Abstract
Purpose
The success of the Ponseti method for treating idiopathic clubfoot deformity is dependent on the casting techniques and the adherence of the patient to the foot abduction brace protocol. Newly developed brace designs claim to be more comfortable, to be easier to use and to prevent dislodgement of the foot from the brace, making them more efficient and improving patient compliance. They are, however, more costly, and, therefore, accessible to fewer patients. We compared the compliance and treatment outcome using two brace designs, the traditional simple brace of pre-walking shoes attached to a Dennis Browne (DB) bar and the new sophisticated Mitchell brace.
Methods
We compared the functional outcome and compliance with the post-corrective bracing protocol of 38 children with idiopathic clubfoot treated in our institution using two brace designs. Twenty-one chose the DB brace and 17 chose the Mitchell brace.
Results
There was no difference in the compliance rate or in the final clinical and radiological outcomes of the two groups after a minimum of 2 years of follow-up. A positive correlation was found between the Pirani score at the beginning of treatment and the final functional score for both groups. Both groups were satisfied with the selected brace. Both groups were equally compliant with the brace protocol.
Conclusion
We conclude that new and more expensive brace designs do not necessarily provide better clinical results. Fully corrected foot and a strong family–treating team partnership are crucial to adherence with the brace protocol.
Keywords: Clubfoot, Ponseti, Brace
Introduction
The Ponseti method for the treatment of clubfoot deformity gained worldwide popularity and became the standard of care in many medical centres, including those in third-world countries, due to its simplicity and high rate of success [1, 2]. Ponseti first introduced his non-surgical method of clubfoot correction more than 50 years ago [3] and he has reported satisfactory results in 89% of treated feet [1]. Reports on failures with the Ponseti method have shown that the decisive factor that led to recurrence of the clubfoot deformity in 50% of the cases was non-compliance with the foot abduction brace protocol [2, 4–7]. Once the last cast has been removed, adherence to the brace protocol is crucial to success and the prevention of recurrence. Newly developed brace designs are focused on improving compliance and success rates [8]. The new brace designs include different types of bars [9], shoes, ankle–foot orthoses (AFO) and hinged attachments [8].
The Ponseti method has been proven to be both effective and relatively inexpensive, and its cost-effectiveness was found to surpass that of surgical treatment [10]. The newly designed and expensive braces may be economically unobtainable to low-income populations. The purpose of the current study was to compare two designs of braces that are used in adherence to the Ponseti treatment protocol of clubfoot. One is the traditional pre-walking shoes attached to a Dennis Browne bar and the other is the new Mitchell brace, also known as the Ponseti brace (MD Orthopaedics, Wayland, Iowa, USA). The Mitchell brace includes detachable shoes and soft silicone AFO-type inserts. Our aim was to find out whether the added components of the newer brace and its claimed increased comfort would improve treatment outcome as measured by two parameters: compliance with the brace protocol and the clinical and radiological results after a minimum of 2 years of follow-up.
Patients and methods
Patients
Two groups of children with idiopathic clubfoot treated by the Ponseti method in our institution from the beginning and followed up for at least 2 years (2002–2006) were included. Children initially treated elsewhere and those with atypical clubfoot were excluded. The study was approved by our institutional review board.
Treatment
All patients were treated in our clubfoot clinic by senior orthopaedic surgeons (YH, ES) and a dedicated physiotherapist (AY), who offered the families unlimited access to information and was available to address whatever problems they encountered. Serial casts were applied weekly according to the Ponseti protocol. Before applying each cast, the physiotherapist manipulated the foot and performed stretching exercises to improve the range of motion. The feet were examined and scored according to the Pirani classification [11]. Since there is good correlation between the two widely used classification systems, i.e. the Diméglio [12] and the Pirani [11, 13] classifications, we only used the latter. Once the forefoot was corrected, an Achilles tenotomy was performed for the management of residual equinus. The procedure took place in a clinical setting using local anaesthetics, followed by a cast that was applied for 3 weeks. After the last cast was removed, a foot abduction brace was applied for 23 h during the first 3 months and the brace time was gradually decreased thereafter. The precise instructions given to the parents were to ensure 20 h of uninterrupted wear after 3 months, 18 h after 6 months and, after the first year of brace application, only night-time use until the age of 3 or 4 years.
Braces
We offered the families two brace options: the traditional foot abduction brace that includes pre-walking shoes attached to a Dennis Browne bar (DB group) or the Mitchell brace, in which the shoe design includes a silicone insert resembling an AFO and a detachable shoe mechanism (Mitchell group). The two braces differ in cost and ease of use, and the families were free to select the brace type they preferred.
Study protocol
We compared the DB group with the Mitchell group. The data that were collected by reviewing the charts of all participants included the child’s age at first visit, the Pirani scoring at that time and the total number of casts used. Each child was graded according to a functional scale for clubfoot as reported by Ezra et al. [14] at the last follow-up visit. That scale incorporates a number of different parameters, such as ankle and subtalar motion, position of the heel and forefoot during standing, gait pattern, shoe type worn, functional limitations, pain and parental satisfaction. Radiographs were taken after the age of 2 years, according to a protocol in which a wooden rectangle is taped to the plantar aspect of the foot for standardisation. An antero-posterior (AP) view and a lateral view in maximum dorsiflexion were obtained and measured [15–17]. In addition to the data collected from the patient’s charts, we asked each family to fill in a questionnaire on the extent of their compliance with the instructions, the level of satisfaction with the brace they chose and if they would recommend it to others. The parents were asked about brace use during each quarter of the first year, the age at which bracing was discontinued and about any problems encountered during the bracing period, such as blistering, sleeping problems and dislodgment of the foot from the brace.
Statistical analysis
The SPSS 18 software and the non-parametric Mann–Whitney test and Spearman correlation were used for all assessments. The results were considered to be significant at the level P < 0.05.
Results
The study included 30 males and eight females. Nineteen children had unilateral clubfoot and 19 had bilateral clubfoot. The mean age at the initiation of treatment was 1.7 weeks (range 1–12 weeks) for the entire cohort. The mean follow-up was 44 months (range 24–88 months). The mean number of casts required for the correction of a foot was 6.5 (range 4–10 casts). The average age at the time of Achilles tenotomy was 7.7 weeks (range 6–16 weeks). The mean Pirani score at the beginning of treatment for the entire group was 4.5 (range 2.5–6). The mean walking age was 15 months (range 10–21 months). The average functional score was 139 points (range 113–150). An Achilles tenotomy was performed in all cases in both groups. The DB group included 21 children and the Mitchell group included 17 children.
The two groups were equal in severity at the beginning of treatment. There were no differences between the two groups in age (P = 0.4) or Pirani score (P = 0.382) at presentation, nor in the number of casts used (P = 0.089) (Fig. 1).
Fig. 1.
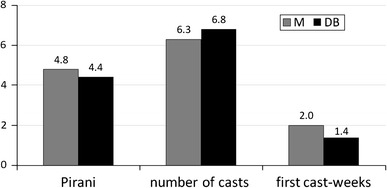
Pirani score for the first cast, number of casts used for correction and the age at the time of the first cast (in weeks). P = 0.38 for the Pirani score; P = 0.09 for the number of casts; P = 0.4 for the age at first cast. M = Mitchell, DB = Dennis Browne
We found no differences in the last follow-up visit between the two groups. The final functional score was 138 for the Mitchell group and 139.8 for the DB group (P = 0.544). The mean AP talocalcaneal angles were 29.8° (±6.6°) for the Mitchell group and 28° (±4.7°) for the DB group (P = 0.146), and the mean lateral talocalcaneal angles in maximal dorsiflexion were 32.4° (±8.2°) for the Mitchell group and 35.55° (±8.1°) for the DB group (P = 0.262) (Fig. 2).
Fig. 2.
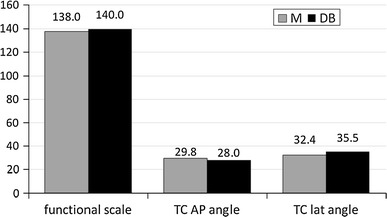
Functional scale and radiographic differences at the last visit. P = 0.544 for the functional scale; P = 0.146 for the talocalcaneal antero-posterior (AP) angle; P = 0.262 for the talocalcaneal lateral angle in maximal dorsiflexion. M = Mitchell, DB = Dennis Browne
There were significant correlations between the Pirani score at the beginning of treatment and the lateral talocalcaneal angle at the end of treatment and between the Pirani score at the beginning of treatment and the final functional score for both groups (P = 0.047 and P = 0.022, respectively). Feet that had an initial high Pirani score ended up with lower lateral talocalcaneal angles and lower functional scores (r = −0.265 and r = −0.324, respectively). There were no significant correlations between the functional score and the AP or the lateral talocalcaneal angles (P = 0.295 and P = 0.439, respectively), nor between the Pirani scores and the AP talocalcaneal angles (P = 0.952). The parents of both brace groups reported having fully complied with the treatment instructions for the first 2 years. Most of the parents reported difficulties with bracing due to sleeping problems, which was the reason for non-compliance beyond the second year. Both groups stated that they would recommend the same brace that they had selected to others.
Discussion
The rationale of developing new brace designs is to improve the effectiveness of the brace treatment and to reduce the incidence of non-compliance. Some of the features incorporated in the new braces are detachable shoes, soft silicone AFO-type inserts, leather or Velcro straps and articulating abduction braces, as in the dynamic brace introduced by Dobbs [8]. On the other hand, these new braces are much more expensive [18]. The approximate cost of commonly used foot abduction orthoses as Dobbs [8] is 1,200 USD, with the Mitchell brace costing around 350 USD, while the DB braces cost around 70 USD in the United States [19], and probably less than that in developing nations when manufactured locally. The foot grows quickly during infancy and usually in the first year, up to two pairs of shoes or orthotic shoes will be needed; this also should be taken into account in the calculation of price.
Several studies have found a higher compliance rate and better results of treatment when the new braces were used as compared to historic control groups that used the traditional DB brace [8, 19]. To our knowledge, there are no studies that compare groups which used different brace designs at the same time.
The results of this case series have shown that adherence and compliance with the bracing protocol was not influenced by the type and design of the brace. Importantly, the results of treatment by following the Ponseti method were the same in both groups. The challenge in achieving successful results with the Ponseti protocol lies in the prevention of relapse and not by the correction of the deformity. There has been increasing emphasis on the importance of brace treatment and its influence on the final results, to the extent that comparing groups treated during different periods of time will give the new group an advantage over a historical group [8]. For that reason, we compared two groups that were matched for the time during which the braces were applied. Both groups underwent the same treatment protocol and the same strict surveillance.
The traditional DB brace and the newly designed Mitchell AFO maintain the foot in 70° of external rotation. The addition of an AFO component may, theoretically, offer better control over the ankle’s range of motion, thus, preventing an equinus foot deformity. It was also thought to prevent dislodgment of the foot from the shoe. Dislodgement of the foot from the brace is probably related to under-correction of the foot and not to the brace design.
A corrected foot that does not reach 15° of dorsiflexion or an “empty heel feeling” at the heel of the foot is an indication to perform an Achilles tenotomy. All of our patients underwent an Achilles tenotomy, since we contend that full correction of the foot and prevention of a rocker-bottom foot is essential. A vicious cycle is created when a foot that is not fully corrected is placed in the brace, followed by dislodgment from the brace; difficulty in strapping the foot while trying to put more pressure on the straps will lead to more crying and discomfort that further reduces the compliance of the family.
Allowing parents to choose the brace type may influence the family to be more compliant with their choice or influence the reported compliance. We were aware that ascertaining compliance by a parental questionnaire may be unreliable. Our physiotherapist, therefore, double-checked our results by comparing them to the reports that the same parents had submitted on a regular basis throughout the first 2 years. A pressure sensor introduced in the brace would probably have provided more accurate data. One of the reasons for non-compliance may be the lack of precise instructions given to the families. For example, Ponseti [20] recommends using the brace at night and during nap time, while others practice gradual decrease from full-time use. In order to prevent any misunderstanding, we instructed the parents of our patients to apply the brace for an exact number of hours according to an established protocol and offered unrestricted access to our team for solving any problems that might have arisen. We also practice a weekly visit with the family and the physiotherapist until we feel that the infant tolerates the brace and not losing correction of the foot.
Allowing the parents to have the choice of brace type and not randomly selecting the groups may have caused a selection bias. Since both braces were privately purchased (and only a small percentage of the price was reimbursed by the family’s medical insurance), the less affluent families tended to choose the less expensive DB brace. When we opened this study, we were inclined to prefer the newer Mitchell brace because it seemed to offer advantages over the traditional DB brace, although there were no comparative data on its effectiveness at that time. The treating team and the parents were not blinded to the treatment and brace type used, and the parents were able to share their experience with others who were using the other type of brace. We believe that these “biases” do not influence the validity of our results but, rather, reinforce them.
Clinically, there were no differences between the two braces. While the Mitchell brace may be more attractive to some parents, the simpler and less expensive brace functions just as well in terms of compliance rates and treatment outcomes. A testimony to the apparent equality of the two brace types is that none of the parents chose to change the brace that they had initially chosen.
The superiority of new and expensive brace designs must first be proven before we abandon the simpler tools available to us. Ease of use and more attractive packaging do not necessarily provide better clinical results.
Contributor Information
Yoram Hemo, Phone: +972-52-4262007, FAX: +972-3-6974542, Email: yoramh@tasmc.health.gov.il.
Eitan Segev, Email: esegev@tasmc.health.gov.il.
Ariella Yavor, Email: clubfoot-dana@tasmc.health.gov.il.
Dror Ovadia, Email: dovadia@tasmc.health.gov.il.
Shlomo Wientroub, Email: shlomowi@tasmc.health.gov.il.
Shlomo Hayek, Email: shayek@tasmc.health.gov.il.
References
- 1.Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am. 1980;62:23–31. [PubMed] [Google Scholar]
- 2.Herzenberg JE, Radler C, Bor N. Ponseti versus traditional methods of casting for idiopathic clubfoot. J Pediatr Orthop. 2002;22:517–521. [PubMed] [Google Scholar]
- 3.Ponseti IV, Smoley EN. Congenital club foot: the results of treatment. J Bone Joint Surg Am. 1963;45:261–275. [Google Scholar]
- 4.Dobbs MB, Rudzki JR, Purcell DB, Walton T, Porter KR, Gurnett CA. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am. 2004;86:22–27. doi: 10.2106/00004623-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Thacker MM, Scher DM, Sala DA, van Bosse HJ, Feldman DS, Lehman WB. Use of the foot abduction orthosis following Ponseti casts: is it essential? J Pediatr Orthop. 2004;25:225–228. doi: 10.1097/01.bpo.0000150814.56790.f9. [DOI] [PubMed] [Google Scholar]
- 6.Haft GF, Walker CG, Crawford HA. Early clubfoot recurrence after use of the Ponseti method in a New Zealand population. J Bone Joint Surg Am. 2007;89:487–493. doi: 10.2106/JBJS.F.00169. [DOI] [PubMed] [Google Scholar]
- 7.Lehman WB, Mohaideen A, Madan S, Scher DM, Van Bosse HJ, Iannacone M, Bazzi JS, Feldman DS. A method for the early evaluation of the Ponseti (Iowa) technique for the treatment of idiopathic clubfoot. J Pediatr Orthop B. 2003;12:133–140. doi: 10.1097/01.bpb.0000049579.53117.4a. [DOI] [PubMed] [Google Scholar]
- 8.Chen RC, Gordon JE, Luhmann SJ, Schoenecker PL, Dobbs MB. A new dynamic foot abduction orthosis for clubfoot treatment. J Pediatr Orthop. 2007;27:522–528. doi: 10.1097/bpo.0b013e318070cc19. [DOI] [PubMed] [Google Scholar]
- 9.Kessler JI. A new flexible brace used in the Ponseti treatment of talipes equinovarus. J Pediatr Orthop B. 2008;17:247–250. doi: 10.1097/BPB.0b013e32830cc3e5. [DOI] [PubMed] [Google Scholar]
- 10.Halanski MA, Huang JC, Walsh SJ, Crawford HA. Resource utilization in clubfoot management. Clin Orthop Relat Res. 2009;467:1171–1179. doi: 10.1007/s11999-008-0674-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pirani S, Outerbridge HK, Moran M, Sawatzky B (1995) A method of evaluating the virgin clubfoot with substantial inter-observer reliability. Presented at the Pediatric Orthopaedic Society of North America (POSNA) Annual Meeting 1995, Miami, Florida, May 1995
- 12.Diméglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F. Classification of clubfoot. J Pediatr Orthop B. 1995;4:129–136. doi: 10.1097/01202412-199504020-00002. [DOI] [PubMed] [Google Scholar]
- 13.Flynn JM, Donohoe M, Mackenzie WG. An independent assessment of two clubfoot-classification systems. J Pediatr Orthop. 1998;18:323–327. [PubMed] [Google Scholar]
- 14.Ezra E, Hayek S, Gilai AN, Khermosh O, Wientroub S. Tibialis anterior tendon transfer for residual dynamic supination deformity in treated club feet. J Pediatr Orthop B. 2000;9:207–211. doi: 10.1097/01202412-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Kite JH. Principles involved in the treatment of congenital club-foot. 1939. J Bone Joint Surg Am. 2003;85-A:1847. doi: 10.2106/00004623-200309000-00032. [DOI] [PubMed] [Google Scholar]
- 16.Turco VJ. Resistant congenital club foot—one-stage posteromedial release with internal fixation. A follow-up report of a fifteen-year experience. J Bone Joint Surg Am. 1979;61:805–814. [PubMed] [Google Scholar]
- 17.Joseph B, Bhatia M, Nair NS. Talo-calcaneal relationship in clubfoot. J Pediatr Orthop. 2001;21:60–64. doi: 10.1097/01241398-200101000-00013. [DOI] [PubMed] [Google Scholar]
- 18.Zionts LE, Dietz FR. Bracing following correction of idiopathic clubfoot using the Ponseti method. J Am Acad Orthop Surg. 2010;18:486–493. doi: 10.5435/00124635-201008000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Garg S, Porter K. Improved bracing compliance in children with clubfeet using a dynamic orthosis. J Child Orthop. 2009;3:271–276. doi: 10.1007/s11832-009-0182-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ponseti IV. Treatment of congenital club foot. J Bone Joint Surg Am. 1992;74:448–454. [PubMed] [Google Scholar]


