Abstract
Purpose
It is desirable to identify a potential organ donor (POD) as early as possible to achieve a donor conversion rate (DCR) as high as possible which is defined as the actual number of organ donors divided by the number of patients who are regarded as a potential organ donor. The DCR is calculated with different assessment tools to identify a POD. Obviously, with different assessment tools, one may calculate different DCRs, which make comparison difficult. Our aim was to determine which assessment tool can be used for a realistic estimation of a POD pool and how they compare to each other with regard to DCR.
Methods
Retrospective chart review of patients diagnosed with a subarachnoid haemorrhage, traumatic brain injury or intracerebral haemorrhage. We applied three different assessment tools on this cohort of patients.
Results
We identified a cohort of 564 patients diagnosed with a subarachnoid haemorrhage, traumatic brain injury or intracerebral haemorrhage of whom 179/564 (31.7%) died. After applying the three different assessment tools the number of patients, before exclusion of medical reasons or age, was 76 for the IBD-FOUR definition, 104 patients for the IBD-GCS definition and 107 patients based on the OPTN definition of imminent neurological death. We noted the highest DCR (36.5%) in the IBD-FOUR definition.
Conclusion
The definition of imminent brain death based on the FOUR-score is the most practical tool to identify patients with a realistic chance to become brain dead and therefore to identify the patients most likely to become POD.
Keywords: Brain death, Critical care organisation, Ethics, Neurotrauma, Stroke, Transplantation
Introduction
In most Western countries, absolute numbers of brain dead patients are declining [1–3]. Approximately 80–90% of these patients suffer from aneurysmal subarachnoid haemorrhage (SAH), traumatic brain injury (TBI) or intracerebral haemorrhage (ICH) [2, 4–7]. Progress in the prevention and treatment of these three conditions has led to a steady decline in the pool of potential heart-beating organ donors over the past few decades [8–14].
Organ donation rates in countries are often expressed as the donor rate per million population. This comparison tool is not an appropriate measure because several factors may influence the total number of potential organ donors (PODs). For instance, the number of intensive care beds, neurosurgical facilities, road traffic accidents and cerebral haemorrhages differ per country and are not considered in this comparison tool [1]. Another comparison tool that is often used and is not affected by the above-mentioned factors is the donor conversion rate (DCR). The DCR is defined as the actual number of organ donors divided by the number of patients who are regarded as PODs. Organ procurement organisations in the USA aim to achieve a DCR of at least 75% [15], but the actual DCRs in the USA, UK and Germany are estimated to be in the range of 42–68% [1, 16–18]. However, using a DCR has practical limitations. The DCR is calculated with different assessment tools to identify a POD. Using different assessment tools results in different DCRs, which make comparison difficult.
One of the difficulties associated with the quantification of the number of PODs is the different definitions of a POD [19, 20]. To compare groups of PODs between different hospitals or countries, a uniform definition of a POD is needed. This may be hampered by international differences concerning inclusion or exclusion of PODs based on age or medical contraindications to organ donation. With a uniform definition, the causes of non-procurement can be assessed, and ways of improving DCRs can be developed. Recently, we formed an international expert consensus panel and proposed a definition of a POD by defining imminent brain death [21].
In the present study we investigate the pool of potential heart-beating organ donors in a cohort of patients, who died from SAH, TBI or ICH in the intensive care unit (ICU), using three different assessment tools for PODs. Our aims were to determine if these tools could be used for an accurate estimation of a potential donor pool and to ascertain how they compare to each other with regard to the DCRs, by using a cohort of PODs.
Materials and methods
We conducted a retrospective chart review of patients who were admitted to a 32-bed medical/surgical ICU in a university hospital between 1 January 2006 and 31 December 2008, and died from SAH, TBI or ICH. Lists of these patients were obtained from three independent sources: the patient-data management system of the ICU (Critical Care Manager 8.1; Picis, Inc. Wakefield, MA, USA), the central hospital patient registry and the medical chart review database of the Dutch Transplant Foundation. These three lists were then crosschecked. Patient age, sex, dates of admission and death, definitive diagnosis based on computed tomography, cerebral angiography, clinical examination and outcome on ICU discharge were extracted from the medical records. From the patients who died in the ICU from SAH, TBI or ICH, we extracted the last known absent brain stem reflexes and the reason for non-procurement, if applicable. After identifying this cohort of patients, we applied the following three different assessment tools, which included two definitions of imminent brain death (IBD) that we recently proposed in this journal [21] and a definition used in the USA:
Imminent brain death [21], Glasgow Coma Score (GCS) based (IBD-GCS): defined by a GCS score of 3 and at least 3 out of 6 absent brain stem reflexes [21].
Imminent brain death [21], based on a Full Outline of UnResponsiveness (FOUR) score [22–24] of E0M0B0R0 (IBD-FOUR), which represents eyelids remaining closed with pain (E0), no response to pain or generalised myoclonus status (M0), absent pupillary, corneal and cough reflex (B0) and absence of spontaneous ventilation or apnoea (R0) [21].
Imminent neurological death (IND) as defined by the Organ Procurement Transplantation Network (OPTN) in the USA and published on their website (see http://optn.transplant.hrsa.gov). The OPTN defined imminent neurological death as “a patient … with severe neurological injury and requiring ventilator support, who upon clinical evaluation … has an absence of at least three brain stem reflexes”. Age, which is part of this definition, is excluded from our statistical analysis to prevent its influence on the comparison.
All patients in our cohort underwent regular neurological evaluations by a neurologist during their stay in the ICU because of their deteriorating neurological condition. This resulted in an accurate record of neurological examinations in the medical charts that could be used for retrospective analysis of the defined neurological assessment tools.
Statistics
Normally distributed continuous variables are described as means with standard deviations (SD), and skewed continuous variables are described as medians with interquartile ranges (IQR). Binary variables are described as proportions. Differences between the three subgroups were tested with analysis of variance (ANOVA) with the Tukey post hoc test for normal continuous distributed variables; the Kruskal–Wallis test was used for skewed continuous variables. All binary variables were analysed using the chi-square test.
Results
Demographics
Between 1 January 2006 and 31 December 2008, 3,429 patients were admitted to the ICU, where the overall mortality was 647/3,429 (18.9%). We identified a cohort of 564/3,429 (16.4%) patients who were diagnosed with SAH, TBI or ICH, of whom 179/564 (31.7%) died. These 179 patients comprised 27.6% of the overall ICU mortality. The medical charts of two patients, who died as a result of SAH, could not be retrieved and were therefore excluded from the analysis.
Table 1 shows the demographics of the non-survivors divided into three subgroups. Between the period from 2006 to 2008, 25 patients became heart-beating organ donors, 23 of whom died from SAH, ICH or TBI; one patient became brain dead as a result of post-anoxic encephalopathy after cardiac arrest and one patient with TBI, who was transferred directly from the emergency department to the operating theatre for multi-organ donation, was excluded from the analysis. A total of 36 patients, who were admitted to the ICU with SAH, ICH or TBI, donated one or more organs; 13 of these patients were non-heart-beating (NHB) organ donors.
Table 1.
Demographics of patients died from SAH, TBI or ICH (n = 179)
| SAH | ICH | TBI | P value | |
|---|---|---|---|---|
| No. of patients (%) | 73 (40.8) | 45 (25.1) | 61 (34.1) | |
| Age, year (±SD) | 56.7 (10.3) | 58.7 (14.1) | 49.8 (±20.5) | <0.05 |
| Female sex, no. (%) | 48 (65.7) | 19 (42.2) | 15 (24.6) | <0.001 |
| Length of stay, no. days (IQR) | 2 (1–9) | 2 (1–6) | 1 (1–6) | 0.318 |
| Mortality at day 2, no. (%) | 35 (47.9) | 21 (46.7) | 32 (52.5) | 0.810 |
| Year of admission, no. (%) | ||||
| 2006 | 32 (43.8) | 12 (26.6) | 16 (26.3) | |
| 2007 | 22 (30.1) | 15 (33.3) | 29 (47.5) | |
| 2008 | 19 (26.0) | 18 (40.0) | 16 (26.2) | |
Potential organ donors
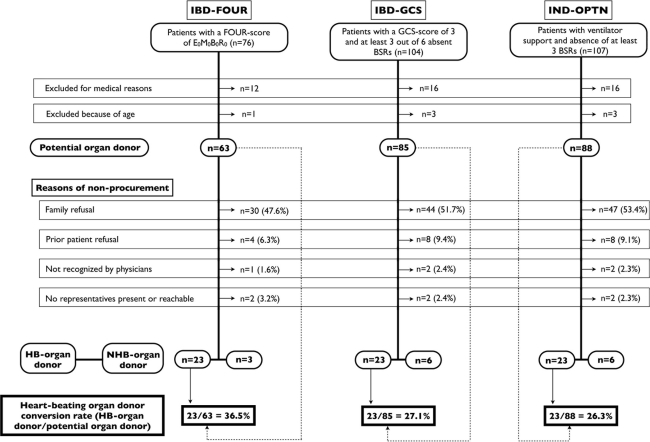
After we applied the three different assessment tools, the numbers of patients who fulfilled the criteria for IBD or IND, before exclusion due to medical reasons or age, and were regarded as PODs were as follows: 76 according to the IBD-FOUR definition, 104 according to the IBD-GCS definition and 107 based on the OPTN definition of IND (Fig. 1). Examining the detection rates of the different assessment tools before exclusion for medical reasons or age revealed incremental increases in the percentages of detection of PODs as a result of the broadening of the selection criteria (see Table 2). The highest detection of PODs was noted in the SAH admission group.
Fig. 1.
Flowchart of the assessment tools. IBD-FOUR imminent brain death based on FOUR criteria, IBD-GCS imminent brain death based on GCS criteria, IND-OPTN imminent neurological death used by the OPTN, BSRs brain stem reflexes, HB-organ donor heart-beating organ donor, NHB-donor non-heart-beating organ donor
Table 2.
Detection rates of the different assessment tools per admission diagnosis before exclusion of medical reasons or age greater than 76 years
| SAH | ICH | TBI | Total | |
|---|---|---|---|---|
| IBD-FOUR (%) | 58.9 | 31.1 | 31.1 | 42.5 |
| IBD-GCS (%) | 72.6 | 53.3 | 44.2 | 58.1 |
| IND-OPTN (%) | 75.3 | 55.5 | 44.2 | 59.8 |
Total population n = 179
IBD-FOUR
Of the 179 patients who died from SAH, TBI or ICH, 76 (42.5%) were eligible for organ donation after applying the IBD definition based on the FOUR score. After exclusion due to age (1 patient) and medical reasons, such as malignancy, sepsis or viral infections (12 patients), 63 patients (35.1%) were identified as PODs. Of this cohort, 26 patients donated one or more organs: 23 were heart-beating organ donors and 3 were non-heart-beating organ donors. The majority of the patients (56.6%) who were identified as PODs by this definition were admitted to the ICU after an SAH, followed by 25.0% after TBI and 18.4% after ICH.
IBD-GCS
Of the 179 patients who died from SAH, TBI or ICH, 104 (58.1%) were eligible for organ donation, after applying the IBD-GCS definition. After exclusion due to age (3 patients) and medical reasons, such as malignancy, sepsis or viral infections (16 patients), 85 patients (47.5%) were identified as PODs. Of this cohort, 29 patients donated one or more organs; 23 were heart-beating organ donors and 6 were non-heart-beating organ donors. The majority of the patients (51.0%) who were identified as PODs by this definition were admitted to the ICU after an SAH, followed by 26.0% after TBI and 23.1% after ICH.
IND-OPTN
Of the 179 patients who died from SAH, TBI or ICH, 107 (59.8%) were eligible for organ donation, after applying the IND-OPTN definition. After exclusion due to age (3 patients) and medical reasons, such as malignancy, sepsis or viral infections (16 patients), 88 patients were identified as PODs. Of this cohort, 29 patients donated one or more organs; 23 were heart-beating organ donors and 6 were non-heart-beating organ donors. The majority of the patients (51.4%) who were identified as PODs by this definition were admitted to the ICU after an SAH, followed by 25.2% after TBI and 23.4% after ICH.
Reasons for non-procurement
After we applied the assessment tools to define a POD, family refusal accounted for more than 50% of the non-procurements in two of the three definitions. Comparison between the three assessment tools showed a family refusal rate of approximately 75% in the ICH group and approximately 40–50% in the SAH and TBI groups. Other reasons for non-procurement included malignancy, sepsis, age, prior patient refusal, no representative who could give consent to organ donation and, in two cases, failure of the treating physicians to recognise a POD.
Discussion
In this retrospective study, we used three different assessment tools for PODs to calculate the DCR and to analyse the reasons for non-procurement. Resulting from restrictions that are incorporated into the IBD-FOUR definitions, three NHB donors were not identified as potential heart-beating organ donors. These patients sustained serious neurological damage but retained one or more brainstem reflexes (one patient was ventilated on pressure support settings and two patients had positive cornea reflexes) and were excluded by the application of the IBD-FOUR definition. The IBD-FOUR definition showed the highest DCR of 36.5%, which is still low when compared to other published DCRs [1, 16, 17]. As stated before, comparison is difficult with different definitions of a POD. An additional seven potential NHB donors were not identified in our cohort by using the three assessment tools, reflecting the high sensitivity of these tools for potential heart-beating organ donors.
Regardless of the definitions of a POD, we identified a considerably substantial group of patients with a high risk of becoming brain dead. However, most of the patients, who we considered to be PODs, did not proceed to fulfil official brain death criteria. Before the formal brain death determination, relatives were often informed about the poor prognosis and the possibility of organ or tissue donation. If relatives of a patient declined organ donation, mechanical ventilation was withdrawn and the patient subsequently died after cardiopulmonary arrest. Some patients, when treatment was withdrawn, had some remaining positive brain stem reflexes and, hypothetically, were not identified by using one of the assessment tools. It is possible that some of these patients would have deteriorated into a state of imminent brain death after continuation of treatment, probably resulting in an underestimation of the full potential of PODs.
A POD, as defined in this study, is considered a risk estimate of a possible outcome for a patient. This risk estimate has to be realistic to provide health-care professionals with accurate data. For instance, if every patient admitted to an ICU was considered a POD, a DCR will never achieve a goal of 75% or higher. The OPTN definition is illustrative of this because it is the only definition that does not include any formal and validated neurological assessment tool for the level of consciousness. This results in the largest group of patients who could be regarded as PODs before exclusion due to medical reasons and age; this did not increase the identification of PODs who actually proceeded to organ donation. The result of this definition is a low DCR. The use of a less specific definition of a POD, such as the OPTN, results in a low DCR and a high estimate of the reasons for non-procurement if we examine heart-beating organ donation. The high estimate of reasons for non-procurement is the result of the inclusion of a large group of patients who are ineligible for heart-beating organ donation. Regardless of the definitions used, the patients who died from SAH were most likely to become heart-beating organ donors. After reviewing our data, we conclude that using the definition of imminent brain death, based on the FOUR score [23], offers the most accurate estimation of a pool of PODs, due to a more detailed neurological assessment of critically ill neurological patients in the ICU. One should keep in mind that although a high DCR correlates with a higher specificity of the assessment tools used in our study, it does not necessarily translate into an increased rate of organ procurement. Therefore, a prospective validation of the different assessment tools is necessary.
Our study has some limitations. First, it is a single-centre study, and data were obtained by retrospective medical chart review. As is the case for all observational studies, some cases may have been missed in a non-random manner. Second, the neurologists who assessed the patients did not record the data regarding the GCS score and the last known absent brain stem reflexes at a predefined moment, resulting in data recorded at different stages during treatment. This is a troublesome limitation of the retrospective nature of this study. Third, to illustrate the use of the different assessment tools, we selected patients based on their diagnosis and outcome. We used this cohort to apply three different definitions to analyse our ICU population to determine the donor potential and the reasons for non-procurement in a transparent way.
Conclusion
Brain dead patients are a scarce but important source of organs. This report shows that the assessment tools used are easy to apply and easy to report in a comprehensive way. The definition of imminent brain death based on the FOUR score appears to be the more neurologically practical tool for identifying patients with a realistic chance of becoming brain dead. A prospective study is necessary to validate these assessment tools.
Acknowledgments
We would like to thank Julius de Vries of the Department of Information Technology, Erasmus MC Rotterdam, in the Netherlands for extracting the necessary data for this study. We are also grateful to Nichon Jansen and Andries Hoitsma for their critical comments on the manuscript. We thank Nichon Jansen and Rik van Leiden (Dutch Transplant Foundation) for providing data from their database.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Barber K, Falvey S, Hamilton C, Collett D, Rudge C. Potential for organ donation in the United Kingdom: audit of intensive care records. BMJ. 2006;332:1124–1127. doi: 10.1136/bmj.38804.658183.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kompanje EJ, Bakker J, Slieker FJ, IJzermans JN, Maas AI. Organ donations and unused potential donations in traumatic brain injury, subarachnoid haemorrhage and intracerebral haemorrhage. Intensive Care Med. 2006;32:217–222. doi: 10.1007/s00134-005-0001-9. [DOI] [PubMed] [Google Scholar]
- 3.Tuttle-Newhall JE, Krishnan SM, Levy MF, McBride V, Orlowski JP, Sung RS. Organ donation and utilization in the United States: 1998–2007. Am J Transplant. 2009;9:879–893. doi: 10.1111/j.1600-6143.2009.02565.x. [DOI] [PubMed] [Google Scholar]
- 4.Gortmaker SL, Beasley CL, Brigham LE, Franz HG, Garrison RN, Lucas BA, Patterson RH, Sobol AM, Grenvik NA, Evanisko MJ. Organ donor potential and performance: size and nature of the organ donor shortfall. Crit Care Med. 1996;24:432–439. doi: 10.1097/00003246-199603000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Opdam HI, Silvester W. Identifying the potential organ donor: an audit of hospital deaths. Intensive Care Med. 2004;30:1390–1397. doi: 10.1007/s00134-004-2185-9. [DOI] [PubMed] [Google Scholar]
- 6.Wijdicks EF, Pfeifer EA. Neuropathology of brain death in the modern transplant era. Neurology. 2008;70:1234–1237. doi: 10.1212/01.wnl.0000289762.50376.b6. [DOI] [PubMed] [Google Scholar]
- 7.Kompanje EJO. Organ donation from brain-dead donors: a dead-end street. In: den Exter A, editor. Human rights and biomedicine. Antwerp: Maklu; 2010. pp. 235–251. [Google Scholar]
- 8.Connolly ES, Jr, Poisik A, Winfree CJ, Kim LJ, Huang J, McMahon DJ, Solomon RA. Cigarette smoking and the development and rupture of cerebral aneurysms in a mixed race population: implications for population screening and smoking cessation. J Stroke Cerebrovasc Dis. 1999;8:248–253. doi: 10.1016/S1052-3057(99)80074-3. [DOI] [PubMed] [Google Scholar]
- 9.Goldacre MJ, Duncan M, Griffith M, Rothwell PM. Mortality rates for stroke in England from 1979 to 2004: trends, diagnostic precision, and artifacts. Stroke. 2008;39:2197–2203. doi: 10.1161/STROKEAHA.107.509695. [DOI] [PubMed] [Google Scholar]
- 10.Jimenez-Yepes CM, Londono-Fernandez JL. Risk of aneurysmal subarachnoid hemorrhage: the role of confirmed hypertension. Stroke. 2008;39:1344–1346. doi: 10.1161/STROKEAHA.107.504019. [DOI] [PubMed] [Google Scholar]
- 11.Raja PV, Huang J, Germanwala AV, Gailloud P, Murphy KP, Tamargo RJ. Microsurgical clipping and endovascular coiling of intracranial aneurysms: a critical review of the literature. Neurosurgery. 2008;62:1187–1202. doi: 10.1227/01.neu.0000333291.67362.0b. [DOI] [PubMed] [Google Scholar]
- 12.Sargent RP, Shepard RM, Glantz SA. Reduced incidence of admissions for myocardial infarction associated with public smoking ban: before and after study. BMJ. 2004;328:977–980. doi: 10.1136/bmj.38055.715683.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wijdicks EF, Kallmes DF, Manno EM, Fulgham JR, Piepgras DG. Subarachnoid hemorrhage: neurointensive care and aneurysm repair. Mayo Clin Proc. 2005;80:550–559. doi: 10.4065/80.4.550. [DOI] [PubMed] [Google Scholar]
- 14.Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009;8:635–642. doi: 10.1016/S1474-4422(09)70126-7. [DOI] [PubMed] [Google Scholar]
- 15.Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant. 2006;6:190–198. doi: 10.1111/j.1600-6143.2005.01130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lytle FT, Afessa B, Keegan MT. Progression of organ failure in patients approaching brain stem death. Am J Transplant. 2009;9:1446–1450. doi: 10.1111/j.1600-6143.2009.02575.x. [DOI] [PubMed] [Google Scholar]
- 17.Sheehy E, Conrad SL, Brigham LE, Luskin R, Weber P, Eakin M, Schkade L, Hunsicker L. Estimating the number of potential organ donors in the United States. N Engl J Med. 2003;349:667–674. doi: 10.1056/NEJMsa021271. [DOI] [PubMed] [Google Scholar]
- 18.Wesslau C, Grosse K, Kruger R, Kucuk O, Mauer D, Nitschke FP, Norba D, Manecke A, Polster F, Gabel D. How large is the organ donor potential in Germany? Results of an analysis of data collected on deceased with primary and secondary brain damage in intensive care unit from 2002 to 2005. Transpl Int. 2007;20:147–155. doi: 10.1111/j.1432-2277.2006.00413.x. [DOI] [PubMed] [Google Scholar]
- 19.Cuende N, Cuende JI, Fajardo J, Huet J, Alonso M. Effect of population aging on the international organ donation rates and the effectiveness of the donation process. Am J Transplant. 2007;7:1526–1535. doi: 10.1111/j.1600-6143.2007.01792.x. [DOI] [PubMed] [Google Scholar]
- 20.Jansen NE, Haase-Kromwijk BJ, van Leiden HA, Weimar W, Hoitsma AJ. A plea for uniform European definitions for organ donor potential and family refusal rates. Transpl Int. 2009;22:1064–1072. doi: 10.1111/j.1432-2277.2009.00930.x. [DOI] [PubMed] [Google Scholar]
- 21.de Groot YJ, Jansen NE, Bakker J, Kuiper MA, Aerdst S, Maas AIR, Wijdicks EF, van Leiden HA, Hoitsma AJ, Kremer HPH, Kompanje EJO. Imminent brain death: point of departure for potential heart-beating organ donation. Intensive Care Med. 2010;36:1488–1494. doi: 10.1007/s00134-010-1848-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wijdicks EF. Clinical scales for comatose patients: the Glasgow Coma Scale in historical context and the new FOUR score. Rev Neurol Dis. 2006;3:109–117. [PubMed] [Google Scholar]
- 23.Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: the FOUR score. Ann Neurol. 2005;58:585–593. doi: 10.1002/ana.20611. [DOI] [PubMed] [Google Scholar]
- 24.Wolf CA, Wijdicks EF, Bamlet WR, McClelland RL. Further validation of the FOUR score coma scale by intensive care nurses. Mayo Clin Proc. 2007;82:435–438. doi: 10.4065/82.4.435. [DOI] [PubMed] [Google Scholar]