Introduction
Pain is a multidimensional experience influenced by complex interactions between biological, psychological, social, and cultural factors (1). Low back pain (LBP) is an important public health problem due to its high impact on disability (2, 3) and work-related disability (4). The development of chronic LBP, has been related with a Fear Avoidance Model of Musculoskeletal Pain (FAM). The FAM refers to generation of fear due to catastrophic thoughts followed by the avoidance of movement due to the fear of pain and re-injury. The FAM has highlighted the importance of pain catastrophizing and pain-related fear in the development of chronic low back pain from an acute episode (5).
In addition to this psychological model, the prevalence of chronic pain has been reported to vary with socio-economic levels (6). In general, differences in socioeconomic status are associated with differences in lifestyle and health conditions, where low socioeconomic status is related with an adverse health outcome (7, 8). Therefore, researchers studying biopsychosocial models should consider the mechanisms by which SES influences psychosocial pathways and health outcomes (9). Theoretically, individuals are exposed to more demands as SES decreases, and psychosocial responses to such stress may be adaptable at short time but can be harmful on health over time (9). Over time, a combination of stress and stress reactivity decrease individual’s reserve capacity to respond to the challenges of the environment, and may make them more vulnerable to different disease and chronic conditions (10).
Given these assumptions, it is notable that most investigations of biopsychosocial models have focused on psychological variables with less of an emphasis on the influence of SES interferences on LBP outcomes. This current paper attempted to address that shortcoming by investigating the influence of SES between psychological factors relevant to fear-avoidance models. Specifically, the purposes of this study were two fold. First we examined whether SES should be considered as mediator between the relationship of fear-avoidance beliefs and pain catastrophizing on disability, pain intensity and physical impairment. Second, we investigated whether the effect of fear-avoidance beliefs and pain catastrophizing on disability, pain intensity and physical impairment are moderated by SES on patients with acute and sub-acute LBP. We recruited patients with acute and sub-acute LBP for this study, because these subjects allowed an opportunity to investigate influence of SES and psychology before the onset of chronic LBP.
Methods
Subjects
This planned secondary analysis includes data from a randomized clinical trial (11) with patients with acute or sub-acute LBP, which were recruited from University of Florida affiliated orthopedic physical therapy clinics. The study was approved by the Institutional Review Board at the University of Florida and all patients provided informed consent. The inclusion and exclusion criteria for the randomized clinical trial were based on guidelines from the Quebec Task Force on Spinal Disorders (QTFSD) (12). Inclusion criteria were: (1) patient with acute or sub-acute LBP (duration of symptoms from 1 to 24 weeks) without radiation below the gluteal fold; (2) patient with acute or sub-acute LBP with proximal radiation to the knee; (3) patient with acute or sub-acute LBP with distal radiation below the knee; (4) between 15 and 60 years old and English speaking. Patients were excluded for meeting any one of the following exclusion criteria. (1) chronic LBP (duration of symptoms greater than 24 weeks) without radiation below the gluteal fold; (2) chronic LBP with proximal radiation to the knee; (3) chronic LBP with distal radiation below the knee; (4) acute or sub-acute or chronic low back pain with distal radiation below the knee and neurological signs; (5) presumptive lumbar nerve root compression; (6) confirmed lumbar nerve root compression; (7) confirmed lumbar spinal stenosis; (8) post-surgical status (less than 6 months after surgical intervention); (9) post-surgical status (more than 6 months after surgical intervention, asymptomatic); (10) other spinal disorders including metastatic disease, visceral disease, or fracture; (11) pregnancy or (12) osteoporosis.
Measures
All patient received a baseline examination to collect demographic data (age, sex, race, employment status), socioeconomic data (level of education, and income), and clinical data (pain intensity, physical impairment, disability, fear-avoidance belief, and pain catastrophizing). Pain intensity, disability, and fear-avoidance belief were also collected at 4-weeks and 6-months.
Socioeconomic Status
Many validated indicators of socioeconomic status (SES) exist (13–15); however, for the current study we created an idiosyncratic measure of SES by combining the available income and education measures. Our rationale for using income and education to represent SES in this study was that these factors are considered a valid proxy for SES (16). The income variable categorized subjects into five different levels of yearly household income: (1) less than $20,000, (2) $ 20,000 to $ 35.000, (3) $ 35,001 to $ 50,000, (4) $ 50,001 to 70,000, and (5) greater than $ 70,000. The education variable categorized subjects into six different levels of education: (1) Less than high school, (2) Graduated from high school, (3) Some college, (4) Graduated from college, (5) Some post-graduate course work, and (6) Completed post graduate degree. The SES variable was then created by adding the income score (from 1–5) and education scores (from 1–6) creating a variable that had a total score ranging from 2–11. This SES variable was treated as a continuous variable in the subsequent analyses because descriptive analyses indicated it met normality assumptions.
Pain Intensity
Patients rated their pain intensity using a numeric rating scale (NRS) from “0” corresponding with “no pain” to “100” corresponding with “worst pain intensity imaginable” (17).
Physical Impairment
Physical impairment was assessed using the physical impairment scale (PIS) described by Waddell et al. (18). The PIS consists of seven different physical examination procedures (total lumbar flexion, total lumbar extension, average side-bending, average straight leg raise, active sit-up, bilateral straight leg raise, and spinal tenderness) performed by the patient. Each procedure is scored as positive (1) or negative (0), resulting in a total score ranging from 0 to 7. In previous study has been demonstrated an excellent interrater reliability in these measures (intraclass correlation coefficient [ICC] = 0.94) (18).
Disability
Pain disability was assessed with the modified Oswestry Disability Index (ODI). The original version described by Fairbank et al (19) was modified from employment/homemaking ability for the section related to sex life (20, 21). The ODI has been found to have high levels of test-retest reliability (ICC=0.90), construct validity (>0.80), and responsiveness (effect size=1.8) in patients receiving physical therapy interventions for LBP (20, 21) and is recommended as a primary outcome measure of self-report of disability for patients with LBP.
Fear-Avoidance Beliefs
The Fear-Avoidance Beliefs Questionnaire (FABQ) was used to quantify fear-avoidance beliefs. This questionnaire focuses on patient’s beliefs about how work and physical activity affect patient’s LBP. The FABQ is an 11-item, 7-point rating scale (0, “strongly disagree” to 6, “agree”) with physical activity (FABQPA) and work (FABQW) scales. Higher FABQ scores indicated higher levels of fear-avoidance beliefs and the FABQPA ranges from 0 – 24 while the FABQW ranges from 0 – 42. The test-retest stability of the FABQ has been reported in the literature for patients with chronic low back pain with a Kappa for individual items of 0.74 (22).
Pain Catastrophizing
Pain catastrophizing was measured by the Pain Catastrophizing Scale (PCS) (23). The PCS has 13 items assessing catastrophic cognitions and subjects used a 5-point scale (0, “not at all” to 4, “all the time”) to rate the frequency of these cognitions. A PCS sum score was calculated for all items (range, 0 – 52), with a high score indicating a high level of pain catastrophizing.
Data analysis
Data analysis was performed using SPSS, Version 15.0 at alpha level of 0.05. Descriptive statistics (mean, standard deviation) were calculated for all variables. Variables were tested for normality using Kolmogorov-Smirnof test before analysis. The primary purpose of this study was to investigate the association of SES, variables associated with fear-avoidance model of musculoskeletal pain (fear-avoidance beliefs and pain catastrophizing) on disability, pain intensity, and physical impairment in patients with LBP. Mediation was investigated by the method described by Baron and Kenny. First, potential mediation models were tested with correlations to determine whether preconditions for mediation were obtained, that is, mediating factor (SES) correlated with the independent variables (fear-avoidance beliefs, and pain catastrophizing), outcome variable (disability, pain intensity, and physical impairment) correlated with independent variable (fear-avoidance beliefs, and pain catastrophizing), and the mediation factor (SES) correlated with outcome variable. Second, hierarchical multiple regression was used to ascertain whether controlling for the mediator (SES) significantly attenuated the relationship between independent variables (fear avoidance belief, pain catastrophizing) and outcome variable (disability, pain intensity, and physical impairment). In addition, the association between the mediator and the outcomes was tested with the independent variables controlled.
Moderation models were evaluated with hierarchical multiple regression. These analyses tested whether psychological factors x SES interaction terms accounted for significant variance in disability, pain intensity and physical impairment score after the psychosocial factors and SES main effect terms had been entered in the model. For any significant interaction, the SES was dichotomized at the median value into low socioeconomic status, and high socioeconomic status. To establish the nature of the interaction effect, correlations between psychological factors and outcome measurements score were performed for each low and high socioeconomic group.
Baseline variables were used for the mediation and moderation analysis. In the event a significant regression model was detected involving SES, the model was further investigated using longitudinal data. Specifically, the baseline model was used to predict 4-week and 6-month outcomes in an attempt to further validate the model.
Results
Descriptive statistics for study participants (N =108) are reported in Table 1. All variables were found to approximate a normal distribution by Kolmogorov-Smirnof test (P > 0.05) and were appropriate for our planned correlation and regression analyses.
Table 1.
Descriptive data from Clinical Trial
| Variable | N=108 | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| AGE | 106 | 15.00 | 60.00 | 37.16 | 14.46 |
| Sex: Male | 37 (34.3%) | ||||
| Female | 69 (63.9%) | ||||
| FABQPA | 108 | .00 | 24.00 | 14.77 | 5.68 |
| FABQW | 108 | .00 | 51.00 | 13.30 | 11.51 |
| PCS | 108 | .00 | 49.00 | 16.12 | 11.31 |
| SES | 102 | 2.00 | 11.00 | 6.58 | 2.50 |
| ODI | 108 | .00 | 78.00 | 29.21 | 16.34 |
| PAIN | 108 | .00 | 9.00 | 4.67 | 2.10 |
| Physical impairment | 104 | .00 | 7.00 | 3.17 | 1.87 |
FABQPA – Fear-Avoidance Beliefs Questionnaires related Physical Activity, FABQW – Fear- Avoidance Beliefs Questionnaires related Work, PCS – Pain Catastrophizing Scale, SES – Socioeconomic Status, ODI – Oswestry Disability Index.
Mediation Effects
The preconditions for testing mediation models in which SES would influence disability, pain intensity, or physical impairment outcomes via fear avoidance beliefs and pain catastophizing is reported in Table 2. Consistent with past research, fear avoidance belief physical activity (FABQPA), and fear avoidance belief related work (FABQW) were significantly correlated with disability outcome (ODI), pain intensity (NRS), and physical impairment. Pain catastrophizing was significantly correlated with disability and pain intensity, but not with physical impairment. SES was only significantly correlated with pain catastrophizing (r=−0.37, p<0.01). We have checked potential mediation from pain catastrophizing to outcomes measures (pain intensity, and disability) and SES did not predict pain intensity (Beta = −0.02, p = 0.91) or disability (Beta = 0.09, p = 0.36) while controlling for PCS. Therefore, the relationship required for testing mediation model was not met (24). Additional tests for mediation were not performed.
Table 2.
Pearson Correlations among variables
| Pain | ODI | FABQPA | FABQW | PCS | SES | |
|---|---|---|---|---|---|---|
| Physical impairment | .48(**) | .39(**) | .23(*) | .34(**) | .17 | −.08 |
| Pain | 1 | .44(**) | .42(**) | .34(**) | .39(**) | −.13 |
| ODI | - | 1 | .48(**) | .47(**) | .48(**) | −.08 |
| FABQPA | - | - | 1 | .41(**) | .40(**) | −.18 |
| FABQW | - | - | - | 1 | .32(**) | −.19 |
| PCS | - | - | - | - | 1 | −.37(**) |
| SES | - | - | - | - | - | 1 |
ODI – Oswestry Disability Index, FABQPA – Fear-Avoidance Beliefs Questionnaires related Physical Activity, FABQW – Fear- Avoidance Beliefs Questionnaires related Work, PCS – Pain Catastrophizing Scale, SES – Socioeconomic Status.
p< 0.01.
p<0.05.
Moderation Effects
Hierarchical multiple regressions were used to determine whether SES moderated relationships between the psychological factors and disability, pain intensity and physical impairment outcome. To reduce multicollinearity we performed a centering process for each predictor variable by subtracting its own mean before entering into the regression model. If the independent variables (IV’s) with interactions are not centered, their product would be highly correlated with the component IV’s. Interaction terms were then computed by multiplying centered psychological variables (FABQPA, FABQW, PCS) with centered SES.
Predicting Disability
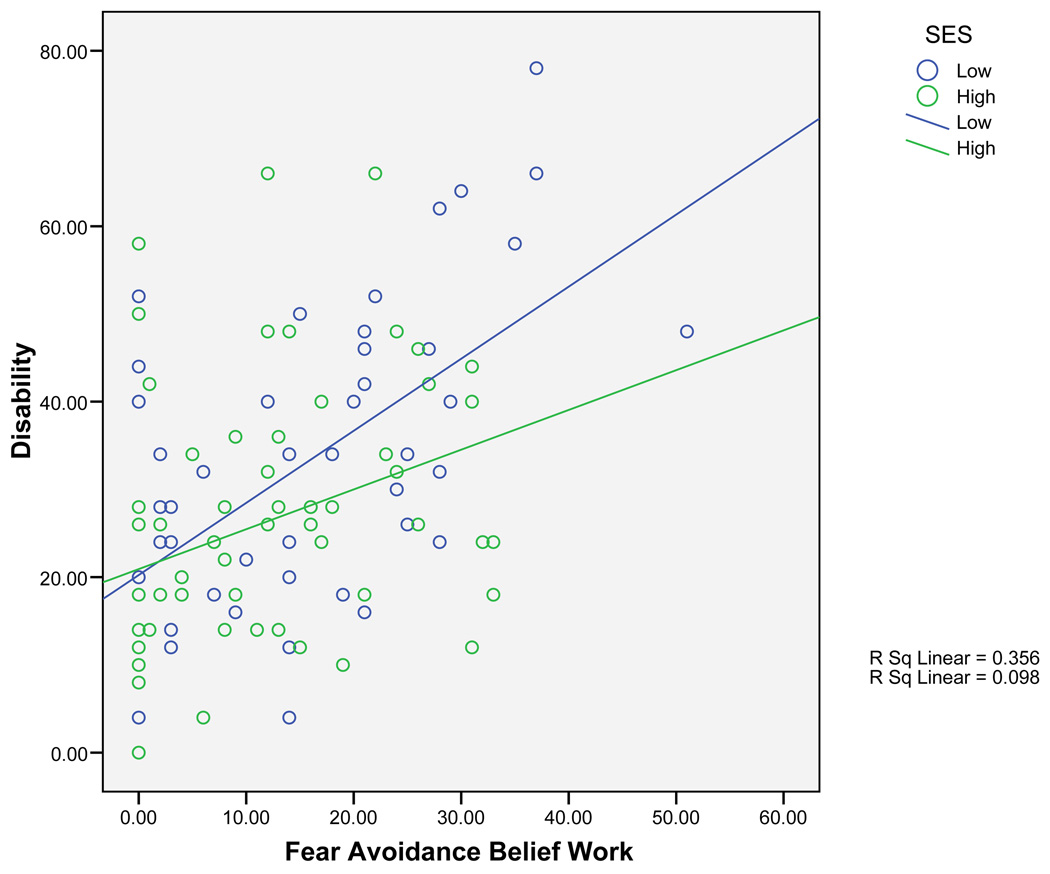
All regression models for disability are reported in Table 3. The first disability model included the FABQPA and explained a significant amount of variance in disability (R2= 0.17), [F(1,99)=6.52, p<0.001]. Standardized beta was significant for FABQPA main effect, but not for the SES main effect or interaction term (Table 3). The second disability model included the FABQW and explained a significant amount of variance in disability (R2= 0.26), [F(1,99)=11.79, p<0.001]. A significant main effect was found for FABQW, but not for SES (Table 3). The interaction term accounted for additional variance in disability outcome, suggesting that the link between FABQW and disability depended on different socioeconomic levels (Table 3). In order to analyze the significant interaction term SES was divided into low and high socioeconomic groups. As shown in Figure 1, a lower association for FABQW related disability was noted in the high socioeconomic group. In contrast, people in the low socioeconomic group experience a higher association of FABQW related disability. The third disability model included the PCS and explained a significant amount of variance in disability (R2= 0.21), [F(1,99)=8.88, p<0.001]. A significant main effect was found for PCS, but not for SES or the interaction term (Table 3)
Table 3.
Summary of Hierarchical Regression Analysis for variables predicting Disability and their interaction term with Socioeconomic Status (SES)
| Variables | R2 | P-Value | B (Std.Error) | Beta | P-value | |
|---|---|---|---|---|---|---|
| 1.Model predicting Disability | 0.17 | <0.001 | ||||
| Step 1 | FABQPA | 1.14 (0.31) | 0.37 | <0.001 | ||
| SES | −0.08 (0.59) | −0.01 | 0.897 | |||
| Step 2 | FABQPA × SES | −0.09 (0.12) | −0.07 | 0.46 | ||
| 2.Model predicting Disability | 0.26 | <0.001 | ||||
| Step 1 | FABQW | 0.58 (0.13) | 0.41 | <0.001 | ||
| SES | 0.08 (0.56) | 0.01 | 0.891 | |||
| Step 2 | FABQW × SES | −0.15 (0.05) | −0.24 | 0.008 | ||
| 3.Model predicting Disability | 0.21 | <0.001 | ||||
| Step 1 | PCS | 0.61 (0.14) | 0.43 | <0.001 | ||
| SES | 0.75 (0.62) | 0.12 | 0.229 | |||
| Step 2 | PCS × SES | −0.08 (0.05) | −0.14 | 0.135 | ||
Figure 1.
Correlation Between FABQW scores and Disability scores among patients with low SES and High SES.
Predicting Pain intensity
All regression models for pain intensity are reported in Table 4. The first model included the FABQPA and explained a significant amount of variance predicting pain intensity (R2= 0.10), [F(1,99)= 3.73, p<0.05]. There was a significant main effect for FABQPA, but not for SES or the interaction term (Table 4). The second model included the FABQW and explained a significant amount of variance predicting pain intensity (R2= 0.10), [F(1,99)= 3.56, p<0.05], only the FABQW main effect was significant. No significant interaction with SES was found in this model (Table 4). The third model included the PCS and explained a significant amount of variance predicting pain intensity (R2= 0.11), [F(1,99)= 4.13, p<0.05]. Standardized beta was significant for PCS main effect, but not for the SES main effect or interaction term (Table 4).
Table 4.
Summary of Hierarchical Regression Analysis for variables predicting Pain Intensity and their interaction term with Socioeconomic Status (SES)
| Variables | R2 | P-Value | B (Std.Error) | Beta | P-value | |
|---|---|---|---|---|---|---|
| 1.Model predicting Pain | 0.10 | <0.05 | ||||
| Step 1 | FABQPA | 0.10 (0.04) | 0.27 | 0.011 | ||
| SES | −0.06 (0.08) | −0.08 | 0.407 | |||
| Step 2 | FABQPA × SES | −0.01 (0.02) | −0.05 | 0.606 | ||
| 2.Model predicting Pain | 0.10 | <0.05 | ||||
| Step 1 | FABQW | 005 (0.02) | 0.26 | 0.012 | ||
| SES | −0.06 (0.08) | −0.08 | 0.429 | |||
| Step 2 | FABQW × SES | −0.01 (0.01) | −0.09 | 0.354 | ||
| 3.Model predicting Pain | 0.11 | <0.05 | ||||
| Step 1 | PCS | 0.06 (0.02) | 0.31 | 0.004 | ||
| SES | −0.01 (0.08) | −0.00 | 0.989 | |||
| Step 2 | PCS × SES | −0.003 (0.007) | −0.05 | 0.614 | ||
Predicting Physical Impairment
All regression models for physical impairment are reported in Table 5. The first model included the FABQPA and was non-significant (R2=0.04), [F(1,97)= 1.19, p=0.32]. The model with the FABQW explained a significant amount of variance predicting physical impairment (R2=0.13), [F(1,97)= 4.67, p<0.05]. The standardized beta indicated that the FABQW was the only unique main effect (Table 5). The third model included the PCS and was non-significant (R2=0.04), [F(1,97)= 1.28, p=0.29].
Table 5.
Summary of Hierarchical Regression Analysis for variables predicting Physical Impairment and their interaction term with Socioeconomic Status (SES)
| Variables | R2 | P-Value | B (Std.Error) | Beta | P-value | |
|---|---|---|---|---|---|---|
| 1.Model predicting Ph. Imp | 0.04 | >0.05 | ||||
| Step 1 | FABQPA | 0.06 (0.04) | 0.17 | 0.125 | ||
| SES | −0.03 (0.08) | −0.04 | 0.692 | |||
| Step 2 | FABQPA × SES | −0.002 (0.15) | −0.02 | 0.87 | ||
| 2.Model predicting Ph. Imp | 0.13 | <0.05 | ||||
| Step 1 | FABQW | 0.06 (0.16) | 0.36 | <0.001 | ||
| SES | −0.01 (0.07) | −0.01 | 0.893 | |||
| Step 2 | FABQW × SES | 0.01 (0.01) | 0.07 | 0.502 | ||
| 3.Model predicting Ph. Imp | 0.04 | >0.05 | ||||
| Step 1 | PCS | 0.02 (0.02) | 0.10 | 0.350 | ||
| SES | −0.01 (0.08) | −0.01 | 0.940 | |||
| Step 2 | PCS × SES | −0.01 (0.01) | −0.14 | 0.181 | ||
Longitudinal Analysis
Only the moderation model for the FABQ and SES predicting disability was considered in the longitudinal analysis. Interestingly, longitudinal analysis show that the regression model explaining disability at 4 weeks and at 6 months after controlling for initial disability was also significant (R2= 0.22), [F(4,87) = 5.86, p<0.001] and (R2= 0.33), [F(4,69) = 7.83, p<0.001] respectively. The interaction term accounted for additional variance in disability at 4 weeks (Beta= −0.25, p= 0.01), and 6 months (Beta= −0.27, p= 0.01) suggesting that socioeconomic levels affect FABQW and disability over time.
Discussion
The present study examined the influence of SES and psychological factors consistent with fear-avoidance models on 3 different outcome measures for patients with acute and sub-acute LBP. The analyses considered both mediation and moderator effects of SES. Our results indicate that SES has a minimal influence on pain and physical impairment, but there is potential for an influence on disability. Specifically, SES altered the association between FABQW and disability such that those with lower SES had a higher association between FABQW and disability. This association was observed at baseline, 4-weeks, and at 6-months. This study makes a novel contribution to the literature because we have incorporated SES when assessing psychological factors for influence on disability. Furthermore, we have investigated these factors in a cohort of subjects with acute and sub-acute LBP, so these data supplement studies that have studied SES in patients with chronic LBP.
Previous research has reported that fear avoidance beliefs, pain catastrophizing, coping strategies and anxiety level are important factors in low back pain outcome (4, 22, 25–29). Nevertheless, the interference of SES in psychological models has been under-reported in the literature. Our analyses indicated that psychological factors were consistently correlated with outcome measures. In contrast, SES was not correlated with the outcome measures, suggesting SES had a minimal direct influence on disability, pain, and physical impairment in this sample.
Only a significant interaction between SES and the FABQW was detected. This interaction was such that people in low SES group experienced a higher association of fear avoidance belief work related disability. Longitudinal analysis show that this interaction detected at baseline was also related to disability at 4 weeks and 6 months. Previous studies show that SES could have a marked impact on chronic LBP (30), and also described that individuals with chronic LBP and lower SES are more likely to have increased pain, mental distress, and disability (30–32). The specific interaction of SES with the FABQW is important because previous studies have indicated the FABQW is predictive of disability and work loss (28, 33). These findings add to the limited literature of SES in patients with acute and sub-acute LBP by suggesting the development of chronic disability is accentuated through fearful work beliefs for patients with lower SES.
This study has important limitations to be considered for future study in this area. First, patients seeking health care from three different orthopedic physical therapy centers associated with an academic medical center were recruited into this study, and do not necessarily represent the general population with LBP. Future studies may consider probability sampling techniques to investigate SES influence for those with LBP that do not seek health care. Second, our SES measure was compromised of only education and income and although there is evidence to suggest this is a proxy measure of SES (16), our measure should not be considered a comprehensive assessment of SES. Furthermore, we used an idiosyncratic SES measure that had not been validated in other studies. Future studies in this area should consider more sophisticated assessment of SES using validated measures. For example, perceived adequacy of income, and social network or living arrangement were included in a recent report from Jordan et al. (34) and assessment of these factors could lead to different results. Third, this is a secondary analysis without a priori power analysis; however the sample size was sufficient to investigate our models. Fourth, as we only have one significant interaction, there is a probability that this finding could be attributed to chance.
Conclusions
Our findings indicate limited potential for SES (measured as by education and income) to directly influence disability, pain, and physical impairment in this cohort of patients with acute and sub-acute LBP. We did find that people in lower SES groups experienced a higher association with fear avoidance beliefs about work and low back pain disability. This interaction was present at baseline, 4-weeks, and 6-months. Clinicians and researchers involved with management of LBP should be aware that fear-avoidance beliefs about work may have a stronger association with disability for patients with low SES, but future studies are needed to confirm these findings.
Acknowledgments
Michael Borut, Melissa Cere, Tony Cere, Michael Hodges, Dalton Reed, and Giorgio Zeppieri, JR collected data for this study.
SZG (PI), MER, and CV were supported by Grant # AR051128 from NIAMS/NIH while preparing this manuscript.
Footnotes
The authors of this manuscript have no financial or other relationship with any individuals or organizations that constitute a conflict of interest.
References
- 1.Robinson ME, Riley JL, 3rd, Myers CD, Papas RK, Wise EA, Waxenberg LB, et al. Gender role expectations of pain: relationship to sex differences in pain. J Pain. 2001;2:251–257. doi: 10.1054/jpai.2001.24551. [DOI] [PubMed] [Google Scholar]
- 2.Picavet HS, van den Bos GA. The contribution of six chronic conditions to the total burden of mobility disability in the Dutch population. Am J Public Health. 1997;87:1680–1682. doi: 10.2105/ajph.87.10.1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Badley EM, Webster GK, Rasooly I. The impact of musculoskeletal disorders in the population: are they just aches and pains? Findings from the 1990 Ontario Health Survey. J Rheumatol. 1995;22:733–739. [PubMed] [Google Scholar]
- 4.Fritz JM, George SZ. Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Phys Ther. 2002;82:973–983. [PubMed] [Google Scholar]
- 5.Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. doi: 10.1007/s10865-006-9085-0. [DOI] [PubMed] [Google Scholar]
- 6.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. Jama. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 7.Blaxter M. Whose fault is it? People's own conceptions of the reasons for health inequalities. Soc Sci Med. 1997;44:747–756. doi: 10.1016/s0277-9536(96)00192-x. [DOI] [PubMed] [Google Scholar]
- 8.Blaxter M. Evidence on inequality in health from a national survey. Lancet. 1987;2:30–33. doi: 10.1016/s0140-6736(87)93062-5. [DOI] [PubMed] [Google Scholar]
- 9.Adler N, Matthews K. Health psychology: why do some people get sick and some stay well? Annu Rev Psychol. 1994;45:229–259. doi: 10.1146/annurev.ps.45.020194.001305. [DOI] [PubMed] [Google Scholar]
- 10.Gallo LC, Matthews KA. Understandinf the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bullertin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 11.George SZ, Zeppieri G, Jr, Cere AL, Cere MR, Borut MS, Hodges MJ, et al. A randomized trial of behavioral physical therapy interventions for acute and sub-acute low back pain ( NCT00373867) Pain. 2008;140:145–157. doi: 10.1016/j.pain.2008.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine (Phila Pa 1976) 1987;12:S1–S59. [PubMed] [Google Scholar]
- 13.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–784. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- 14.Nam CB, Powers MG. Variations in socioeconomic structure by race, residence, and the life cycle. American Sociological Review. 1965;30:97–103. [Google Scholar]
- 15.Hollingshead AB. Commentary on the indiscriminate state of social class measurement. Social Forces. 1971;49:563–567. [Google Scholar]
- 16.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 17.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 18.Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine. 1992;17:617–628. doi: 10.1097/00007632-199206000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Fairbank JC, Couper J, Davies B, O´Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 20.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25:3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 21.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 52. [DOI] [PubMed] [Google Scholar]
- 22.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. doi: 10.1016/0304-3959(93)90127-B. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan MJ, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychological Assessment. 1995;7:524–532. [Google Scholar]
- 24.Baron RM, Kenny DA. The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 25.Leeuw M, Houben RM, Severeijns R, Picavet HS, Schouten EG, Vlaeyen JW. Pain-related fear in low back pain: a prospective study in the general population. Eur J Pain. 2007;11:256–266. doi: 10.1016/j.ejpain.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 26.George SZ, Fritz JM, Bialosky JE, Donald DA. The effect of a fear-avoidance-based physical therapy intervention for patients with acute low back pain: results of a randomized clinical trial. Spine. 2003;28:2551–2560. doi: 10.1097/01.BRS.0000096677.84605.A2. [DOI] [PubMed] [Google Scholar]
- 27.Feuerstein M, Beattie P. Biobehavioral factors affecting pain and disability in low back pain: mechanisms and assessment. Phys Ther. 1995;75:267–280. doi: 10.1093/ptj/75.4.267. [DOI] [PubMed] [Google Scholar]
- 28.Fritz JM, George SZ, Delitto A. The role of fear-avoidance beliefs in acute low back pain: relationships with current and future disability and work status. Pain. 2001;94:7–15. doi: 10.1016/S0304-3959(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 29.Crombez G, Vlaeyen JW, Heuts PH, Lysens R. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain. 1999;80:329–339. doi: 10.1016/s0304-3959(98)00229-2. [DOI] [PubMed] [Google Scholar]
- 30.Carr JL, Moffett JA. The impact of social deprivation on chronic back pain outcomes. Chronic Illn. 2005;1:121–129. doi: 10.1177/17423953050010020901. [DOI] [PubMed] [Google Scholar]
- 31.Brekke M, Hjortdahl P, Kvien TK. Severity of musculoskeletal pain: relations to socioeconomic inequality. Soc Sci Med. 2002;54:221–228. doi: 10.1016/s0277-9536(01)00018-1. [DOI] [PubMed] [Google Scholar]
- 32.Latza U, Kohlmann T, Deck R, Raspe H. Can health care utilization explain the association between socioeconomic status and back pain? Spine. 2004;29:1561–1566. doi: 10.1097/01.brs.0000131435.56714.15. [DOI] [PubMed] [Google Scholar]
- 33.George SZ, Fritz JM, Childs JD. Investigation of elevated fear-avoidance beliefs for patients with low back pain: a secondary analysis involving patients enrolled in physical therapy clinical trials. J Orthop Sports Phys Ther. 2008;38:50–58. doi: 10.2519/jospt.2008.2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jordan KP, Thomas E, Peat G, Wilkie R, Croft P. Social risks for disabling pain in older people: a prospective study of individual and area characteristics. Pain. 2008;137:652–661. doi: 10.1016/j.pain.2008.02.030. [DOI] [PubMed] [Google Scholar]