Abstract
Shared family mealtimes have been identified as potential promoters of healthy child development. This observational study of 200 family mealtimes examined the relation between child health indicators in a group of children with persistent asthma and three dimensions of mealtime interaction: Action, Behavior Control, and Communication. Mealtimes lasted, on average, 18 minutes with a range of 2 to 47. Percent of time spent in Action and Positive Communication varied by asthma symptom severity and child quality of life as well as family socio-demographic variables (maternal education, child ethnicity, family structure). Stepwise regression analyses revealed that controlling for maternal education and overall general family functioning, positive communication during family mealtimes predicted child quality of life. Significant interactions between demographic variables and behavior control suggested that higher levels of behavior control affected child quality of life in the context of lower maternal education. Guidance is offered for practitioners and policymakers toward promoting healthy family mealtimes as a public health priority.
Family mealtimes are regular and repetitive events experienced by the vast majority of children and adolescents in the United States. Survey responses from nationally representative samples such as the National Longitudinal Study of Adolescent Health (Add Health) and the Early Childhood Longitudinal Study (ECLS-K) indicate that approximately 70% of children and adolescents share a meal with at least one adult three or more times a week (Gable, Chang, & Krull, 2007; Videon & Manning, 2003). The frequency of shared family mealtimes has been associated with diverse positive child health outcomes such as the consumption of fruits and vegetables (Videon & Manning, 2003) and reduced risk of substance abuse (Eisenberg, Neumark-Sztainer, Fulkerson, & Story, 2008). Conversely, low frequency of shared family mealtimes (fewer than three times a week) has been associated with poorer health outcomes such as eating disorders (Neumark-Sztainer, Eisenberg, Fulkerson, Story, & Larson, 2008) and obesity (Gable, et al., 2007). However, yet to be determined is how the more precise quality of family interactions observed at mealtimes relates to child health. Thus, the main purpose of this study is to extend research linking frequency of family mealtimes to children’s health and consider how the ABCs of family interactions observed during family mealtimes (Action, Behavior Control, and Communication) are related to indicators of children’s health-related outcomes.
Pediatric psychologists have found mealtimes a useful setting to examine family functioning for children with a chronic health condition. Because mealtimes are a unique opportunity to check in with family members, observations during meals have been particularly useful in instances where the child’s condition requires careful attention to diet such as diabetes (Patton, Dolan, & Powers, 2008). There is also reason to consider other chronic health conditions such as asthma, where careful monitoring of the child’s symptoms may be associated with better outcomes. For example, in a previous report open and direct forms of communication during mealtimes were found to mediate the relation between lung functioning and separation anxiety symptoms in children with persistent asthma (Fiese, Winter, Wamboldt, Wamboldt, & Anbar, 2010). Although the proposed mechanisms of effect have yet to be specified due to the cross-sectional nature of the majority of this research, mealtimes provide an opportunity for emotional support and parental monitoring that is regular, repetitive, and involves the entire family. Thus, it is an ideal setting to identify family level variables that may be related to children’s health outcomes such as quality of life.
In this study, we extend previous work linking the frequency of shared family mealtimes and global ratings of family functioning to children’s health and wellbeing to consider how the quality of time spent during mealtimes may either promote or derail healthy outcomes for children with a chronic health condition. We also extend the work of the pediatric literature to consider how the socio-demographic context may alter the quality of observed mealtimes.
Multiple Layers of Family Mealtimes
Mealtimes are part and parcel of family routine life that is composed of at least two layers: the repetitive nature of the routine (i.e., the frequency) and what is conveyed and communicated during the event (Fiese, 2006). While they typically last only about 20 minutes (Ramey & Juliusson, 1998), family mealtimes are densely packed events where the news of the day is shared, rules of interaction are embedded in how the meal is conducted, and emotions are regulated on a moment-by-moment basis. Thus, this regular everyday routine includes aspects of family interaction that child development researchers have long recognized as significant to child outcomes.
Some observational studies of mealtimes have gone beyond examining the frequency of mealtimes to examine family interaction during the meal. For example, studies using global coding schemes, primarily the Mealtime Interaction Coding System (Dickstein, Hayden, Schiller, Seifer, & San Antonio, 1994) based on the McMaster model of family functioning (Epstein, Baldwin, & Bishop, 1983) have revealed associations between family mealtime functioning and child outcomes including better mental (Dickstein, Seifer, Hayden, Schiller, Sameroff, Keitner, et al., 1998) and physical (Speith, et al., 2001) health. Consistent across these observational studies is the importance of clear and direct communication in predicting healthy child outcomes (Mitchell, Powers, Byars, Dickstein, & Stark, 2004).
A second important feature of family interaction that has often been detected during family mealtimes is the relative amount of control or intrusiveness exerted by parents towards their children. For example, authoritative parenting styles during mealtime have been associated with more optimal health outcomes for preschool age children (Patrick, Nicklas, Hughes, & Morales, 2005). Yet, findings are somewhat mixed in regards to which parenting styles observed during mealtimes are optimal for healthy child outcomes. For example, both laissez-faire styles (Hughes, Shewchuk, Baskin, Nicklas, & Qu, 2008) and restrictive styles (Faith, Scanlon, Birch, Francis, & Sherry, 2004) have been associated with poorer children’s health. The degree to which behavior is managed or controlled appears to be an essential feature of the task of feeding children (Hughes, Power, Fisher, Mueller, & Nicklas, 2005).
A third interactive feature associated with child health outcomes is the apparent activity level or distractions evident during the meal. For instance, a noted public health concern is the presence of television during shared mealtimes (Deitz & Gortmaker, 1985), in part because high rates of television viewing during mealtimes have been associated with greater consumption of pizza and snack foods and less consumption of fruits and vegetables for children (Coon, Goldberg, Rogers, & Tucker, 2001). Other mealtime activities shown to be associated with poor health outcomes include playing computer games (Brunstrom & Mitchell, 2006) and being away from the table (Patton, Dolan, & Powers, 2008). Of central concern to us is the role that this type of added “action” can play in distracting family members from interaction and disrupting effective communication. Indeed, parents who report having television on during mealtimes often admit to doing so to avoid conflict at the table (Hersey & Jordan, 2007).
Therefore, in this study we specifically focus on three critical aspects of family mealtimes by examining the amount of time families engage in Action, Behavior Control, and Communication. The Action domain reflects the amount of time that a family member is physically away from the group, talking on the phone, watching television, or engaged with an electronic device. Our second domain, Behavior Control, is intended to capture the amount of time spent engaging in overly restrictive behaviors during mealtimes. Communication, the third domain we focus on, is based on the previously mentioned research suggesting that open and direct forms of communication are associated with more optimal outcomes for children. We expand this work by including three specific forms of communication: communication directly related to the meal itself, critical forms of communication, and positive communication that conveys genuine concern about others’ ideas and feelings. We reasoned that meal-related conversations would reflect the more mundane aspects of the routine and would be less likely to be associated with the more meaningful aspects of the mealtime ritual that involves interpersonal commitment and emotional connections (Fiese, Foley, & Spagnola, 2006). We also included critical forms of communication based on a plethora of evidence that criticism and conflict can have harmful effects on children (Davies, Sturge-Apple, Winter, Cummings, & Farrell, 2006); we predicted that more critical communication would be associated with poorer child health. Last, we examine positive forms of communication as exchanges concerned with others and affording emotional connections and genuine investment in others’ activities (including health-related activities), and expected them to be associated with better health outcomes for children. Thus, we examined the A (Action), B (Behavior Control), C’s (Communication) of family mealtimes. We expected that healthy mealtimes would be characterized by a greater relative amount of time dedicated to positive communication than to behavior control or action.
A nagging concern in the study of family routines, in general, and shared mealtimes in particular is whether they are but markers of general family functioning (Dickstein, 2002). Although it can be argued that the qualities that make for a healthy mealtime interaction (i.e., clear and direct communication, positive affect, clear boundaries) are also qualities expected in healthy families in general, we contend that there may also be unique characteristics of mealtime as an organized family event. Family routines address one aspect of daily family life- the organization of family interactions. Although it is beyond the scope of this study, the study of routines provides an opportunity to examine episodic events that have a clear beginning and end, are communal, goal-directed activities, and the meaning conveyed during these interactions serve as “informational events” for the entire group (Howe, 2002). To begin to consider whether the organization of the interactions observed during this family routine are distinct from overall family functioning, we simultaneously considered the effects of such qualities as being able to freely express feelings and family acceptance and mealtime interactions.
Persistent Asthma as a Family and Public Health Concern
The family context in which we conducted our observations is raising children with a chronic health condition: persistent asthma. Asthma is one of the most common chronic diseases of childhood, affecting over six million children in the United States (NEPR-3, 2007). On average, in a classroom of 30 children about three are likely to have asthma. Several family interaction variables have been found to moderate and mediate the expression of asthma symptoms, including open and direct communication, positive affect, and low levels of conflict (Kaugers, Klinnert, & Bender, 2004) Although the precise mechanisms of effect have yet to be fully explicated, the presence of a calm and supportive environment able to monitor medication use is speculated to promote better lung functioning and reduce overall family stress (Kaugers, et al., 2004). Thus, we expected that children in families with mealtimes characterized by more engaged communication and less time in conflict would have better overall health. Mealtimes afford an opportunity to check in on how the child is feeling that day and thus can index symptom monitoring, a known feature of better adjustment in children with asthma (McQuaid, 2001).
While not curable, per se, the symptoms of asthma (shortness of breath, wheezing, waking in the middle of the night) can be controlled when patients adhere to prescribed medications and avoid environmental allergens. Yet, adherence to prescribed medication regimens is typically low, hovering less than fifty percent in many cases (Bender, et al., 2000). Adherence to medical protocols is frequently considered a marker of family management (McQuaid, Walders, Kopel, Fritz, & Klinnert, 2005) as well as symptom control (Bender, et al., 2000). Thus, we considered adherence to prescribed medications as one of our family level health indicators.
Children with persistent asthma are also known to experience compromised quality of life (Annett, Bender, Lapidus, DuHamel, & Lincoln, 2001). Quality of life refers to the impact of the illness on daily activities and how the individual adapts to the illness in a variety of domains (e.g., emotional, physical activities, social. Assessing child quality of life has the added advantage of capturing health indicators that vary on a daily basis that may be not be reflected in measures of lung functioning such as how much the child worries about their symptoms, how much their symptoms get in the way of participation in sports and other activities, and how much their symptoms affect exchanges with peers. Thus, we examined multiple health indicators associated with wellbeing in children with persistent asthma, including: an objective assessment of lung functioning; adherence to prescribed medications thought to reflect family management as well as reduce health symptoms; parent report of child asthma symptoms; and child report of quality of life as it pertains to his or her asthma influencing daily life.
Socio-demographic Context
Compared to the general population, low-income, minority children and children residing in inner cities are most likely to visit emergency departments, be hospitalized, and die due to asthma (NEPR-3, 2007). African Americans are about 20% more likely to have ever have been diagnosed with asthma than Caucasians and access to health care is more problematic for non-white families (Brim, Rudd, Funk, & Callahan, 2008). Moreover, these socio-economic and ethnic factors can interact and affect the expression of asthma symptoms in children (Chen, Bloomberg, Fisher, & Strunk, 2003). Thus, it is important for studies of child health to attend to socio-demographic variables.
Although we expected socio-demographic factors such as ethnicity and parental education to be associated with child health outcomes, we were less sure of the nature of their association with the mealtime family interaction variables. There is considerable inconsistency in the literature regarding relations among mealtime frequency and practices and socio-economic status. Variations in the frequency of shared mealtimes according to ethnicity and parent education have been reported across several large scale studies (Bradley, Corwyn, McAdoo, & Coll, 2001; Flores, Tomany-Korman, & Olson, 2005) whereas other surveys do not find such differences (Moore, Whitney, & Kinukawa, 2009). The pediatric literature that incorporates mealtime observations typically controls for socio-demographic differences or does not report variations by education or ethnic background. Thus, we present socio-demographic differences for descriptive purposes and to inform future prevention and intervention efforts.
Restatement of Goals
We had three major goals in this report. First, we aimed to describe, in general, the amount of time that families engage in action, behavior control, and communication during a shared mealtime. We present the percent of time in relation to child health indicators for a group of families raising a child with persistent asthma. Second, we examine whether the percent of time engaged in family mealtime behaviors varies by socio-demographic variables. Third, to test whether our mealtime ABCs are merely a marker of overall family functioning, we examine simultaneously the prediction of mealtime behaviors in predicting child health variables while controlling for socio-demographic variables and overall family functioning. We included this analysis to consider whether our observational measures of shared family mealtimes were just markers of overall family functioning or somehow unique. Last, we explored the multiplicative interplay of socio-demographic variables and mealtime ABC’s in predicting child health outcomes.
Method
Participants
Data were drawn from a larger study of family life and asthma. Families were recruited through an ambulatory clinic at a teaching hospital, a pediatric pulmonary clinic, or area group pediatric practices in a mid-size city. A child was enrolled in the study if, at the time of recruitment, he or she: (1) was between the ages of five and twelve, (2) had an asthma diagnosis (of at least one year) as indicated by physician notes in medical records and by a spirometric test conducted by a licensed respiratory therapist and analyzed by a pediatric pulmonologist, (3) was prescribed daily asthma controller medication for at least six months, and (4) was not diagnosed with another chronic medical condition that required a daily medication. Participants included in this report include 215 children (136 boys and 79 girls), ages 5 – 12 (M = 7.9; SD = 2.18), and their primary caregivers (94% mothers, 3.7% fathers, and 2.3% grandmothers). Caregiver-reported child race was 53% Non-Hispanic White and 47% Non-White non-Latino(31% African-American, 13% Other (typically mixed ethnicity), .5% Asian-American, and 3% Hispanic). Socioeconomic status, as indexed by the Hollingshead index (Hollingshead, 1975), ranged from 8.0 – 66.0 (M = 38.58; SD = 16.34). Forty-seven percent of primary caregivers reported being in their first marriage, 11% living with a partner, 7% remarried, 23% single or widowed, and 12% separated or divorced. Thirty percent of the mothers reported having a high school education or less. Family size ranged from two to 11, with a median household size of four members.
We report on 200 of the recorded family mealtimes. Fifteen mealtimes were not coded either due to inability to schedule (6 families) or poor quality of tape (9 families). The families whose meals were not coded did not differ from the total sample in terms of maternal education or household structure; there was trend for more non-Hispanic white children than non-Latino non-white children to have a mealtime coded (X2 (215) = 4.49, p = .057.)
Procedure
In this Institutional Review Board approved study, caregiver written consent and child verbal assent were obtained and then children and caregivers were interviewed in a laboratory setting (a research home adjacent to a university). Also during the laboratory visit, lung functioning was determined through a pulmonary function test conducted by a licensed respiratory therapist. Within approximately one week of the laboratory visit, family general functioning via caregiver report and family mealtime interaction were assessed in a home visit. Research assistants went to the family’s home, set up a video camera, and instructed the family on how to record the meal. Medication adherence was recorded for six weeks.
Measures
Demographics and Socio-Economic Indicators
Primary caregivers reported all demographics via questionnaire including child ethnicity. Primary caregivers indicated their level of education and relationship status (e.g, married, remarried, co-habitating, single).
Medication Adherence
The assessment of medication adherence depended on the prescribed medication. Inhaled medication dispensed in canisters, were monitored using MDIlog-II devices that automatically record the date and time of day when the medication is used. DPIs (e.g., Advair®) or oral controller medications (e.g., Singulair®), were monitored by telephone once per week for a six week tracking period. While the MDIlog ratings may provide a more objective measure of adherence (Bender, et al., 2000), telephone diaries are also thought to provide acceptable estimates of medication adherence (Rapoff, 1999). We divided the number of doses taken by doses prescribed for each day and calculated an average percentage of adherence across the six week period. The average rate of adherence was 72% (SD = .32) with a range of .01 to 1.00. We had the complete six week adherence data for 187 of the 200 mealtime participating families (missing data was due to mechanical failure in 10 of the cases, two lost devices, and one family failed to complete). These families with missing data did not differ in any significant ways from the participating families.
Functional Asthma Severity
The Functional Severity of Asthma Scale (FSS; (Rosier, 1994) is completed by the caregiver and includes six items assessing the child’s asthma symptom severity over the past year. We report the total functional severity score. Validity of the FSS has been demonstrated by its meaningful associations with school days missed, functional impairment, and medical care visits (Rosier, 1994). For this sample, internal consistency was α = .71.
Asthma Severity/Lung Function (Spirometry)
Consistent with standard procedures, testing was performed by a respiratory therapist using a PDS 313100-WSU KOKO Spirometer and yielded measurements of forced vital capacity (FVC), forced expiratory flow in one second (FEV1), and forced expiratory flow, 25% to 75% of vital capacity (FEV25–75). Each child performed three FVC maneuvers into a spirometer while at rest, and the test with the largest sum of FVC and FEV was used for analysis. Spirometry was repeated ten minutes after AlbuterolR was administered by metered dose inhaler with aid of an Aerochamber. We report FEV1 as a baseline measurement of child lung functioning. Mean FEV1 for this sample was 1.56 (SD = .50) with a range of .61–3.29. Degree of severity was classified as: FEV1 ≤ 40% of predicted = severe; FEV1 > 40% and ≤ 60% = moderate; FEV1 > 60% and ≤ 80% = mild; and FEV1 80% or greater = slight, or normal. These classifications, made by a board certified pediatric pulmonologist, yielded a 1–4 scale where higher scores indicate more compromised lung function. Based on the PFT readings, 63% of the sample were determined to have mild to moderate asthma, 30% moderately severe, and 7% severe.
Child Quality of Life
Children eight years and older completed the Pediatric Asthma Quality of Life questionnaire (PAQL; (Juniper, 1993), a 23-item asthma-specific quality of life measure that assess physical, emotional, and social impairment due to asthma over the past week. Higher scores denote less impairment, or higher quality of life. Internal consistency of the subscales for this sample (Chronbach’s alpha) were Action = .90, Symptoms = .78, Emotion = .78, and Total Score = .87. Children under the age of eight years completed the Pictorial Version of the Pediatric Asthma Quality of Life (Everhart & Fiese, 2009). Predictive validity has been demonstrated, and similar factor structures of emotion and social impairment evidenced, for the pictorial version and the standard PAQL . Chronbach’s alpha for this sample were Symptoms = .83, Emotions = .71 and Total = .86. Items were standardized and the Symptoms, Emotions, and Total scores were used.
Family General Functioning
The General Functioning (GF) scale of the Family Assessment Device (FAD; (Epstein, et al., 1983) was used to determine overall family climate/functioning. The FAD has been used extensively with families experiencing a chronic illness (Alderfer, et al., 2008) and the General Functioning scale has proven to reliably distinguish well-functioning from poorly functioning families (Epstein, et al., 1983). Sample items from the GF scale include “individuals are accepted for who they are,” “we can express our feelings to each other,” and “we don’t get along with each other” (reverse scored). Internal consistency for this sample was α = .82.
Mealtime Interaction
Videotaped family meals were coded using the ABC Mealtime Coding System (Fiese, Botti, & Greenberg, 2007), a micro-coding system designed to assess five dimensions of mealtime behavior: (1) Action-oriented behaviors are those in which a participant’s attention is diverted away from the meal. Examples include answering the phone or door, leaving the table to retrieve something for the meal (e.g., dishes), or watching television; (2) Behavior Control behaviors intended to stop, direct, or otherwise modify another person’s behavior. Examples include commands (“stop hitting your sister”) or physical action (bringing a child back to the table in a harsh manner); (3) Meal-Oriented Communication includes verbal exchanges or directives pertaining to the food and other routine aspects of the meal. Examples include whether someone wants seconds, who will clean up after the meal, and requests to pass a dish; (4) Positive communication includes statements that share information among participants. Examples include discussion of one’s feelings/emotions, discussion of beliefs or interests outside of the food being served, friendly joking, and discussion of life and family events; and (5) Critical Communication includes disapproving or harsh statements (verbal content and/or tone) regarding another participant’s behavior or personality. Examples include “You’re so annoying,” “You eat like a pig,” and “You always forget to put your dishes in the dishwasher.”
Two coders, blind to the objectives of this study, independently viewed and coded each videotaped meal recording. Each time a behavior occurred during the meal, the rater noted the participant (primary caregiver, target child, secondary caregiver, sibling), the category of behavior, and the beginning and ending time of the behavior. Twenty percent of the interactions were double-coded by both raters. Interrater reliability for the occurrence of the five categories, indexed by intraclass correlation coefficients, were Action = .86; Behavior Control = .96; Mealtime Communication = .97; Positive Communication = .98; Critical Communication = .96. INTERACT software, which allows for the simultaneous coding of multiple individuals across categories of behaviors, was used to record the observations.
The total time spent participating in each category of behavior was calculated by summing the time for all behaviors for a meal participant. Total time spent in each category was then summed across family members. Finally, total time spent in a given category of behavior was divided by total interaction time for the entire family, yielding a total proportion of time spent in each type of behavior for each family meal. This approach allowed for comparisons across families, weighted by the amount of time each family spent interacting during their particular mealtime. For purposes of this study, in which we were interested in whole family patterns of response, we summed scores across family members to yield the total percent time spent in Action, Behavior Control, Meal-Related, Positive, and Critical Communication.
Data analytic strategy
We began by conducting descriptive analyses on the main study variables. To address the first objective of this study - to describe the amount of time that families engage in various activities during a shared mealtime - we examined variations in the percent of time families spent in the five mealtime behaviors by child health variables. We used an ANOVA strategy with follow-up univariate tests except in instances of continuous child health variables, in which we examined bivariate correlations. Next, we used ANOVA’s and follow-up univariate tests to address the second objective of examining the percent of time spent engaging in the five mealtime behaviors according to the socio-demographic variables. Finally, we addressed the third study objective by examining the unique contribution of family mealtime behaviors to child health variables above and beyond socio-demographic and general family functioning in a series of regression analyses controlling for child ethnicity, maternal education and parent report of family functioning. We also considered the interactive effects of socio-demographic variables and mealtime variables in predicting child health variables using the procedures outlined in Baron & Kenny, 1986.
Results
Consistent with previous studies, meals lasted an average of 18.7 minutes, with a range of 8.3 to 46.3 minutes. The greatest percent of time was spent either in some form of Action or Positive Communication. There was considerable range across these mealtime interaction categories (see Table 1). The amount of time spent in Action was negatively related to time spent in Positive Communication and Mealtime Communication. Time spent controlling behavior was positively related to Critical Communication and Mealtime Communication (Table 1). Age of target child was not associated with time spent in interaction categories, with the exception of Mealtime Communication which was negatively associated with age, r = −.19, p < .001.
Table 1.
Intercorrelations and Average Percent Time Spent in Mealtime Interaction Behaviors
| Mealtime Behavior | 1 | 2 | 3 | 4 | 5 | M | SD | Range |
|---|---|---|---|---|---|---|---|---|
| 1. Action | −.09 | −.41*** | −.86*** | .03 | .40 | .24 | .01–.94 | |
| 2. Behavior Control | .21** | −.10 | .20** | .01 | .02 | .00–.18 | ||
| 3. Mealtime Communication | −.10 | −.10 | .19 | .11 | .02–.76 | |||
| 4. Positive Communication | −.03 | .40 | .22 | .02–.95 | ||||
| 5. Critical Communication | .002 | .01 | .00–.05 |
p < .01; p < .001
Several significant, albeit modest, bivariate correlations between the asthma indicators and mealtime behavior were evidenced (Table 2). The most consistent pattern of findings was with Communication and Action. Positive Communication was positively associated with child QOL, medical adherence and reduced number of parent-reported asthma symptoms. Action and Critical Communication were negatively related to child QOL.
Table 2.
Associations Between Mealtime Behaviors and Asthma Health Indicators
| Mealtime Behaviors | |||||
|---|---|---|---|---|---|
| Activities | Behavior Control | Communication | |||
| Mealtime | Positive | Critical | |||
| Asthma Indicators | |||||
| Lung Functioning (FEV1) | .01 | −.07 | −.18** | .09 | −.05 |
| Medical Adherence | −.14 | −.07 | −.05 | .20** | −.16* |
| Functional Severity | .10 | .15* | .06 | −.16* | .13 |
| Child Quality of Life | |||||
| Symptoms | −.16* | −.15* | −.02 | .20** | −.19** |
| Emotions | −.16* | .03 | −.04 | .20** | −.15 |
| Total | −.18** | −.08 | −.01 | .21** | −.18** |
p < .05
p < .01
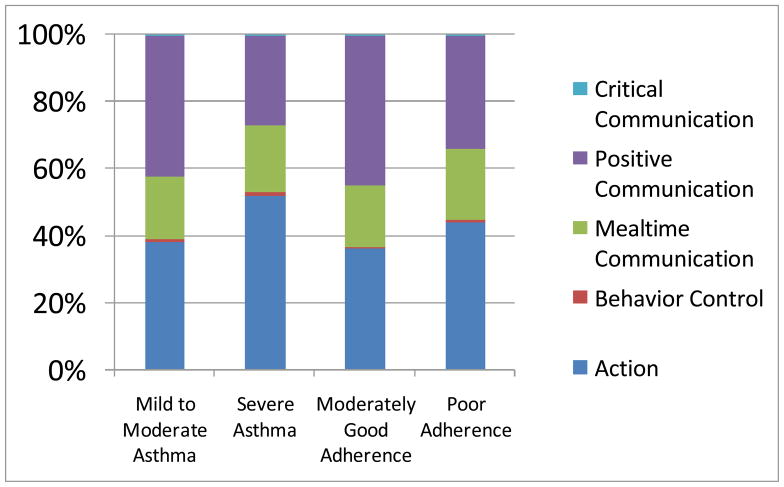
We also considered degree of asthma severity based on lung functioning. Children with the most severe forms of asthma experienced more time in Action, F (3, 191) = 3.82, p < .01, and less time in Positive Communication, F (3, 191) = 4.85, p < .002, than children with less severe forms of asthma (see Figure 1).
Figure 1.
Percent of time spent in mealtime interactions and asthma indicators
We also separately examined families who evidenced poor medical adherence patterns. The average rate of adherence in this sample was 72% over the six week period. Though there is no gold standard for medical adherence, researchers and clinicians alike have found that adherence below 70% often presents increased risk for poor health outcomes (Bender, Rankin, Tran, & Wamboldt, 2008). For descriptive purposes, we compared mealtime behaviors in those families who adhered to their child’s medications less than 70% of the time vs. those who adhered greater than 70% of the time. Families in the low adherence group engaged in more mealtime Action (F (1, 171), = 5.52, p < .01), more Critical Communication (F (1, 171) = 4.49, p < .05), and less Positive Communication (F (1, 171) = 12. 27, p < .0001) than families who adhered to their child’s medical protocol more than 70% of the time (see Figure 1).
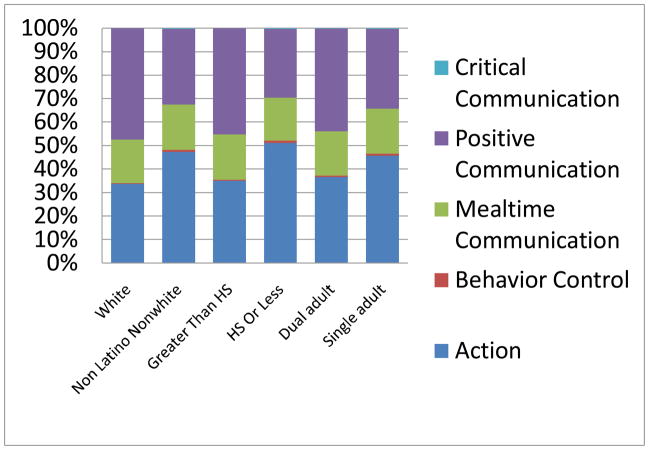
We next examined differences according to demographic variables. Overall, there were significant differences according to child ethnicity (F (4, 195) = 12.36, p < .001) across the four mealtime categories. Follow-up univariate analyses revealed that families with non-Latino non-white children engaged in more time around Action (F (1, 198) = 17.01, p < .001), less time in Positive Communication (F (1, 198) = 27.10, p < .0001), more time in Behavior Control (F (1, 198) = 12.67, p < .001) and more time in Critical Communication (F (1, 198) = 11.74, p < .001) than families of non-Hispanic white children. There were no significant differences in amount of time spent in Mealtime Communication. A similar pattern held according to maternal education, with families whose mother had a high school education or less showing significant differences overall (F (4, 193) = 9.25, p < . 001). Follow-up univariate analyses revealed that families whose mothers had a high school education or less spent more time in Action (F (1, 196) = 21.25, p < .0001), Critical Communication (F (1, 196) = 8.70, p < .01) and less time in Positive Communication (F (1, 196) = 24.94, p < .0001). There were no significant differences in time spent around Mealtime Communication. In terms of household structure, there was an overall effect for single adult versus dual adult households (F (4, 193) 3.61, p < .01). Follow up univariate analyses revealed that single parent households engaged in more Action (F (1, 198) = 6.28, p < .01), more Behavior Control (F 1, 198) = 4.21, p < .05), and less Positive Communication (F (1, 198) = 10.32, p < .01) than households with two adult caregivers. There were no differences according to amount of time spent in Mealtime Communication or Critical Communication. Percent of time spent in the various mealtime behaviors according to socio-demographic variables are presented in Figure 2.
Figure 2.
Percent time spent in mealtime interactions and socio-demographic variables
Our third set of analyses examined the effects of mealtime behavior predicting child health variables above and beyond socio-demographic variables and general family functioning. We used a regression strategy blocking child ethnicity or maternal education and parent report of general family functioning in the first block and family mealtime behaviors in the second block. In most cases, child ethnicity and maternal education were significant predictors of child health variables to the exclusion of mealtime behaviors. The exceptions were the contribution of Positive Communication predicting child Emotions and total QOL beyond mother education and family functioning (See Table 3).
Table 3.
Contribution of Mealtime Interpersonal Communication to Child Quality of Life
| β | ΔF | ΔR2 | |
|---|---|---|---|
| Quality of Life Emotions | |||
| Step 1 | |||
| Mother Education | −.16 | 3.76 | .04* |
| Step 2 | |||
| General Family Functioning | −.19 | 1.01 | |
| Step 3 | |||
| Mealtime Personal Communication | .75 | 4.76 | .03* |
| Total Quality of Life | |||
| Step 1 | |||
| Mother Education | −.21 | 6.49 | .06* |
| Step 2 | |||
| General Family Functioning | −.11 | 0.31 | |
| Step 3 | |||
| Mealtime PersonalCommunication | .69 | 3.79 | .02* |
p < .05
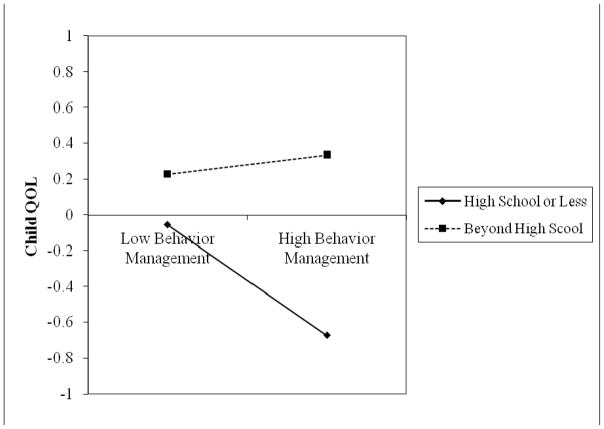
Finally, we explored the interactions between mealtime behaviors and socio-demographic characteristics in predicting child health indicators. We found a significant interaction between maternal education and Behavior Control predicting child QOL (F (3,168) = 4.83, p < .05). For households in which mothers had a high school education or less, child QOL was compromised when there were higher levels of Behavior Control. There was no such effect for households in which mothers had greater than a high school education (Figure 3). Reflecting a similar pattern, the interaction of ethnicity and Behavior Control predicted child QOL (F (3,194) = 4.57, p < .05) and medication adherence (F (3, 172) = 4.65, p < .05), such that high Behavior Control was associated with lower QOL and adherence only in non-Hispanic white families.
Figure 3.
Interaction between mealtime behavior control and maternal education level predicting child QOL
Discussion
We offer this report as a glimpse into a family routine that holds promise for affecting child health: family mealtimes. Although mealtimes lasted on average only 18 minutes, we found significant relations between time spent in specific forms of mealtime interactions and child health variables. In addition, our results highlight that the intertwined nature between socioeconomic risk and children’s health cannot be ignored, as we found strong associations for child ethnicity and maternal education in relation to asthma symptoms and child quality of life. We frame our discussion by considering the relative time spent in different types of family interactions during the course of a mealtime, the potential for specific types of mealtime behaviors to be associated with different types of health variables, the social roots of children’s health in a socio-demographic context, and potential applications to practice and policy.
The bulk of family mealtime interactions were divided between some form of activity (e.g., getting up and down from the table, talking on the phone, watching television) or communication about personal events (e.g., school happenings, whether the family should get a new puppy, homework assignments). It was the relative amount of time spent in these two types of interaction that distinguished families from different ethnic backgrounds, maternal education, single versus dual adult households, child quality of life, severity of asthma symptoms, and adherence to the asthma treatment regimen. When family members were more engaged with each other and demonstrated an interest in daily events during their mealtime conversations, child asthma symptoms were less likely to be severe and adherence to the medical regimen was likely to be greater. When mealtimes were characterized by more distractions, asthma symptoms were more pronounced. Of course, it is not possible to effectively communicate about personal events of the day if attention is turned to the television or catching up with a best friend on a cell phone. In terms of asthma symptoms and medical adherence, it may be that mealtime conversations afford one opportunity to observe wheezing, coughing, and to check in on whether the child has taken his or her medication that day. These brief encounters may have long term consequences for the child’s health.
This observational study also underscores how the socio-demographic context of raising a child with a chronic health condition cannot be ignored. Families in which the primary caregiver had less education, children were non-Latino non-white, or there was only one adult caregiver in the household experienced more action during mealtime and less time spent catching up on the day’s events. These are also the children believed to be at greatest risk for poorly controlled asthma and most likely to use the emergency room for healthcare (Chen, et al., 2003). Researchers have pointed out that a more comprehensive understanding of health disparities requires attention to environmental factors that add to the chronic stress associated with compromised health in low income, minority, under-resourced individuals (Adler & Rehkopf, 2008). An interesting characteristic of chronically stressed environments that has been linked to compromised physical and mental health includes the relative amount of “hubbub” or inconsistent, socially non-responsive activities apparent in the family home (Evans, Gonnella, Marcynyszyn, Gentile, & Salpekar, 2005). Recent research suggests that lack of organization, or chaos, can disrupt learning and portend for poor socio-emotional development (Johnson, Martin, Brooks-Gunn, & Petrill, 2008). The action we observed during mealtime interactions are consistent with this notion, as they often included a “hubbub” of movement by multiple members of the family that made it difficult to follow conversations. Conversely, when conversations were sustained there was the appearance of a more organized mealtime.
The glimpse of family life we obtained through our observations suggests that potentially important mechanisms of protection or risk in chronically stressed environments may involve organizational and communication features of shared family mealtimes. Historically, the study of family routines has included a focus on their organizational features as a protective force from disruptions in the outside world. Indeed, family mealtimes as a set aside time for the family group evolved in response to the challenges of juggling work and school schedules in middle class families (Cinotto, 2006). However, our results also indicate that while organizing daily routines may be an avenue of protection, a tailored and culturally sensitive approach is necessary for families who are stressed by managing a chronic illness, are under-resourced economically and educationally, and have few means of social support.
There was one class of mealtime behaviors that was relatively infrequent that nevertheless were related to child health and socio-demographic variables: behavior control. Behavior control was modestly related to the severity of asthma symptoms and varied by child ethnicity and single vs. dual parent household status. Single parents were more likely to engage in some form of behavior control than households with another caregiver present. Behavior control was the only mealtime behavior that significantly interacted with education and ethnicity to predict one of the child health indicators, child quality of life. Consistent with previous reports that have found intrusive or indulgent parenting styles more prevalent in African American or low income families (Faith, et al., 2004; Hughes, et al., 2008) our results indicated that the relationship between more controlling mealtime behavior and child health depended on socio-demographic context. More specifically, time spent in behavior control was particularly deleterious to child QOL in the context of lower maternal education. In other words, children in families with less educated mothers experienced more social, emotional, and activity impairments due to asthma, particularly in the context of more controlling parenting. Likewise, more time in behavioral control was deleterious to child quality of life and medication adherence, but only for non-Hispanic white families; white children experienced less impairment in social, emotional, and activity functioning due to asthma compared to minority children, but only in the context of low behavior control. Thus, the impact of higher behavior control was most pronounced in the context of other socio-demographic risk factors (minority status and lower mother education). Consistent with other reports that have highlighted the complexity with which family interaction and socio-demographics may interact (McLoyd, Cauce, Takeuchi, & Wilson, 2000), the role that behavior control during mealtime may play for promoting health for some children deserves further elucidation.
In interpreting these results, it is important to note that our assessment of behavior control focuses on how parents attempt to manage behavior in ways that are most commonly thought of as intrusive and harsh. Although there may be some overlap with what is typically captured in parenting style scales concerned with “strict” styles of parenting (e.g., of authoritarian parenting), the fact that we did not find the same protective role in more disadvantaged families suggests we are not measuring the same construct. Instead, we believe that we are capturing a family dynamic that may be specific to mealtime settings and has been found to vary by socio-demographic context. Hughes and colleagues (Hughes, et al., 2006; Hughes, et al., 2008) report both indulgent and restrictive feeding styles in low income parents of young children. Whether our coding system accurately reflects important variations along dimensions of behavior control will require further investigation across families that are diverse not only in socio-economic status but also in developmental status of their children. We also note that this was a relatively infrequent behavior in our observations, which may be due to the definitions used in our coding scheme (e.g., our purposeful separation of behavior control from positive communication) or to the nature of the behavior itself that requires very little time to get the message across.
Although we were able to demonstrate modest effects of mealtime communication patterns on child quality of life above and beyond maternal education and general family functioning, these findings were very limited. We believe this does not detract from the potential contribution of the family mealtime to promoting health. Rather, it suggests that mealtime is but one proximal routine that may be associated with child health. Previous research has indicated that family routines tend to cluster together (McLoyd, Toyokawa, & Kaplan, 2008) and that disruptions in one routine, such as mealtime, can influence other routines such as bedtime (Fiese, Winter, Sliwinski, & Anbar, 2007). Mealtimes represent a regular event for the vast majority of families with young, school age and adolescent children (Bradley, et al., 2001). Thus, they provide an optimal setting for public health initiatives and prevention efforts and we hope this is a focus for the future. We also believe that future studies concerning the unique elements of routines such as how they begin and end over time, serve as communal goal setting environments, provide unique opportunities for sharing information, and provide a means to cope with stressful transitions would be fruitful.
There are several limitations to our study, including the single observation of one mealtime. Our method is consistent with other reports (Dickstein, et al., 1998) and 90% of the families reported that the recorded meal was “typical” or “very typical” of their usual mealtimes. Nevertheless, future efforts are warranted to determine whether multiple observations reveal the same pattern of results. We were also limited by the information we had available on socioeconomic context. Neighborhood poverty, parental work pressures, and access to healthy foods have been found to play a significant role in family mealtimes (Fiese & Schwartz, 2008). We recognize that this report is but one snapshot of a multifaceted setting embedded in a complex socio-cultural context. Future studies could add to our understanding of how culture, economic context, and the home environment (Harrison, et al., in press) may also influence patterns of mealtime interaction associated with child health.
Raising Healthy Children: Implications for Policy and Practice
We believe there are several practical implications suggested within our findings and the related literatures. First, it is important to emphasize that family mealtimes last only about 18 minutes, on average, and are casual affairs. The notion that family meals must be complicated, elaborate affairs can dissuade parents from engaging in this important activity. Second, families need guidance and support in creating communication strategies for their mealtimes. It may not be enough to suggest that families eat together four or more times a week if they come prepared to criticize, control, or avoid conversation altogether. Our analyses of time spent in this brief encounter suggests that families who spent seven or more minutes, on average, disengaged with each other by watching television, talking on the phone, or being otherwise disengaged from the mealtime conversation had children who experienced poorer health. These can also be families who experience more economic and parenting pressures in their lives by virtue of being single parents and having less educational resources available to them. This suggests a need to assist families to more effectively communicate and find compelling ways to remain at the table while shutting out distractions, a notion that may be particularly necessary in our current culture so often espousing the virtues associated with “multitasking.”
There are also developmental challenges to understanding how to construct healthy family mealtimes, both to researchers (methodologically) and to families (practically). From a methodological perspective, our study included families who ranged in size from two to 11, with ages of the children present at meals ranging from two months to 21 years. Methodologically, an average age approach does not reveal the interactional complexity and developmental demands placed on a family system with toddlers and school age children, infants and adolescents, four children under the age of five, or a set of twins. This is the reality of family mealtimes that statistical strategies have yet to successfully unravel. From a practitioner and curriculum perspective, it would be helpful to have succinct and useful guidelines to offer families for managing behaviors at different developmental periods as well as communication tips that extend across two or more age ranges. This will require not only careful thought but a theoretical framework to guide evidence based approaches.
Finally, there are active steps that policy makers can take in making family mealtimes a priority for communities and their constituents. There are opportunities for local, state, and federal governments to work toward incorporating family mealtimes into the public health agenda. Examples include food labeling, access to healthy foods in low income neighborhoods, public service announcements promoting healthy family mealtimes, and support for education programs (Fiese & Schwartz, 2008). State and federal governments subsidize food programs to children through WIC, SNAP, and school lunch programs. Incorporating healthy ways of relating during shared mealtimes in addition to evidence based nutrition practices is practical, has the opportunity to reach a large number of children, and is also based on an increasingly large evidence base. Just as children’s safety became a national priority through campaigns and legislation surrounding seat belt use, raising awareness and investing in public support for healthy family mealtimes would not only be money well spent but may also be as simple as ABC.
Acknowledgments
This research was supported, in part, by grants from the National Institutes of Health to the first author (MH 51771, HD057447). The authors express their gratitude to the families who allowed us into their homes as a part of this study and to Stacey Greenberg who assisted in developing an earlier version of the ABC manual.
Contributor Information
Barbara H. Fiese, University of Illinois at Urbana-Champaign
Marcia A. Winter, University of Rochester Medical Center
Joanna C. Botti, Upstate Medical Center
References
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Alderfer MA, Fiese BH, Gold JI, Cutuli JJ, Holmbeck GN, Goldbeck L, et al. Evidence-based assessment in pediatric psychology: Family measures. Journal of Pediatric Psychology. 2008;33(9):1046–1061. doi: 10.1093/jpepsy/jsm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annett RD, Bender BG, Lapidus J, DuHamel TR, Lincoln A. Predicting children’s quality of life in an asthma clinical trial: What do children’s reports tell us? Journal of Pediatrics. 2001;139:854–861. doi: 10.1067/mpd.2001.119444. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bender BG, Rankin A, Tran ZV, Wamboldt FS. Brief-interval telephone surveys of medication adherence and asthma symptoms in the Childhood Asthma Management Program Continuation Study. Annals Allergy, Asthma, & Immunology. 2008;101:382–386. doi: 10.1016/S1081-1206(10)60314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender BG, Wamboldt FS, O’Connor SL, Rand C, Szefler S, Milgrom H, et al. Measurement of children’s asthma medication adherence by self-report, mother report, canister weight, and Doser CT. Annals of Allergy, Asthma, & Immunology. 2000;85:416–421. doi: 10.1016/s1081-1206(10)62557-4. [DOI] [PubMed] [Google Scholar]
- Bradley RH, Corwyn RF, McAdoo HP, Coll CG. The home environments of children in the United States Part I: Variations by age, ethnicity, and poverty status. Child Development. 2001;72:1844–1867. doi: 10.1111/1467-8624.t01-1-00382. [DOI] [PubMed] [Google Scholar]
- Brim SN, Rudd RA, Funk RH, Callahan DB. Asthma prevalence among US children in underrepresented minority populations: American Indian/Alaska Native, Chinese, Filipino, and Asian Indian. Pediatrics. 2008;122:e217–222. doi: 10.1542/peds.2007-3825. [DOI] [PubMed] [Google Scholar]
- Brunstrom JM, Mitchell GM. Effects of distraction on the development of satiety. British Journal of Nutrition. 2006;96:761–769. [PubMed] [Google Scholar]
- Chen E, Bloomberg GR, Fisher EB, Strunk RC. Predictors of repeat hospitalization in children with asthma: The role of psychosocial and socioenvironmental factors. Health Psychology. 2003;22:12–18. doi: 10.1037//0278-6133.22.1.12. [DOI] [PubMed] [Google Scholar]
- Cinotto S. “Everyone would be around the table”: American family mealtimes in historical perspective, 1850–1960. Family Mealtime as a Context of Development and Socialization. In: Larson RW, Wiley AR, Branscomb KR, editors. New Directions in Child and Adolescent Development. Vol. 111. New York: Wiley; 2006. pp. 17–34. [PubMed] [Google Scholar]
- Coon KA, Goldberg J, Rogers BL, Tucker KL. Relationships between use of television during meals and children’s food consumption patterns. Pediatrics. 2001;107:e7. doi: 10.1542/peds.107.1.e7. [DOI] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Winter MA, Cummings EM, Farrell D. Child adaptational development in contexts of interparental conflict over time. Child Development. 2006;77:218–233. doi: 10.1111/j.1467-8624.2006.00866.x. [DOI] [PubMed] [Google Scholar]
- Deitz WH, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985;75:281–286. [PubMed] [Google Scholar]
- Dickstein S. Family routines and rituals: The importance of family functioning. Journal of Family Psychology. 2002;16:441–444. [PubMed] [Google Scholar]
- Dickstein S, Hayden LC, Schiller M, Seifer R, San Antonio W. Adapted from the McMaster Clinical Rating Scale. East Providence, RI: E. P. Bradley Hospital; 1994. Providence Family Study mealtime family interaction coding system. [Google Scholar]
- Dickstein S, Seifer R, Hayden LC, Schiller M, Sameroff AJ, Keitner GI, et al. Levels of family assessment: II. Impact of maternal psychopathology on family functioning. Journal of Family Psychology. 1998;12:23–40. [Google Scholar]
- Eisenberg ME, Neumark-Sztainer D, Fulkerson JA, Story M. Family meals and substance use: Is there a long-term protective association? Journal of Adolescent Health. 2008;43(2):151–156. doi: 10.1016/j.jadohealth.2008.01.019. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos and poverty and children’s socioemotional adjustment. Psychological Science. 2005;16:560–565. doi: 10.1111/j.0956-7976.2005.01575.x. [DOI] [PubMed] [Google Scholar]
- Everhart RS, Fiese BH. Development and Initial Validation of a Pictorial Quality of Life Measure for Young Children with Asthma. Journal of Pediatric Psychology. 2009;34:966–976. doi: 10.1093/jpepsy/jsn145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith MS, Scanlon KS, Birch LL, Francis LS, Sherry B. Parent-child feeding strategies and their relationships to child eating and weight status. Obesity Research. 2004;12:1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Botti JC, Greenberg S. ABC Family Mealtime Coding Manual. University of Illinois; Urbana-Champaign: 2007. [Google Scholar]
- Fiese BH, Foley KP, Spagnola M. Routine and ritual elements in family mealtimes: Contexts for child wellbeing and family identity. New Directions for Child and Adolescent Development. 2006;111:67–90. doi: 10.1002/cd.156. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Schwartz M. Reclaiming the family table: Mealtimes and child health and wellbeing. Society for Research in Child Development Social Policy Report. 2008;XXII(IV) [Google Scholar]
- Fiese BH, Winter MA, Sliwinski M, Anbar RD. Nighttime Waking in Children with Asthma: An exploratory study of daily fluctuations in family climate. Journal of Family Psychology. 2007;21:95–103. doi: 10.1037/0893-3200.21.1.95. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Winter MA, Wamboldt FS, Wamboldt MZ, Anbar RD. Do family mealtime behaviors predict separation anxiety symptoms in children with persistent asthma? Journal of Child Psychology and Psychiatry. 2010;51:144–151. doi: 10.1111/j.1469-7610.2009.02138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores G, Tomany-Korman SC, Olson L. Does disadvantage start at home? Racial and ethnic disparities in health-related early childhood home routines and safety practices. Archives Pediatric and Adolescent Medicine. 2005;159:158–165. doi: 10.1001/archpedi.159.2.158. [DOI] [PubMed] [Google Scholar]
- Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-age children. Journal of the American Dietetic Association. 2007;107:53–61. doi: 10.1016/j.jada.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, Kim J, et al. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: The Six-C’s model. Child Development Perspectives (in press) [Google Scholar]
- Hersey JD, Jordan A. Reducing children’s TV time to reduce the risk of childhood overweight: The children’s media use report. (No. RTI Project Number 8680.006) Center for Disease Control and Prevention and the Association for Prevention Teaching and Research (ATPR); 2007. [Google Scholar]
- Hollingshead AB. A four-factor classification of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- Howe GW. Integrating family routines and rituals with other family research paradigms. Journal of Family Psychology. 2002;16:437–440. doi: 10.1037//0893-3200.16.4.437. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Anderson CB, Power TG, Micheli N, Jaramillo S, Nicklas TA. Measuring feeding in low-income African-American and Hispanic parents. Appetite. 2006;46(2):215–223. doi: 10.1016/j.appet.2006.01.002. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Power TG, Fisher JO, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44(1):83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- Hughes SO, Shewchuk RM, Baskin ML, Nicklas TA, Qu H. Indulgent feeding style and children’s weight status in preschool. Journal of Developmental and Behavioral Pediatrics. 2008;29:403–410. doi: 10.1097/DBP.0b013e318182a976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson AD, Martin A, Brooks-Gunn J, Petrill SA. Order in the House! Associations among household chaos, the home literacy environment, maternal reading ability and children’s early reading. Merrill-Palmer Quarterly-Journal of Developmental Psychology. 2008;54:445–472. doi: 10.1353/mpq.0.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Ferrie PJ, Griffith LE. Measuring quality of life in asthma. American Review of Respiratory Distress. 1993;147:832–838. doi: 10.1164/ajrccm/147.4.832. [DOI] [PubMed] [Google Scholar]
- Kaugers AS, Klinnert MD, Bender BG. Family influences on pediatric asthma. Journal of Pediatric Psychology. 2004;29:475–491. doi: 10.1093/jpepsy/jsh051. [DOI] [PubMed] [Google Scholar]
- McLoyd VC, Cauce AM, Takeuchi D, Wilson L. Marital processes and parental socialization in families of color: A decade review of research. Journal of Marriage and the Family. 2000;62:1070–1093. [Google Scholar]
- McLoyd VC, Toyokawa T, Kaplan R. Work demands, work family conflict, and child adjustment in African-American Families: The mediating role of family routines. Journal of Family Issues. 2008;29:1247–1267. [Google Scholar]
- McQuaid EL. Behavioral adjustment in children with asthma: A meta-analysis. Journal of Developmental and Behavioral Pediatrics. 2001;22:430–439. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- McQuaid EL, Walders N, Kopel SJ, Fritz GK, Klinnert MD. Pediatric asthma management in the family context: The family asthma management system scale. Journal of Pediatric Psychology. 2005;30:492–502. doi: 10.1093/jpepsy/jsi074. [DOI] [PubMed] [Google Scholar]
- Mitchell MJ, Powers SW, Byars KC, Dickstein S, Stark LJ. Family functioning in young children with cystic fibrosis: Observations of interactions at mealtime. Journal of Developmental and Behavioral Pediatrics. 2004;25:335–346. doi: 10.1097/00004703-200410000-00005. [DOI] [PubMed] [Google Scholar]
- Moore KA, Whitney C, Kinukawa A. Exploring the links between family strengths and adolescent outcomes. Child Trend Briefs 2009 [Google Scholar]
- NEPR-3. National Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. National Heart Lung and Blood Institute; 2007. [Google Scholar]
- Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents - Longitudinal findings from project EAT. Archives of Pediatrics & Adolescent Medicine. 2008;162(1):17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- Patrick H, Nicklas TA, Hughes SO, Morales M. The benefits of authoritative feeding style: caregiver feeding styles and children’s food consumption patterns. Appetite. 2005;44:243–249. doi: 10.1016/j.appet.2002.07.001. [DOI] [PubMed] [Google Scholar]
- Patton SR, Dolan LM, Powers SW. Differences in family mealtime interactions between young children with type 1 diabetes and controls: Implications for behavioral intervention. Journal of Pediatric Psychology. 2008;33:885–893. doi: 10.1093/jpepsy/jsn026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramey SL, Juliusson HK. Family dynamics at dinner: A natural context for revealing basic family processes. In: Lewis M, Feiring C, editors. Families, risk, and competence. Mahwah, New Jersey: LEA; 1998. pp. 31–52. [Google Scholar]
- Rapoff MA. Adherence to pediatric medical regimens. New York: Kluwer Academic; 1999. [Google Scholar]
- Rosier MJ, Bishop J, Nolan T, Robertson CF, Carlin JB, Phelan PD. Measurement of functional severity of asthma in children. American Journal of Respiratory and Critical Care Medicine. 1994;149:1434–1441. doi: 10.1164/ajrccm.149.6.8004295. [DOI] [PubMed] [Google Scholar]
- Speith LE, Stark LJ, Mitchell MJ, Schiller M, Cohen LL, Mulvihill M, et al. Observational assessment of family functioning at mealtime in preschool children with cystic fibrosis. Journal of Family Psychology. 2001;26:215–224. doi: 10.1093/jpepsy/26.4.215. [DOI] [PubMed] [Google Scholar]
- Stark LJ, Jelalian E, Powers SW, Mulvihill MM, Opipari LC, Bowen A, et al. Parent and child mealtime behavior in families of children with cystic fibrosis. Journal of Pediatrics. 2000;136:195–200. doi: 10.1016/s0022-3476(00)70101-6. [DOI] [PubMed] [Google Scholar]
- Videon TM, Manning CK. Influences on adolescent eating patterns: The importance of family meals. Journal of Adolescent Health. 2003;32:365–373. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]