84 | −.01 | .87 |
| Intermittent explosive disorder | 6.9 | 32.5 | 4.2 | 28.1 | 5.1 | 29.9 | .15 | .61 | .48 | .30 | .29 | .47 |
| Oppositional-defiant disorder | 4.9 | 34.0 | 3.3 | 20.9 | 3.9 | 26.1 | .10 | .80 | −.02 | .73 | .02 | .78 |
| Alcohol abuse6 | 9.7 | 42.3 | 8.0 | 34.7 | 8.5 | 37.5 | .01 | .76 | −.14 | .63 | −.06 | .73 |
| Drug abuse5 | 6.4 | 31.3 | 2.7 | 21.0 | 3.9 | 25.0 | −.06 | .79 | −.15 | .69 | −.08 | .77 |
| (n)7 | (7,360) | (13,869) | (21,229) | |||||||||
Results are based on principal axis factor analysis of tetrachoric correlation matrices estimated in person-year datasets.
with or without panic disorder
with or without agoraphobia
e.g., bullying, fighting, being physically cruel to people
e.g., lying, shoplifting
with or without dependence
The n’s are for the numbers of respondents. The numbers of person-years (every year of life of the respondents beginning at age 4 up to and including the age at interview) are 214,738 (developed), 376,961 (developing), and 591,699 (total).
Bivariate and multivariate associations between earlier and later disorders
As noted above, we estimated 306 bivariate survival equations, each with first onset of one disorder predicted by the prior occurrence of one of the other 17 disorders. 98.0% of the 306 survival coefficients were positive and 95.1% significant. (Table 3) (Detailed results are not reported, but are available on request.) The median (and IQR) odds-ratios (ORs) were 3.4 (2.7–4.3). None of the negative ORs was significant. Within-domain ORs were generally larger than between-domain ORs, with within-domain median ORs of 3.6–5.5 compared to between-domain medians of 3.0–3.2.
Table 3.
Associations (odds-ratios) of lifetime DSM-IV/CIDI disorders with subsequent first onset of other DSM-IV/CIDI disorders based on bivariate and multivariate survival models in the total sample (n = 21,229)1
| Distribution of odds-ratios |
||||||
|---|---|---|---|---|---|---|
| Median | Range | Inter-quartile Range | % positive | % positive and significant | Number of odds-ratios | |
| I. Internalizing predicting internalizing | 90 | |||||
| Bivariate | 3.6 | 1.2–10.4 | 3.0–4.3 | 100 | 97.8 | |
| Multivariate | 1.6 | 0.4–5.5 | 1.1–2.0 | 87.8 | 58.9 | |
| II. Externalizing predicting internalizing | 80 | |||||
| Bivariate | 3.2 | 1.7–7.5 | 2.6–3.7 | 100 | 98.8 | |
| Multivariate | 1.3 | 0.5–3.2 | 1.0–1.6 | 80.0 | 28.8 | |
| III. Internalizing predicting externalizing | 80 | |||||
| Bivariate | 3.0 | 0.4–10.3 | 2.4–3.9 | 96.3 | 90.0 | |
| Multivariate | 1.3 | 0.1–3.2 | 0.9–1.6 | 70.0 | 33.8 | |
| IV. Externalizing predicting expernalizing | 56 | |||||
| Bivariate | 5.5 | 0.5–30.0 | 3.3–8.2 | 94.5 | 92.7 | |
| Multivariate | 1.6 | 0.2–13.4 | 1.2–2.9 | 81.8 | 50.9 | |
| V. Total | 306 | |||||
| Bivariate | 3.4 | 0.4–30.0 | 2.7–4.3 | 98.0 | 95.1 | |
| Multivariate | 1.4 | 0.1–13.4 | 1.1–1.9 | 80.0 | 43.0 | |
First lifetime onset of each of 18 DSM-IV/CIDI disorders was predicted either by a single dummy variables for prior lifetime history of one of the other disorders (bivariate model) or 17 dummy variables for prior history of each of the 17 other disorders (multivariate model). in discrete-time (person-year) survival models. The predictor disorders and latent variables were treated as time-varying covariates. Controls were included for respondent age at interview, person-year, sex, and country.
This largely positive pattern persisted in attenuated form in multivariate models, with 80.0% of ORs positive and 43.0% positive and statistically significant. (Table 3) The median (1.4) and IQR (1.1–1.9) of ORs are considerably lower than in bivariate models due to strong inter-correlations among predictor disorders. Nine of the 306 multivariate ORs were negative and significant (GAD predicting agoraphobia and specific phobia and HD, PTSD and CD1 predicting OCD, CD2 predicting GAD and PTSD, and alcohol abuse predicting AD and HD). 50.9–58.9% of within-domain ORs were positive and significant compared to 28.8–33.8% of between-domain ORs. The median OR was higher within (1.6) than between (1.3) domains.
Multivariate associations in the latent variable model
The latent variable model fit the observed data better than the observed variable model, as indicated by both a lower Bayesian Information Criterion (BIC)45 of 7514.3 (latent) versus 7530.0 (observed) and an insignificant improvement in likelihood-ratio χ2 of the observed variable model (χ2270 = 107.8, p = .99). Latent variable coefficients are quite stable, as indicated by the Pearson correlations of model coefficients across four samples (the total sample and the three subsamples of all developed countries, all developing countries, and all countries excluding the four with survey response rates less than 60% [Belgium, France, Germany, Spain]) being .88–.97. (Detailed results are not reported, but are available on request.)
As noted earlier, the latent variables are actually weighted (by ORs of disorders predicting latent variables) composites of all predictor disorders. The assumption that a single weighted composite can represent the effects of all the predictor disorders on all outcomes is equivalent to assuming that the ratios of the ORs across predictors are constant across outcomes. The good fit of the latent variable model shows that this assumption is generally consistent with the data, which means the predictive effects of these disorders on each other can plausibly be assumed to be mediated by common internalizing and externalizing pathways.
The metric of the time t latent variables was set by fixing the slope of the latent variable on the strongest time t predictor to 1.0 and scaling other slopes relative to that value. (Table 4) Within the internalizing domain, specific phobia is by far the most powerful predictor (1.00 by definition) followed by OCD (.62) and other phobias (.46–.48). (Table 4) GAD and panic disorder, at the other extreme, are insignificant predictors. The remaining internalizing disorders have ORs of intermediate strength (.18–.44). Within the externalizing domain, HD (1.00) and ODD (.97) are the most powerful predictors. Alcohol and drug abuse are insignificant and the remaining externalizing disorders have ORs in the range .43–.77.
Table 4.
Parameter estimates for associations between observed disorders and latent variables in the latent variable model (n = 21,229)1
| Time t disorders predicting time t latent variables | Time t+1 latent variables predicting time t+1 first onset of disorders | |||
|---|---|---|---|---|
| Est1 | (SE) | Est2 | (SE) | |
| I. Internalizing | ||||
| Agoraphobia | .48* | (.09) | 1.00* | (.09) |
| Bipolar disorder | .18* | (.08) | .85* | (.05) |
| Generalized anxiety disorder | .02 | (.07) | .72* | (.05) |
| Major depressive episode | .29* | (.06) | .68* | (.04) |
| Obsessive-compulsive disorder | .62* | (.07) | .87* | (.06) |
| Panic disorder | −.02 | (.10) | .82* | (.05) |
| Post-traumatic stress disorder | .21* | (.08) | .68* | (.05) |
| Separation anxiety disorder | .44* | (.06) | .74* | (.05) |
| Social phobia | .46* | (.05) | .97* | (.05) |
| Specific phobia | 1.00* | (.09) | .86* | (.10) |
| II. Externalizing | ||||
| Attention-deficit disorder | .77* | (.24) | 1.00* | (.31) |
| Hyperactivity disorder | 1.00* | (.23) | .95* | (.16) |
| Conduct disorder I | .43* | (.18) | .74* | (.16) |
| Conduct disorder II | .57* | (.23) | .78* | (.16) |
| Intermittent explosive disorder | .77* | (.15) | .52* | (.08) |
| Oppositional-defiant disorder | .97* | (.18) | .69* | (.15) |
| Alcohol use disorder | −.53 | (.35) | .44* | (.08) |
| Drug use disorder | .51 | (.31) | .38* | (.13) |
Significant at the .05 level, two-sided test
Based on an iteratively estimated pooled discrete-time (person-year) survival model with 17 dummy variables for prior history of each other disorder predicting subsequent first onset of each of the 18 disorders assuming the existence of latent internalizing and externalizing disorders that explain the direct effects of the observed predictor disorders on the outcome disorders. The predictor disorders and latent variables were treated as time-varying covariates. Controls were included for respondent age at interview, person-year, sex, and country. See the text for a discussion of estimation methods.
The ORs for the disorders as outcomes are much more consistent than for the disorders as predictors, with ranges of .68–1.00 (internalizing) and .44–1.00 (externalizing). Agoraphobia and social phobia are the most strongly predicted internalizing disorders, while AD and HD are the most strongly predicted externalizing disorders. The relative importance of internalizing and externalizing disorders predicting each other is estimated in the set of four ORs between the latent variables at times t and t+1. (Table 5) Weighted (by relative prevalence of disorders) within-domain ORs (1.6 for internalizing; 1.4 for externalizing) are higher than between-domain ORs (1.3 for time t internalizing predicting time t+1 externalizing; 1.1 for time t externalizing predicting time t+1 internalizing), but between-domain ORs are nonetheless statistically significant.
Table 5.
Parameter estimates for associations among latent variables in the latent variable model (n = 21,229)
| Time 1 predictor group | Time 2 dependent group | |||
|---|---|---|---|---|
| Internalizing | Externalizing | |||
| OR | (95% CI) | OR | (95% CI) | |
| Internalizing | 1.6* | (1.5–1.6) | 1.3* | (1.2–1.3) |
| Externalizing | 1.1* | (1.1–1.2) | 1.4* | (1.3–1.4) |
Significant at the .05 level, two-sided test
Residual associations not explained by the latent variable model
Only 13 of the 306 residual pair-wise time-lagged associations between observed disorders passed our test of statistical significance. Nine of these are positive. Four involve within-disorder reciprocal ORs: between CDI and CD2 (3.2–4.8) and between AD and HD (4.0–19.4). Two others involve asymmetrical associations between well-known disorder pairs (panic predicting agoraphobia [2.0–2.22] and depression predicting GAD [2.0–6.0], although the latter association is limited to child-adolescent onsets). Two others might reflect diagnostic confusions rather: agoraphobia predicting specific phobia (2.2–4.8); and HD (but, importantly, not AD) predicting BPD (1.9–3.9). The final significant positive association is for IED predicting OCD (1.5–4.0). The four significant negative residual associations include PTSD predicting OCD (0.4–0.7), CD2 predicting both BPD (0.2–0.5) and PTSD (0.2–0.4) and IED (0.5–0.6) predicting drug abuse.
DISCUSSION
Six limitations are noteworthy. First, diagnoses were based on fully-structured lay interviews. These typically produce more reliable (i.e., reproducible across multiple interviewers) diagnoses than semi-structured clinical interviews46 and their prevalence estimates typically correspond well with those based on clinical interviews.47 However, fully-structured interviews, unlike semi-structured clinical interviews, are unable to clarify symptom responses or check questions across disorders to facilitate differential diagnosis, potentially leading to inflated estimates of comorbidity. Second, disorders were assessed dichotomously rather than dimensionally, presumably reducing our ability to detect for subtle aspects of structure in the data. This might help explain why we did not detect higher-order sub-factors in the two-factor exploratory factor analysis model. Third, data were combined across countries with very different cultures and across surveys with very different response rates (which could have introduced variation in sample selection bias), different rates of sample exclusion (due to cross-national differences in rates of suicide, homelessness, and institutionalization), and different languages in which interviews were administered. Even though every effort was made to make the translations as comparable as possible,34 residual variation in meaning almost certainly contributed to cross-national variation in results.
Fourth, lifetime diagnoses were based on retrospective reports rather than prospective assessments, probably leading to recall bias that under-estimated prevalence48 and distorted age-of-onset estimates49 despite the use of special memory priming methods.38 Bias in model coefficients might have varied across disorders as a function of age of onset and/or recency. Given the importance of this potential bias, it is noteworthy that the onset distributions based on these retrospective data are quite consistent with those based on prospective studies and studies carried out at separate life course stages.50 In addition, model coefficients in subsamples defined by life course stage are very consistent, suggesting that variation in recall across the sample age range does not importantly influence results. Fifth, models were based on the simplifying assumptions that the time-lagged associations among mental disorders are constant across countries and gender, stable across the life course, and unrelated either to age-of-onset or time-since-onset of the predictor disorders. Preliminary analyses showed that these assumptions are a reasonable first approximation, but the investigation of these specifications needs to be a focus of ongoing WMH analysis. Sixth, we did not take history of treatment into consideration even though early treatment, which varies in frequency across countries,51 might interrupt the progression of comorbidity and thereby distort estimates of predictive associations.
In the context of these limitations, our finding of a two-factor internalizing-externalizing structure among WMH disorders is consistent with previous research,4–9 but does not support the distinction in some previous studies between distress (e.g., depression, GAD, PTSD) and fear (i.e., panic and phobias) disorders. As noted in the introduction, others also failed to find a distinction between distress and fear disorders.16, 52 This less differentiated structure in the WMH data might be due to our focus on lifetime disorders, whereas 12-month disorders were the focus of most studies that distinguished distress and fear disorders.
Our finding of significant time-lagged associations across virtually all pairs of the disorders considered here is broadly consistent with evidence of associations between earlier and later disorders in previous longitudinal studies,18–23 although most previous studies focused on prevalent cases whereas we studied first onsets. We found, again consistent with previous studies, stronger and more consistent time-lagged associations within than between the internalizing and externalizing domains. However, again like previous studies, we also found significant between-domain time-lagged associations.22, 23
Our analysis then went beyond previous studies to investigate the role of latent variables in the development of comorbidity. We showed that the vast majority of the 306 pair-wise time-lagged associations among the 18 disorders considered here can be explained by a model that assumes the existence of mediating latent internalizing and externalizing variables. This finding extends previous cross-cultural work on the structure of comorbidity.53 The fact that the predictive associations across this large number of disorders is mediated by two higher-order variables makes the internalizing and externalizing spectrum dimensions compelling targets for inquiry aimed at reducing burden of mental disorder around the world by interrupting the processes leading to the onset of comorbidity.
Specific phobia and OCD stood out as the most important internalizing predictors and HD and ODD the most important externalizing predictors. The time-lagged associations involving these four predictors were largely mediated by the latent variables, with only two of the 13 significant residual associations involving these four strongest predictors (HD predicting AD and BPD). Both of these were positive, showing that the comparatively high ORs of these four predictor disorders are relatively constant across the range of WMH outcomes. Although it is unclear why specific phobia and OCD should be the most important predictors among the internalizing disorders or HD and ODD among the externalizing disorders, the fact that all four are typically early-onset disorders50 means they might be useful markers of youth at high risk for progression to later disorders. Even this possibility requires further analysis, though, as we did not investigate non-proportional hazards that might include differential predictive associations related to age-of-onset or time-since-onset. These more in-depth analyses go beyond the scope of this first report, but will be pursued in ongoing WMH analyses.
Our finding of 13 significant residual associations shows that the latent variables do not explain all the comorbidity among the disorders considered here. The four negative residual associations are most plausibly interpreted as suggesting the existence of more differentiated dimensions underlying internalizing and externalizing disorders. The negative association of IED with subsequent drug abuse, for example, could be due to externalizing disorders being made up of multiple dimensions, one or more of which is significantly more strongly related to drug abuse than to IED. Evidence consistent with this possibility exists in the literature54–56 The negative residual association of CD2 (overt CD) with subsequent PTSD, in comparison, might be related to the findings that blunted psychophysiological and emotional reactivity to fear stimuli are predictors of CD57, 58 whereas heightened physiological reactivity to trauma-related stress cues is a predictor of PTSD.59, 60 These observations suggest that a more differentiated latent variable model that includes internalizing and externalizing sub-dimensions might explain the significant negative associations found here in the less differentiated WMH latent variable model.
The positive residual associations in the WMH data, in comparison, are most plausibly interpreted as disorder subtypes rather than comorbidities, including the reciprocal associations between CD1 (covert CD) and CD2 (overt CD) and between AD and HD, or a severity marker in the association between panic disorder and subsequent agoraphobia. At least one other association, between agoraphobia and subsequent specific phobia, could be due to diagnostic confusion in the CIDI. The same kind of confusion might account at least in part for the positive association between HD and subsequent BPD, as differentiation between these two disorders can be difficult, especially within the constraints of a fully-structured diagnostic interview,61, 62 although a number of common neurobiological correlates have also been found for HD and BPD,63, 64 arguing that ADHD might be a risk marker for BPD. The WMH finding that this association is specific to HD and does not apply to AD has not to our knowledge been investigated previously.
It is important to caution that these few unique significant residual pair-wise associations should be treated as no more than preliminary due to the problem of multiple testing and the limitations noted at the beginning on this section. Replication in other datasets, most importantly prospective datasets, is needed before these associations should be considered reliable. Furthermore, even if they are subsequently found to be reliable, their existence should not deflect attention from our main finding: that the consistently significant comorbidities found among the 306 disorder-pairs considered here are likely due to common underlying processes that should be a major focus of future research on the development of comorbidity. One important implication of this finding is that future research on specific pair-wise comorbid associations needs to guard against interpreting results as unique without first demonstrating, as we did here, that they are specific rather than mere realizations of larger processes involving all internalizing and/or externalizing disorder. The fact that we found only two factors, finally, does not mean that only two underlying processes are at work, as multiple processes could underlie each factor and these diverse processes need to be studied in order to enrich our understanding of the causal influences leading to the higher-order structure found here.
Acknowledgments
This report was prepared as part of the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, the Eli Lilly & Company Foundation, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, Bristol-Myers Squibb, and Shire. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/. The São Paulo Megacity Mental Health Survey is supported by the State of São Paulo Research Foundation (FAPESP) Thematic Project Grant 03/00204-3. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection. The WMHI is funded by WHO (India) and helped by Dr R Chandrasekaran, JIPMER. The Lebanese National Mental Health Survey (LEBANON) is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon), Fogarty International, anonymous private donations to IDRAAC, Lebanon, and unrestricted grants from Janssen Cilag, Eli Lilly, GlaxoSmithKline, Roche, and Novartis. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the PanAmerican Health Organization (PAHO). The Shenzhen Mental Health Survey is supported by the Shenzhen Bureau of Health and the Shenzhen Bureau of Science, Technology, and Information. The Romania WMH study projects “Policies in Mental Health Area” and “National Study regarding Mental Health and Services Use” were carried out by National School of Public Health & Health Services Management (former National Institute for Research & Development in Health), with technical support of Metro Media Transilvania, the National Institute of Statistics-National Centre for Training in Statistics, SC. Cheyenne Services SRL, Statistics Netherlands with funding by the Ministry of Public Health (former Ministry of Health) with supplemental support from Eli Lilly Romania SRL. The ESEMeD project (which includes surveys in Belgium, France, Germany, Italy, Netherlands, and Spain) is funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Departament de Salut, Generalitat de Catalunya, Spain, Instituto de Salud Carlos III (CIBER CB06/02/0046, RETICS RD06/0011 REM-TAP), and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044708), and the John W. Alden Trust. Preparation of the current report was funded by a grant from Shire Pharmaceuticals to investigate the long-term effects of ADHD on the later onset of secondary comorbid disorders. Neither Shire nor any of the other funders of the larger WMH Survey Initiative played any role in defining the research question, carrying out the analysis, interpreting the results, writing the paper, or approving g the paper for submission, although one of the collaborators in the workgroup that supervised the analysis and wrote the report (Russo) is a Shire employee.
Role of the Sponsors: The sponsors had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; and the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr. Kessler had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: As noted above, support for the WMH Surveys was obtained from a variety of government agencies, academic institutions, foundations, and private companies. In addition, Dr. Andrade received partial research support for the São Paulo Megacity Mental Health Survey from Eli Lilly & Company, Brazil. Dr. Kessler has been a consultant for GlaxoSmithKline Inc., Kaiser Permanente, Pfizer Inc., Sanofi-Aventis, Shire Pharmaceuticals, and Wyeth-Ayerst; has served on advisory boards for Eli Lilly & Company, Johnson & Johnson Pharmaceuticals, and Wyeth-Ayerst; and has had research support for his epidemiological studies from Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Johnson & Johnson, Ortho-McNeil, Pfizer, and Sanofi-Aventis. Dr. Lepine has served on advisory boards for Wyeth Ayerst, Sanofi Aventis and Pope TBI and has had research support from Eli Lilly and Pfizer. Dr. Russo is an employee of Shire Pharmaceuticals. Dr. Stein has received research grants and/or consultancy honoraria from Astrazeneca, Eli Lilly, GlaxoSmithKline, Johnson & Johnson, Lundbeck, Orion, Pfizer, Pharmacia, Roche, Servier, Solvay, Sumitomo, Tikvah, and Wyeth-Ayerst. The remaining authors report nothing to disclose.
References
- 1.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Angermeyer MC, Bernert S, de Girolamo G, Morosini P, Polidori G, Kikkawa T, Kawakami N, Ono Y, Takeshima T, Uda H, Karam EG, Fayyad JA, Karam AN, Mneimneh ZN, Medina-Mora ME, Borges G, Lara C, de Graaf R, Ormel J, Gureje O, Shen Y, Huang Y, Zhang M, Alonso J, Haro JM, Vilagut G, Bromet EJ, Gluzman S, Webb C, Kessler RC, Merikangas KR, Anthony JC, Von Korff MR, Wang PS, Brugha TS, Aguilar-Gaxiola S, Lee S, Heeringa S, Pennell BE, Zaslavsky AM, Ustun TB, Chatterji S. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 4.Beesdo-Baum K, Höfler M, Gloster A, Klotsche J, Lieb R, Beauducel A, Bühner M, Kessler RC, Wittchen HU. The structure of common mental disorders: a replication study in a community sample of adolescents and young adults. Int J Methods Psychiatr Res. 2009;18(4):204–220. doi: 10.1002/mpr.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox BJ, Swinson RP. Instrument to assess depersonalization-derealization in panic disorder. Depress Anxiety. 2002;15(4):172–175. doi: 10.1002/da.10051. [DOI] [PubMed] [Google Scholar]
- 6.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, Garriock HA, Chapman DA, Waldman ID. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. J Abnorm Child Psychol. 2008;36(2):187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- 8.Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychol Med. 2006;36(11):1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- 9.Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58(6):597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 10.Andrews G, Goldberg DP, Krueger RF, Carpenter WT, Hyman SE, Sachdev P, Pine DS. Exploring the feasibility of a meta-structure for DSM-IV and ICD-11: could it improve utility and validity? Psychol Med. 2009;39(12):1993–2000. doi: 10.1017/S0033291709990250. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg DP, Krueger RF, Andrews G, Hobbs MJ. Emotional disorders: cluster 4 of the proposed meta-structure for DSM-IV and ICD-11. Psychol Med. 2009;39(12):2043–2059. doi: 10.1017/S0033291709990298. [DOI] [PubMed] [Google Scholar]
- 12.Krueger RF, Markon KE. Understanding Psychopathology: Melding Behavior Genetics, Personality, and Quantitative Psychology to Develop an Empirically Based Model. Curr Dir Psychol Sci. 2006;15(3):113–117. doi: 10.1111/j.0963-7214.2006.00418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson D. Rethinking the mood and anxiety disorders: a quantitative hierarchical model for DSM-V. J Abnorm Psychol. 2005;114(4):522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- 14.Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychol Med. 2010;40(2):273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- 15.Kramer MD, Krueger RF, Hicks BM. The role of internalizing and externalizing liability factors in accounting for gender differences in the prevalence of common psychopathological syndromes. Psychol Med. 2008;38(1):51–61. doi: 10.1017/S0033291707001572. [DOI] [PubMed] [Google Scholar]
- 16.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol. 1998;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 17.Wittchen HU, Beesdo-Baum K, Gloster A, Höfler M, Klotsche J, Lieb R, Beauducel A, Bühner M, Kessler RC. The structure of mental disorders re-examined: is it developmentally stable and robust against additions? Int J Methods Psychiatr Res. 2009;18(4):189–203. doi: 10.1002/mpr.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: results of a 25-year longitudinal study. Drug Alcohol Depend. 2007;88 (Suppl 1):S14–26. doi: 10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Stein MB, Fuetsch M, Muller N, Hofler M, Lieb R, Wittchen HU. Social anxiety disorder and the risk of depression: a prospective community study of adolescents and young adults. Arch Gen Psychiatry. 2001;58(3):251–256. doi: 10.1001/archpsyc.58.3.251. [DOI] [PubMed] [Google Scholar]
- 20.Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- 21.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 23.Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. J Consult Clin Psychol. 1996;64(3):552–562. [PubMed] [Google Scholar]
- 24.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- 25.Jensen PS. Comorbidity and child psychopathology: recommendations for the next decade. J Abnorm Child Psychol. 2003;31(3):293–300. doi: 10.1023/a:1023281513936. [DOI] [PubMed] [Google Scholar]
- 26.Geller DA, Biederman J, Griffin S, Jones J, Lefkowitz TR. Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 1996;35(12):1637–1646. doi: 10.1097/00004583-199612000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Thomsen PH, Jensen J. Latent class analysis of organic aspects of obsessive-compulsive disorder in children and adolescents. Acta Psychiatr Scand. 1991;84(4):391–395. doi: 10.1111/j.1600-0447.1991.tb03165.x. [DOI] [PubMed] [Google Scholar]
- 28.Hoehn-Saric R, Barksdale VC. Impulsiveness in obsessive-compulsive patients. Br J Psychiatry. 1983;143:177–182. doi: 10.1192/bjp.143.2.177. [DOI] [PubMed] [Google Scholar]
- 29.Matsunaga H, Kiriike N, Matsui T, Oya K, Okino K, Stein DJ. Impulsive disorders in Japanese adult patients with obsessive-compulsive disorder. Compr Psychiatry. 2005;46(1):43–49. doi: 10.1016/j.comppsych.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 30.Chamberlain SR, Blackwell AD, Fineberg NA, Robbins TW, Sahakian BJ. The neuropsychology of obsessive compulsive disorder: the importance of failures in cognitive and behavioural inhibition as candidate endophenotypic markers. Neurosci Biobehav Rev. 2005;29(3):399–419. doi: 10.1016/j.neubiorev.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York, NY: Cambridge University Press; 2008. [Google Scholar]
- 32.Heeringa SG, Wells EJ, Hubbard F, Mneimneh ZN, Chiu WT, Sampson NA, Berglund PA. Sample designs and sampling procedures. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global perspectives on the epidemiology of mental disorders. New York, NY: Cambridge University Press; 2008. pp. 14–32. [Google Scholar]
- 33.Kessler RC, Üstün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harkness J, Pennell BE, Villar A, Gebler N, Aguilar-Gaxiola S, Bilgen I. Translation procedures and translation assessment in the World Mental Health Survey Initiative. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global perspectives on the epidemiology of mental disorders. New York, NY: Cambridge University Press; 2008. pp. 91–113. [Google Scholar]
- 35.Pennell B-E, Mneimneh Z, Bowers A, Chardoul S, Wells JE, Viana MC, Dinkelmann K, Gebler N, Florescu S, He Y, Huang Y, Tomov T, Vilagut G. Implementation of the World Mental Health Surveys. In: Kessler RC, Üstün TB, editors. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York, NY: Cambridge University Press; 2008. [Google Scholar]
- 36.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, Wang P, Zaslavsky A, Zheng H. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13(2):122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 38.Knäuper B, Cannell CF, Schwarz N, Bruce ML, Kessler RC. Improving accuracy of major depression age-of-onset reports in the US National Comorbidity Survey. Int J Methods Psychiatr Res. 1999;8(1):39–48. [Google Scholar]
- 39.Efron B. Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc. 1988;83:414–425. [Google Scholar]
- 40.Willett JB, Singer JD. Investigating onset, cessation, relapse, and recovery: why you should, and how you can, use discrete-time survival analysis to examine event occurrence. J Consult Clin Psychol. 1993;61(6):952–965. doi: 10.1037//0022-006x.61.6.952. [DOI] [PubMed] [Google Scholar]
- 41.SAS Institute Inc. SAS/STAT® Software, Version 9.1 for Windows. Cary, NC: SAS Institute Inc; 2002. [Google Scholar]
- 42.Shaffer JP. Multiple Hypothesis Testing. Ann Rev Psychology. 1995;46:561–584. [Google Scholar]
- 43.Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316(7139):1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wolter KM. Introduction to Variance Estimation. New York: Springer-Verlag; 1985. [Google Scholar]
- 45.Kass RE, Raftery AE. Bayes factors. J Am Stat Assoc. 1995;90:773–795. [Google Scholar]
- 46.Wittchen HU. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 47.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Simon GE, VonKorff M. Recall of psychiatric history in cross-sectional surveys: implications for epidemiologic research. Epidemiol Rev. 1995;17(1):221–227. doi: 10.1093/oxfordjournals.epirev.a036180. [DOI] [PubMed] [Google Scholar]
- 50.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang PS, Angermeyer M, Borges G, Bruffaerts R, Tat Chiu W, GDEG, Fayyad J, Gureje O, Haro JM, Huang Y, Kessler RC, Kovess V, Levinson D, Nakane Y, Oakley Brown MA, Ormel JH, Posada-Villa J, Aguilar-Gaxiola S, Alonso J, Lee S, Heeringa S, Pennell BE, Chatterji S, Ustun TB. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):177–185. [PMC free article] [PubMed] [Google Scholar]
- 52.Krueger RF, Finger MS. Using item response theory to understand comorbidity among anxiety and unipolar mood disorders. Psychol Assess. 2001;13(1):140–151. [PubMed] [Google Scholar]
- 53.Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112(3):437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- 54.Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: Patterns of lifetime liability from mid-adolescence through early adulthood. J Abnorm Psychol. 2009;118(4):699–710. doi: 10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Helfritz L, Stanford M. Personality and psychopathology in an impulsive aggressive college sample. Aggressive Behav. 2006;32(1):28–37. [Google Scholar]
- 56.Sher KJ, Trull TJ. Personality and disinhibitory psychopathology: alcoholism and antisocial personality disorder. J Abnorm Psychol. 1994;103(1):92–102. doi: 10.1037//0021-843x.103.1.92. [DOI] [PubMed] [Google Scholar]
- 57.Herpertz SC, Mueller B, Qunaibi M, Lichterfeld C, Konrad K, Herpertz-Dahlmann B. Response to emotional stimuli in boys with conduct disorder. Am J Psychiatry. 2005;162(6):1100–1107. doi: 10.1176/appi.ajp.162.6.1100. [DOI] [PubMed] [Google Scholar]
- 58.Sterzer P, Stadler C, Krebs A, Kleinschmidt A, Poustka F. Abnormal neural responses to emotional visual stimuli in adolescents with conduct disorder. Biol Psychiatry. 2005;57(1):7–15. doi: 10.1016/j.biopsych.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 59.Marshall RD, Garakani A. Psychobiology of the acute stress response and its relationship to the psychobiology of post-traumatic stress disorder. Psychiatr Clin North Am. 2002;25(2):385–395. doi: 10.1016/s0193-953x(01)00005-3. [DOI] [PubMed] [Google Scholar]
- 60.Orr SP, Roth WT. Psychophysiological assessment: clinical applications for PTSD. J Affect Disord. 2000;61(3):225–240. doi: 10.1016/s0165-0327(00)00340-2. [DOI] [PubMed] [Google Scholar]
- 61.Kim EY, Miklowitz DJ. Childhood mania, attention deficit hyperactivity disorder and conduct disorder: a critical review of diagnostic dilemmas. Bipolar Disord. 2002;4(4):215–225. doi: 10.1034/j.1399-5618.2002.01191.x. [DOI] [PubMed] [Google Scholar]
- 62.Wingo AP, Ghaemi SN. A systematic review of rates and diagnostic validity of comorbid adult attention-deficit/hyperactivity disorder and bipolar disorder. J Clin Psychiatry. 2007;68(11):1776–1784. doi: 10.4088/jcp.v68n1118. [DOI] [PubMed] [Google Scholar]
- 63.Galanter CA, Leibenluft E. Frontiers between attention deficit hyperactivity disorder and bipolar disorder. Child Adolesc Psychiatr Clin N Am. 2008;17(2):325–346. viii–ix. doi: 10.1016/j.chc.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 64.Hegerl U, Himmerich H, Engmann B, Hensch T. Mania and attention-deficit/hyperactivity disorder: common symptomatology, common pathophysiology and common treatment? Curr Opin Psychiatry. 2010;23(1):1–7. doi: 10.1097/YCO.0b013e328331f694. [DOI] [PubMed] [Google Scholar]