Abstract
Objective
People living in rural areas have the same incidence of mental illness but far less access to mental health services compared with people living in urban areas. This brief report describes the workforce of advanced-practice psychiatric nurses (APPNs) and explores their potential to ease the rural mental health workforce shortage.
Methods
National certification data were used to describe workforce characteristics and the rural distribution of APPNs. All nationally certified APPNs in 2003 were included (N=8,751).
Results
APPNs were more likely than psychiatrists to live in rural areas. The ratio of APPNs to state rural populations ranged from .06 to 14.9. The mean±SD ratio of APPNs per 100,000 in the rural population was 3.0±3.0.
Conclusions
APPNs have great potential to be a solution to the rural mental health workforce shortage. Even so, the number of APPNs must increase and barriers to their full scope of practice must be removed.
Rurally dwelling Americans have the same incidence of mental illness as urban dwellers (1,2). However, rural access to any type of mental health providers is severely limited (1). This disparity is due largely to the shortage and uneven distribution of mental health providers (2). A multidisciplinary group called the Annapolis Coalition performed a comprehensive analysis of the state of the behavioral health workforce. Subsequently they proposed a national strategic workforce plan (3). Improving the documentation about the workforce of rural mental health professionals was cited as an area needing urgent attention.
Although advanced-practice psychiatric nurses (APPNs) have long been providers of a full spectrum of mental and behavioral health services, little is known about them. This research describes workforce characteristics and the rural distribution of APPNs, thereby assembling essential workforce data that can be used to support the national strategic behavioral health workforce plan.
APPNs hold a minimum of a master’s degree in psychiatric mental health nursing. The graduate education of an APPN builds upon an undergraduate degree in nursing. APPN education is based on competencies outlined in a document called the Psychiatric–Mental Health Nursing Scope and Standards of Practice (4). The competencies concern advanced assessment, diagnosis, and treatment of mental health problems and complex psychiatric conditions. APPNs integrate biological, emotional, and social factors when interpreting mental health problems and major psychiatric conditions. APPNs base their plans of treatment on client strengths to optimize clients’ capacity for self-care management of their illness and recovery. Some APPNs go further to obtain specialty education in the management of diabetes and other chronic illnesses that are common among people with serious mental illness (5). Moreover, APPNs have specialized education in various types of psychotherapy, psychopharmacology, and complementary treatments (4). In 36 states, these nurses are authorized to prescribe psychotropic medication (6).
Methods
A secondary analysis was conducted of 2003 data for all 8,751 nationally certified APPNs. Data were provided by the American Nurses Credentialing Center (ANCC). According to the National Nurse Survey 2004, the total number of APPNs is estimated to be between 16,000 and 20,000 (7). The reason that only half of APPNs are nationally certified is because they work in institutions, such as hospitals, that do not always require certification. Even so, most state regulation of APPNs requires national certification, particularly if prescription rights are authorized. ANCC offers board certification by age group treatment specialty, including children, adolescents, families, and adults. For example, 11% of APPNs are board certified as child and adolescent clinical nurse specialists or child and family psychiatric nurse practitioners. However, a large majority (84%) of the credentialed APPNs are certified to work with the adult population (7).
ANCC data are from the application process (8). To be eligible for the ANCC exam, the psychiatric nurse must be a registered nurse in the United States and hold a master’s or doctoral degree in nursing from a nationally accredited university. In addition, candidates must show they have met a minimum of 500 hours of clinically supervised practice in psychiatric mental health care (8). For this research, the data were deidentified to meet requirements for exempt status from the institutional review board of the University of Pennsylvania.
Analysis included a description of the APPN workforce characteristics and rural distribution. The APPN’s home zip code was matched with rural categories defined by the 1990 zip code version of Rural-Urban Commuting Areas (9). Unfortunately, work zip codes were not available, which poses a limitation, because many APPNs may live in rural areas but not work in them. At this time, however, no better data exist. Next, we calculated the ratio of APPNs to 100,000 rural residents by state, using state fact sheets found on the U.S. Department of Agriculture’s Economic Research Service site, www.ers.usda.gov/statefacts.
Results
The APPNs in the sample worked an average of 16–20 years as registered nurses, and more than a quarter of these nurses reported specializing in psychiatric mental health care for over 30 years. Ninety-five percent were female, and 81% were white. The mean±SD age of APPNs in the sample was 51.3±8.4 years. A total of 6,563 APPNs (75%) were employed fulltime. Most were employed by hospitals (3,154 APPNs, or 36%), solo practitioners (1,554, or 18%), or home health agencies (1,092, or 13%). Other settings, in descending frequency, included group practice, ambulatory care, public health, office nurse, managed care, school of nursing, nursing home, nurse managed practice, school health, hospice, and occupational health. A total of 7,759 APPNs (89%) listed one place of employment, 1,377 (16%) listed two places, and 375 (4%) listed three places. Among those who were working in facilities, a majority worked in institutions with 101–500 beds. These nurses had varying titles, positions, and responsibilities, including 4,357 clinical specialists (50%), 1,209 nurse practitioners (14%), 968 consultants (11%), 391 nurse managers (9%), 749 staff nurses (9%), and 648 researcher-educators (7%). A total of 7,367 APPNs (80%) reported supervising other clinicians.
Broadly, 13% of all APPNs in the sample lived in rural areas, compared with 7% of all psychiatrists living in rural areas (10). The highest ratio of APPNs was found in Massachusetts (14.8 per 100,000 rural population), then Hawaii (11.7), Vermont (10.9), New Hampshire (8.7), Maine (8.5), Connecticut (6.4), and Maryland (5.0). Figure 1 shows a map of the ratio of rurally dwelling APPNs to 100,000 in the rural population by state. The New England area and Hawaii had the highest density of APPNs in rural populations. The northern states had the second highest density of APPNs in rural areas, and the southern states had the lowest density. The ratio of APPNs to 100,000 rural population ranged from .06 to 14.9. The mean ratio of APPNs per 100,000 rural population was 3.0±3.0 at the state level. The five states with the highest proportion of rurally dwelling APPNs were Vermont (77%), Wyoming (67%), Montana (65%), South Dakota (50%), and Arkansas (48%). When compared with total rural population by state, Vermont and Maine had the highest proportion of rural population (62% and 60%, respectively) and the highest ratio of APPNs to 100,000 in the rural population, 10.9 and 8.5, respectively. In 20 states, rural APPNs accounted for 20% or fewer of all APPNs practicing in those states.
Figure 1.
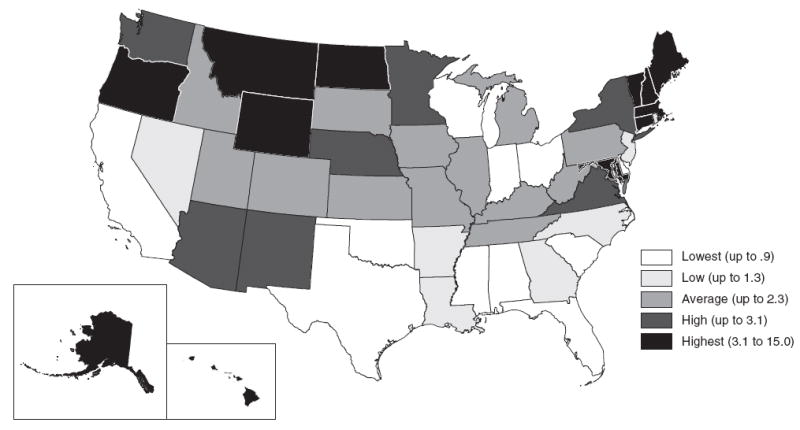
Density (per 100,000 rural population) of advanced-practice psychiatric nurses in rural populations in the United States
Discussion
Unfortunately, APPNs account for a very small portion of the total mental health workforce. Although our data indicate a total of 8,751 nationally certified APPNs practicing in the United States, there are an estimated 38,258 psychiatrists, 76,968 psychologists, and 96,268 social workers (11). Using the ratio of providers per 100,000 population, for the nation as a whole, current estimates are 11.3 psychiatrists, 27.5 psychologists, and 36.2 social workers. Nationally there are 3.11 APPNs per 100,000 population. Another troubling fact is that the average age of an APPN is 52 years, which means that without an infusion of new graduates, the APPN workforce could become significantly thinner in the next ten to 25 years. Even so, aging is pronounced in all the core mental health disciplines. For example, the average age of a psychiatrist is 55 years, and almost 18% are age 69 years or older (11).
This study focused on APPNs because so little information about them was available. But more needs to be done to increase the number of these practitioners to improve access to behavioral health services in rural areas. In the late 1960s and early 1970s, graduate education was funded for psychiatric nurses and resulted in a large infusion of APPNs in the workforce. Regrettably, this federal funding was discontinued in the early 1980s and was followed by a decline in enrollment. Federal education funding works and would work again to attract APPNs to specialize in mental health. In addition, we recommend a reimbursement differential under Medicare and Medicaid for those practicing in areas designated to have a shortage of mental health professionals, as well as loan repayment programs under the National Health Service Corps or similar state programs (12).
Other incentives for encouraging APPN workforce growth should be considered. Currently, wide variations exist in the titling and credentialing of APPNs among states. The result is confusion about the scope and practice of these nurses and significant barriers to practice. We recommend consistent regulatory language, titling, and scope of practice among the states.
Conclusions
It is prudent and cost-effective to build on the strengths of the existing workforce when developing a strategic plan to address workforce shortages. Nurses have long provided community health services, often when access to any other providers is limited. APPNs may be well suited to rural realities and primary care practices. Because of their breadth of training and scope of practice, APPNs may well be the ideal rural mental health professionals.
Acknowledgments
Major support for this study came from the Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, under National Institute for Nursing Research grants P30-NR-005043 and T32-NR-007104 (Linda H. Aiken, Ph.D., R.N., principal investigator for both). This study was funded in part by grant 4-UIC-RH-00013-04-05 from the federal Office of Rural Health Policy, Health Resources and Services Administration of the Department of Health and Human Services. The authors acknowledge Benjamin Dubow from Urban Studies at the University of Pennsylvania for his GIS mapping expertise. The conclusions and opinions expressed in this report are the authors’, and no endorsement by the University of Southern Maine or the funding source is intended or should be inferred.
Footnotes
disclosures
The authors report no competing interests.
Contributor Information
Nancy P. Hanrahan, Center for Health Outcomes and Policy Research, University of Pennsylvania School of Nursing, Claire Fagin Hall, 418 Curie Blvd., Philadelphia, PA 19104 (nancyp@nursing.upenn.edu)
David Hartley, Maine Rural Health Research Center, University of Southern Maine, and the Institute for Health Policy, Edmund S. Muskie School of Public Service, both in South Portland, Maine
References
- 1.Subcommittee on Rural Issues: Background Paper. Rockville, Md: President’s New Freedom Commission on Mental Health; 2004. [Google Scholar]
- 2.National Institute of Medicine Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders: Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 3.Hoge MA, Morris JA, Daniels AS, et al. An Action Plan for Behavioral Health Workforce Development. Cincinnati, Ohio: Annapolis Coalition on the Behavioral Health Workforce; 2007. [Google Scholar]
- 4.Psychiatric–Mental Health Nursing Scope and Standards of Practice. Silver Spring, Md: American Nurses Association; 2007. Available at www.nursebooks.org. [Google Scholar]
- 5.Kessler RC, Demler O, Frank RG, et al. Prevalence and treatment of mental disorders, 1990–2003. New England Journal of Medicine. 2005;352:2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Staten RR, Hamera E, Hanrahan NP, et al. Advanced practice psychiatric nurses: 2005 legislative update. Journal of the American Psychiatric Nurses Association. 2006;11:371–382. [Google Scholar]
- 7.Health Resources and Services Administration: National Sample Survey of Registered Nurses March 2004. Available at bhpr.hrsa.gov/healthworkforce/reports/rnpopulation/preliminaryfindings.htm.
- 8.National Certification Data for Psychiatric Nurses. Rockville, Md: American Nurses Credentialing Center; Oct, 2006. [Google Scholar]
- 9.Hart GL. Uses of RUCAS in health services research. Presented at the Academy Health Annual Conference; Seattle, Wash. June 2006; Available at depts.washington.edu/uwruca/new.html. [Google Scholar]
- 10.Hartley D, Britain C, Sulzbacher S. Behavioral health: setting the rural health research agenda. Journal of Rural Health. 2002;18(suppl):242–255. doi: 10.1111/j.1748-0361.2002.tb00934.x. [DOI] [PubMed] [Google Scholar]
- 11.West J, Kohout J, Pion G, et al. In: Mental health practitioners and trainees, in Mental Health Statistics, 2004. Mandersheid RW, editor. Rockville, Md: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 2006. [Google Scholar]
- 12.Hartley D. Rural health disparities, population health, and rural culture. American Journal of Public Health. 2004;94:1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]


