Abstract
Purpose: Medicare hospice is a valuable source of quality care at the end of life, but its lower use by racial minority groups is of concern. This study identifies factors associated with hospice use among urban Black and White nursing home (NH) decedents in the United States. Design and Methods: Multiple data sources are combined and multilevel logistic regression is utilized to examine hospice use among urban Black and White NH residents who had access to hospice and died in 2006 (N = 288,202). Results: In NHs, Blacks are less likely to use hospice than Whites (35.4% vs. 39.3%), even when controlling for covariates, interactions, and clustering of decedents in NHs and counties (adjusted odds ratio = 0.81, 95% confidence interval = 0.77-0.86). Variation in hospice use is greater among subgroups of Blacks than between Blacks and Whites, and these variations are predominantly due to individual-level factors, with some influence of NH-level factors. Hospice use is higher for Blacks versus Whites with do-not-resuscitate orders and lower for Blacks versus Whites with congestive heart failure (CHF). Additionally, hospice use is greater among Blacks with versus without do-not-resuscitate or do-not-hospitalize orders or cancer and those in low-tier versus other NHs. There was also lower hospice use among Blacks with versus without CHF. Implications: Efforts to reduce racial differences in hospice use should attend to individual-level factors. Heightening use of advance directives and targeting Blacks with CHF for hospice could be particularly helpful.
Keywords: End-of-life care, Race, Disparities
Introduction
At the end of life, hospice provides palliative care as an alternative to curative treatments. Since the enactment of the Medicare Hospice Benefit in 1982, the number of people dying under hospice has been increasing (Medicare Payment Advisory Commission [MedPAC], 2009). Among individuals dying in nursing homes (NHs), national rates of hospice use more than doubled from 1999 to 2006 (14% to 33%; Miller, Lima, Gozalo, & Mor, 2010). Currently over 80% of NHs contract with at least one hospice agency, thereby providing most NH residents access to hospice, and one-in-four hospice users live in an NH (Miller et al., 2010). Hospice eligibility requires terminal prognosis of six months or less and forfeiture of other Medicare benefits, including hospitalization and skilled nursing care for the terminal condition (National Hospice and Palliative Care Organization, 2009). Hospice use has been associated with improved care, including better pain management (Miller, Mor, Wu, Gozalo, & Lapane, 2002), and lower costs (Miller et al., 2004), particularly by reducing end-of-life hospitalizations (Gozalo & Miller, 2007). The increasing use and beneficial results of hospice make it a critical service. However, underutilization of hospice by minority racial groups (MedPAC, 2004) indicates that room for improving the equitability of hospice services exists.
Within and outside NHs, Whites use hospice at a greater rate than minority racial groups, including African Americans (Connor, Elwert, Spence, & Christakis, 2008). Differences in hospice use between Blacks and Whites in the general population have dissipated over time (Han, Remsburg, & Iwashyna, 2006), but racial differences in hospice use in NHs have been found to persist, for instance, among dual-eligible (Medicare and Medicaid) NH decedents in Florida (Kwak, Haley, & Chiriboga, 2008). This study examines hospice use among urban NH decedents nationally and identifies factors associated with racial differences in hospice use.
Though explanations of racial differences in hospice use highlight individual preferences, suggesting Blacks prefer more aggressive (rather than palliative) end-of-life treatments (Fishman et al., 2009), characteristics of health care organizations and communities might also influence racial differences in hospice utilization (Connor et al., 2008). A study of hospice use among individuals who died in an NH between 1995 and 1997 shows NH attributes, such as aggregate resident payment sources, and community characteristics, including the number of NH beds in the county, influence the likelihood of hospice use (Gozalo & Miller, 2007). The influence of NH and community factors on racial differences in hospice use, however, has not been examined.
Individual, NH, and county characteristics have been found to influence hospice utilization, but no national studies have quantified the influence of all three levels of factors on racial differences in hospice use. Prior studies of racial differences in hospice utilization among NH decedents focus on narrow subsets of the population, such as dual-eligible decedents in a single state (Kwak et al., 2008), or reflect trends from earlier decades (Greiner, Subashan, & Ahluwalia, 2003). We examine racial differences in hospice utilization among recent (2006) NH decedents nationally and account for individual-, facility-, and county-level factors.
An Ecological Conceptual Framework
Multiple levels of factors have been found to influence hospice use, including individual, facility, and county characteristics. Accordingly, the literature on hospice use parallels the perspective of the ecological framework, in which individuals are recognized as embedded within mezzo-social environments, such as NHs, and more macro-social environments, such as counties (Bronfenbrenner, 1986). The ecological framework has been utilized to examine how various levels of factors influence end-of-life care among NH residents and to inform research agendas and policy reforms (Blevins & Deason-Howell, 2002). An ecological perspective also guided examination of short hospice stays, revealing patient, family, and provider factors effect timing of hospice uptake (Waldrop, 2006). Our study extends this literature by considering racial differences in hospice utilization among NH decedents in an ecological framework. Motivated by this framework, we utilize a multilevel modeling approach to account for the clustering of individuals within NHs and counties.
Individual, NH, and county variables are included in our conceptual framework based on prior research. Numerous individual factors, including gender, marital status, education, diagnoses, and advance directives, have been found to influence the likelihood of hospice use and several are associated with racial differences in hospice use among NH decedents. Women, individuals who are married, and individuals with more education are more likely to use hospice (Gozalo & Miller, 2007; Greiner et al., 2003), and these effects have been found to hold for White, but not Black, NH decedents (Kwak et al., 2008). Additionally, individuals whose principal cause of death is cancer are more likely to use hospice, but principal cause of death has been found to explain nearly twice as much variance in hospice use for Black versus White NH decedents (Kwak et al., 2008). Research also shows that NH residents with advance directives—including do not resuscitate (DNR) or do not hospitalize (DNH) orders, a living will, or durable power of attorney—are more likely to use hospice (Casarett, Hirschman, & Henry, 2001; Gozalo & Miller, 2007; Greiner et al., 2003). However, Black NH residents are less likely than Whites to have advance directives (Levy, Fish, & Kramer, 2005; Resnick, Schuur, Heineman, Stone, & Weissman, 2008; Rich, Gruber-Baldini, Quinn, & Zimmerman, 2009). Furthermore, for NH decedents, shorter NH stays are negatively associated with hospice use (Kwak et al., 2008). Given this background, our conceptual framework includes all of the previously discussed individual factors.
Research suggests that several NH and county factors also might be associated with racial differences in hospice use, including factors associated with the likelihood that an NH resident will utilize hospice, end-of-life hospitalization (which hospice limits; Gozalo & Miller, 2007), and a NH's racial mix (e.g., the proportion of Black residents). We include each type of factor in our conceptual framework.
Relevant NH factors include resident payment sources, ownership, and quality. The percent of private-pay residents in an NH is positively related to the likelihood of hospice use among NH decedents (Gozalo & Miller, 2007), and the percent of Medicaid residents is associated with a NH's racial mix (Mor, Papandonatos, & Miller, 2005). We include the three primary NH payment sources (Medicaid, Medicare, and private pay) in our conceptual framework. Research also shows NH ownership is associated with hospitalization (Chou, 2002); therefore, a NH's profit status and chain affiliation are included in our conceptual model. Finally, research shows Blacks tend to live in lower quality NHs (Mor, Zinn, Angelelli, Teno, & Miller, 2004); we include quality in our conceptual model by examining each NH's number of health care deficiencies relative to all NHs in the state.
County factors in our conceptual model include several health care market attributes, particularly the availability of hospice, medical services, and long-term care beds. Regarding hospice availability, research shows growth in hospice providers is positively correlated with growth in hospice use among NH decedents (Miller et al., 2010). Additionally, the numbers of doctors and NH beds in a county are associated with the likelihood that an NH resident will utilize hospice (Gozalo & Miller, 2007).
The core aim of this study was to determine what factors, and what levels of factors (individual, NH, county), influence hospice use among urban Black and White NH decedents. Because individual—but not NH or county—factors have been found to be associated with racial differences in hospice use, we hypothesized that individual factors, including race, would have the strongest and most direct effect on hospice utilization (including racial differences in hospice use), followed by NH and county factors, respectively. Understanding the relationship between each level of factors and hospice use is necessary for developing well-informed strategies aimed at influencing hospice enrollment among NH decedents.
Design and Methods
Data Sources
Data from five sources were merged to create a multilevel database, in which decedents are nested within NHs and counties. Individual data were obtained from the Minimum Data Set (MDS) and Medicare files; NH data were obtained from the Online Survey, Certification, and Reporting (OSCAR) database; and county data were obtained from hospice provider of service (POS) files and the Area Resource File (ARF).
Selection of NHs and Decedents
For this study, we selected only NHs contracting with hospice to ensure all decedents could access hospice. Additionally, we selected only freestanding (e.g., non-hospital based) NHs with between 30 and 500 residents, excluding very small and large NHs, which may have different relationships with hospice providers on account of their size. We also included only NHs in non-rural areas, as indicated by the ARF, because hospice use substantially differs between urban and rural areas (Virnig, Moscovice, Durham, & Casey, 2004). We excluded NHs in counties with no other NHs (n = 5,286), and decedents in NHs with no other decedents in 2006 (n = 44), because at least two observations per higher level unit (e.g., decedents per NH) are required to evaluate multilevel models (discussed subsequently; Degenholtz & Bhatnagar, 2009). Only Black and White individuals who died over the age of 65 years in 2006 (in the NH or a hospital within seven days of NH transfer) were included. Among these decedents (326,514), cases were removed due to missing data (total removed: 36,839; 11.3%) on one or multiple factors.
Variables
To conduct this study, we used individual-level data from the 2006 MDS (version 2.0; transition to MDS 3.0 in 2010), including sex, age, marital status, education, advance directives, diagnoses, and length of NH stay. Age—a continuous variable in the MDS—was categorized into five groups (years): less than or equal to 75, greater than 75-80, greater than 80-85, greater than 85-90, and greater than 90 (Gozalo & Miller, 2007). In the MDS, marital status is categorized as married, widowed, divorced, separated, or never married. Previous study of hospice use among NH decedents examines marital status as married versus unmarried (Kwak et al., 2008). We categorize marital status into three groups (married, widowed, and single) retaining widowed separately because widowed individuals have been found less likely than married individuals to use hospice (Greiner et al., 2003). Education is categorized as less than high school, high school, or at least some college. Four advance directives are included as dichotomous variables, indicating whether decedents had a DNR order, a DNH order, a living will, or a durable power of attorney. Five prevalent diagnoses also are included: cancer, Alzheimer's disease (Alz.), non-Alz., dementia, congestive heart failure (CHF), and stroke. We also included a dichotomous variable for decedent's length of NH stay, with the commonly utilized cutoff at 90 days (Gozalo & Miller, 2007; Miller et al., 2004).
Facility-level variables were drawn from the OSCAR database or aggregated from the MDS. Dichotomous variables indicate if the NH was chain-affiliated or for-profit. A composite variable indicates if the NH was low tier (resource poor), which required having over 85% Medicaid-pay residents, and under 8% Medicare-pay and 10% private-pay residents (Mor et al., 2004). Additionally, we include a dichotomous variable indicating if the number of health care deficiencies in the NH is greater the median number of health care deficiencies across all study NHs in the state.
County attributes were identified in the hospice POS files and the ARF. From the POS, we include the number of hospice providers in the county, categorized by quartile. The number of doctors, hospital beds, and NH beds, per 100 individuals aged over 65 years living in the county, and the percent of occupied NH beds were drawn from the ARF and are categorized by tercile.
Statistical Methods
Descriptive analyses were conducted for all decedents stratified by hospice use and race. Percentages and means with standard deviations are reported. Multivariate analyses utilized two-level nested models to account for correlation between data among individuals clustered within NHs and counties and to identify the extent to which variation in hospice use is explained by each level of factors.
Results of two multilevel logistic models of hospice use for decedents nested within NHs and counties, controlling for covariates and state fixed effects, are reported. Model 1 includes all covariates and Model 2 also includes several interaction terms with decedent race. Based on previous research, covariates were tested for interactivity with race in relation to hospice use, and interaction terms significantly related (p < .05) to hospice use are included in Model 2. Interaction effects—which represent differential effects of race or interactive covariates on hospice use—were calculated following a formula for concatenating the main effects of race and the covariates with the interaction terms (Jaccard, 2004). By including dichotomous indicator variables for all continental U.S. states and Washington, DC, with California as the reference, we control for unobserved state effects.
Results
In 2006, 288,202 deaths occurred in the study population of Black and White urban NH decedents. Decedents had lived in 8,732 NHs (90% of Medicare/Medicaid certified urban NHs with any hospice use in 2006, and over half of all NHs nationally), located in 830 counties. Of all decedents, 112,184 (38.9%) used hospice. Attributes of decedents at the time of their last MDS assessment prior to death, NH attributes, and county characteristics are presented in Table 1.
Table 1.
Characteristics of NH Decedents in Study, by Hospice Use and Race
| Variables | All (N = 288,202) |
White (n = 263,109) |
Black (n = 25,093) |
|||
| No hospice (n = 176,018) | Hospice (n = 112,184) | No hospice (n = 159,803) | Hospice (n = 103,306) | No hospice (n = 16,215) | Hospice (n = 8,878) | |
| Decedent attributes | ||||||
| Women | 64.4% | 70.0% | 64.8% | 70.5% | 61.1% | 64.9% |
| Age | 85.7 ± 7.8 | 86.1 ± 7.7 | 86.0 ± 7.6 | 86.3 ± 7.5 | 83.1 ± 8.7 | 83.8 ± 8.8 |
| Married | 25.4% | 23.6% | 25.9% | 24.0% | 20.2% | 17.8% |
| Widowed | 58.6% | 61.8% | 59.1% | 62.2% | 53.2% | 56.5% |
| Single | 16.1% | 14.7% | 15.0% | 13.8% | 26.6% | 25.7% |
| <High school | 31.4% | 29.8% | 29.3% | 27.9% | 48.0% | 47.5% |
| High school | 44.1% | 44.6% | 45.0% | 45.5% | 34.4% | 34.1% |
| Some college | 24.5% | 25.6% | 25.6% | 26.7% | 13.6% | 13.5% |
| Power-attorney | 38.6% | 45.3% | 41.0% | 47.5% | 14.9% | 19.9% |
| DNR | 65.9% | 77.3% | 68.6% | 79.0% | 38.4% | 57.6% |
| DNH | 8.8% | 11.4% | 9.2% | 11.7% | 4.4% | 7.9% |
| Living will | 11.5% | 18.5% | 12.4% | 19.7% | 2.7% | 5.0% |
| Cancer | 6.0% | 11.5% | 6.0% | 11.3% | 6.0% | 13.5% |
| Alz. | 7.8% | 11.3% | 7.9% | 11.5% | 6.1% | 10.2% |
| Non-Alz. dementia | 18.0% | 24.1% | 18.1% | 24.1% | 17.5% | 25.2% |
| CHF | 30.5% | 26.3% | 30.7% | 26.4% | 28.7% | 24.0% |
| Stroke | 21.5% | 21.3% | 20.3% | 20.4% | 32.7% | 32.0% |
| Long stay (>90 days) | 68.5% | 81.8% | 68.1% | 81.5% | 72.9% | 84.4% |
| NH attributes | ||||||
| Low tier | 2.4% | 2.5% | 1.9% | 1.9% | 7.8% | 9.4% |
| Chain-affiliated | 56.4% | 56.7% | 55.9% | 56.4% | 61.4% | 60.8% |
| For-profit | 70.7% | 68.5% | 69.7% | 67.6% | 80.5% | 79.3% |
| High deficiencies | 54.7% | 54.3% | 53.8% | 53.5% | 63.9% | 63.2% |
| County attributes | ||||||
| No. of hospices | 11.6 ± 12.1 | 12.8 ± 11.8 | 11.3 ± 11.8 | 12.6 ± 11.6 | 14.2 ± 14.7 | 15.3 ± 13.5 |
| No. of MDsa | 2.1 ± 1.3 | 2.1 ± 1.3 | 2.1 ± 1.3 | 2.1 ± 1.3 | 2.6 ± 1.4 | 2.6 ± 1.3 |
| No. of hospital bedsa | 2.2 ± 1.4 | 2.2 ± 1.4 | 2.2 ± 1.3 | 2.2 ± 1.4 | 2.9 ± 1.8 | 2.9 ± 1.8 |
| No. of NH bedsa | 4.8 ± 1.6 | 4.8 ± 1.6 | 4.8 ± 1.6 | 4.8 ± 1.7 | 4.8 ± 1.4 | 4.8 ± 1.5 |
| % Occupied NH beds | 87.4 ± 6.4 | 86.2 ± 7.0 | 87.5 ± 6.4 | 86.2 ± 7.0 | 87.1 ± 7.1 | 86.0 ± 7.2 |
Note: DNR = do not resuscitate; DNH = do not hospitalize; Alz. = Alzheimer's disease; CHF = congestive heart failure; NH = nursing home; MD = medical doctor.
Per 100 aged >65 years.
Descriptive results show a lower proportion of Blacks than Whites used hospice (35.4% vs. 39.3%), a slightly higher percentage of Blacks with cancer used hospice than Whites with cancer, and among Blacks but not Whites hospice use was more prevalent in low-tier NHs.
Multivariate Results
Table 2 presents results of the multilevel models, showing adjusted odds ratios (AORs) that indicate the strength and direction of the relationships between covariates and hospice use, as well as confidence intervals (CIs) that show the extent of variability across covariates in relation to hospice use. Model 1 includes all covariates, but no interaction terms, and thereby shows the overall adjusted relationships between every covariate and hospice use. According to Model 1, the likelihood of Black NH decedents using hospice is minimally less than that of Whites (AOR = 0.97, 95% CI = 0.94-1.01). Model 2 includes interaction terms, showing several covariates are associated with hospice use differently for Blacks and Whites. Five individual-level interaction terms (between race and DNR, DNH, cancer, CHF, and single marital status) and one cross-level interaction term (between race and low-tier NH) are significantly related to hospice use. When controlling for these interactions and all covariates, the likelihood of Black NH decedents utilizing hospice is lower than that of Whites (AOR = 0.81, 95% CI = 0.77-0.86). Testing of model fit was performed by comparing Akaike's Information Criterion (AIC) statistics for Models 1 and 2 and for a “null model” that includes only an intercept (Akaike, 1987). Comparison of the AIC across the three models, wherein smaller numbers indicate better fit, shows that Model 2 fit the data best (Model 2 AIC: 334120.7; Model 1 AIC: 334228.8; null model AIC: 352432.1).
Table 2.
Multilevel Models of Hospice Use by NH Decedents, With and Without Interactions
| AOR (95% CI) |
||
| Independent variables | Model 1 | Model 2 (Model 1 + interaction terms) |
| Decedent attributes | ||
| Race: Black | 0.97 (0.94-1.01) | 0.81 (0.77-0.86) |
| Sex: women | 1.22 (1.20-1.24) | 1.23 (1.20-1.25) |
| Age at death: <75 years | Ref | Ref |
| Age at death: >75-80 years | 0.97 (0.94-1.00) | 0.97 (0.93-1.01) |
| Age at death: >80-85 years | 0.94 (0.91-0.97) | 0.94 (0.90-0.97) |
| Age at death: >85-90 years | 0.92 (0.89-0.95) | 0.92 (0.89-0.95) |
| Age at death: >90 years | 0.87 (0.84-0.90) | 0.87 (0.84-0.90) |
| Married | Ref | Ref |
| Widowed | 0.96 (0.94-0.98) | 0.97 (0.95-0.99) |
| Single | 0.91 (0.88-0.94) | 0.90 (0.88-0.92) |
| <High school | 1.00 (0.98-1.02) | 1.00 (0.98-1.02) |
| High school | Ref | Ref |
| Some college+ | 1.01 (0.99-1.03) | 1.01 (0.99-1.03) |
| Power attorney | 1.12 (1.09-1.15) | 1.12 (1.10-1.14) |
| DNR | 1.83 (1.79-1.87) | 1.77 (1.73-1.81) |
| DNH | 1.47 (1.42-1.52) | 1.45 (1.35-1.43) |
| Living will | 1.26 (1.23-1.29) | 1.45 (1.41-1.50) |
| Cancer | 2.51 (2.42-2.59) | 2.47 (2.39-2.55) |
| Alz. | 1.25 (1.21-1.29) | 1.25 (1.19-1.25) |
| Non-Alz. dementia | 1.25 (1.22-1.28) | 1.25 (1.22-1.28) |
| CHF | 0.86 (0.84-0.88) | 0.87 (0.85-0.89) |
| Stroke | 0.96 (0.94-0.98) | 0.96 (0.95-0.99) |
| Long stay (>90 days) | 2.16 (2.11-2.20) | 2.16 (2.12-2.20) |
| NH attributes | ||
| For-profit | 0.94 (0.90-0.98) | 0.94 (0.90-0.98) |
| Low tier | 1.01 (0.92-1.10) | 0.96 (0.87-1.06) |
| Chain-affiliated | 1.07 (1.03-1.10) | 1.07 (1.03-1.10) |
| High deficiencies | 1.02 (0.98-1.04) | 1.01 (0.98-1.03) |
| County attributes | ||
| Bottom quartile of hospices | Ref | Ref |
| Second quartile of hospices | 1.39 (1.26-1.54) | 1.39 (1.26-1.54) |
| Third quartile of hospices | 1.58 (1.39-1.80) | 1.58 (1.39-1.80) |
| Top quartile of hospices | 1.73 (1.48-2.03) | 1.73 (1.48-2.03) |
| Low MDsa | 0.89 (0.80-0.99) | 0.89 (0.80-0.99) |
| Middle MDsa | Ref | Ref |
| High MDsa | 1.04 (0.93-1.17) | 1.04 (0.93-1.17) |
| Low hospital bedsa | 1.17 (1.02-1.25) | 1.13 (1.02-1.25) |
| Middle hospital bedsa | Ref | Ref |
| High hospital bedsa | 1.02 (0.91-1.15) | 1.04 (0.91-1.15) |
| Low NH bedsa | 0.98 (0.88-1.10) | 0.98 (0.88-1.10) |
| Middle NH bedsa | Ref | Ref |
| High NH bedsa | 1.00 (0.90-1.11) | 0.99 (0.90-1.11) |
| Low % occupied NH bedsa | 1.18 (1.05-1.32) | 1.18 (1.05-1.32) |
| Middle % occupied NH bedsa | Ref | Ref |
| High % occupied NH bedsa | 1.03 (0.93-1.13) | 1.03 (0.93-1.13) |
| Interaction terms | ||
| Black and single | n/a | 1.10 (1.01-1.17) |
| Black with cancer | n/a | 1.16 (1.04-1.29) |
| Black with CHF | n/a | 0.90 (0.84-0.97) |
| Black with DNR | n/a | 1.33 (1.25-1.42) |
| Black with DNH | n/a | 1.17 (1.02-1.33) |
| Black in low-tier NH | n/a | 1.20 (1.03-1.39) |
| Model validation results | ||
| Model 1 | Model 2 | |
| NH variance | 0.4677 | 0.4674 |
| NH-level correlation | 14.54% | 14.55% |
| County variance | 0.1781 | 0.1786 |
| County-level correlation | 4.58% | 4.02% |
| Log likelihood | -16,7028.41 | -16,6968.37 |
| AIC | 334228.8 | 334120.7 |
| Wald χ2 | 16,670.09 (83) | 16,768.13 (89) |
Note: AOR = adjusted odds ratio; NH = nursing home; CI = confidence interval; DNR = do not resuscitate; DNH = do not hospitalize; Alz. = Alzheimer's disease; CHF = congestive heart failure; MD = medical doctor; AIC = Akaike's Information Criterion; n/a = not applicable.
Per 100 aged >65 years.
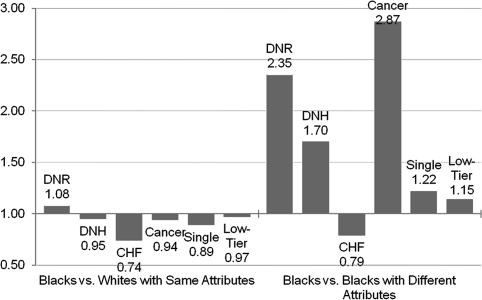
Figure 1 illustrates the interaction effects. Holding constant all covariates including the other interaction terms, several meaningful interactions are identified. The interaction effects show greater variation in hospice use among subgroups of Blacks than between Blacks and Whites. The differences in odds of hospice use between Blacks and Whites with the same characteristics (e.g., Blacks with DNR orders vs. Whites with DNR orders) are depicted on the left side of the figure, and differences in odds of hospice use between Blacks with and without specific characteristics (e.g., Blacks with cancer vs. Blacks without cancer) are depicted on the right side of the figure. The bar on the far left of the figure indicates the odds of using hospice are 8% greater for Blacks with DNR orders versus Whites with DNR orders. Additionally, the third bar from the left shows the odds of hospice use are 26% lower among Blacks with CHF versus Whites with CHF. Comparing Blacks by covariates, the bars on the right side of the figure show the odds of hospice use are over two times greater for Blacks with DNR orders, approximately 70% greater among Blacks with DNH orders, about 20% lower among Blacks with CHF, and nearly 15% greater among Blacks in low-tier versus higher-tier NHs.
Figure 1.
Interactions between race and covariates: the odds of hospice use for Blacks versus Whites and for Blacks with and without the covariate of interest.
Statistically significant clustering effects are identified at the NH and county levels. Of the total variability in outcomes, 2% is explained by county-level unobserved factors, whereas an additional 6.5% is explained by unobserved factors at the NH level. The remaining 91.5% of unexplained variance is over measurements within residents. State-fixed effects (not presented) indicate variation in hospice use exists across states. Of the 48 state indicator variables, 25 had significantly different hospice use than our reference state California at the p < .05 level, with AORs ranging from the highest value of 5.99 for Oklahoma to the lowest value of 0.11 for Vermont.
Discussion
There exists a 4% difference in hospice use between Blacks and Whites who died in urban U.S. NHs in 2006, and when controlling for covariates, interactions, and clustering of decedents in NHs and counties, the race difference is greater (AOR = 0.81, 95% CI = 0.77-0.86). However, although Blacks had an overall lower hospice utilization rate, there were circumstances in which subgroups of Blacks used hospice at slightly higher rates than comparable subgroups of Whites, for instance, among individuals with DNR orders. On the other hand, among Blacks and Whites with CHF, Blacks used hospice at a lower rate. Also, we found substantial variation in hospice use between Blacks, including higher hospice use among Blacks with versus without DNR or DNH orders or cancer, and those in low-tier versus other NHs. Additionally, there was lower hospice use among Blacks with versus without CHF. Broadly, findings show Black NH decedents are not a homogeneous group, depending on other factors Blacks have different propensities to enroll in hospice.
An ecological framework guided this study, drawing attention to the influence of individual, NH, and county factors on hospice use, as well as the correlation of data between decedents within NHs and counties. Consistent with prior research, however, we find individual-level factors have the strongest and most direct effect on racial differences in hospice use. Still, there are also meaningful effects of NH factors, particularly death in a low-tier (largely Medicaid) NH.
At the individual level, there are some notable differences by race regarding the factors associated with hospice use or the magnitude of their effect, especially advance directives and diagnoses at death. Regarding advance directives, Blacks with DNR orders are found to be more likely to use hospice than Whites with DNR orders, and Blacks with DNR or DNH orders are more likely to utilize hospice than Blacks without these advance directives. However, Black NH residents are less likely than Whites to have advance directives (Resnick et al., 2008), or even to have had advance directive discussions with NH staff (Rich et al., 2009). Regarding diagnoses at death, we find Blacks and Whites with cancer utilize hospice at similar rates, but Blacks with cancer are far more likely to use hospice than Blacks without cancer. In contrast, Blacks with CHF are found to be less likely to use hospice than both Whites with CHF and Blacks without CHF. These findings are consistent with research that identifies 41.0% lower odds of hospice use among Black versus White Medicare beneficiaries with end-stage heart failure (Givens, Tija, Zhou, Emanuel, & Ash, 2010). However, these findings vary from that of research that identifies no interaction between race and CHF in relation to hospice use among NH decedents in Florida (Kwak et al., 2008), and this variation may be due to differences in hospice utilization among CHF sufferers in Florida compared with those nationally. However, the interaction we identify reflects a persistent racial difference in the choice of treatment for chronic terminal illnesses. As previously noted, research indicates that Blacks prefer more aggressive end-of-life treatments than Whites (Fishman et al., 2009) and suggests racial differences in end-of-life care preferences may be due to mistrust of health care systems among Blacks (Degenholtz, Thomas, & Miller, 2003).
One NH factor is found to be interactive with race in relation to hospice use: Blacks in low-tier NHs are more likely to use hospice than Blacks in other NHs. This indicates that individuals who would otherwise be at risk of receiving poor care in low-tier NHs (Mor et al., 2004) are likely receiving better care through hospice (Miller et al., 2002). This cross-level interaction and the significant influence that clustering of decedents in NHs has on the variability of hospice use substantiate the relevance of the ecological framework, and the appropriateness of the multilevel modeling approach, for examining racial differences in hospice use.
The clustering of decedents in counties also helps explain variation in hospice utilization, suggesting that intra-county similarities exist between individuals with regards to hospice use. However, no county factors are associated with racial differences in hospice use, suggesting that community factors have minimal influence on racial differences in hospice use in NHs, the geographic scope of influential factors is more localized or more generalized than county-level, or county variables not in our analyses are of importance.
Implications
Several implications for policy, practice, and research follow from our findings. Most broadly, by highlighting the continued lower use of hospice by Black compared with White NH decedents, our findings support recent recommendations for revising hospice eligibility criteria to allow some level of “curative” care be permitted under hospice (Fishman et al., 2009; Landers, 2009). Enrollment in Medicare hospice currently requires forfeiture of other Medicare Part-A benefits when they are provided for the terminal condition (including hospital and skilled nursing facility [SNF] care), and this may deter hospice use particularly among Blacks. For Blacks, forfeiture of benefits/services could be especially unattractive, given individuals’ histories and fears of undertreatment in health care (Degenholtz et al., 2003). Accordingly, changing Medicare hospice policy to allow for simultaneous receipt of curative treatments and/or hospital and SNF care has the potential to reduce racial differences in hospice use. Examining the impact of such a change on overall hospice use, equity of use, and costs appears warranted (Landers, 2009) and will be supported by the “Medicare Hospice Concurrent Care Demonstration Program.” This demonstration will allow patients who are eligible for hospice to receive all other Medicare services simultaneously with hospice care (Congressional Research Service, 2010).
Because hospice care in NHs has been associated with higher quality end-of-life care, such as better pain management (Miller et al., 2002), it may follow that lower use of hospice by Black NH residents results in their receipt of a lower quality of care. However, whether hospice use similarly affects quality outcomes for Black and White NH residents has not been empirically tested. Accordingly, research comparing quality of care outcomes between Black and White hospice users could be an important next step.
Our findings of racial differences in hospice utilization associated with decedents’ diagnoses also have practice and research implications. Given the low likelihood of hospice use among Blacks with CHF, targeted hospice outreach to Blacks with CHF and other chronic terminal diseases also could help level racial differences in hospice use. Because Blacks with cancer are highly likely to utilize hospice, educational outreach efforts highlighting that hospice is for all terminally diagnosed Medicare beneficiaries and not just those with cancer could be helpful. Research examining facilitators and barriers of hospice use among Blacks with CHF also would be informative.
Our findings on the greater positive association between DNR and DNH orders and hospice use for Black versus White NH residents suggest that physicians and NH staff engaging in discussion about advance directives with NH residents might support racial equality in hospice use (Rich et al., 2009). Considering our findings, concerns are raised regarding certain changes occurring in NH care planning, particularly the national transition from MDS 2.0 to MDS 3.0, which entails the elimination of advance directive items. To the extent that removing these items from the MDS detracts from explicit discussion of advance directives between NH staff and residents, this change could have deleterious effects on advance care planning and hospice use among NH residents. Longitudinal research on advance care planning and hospice use among NH residents before and after implementation of MDS 3.0 could address these concerns.
We also found Blacks in low-tier versus other NHs were more likely to use hospice. Future research could examine the dynamics of hospice use in low-tier NHs to clarify the meaning of this finding. Potentially low-tier NHs engage hospice as a supplemental form of staffing, given their limited resources (Banaszak-Holl, Zinn, & Mor, 1996). Such a strategy could result in higher hospice use among Blacks because low-tier NHs disproportionately serve Blacks (Mor et al., 2004). Alternatively, low-tier NHs might have higher proportions of Black staff than upper-tier NHs, and Black residents might be better informed about hospice (and/or advance directives) by Black staff. Examination of these possibilities would be a valuable contribution to the literature.
Limitations of this cross-sectional study are acknowledged. Though we identified numerous associations between individual, NH, and county factors and hospice use, causality could not be identified. Longitudinal study of racial differences in hospice use is advised. Additionally, analyses relied on categorization of individuals’ races as Black or White, which obscures potential differences in hospice use between native-born and foreign-born Blacks, and ignores other racial/ethnic groups. Identifying factors that influence hospice use among all groups is important for supporting equitable end-of-life care. Also, we found substantial differences in hospice use between states. We controlled for state-level differences in calculating national findings, but did not examine the differences explicitly. Comparison of racial differences in hospice use across states could inform state policies for supporting racially equitable care. Furthermore, our data set was relatively rich, but several measures of interest were unavailable. The MDS includes no data on religious affiliation, but religion could be related to racial differences in care preferences. In some Christian views held among many African Americans, pain and suffering are essential aspects of spiritual commitment, but these beliefs contrast with hospice and palliative care philosophies (Crawley et al., 2000). A potentially important NH-level measure unavailable is the aggregate race of staff (e.g., percent of White staff). Racial differences between NH residents and staff are associated with various forms of racist behavior, and staff often avoid racist residents (Berdes & Eckert, 2001). Therefore, patterns of hospice referral might differ between NHs where residents and staff are racially similar versus racially dissimilar. To our knowledge, we examined all relevant county variables. However, examining variations in the geographic scope of decedent clustering, such as zip-code or state-level clustering, could be valuable. Finally, as a test between models, the AIC does not provide information for concluding whether a given model is a good fit for the data, but does permit identification of which tested model fits the data best. Unfortunately, the trade off in using our sophisticated multilevel model is that traditional tests of model fit cannot be applied.
Conclusions
This study makes several important contributions to the existing literature on racial differences in hospice use. It presents national data about hospice use among NH decedents, thus renewing attention to variations in end-of-life care and showing that racial differences in end-of-life care continue to exist nationally. By merging multiple data files, our analyses account for individual, facility, and community factors. This contribution is particularly important because few prior studies of racial differences in hospice use take into account NH-level factors; however, for NH decedents—who are a fourth of Medicare hospice users (Miller et al., 2010)—we found some NH characteristics to have a significant association with hospice use. Increasing hospice enrollment is a national priority with potentially substantial implications for quality of care and life and health care costs. Policy and practice initiatives aiming to increase hospice use among minority groups can be informed by our findings.
Funding
This research was made possible, in part, by the Shaping Long-Term Care in America Project funded by the National Institute on Aging (1P01AG027296) and by funding from the Agency for Health Care Research and Quality (R03HS016918, 5T32HS000011-24).
Acknowledgments
The authors wish to thank Drs Zhanlian Feng, Ramona Rhodes, and Natalie Leland for their assistance reviewing early drafts of the article.
References
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- Banaszak-Holl J, Zinn JS, Mor V. The impact of market and organizational characteristics on nursing care facility service innovation: A resource dependency perspective. Health Services Research. 1996;31:97–117. [PMC free article] [PubMed] [Google Scholar]
- Berdes C, Eckert JM. Race relations and caregiving relationships: A qualitative examination of perspectives from residents and nurse's aides in three nursing homes. Research on Aging. 2001;1:109–126. [Google Scholar]
- Blevins D, Deason-Howell LM. End-of-life care in nursing homes: The interface of policy, research, and practice. Behavioral Sciences and the Law. 2002;20:271–286. doi: 10.1002/bsl.486. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:726–742. [Google Scholar]
- Casarett DJ, Hirschman KB, Henry MR. Does hospice have a role in nursing home care at the end of life? Journal of the American Geriatrics Society. 2001;49:1493–1498. doi: 10.1046/j.1532-5415.2001.4911242.x. [DOI] [PubMed] [Google Scholar]
- Chou SY. Asymmetric information, ownership and quality of care: An empirical analysis of nursing homes. Journal of Health Economics. 2002;2:293–311. doi: 10.1016/s0167-6296(01)00123-0. [DOI] [PubMed] [Google Scholar]
- Congressional Research Service. Medicare provisions in the Patient Protection and Affordable Care Act (PPACA) 2010. Retrieved June 15, 2010, from http://www.aamc.org/reform/summary/crsmedicare052710.pdf. [Google Scholar]
- Connor SR, Elwert F, Spence C, Christakis NA. Racial disparity in hospice use in the United States in 2002. Palliative Medicine. 2008;22:205–213. doi: 10.1177/0269216308089305. [DOI] [PubMed] [Google Scholar]
- Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the African American community. Journal of the American Medical Association. 2000;19:2518–2521. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- Degenholtz HB, Arnold R, Meisel A, Lave JR. Persistence of racial disparities in advance care plan documents among nursing home residents. Journal of the American Geriatrics Society. 2002;50:378–381. doi: 10.1046/j.1532-5415.2002.50073.x. [DOI] [PubMed] [Google Scholar]
- Degenholtz HB, Bhatnagar M. Introduction to hierarchical modeling. Journal of Palliative Medicine. 2009;12:631–638. doi: 10.1089/jpm.2009.9595. [DOI] [PubMed] [Google Scholar]
- Degenholtz HB, Thomas SB, Miller MJ. Race and the intensive care unit: Disparities and preferences for end-of-life care. Critical Care Medicine. 2003;31:S373–S378. doi: 10.1097/01.CCM.0000065121.62144.0D. [DOI] [PubMed] [Google Scholar]
- Fishman J, O’Dwyer P, Lu HL, Henderson H, Asch DA, Casarett DJ. Race, treatment preferences, and hospice enrollment: Eligibility criteria may exclude patients with the greatest needs for care. Cancer. 2009;115:689–697. doi: 10.1002/cncr.24046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Givens JL, Tija J, Zhou C, Emanuel E, Ash AS. Racial and ethnic differences in hospice use among patients with heart failure. Archives of Internal Medicine. 2010;170:427–432. doi: 10.1001/archinternmed.2009.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozalo PL, Miller SC. Hospice enrollment and evaluation of its causal effect on hospitalization of dying nursing home patients. Health Services Research. 2007;42:587–610. doi: 10.1111/j.1475-6773.2006.00623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greiner KA, Subashan P, Ahluwalia JS. Hospice usage by minorities in the last year of life: Results from the National Mortality Followback Survey. Journal of the American Geriatrics Society. 2003;53:970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- Han B, Remsburg RE, Iwashyna TJ. Differences in hospice use between Black and White patients during the period 1992 through 2000. Medical Care. 2006;44:731–737. doi: 10.1097/01.mlr.0000215858.37118.65. [DOI] [PubMed] [Google Scholar]
- Jaccard J. Interaction effects in logistic regression. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- Kwak J, Haley WH, Chiriboga DA. Racial differences in hospice use and in-hospital death among Medicare and Medicaid dual-eligible nursing home residents. The Gerontologist. 2008;48:32–41. doi: 10.1093/geront/48.1.32. [DOI] [PubMed] [Google Scholar]
- Landers SH. The other medical home. Journal of the American Medical Association. 2009;301:97–99. [Google Scholar]
- Levy CR, Fish R, Kramer A. Do-not-resuscitate and do-not-hospitalize directives of persons admitted to skilled nursing facilities under the Medicare benefit. Journal of the American Geriatrics Society. 2005;53:2060–2068. doi: 10.1111/j.1532-5415.2005.00523.x. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission [MedPAC] Report to the Congress: New approaches in Medicare. 2004. Retrieved October 29, 2009, from http://www.medpac.gov/publications/congressional_reports/June04_Entire_Report.pdf. [Google Scholar]
- MedPAC. Report to the Congress: Medicare Payment Policy. 2009. Retrieved June 1, 2009, from http://www.medpac.gov/documents/Mar09_March%20report%20testimony_WM%20FINAL.pdf. [Google Scholar]
- Miller SC, Intrator O, Gozalo P, Roy J, Barber J, Mor V. Government expenditures at the end of life for short- and long-stay nursing home residents: Differences by hospice enrollment status. Journal of the American Geriatrics Society. 2004;8:1284–1292. doi: 10.1111/j.1532-5415.2004.52357.x. [DOI] [PubMed] [Google Scholar]
- Miller SC, Lima J, Gozalo PL, Mor V. The growth of hospice care in U.S. nursing homes. Journal of the American Geriatrics Society. 2010;58:1481–1488. doi: 10.1111/j.1532-5415.2010.02968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller SC, Mor V, Wu N, Gozalo P, Lapane K. Does receipt of hospice care in nursing homes improve the management of pain at the end-of-life? Journal of the American Geriatrics Society. 2002;50:507–515. doi: 10.1046/j.1532-5415.2002.50118.x. [DOI] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. Millbank Quarterly. 2004;82:227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Papandonatos G, Miller SC. End-of-life hospitalization for African American and non-Latino White nursing home residents: Variation by race and a facility's racial composition. Journal of Palliative Medicine. 2005;8:58–68. doi: 10.1089/jpm.2005.8.58. [DOI] [PubMed] [Google Scholar]
- National Hospice and Palliative Care Organization. The Medicare conditions of participation for hospice care. 2009. Retrieved May 28, 2010, from http://www.nhpco.org/files/public/COPS_RevisedSubpartBFG_0106.pdf. [Google Scholar]
- Resnick HE, Schuur JD, Heineman J, Stone R, Weissman JS. Advanced directives in nursing home residents aged >65 years: United States 2004. American Journal of Hospice & Palliative Care. 2008;25:476–482. doi: 10.1177/1049909108322295. [DOI] [PubMed] [Google Scholar]
- Rich SE, Gruber-Baldini AL, Quinn CC, Zimmerman SI. Discussion as a factor in racial disparity in advance directive completion at nursing home admission. Journal of the American Geriatrics Society. 2009;57:146–152. doi: 10.1111/j.1532-5415.2008.02090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virnig B, Moscovice I, Durham S, Casey M. Do rural elders have limited access to Medicare hospice services? Journal of the American Geriatrics Society. 2004;52:731–735. doi: 10.1111/j.1532-5415.2004.52213.x. [DOI] [PubMed] [Google Scholar]
- Waldrop DP. At the eleventh hour: Psychosocial dynamics in short hospice stays. The Gerontologist. 2006;46:106–114. doi: 10.1093/geront/46.1.106. [DOI] [PubMed] [Google Scholar]