Abstract
Untreated perinatal substance abuse is associated with serious adverse maternal and neonatal outcomes. Historically, many barriers have prevented pregnant women from seeking treatment. Early Start (ES) breaks new ground by sidestepping these barriers with a fully integrated service delivery model.
ES is the largest HMO-based prenatal substance-abuse program in the United States targeting all pregnant women seen at Kaiser Permanente Northern California (KPNC) prenatal clinics, currently screening more than 39,000 women each year. The program is based on the premise that substance abuse is a treatable disease and addresses it in a nonjudgmental, accepting manner. A substance-abuse counselor is located in each obstetrics clinic providing accessible one-to-one counseling to pregnant women screened at risk for alcohol, tobacco, or drug use as part of the routine prenatal care package offered to all patients.
A 2006 ES study, sponsored by the Kaiser Foundation Research Institute, evaluated program effectiveness in terms of its impact on neonatal and maternal outcomes. Preliminary results that included 49,986 KPNC patients indicate that compared with pregnant women whose results on screening for substance use were positive but who were untreated, ES-treated women had significantly lower rates on a number of outcome measures.
The originality and transferability of ES has led to both local and national recognition. Universal screening of all pregnant women with access to an integrated model of substance-abuse treatment should be the standard of care for every prenatal patient because of the significant benefits for mothers and their babies.
Introduction
In the early 1990s, two prevalence studies confirmed that prenatal substance abuse was a significant problem among Kaiser Permanente Northern California (KPNC) patients. An internal prevalence study conducted by neonatologist Marc Usatin, MD (Walnut Creek), from 1989 to 1990 tested newborn meconium for prenatal exposure to street drugs but not alcohol. An overall exposure rate of 3.2% was found for all KPNC birthing facilities. Shortly thereafter, the California Department of Alcohol and Drug Programs conducted a study that included five KPNC hospitals and found rates of perinatal alcohol and drug exposure ranging from 10% to 18% of all births (two KPNC sites had rates higher than the statewide average of 11.35%).1 This information, coupled with a body of literature documenting adverse neonatal outcomes such as placental abruption, fetal death, premature delivery, and babies born small for gestational age,2–7 prompted the development of a new approach to treating this population.
Historically, pregnant women at KPNC who were identified as having substance abuse problems were referred by their prenatal clinician to existing internal or community-based treatment programs. These efforts were largely unsuccessful …
Historically, pregnant women at KPNC who were identified as having substance abuse problems were referred by their prenatal clinician to existing internal or community-based treatment programs. These efforts were largely unsuccessful; only a fraction of the women referred to these programs attended them. Several clinicians, concerned about the poor outcomes and poor intervention record with this approach, explored other successful prenatal substance abuse intervention models, all of which were in the public sector at that time. To capitalize on KPNC's strength and history as a vertically integrated program, the clinicians identified models that would further integrate services. Experts from Born Free, a program in Contra Costa County that routinely screened all pregnant women for alcohol, tobacco, and other drug use and referred them to an on-site substance abuse specialist, as well as administrators for programs that were integrating a variety of mental health and behavioral health services with primary care, were consulted.
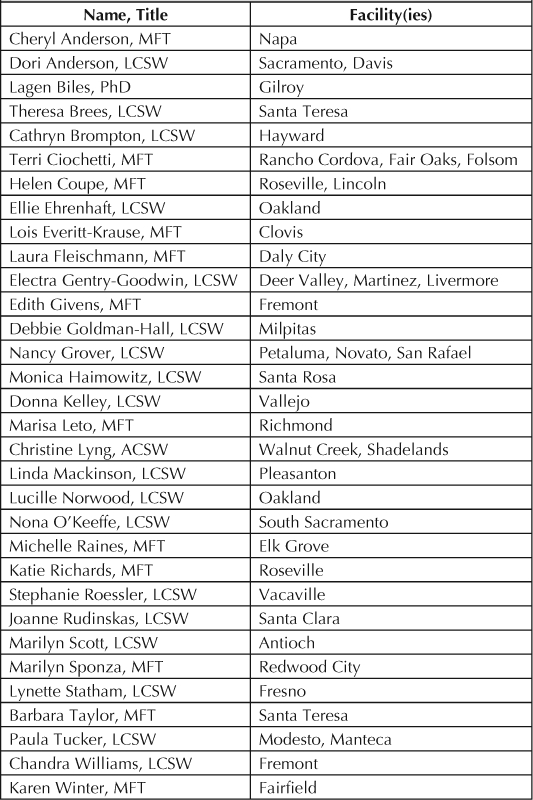
Through a Garfield Memorial Fund sponsored grant, KPNC began an obstetric, clinic-based perinatal substance abuse intervention program known as Early Start (ES)8 and piloted the program at the Oakland Medical Center from 1990 to 1993. At the same time, the multi-disciplinary Perinatal Substance Abuse Task Force was initiated. The innovative aspect of ES was stationing a licensed substance abuse expert, or ES specialist (ESS), within the Obstetrics Department to work as part of the prenatal care team. The role of the ESS was to assess, educate, and provide ongoing counseling to at-risk women. The ES model also implemented universal substance use risk screening and education for all pregnant women and ongoing professional education, consultation, and training for obstetrics/gynecology (Ob/Gyn) clinicians and staff. The Early Start Intervention Specialists are listed in Table 1.
Table 1.
Early Start Intervention Specialists
Evaluation of the pilot project found that 92% of the patients who were referred to the ESS by their clinician accepted the referral. For 81% of these women, the ESS diagnosed moderate to severe substance abuse problems. These women were regularly tested for alcohol and other drugs during their prenatal care. Subsequently, 69% had negative findings on toxicology screens by the 32-week point in their pregnancies, and their babies had significantly better birth outcomes and shorter hospitalizations compared with women who continued to use alcohol and street drugs (Boddum A, Chin V, Gordon, N, Soghikian, K. Unpublished final report to Garfield Committee: a model system for early identification and management of substance abuse during pregnancy. August 1992).
Surveys of prenatal clinicians involved in the pilot project indicated that they were very satisfied with the model and felt that it enhanced their clinical practice. Prior to the ES program, clinicians indicated that they were not likely to identify substance-abusing patients. After the in-service training and implementation of ES, these same clinicians reported that they were much more likely to obtain a substance abuse history and make a referral if appropriate. All but one of the 15 clinicians involved in the pilot project felt that it was very important to have the substance abuse specialist located in the Ob/Gyn department rather than to only be able to refer to the chemical-dependency treatment program at the facility.8
In 1994, after these successful pilot results,8 the Perinatal Substance Abuse Task Force lobbied The Permanente Medical Group (TPMG) board of directors and regional Kaiser Foundation Hospitals (KFH) to transfer the program to four new sites and to hire a regional coordinator. ES rolled out at 16 additional sites during the next 10 years through local TPMG funding and seed money from Regional Successful Practices. In 2003, KFH and TPMG leadership agreed to jointly fund the program for full regional implementation (see Figure 1).
Figure 1.
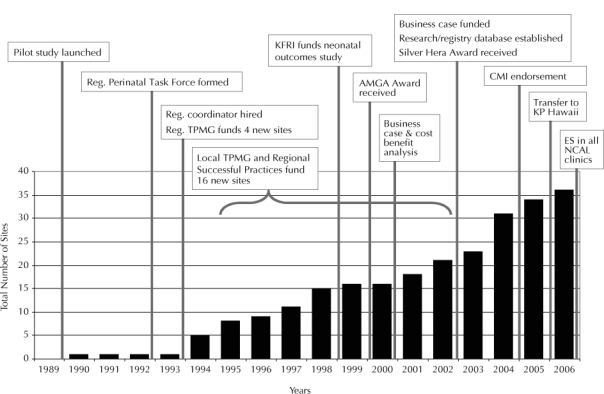
Early Start: growth and critical events. AMGA = American Medical Group Administrators; CMI = Care Management Institute; ES = Early Start; KFR I = Kaiser Foundation Research Institute; KP = Kaiser Permanente; NCAL = Northern California; TMPG = The Permanente Medical Group.
Objectives
The KPNC ES program created four objectives that are the core of the program:
To decrease substance abuse in pregnant women
To reduce negative birth outcomes and medical costs associated with prenatal substance abuse
To improve access to substance abuse services for pregnant women
To enhance clinician satisfaction and efficacy.
Scope and Significance
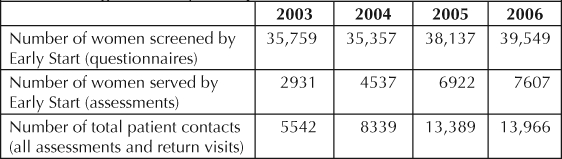
ES is the largest HMO-based prenatal substance abuse program in the United States. ES targets all pregnant women seen at KPNC prenatal clinics, currently screening more than 39,000 women each year. In 2006, ES provided over 13,900 patient visits to more than 7600 KPNC patients (Table 2).
Table 2.
Regional Early Start patient care metrics
Although this program focuses on obstetrics, a pilot program was recently launched at the KPNC Richmond facility that links ES mothers and babies to pediatrics with the goal of providing them with seamless services.
The ES program changed the existing service delivery care model to one that improves quality and access for patients. Some of these clinical and operational changes include:
Adding a substance abuse specialist to the prenatal care team and physically stationing the specialist in the prenatal clinic (the most innovative aspect of the program model)
Educating all pregnant women about the risks of alcohol, tobacco, and other drugs through various media and at multiple points in pregnancy (information is included in published newsletters, given orally at prenatal group visits, available on the national help line and the ES Web site, and provided individually through customized educational pamphlets and one-to-one counseling)
Screening for risk at the first prenatal visit by a self-administered questionnaire and by urine toxicology testing (with signed consent)
Intensive training (eg, using addiction-medicine physicians and other specialists) for obstetric clinicians about the medical aspects of prenatal substance abuse and techniques for effective referrals
Ongoing counseling and case management for pregnant women identified as being at risk, with the option for continued care for up to one year after childbirth
Multidisciplinary training, consultation, and work groups with relevant departments, including pediatrics, chemical dependency, psychiatry, and social services
Maintaining an underlying philosophy that prenatal substance abuse and addiction are diseases that should be addressed, just as any other complication of pregnancy
Partnering with the KPNC Division of Research to conduct program evaluation, research projects, and report development
Aligning with the organizational goal of providing quality, personalized care, and specialized services for women.
The ES model provides nonthreatening, accessible, clinic-based substance abuse counseling to pregnant women. At the time of the first prenatal office visit, at-risk patients are referred by the prenatal care clinician directly to the ESS, who has a confidential office space in close proximity to examination rooms within the obstetrics clinic. The ESS completes a thorough psychosocial assessment with the patient, educates her about risks, and provides support, resources, and referrals to appropriate services. With an emphasis on abstinence, the ESS and patient work collaboratively to achieve behavioral-change goals related to the patient's substance abuse patterns. Follow-up ES appointments occur throughout the pregnancy in conjunction with the medical prenatal visit. The ES program boldly embraces innovation, supplanting typical obstacles to care to successfully provide uniquely tailored services to this high-risk group of patients.
With an emphasis on abstinence, the ESS and patient work collaboratively to achieve behavioral-change goals related to the patient's substance abuse patterns.
ACOG Ethics Committee Opinion.
In May 2004, the American College of Obstetricians and Gynecologists Committee on Ethics wrote:9
Abuse of alcohol and drugs is a major health problem for American women across differences in socioeconomic status, race, ethnicity, and age, and it is costly to individuals and to society. Obstetrician-gynecologists have an ethical obligation to learn and use a protocol for universal screening questions, brief intervention, and referral to treatment. . . . This is the clinically appropriate professional action, both medically and ethically . . . and it results in a mean net savings of $4644 in medical expenses per mother/infant pair. . . . [Although] few treatment programs focus on the needs of pregnant women … there are successful models for prevention and treatment for women and their families (AR-Cares, Choices, Safeport, Early Start and Mom/Kid Trial).
Quality Measures
With the implementation of ES, KPNC is poised as the quality leader in the field. The 2006 ES study, sponsored by the Kaiser Foundation Research Institute and conducted by the Division of Research, evaluates program effectiveness in terms of its impact on neonatal and maternal outcomes.
Preliminary results indicate that compared with pregnant women whose results on screening for substance use were positive but who were untreated, ES-treated women had significantly lower rates on a number of outcome measures (see more detail in the Design and Methodology section).
In 2000, a cost–benefit analysis of ES was conducted as part of a business case to promote full regional implementation. The analysis showed a savings in variable direct costs of $1504 per baby whose mother received ES intervention, compared with babies of mothers who abused substances and received no intervention, after six months of follow-up monitoring after delivery. The business case conclusion was that regional implementation would be highly cost effective, providing a simple return on investment of >30%.
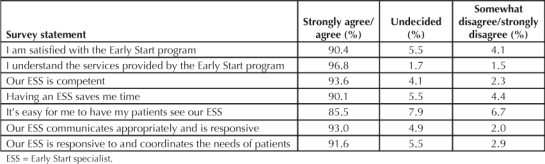
In 2005, Ob/Gyn clinicians were surveyed about their satisfaction with the ES program, and their responses exceeded the already high ratings from a similar survey done in 2004. With a 58% response rate, 90% of clinicians across the region agreed or strongly agreed with the statement that the program “saves me time,” and 92% to 94% agreed or strongly agreed that the ESS was competent, communicated appropriately, and was responsive to and coordinated solutions for patient needs (Table 3).
Table 3.
2005 Early Start clinician satisfaction survey (n = 631)
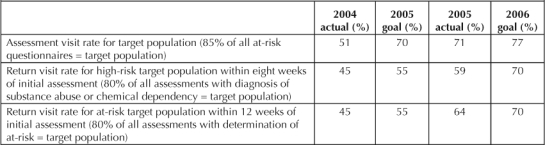
ES met both of the 2005 quality and access performance goals of increasing consistency of service delivery across the region through assessment and return visits for both high-risk and at-risk populations. Preliminary analysis of rates for 2006 shows that ES also met the 2006 assessment rate goal of 77% (Table 4).
Table 4.
Regional achievement rates for Early Start quality and access goals
ES exceeds the recommendations of the 2004 American College of Obstetricians and Gynecologists Committee on Ethics Opinion9 and addresses two top priorities for the Healthy People 2010 initiative,10 which has a national goal (See Sidebar: Healthy People 2010) of increasing the percentage of pregnant women who achieve abstinence from alcohol to 94%, and to 100% from street drugs.
Design and Methodology
A follow-up study to the first ES retrospective study, which was reported in 2003,11 was conducted in 2006 and produced similar results. The KP Community Benefit-funded 2006 ES retrospective study included 49,986 KPNC patients who completed the ES prenatal substance abuse screening questionnaires between January 1, 1999, and June 30, 2003; underwent urine toxicology screening tests; and had either a live birth or an intrauterine fetal death.12
The investigators concluded that substance abuse treatment for pregnant women that is integrated with prenatal care significantly benefits newborns and their mothers.
Four groups were then compared on neonatal and maternal outcomes: 1) substance abusers screened, assessed, and treated (SAT); 2) substance abusers screened and assessed who had no follow-up treatment (SA); 3) substance abusers who were only screened (S); and 4) control study subjects whose screens had negative results.
Results
The study showed that SAT women had statistically significantly lower rates than S women for placental abruption, preterm labor, and stillbirth and often had outcomes that compared favorably with those of the control study subjects.
For most major neonatal outcomes such as assisted ventilation, low birth weight, and preterm delivery, a similar trend was observed, with control study subjects having the lowest rates, followed by SAT and SA women, with S women having the highest rates. In most cases, the rates for the S women were significantly higher than those for the control study subjects. This pattern persisted in multivariate analyses controlled for maternal age, ethnicity, and amount of prenatal care.
To assess possible bias caused by self-selection and severity of illness, the three groups of substance-abusing women were compared regarding available risk factors (such as smoking and family history) and variables indicative of severity of substance abuse (such as frequency of use and poly-drug use). The assessed and treated women had similar or higher rates for these factors than did the women in the nonintervention group, indicating that their problems were no less severe.
The investigators concluded that substance abuse treatment for pregnant women that is integrated with prenatal care significantly benefits newborns and their mothers.
Clinical Impact
Prior to ES, many barriers prevented pregnant women from attending traditional addiction treatment programs, including lack of transportation, lack of child care services, intensive time requirements, additional costs and copayments, stigma, and lack of services tailored to meet their needs. ES breaks new ground by sidestepping these barriers with a fully integrated service delivery model. The multidimensional nature of prenatal substance abuse requires a multidisciplinary approach and the commitment of the entire Ob/Gyn Department.
Early Start is based on the premise that substance abuse is a treatable disease and addresses it in a nonjudgmental, accepting manner. Accordingly, all women are screened through a confidential prenatal screening questionnaire and are expected to undergo urine toxicology screening, although they can decline the latter (but the vast majority do consent). The purpose is to cast a wide net such that no woman who abuses street drugs or alcohol will be missed. At the first prenatal office visit, patients whose questionnaire or toxicology screening results are positive are referred by the prenatal clinician directly to the ESS. The ESS completes a thorough psychosocial assessment with the patient, educates her about risks, and provides support, resources, and referrals. After the assessment, the ESS works hand in hand with the clinician to coordinate the patient's care throughout pregnancy. If the ESS determines that the woman has chemical dependency, substance abuse, or increased risk for substance abuse, then follow-up ES appointments are continued throughout the pregnancy in conjunction with the medical prenatal visit.
The program at each clinic is managed by the ES team, composed of a physician or nurse practitioner “champion,” an Ob/Gyn nurse manager, an ES medical assistant, and the ESS. The ES medical assistant continues to monitor, book, and reschedule appointments for ES patients throughout the pregnancy. The assistant works very closely with the ESS to coordinate care and assists with case-management needs. All prenatal clinicians are trained with standardized scripts to assist them in talking with and referring patients to the ESS, and the ES champion at each site is actively involved in their training, education, and support. The Ob/Gyn nurse manager is also a key player, maintaining well-coordinated and streamlined ES systems. The teams meet monthly at their sites to review their quality goals, improve systems, and celebrate successes. Twice a year, these teams meet with all of the other ES teams regionwide to address obstacles and to share and develop best practices. The local sites are supported by a multidisciplinary regional team with endorsement from the regional women's health leader and sponsorship and joint financial support from TPMG and KFH executive leadership.
The originality and ease of replicability of ES has led to considerable local and national recognition for the program model and its research efforts.
Transferability Results
As seen in Figure 1, the ES program was funded for full regional implementation in 2003 on the basis of the results of a business case that was developed with support from ES research.11 The program continues to be implemented and expanded throughout all of Northern California. In 2003, ES was one of the successful transfer practices studied for a research project completed by Kaiser Permanente's (KP's) Care Experience Council. In 2004 the program was the first to be endorsed for national transfer by the Care Management Institute Maternal and Newborn workgroup, and in August 2006 the program officially transferred to the Hawaii Region.
The pioneering practices of ES have also been successfully adopted by the KP Southern California Bell-flower obstetrics clinic and by San Bernardino County (the largest county in the state). Using ES as the model, San Bernardino County successfully secured March of Dimes funding to support hiring substance abuse specialists for the four major prenatal practices serving county patients. The ES model is currently being studied by Contra Costa, Alameda, Solano and Santa Clara counties for implementation.
The originality and ease of replicability of ES has led to considerable local and national recognition for the program model and its research efforts. Early Start:
Was given the Models of Excellence for High-Risk Patient Management Award by the American Medical Groups Association, 2000
Was chosen as one of four women's health priorities targeted by KPNC for full implementation in the Northern California Region, 2001
Was included as a model of care in the American Association of Health Plans publication Improving Maternal Child Health: Innovation Program Approaches for Health Plans, 2001
Won Best Maternal and Child Health Research Presentation at the California Maternal and Child Health Conference, 2001
Was given the Silver Hera Award by the American Association of Health Plans, recognizing significant improvement in women's and children's health outcomes, 2003
Was chosen as priority to transfer programwide by the Care Management Institute Maternal Newborn Health Group, 2004
Was included as a successful model for pregnant women by the American College of Obstetrics and Gynecology Committee on Ethics Opinion, 2004.
ES has two comprehensive Web sites with resources for internal (http://kpnet.kp.org/california/earlystart) and external (www.kp.org/earlystart) clients. The internal site is robust, containing such items as toolkits for specialists, managers, and champions. Toolkit information ranges from screening guidelines, hiring and posting information, scripts for clinicians to discuss substance abuse with patients, reference articles, core competencies, getting-started guides for each member of the team, and quality-assurance information to the forms, documents, and materials used to implement and support the program. The external Web site can be accessed by employees as well as patients and provides direct links to the home pages of the ESS, a self-test for assessing risk during pregnancy, educational materials on drug use in pregnancy, and references to numerous available internal and external resources. The regional team has also developed a two-day in-service program for teams from visiting KP regions who are implementing ES; the training includes didactic information as well as an ES site visit and mock patient experience at the clinic level.
Conclusions
ES exemplifies the four cornerstones that constitute the KP promise: The ES outcomes research clearly demonstrates that implementation of universal screening practices and providing substance abuse treatment for pregnant women that is integrated with prenatal care creates “quality that you can trust,” resulting in significant beneficial effects on newborn and maternal health. Locating the ESS in the obstetrics clinic and providing a unique one-to-one counseling experience focuses attention on the individual needs of our patients, addressing KP's commitment to “caring with a personal touch” and making services “convenient and affordable.” Ensuring that ES appointments are linked with routine prenatal care and that copayments are waived for ES appointments and laboratory visits meets the goal of providing affordable services.
ES is a national model of choice for prenatal substance abuse intervention and will continue to benefit our patients, KP, and the broader community for generations to come.
ES is a national model of choice for prenatal substance abuse intervention …
Acknowledgments
Katharine O'Moore-Klopf of KOK Edit provided editorial assistance.
References
- Vega WA, Kolody B, Hwang J, Noble A. Prevalence and magnitude of perinatal substance exposures in California. N Engl J Med. 1993 Sep 16;329(12):850–4. doi: 10.1056/NEJM199309163291207. [DOI] [PubMed] [Google Scholar]
- Shiono PH. Prevalence of drug-exposed infants. Future Child. 1996 Summer–Fall;6(2):159–63. [PubMed] [Google Scholar]
- Chomitz VR, Cheung LW, Lieberman E. The role of lifestyle in preventing low birth weight. Future Child. 1995 Spring;5(1):121–38. [PubMed] [Google Scholar]
- Dattel BJ. Substance abuse in pregnancy. Semin Perinatol. 1990 Apr;14(2):179–87. [PubMed] [Google Scholar]
- Ostrea EM, Lucena JL, Silvestre MA. The infant of the drug-dependent mother. In: Avery GB, editor. Neonatology: pathophysiology and management of the newborn. 6th edition. Philadelphia: JB Lippincott; 2005. editor. Chapter 15. [Google Scholar]
- Kaye K, Elkind L, Goldberg D, Tytun A. Birth outcomes for infants of drug abusing mothers. N Y State J Med. 1989 May;89(5):256–61. [PubMed] [Google Scholar]
- Bauer CR. Perinatal effects of prenatal drug exposure. Neonatal aspects. Clin Perinatol. 1999 Mar;26(1):87–106. [PubMed] [Google Scholar]
- Armstrong MA, Lieberman L, Carpenter DM, et al. Early Start: an obstetric clinic-based, perinatal substance abuse intervention program. Qual Manag Health Care. 2001 Winter;9(2):6–15. doi: 10.1097/00019514-200109020-00004. [DOI] [PubMed] [Google Scholar]
- ACOG Committee on Ethics. ACOG Committee Opinion. Number 294, May 2004. At-risk drinking and illicit drug use: ethical issues in obstetric and gynecologic practice. Obstet Gynecol. 2004 May;103(5 Pt 1):1021–31. [PubMed] [Google Scholar]
- Office of Disease Prevention & Health Promotion, Department of Health and Human Services. Healthy People 2010: Volume 2: Objectives for improving health (Part B: Focus areas 15–28) Washington, DC: Department of Health and Human Services; 2000. [Google Scholar]
- Armstrong MA, Gonzales Osejo V, Lieberman L, et al. Perinatal substance abuse intervention in obstetric clinics decreases adverse neonatal outcomes. J Perinatol. 2003 Jan;23(1):3–9. doi: 10.1038/sj.jp.7210847. [DOI] [PubMed] [Google Scholar]
- Goler N, Armstrong MA, Taillac C, Osejo V, Folck B. Impact of the Early Start program on maternal and neonatal outcomes: 2006 preliminary results. 2007 In Press. [Google Scholar]


