Abstract
Rates of suicide are increasing among African American adolescents and pose a significant public health concern. One area that has received little attention is the relationship between various types of social support and suicide, and the extent to which support moderates the relationship between depressive symptoms and suicidality. A total of 212 African American adolescents completed in-school surveys on three types of social support: family support, peer support, and community connectedness. The survey also addressed depressive symptoms and suicidality, as measured by reasons for living, a cognitive measure of suicide risk. Hierarchical multiple regression analyses were used to examine direct and moderating relationships between types of social support and suicidality. The results indicated that increased family support and peer support are associated with decreased suicidality, and peer support and community connectedness moderated the relationship between depressive symptoms and suicidality. Over a third of the variability in reasons for living was predicted by family support, peer support, and community connectedness. Implications for research and preventative interventions for African American adolescents are discussed.
Keywords: African American adolescents, depression, suicide, protective factors, social support, family support, peer support, community connectedness
In 2006, suicide was ranked as the 11th leading cause of death among persons aged 10 years and older, accounting for 33,289 deaths. However, suicide is the third leading cause of death among individuals aged 15 to 24 years. It accounts for 12% of all deaths annually within this age group in the United States (Center for Disease Control [CDC], 2010). Although overall rates of suicide attempts among adolescents declined from 2001 to 2007, rates among African American adolescents, a group that has traditionally had lower suicide rates, did not. Indeed, in 2009, African American adolescents reported higher rates of suicide attempts than Caucasian adolescents (CDC, 2010). Despite recent increases in suicide rates among African American youth, Caucasian Americans continue to be the focus of most research on suicide (Molock, Puri, Matlin, & Barksdale, 2006).
Key risk factors for suicide among youth include presence of a psychiatric disorder, a family history of suicide and psychopathology, stressful life events, and access to firearms (Gould, Greenberg, Velting, & Shaffer, 2003). Risk factors are defined as those characteristics that increase the likelihood that a person develops psychopathology or a problem behavior (Tebes, Kaufman, Adnopoz, & Racusin, 2001). Although some risk factors for suicide seem to differ across racial and ethnic groups, depression is consistently identified as one of the most significant risk factors associated with adolescent suicidal behavior (Colluci & Martin, 2007; Kung, Liu, & Juon, 1998; Lyon et al., 2000; Reifman & Windle, 1995). Findings on the prevalence of racial and ethnic group differences in depression and depressive symptoms have been somewhat inconsistent in the literature. However, recent national estimates from the 2010 Youth Risk Behavior Survey (YRBS) indicate that a high prevalence (27.7%) of African American students report having felt sad or hopeless almost every day for 2 or more weeks in a row (CDC, 2010). This overall rate is higher than compared to Caucasian students (23.7%), with African American females reporting rates over 6% higher than their Caucasian female peers. Although not all young people who exhibit suicidal behaviors are depressed (Lewinsohn, Rohde, & Seeley, 1996; Sanchez, 2001), depressive symptoms increase during adolescence and thus increase the likelihood of suicidal behavior and are an important risk factor to target in suicide prevention (Varley, 2002).
In contrast, social support has been found to serve as a potential protective factor for suicidal behavior (Merchant, Kramer, Joe, Venkataraman, & King, 2009). Protective factors are characteristics in the individual’s world that mitigate against the development of psychopathology or problem behaviors, often by interacting with the risk factor to moderate risk (Tebes, Kaufman, Adnopoz, & Racusion, 2001). Social support can be broadly defined as those interpersonal social resources that involve either the presence or the implication of stable human relationships (Turner & Turner, 1999). Social support has also been defined as a component of connectedness, or the degree to which a person or group is socially close, interrelated, or shares resources with other persons or groups (CDC, 2008). The importance of connectedness and its relation to suicide dates back to Durkheim’s (1897/1951) theory of suicide, which states that suicide is related to an individual’s level of social integration. Previous research has delineated multiple types of social support, including family and peer support (Barrera & Garrison-Jones, 1992). Little research has focused on community connectedness as a type of social support; however, available studies suggests it may play an important role in mental health by providing a sense of belonging or mattering to a group, a sense of personal value or worth, and access to a larger source of support (CDC, 2008).
Some research has also suggested that measuring social support as a global, unitary construct fails to address important differences in the protective qualities of social support and its potential to differentially moderate risk (Felner, 1984), particularly among adolescents with depressive symptoms (Barrera & Garrison-Jones, 1992; Stice, Ragan & Randall, 2004). Furthermore, since adolescence is a developmental period marked by changes in interactions with families and peers, and within neighborhood contexts, examination of these separate influences and interactions is essential (Barrera & Garrison-Jones, 1992; Cauce, Mason, Gonzales, Hiraga, & Liu, 1996).
In order to examine the relationship between depression and suicidality among African American adolescents and to identify factors that buffer this relationship, the present study utilizes an ecological perspective and focuses on key contexts in adolescent’s lives – family, peers, and neighborhood (Jessor, 1993). An ecological perspective recognizes that individuals are embedded within social, political, and economic systems that shape behaviors and access to resources necessary to maintain health (Bronfenbrenner, 1977, 1979). Ecological theories specify the contribution of external factors (e.g., school or neighborhood conditions) to health. This perspective allows for the examination of positive social or community forces that can help an individual thrive despite exposure to certain risk factors, such as depression. The present study examines three types of social support – family, peer, and community connectedness – for their direct influence on suicidality among African American adolescents, and the extent to which each moderates the previously established empirical relationship between depression and suicidality. The term suicidality is used in this study to encompass suicide risk (as measured by the reasons for living scale), suicidal ideation, and suicidal attempts.
Suicidality and Types of Social Support
Family Support
Although adolescence is a time when family relations often change, there is considerable evidence that family support is important to adolescent psychological adjustment. Cauce, Felner, and Primavera (1982) found family support to be the single most important type of social support among lower-income adolescents. Among African Americans, family support is considered a culturally salient variable because connectedness to family is historically important in coping with a society that is antagonistic (Billingsley, 1992). Further, family connectedness is consistent with the communal values promoted in African American culture, in that communalism emphasizes the extended self, the fundamental interdependence of people, and the importance of social bonds (Harris & Molock, 2000).
Indeed, family support has been found to function as a protective factor for suicidality among African American adolescents. Kandel, Ravies, and Davies (1991) showed that closeness to parents has a direct effect in reducing suicidal ideation in high school students, independent of depressive symptoms. Longitudinal studies in both Caucasian (Stice, Ragan, & Randall, 2004) and economically disadvantaged African American adolescents (O’Donnell, O’Donnell, Wardlaw & Stueve, 2004) also found that family closeness and parental support predict depression and suicidality over time. In addition, studies have shown that family support and cohesive families protect African American college students from depression and suicidal ideation (Kimbrough, Molock, & Walton, 1996; Marion & Range, 2003). Finally, the support provided from families has been shown to protect against depressive symptoms, which is a critical risk factor for suicidality (Plant & Sachs-Ericsson, 2004).
Peer Support
Adolescence is a developmental period that is typically marked by an increase in the amount of time individuals spend with peers, rather than with their families (Cole & Cole, 1996). Furthermore, adolescents who perceive their friends as supportive report fewer school-related and psychological problems, greater confidence in their social acceptance by peers, and less loneliness (Cole & Cole, 1996; Lagana, 2004).
Peer support has been shown to be influential in many mental health outcomes, including suicidal behavior. Some investigators have noted that a poor quality of peer interactions is related to depression, which is a strong predictor of suicidality (Kandel, Ravies, & Davies, 1991). Suicidal adolescents also have been found to be more socially isolated than nonsuicidal adolescents (Berman & Schwartz, 1990; Hawton, Fagg, & Simkin, 1996) and to perceive themselves as more rejected by peers (Prinstein, Boergers, Spirito, Little, & Grapentine, 2000). In addition, among females, social support has been shown to significantly predict suicidal ideation 1 year later (Mazza & Reynolds, 1998). And finally, a high level of social support from friends has been found to protect against suicidality among highly depressed high school adolescents (Reifman & Windle, 1995).
Very few studies, however, have examined the relationship of peer support and suicidality among ethnic minority adolescents. Studies that do exist have contradictory findings: Kimbrough, Molock, and Walton (1996) found family and peer support to be protective for suicidal ideation in African American college students, and O’Donnell and colleagues (2004) found that peer support was not protective against suicidality among urban African American and Latino adolescents. Thus, although the relationship of peer support to suicide among African American adolescents is less well understood than that of family support, it remains an important possible protective factor. Further study is warranted due to the potential of peer support to reduce risk associated with poor outcomes in other domains, such as school drop out (Lagana, 2004).
Community Connectedness
The community, often defined as one’s neighborhood, is a key setting in an adolescent’s life (Bronfenbrenner, 1979; Jessor, 1993; Shinn & Toohey, 2003), and provides the basis for a third type of social support, community connectedness. The term community connectedness is intended to encompass a number of terms used to describe strength-based properties of neighborhoods, including social cohesion, collective efficacy, social capital and social support (CDC, 2008). Community connectedness, or stronger connections in a community, may increase an individual’s motivation and ability to adaptively respond to adversity (CDC, 2008). Greater community connectedness may provide adolescents with coping resources outside their home, including having additional adults to talk with, persons to provide aid in times of need, and feelings of protection (Kliewer et al., 2004). These protective factors may guard against depression and other problem behaviors (Aneshensel & Succoff, 1996).
Factors that impede social cohesion, or social connections, include high residential mobility and concentrations of low socioeconomic families in a relatively small space (Sampson, Raudenbaush, & Earls, 1997). Given the extent of residential racial segregation in the United States, community connectedness serves as a potentially critical protective factor for understanding developmental outcomes among children of color (Coll & Szalacha, 2004). Some have argued that reduced collectivism, or neighborhood closeness, in African American communities is contributing to increased risk for suicide among African American males (Willis, Coombs, Cockerham, & Frison, 2002). This is consistent with Durkheim’s theory of suicide (1897 (1951) which posits that individuals who are not sufficiently connected to social groups have limited access to social support or guidance and therefore are at increased risk for suicide.
A few studies have examined the relationship between neighborhood quality and individual mental health and well-being. In a large community-based study of adolescents, increased perceptions of neighborhood cohesion, or closeness, were significantly related to lower depression (Aneshensel & Succoff, 1996). However, in a study of African American female caregivers and their children living in high-violence areas, Kliewer and colleagues (2004) found no protective effect of perceived neighborhood cohesion on internalizing or externalizing adjustment problems. Further, in a community-based sample of inner-city adolescents from Philadelphia, Furstenberg (2001) found little evidence that neighborhoods with greater social cohesion directly affected individual well-being, but did note that neighborhood cohesion positively affected family management practices, which in turn significantly affected adolescent adjustment. This suggests that neighborhood cohesion may function as a moderator of youth depression by influencing family relationships. To address the limited research in this area and consistent with the CDC’s (2008) call for increased research on community connectedness and suicidal behavior, the present study examines the relationship between community connectedness and suicidality among African American adolescents.
The Present Study
The present study examines suicidality and depression in a community sample of African American adolescents in the context of three types of social support -- family support, peer support, and community connectedness. Suicidality is examined using the Reasons for Living-Adolescent (RFL-A) scale (Osman et al., 1998), a positive, indirect approach to assess suicidality among adolescents. Indirect methods to assess suicidality are important because of the stigma often associated with suicide and may be particularly appropriate for use with African American adolescents because they are less likely to disclose suicidal ideation than adults (Molock, Kimbrough, Blanton, McClure, & Williams, 1994; Morrison & Downey, 2000), even in the midst of a suicide crisis (Summerville, Abbate, Siegel, Serravezza, & Kaslow, 1992). Depression is regarded as a risk factor for suicidality and types of social support as potential protective factors. In addition, the interaction of each social support type with depression is examined for its potential as a moderator of risk.
Based on previous research, it was hypothesized that both family and peer support would each have a direct effect on suicidality, so that African American adolescents who reported more family support and peer support would be more likely to report greater reasons for living than adolescents who report less family and peer support. It was also hypothesized that family support, peer support, and community connectedness would moderate the relationship between depressive symptoms and reasons for living.
Method
Participants
Two hundred and twelve African American high school students (79 males and 133 females) participated in this study as part of a larger investigation that examined risk and protective factors for suicidal behaviors in African American adolescents. Participants were recruited from three public high schools in a suburb of Washington, DC (see Table 1 for sample characteristics). Exclusionary criteria included enrollment in special education classes. Students’ participation rate was 55% for the three schools, a response rate similar to other studies requiring active parental consent (Pokorny, Jason, Schoeny, Townsend, & Curie, 2001). Participating students were between the ages of 13 and 19 (M = 15.54, SD = 1.27), and the majority (61.7%) were in the 9th and 10th grade. Most of the students came from middle-class families, as measured by parental education level and family income. The median family income was measured by student’s zip code, collected through census data, and totaled $69,444.60 (SD = $14,570.38).
Table 1.
Descriptive Characteristics of Sample
| Variables | Percent | N |
|---|---|---|
| Gender | ||
| Male | 37.3 | 79 |
| Female | 62.7 | 133 |
| Age | ||
| 13 | .9 | 2 |
| 14 | 24.1 | 51 |
| 15 | 26.4 | 56 |
| 16 | 25.0 | 53 |
| 17 | 17.0 | 36 |
| 18 | 5.2 | 11 |
| 19 | 1.4 | 3 |
| Father’s education | ||
| Some high school | 5.1 | 10 |
| High school | 23.6 | 46 |
| Some college | 25.6 | 50 |
| College | 33.3 | 65 |
| Graduate school | 12.3 | 24 |
| Mother’s education | ||
| Some high school | 2.9 | 6 |
| High school | 26.2 | 54 |
| Some college | 26.7 | 55 |
| College | 26.7 | 55 |
| Graduate school | 17.5 | 36 |
Procedure
Three high schools from a suburb of Washington, DC, were selected to participate in this study. An application for permission to conduct the study was made to the central administrative office of the school district. Once permission was granted, the principals from each school were contacted. Two classes were randomly selected at each grade level and school and asked to participate in the study. Participants were recruited by members of the research team, who visited each class individually to explain the study. Written materials were then provided to parents and students that explained the nature of the study. Parental consent and active assent from students were obtained prior to students participating in the study. Students received extra credit from their classroom teacher as an incentive for returning the consent form, even if parental permission was denied. All communications emphasized the voluntary and confidential nature of the study. The survey protocol was approved by the Internal Review Board at the primary investigator’s university, the school system, and the National Institute of Mental Health (NIMH).
Graduate research assistants and a Ph.D. level clinical psychologist administered the surveys. Students in Grades 9–12 completed written, self-report questionnaires during two 45-minute class periods or one 90-minute period. Due to the sensitive nature of the research, special precautions were taken to ensure that risk was minimized. Students were informed that confidentiality would be required to be broken if a student indicated a clear danger to self or others. All questionnaires were reviewed at the time of survey administration to check for endorsement of key items regarding suicidal ideation, recent suicide attempt, and intent. Those students who endorsed moderate to severe ideation or intent within the previous month were referred to the school guidance counselor, which was the policy of the school district where the data was collected. The licensed psychologist later followed up with the school guidance counselor to check on the student’s status. After all data had been collected, the research team provided each school with a summary of the overall findings, as well as information on possible warning signs of suicide and sources of help in the community.
Instruments
Demographic information
The Demographic Questionnaire is a 21-item questionnaire that includes open-ended questions such as “How old are you?” and forced choice items regarding background information about participants, such as race, and parent’s level of education.
Depression
The Reynolds Adolescent Depression Scale (RADS; Reynolds, 1987) is a measure used to assess severity of depressive symptoms. It consists of 30 items and assesses five dimensions of depression in adolescents: somatic, anhedonia, cognitive, negative view of self, and loneliness. Each item is answered on a 4-point Likert scale ranging from 1 (almost never) to 4 (most of the time). Sample items included: “I feel sad” and “I feel like nothing I do helps anymore.” Higher scores on the measure indicate greater depressive symptomatology. This widely used scale has good psychometric properties and has been used extensively with African American adolescents. Internal consistency of the measure was strong (α = .90).
Family and peer support
The Perception of Support Inventory (PSI; Rosen, 1981) is a self-report questionnaire designed to assess the perception of support that children and adolescents receive from their peers and families. The original scale was modified from a true/false to a 6-point Likert scale ranging from 1 (strongly disagree) to 6 (strongly agree). Sample items include: “My family makes me feel better when I am upset” and “My friends listen to me when I have a problem.” The scale has been used with adolescents and college students, with internal consistency reliability coefficients of .78 for the peer scale, .84 for the family scale, and .83 for the total score (Harris & Molock, 2000). Internal consistency of the measure was strong, with a coefficient of .89 for peer support and .94 for family support.
Community connectedness
The Social Cohesion subscale of the Collective Efficacy Scale (CES; Sampson, Raudenbaush, & Earls, 1997) was used to measure community connectedness. This scale contains five items that asks participants about the likelihood of their neighbors engaging in helpful behaviors or exhibiting trust with one another. Each item is answered on a 5-point Likert scale ranging from 1 (very unlikely) to 5 (very likely). Sample items include: “I live in a close-knit neighborhood” and “People around my neighborhood are willing to help their neighbors.” The reliability of the subscale was good (α = .72).
Reasons for living
The Reasons for Living Inventory - Adolescent (RFL-A; Osman et al., 1998) is a 32-item self-report questionnaire that measures potential reasons for not committing suicide should the thought occur (e.g., “I believe that I could cope with anything life has to offer”). This measure is modeled after the adult RFL scale (Linehan, Goodsteing, Nielsen, & Chiles, 1983), a well-validated and recommended instrument for suicide assessment (Winters, Myers, & Proud, 2002). The RFL-A scale offers a positive approach for assessing suicide risk by measuring adaptive reasons for living if the thought to attempt suicide should occur. This measure allows for suicidal and nonsuicidal individuals to be assessed on a continuum and characterizes adolescents on the content of their belief systems (Connell & Meyer, 1991; Hirsch & Ellis, 1996). The measure has been shown to be useful as an assessment of suicide risk in both clinical and nonclinical settings and for use in research (Malone et al., 2000; Range & Knott, 1997).
Each item of the RFL-A is answered on a six-point Likert scale ranging from 1 (extremely unimportant) to 6 (extremely important). Sample items include: “It would be painful and frightening to take my own life” and “I am afraid to die, so I would not consider killing myself.” Item scores can be totaled for a composite score as well as five factor scores: Future Optimism, Suicide-Related Concerns, Family Alliance, Peer Acceptance and Support, and Self-Acceptance. The RFL-A scale has demonstrated both discriminant (e.g., the ability to differentiate between suicide attempters and non-attempters among clinical and nonclinical samples) and predictive validity (i.e., negatively correlated with future attempts) (Gutierrez, Osman, Kopper, & Barrios, 2000; Osman et al., 1998). The RFL-A has also been found to have high internal consistency (.89 – .93) (Osman et al., 1998). Internal consistency for this sample was .85.
Suicide ideation and suicide attempts
The Suicide Experience Questionnaire (SEQ; Molock, Kimbrough, Lacy, McClure, & Williams, 1994) is a 25-item measure developed to assess the suicide experiences of youth. For this study, two questions were used to assess suicide ideation (“Have you ever thought about committing suicide?”) and suicide attempts (“Did you ever attempt suicide?”). Response choices were no and yes. If participants responded in the affirmative, they were asked to indicate the last time they experienced suicide ideation (“When was the last time you felt that way?”) and suicide attempts (“When last did you attempt?”). Response choices ranged from 1–2 weeks ago to over 1 year ago. For the analyses, the questions for presence of suicide ideation and attempts were collapsed to create a dichotomous variable for ideation and attempts within the previous year.
Data Analyses
Descriptive statistics (e.g., frequency distributions) were conducted to describe demographic characteristics of the sample (e.g., age). Logistic regressions were used to examine the relationship between depressive symptoms, reasons for living, and suicidal ideation and attempts. Pearson correlations were used to examine the relationships among continuous variables. In order to test the major hypotheses of the study, a hierarchical multiple regression was conducted in which gender, age, depressive symptoms, perceived family support, perceived peer support, and perceived community connectedness served as continuous predictor variables, and the participant’s reasons for living score served as the continuous dependent variable. Each of the predictor variables were centered to maximize interpretability and to minimize problems of multicollinearity. The predictor for the interaction of each type of support with depression was formed by multiplying the two predictors. A simultaneous method of variable entry within each step of the regression results in a test of only the unique variance associated with each effect (Cohen & Cohen, 1975). Thus, the multiple regression form of the GLM was implemented with the interaction term being entered in the last step of the regression, as recommended by Baron and Kenney (1986). In Step 1 of the analysis, the main effect for gender and age were entered. The main effects for depression, perceived family support, perceived peer support, and perceived community connectedness were then entered simultaneously in the regression equation in Step 2 of the analysis. Finally, in Step 3, the two-way interactions of depression with each support variable were entered simultaneously into the regression equation.
Results
Descriptive Analyses
Of the students participating in the study, 22% (n = 44) reported suicide ideation in the past year, and 9.2% (n = 18) reported making a suicide attempt in the past year. An examination of the clinical cutoff score for depression (≥77) (Reynolds & Mazza, 1998) showed that 8.97% of the students reported clinical levels of depression (n = 14). Further analyses included all participants’ depression scores as a continuous variable. Depression scores were significantly related to suicidal ideation, χ2 (1, N = 181) = 23.40, p < .001, B = 2.18 (SE = .45), OR = 8.84. Depression scores were significantly related to suicide attempts, χ2 (1, N = 183) = 19.59, p < .001, B = 2.87 (SE = .65), OR = 17.65. Although the relationship between reasons for living and suicide ideation was in the expected direction, it was not significant, χ2 (1, N =188) = 2.02, ns; B = −.433 (SE = .31), OR = .648. However, reasons for living was significantly related to suicide attempts, χ2 (1, N = 186) = 6.35, p < .01, B = −1.01 (SE = .40), OR = .365.
Correlational analyses revealed significant positive relationships between peer support, family support, and community connectedness with reasons for living (see Table 2). There was also a significant negative relationship between peer support, family support, community connectedness, and reasons for living with depression. Community connectedness was not significantly related to perceived peer support.
Table 2.
Correlations and Descriptive Statistics for Independent and Dependent Variables (N = 179)
| Variables | M (SD) | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 1. Family Support | 4.55 (.96) | -- | ||||
| 2. Peer Support | 4.67 (.85) | .580*** | -- | |||
| 3. Community Connectedness | 3.27 (.76) | .246*** | .109 | -- | ||
| 4. Depression | 1.93 (.50) | −.466*** | −.309*** | −.186** | -- | |
| 5. Reasons for Living | 4.65 (.54) | .540*** | .436*** | .240*** | −.406*** | -- |
p <.05.
p < .01.
p < .001.
Regression Analyses
In Step 1, there was no main effect for gender or age, and R was not significantly different from 0, R2 = .01, F(1, 169) = .47, p > .05. In Step 2, there was a significant main effect for depressive symptoms that indicated a significant negative relationship between depression and reasons for living, β = −.20, t (179) = −2.83, p < .01. Results also indicated a significant main effect for family and peer support on reasons for living. Adolescents who reported higher levels of family support also indicated significantly higher reasons for living, β = .31, t (179) = 3.87, p< .001. As well, those who reported higher levels of peer support reported significantly higher reasons for living, β = .17, t (179) = 2.20, p < .05. There was a trend for community connectedness on reasons for living: adolescents with higher levels of community connectedness reported higher reasons for living, β = .12, t (179) = 1.91, p < .1). More than a third of the variability, R2 = .36, F (1, 169) = 16.16, p < .001, of reasons for living was predicted by family support, peer support, and community connectedness after Step 2 (see Table 3 for more results from the hierarchical multiple regression analyses).
Table 3.
Hierarchical Multiple Regression of Depression, Family Support, Peer Support, and Community Connectedness With Reasons for Living (N = 179)
| Variable | Final B | SEb | Final β | R2 Change |
|---|---|---|---|---|
| Step 1 | ||||
| Sexa | .057 | .085 | .050 | |
| Age | −.022 | .032 | −.051 | .005 |
| Step 2 | ||||
| Sexa | .075 | .073 | .067 | |
| Age | .028 | .027 | .066 | |
| Depression | −.223 | .079 | −.204** | |
| Family Support | .184 | .048 | .325*** | |
| Peer Support | .106 | .048 | .166* | |
| Community Connectedness | .088 | .046 | .123+ | .355*** |
| Step 3 | ||||
| Sexa | .067 | .072 | .060 | |
| Age | .026 | .027 | .060 | |
| Depression | −.174 | .078 | −.160* | |
| Family Support | .178 | .047 | .315*** | |
| Peer Support | .116 | .048 | .183* | |
| Community Connectedness | .109 | .046 | .152* | |
| Depression x Family Support | .151 | .083 | .181+ | |
| Depression x Peer Support | −.194 | .083 | −.218* | |
| Depression x Community Connectedness | .195 | .090 | .145* | .042** |
Note. Final R2 = .399 F(8, 170) = 14.09***
Reference group for sex is male.
p <.05.
p < .01.
p < .001.
p < .10.
It was hypothesized that family support, peer support, and community connectedness would function as moderators of the relationship between depression and reasons for living. In Step 3, the results indicated that the interaction term of depression x family support had a trend effect, β =.18, t (179) =1.82, p < .1, but that the interaction of depression x peer support and depression x community connectedness were each significant, β = −.22, t (179) = −.2.33, p < .05, and β = .15, t (179) = 2.17, p < .05, respectively. After Step 3, the addition of the interaction terms with the main effects resulted in a significant increment in R2, R2 = .40, F (1, 169) = 12.63, p < .01. This pattern of results suggests that gender and age do not significantly contribute to the prediction of the variability of the reasons for living. However, over a third of the variability in reasons for living is predicted by family support, peer support, and community connectedness. The inclusion of the interaction terms contributes modestly to this relationship.
Interpretation of Interaction Effects
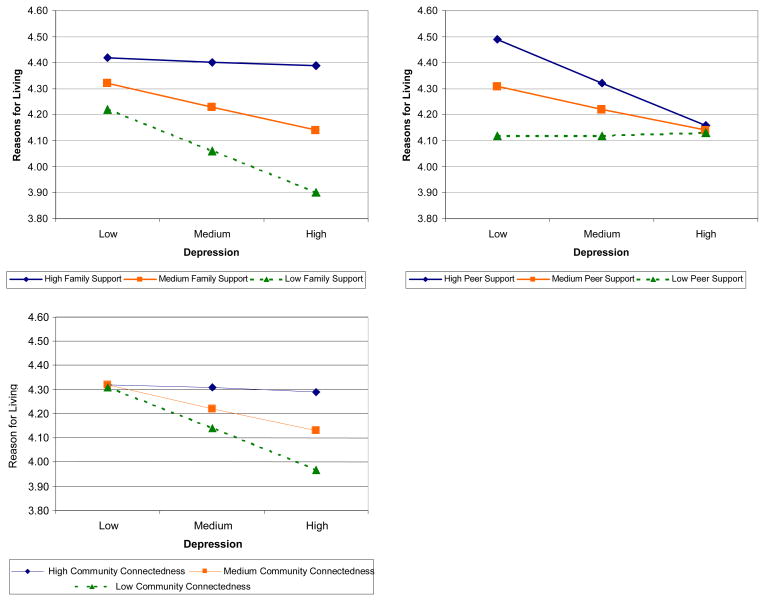
To facilitate interpretation, Figure 1 depicts the underlying pattern of the interaction effects using Aiken and West’s (1991) method for plotting interactions. For each type of support, the low value along the x-axis represents one standard deviation below the mean, the high value represents one standard deviation above the mean, and the medium value represents the overall mean for that variable. Next, the relationship of depression – computed similarly at low, medium, and high values – to reasons for living was plotted for each type of support.
Figure 1.
Interaction effects of family support, peer support, community connectedness with depression and reasons for living (N = 179).
As is shown, the effect of family support was strongest at higher levels of depression. At high levels of depression, adolescents who reported high family support also reported more reasons for living. For peer support, the effect is strongest at low levels of depression. At low levels of depression, adolescents who report high peer support indicate more reasons for living. For community connectedness, there was little effect on adolescents who reported low levels of depression, as they tended to report similar levels of reasons for living regardless of their level of community connectedness. Among adolescents who reported high levels of depression, however, those who reported high community connectedness reported more reasons for living than adolescents who reported low or medium community connectedness.
Discussion
The present study examined the relationship of three types of social support – family support, peer support, and community connectedness–to depression and suicidality among African American adolescents. Overall, the results strongly supported the study hypotheses that family support and peer support would be positively related to suicidality. In addition, community connectedness was also shown to have a direct positive affect on suicidality, albeit at a trend level. Furthermore, as expected, both peer support and community connectedness moderated the relationship of depression and suicidality, but contrary to expectations, family support did not significantly moderate this relationship, although a trend effect was observed.
These findings indicate that family support directly protects adolescents from depressive symptoms and suicidal thoughts, but that peer support and community connectedness may exert both direct and indirect affects on these behaviors among African American adolescents. The family support finding also suggests that, although adolescence may be marked by increasing autonomy from parents, parental support continues to be critical to adolescent development. Further, these results provide additional support for the importance of family as a source of support among African Americans.
The results for peer support indicate that this type of support has both direct and moderating affects on suicidality, particularly at lower levels of depressive symptoms. At higher levels of depression, the level of peer support does not seem to have much of an impact on suicidality. This is consistent with research finding about the importance of peer support to general mental health, but it suggests that among adolescents who are experiencing depression, peer support does not greatly impact suicidality. Indeed, adolescents may not be able to provide sufficient help to troubled peers (Offer, Howard, Schonert, & Ostrov, 1991).
Although community connectedness had a trend affect on suicidality, in contrast to peer support, the protective effect for community connectedness occurred at higher levels of depression. This finding indicates that for African American adolescents experiencing elevated levels of depression, strengthening community connectedness could be an effective target for suicide prevention efforts.
Considered together, these findings provide continuing evidence that both family and peer support are important protective factors (Kandel, Ravies, & Davies, 1991; Greening & Stopplebein, 2002) and that community connectedness is also a protective factor for suicidality among African American adolescents. This is consistent with the CDC’s 2008 “Strategic Direction for the Prevention of Suicidal Behavior.” Future research should examine these constructs with a larger sample of African American youth utilizing longitudinal data.
Descriptive results from this study also indicate that a large proportion of African American adolescents experience depressive symptoms and suicidal ideation and attempts. A total of 9% of the students reported clinical levels of depression, a figure that is comparable to the 8% of adolescents ranging in age from 12 to 17 found to have depression in the general population (Department of Health and Human Services, 2008). Similar rates of suicidal attempts were reported by study participants in the 2009 Youth Risk Behavior Surveillance (YRBS; CDC, 2010). A higher percentage of students in the current study reported suicide ideation than found in the YRBS; however, the rates are more consistent with African American females, who represent the majority of the study participants.
As expected, the results indicated that depressive symptoms are inversely related to suicidal ideation and attempts, as well as the RFL scale. These findings are consistent with the literature suggesting that depressive symptoms are a significant risk factor for suicidal thoughts and behavior (Kung, Liu, & Juon, 1998; Lyon et al., 2000). In addition, this study provides support for the validity of the RFL scale, particularly for use in research with African American adolescents. Results indicated that the reasons for living scores are inversely related to suicide attempts but not suicide ideation. This suggests that the RFL scale is an appropriate measure for suicide risk, particularly suicide attempts. This finding is consistent with recent findings that suggest cognitive factors measured by the RFL scale may serve as a protective factor against later suicide attempts among youth (Goldston, Daniel, Reboussin, Frazier, & Harris, 2001). For this group of adolescents, reasons for living may be a more ecologically valid measure to assess suicide risk.
Limitations
This study has several limitations. First, the results may not be generalizable to all African American high school students. The sample consisted of three high schools in one county in the Mid-Atlantic region, and thus, the results may not be representative of all African American adolescents. In addition, the high schools selected for study participation were in a suburban area and were comprised mostly of African American adolescents. Additionally, the adolescents themselves came primarily from middle-income families. Therefore, the findings may not be generalizable to African American students who attend urban public high schools, come from low-income families, or attend schools with mostly Caucasian students. Further, the sample consisted of a higher proportion of younger adolescents and females, perhaps because these groups tend to return active parental consent forms in greater numbers (Pokorny, Jason, Schoeny, Townsend, & Curie, 2001). Thus, there may be additional constraints on the study’s generalizability.
A second limitation of the study was that the measures used were self-report questionnaires. In previous research, however, such measures have been widely used with success to assess depression, social support, and suicidality among adolescents (McCaskill & Lakey, 2000). Additionally, the RFL scale has been effective in measuring suicidal thoughts and behavior (Osman et al., 1998).
A third limitation of this study was the cross-sectional design used to sample participants. This was partially offset by examining a previously neglected area of research, suicidality and social support, among African American adolescents.
Conclusion
Despite these limitations, this study contributes to the scholarly literature on African American adolescents in five primary ways: (a) it adds to the limited research on suicidality among African American adolescents, and thus provides an important contribution to increasing the quality and quantity of ethnic-specific research; (b) it supports previous research that both family support and peer support are significant protective factors for suicidality; (c) it provides new evidence in support of the importance of community connectedness as a protective factor for suicidality; (d) it specifies how various types of support moderate the established relationship between depression and suicidality; and (e) it provides guidance on the development of targeted suicide prevention and intervention efforts.
Acknowledgments
This study was supported in part by a K-01 Career Development Award from the National Institute of Mental Health for Molock.
We would like to thank the African American Intervention Research in Suicidality (AIRIS) lab for their contribution towards this study. We would also like to acknowledge Christian Connell and members of the Risk & Resilience Lab Group for helpful comments on earlier drafts of the manuscript.
Contributor Information
Samantha L. Matlin, Yale University
Sherry Davis Molock, The George Washington University.
Jacob Kraemer Tebes, Yale University.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. Journal of Health and Social Behavior. 1996;37:293–310. [PubMed] [Google Scholar]
- Baron RM, Kenney DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrera M, Garrison-Jones C. Family and peer social support as specific correlates of adolescent depressive symptoms. Journal of Abnormal Child Psychology. 1992;20:1–16. doi: 10.1007/BF00927113. [DOI] [PubMed] [Google Scholar]
- Berman AL, Schwartz RH. Suicide attempts among adolescent drug users. American Journal of Diseases of Children. 1990;144:310–314. doi: 10.1001/archpedi.1990.02150270060026. [DOI] [PubMed] [Google Scholar]
- Billingsley A. Climbing Jacob’s ladder: The enduring legacy of African American families. New York, NY: Simon & Schuster; 1992. [Google Scholar]
- Bronfenbrenner U. Toward and experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Cauce M, Felner RD, Primavera J. Social support in high-risk adolescents: Structural components and adaptive impact. American Journal of Community Psychology. 1982;10:417–428. doi: 10.1007/BF00893980. [DOI] [PubMed] [Google Scholar]
- Cauce AM, Mason C, Gonzales N, Hiraga Y, Liu G. Social support during adolescence: Methodological and theoretical considerations. In: Hurrelmann K, Hamilton SF, editors. Social problems and social contexts in adolescence: Perspectives across boundaries. New York, NY: Aldine de Gruyter; 1996. pp. 131–151. [Google Scholar]
- Centers for Disease Control and Prevention. Strategic direction for the prevention of suicidal behavior: Promoting individual, family, and community connectedness to prevention suicidal behavior. Atlanta, GA: Author; 2008. [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance. Surveillance summaries. MMWR. 2010;59:SS–5. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum; 1975. [Google Scholar]
- Cole M, Cole SR. The development of children. 3. New York, NY: W.H. Freeman and Company; 1996. [Google Scholar]
- Coll CG, Szalacha LA. The multiple contexts of middle childhood. The Future of Children. 2004;14:81–97. [Google Scholar]
- Colluci E, Martin G. Ethnocultural aspects of suicide in young people: A systematic literature review. Part 2: Risk factors, precipitating agents, and attitudes toward suicide. Suicide and Life-Threatening Behavior. 2007;37:222–237. doi: 10.1521/suli.2007.37.2.222. [DOI] [PubMed] [Google Scholar]
- Connell DK, Meyer RG. Adolescent suicidal behavior and popular self-report instruments of depression, social desirability, and anxiety. Adolescence. 1991;26:113–119. [PubMed] [Google Scholar]
- Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Results from the 2007 National Survey on Drug Use and Health: National findings (DHHS Publication No. SMA 08-4343) Rockville, MD: Author; 2008. [Google Scholar]
- Durkheim E. Suicide: A study in sociology. Glencoe Press; New York: 1951. Original work published 1897. [Google Scholar]
- Felner RD. Vulnerability in childhood: A preventative framework for understanding children’s efforts to cope with life stress and transitions. In: Roberts MC, Peterson LH, editors. Prevention of problems in childhood: Psychological research and applications. New York, NY: Wiley-Interscience; 1984. pp. 133–169. [Google Scholar]
- Furstenberg FF. Managing to make it: Afterthoughts. Journal of Family Issues. 2001;22:150–162. [Google Scholar]
- Goldston DB, Daniel SS, Reboussin BA, Frazier PH, Harris AE. Cognitive risk factors and suicide attempts among formerly hospitalized adolescents: A prospective naturalistic study. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:386–405. doi: 10.1097/00004583-200101000-00021. [DOI] [PubMed] [Google Scholar]
- Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- Greening L, Stoppelbein L. Religiosity, attributional style, and social support as psychosocial buffers for African American and White adolescents' perceived risk for suicide. Suicide and Life-Threatening Behavior. 2002;32:404–417. doi: 10.1521/suli.32.4.404.22333. [DOI] [PubMed] [Google Scholar]
- Gutierrez PM, Osman A, Kopper BA, Barrios FX. Why young people do not kill themselves: The reasons for living inventory for adolescents. Journal of Clinical Child Psychology. 2000;29:177–187. doi: 10.1207/S15374424jccp2902_4. [DOI] [PubMed] [Google Scholar]
- Harris TL, Molock SD. Cultural orientation, family cohesion, and family support in suicide ideation and depression among African American college students. Suicide and Life Threatening Behavior. 2000;30:341–353. [PubMed] [Google Scholar]
- Hawton K, Fagg J, Simkin S. Deliberate self-poisoning and self-injury in children and adolescents under 16 years of age in Oxford, 1976–1993. British Journal of Psychiatry. 1996;169:202–208. doi: 10.1192/bjp.169.2.202. [DOI] [PubMed] [Google Scholar]
- Hirsch JK, Ellis JB. Differences in life stress and reasons for living among college suicide ideators and non-ideators. College Student Journal. 1996;30:377–384. [Google Scholar]
- Jessor R. Successful adolescent development among youth in high-risk settings. American Psychologist. 1993;48:117–126. doi: 10.1037//0003-066x.48.2.117. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Ravies VH, Davies M. Suicidal ideation in adolescence: Depression, substance use, and other risk factors. Journal of Youth and Adolescence. 1991;20:289–309. doi: 10.1007/BF01537613. [DOI] [PubMed] [Google Scholar]
- Kimbrough RM, Molock SD, Walton K. Perception of social support acculturation, depression, and suicidal ideation among African American college students at predominantly black and predominantly white universities. Journal of Negro Education. 1996;65:295–307. [Google Scholar]
- Kliewer W, Nelson J, Cunningham RD, Parrish KA, Walker JM, Atiyeh C, Mejia R. Violence exposure and adjustment in inner-city youth: Child and caregiver emotion regulation skill, caregiver-child relationship quality, and neighborhood cohesion as protective factors. Journal of Clinical Child &Adolescent Psychology. 2004;33:477–487. doi: 10.1207/s15374424jccp3303_5. [DOI] [PubMed] [Google Scholar]
- Kung HC, Liu X, Juon HS. Risk factors for suicide in Caucasians and in African Americans: A matched case-control study. Social Psychiatry and Psychiatric Epidemiology. 1998;33:115–161. doi: 10.1007/s001270050038. [DOI] [PubMed] [Google Scholar]
- Lagana MT. Protective factors for inner-city adolescents at risk of school dropout: Family factors and social support. Children and Schools. 2004;26:211–220. [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Adolescent suicidal ideation and attempts: Prevalence, risk factors, & clinical implications. Clinical Psychology: Science and Practice. 1996;3:25–46. [Google Scholar]
- Linehan MM, Goodstein JL, Nielsen SL, Chiles JA. Reasons for staying alive when you're thinking of killing yourself: The reasons for living inventory. Journal of Consulting and Clinical Psychology. 1983;51:276–286. doi: 10.1037//0022-006x.51.2.276. [DOI] [PubMed] [Google Scholar]
- Lyon ME, Benoit M, O’Donnell RM, Getson PR, Silber T, Walsh T. Assessing African American adolescents’ risk for suicide attempts: Attachment theory. Adolescence. 2000;35(137):122–134. [PubMed] [Google Scholar]
- Malone KM, Oquendo MA, Haas GL, Ellis SP, Li S, Mann JJ. Protective factors against suicidal acts in major depression: Reasons for Living. American Journal of Psychiatry. 2000;157:1084–1088. doi: 10.1176/appi.ajp.157.7.1084. [DOI] [PubMed] [Google Scholar]
- Marion MS, Range LM. African American college women’s suicide buffers. Suicide and Life-Threatening Behavior. 2003;33:33–43. doi: 10.1521/suli.33.1.33.22780. [DOI] [PubMed] [Google Scholar]
- Mazza JJ, Reynolds WM. A longitudinal investigation of depression, hopelessness, social support, and major and minor life events and their relation to suicidal ideation in adolescents. Suicide and Life Threatening Behavior. 1998;28:358–374. [PubMed] [Google Scholar]
- McCaskill JW, Lakey B. Perceived support, social undermining, and emotion: Idiosyncratic and shared perspectives of adolescents and their families. Personality and Social Psychology Bulletin. 2000;26:820–832. [Google Scholar]
- Merchant C, Kramer A, Joe S, Venkataraman S, King C. Predictors of multiple suicide attempts among suicidal Black adolescents. Suicide and Life-Threatening Behavior. 2009;39:115–124. doi: 10.1521/suli.2009.39.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molock SD, Kimbrough R, Lacy MB, McClure KP, Williams S. Suicidal behavior among African American college students: A preliminary study. Journal of Black Psychology. 1994;20:234–251. [Google Scholar]
- Molock SD, Puri R, Matlin S, Barksdale C. Relationship between religious coping and suicidal behaviors among African American adolescents. Journal of Black Psychology. 2006;32:366–389. doi: 10.1177/0095798406290466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison LL, Downey DL. Racial differences in self disclosure of suicidal ideation and reasons for living: Implications for training. Cultural Diversity & Ethnic Minority Psychology. 2000;6:374–386. doi: 10.1037/1099-9809.6.4.374. [DOI] [PubMed] [Google Scholar]
- O’Donnell L, O’Donnell C, Wardlaw DM, Stueve A. Risk and resiliency factors influencing suicidality among urban African American and Latino youth. American Journal of Community Psychology. 2004;33:37–49. doi: 10.1023/b:ajcp.0000014317.20704.0b. [DOI] [PubMed] [Google Scholar]
- Offer D, Howard KI, Schonert KA, Ostrov EJD. To whom adolescents turn for help? Differences between disturbed and nondisturbed adolescents. Journal of the American Academy for Child and Adolescent Psychiatry. 1991;30:623–630. doi: 10.1097/00004583-199107000-00015. [DOI] [PubMed] [Google Scholar]
- Osman A, Downs WR, Kopper BA, Barrios FX, Baker MT, Osman JR, Linehan MM. The Reasons for Living Inventory for Adolescents (RFL–A): Development and psychometric properties. Journal of Clinical Psychology. 1998;54:1063–1078. doi: 10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Plant EA, Sachs–Ericsson N. Racial and ethnic differences in depression: The roles of social support and meeting basic needs. Journal of Consulting and Clinical Psychology. 2004;72:41–52. doi: 10.1037/0022-006X.72.1.41. [DOI] [PubMed] [Google Scholar]
- Pokorny SB, Jason LA, Schoeny ME, Townsend SM, Curie CJ. Do participation rates change when active consent procedures replace passive consent? Evaluation Review. 2001;25:567–580. doi: 10.1177/0193841X0102500504. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, Spirito A, Little T, Grapentine WL. Peer functioning, family dysfunction, and psychological symptoms in a risk factor model for adolescent inpatients’ suicidal ideation survey. Journal of Clinical Child Psychology. 2000;29:392–406. doi: 10.1207/S15374424JCCP2903_10. [DOI] [PubMed] [Google Scholar]
- Range LM, Knott EC. Twenty suicide assessment instruments: Evaluation and recommendations. Death Studies. 1997;21:25–58. doi: 10.1080/074811897202128. [DOI] [PubMed] [Google Scholar]
- Reifman A, Windle M. Adolescent suicidal behavior as a function of depression, hopelessness, alcohol use, and social support: A longitudinal investigation. American Journal of Community Psychology. 1995;13:329–341. doi: 10.1007/BF02506948. [DOI] [PubMed] [Google Scholar]
- Reynolds WW. Reynolds Adolescent Depression Scale: Professional manual. Odessa, FL: Psychological Assessment Resources; 1987. [Google Scholar]
- Reynolds WM, Mazza JJ. Reliability and validity of the Reynolds Adolescent Depression Scale with young adolescents. Journal of School Psychology. 1998;36:295–312. [Google Scholar]
- Rosen R. Unpublished manuscript. Children’s National Medical Center; Washington, DC: 1981. Perception of Support Inventory. [Google Scholar]
- Sampson RJ, Raudenbaush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sanchez HG. Risk factor model for suicide assessment and intervention. Professional Psychology: Research and Practice. 2001;32:351–358. [Google Scholar]
- Shinn M, Toohey SM. Community context of human welfare. Annual Review of Psychology. 2003;54:427–459. doi: 10.1146/annurev.psych.54.101601.145052. [DOI] [PubMed] [Google Scholar]
- Stice E, Ragan J, Randall P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support. Journal of Abnormal Psychology. 2004;113:155–159. doi: 10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- Summerville MB, Abbate MF, Siegel A, Serravezza J, Kaslow NJ. Psychopathology in urban female minority adolescents with suicide attempts. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:663–668. doi: 10.1097/00004583-199207000-00013. [DOI] [PubMed] [Google Scholar]
- Tebes JK, Kaufman JS, Adnopoz J, Racusion GR. Resilience and family psychosocial processes among children of parents with serious mental disorders. Journal of Child and Family Studies. 2001;10:115–136. [Google Scholar]
- Turner RJ, Turner JB. Social integration and support. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. New York, NY: Kluwer Academic/Plenum; 1999. pp. 131–151. [Google Scholar]
- Varley CK. Don't overlook depression in youth. Contemporary Pediatrics. 2002;19:70–76. [Google Scholar]
- Willis LA, Coombs DW, Cockerham WC, Frison SL. Ready to die: A postmodern interpretation of the increase of African–American adolescent male suicide. Social Sciences & Medicine. 2002;55:907–920. doi: 10.1016/s0277-9536(01)00235-0. [DOI] [PubMed] [Google Scholar]
- Winters NC, Myers K, Proud L. Ten-year review of rating scales. III: Scales assessing suicidality, cognitive style, and self-esteem. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1150–1181. doi: 10.1097/00004583-200210000-00006. [DOI] [PubMed] [Google Scholar]