Abstract
Objective
Describe the clinical and imaging characteristics of spinal cord ring enhancement in multiple sclerosis (MS).
Design
Clinical case series.
Setting
Academic referral center.
Patients
Twenty MS subjects with spinal cord ring enhancement were retrospectively identified from 322 cervical and thoracic spinal cord MRI studies over a 3 year period.
Main Outcome Measures
Demographics, disability, pattern of enhancement on spinal cord imaging, and concomitant brain magnetic resonance imaging (MRI) were determined.
Results
Ring enhancement was seen in 20 subjects with spinal cord enhancement, most commonly in the cervical cord. Incomplete or ‘open’ ring enhancement was the dominant pattern in 19 of 20 (95%) subjects. Concurrent ring enhancing brain lesions were present in 40% of subjects. At the time of the MRI, the Expanded Disability Status Scale (EDSS) ranged from 1.0–7.0 (median 3.0).
Conclusion
Ring enhancement is not an uncommon pattern for MS spinal cord lesions, occurring with a prevalence of 6.2% (20/322). The most common pattern was incomplete ring enhancement in the cervical spinal cord. Recognition of this pattern may improve and expedite the diagnosis of MS and preclude need for invasive diagnostic interventions.
INTRODUCTION
Multiple sclerosis (MS) is a demyelinating disease affecting brain and spinal cord. Enhancement after administration of contrast in MS indicates increased blood brain barrier permeability with active inflammation, typically persisting weeks.1 Ring enhancement, particularly the open ring sign, is a frequently observed pattern on brain MRI.2 Spinal cord abnormalities have been reported in greater than 80% of newly diagnosed MS patients.3 Ring enhancement within the spinal cord in MS has only recently been described as a rare pattern of enhancement.4–6 The significance and features of this enhancement pattern have not been commented upon. Recognition of this pattern has the potential to improve diagnosis of MS. We report a series of 20 MS subjects from one center over three years that demonstrated ring enhancing lesions within the spinal cord.
METHODS
Institutional Review Board (IRB) approval was obtained for the use of human subject records for this study. A search of all clinical imaging studies at Barnes-Jewish Hospital in St. Louis, MO was conducted including the dates January 2006–January 2009, a 37-month period. A search including the terms “multiple sclerosis” and “spinal cord MRI” yielded 322 patient scans. Cervical and thoracic spinal cord MRIs were analyzed for enhancement on T1-weighted imaging post administration of gadolinium. Thirty-six patient scans included enhancing lesions, of which 20 scans included a ring or incomplete ring pattern. Patterns that were labeled as ring enhancement were identified by the principal investigator (E.C.K.) and confirmed by a neuroradiologist (T.B.). All subjects were imaged on either a 1.5T or 3.0T scanner with a standard spine MRI protocol. Inclusion criteria included: 1) ages 18–80, 2) meeting McDonald criteria for clinically definite multiple sclerosis and 3) ring enhancement pattern on T1-weighted spinal cord imaging post administration of gadolinium. The pattern of ring enhancement was classified by location in the axial dimension of the spinal cord, single or multiple rings, complete or incomplete rings, and opening toward the center or the periphery of the spinal cord. If enhancement was incomplete or ‘open’ at any axial or sagittal slice on the MRI it was considered open for the purpose of analysis. A concurrent brain MRI was available in all cases and was analyzed for presence and pattern of contrast enhancement.
Subject demographics compiled included age, gender, ethnicity, disease duration, disease subtype, use of disease modifying therapy at the time of MRI, and disability by the Expanded Disability Status Scale (EDSS).7 Neurologic examination was available in 18 of the 20 subjects. A Multiple Sclerosis Severity Scale (MSSS) was calculated based on EDSS and disease duration as previously reported.8
RESULTS
Clinical Characteristics
Twenty MS subjects were identified with spinal cord ring enhancement (Table 1). Median age at the time of the MRI was 35 years (range 21–62). Median disease duration was 2.5 years (range <1–20). Of the 20 subjects, 95% (19/20) could be classified as relapsing remitting MS and 5% (1/20, Case 11) secondary progressive MS. Disease modifying therapy approved for MS was being taken in 40% (8/20) of subjects at the time of the imaging study. Eighty-five percent (17/20) were in a clinical relapse at the time of imaging. Median EDSS was 3.0 (range 1.0–7.0) at the time of the imaging study with a median MSSS of 6.46 (range, 4.54–9.84).
Table 1.
Patient Demographics and MRI Characteristics
| Case # | Age/Gender/Ethnicity | Disease Duration (yrs) | Spinal Cord Level | Spinal Cord Enhancement Pattern | Brain MRI enhancement | EDSS | MSSS |
|---|---|---|---|---|---|---|---|
| 1 | 44/F/C | 1 | C4 | Mult, D, OI | +, ring | 6.5 | 9.84 |
| 2 | 35/M/C | <1 | C2-3 | S, L, OO | +, round | 2.0 | N/A* |
| 3 | 28/F/C | 3 | C4 | S, D, OO | +, punctate | N/A | N/A |
| 4 | 48/M/C | 2 | C1-2 | S, AL, OO | - | 2.5 | 6.46 |
| 5 | 25/F/AA | 1 | C3-7 | S, L, OO | +, ring | 6.5 | 9.84 |
| 6 | 35/F/AA | <1 | C3-4 | S, L, OO | +, punctate | 2.0 | N/A* |
| 7 | 28/F/C | 4 | C3-5 | Mult, AL, OO | - | 2.5 | 5.41 |
| 8 | 44/F/C | 5 | C5 | S, L, OO | +, ring | 3.0 | 5.79 |
| 9 | 42/F/C | 21 | C4-5, T1 | Mult, DL, OI | - | N/A | N/A |
| 10 | 37/F/AA | 8 | C4 | S, L, OO | +, ring | 3.0 | 4.57 |
| 11 | 62/F/AA | 5 | T3 | S, L, OO | +, punctate | 7.0 | 9.60 |
| 12 | 31/F/C | 3 | C4-5, T2 | Mult, DL, OO | +, round | 2.5 | 6.00 |
| 13 | 35/F/C | <1 | T10 | S, L, closed | - | 2.0 | N/A* |
| 14 | 32/F/C | <1 | C4-5 | S, D, OO | -, round | 1.0 | N/A* |
| 15 | 27/M/AA | 1 | C1,C4,C7 | Mult, D, OI | +, ring | 3.5 | 8.64 |
| 16 | 46/M/C | 5 | C1, C3, C5 | Mult, DL, OO | +, ring | 3.0 | 5.79 |
| 17 | 47/M/C | 7 | C2 | S, L, OI | +, ring | 3.0 | 4.96 |
| 18 | 21/F/C | 1 | C2-3 | Mult, A, OI | - | 3.5 | 8.64 |
| 19 | 32/F/AA | <1 | C3, C4-5 | Mult, D, OI | - | 3.5 | N/A* |
| 20 | 40/F/C | 5 | T3-5 | Mult, D, OI | +, ring | 6.0 | 8.83 |
| Median | 35 | 3.5 | 3.0 | 6.46 |
EDSS = Expanded Disability Status Scale; MSSS = Multiple Sclerosis Severity Score; M = male; F = female; C = Caucasian; AA = African-American; Mult = Multiple; S = Single; D= Dorsal; L = Lateral; A = Anterior; DL = Dorsolateral; AL = Anterolateral; N/A = not available;
MSSS unreliable in first year of disease
MRI Characteristics
Analysis of the spinal cord enhancement pattern revealed a pattern of incomplete ring in 95% (19/20) of subjects (Figure 1). Of the incomplete ring enhancements, 63% (12/19) of the rings opened toward the outer edge and 37% (7/19) of the rings opened toward the center of the spinal cord within its axial plane. Forty-five percent (9/20) of the subjects had multiple spinal cord ring enhancements, located at the same or different spinal cord levels. The most common location in the axial plane was lateral in 40% (8/20), followed by dorsal in 30% (6/20), dorsolateral in 15% (3/20), anterolateral in 10% (2/20) and anterior in 5% (1/20). Ring enhancement was located within the cervical region in 75% (15/20), the thoracic region in 15% (3/20), and within both cervical and thoracic regions in 10% (2/20). Concurrent brain MRI revealed contrast enhancement in 70% (14/20) of subjects, 57% (8/14) of which demonstrated a ring enhancing pattern in at least one of the areas of brain enhancement. All subjects had white matter T2 hyperintensities in a pattern diagnostic for MS.
Figure 1. Spinal cord ring enhancement patterns in multiple sclerosis.
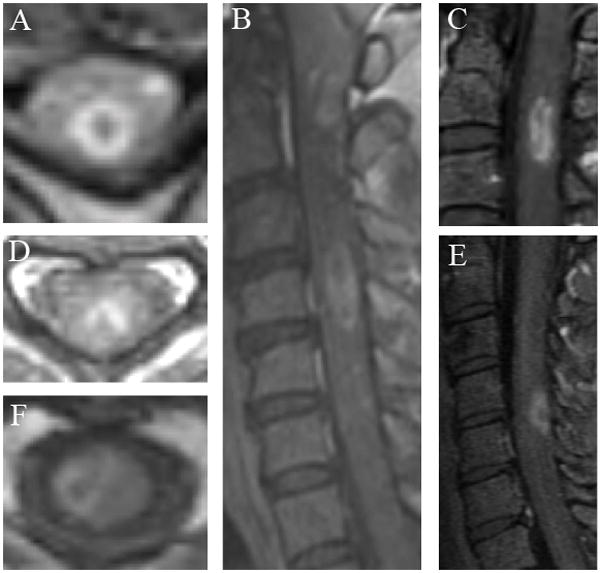
A. Case 1: Axial T1-weighted imaging post gadolinium (TR=908, TE=14) demonstrates closed ring enhancement at the level of C4. B. Case 1: Sagittal T1-weighted imaging post gadolinium (TR=828, TE=9.7) reveals multiple ring enhancements a different levels (C1 and C4) and within the same lesion (C4). C. Case 2: Sagittal T1-weighted imaging post gadolinium (TR=500, TE=14) shows a ring extending longitudinally and opening superiorly at the level C2-3. D. Case 3: Axial T1-weighted imaging post gadolinium (TR=615, TE=11) demonstrates ring enhancement opening out dorsally at the level C4. E. Case 14. Sagittal T1-weighted imaging post gadolinium (TR=600, TE=16.4) shows open ring enhancement opening out dorsally at the level C4-5. F. Case 17. Axial T1-weighted imaging post gadolinium (TR=460, TE=14) demonstrates ring enhancement opening toward the center of the cord at the level C2.
COMMENT
The 20 reported cases highlight the pattern of spinal cord ring enhancement in MS. Previous reports would indicate that this enhancement pattern is rare in the spinal cord even though ring enhancement has been commonly reported in the brain of MS patients. However, this case series of 20 subjects from a three year period at a single institution would indicate that this pattern is not uncommon in the spinal cord of MS patients, occurring with a prevalence of 6.2% (20/322). This pattern has been either previously under-recognized or under-reported. Another possible explanation is spine imaging is more routinely conducted due improved acquisition time and greater recognition of its clinical importance. The differential diagnoses for spinal cord ring enhancement should include MS, in addition to neoplasm, abscess, and granulomatous disease. Ring-enhancement, particularly an incomplete ring pattern, should prompt further work-up for demyelinating diseases, which may include brain MRI, cerebrospinal fluid (CSF) examination, and visual evoked potentials. Further evidence supporting the diagnosis of MS might then preclude a need for spinal cord biopsy in some patients where other diagnoses are suspected.
The imaging characteristics of this series are similar in location and appearance to previously reported cases. Lesions were typically asymmetrically placed, dorsal or lateral in the axial plane, and spanning ≤1 vertebral segment. The cervical region was preferentially involved, which is the region previously noted to contain the most overall enhancement.3 The high prevalence of coexisting ring enhancements in brains of these 20 subjects suggests a common pathophysiologic process occurring throughout the CNS.
All subjects in the series had relapsing MS, and 19 of the 20 were relapsing remitting and relatively early in their disease course. African-Americans comprised 30% of this series, which may be high and notable because African-Americans may be at increased risk for disability due to spinal cord disease.9 Overall, a high level of disability was found relative to disease duration based on the MSSS. However, it should be noted that neurologic exams were at the time of spinal cord enhancement and during a relapse in the majority of cases. We cannot speculate whether spinal cord ring enhancement has prognostic significance, due to lack of long term follow-up in this cohort.
Spinal cord ring enhancement can be seen in MS, and is often an incomplete ring. Recognition of open ring enhancement in the spinal cord may help to expedite the diagnosis of MS. The specificity of the “open-ring” sign has been determined for the brain.10 Further studies to determine the specificity of the incomplete ring pattern in the spinal cord are warranted.
Acknowledgments
NIH funding included UL1RR024992 (ECK), K23NS052430-01A1 (RTN), National MS Society funding included CA-1012 (AHC). AHC was supported in part by the Manny and Rosalyn Rosenthal-Dr. John L. Trotter Chair in Neuroimmunology. ECK was supported by an American Academy of Neurology Foundation Clinical Research Training Fellowship. TB was supported by a Bracco/American Roentgen Ray Society Scholar Award.
Footnotes
The corresponding author takes full responsibility for the data, the analyses and interpretation, and the conduct of the research. The corresponding author guarantees the accuracy of the references. The corresponding author has full access to all the data and has the right to publish any and all data, separate and apart from the attitudes of the sponsor.
All authors have agreed to conditions noted on the Authorship Agreement Form.
Disclosures: The study has no sponsors.
Dr. Klawiter has received speaking honoraria from Teva Neuroscience.
Dr. Benzinger has received travel expenses from Siemens and consulting fees from Biomedical Systems.
Dr. Roy has nothing to disclose
Dr Parks is a participant in clinical trials for Genzyme, Biogen Idec, Novartis, BioMS Medical, Teva Neuroscience and the NIH. She has received consulting fees or speaking honoraria from Biogen Idec, Bayer Healthcare, Teva Neurosciences, Pfizer and EMD Serono.
Dr. Naismith is a participant in clinical trials sponsored by Acorda Therapeutics. He has received consulting fees and speaking honoraria from Bayer Healthcare, Biogen Idec, Elan Pharmaceuticals, and Teva Neuroscience, and research funding from the NIH and National Multiple Sclerosis Society USA.
Dr. Cross has received research funding, clinical trial funding, honoraria or consulting fees from the NIH, National Multiple Sclerosis Society USA, Consortium of Multiple Sclerosis Centers, Genentech, Inc., Bayer Healthcare, Biogen Idec, Teva Neuroscience, Acorda Therapeutics, EMD Serono, and BioMS Medical.
References
- 1.Cotton F, Weiner HL, Jolesz FA, Guttmann CR. MRI contrast uptake in new lesions in relapsing-remitting MS followed at weekly intervals. Neurology. 2003 Feb 25;60(4):640–646. doi: 10.1212/01.wnl.0000046587.83503.1e. [DOI] [PubMed] [Google Scholar]
- 2.Masdeu JC, Moreira J, Trasi S, Visintainer P, Cavaliere R, Grundman M. The open ring. A new imaging sign in demyelinating disease. J Neuroimaging. 1996 Apr;6(2):104–107. doi: 10.1111/jon199662104. [DOI] [PubMed] [Google Scholar]
- 3.Bot JC, Barkhof F, Polman CH, et al. Spinal cord abnormalitiesin recently diagnosed MS patients: added value of spinal MRI examination. Neurology. 2004 Jan 27;62(2):226–233. doi: 10.1212/wnl.62.2.226. [DOI] [PubMed] [Google Scholar]
- 4.Dohi N, Ishikawa S, Kamijyo Y, Nakamura T, SOH, Maruyama K. Multiple sclerosis with open-ring enhancement in the cerebrum and spinal cord. Intern Med. 2003 Mar;42(3):273–276. doi: 10.2169/internalmedicine.42.273. [DOI] [PubMed] [Google Scholar]
- 5.Pyle W, Dastur K, Rahman M, Tsay J. Open-ring peripherally enhancing lesion of the cervical spine. Neurology. 2009 Jan 27;72(4):381. doi: 10.1212/01.wnl.0000341324.55937.d9. [DOI] [PubMed] [Google Scholar]
- 6.Xia L, Lin S, Wang ZC, et al. Tumefactive demyelinating lesions: nine cases and a review of the literature. Neurosurg Rev. 2009 Apr;32(2):171–179. doi: 10.1007/s10143-009-0185-5. [DOI] [PubMed] [Google Scholar]
- 7.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983 Nov;33(11):1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 8.Roxburgh RH, Seaman SR, Masterman T, et al. Multiple Sclerosis Severity Score: using disability and disease duration to rate disease severity. Neurology. 2005 Apr 12;64(7):1144–1151. doi: 10.1212/01.WNL.0000156155.19270.F8. [DOI] [PubMed] [Google Scholar]
- 9.Naismith RT, Trinkaus K, Cross AH. Phenotype and prognosis in African-Americans with multiple sclerosis: a retrospective chart review. Mult Scler. 2006 Dec;12(6):775–781. doi: 10.1177/1352458506070923. [DOI] [PubMed] [Google Scholar]
- 10.Masdeu JC, Quinto C, Olivera C, et al. Open-ring imaging sign: highly specific for atypical brain demyelination. Neurology. 2000 Apr 11;54(7):1427–1433. doi: 10.1212/wnl.54.7.1427. [DOI] [PubMed] [Google Scholar]


