Abstract
Purpose
The purpose of the study was to discover which patient and support system characteristics and interventions documented by home health clinicians were associated with improvement in urinary and bowel incontinence contrasting logistic regression and data mining approaches.
Subjects and Setting
1,793 patients in this study had 2,072 episodes of care representing all non-maternity patients who were ages 18 or older and receiving skilled home health services in 2004 from a convenience sample of 15 home health agencies.
Design
This study is a secondary analysis of data from 15 home health agencies' electronic health records.
Instruments
Data for this study were documented by home care clinicians using the Outcome and Assessment Information Set (OASIS) structured assessment form and the Omaha System interventions, which is a standardized terminology.
Results
There were 684 patients with urinary incontinence and 187 with bowel incontinence. By discharge 38% improved in urinary incontinence and 45% improved their bowel incontinence. Using logistic regression, no patient or support system characteristics were associated with improvement in either urinary or bowel incontinence, only a limited number of interventions were significant. A data mining decision tree was producible only for bowel incontinence, demonstrating a combination of patient and support system factors as well as selected interventions were important in determining whether patients would improve in bowel incontinence.
Conclusions
Home health patients have complex comorbid conditions requiring home care nurses to have broad, generalized knowledge. Future research is needed to determine if the inclusion of a certified wound, ostomy, and continence nurse would improve outcomes.
Introduction
The Institute of Medicine called for the implementation of evidence-based practice (EBP) and use of electronic health records (EHRs) in response to the rising number of adverse events, unexpected deaths, and costs in health care.1, 2 Among the barriers to meet this objective are the paucity of research in home health3 and the difficulty of disseminating research in practice to improve outcomes.4 Health care providers spend an inordinate amount of time meeting regulatory and quality improvement documentation requirements. Use of an EHR is one strategy for reducing the time required for documentation. Documentation via an HER also enables secondary analysis of date to support quality improvement and research to develop evidence-based practice (EBP) from real-life experiences.
EHRs used by home health care clinicians include structured data for documentation which may be useful for research to develop and test EBP. Since 1998, the Centers for Medicare and Medicaid Services (CMS) require Medicare certified home health agencies to use the Outcome and Assessment Information Set (OASIS), a structured form for routine documentation of patient needs. This structured, standardized assessment tool provides a valuable source for research using home health data.5 The most recent version of OASIS under development (OASIS C)6 requires clinicians to document a plan of care for identified problems. However, because no standards for intervention data are specified, it is difficult to compare the effectiveness of interventions with outcomes. The Omaha System is a nationally recognized standard for interventions incorporated into an increasing number of home health software vendors7 that can support intervention research in home health. The purpose of this study was to conduct a secondary analysis of home health EHR data to discover patient and support system factors and interventions associated with improvement in urinary and bowel incontinence.8
Background
Improvement in urinary and bowel incontinence are important outcomes to address in home health. CMS requires home health agencies to conduct outcome based quality improvement (OBQI). Two outcome measures included in OBQI are improvement in urinary and bowel incontinence. Urinary incontinence is publicly reported for consumers in comparing the quality of home health agencies.8 The importance of an outcome is determined by its prevalence, variability, costs, impact on quality of life, and ability to be modified. Urinary and bowel incontinence are highly important. Urinary incontinence was identified for 26.7% of home health patients on admission in 2006, while bowel incontinence was reported as occurring for 7.4% of home health admissions.9, 10 The higher costs associated with incontinence care and adverse effects of both urinary and bowel incontinence on quality of life are well documented.11, 12 For patients with incontinence on admission, national rates show that improvement in urinary incontinence (UI) varied from 32.0% to 67.0% of patients while improvement in bowel incontinence (BI) ranged from 52.0% to 73.0%. Clearly, there is room for improvement in both of these home health outcomes.
UI and BI lower quality of life and are costly to manage and commonly result in psychological distress, social isolation, poorer quality of life, and secondary complications such as pressure ulcers and infections.11-13 The total cost of care for individuals with incontinence include supplies, drugs, health care services, surgery, and possible hospitalization or nursing home placement as a result of complications.12-14 UI is estimated to cost $14 billion annually and expected to increase to $20 billion as the baby boomers age.15 Costs associated with BI have not been estimated but are hypothesized to be high.
Predictors of Incontinence
A synthesis of research on predictors for UI and BI in community-living and nursing home adults was presented at a National Institutes of Health15 conference and synthesized in an Evidence Report/ Technology Assessment.13 While UI has been studied extensively, research addressing BI is comparatively sparse. Factors associated with an increased likelihood of UI include older age, higher body mass index, decreased functional status, diabetes mellitus, specific neurological conditions such as stroke, cognitive impairment, depression, and cigarette smoking. The rate of UI is also higher in females and increases with the number of births for younger women. Factors associated with an increased likelihood of BI are old age, stroke, deficits in activities of daily living, cognitive impairment, bowel impaction, constipation, high doses of laxatives, diarrhea, urinary incontinence, certain bowel diseases and surgery or radiation damaging sphincter control. Patients with either type of incontinence require more caregiver support, particularly those with dementia or cognitive impairment. Few studies have been conducted in home health care, and additional research is needed to determine if there are similar or additional factors associated with incontinence than those reported in other care settings.
Interventions to Improve Incontinence
Studies have demonstrated the efficacy of some interventions for improving UI and BI but the evidence supporting interventions for UI tends to be stronger. Interventions for prevention and treatment of urinary and bowel incontinence that may be useful in home health are summarized from systematic reviews and guidelines in Tables 1 and 2. Specific interventions may vary based on the severity and underlying causes of incontinence; multiple approaches are often recommended. Most studies included in systematic reviews and guidelines focus on hospitalized patients, nursing home residents, or people living in the community. Few studies focus on home health patients and it is not known whether these interventions can be generalized to the home health care setting. Therefore, research is needed to build on previous investigations about the effectiveness of interventions for improvement of urinary and bowel incontinence in home health.
Table 1.
Urinary Incontinence Interventions from Systematic Reviews and Guidelines
| Action | Problem/ Target | Full Intervention |
|---|---|---|
| Monitoring | Genito-urinary Function Nutrition Functional Status Cognition |
Comprehensive assessment of incontinence and contributing factors, including fluid intake, bowel status, functional status, and cognition23, 24 |
| Monitoring | Bowel Function | Medical & surgical problems that might affect bowel status 23 |
| Monitoring | Medications | Medications which may have an impact on the incontinence23, 24 |
| Monitoring | Environment | Proximity and availability bathrooms or commode and adequacy of lighting23, 24 |
| Monitoring | Genito-urinary Function | Use of voiding record23 |
| Treatment | Integument | Skin cleansing after in incontinent episode and utilizing barrier ointments24 |
| Treatment | Bladder Care | Provide bladder training / prompted voidings with gradual increasing time between voidings23, 24, 28-30 |
| Teach | Nutrition | Minimize foods that irritate the bladder24 |
| Teach | Nutrition | Adequate level of fluid intake, minimize the use of caffeinated and alcoholic beverages 23 |
| Teach | Nutrition | Weight reduction13 |
| Teach | Bladder care | Pelvic floor muscle exercises13, 24, 25 |
| Teach | Bladder Care | Absorbent products consistent with patient preferences24, 31, 31 |
| Teach | Medications | Teach about use of anticholinerics for overactive bladder, including side effects32 |
| Coordinate | Community Resources | Nurses should be knowledgeable about community resources for personal development, referral, and ongoing assistance23, 24 |
| Coordinate | Community Resources | Refer to specialist nurse for incontinence management33 |
Table 2.
Bowel Incontinence Interventions from Systematic Reviews and Guidelines
| Action | Problem/Target | Full Intervention |
|---|---|---|
| Monitoring | Bowel Function | Comprehensive history, assessment, and physical exam34-36 |
| Treatment | Bowel Care | Bowel irrigation/ enemas35, 37, 38 |
| Treatment | Bowel Care | Biofeedback 13, 34, 35, 38, 39 |
| Treatment | Bowel Care | Bowel retraining/ consistency of schedule34-36 |
| Treatment | Bowel & Bladder | Mechanical and/or chemical rectal stimulation to predictably and effectively evacuate stool36 |
| Teach | Nutrition | Dietary Management (high fiber, adequate fluids) 34-36, 38 |
| Teach | Medications | Antidiarrheal agents 34, 35, 38, 40 |
| Teach | Medications | Laxatives, stool bulking agents, and suppositories34, 35, 38 |
| Teach | Disease treatment | Continence products consistent with patient preferences 37 |
| Teach | Disease treatment | Use of assistive techniques such as push-ups, abdominal massage, Valsalva maneuver, deep breathing, and positions for emptying bowel36 |
| Teach | Disease treatment | Pelvic floor muscle training13, 35, 37 |
| Teach | Emotional & Cognitive Issues | Social and emotional support to help manage actual or potential disabilities and emotional responses36 |
| Teach | Disease Treatment | Advice on skin care (cleansing, skin barriers)34, 38 |
| Coordinate | Community Resources | Referral to specialists if prolonged problem37 |
| Coordinate | Supplies & Equipment | Appropriate adaptive equipment for bowel care should be prescribed based on the individual's functional status and discharge environment36, 37 |
| Coordinate | Community Resources | Support groups37 |
Research Design
Research Objectives
We addresses two objectives in this study: 1) to discover which patient and support system factors and interventions documented by home health clinicians are associated with improvement in urinary and bowel incontinence, and 2) to compare logistic regression vs. data mining to determine their usefulness for predicting improvement in these outcomes. This study is a first step in using EHR data for developing evidence based home health practice for UI and BI.
The specific research questions addressed in this study were:
What is the prevalence of urinary and bowel incontinence on admission to home health?
What percent of patients have improvement in urinary and bowel incontinence by discharge from home health?
What percent of patients had research-based interventions documented for urinary and bowel incontinence?
What variables are associated with improvement in urinary and bowel incontinence?
What rules can be induced to guide clinical decisions for improving urinary and bowel incontinence?
Methods
Data were obtained from 15 home health agencies using either one of two software vendors for their EHR. The two software vendors were selected since they were the only known vendors when the study was initiated that incorporated both the OASIS and Omaha System data for routine documentation in the home health care setting. After approval by the University of Minnesota Institutional Review Board, an agreement was signed with the vendors to obtain data from the home health agencies. The software vendors contacted the home health agencies who used their system for at least six months, explained the study, obtained written agreement for participation, and ran modified reports in the agencies' databases to obtain a limited dataset. Patient and agency identifiers were removed by the vendor with the exception of the admission, discharge, and birth dates for patients. The software vendors then transferred the files through a secure internet connection to the investigators.
Selection Criteria
Data were included in the study for all patients who were ages 18 or older and receiving skilled home health services in 2004. Data were excluded if patients received care for maternity reasons or did not have either a start or resumption of care OASIS assessment followed by a discharge assessment since both were needed to calculate study outcomes. Because the focus of our study was improvement in UI and BI, patients were excluded if they did not have difficulty with incontinence at the start of an episode of care.
Unit of Analysis
The unit of analysis in this study is an episode of care defined as a continuous time during which a patient receives one or more home health visits. Episodes of care were created by matching either an OASIS start or resumption of care with a discharge assessment using the dates the assessments were completed. Patients could potentially have one or more episodes of care.
Instruments
In home health care, OASIS data and the Omaha System interventions have been used to document patient assessments, interventions provided, and outcomes of care. These data can be useful for research to analyze the factors associated with improvement in UI and BI. OASIS assessments include information about socio demographics, social support, physical and emotional-behavioral status, functional status, and service utilization. OASIS was developed over 15 years with Federal and private funding to create a reliable and valid assessment and outcome measurement in home health.16 The OASIS assessment tool is available on CMS's website.8 CMS requires home health agencies to integrate the OASIS data into a comprehensive assessment as part of routine charting and then abstract data for Medicare and Medicaid patients for electronic submission to CMS. The OASIS data are used by CMS for certification, quality improvement, public reporting, and calculation of Medicare's prospective payment rate.
The Omaha System was developed through 18 years of federally funded research to create a classification system for patient problems, interventions, and a problem rating scale for outcomes. It is particularly useful for documenting community-based practice. In the Omaha System (Version 1), there are 44 Problems, 4 Categories of action, and 63 Targets or subject areas for interventions. The 44 problems are divided into four domains: Environmental, Psychosocial, Physical, and Other Health Related problems. The Categories of action include Teaching, Guidance & Counseling; Treatments & Procedures; Case Management; and, Surveillance (Monitoring). Examples of Targets are Medication Administration or Dressing Change. In this study, an intervention was defined as a recorded action provided for a patient that combined an Omaha System Problem, Category of action, and Target. An example would be Genito-urinary Impairment: Teaching about Disease Process. Together, the Omaha System and OASIS provide a comprehensive assessment, ongoing documentation of interventions for problems, and outcomes indicating a change over time.
Independent Variables
Independent variables were included from either the start or resumption of care OASIS assessments as well as some assessment items that changed during an episode of care and were recorded on the discharge assessment. Variables included from the discharge assessment were: medical or treatment conditions that changed in the past 14 days, parenteral or nutritional therapies received, life expectancy, high risk factors, living arrangements, supportive assistance required, speech, pain, integumentary status, respiratory status, neuro-emotional-behavioral status, functional status, medication and equipment management, and emergent care or hospitalization. From the discharge assessment, actual values for nominal variables and a change score for ordinal variables were included.
The Omaha System interventions were matched to the OASIS episodes of care. There were 11,088 potential combinations of intervention terms so interventions were clustered into 23 groups by experts familiar with the Omaha System. Each Omaha System Category of action had several groups of interventions that included similar Problems and Targets. For instance, one group was called “Providing Treatment for Bowel and Bladder.” This group contained all interventions that included the problems or Urinary and Bowel Function” as well as any interventions containing the more specific Target of Bladder Care, Bowel Care, or Ostomy Care. The 23 groups are reported later in this study with the findings of intervention frequencies documented for each group. A summative score was created from the frequency of interventions for each group.
Bowel and bladder incontinence can occur for patients with a variety of clinical and functional conditions. We did not limit which variables to include since the purpose of the study was discovery and not hypotheses testing. However, due to the relatively small sample size compared with the large number of predictive variables to be analyzed, several strategies were used for data reduction. Scales were developed by summing responses for similar items for prognosis, pain, pressure ulcers (stages 2 – 4), stasis ulcers, surgical wounds, and respiratory status. Primary diagnoses were transformed into the Clinical Classification Software groups,17 reducing a potential of 13,000 medical diagnoses into 260 clinically meaningful groups. These were further reduced into 51 groups of similar diagnoses and 11 major categories of diagnoses based on the expertise of the research team. Secondary and additional medical diagnoses were transformed into the Charlson Index of Comorbidity,18 a measure of disease severity. The responses for many ordinal and scaled variables were not normally distributed so indicator or dummy variables were created with “yes” and “no” answers with the reference group equaling “none.” For instance, the frequency of an intervention was divided into low (1 to 10), moderate (11 to 50), and high (> 50). “No interventions” was established as the reference for comparing results in the models.
Outcome Variables
Outcomes variables were created for improvement in UI and BI by comparing the patient's status at discharge with the admission status. Improvement was recorded as a 1 for yes and 0 for no improvement.
Statistical Analysis
Descriptive statistics were used to describe the sample and answer research questions 1 through 3 about the prevalence of incontinence on admission, percent improvement, and frequency of research-based interventions documented. Three different data sets were created for modeling associations of variables with outcomes: one for logistic regression analysis and two for data mining. The logistic regression data set included the dummy variables while the data mining data sets did not since data mining techniques discretized the data as part of analyzing the data. One data mining data set included categorical data and the second included continuous data. Both categorical and continuous data sets were used to test different logistic? models to find the best predictors for the outcomes. Models for improvement in urinary and bowel incontinence using stepwise logistic regression analysis were developed with PROC GEN MOD in SAS v9.1 that takes into account repeated episodes for some subjects. Candidate variables were screened for inclusion in the models using Chi-Square and were retained if the significance level of their association with the outcome was p ≤ .1. The final model included variables associated of the outcome if they were significant at p ≤ .05.
Four different data mining decision trees for each outcome were created using the J48 algorithm in the Weka software (Version 3.5.1). Data mining is an analytic step that builds on traditional statistics, but incorporates artificial intelligence and semi-automated processing of data to discover the association of variables with outcomes. One method of data mining is development of a decision tree that yields rules or steps that can guide clinical decision-making.19 Results may vary between the two methods and provide different insights about the association of variables to the outcomes for UI and BI. The four trees were constructed from 1) all variables represented as categorical data; 2) a subset of selected variables represented as categorical data; 3) all variables represented as continuous data; and, 4) a subset of selected variables represented as continuous data. This approach was used because the large number of variables could produce overfitted trees, in which a random association of variables for correctly predicting outcomes cannot be validated when applying the model to another set of data. Subsets of variables were created by combining results from selection of variables based on their association with the outcomes, called conditional feature selection. Two different search algorithms were used to do this: Best-First and Greedy Stepwise. The Best-First search looks for the “best” variable first, then the second best, and so forth, until some classification accuracy threshold is met. Greedy Stepwise search is faster than Best-First and uses a similar approach, but can miss some important variables. Both search methods were used to optimize the selected variable set.
A 10-fold cross-validation method was used to create the decision trees. In this procedure, the dataset was split into 10 equal partitions (folds). A training data set representing nine folds is used to create the model which is then tested on the tenth. This procedure is repeated until each of the folds has been used as a testing set and the results are averaged over the ten iterations. The goal is to create a parsimonious decision tree that has the highest accuracy (expressed as percent of correctly classified episodes of care). Measures to evaluate the usefulness of a decision tree include the number of leaves (nodes) in a tree (fewer is better), percent of correctly classified episodes of care for the outcome of interest, the true positive and false positive rates for correctly classifying records, and the area under the receiver operating curve (AU ROC). A true positive rate is the percent of time episodes of care are correctly for improvement in the outcomes while the false positive rate is the percent of time episodes of care are classified as improvement when in fact that are not associated with improvement. Correctly classifying patients ideally ranges from 70% to 100%; the closer the true positive rate is to 1 and the false positive rate is to 0, the better the decision tree. The AU ROC is the probability of correctly classifying episodes of care for improvement in the outcome based on the relationship between the true and false positive rates. The closer the AU ROC is to 1, the better the model.
Results
Of the original 4,242 episodes of care in the data set from 15 home health agencies, there were 1,793 patients with 2,072 (49%) episodes of care with a discharge from the agency. One hundred sixteen (6.5%) of patients had more than one episode of care, ranging from 1 to 5 episodes per patient. Patients in this study were primarily elderly Caucasians (98.6%) and female (64%). The mean age was 74 ± 14 years (mean ± SD). Most episodes represent patients discharged from an inpatient facility (79%). The home health length of stay ranged from one day to more than 1 year; the median length of stay was 25.9 days. Medicare was the most frequent payor (78%).
The most frequent primary diagnoses are shown in Table 3. Neurological diseases (neuropathies, degenerative disorders, etc) were the most frequent primary diagnoses associated with both UI and BI. Only two other primary diagnoses groups represented at least 5% of patient episodes for UI, congestive heart failure and mild gastrointestinal symptoms. Three gastro-intestinal diagnoses categories represented about one-fifth of bowel incontinence episodes (Table 3). Risk factors for incontinence identified in the literature are listed in Table 4 with the frequency of episodes for each risk factor.
Table 3.
Percent of the Most Frequent Primary Diagnosis Groups by Episode for Each Outcome
| Primary diagnosis group | Urinary Incontinence | Bowel Incontinence |
|---|---|---|
| Neurological diseases, (neuropathies, degenerative disorders, etc) | 24% | 15% |
| Gastro-intestinal (GI) cancers | 7% | |
| Gastro-intestinal (GI), mild symptoms/ fatigue | 6% | |
| Other Stomach/ intestinal disease | 6% | |
| Respiratory, other (pneumonia, influenza, etc) | 4% | 6% |
| Cerebral vascular disease (CVA), acute | 6% | |
| Therapy/ post-surgery care (e-codes) | 6% | |
| Congestive heart failure (CHF), non-hypertensive | 5% | |
| Joint Disease (arthritis, back problems, contractures, etc.) | 5% | 4% |
| All other diagnoses | 58% | 40% |
| Total percent all episodes | 100% | 100% |
Table 4.
Patient and Support System Characteristics by Outcome
| Evidennce-Based Predictors | Urinary Incontinence | Bowel Incontinence | ||
|---|---|---|---|---|
| Number | Percent | Number | Percent | |
| Urinary incontinence | 684 | 100% | 103 | 55% |
| Bowel incontinence | 103 | 15% | 187 | 100% |
| Prior urinary incontinence | 417 | 61% | 75 | 40% |
| Ambulation assistance | 267 | 39% | 105 | 56% |
| Cognitive impairment | 226 | 33% | 80 | 43% |
| Toileting assistance | 219 | 32% | 58 | 31% |
| Obesity | 171 | 25% | 32 | 17% |
| Heavy smoking | 41 | 6% | 11 | 6% |
| Prior catheter | 41 | 6% | 7 | 4% |
| Pressure ulcer | 34 | 5% | 15 | 8% |
| IV, Parenteral, or Enteral Therapy | 27 | 4% | 13 | 7% |
| Lives alone | 267 | 39% | 50 | 27% |
| None or no single primary caregiver | 144 | 21% | 32 | 17% |
As shown in Table 4, double incontinence (UI and BI) occurred in 103 episodes of care; 15% of patients with UI had BI and 55% of patients with BI also had UI. The small sample size for double incontinence or bowel incontinence prohibited separate analysis. The most frequent factors associated with any incontinence outcomes were: prior urinary incontinence, cognitive impairment, needing assistance for ambulation and toileting, or obesity.
Six hundred eighty-four (33%) of the 2,072 episodes of care, represented patients with UI present on admission. In addition, 187 episodes (9%) had BI on admission. Two hundred sixty-three (38%) of the 684 patient episodes with UI and 84 (45%) of those with BI improved by discharge.
Data analysis revealed a total of 265,966 interventions for all episodes of care, including 118,329 interventions for UI and 39,579 interventions for BI. Table 5 lists the 23 interventions clusters for UI and BI and the frequency of each cluster. The frequency of documenting research-based interventions for UI ranged from 3% to 21.8%; the frequency for BI ranged from 6.9% to 35.3%.
Table 5.
Comparison of Interventions for Outcomes by Clusters of Omaha System Interventions*
| Action | Description | Further Description | % Episodes for Urinary Incontinence | % Episodes for Bowel Incontinence |
|---|---|---|---|---|
| Monitoring | Injury Prevention | Includes Mobility/ Functional Status | 21.8 | 35.3 |
| Monitoring | Genitourinary/ Bowel Function & Other | Also includes Environment, Nutrition, Other Foci | 8.6 | 12.9 |
| Monitoring | Medications | 6.7 | 7.9 | |
| Monitoring | Respiration & Circulation | 9.8 | 10.6 | |
| Monitoring | Pain | 7.9 | 9.1 | |
| Monitoring | Emotional/Cognitive | 3.9 | 8.0 | |
| Monitoring | Skin/ Wound | 1.1 | 1.1 | |
| Treatment | Injury Prevention | Includes Mobility/ Functional Status | 13.2 | 13.7 |
| Treatment | Bowel & Bladder | 3.0 | 6.9 | |
| Treatment | Medications | 5.0 | 6.6 | |
| Treatment | Skin/ Wound care | 9.5 | 12.6 | |
| Treatment | Other | 9.2 | 9.7 | |
| Treatment | Respiration & Circulation | 1.7 | 3.7 | |
| Treatment | Pain | 0.8 | 1.0 | |
| Teach | Disease Treatment | Includes Bladder or Bowel Care, Nutrition, Other Foci | 12.8 | 15.4 |
| Teach | Disease Process | 12.4 | 10.7 | |
| Teach | Medications | 8.8 | 7.9 | |
| Teach | Respiration & Circulation | 6.6 | 5.5 | |
| Teach | Emotional/Cognitive | 4.3 | 3.3 | |
| Teach | Other | Includes Nutrition | 6.8 | 5.9 |
| Coordinate | Supplies & Equip | 2.9 | 3.0 | |
| Coordinate | Resources | 6.1 | 9.9 | |
| Coordinate | Other | 9.9 | 10.3 |
Gray shading indicates EBP interventions found in the literature.
Logistic Regression Results
There were 684 episodes of care for improvement in urinary incontinence. Using Chi-Square analysis, 83 candidate variables (p ≤ 0.1) were identified for inclusion in the final model. Neither patient nor support system characteristics were significantly associated with improvement; only interventions were significant as shown in Table 6.
Table 6.
Predictive Model for Improvement in Urinary Incontinence
| Associated variables | Frequency | Action | OR (95% CI) | P-value |
|---|---|---|---|---|
| Disease Process | Moderate | Teach | 2.86 (1.07, 7.68) | 0.04 |
| Skin/ Wounds | Low | Treatment | 2.58 (1.11, 5.61) | 0.02 |
| Skin/ Wounds | Moderate | Monitoring | 0.13 (0.02, 0.93) | 0.04 |
| Respiration & Circulation | Low | Teach | 0.21 (0.05, 0.82) | 0.02 |
| Respiration & Circulation | High | Teach | 0.15 (0.02, 1.02) | 0.05 |
| Genitourinary/ Bowel Function & Other | Moderate | Monitoring | 0.18 (0.05, 0.59) | <0.01 |
| Medications | High | Teach | 0.02 (0.00, 0.16) | < 0.01 |
Patients were almost three times more likely to improve if they received a moderate frequency of Teaching about their Disease Process (interventions in this category were documented 11 – 50 times during the episode of care) compared with no Teaching. Interventions for skin and wound care varied in their association with improvement of UI. A low frequency of Treatment for Skin and Wounds increased their odds of improvement by almost 2.6 times while moderate frequency of Monitoring was associated with a decreased likelihood of improvement (87%). Either a high or low frequency for Teaching about Respiration and Circulation decreased the likelihood of improvement by 79% and 85%. A moderate frequency of Monitoring of Genitourinary / Bowel Function and Other” conditions or high frequency for Teaching about Medications resulted in a decreased likelihood of improvement in urinary incontinence by 82% and 98%.
There were 187 episodes of care for improvement in BI. Chi-Square analysis resulted in 112 candidate variables (p ≤ 0.1) for inclusion in the final model. In the final model, two types of interventions proved to be significantly associated with the outcome of improvement in bowel incontinence. Results are shown in Table 7. Patients were 6 – 7 times more likely to improve if they had any frequency of Teaching about Respiration and Circulation, however, the confidence intervals were large. Patients were 92% less likely to improve in BI if they had a low number of interventions for Monitoring of Emotional and Cognitive Status. No patient or support system variables were significantly associated with improvement in bowel incontinence.
Table 7.
Predictive Model for Improvement in Bowel Incontinence
| Associated Variables | Frequency | Action | OR | (95% CI) | P-value |
|---|---|---|---|---|---|
| Respiration & Circulation | Low | Teach | 6.39 | (1.53, 26.75) | .01 |
| Respiration & Circulation | Moderate – High | Teach | 7.34 | (1.17 – 46.03) | .03 |
| Emotional & Cognitive Status | Low | Monitoring | 0.08 | (0.01, 0.52) | <.01 |
Data Mining Results
Using the data mining feature selection methods previously described, there were eight features selected that were associated with improvement in UI: gender, receiving intravenous or infusion therapies, lives with paid help, physical aggression at discharge, emergent care for “other reason,” other bladder diagnoses, assistance needed for housekeeping, and providing injury prevention treatment. Creation of the four models resulted in correctly classifying the number of episodes of care for improvement in UI 57% to 62% of the time. The true positive rates for correctly classifying records ranged from .38 to .43 with false positives ranging from .28 to .51. The AU ROC ranged from .50 to .58.
There were more patients who had no improvement in urinary incontinence (n = 421) compared with those who had improvement (n = 263). As this imbalance could affect results, a subset of 263 episodes of care with no improvement stratified by agency was randomly selected. The analysis was redone with equal numbers of episodes with improvement and no improvement outcomes. The results were validated using a more conservative method than originally planned. Instead of the 10-fold procedure for splitting the data, a split of 66% of the records was used for training and 33% for testing the model. Due to the high degree of classification error, however, useful results were not obtained from the decision tree analysis despite these methodological adjustments. Therefore, no useful decision tree was generated.
Bowel Incontinence
Of the four models created using decision tree analyses, the full set of continuous variables produced the best results. On cross-validation, the number of records correctly classified was 75.4%. The true positive rate for improvement was .77 and the false positive rate for improvement was .26. The AU ROC was .77. Figure 1 shows the resulting decision tree. Decision trees are typically read from top to bottom with the top node (diamond shape) representing the variable that is most important in predicting improvement vs no improvement in the outcome (BI). Diamonds represent variables requiring a decision; the lines are links that point to either another diamond or an oval, which is the terminal node or end point for a decision of improvement or no improvement in BI. The link from one node (diamond) to the next are important in classification as they represent the order of decisions; traversing the various branches of the tree, one can construe rules in the form of IF (some condition) THEN (classification i.e. improvement or no improvement in BI).
Figure 1.
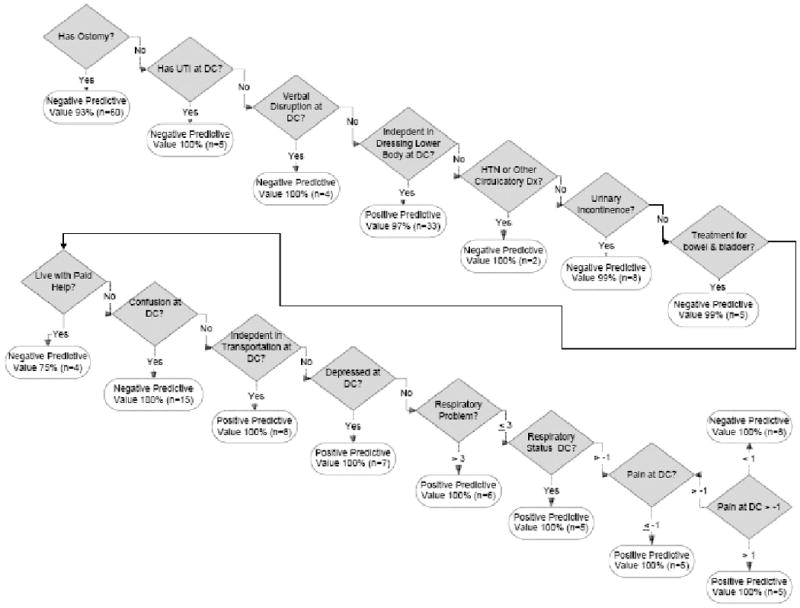
Decision tree to predict improvement in bowel incontinence
There are 15 variables represented by the diamonds and 16 terminal nodes represented by the ovals. From each variable are two lines representing a decision and the value of “yes” or “no” or actual number shown on the lines indicate the criteria for making a decision which branch to select. The ovals that are linked by each line show whether that path negatively or positively predicts, the accuracy of the prediction and the number or episodes of care affected by the prediction.
In this figure, the root node (Ostomy) is dichotomized as No/ Yes, and was selected by the software as the most important classification variable. One rule that can be inferred from this tree as: IF the patient has an Ostomy, THEN no improvement in BI occurred. There were 60 episodes affected by this rule and the rule is accurate 93% of the time. However, more complex rules can be inferred from this tree, simply by following a path through the branches. For example, following the right-hand link from the root node, down two additional levels of the tree, yields the rule: IF the patient does NOT have an ostomy AND IF the patient does NOT have a urinary tract infection at discharge and IF the patient has verbally disruptive behavior at discharge, THEN, there is no improvement in incontinence. Thus, subsequent rules include all previous rules in the decision tree; rules within a tree are dependent and cannot be interpreted in isolation. The rules inferred from decision trees can be used by clinicians as components in clinical guidelines for improving outcomes such as incontinence.
Discussion
The frequency of UI and BI were higher than rates for home health nationally, and rates of improvement for both outcomes were at the lower end of the national range9,10. Compared with the national prevalence of 26.7% for UI in 2006, 33% of patients in this study had UI at the start of an episode of care. The national prevalence for BI was 7.4%9, 10 compared with our study findings of 9%. Differences in our findings could be due to a slightly different time for comparison of results (2006 nationally vs 2004 in the study) or to the fact that this study also included non-Medicare or Medicaid patients while CMS requires data only for Medicare and Medicaid patients.
National risk adjusted rates for improvement in UI ranged from 31.0% to 64.0% and for improvement in bowel incontinence from 53.0% to 73.0% in 2004.20 In comparison, the rates for improvement in this study were 38% for urinary incontinence and 45% for bowel incontinence. The difference may be due a higher prevalence rate for urinary and fecal incontinence found in this study, a slightly different population as previously addressed, or the nonrandom selection of agencies for this analysis, as compared with a national population. While improvement in outcomes in this study appears low, it could also be due the fact that the risk outcomes were not risk adjusted similar to CMS.
One way to improve outcomes is providing care consistent with evidence-based practice (EBP) guidelines. For instance, investigators found that implementing an EBP management protocol in long term care improve outcomes and costs 21. However, clinicians must use their judgment to evaluate the appropriateness of evidence for practice, as there are inconsistencies across studies 13. In this study, EBP interventions were documented infrequently. Since these data were obtained from EHRs, one solution would be to add clinical decision support such as templates for guidelines or pathways to cue clinicians about selecting research-based interventions for follow up when a problem of incontinence is identified on admission. Use of EHR templates and other clinical decision support tools has been useful for compliance with EBP in other studies.22
Another purpose of this study was to discover patient and support system characteristics and nursing interventions that were associated with the likelihood of improvement in UI and BI for home health patients. Since the purpose was discovery rather than hypotheses testing, we included associated variables not supported in previous studies. Significant association of variables was found for improvement in UI status. Surprisingly, none of associations represented patient or support system characteristics; only interventions were associated with the likelihood of improvement for these outcomes. Studies cited in the background of this article identified patient and support system variables associated with urinary incontinence. Interventions included in this study, however, may have mediated (affected) the relationship between previously cited predictors and urinary incontinence.
Based on previous research, improvement in UI would be expected if clinicians provided interventions in the categories: 1) Monitoring for Genito-Urinary Function, 2) Bowel Status, 3) Nutrition, 4) Functional Status, 5) Cognition, 6) Environment, and 7) Medications.23, 24 Monitoring of Cognitive Function and Functional Status were not supported in our study and neither was teaching about nutrition, bladder care, and medications.13, 24, 25 These findings may reflect inadequate documentation of these interventions. Clinicians often monitor, teach, and provide treatment simultaneously for problems such as bladder care, but only document their findings once. The lack of support for the association between Teaching about bladder care and improvement in urinary incontinence is likely a reflection on the method of documentation rather than the lack of teaching. Patients with urinary incontinence frequently had primary diagnoses of neurological and respiratory diseases, as well as CHF, which reflect the primary reason for home care. The significant intervention of Teaching about Respiration and Circulation suggests that urinary incontinence is present in patients with other health problems and inadequate attention or documentation may be given to urinary incontinence. Co morbidities may be a factor; if UI is due to impaired mobility or other intervening factors, just focusing on UI won't solve problem – immobility needs to be addressed. Another example is that if diabetes mellitus exists and blood sugars are not well managed, UI/BI may worsen. Clinicians need to carefully assess and document interventions for improving urinary incontinence in addition to addressing the primary reason for home care.
Monitoring of Skin and Wound problems as well as Treatments for Skin or Wound were significantly associated with an improvement in UI. This is not surprising, as incontinence associated dermatitis is a complication of urinary incontinence 26. One interpretation of these significant associations is that interventions to improve UI may not be initiated unless skin damage develops. Our study lacks details about the type of skin or wound treatments and these associations should be investigated in future studies.
A decision tree could not be created for improvement of UI in this study. When a decision tree is created, the data are partitioned into multiple sets (folds) for testing and validating results. It may be that there are infrequent but influential clinical conditions, such as severe cognitive impairment, that appear in both the test and validation sets. When clinical conditions occur infrequently, it is difficult to construct rules that provide a high level of correctly classifying patients for improvement in urinary incontinence. The lack of a decision tree indicates that a larger data set may be necessary to detect important but infrequent conditions or another method of analyzing the data should be considered in the future. It is also possible, no tree would result because too many variables are involved and more stringent criteria are needed to decrease the number of variables in the model.
For patients with BI, logistic regression and decision tree analysis yielded overlapping and unique results for improvement in BI. Logistic regression included interventions while the decision tree primarily addressed patient and support system characteristics. Both methods determined that characteristics of interventions for emotional and cognitive functioning, functional status, or physiological variables were associated with improvement in BI. Computerized documentation can help with decision making building on rules identified in this study, particularly when multiple decision points are needed to correctly predict improvement in outcomes, such as BI. Additionally, studies such as ours are a first step toward developing decision rules for practice-based evidence to improve outcomes.
In this study, the frequency plus the type of intervention determined the association of interventions with outcomes. It may seem logical to assume that a high frequency of an intervention would be associated with a better outcome. However, a high frequency of Teaching about Medications and Respiration and Circulation was associated with a lower likelihood of improvement in UI. There are several plausible explanations for this association; patients may have a new condition, are not retaining education about medications, or they are more unstable. The association between low to moderate frequency of interventions and the likelihood of improvement in urinary incontinence was not clear; these frequencies for interventions were associated with both an increased and decreased likelihood of improvement for both urinary and bowel incontinence. The frequency associated with an intervention could be a spurious result and further research is needed to investigate not only if the frequency of interventions matter but also the timing of interventions.
Limitations
There are several limitations of this study. Inconsistencies with documentation in the EHR are known problems27 and may have influenced results. There are methods for future studies that could improve consistency in documentation including training clinicians or developing charting guidelines or computerized templates that include EBP guidelines. The later recommendation is especially important for outcomes such as incontinence when it may not be the main reason for providing home health. The relatively small sample size compared with the number of variables required collapsing predictive variables. This may have contributed to our inability to create a decision tree for UI. Analysis without this collapsing of variables may have revealed different results. Another limitation in this study is the lack of randomization in selection of agencies, limiting the generalizability of findings. We failed to produce a decision tree for UI.
Conclusions
The prevalence for UI and BI in this study were higher than published national prevalence rates. The improvement rate for UI fell within national ranges for UI, but was lower than national rates for BI. We found that EBP interventions were documented infrequently. It is unclear if this finding reflects inconsistent documentation or that in fact, EBP interventions were not performed. Logistic regression analysis detected factors associated with an increased or decreased likelihood of improvement for incontinence including: Teaching about Disease, Treating or Monitoring Skin or Wounds, Teaching about Respiration & Circulation, and Medications and Monitoring Emotional & Cognitive Issues. A decision tree was generated for bowel incontinence but not urinary incontinence. It is possible that the sample size and number of variables in the study may have masked clinical conditions that could be useful in creating decision rules for improvement in urinary incontinence; at this time we are unable to know the reasons for the lack of a tree developing. Several possible reasons were offered above. Based on the high prevalence, but low rates of improvement for UI and BI, employment of a certified wound, ostomy, and continence nurse (WOCN) may benefit patients in home health for improving incontinence outcomes and preventing complications. At this time, there is little research supporting the association of certified WOCNs with improved outcomes; while this is a possibility it needs further study.
Key Points.
The prevalence of UI on admission in this study was 33% and the prevalence of BI on admission was 9%.
At discharge, improvement in urinary incontinence was 38% and for bowel incontinence, it was 45%.
Significant associations were found for interventions both for an increased or a decreased likelihood of incontinence.
A decision tree for classifying patients for improvement in bowel incontinence was created, correctly classifying 75.4% of patient episodes of care.
Acknowledgments
This study was supported by the National Institute of Nursing Research (Grant #P20 NR008992; Center for Health Trajectory Research). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
References
- 1.Aspden P, Corrigan JM, Wolcott J, Erickson SM, editors. Patient Safety: Achieving a New Standard for Care. Washington, DC: Institute of Medicine: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 2.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid. MedQIC: Medicare Quality Improvement Community. [11/25/2006];2006 Available at: http://www.medqic.org.
- 4.Marziali E, Serafini JM, McCleary L. A systematic review of practice standards and research ethics in technology-based home health care intervention programs for older adults. J Aging Health. 2005;17:679–696. doi: 10.1177/0898264305281100. [DOI] [PubMed] [Google Scholar]
- 5.Shaughnessy PW, Crisler KS, Schlenker RE. Outcome-based quality improvement in home health care: The OASIS indicators. Qual Manage Health Care. 1998;7:58–67. doi: 10.1097/00019514-199807010-00007. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. Home Health Quality Initiatives: OASIS C. [March, 2009]; Available at: http://www.cms.hhs.gov/HomeHealthQualityInits/06_OASISC.asp.
- 7.Martin KS, Elfrink VL, Monsen KA. The Omaha System: Solving the Clinical Data-Information Puzzle. [October 26, 2008]; Available at: http://www.omahasystem.org/
- 8.Centers for Medicare & Medicaid Services. Outcome and ASsessment Information Set Implementation Manual: Implementing OASIS at a Home Health Agency to Improve Patient Outcome. [January 20, 2009]; Available at: http://www.cms.hhs.gov/HomeHealthQualityInits/
- 9.Abrams P, Cardozo L, Khoudy S, Wein A, editors. Incontinence. Second. Plymouth, England: Plymbridge Distributors; 2000. [Google Scholar]
- 10.Soderland D. State and national case mix data. Minneapolis, MN: Stratis Health. State and National Case Mix Data. 2006:1–3. [Google Scholar]
- 11.Brown J, et al. Proceedings of the national institute of diabetes and digestive and kidney diseases international symposium on epidemiologic issues in urinary incontinence in women. American Journal of Obstetrics & Gynecology. 2003;188:S77–S88. doi: 10.1067/mob.2003.353. [DOI] [PubMed] [Google Scholar]
- 12.Tariq SH. Fecal incontinence in older adults. Clin Geriatr Med. 2007;23:857–869. doi: 10.1016/j.cger.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ. evidence Report/Technology assessment no 161 (prepared by the Minnesota evidence-based practice center under contract no 290-02-0009.) Rockville, MD: Agency for Healthcare Research and Quality; 2007. Prevention of fecal and urinary incontinence in adults. AHRQ Publication No. 08-E003. [Google Scholar]
- 14.Shimanouchi S, Kamei T, Hayashi M. Home care for the frail elderly based on urinary incontinence level. Public Health Nurs. 2000;17:468–473. doi: 10.1046/j.1525-1446.2000.00468.x. [DOI] [PubMed] [Google Scholar]
- 15.Landefeld CS, Bowers BJ, Feld AD, et al. National institutes of health state-of-the-science conference statement: Prevention of fecal and urinary incontinence in adults. Ann Intern Med. 2008;148:449–W99. doi: 10.7326/0003-4819-148-6-200803180-00210. [DOI] [PubMed] [Google Scholar]
- 16.Shaughnessy PW, Crisler KS, Hittle DF, Schlenker RE. VOLUME 1, POLICY AND PROGRAM OVERVIEW, in the Report Series Entitled, OASIS and Outcome-Based Quality Improvement in Home Health Care: Research and Demonstration Findings, Policy Implications, and Considerations for Future Change. Denver, CO: Center for Health Services Research University of Colorado Health Sciences Center; 2002. [Google Scholar]
- 17.AHRQ. Clinical Classifications Software (CCS) for ICD-9-CM. [February 16, 2009]; Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 18.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.DeGruy KB. Healthcare applications of knowledge discovery in databases. J Healthc Inf Manag. 2000;14:59–69. [PubMed] [Google Scholar]
- 20.Centers for Medicare & Medicaid Services. OASIS - Based Home Health Agency Patient Outcome and Case Mix Reports. [December 13, 2008]; Available at: http://www.cms.hhs.gov/OASIS/09a_hhareports.asp.
- 21.Frantz RA, Xakellis GC, Jr, Harvey PC, Lewis AR. Implementing an incontinence management protocol in long-term care. clinical outcomes and costs. J Gerontol Nurs. 2003;29:46–53. doi: 10.3928/0098-9134-20030801-10. [DOI] [PubMed] [Google Scholar]
- 22.Bryan C, Boren SA. The use and effectiveness of electronic clinical decision support tools in the ambulatory/primary care setting: A systematic review of the literature. INFORM PRIM CARE. 2008;16:79–91. doi: 10.14236/jhi.v16i2.679. [DOI] [PubMed] [Google Scholar]
- 23.Registered Nurses' Association of Ontario. Promoting continence using prompted voiding. (revised) [February 13, 2009];Nursing Best Practice Guidelines Program [serial online] 2005 [Google Scholar]
- 24.Dowling-Castronovo A, Bradway C. Urinary incontinence (UI) in older adults admitted to acute care. [February 13, 2009];Evidence-based geriatric nursing protocols for best practice. doi: 10.1016/s0197-4572(98)90047-7. Available at: http://www.consultgerirn.org/topics/urinary_incontinence/want_to_know_more. [DOI] [PubMed]
- 25.Dumoulin C, Hay-Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2006 doi: 10.1002/14651858.CD005654. [DOI] [PubMed] [Google Scholar]
- 26.Gray M, Bliss DZ, Doughty DB, ErmerSeltun J, KennedyEvans KL, Palmer MH. Incontinence-associated dermatitis: A consensus. JWOCN. 2007;34:45–56. doi: 10.1097/00152192-200701000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Westra BL, Oancea CS, Savik K, Marek KD. The feasibility of integrating the omaha system data across homecare agencies and vendors. CIN. doi: 10.1097/NCN.0b013e3181d7812c. Accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2004 doi: 10.1002/14651858.CD001308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eustice S, Roe B, Paterson J. Prompted voiding for the management of urinary incontinence in adults. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2000 doi: 10.1002/14651858.CD002113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ostaszkiewicz J, Johnston L, Roe B. Timed voiding for the management of urinary incontinence in adults. [February 13, 2009];The Cochrane Database of Systematic Reviews [serial online] 2004 doi: 10.1002/14651858.CD002802.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunn S, Kowanko I, Paterson J, Pretty L. Systematic review of the effectiveness of urinary continence products. Journal of Wound, Ostomy & Continence Nursing. 2002;29:129–142. doi: 10.1067/mjw.2002.123646. [DOI] [PubMed] [Google Scholar]
- 32.Alhasso AA, McKinlay J, Patrick K, Stewart L. Anticholinergic drugs versus non-drug active therapies for overactive bladder syndrome in adults. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2006 doi: 10.1002/14651858.CD003193.pub3. [DOI] [PubMed] [Google Scholar]
- 33.Thomas LH, Cross S, Barrett J, et al. Treatment of urinary incontinence after stroke in adults. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2008 doi: 10.1002/14651858.CD004462.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Institute of Diabetes and Digestive and Kidney Diseases. Fecal incontinence. Bethesda, MD: National Digestive Diseases Information Clearinghouse; 2007. NIH Publication No. 07–4866. [Google Scholar]
- 35.Tjandra JJ, Dykes SL, Kumar RR, et al. Standards practice task force of the american society of colon and rectal surgeons. practice parameters for the treatment of fecal incontinence. Dis Colon Rectum. 2007;50:1497–1507. doi: 10.1007/s10350-007-9001-x. [DOI] [PubMed] [Google Scholar]
- 36.Consortium for Spinal Cord Medicine. Neurogenic bowel management in adults with spinal cord injury. Washington, DC: Paralyzed Veterans of America; 1998. Updated 2005. [Google Scholar]
- 37.National Collaborating Centre for Acute Care. NICE clinical guideline [serial online] 2007. [February 13, 2009]. Faecal incontinence: The management of faecal incontinence in adults. [PubMed] [Google Scholar]
- 38.Khaikin M, Wexner SD. Treatment strategies in obstructed defecation and fecal incontinence. World J Gastroenterology. 2006;12:3168–3173. doi: 10.3748/wjg.v12.i20.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Norton CC, Cody JD, Hosker G. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2006 doi: 10.1002/14651858.CD002111.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Cheetham MJ, Brazzelli M, Norton CC, Glazener CM. Drug treatment for faecal incontinence in adults. [February 13, 2009];Cochrane Database of Systematic Reviews [serial online] 2002 doi: 10.1002/14651858.CD002116. [DOI] [PubMed] [Google Scholar]


