Abstract
Background
Cardiovascular deaths among on-duty firefighters are high; double that of police officers and quadruple that of first responders. The aim of this pilot study was to establish the feasibility of obtaining high resolutions ECGs of on-duty firefighters useful for detecting ECG predictors for cardiac events.
Methods
Twenty-eight professional firefighters (age, 46 ± 6 years) wore a 12-lead ECG Holter for 24 hours (16 hours while on-duty and 8 hours post-duty). All activities including fire and medical calls were monitored.
Results
On average the recordings were 92% analyzable. All were in sinus with a heart rate of 80 ±11bpm (35–188 range). The average rr50 over the 24-hour Holter study was 6.2 ±6% (range: 1–23%) and rms-SD was 81 ± 55 (range: 24–209). Using the QRS/Tsimple formula, the average spatial QRS-T angle was 104 ±17 degrees (range 78–132 degrees). Nonsustained ventricular tachycardia occurred irrespectively of activity or time of day in three (11%) firefighters, which was significantly higher than in comparable normal populations (p<0.05).
Conclusions
This preliminary work demonstrates that it is feasible to obtain high resolution ECGs during firefighting activities and further points to the high prevalence of arrhythmias among firefighters. The strategy of continuous field monitoring of firefighters could provide new insight into the association between their specific professional lifestyle and high cardiac risks.
Keywords: 12-lead ECG, firefighter, (sudden) cardiac death, Holter, nonsustained ventricular tachycardia
Despite their superior physical condition at hire, firefighters are professionally at high risk for serious cardiac events including sudden death. In 2005, the National Fire Protection Association (NFPA) reported that 44% of on-duty firefighter fatalities were due to sudden cardiac death 1. In a recent study, Kales and colleagues 2 confirmed that 42% of firefighter deaths occurring while on-duty were cardiac-related, so that many are actually dying of cardiac disease rather than fire-related injuries. The incidence of cardiac deaths among on-duty firefighters is so elevated that it is twice that of police officers and four times that among emergency medical responders 3. It is also triple that of all job related cardiac deaths 1. The cardiac death risk during fire suppression activities is greatest: one to two orders of magnitude higher than during nonemergency activities 2. The only recourse for sudden cardiac death is immediate cardiac defibrillation and resuscitation. However, not all events (e.g., myocardial infarction) result in death due to the availability of timely care 4. Thus, although many firefighters actually survive on-duty cardiac events their resulting incidence of cardiac morbidity remains exceptionally high.
In the case of firefighters, a combination of personal and workplace factors contribute to coronary artery disease (CAD). As in the general population, firefighters’ personal factors include: age, sex, family history, diabetes mellitus, hypertension, smoking, high blood cholesterol, obesity, elevated stress and lifestyle 5. In addition however, numerous workplace factors unique to firefighters substantially contribute to adverse cardiac outcomes. These include: a) airborne exposure to fumes, carbon monoxide and other hazardous chemicals which lead to hypoxia and cellular ischemia, b) inhalation of particulate matter creating hypoxic conditions which results in myocardial infarction or CAD, c) sustained elevated heart rates and heavy physical exertion, d) heat stress which results in dehydration and lower stroke volume 6, 7, v) high noise levels 8 and long hour shift work 9 which favor hypertension and lead to myocardial ischemia and CAD, and e) still second-hand tobacco exposure in some fire houses which leads to vasoconstriction and CAD 10. Notably, a large portion of the firefighters’ shift is spent in a Ready State. Although the Ready State may be a physically resting state, mentally firefighters must remain on alert for rapid all out deployment. Overall, the unpredictable and extreme pattern of alternating sedentary periods with intense exertion and stress puts firefighters at increased risk for acute cardiac events because sudden heavy physical exertion is known to immediately precede and trigger cardiac events 11–13.
Although firefighters begin their career in superior health due to their relative youth and physical requirements at hire, there is no national mandate for them to maintain their initial good health. The National Institute for Occupational Safety and Health (NIOSH) clearly recommends that fire departments establish medical screening guidelines and develop comprehensive wellness/fitness programs 10. The National Fire Protection Association, Standard on Comprehensive Occupational Medical Program for Fire Departments states that firefighters require annual medical evaluation because sudden cardiac death has a significant correlation with a known presence of heart disease in those who were fit for duty 14. Because firefighting taxes virtually all aspects of physical fitness, researchers further recommend replacing traditional firefighter exercise programs that focus on cardiovascular fitness with physical conditioning programs that address all components of fitness 15. Despite such clear recommendations and repeated efforts to implement firehouse fitness programs, firefighters’ prevalence of obesity, elevated total serum cholesterol, lowered high-density lipoprotein, elevated low-density lipoprotein, and elevated blood pressures exceed Healthy People 2010 targets and are substantially higher than the general population 16. Thus, health promotion programs for firefighters are failing 17, 18. Long term efforts clearly need to focus on efficient and targeted modes of intervention. One approach could be to first identify specific firefighters at most risk of a cardiac event to better target modifiable risk factors to reduce catastrophic cardiac events such as sudden death and myocardial infarction.
The 12-lead electrocardiogram (ECG) is an invaluable noninvasive tool to assess and monitor cardiac status and predict cardiac events 19, 20. With the recent availability of sophisticated portable recorders, high resolution ECG recordings can now be continuously collected in nearly any settings. To date, despite the long established cardiac risk for on-duty firefighters especially during emergency activities and its societal importance, there are no available field data recordings of the ECG during firefighter activities. Thus, the primary aim of this prospective pilot study was to evaluate the feasibility of obtaining high resolution continuous ECG tracings in on-duty firefighters to monitor ECG predictors for cardiac events which will be useful to better target cardiovascular disease prevention and care.
Methods
Professional firefighters (n=28) were recruited from the Buffalo New York Fire Department to wear a standard 12-lead ECG Holter (H12+ Digital Holter Recorder, Mortara Instruments, Milwaukee, WI) continuously for 24 hours. Per the Fire Commissioner’s assignment, recruiting occurred at the largest firehouse in Buffalo with three fire apparatus: pumper, ladder and rescue engine. Any professional firefighter engaged in firefighting duty was eligible; there were no exclusions. Appropriate internal review board approval was obtained. Monitoring was initiated at the beginning of their 16-hour on-duty shift and continued for the following 8 post-duty hours, during the winter months. Prior to the monitoring, firefighters were consented and prepped to wear the ten electrodes underneath their uniformed T-shirts connected to the Holter recorder strapped in a pouch. Skin prep included shaving chest hair as needed and the removal of oil or dermal debris with alcohol. The electrodes were accurately positioned as per Mason Likar 21, without the use of additional adhesives. Due to the diaphoretic nature of firefighting, electrode contact and location was routinely checked to ensure accurate monitoring. On the occasion that an electrode failed or was inadvertently disconnected, the Holter recorder continued to record despite missing leads and the electrode was replaced in a timely manner. During the study, firefighters were regularly prompted to report any symptom.
The various activities the firefighters were engaged in during their 16-hour shifts were catalogued into the following emergency categories: (1) Fire calls, (2) Medical calls, and non emergency categories: (3) Physical activities (e.g., exercise, training, physical chores, etc), (4) Sitting/Talking (e.g., shift report, instruction, administration, etc), (5) Meals, and (6) Rest/Sleep. Post-duty activities were also catalogued into the same nonemergency categories according to a questionnaire completed by the post-duty firefighter.
Computer automation with the H-Scribe™ software (Mortara Instruments, Milwaukee, WI) was used for interval measurements of the ECG waveforms; however cardiac rhythms were manually annotated to assess for artifact and subtle vector changes related to ambulatory monitoring by an expert investigator with over 15 years of experience in electrocardiography. All firefighters were given a written summary of their main Holter study statistics, including average, minimum and maximum heart rates and dominate cardiac rhythm. In the case where the firefighter exhibited an abnormal ECG, a written letter summarizing the concern in lay terms and encouraging the firefighter to contact his personal physician was provided.
Statistical Analyses
When appropriate, results are given as mean ± standard deviation. Statistical significance for the greater occurrence of NSVT events was calculated according to the t-test for unequal variances. The degree of association between heart rate variability (HRV) measures and age was determined using the correlation coefficient (r2). P < 0.05 was considered statistically significant.
Results
The present pilot study monitored twenty-eight (n=28) firefighters continuously for 24 hours. Some recordings were shorter because the firefighter opted out of the monitoring at some point during post-duty for personal reasons. However, except in two instances where injuries occurred or the Holter was crushed, it was possible to maintain ECG monitoring during the entire 16-hour shift including all emergency calls. Overall firefighters were receptive to recruitment, and even more so at the end of the enrollment period, which showed that the Holter monitoring was well tolerated.
On average, only 8% of the recordings were unsuitable for analysis with ECG waveforms so poor that QRS complexes were not interpretable. Not surprisingly, the incidence of poor signal increased during intense activity (i.e., fire and medical call and physical activity), although most tracings remained analyzable.
Only male firefighters volunteered for the study, the majority white (69%), and with an average age of 46 ±6 (range: 35–56 years). On average, heart rates were 80 ±11 beats per minute (bpm) and ranged from bradycardia to tachycardia (35–188 bpm). The lowest heart rate was observed in an accomplished triathlete. The higher heart rates were all observed during the physically demanding activities.
Cardiac Abnormalities (arrhythmias & ST segment deviation)
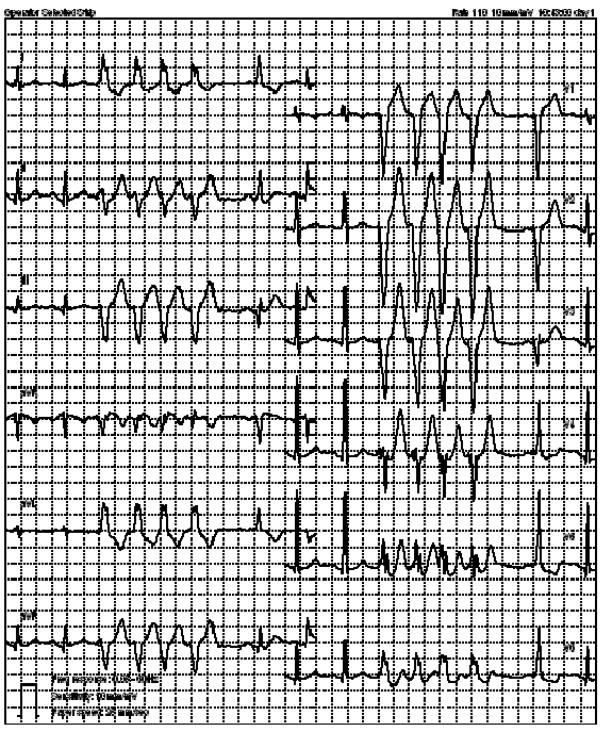
Overall, 16 (57%) of the firefighters had at least one premature ventricular contraction. Nonsustained ventricular tachycardia (NSVT) was defined as three or more consecutive beats emanating from the ventricles at a rate greater than 100 beats per minute (bpm) and terminating spontaneously within 30 seconds. Six episodes of NSVT occurred in three (11%, Table 1) and all events were both monomorphic and asymptomatic, an example is presented in Figure 1. Two firefighters had NSVT composed of four or more beats while the third firefighter only had triplets. The potential dependence of these arrhythmic events on the firefighter’s activity or circadian factors was examined. The NSVT distribution in function of activity revealed no such dependence within this relatively small sample size (Table 2). The majority of NSVT indeed occurred during Sitting/Talking activities which covered nearly half of the monitoring time. Further, one of six (13%) NSVT events took place during emergency activities which also totaled 13% of total firefighters’ activities. The periods between emergencies spent in a ‘Ready-State’ thus comprised the greater majority of the firefighters’ time (87%). Finally, the distribution of NSVT as a function of time period occurrence also did not show any substantial trend (Table 2).
Table 1.
Firefighters with Non Sustained Ventricular Tachycardia (NSVT) Events
| Firefighter | Age | Heart Rate (bpm) | NSVT (number) | |
|---|---|---|---|---|
| average | range | |||
| 1 | 53 | 66 | 45–132 | 3 |
| 2 | 54 | 86 | 47–171 | 2 |
| 3 | 42 | 72 | 42–113 | 1 |
bpm=beats per minute
Figure 1.
Nonsustained Ventricular Tachycardia, on-duty firefighter during Ready State.
Table 2.
Activity and Circadian Distribution of NSVT Events (n=6)
| Activity | Circadian* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fire | Medical | Physical | Sit/Talk | Meals | Rest/Sleep | Morn (06–12) | After (12–18) | Eve (18–24) | Night (00–06) | |
| Percent Time | 7 | 6 | 6 | 47 | 10 | 24 | ||||
| NSVT (number) | 1 | 0 | 0 | 4 | 0 | 1 | 2 | 1 | 1 | 2 |
=24 hour clock
Morn= morning
After= afternoon
Eve= evening
ST segment analysis was conducted using each of the ECG lead trends over the 24 hour period. When a suspicious deviation in the trend was noted, the respective 12 lead ECGs were printed (pre event, event, post event) and the automated ST delta values were calculated. Only one suspicious ST segment elevation event in the anterior wall without an accompanying ST-segment depression was recorded during physical activity. However, while the event would have been classified as an ischemic sign earlier, it should be recognized that it did not quite meet the newest electrocardiographic criteria for myocardial ischemia 22.
Heart Rate Variability
Using high resolution 12-lead ECG, heart rate variability (HRV), as measured by the R-R relationship, is another useful electrocardiographic measure that may predict cardiac events in combination with other ECG variables. The computer-generated square root of the mean squared differences of successive NN intervals (rms-SD) and the portion of NN intervals greater than 50 milliseconds (PNN50) were calculated over the Holter study (Figure 1). The average rr50 over the 24-hour Holter study was 6.2 ±6% (range: 1–23%) and rms-SD was 81 ± 55 (range: 24–209). There was a negative correlation between age and the average R–R interval (r=−0.65, p<0.01); however, there was no significant relationship between age and rms-SD (r=−0.05, NS).
Spatial QRS-T angle
An abnormal spatial QRS-T angle has a larger hazard ratio for fatal cardiac events than established cardiovascular and ECG risk factors. The spatial angle between the QRS and T axes is the angle between the directions of ventricular depolarization and repolarization. Although traditionally obtained from orthogonal leads, computer-derived measurements of this spatial alignment can be calculated from a standard 12-lead ECG using: QRS/Tsimple = ACOS {[(QRSnetV6 × TnetV5) + (QRSnetaVF × TnetaVF) + (QRSnetV2 × TnetV2)]/(QRSsm × Tsm)}19. The first 12 lead ECG was selected and on average the spatial QRS-T angle was 104 ±17 degrees (range 78–132 degrees). According to Rautaharju and co workers19 an abnormal QRS-T angle is >114° for men and >97° for women but others 23, categorized QRS-T angle into three groups: normal (0 – 50°), borderline (50 – 100°), and abnormal (100– 180°).
Technical Challenges
A number of technical difficulties were encountered such as: (1) the loss of electrode contact or electrode shift on the diaphoretic torso which was minimized by routine checks, (2) recurring body positional changes on the ECG were identified and eliminated from the analysis as previously described 24, (3) equipment damage and (4) 60-cycle artifact. Such electrical interference was not surprising given the additional equipment firefighters wear, on occasion. However, a definite advantage of recording 12-lead ECG is that despite a lead failure from electrical interference, other leads remained available for analysis.
Discussion
This preliminary work is the first to report that it is feasible to obtain continuous high resolution 12-lead ECGs from professional firefighters during all of their on-duty activities. Such capability should allow future researchers to prospectively study the various ECG parameters in order to better understand the relationship between the strenuous cardiovascular demands specific to the firefighting lifestyle and electrocardiographic changes of the heart.
The prevalence of NSVT in the healthy general population ranges from 0 to 4% 25, 26. However, it is age-dependent and highest (4%) in seniors (over 60 years) so that the range in healthy adults populations does not exceed 2.3% 26. In contrast, the present pilot study identified an 11% occurrence among on-duty firefighters. This higher prevalence was significantly larger (p<0.05) than in each of the previously-studied groups of similar-aged healthy adults, including the upper occurrence of 2.3% found by the Bjerregaard study (n=260, mean age=54 years, 2/3 males) 27. Although this significantly higher prevalence of firefighters with NSVT will need to be confirmed in a larger study, it still likely points to one of the ECG abnormalities that firefighters are likely to exhibit with some relevance to cardiac disease and their higher cardiac risk while on duty or post-duty. Indeed, the incidence of NSVT is higher in the presence of underlying heart disease, although interpretation caution is in order with the present population since firefighters are medically cleared for duty. Still, the prognosis of NSVT may be ominous because the large, long-term Busselton and Framingham community studies report that ventricular ectopy and NSVT were associated with an approximately three-fold increase in the risk of subsequently developing CAD 28, 29.
Heart rate variability assesses the role of the autonomic nervous system fluctuations. This pilot study establishes that the average rr50 and rms-SD over the 24-hour Holter study is obtainable in active firefighters. Consistent with the literature, we report that the average rr50 interval decreases with age; however, we did not find a relationship between age and rms-SD in this sample but it should be noted that this pilot study was not powered to detect a difference. Future studies can better investigate the relationship between heart rate variabilities during firefighter activities.
Previous cardiac monitoring studies have been directed at firefighters but they have all been limited by the use of just two or three ECG leads and the recording of simple parameters such as heart rate 30, 31. Using a young healthy cohort and limited ECG monitoring (3-lead ECG) Bruce and coworkers 30 evaluated firefighters performing tasks under controlled tasks. When evaluating firefighter heart rate, Heimburg and colleagues found that patient rescue was physically very demanding on firefighters even under simulated conditions 30, 31.
Interestingly, another activity, deer hunting, has been shown to result in sudden sustained rises in heart rate and in excessive cardiac demands during heavy exertion or stressful periods such as the dragging of carcasses or the shooting stage 32. By comparing the 3-lead ECG of deer hunters during actual hunting jaunts to that during maximal treadmill testing, researchers found high heart rates, periods of sustained sinus tachycardia, arrhythmias and ST-segment depression during hunting that were absent during treadmill testing. The report concluded that the strenuous nature of deer hunting coupled with the stress-response contributed to excessive cardiac demands. Similarly to deer hunters, it is likely that firefighters are also experiencing periods of excessive cardiac demands during strenuous activities such as patient rescue, full gear firefighting, etc. However, unlike the occasional nature of deer hunting, firefighting activities are frequent which may result in compounding firefighter cardiac stresses and risks.
Limitations regarding this pilot study include the absence of control for the effect of medications on the ECG. Since all firefighters were cleared for active duty, it was assumed that all medications were likely within therapeutic range. Still, numerous medications can indeed cause primary changes (e.g., beta blockers) or secondary changes on the ECG (e.g., digoxin). Another caveat to consider is the seasonal effect on firefighters’ activities; the present data was collected during the winter in Buffalo NY, a cold snowy North Eastern City. For example, on the second day of data collection a substantial amount of snow fell and the firefighters expanded large efforts shoveling snow, while at the same time snow conditions kept fire calls low. Thus, researchers should consider seasonal effects while monitoring firefighter activities.
As first line responders, firefighters serve all of the nation’s population and their sudden deaths often occur during their most productive years. The societal impact from the sudden loss of such contributing community members is substantial and in addition, they leave their families overwhelmed with loss of income, companionship and support. Due to the disproptionally high incidence of firefighter cardiac events while on-duty or shortly after, the firefighter population is uniquely positioned to provide insight into the association between intense alarm response activities and the high cardiac risk. Continuous 12-lead ECG field monitoring can make this goal attainable by succesful noninvasive detection of firefighters’ ECG abnormalities. This type of research should help develop algorithmic guidelines designed to route at-risk firefighters for optimal cardiac care that would aggressively reduce their modifiable cardiovascular risk factors. Over the longer horizon, the increase understanding of firefighter cardiac risk should, in turn, help advance our understanding of cardiac risk in the general population.
Summary and Implications
Due to the disproptionally high incidence of firefighter cardiac events while on-duty or shortly after, the firefighter population is uniquely positioned to provide insight into the association between intense alarm response activities and the high cardiac risk.
This type of research should help develop algorithmic guidelines designed to route at-risk firefighters for optimal cardiac care that would aggressively reduce their modifiable cardiovascular risk factors.
Over the longer horizon, the increase understanding of firefighter cardiac risk should, in turn, help advance our understanding of cardiac risk in the general population.
Continuous 12-lead ECG Holter monitoring can make this goal attainable by succesful noninvasive detection of ECG abnormalities across many populations.
Acknowledgments
Supported by a Grant from the National Institutes of Health, R21 NR011077
References
- 1.Fahy R. US firefights fatalities due to sudden cardiac death 1995–2004. National Fire Protection Association. National Institute for Occupational Safety and Health (NIOSH); 2005. [Google Scholar]
- 2.Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. N Engl J Med. 2007 Mar 22;356(12):1207–1215. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- 3.Maguire BJ, Hunting KL, Guidotti TL, Smith GS. Occupational injuries among emergency medical services personnel. Prehosp Emerg Care. 2005 Oct–Dec;9(4):405–411. doi: 10.1080/10903120500255065. [DOI] [PubMed] [Google Scholar]
- 4.Mbanu I, Wellenius GA, Mittleman MA, Peeples L, Stallings LA, Kales SN. Seasonality and coronary heart disease deaths in United States firefighters. Chronobiol Int. 2007;24(4):715–726. doi: 10.1080/07420520701535787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.AHA. American Heart Association. [Accessed January 26, 2008];Risk Factors and Coronary Artery Disease. 2007 http://www.americanheart.org/presenter.
- 6.Rossi R. Fire fighting and its influence on the body. Ergonomics. 2003 August 15;46(10):1017–1033. doi: 10.1080/0014013031000121968. [DOI] [PubMed] [Google Scholar]
- 7.Smith D, Manning T, Petruzzello S. Effect of strenuous live-fire drills on cardiovascular and psychological responses of recruit firefighters. Ergonomics. 2001;44(3):244–254. doi: 10.1080/00140130121115. [DOI] [PubMed] [Google Scholar]
- 8.Tubbs R. Noise and hearing loss in firefighting. Occup Med. 1995;10(4):843–856. [PubMed] [Google Scholar]
- 9.Steenland K, Fine L, Belkić K, et al. Research findings linking workplace factors to CVD outcomes. Occup Med. 2000;1(7):7–68. [PubMed] [Google Scholar]
- 10.NIOSH NIfOSaH. National Institute for Occupational Safety and Health. [Accessed January 25, 2008];Preventing Fire Fighter Fatalities Due to Heart Attacks and Other Sudden Cardiovascular Events. 2007 http://www.cdc.gov/niosh/docs/2007-133/
- 11.Willich SN, Lewis M, Lowel H, et al. Physical Exertion as a Trigger of Acute Myocardial Infarction. 1993;329:1684–1690. doi: 10.1056/NEJM199312023292302. [DOI] [PubMed] [Google Scholar]
- 12.Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993 Dec 2;329(23):1677–1683. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- 13.Tofler G, Muller J, Stone P, et al. Modifiers of timing and possible triggers of acute myocardial infarction in the Thrombolysis in Myocardial Infarction Phase II (TIMI II) Study Group. J Am Coll Cardiol. 1992;20:1049–1055. doi: 10.1016/0735-1097(92)90356-r. [DOI] [PubMed] [Google Scholar]
- 14.Association NFP. Dallas. 2003. Standard on Comprehensive Occupational Medical Program for Fire Departments; p. 111. [Google Scholar]
- 15.Rhea M, Alvar B, Gray R. Physical fitness and job performance of firefighters. Journal of Strength & Conditioning Research. 2004;18(2):348–352. doi: 10.1519/R-12812.1. [DOI] [PubMed] [Google Scholar]
- 16.Byczek L, Walton S, Conrad K, Reichelt P, Samo D. Cardiovascular risks in firefighters: implications for occupational health nurse practice. AAOHN. 2004;52(2):66–76. [PubMed] [Google Scholar]
- 17.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999 September 1;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pelletier K. A review and analysis of the clinical- and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: 1993–1995 update. Am J Health Promot. 1996;10:380–388. doi: 10.4278/0890-1171-10.5.380. [DOI] [PubMed] [Google Scholar]
- 19.Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society Scientific Statement on Noninvasive Risk Stratification Techniques for Identifying Patients at Risk for Sudden Cardiac Death: A Scientific Statement From the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation. 2008 September 30;118(14):1497–1518. [PubMed] [Google Scholar]
- 20.Carey M. Electrocardiographic Predictors of Sudden Cardiac Death. J Cardiovasc Nurs. 2008;23(2):175–182. doi: 10.1097/01.JCN.0000305069.64860.51. [DOI] [PubMed] [Google Scholar]
- 21.Mason RE, Likar I. A new system of multiple-lead exercise electrocardiography. Am Heart J. 1966 Feb;71(2):196–205. doi: 10.1016/0002-8703(66)90182-7. [DOI] [PubMed] [Google Scholar]
- 22.Task Force M, Thygesen K, Alpert JS, et al. Universal definition of myocardial infarction: Kristian Thygesen, Joseph S. Alpert and Harvey D. White on behalf of the Joint ESC/ACCF/AHA/WHF Task Force. Redefinition of Myocardial Infarction. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 23.Yamazaki T, Froelicher VF, Myers J, Chun S, Wang P. Spatial QRS-T angle predicts cardiac death in a clinical population. Heart Rhythm. 2005;2(1):73–78. doi: 10.1016/j.hrthm.2004.10.040. [DOI] [PubMed] [Google Scholar]
- 24.Adams MG, Drew BJ. Body position effects on the ECG: implication for ischemia monitoring. J Electrocardiol. 1997 Oct;30(4):285–291. doi: 10.1016/s0022-0736(97)80040-4. [DOI] [PubMed] [Google Scholar]
- 25.Kinder C, Tamburro P, Kopp D, Kall J, Olshansky B, Wilber D. The clinical significance of nonsustained ventricular tachycardia: current perspectives. Pacing Clin Electrophysiol. 1994;17(4 Pt 1):637–664. doi: 10.1111/j.1540-8159.1994.tb02400.x. [DOI] [PubMed] [Google Scholar]
- 26.Fleg J, Kennedy H. Long-term prognostic significance of ambulatory electrocardiographic findings in apparently healthy subjects greater than or equal to 60 years of age. Am J Cardiol. 1992;70(7):748–751. doi: 10.1016/0002-9149(92)90553-b. [DOI] [PubMed] [Google Scholar]
- 27.Bjerregaard P. Premature beats in healthy subjects 40–79 years of age. Eur Heart J. 1982 December 2;3(6):493–503. doi: 10.1093/oxfordjournals.eurheartj.a061344. [DOI] [PubMed] [Google Scholar]
- 28.Cullen K, Stenhouse N, Wearne K, Cumpston G. Electrocardiograms and 13 year cardiovascular mortality in Busselton study. Br Heart J. 1982;47(3):209–212. doi: 10.1136/hrt.47.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bikkina M, Larson M, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham Heart Study. Ann Intern Med. 1992;117(12):990–996. doi: 10.7326/0003-4819-117-12-990. [DOI] [PubMed] [Google Scholar]
- 30.Bruce R, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85:546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- 31.Heimburg Ev, Rasmussen A, Medbø J. Physiological responses of firefighters and performance predictors during a simulated rescue of hospital patients. Ergonomics. 2006;49(2):111–126. doi: 10.1080/00140130500435793. [DOI] [PubMed] [Google Scholar]
- 32.Haapaniemi S, Franklin BA, Wegner JH, et al. Electrocardiographic responses to deer hunting activities in men with and without coronary artery disease. Am J Cardiol. 2007 Jul 15;100(2):175–179. doi: 10.1016/j.amjcard.2007.02.076. [DOI] [PubMed] [Google Scholar]