Abstract
The demand for public health services is being outpaced by a shrinking public health workforce. This creates a unique opportunity for pharmacists to become more engaged in public health activities, particularly in rural underserved areas. To meet the need for additional public health professionals, we designed a master of public health (MPH) program in a rural state under the leadership of a department of pharmacy practice. In addition to a core set of courses, the MPH program has public health specialty tracks (disease state management, emergency management, health promotion practice, infectious disease management, food safety, gerontology, and medical management and administration) that could be completed as a certificate program or used towards an MPH degree. The program allows students to complete the graduate degree with a minimum of prerequisite coursework. The MPH degree provides an opportunity for pharmacists and other health care professionals to gain an understanding of the interprofessional approach to solving public health problems and will enhance their role in public health and within their health care team.
Keywords: outcomes, interprofessional, pharmacists, public health, rural health, graduate program
INTRODUCTION
The shortage of public health professionals in the United States will exceed a quarter of a million individuals within the next decade.1 The growing demand for public health services combined with a shrinking workforce has created a unique opportunity for pharmacists to become more engaged in public health activities on the local, state, and national levels. Pharmacists have long been recognized for their clinical expertise and have demonstrated their value in chronic disease state management (DSM), medication therapy management (MTM), and health education.2,3 Pharmacists provide patient care in a variety of practice settings in both urban and rural areas. In many cases, retail pharmacies are the primary point of health care access in rural communities.4-6 Pharmacists' clinical expertise, along with their broad and often critical access to patients, have placed them in a unique position to improve the public's health through health education, health promotion, and public health advocacy.
Many schools and colleges of pharmacy have incorporated public health topics into the doctor of pharmacy (PharmD) curriculum. In many cases, the content is incorporated into existing courses, although standalone courses on public health certainly exist. However, educators contend that this approach to public health pharmacy education is insufficient, and a more concerted effort must be made to explicitly and uniquely incorporate public health components into pharmacy curricula.7,8
In response to this call, the College of Pharmacy, Nursing, and Allied Sciences at North Dakota State University began development of a master of public health (MPH) program in 2008. Initially, a limited number of students, primarily pharmacy students, will enroll in the MPH program in 2011, followed by open enrollment across all disciplines in 2012. The rationale for building an MPH program (including an informal needs assessment) and identifying the institutional and political challenges encountered has been described.9 That paper described the program in its entirety, including the collaborative efforts among the university's departments and the school of medicine and health sciences located at another university in North Dakota. This manuscript will describe the MPH curriculum established at North Dakota State University and will serve as a case study illustrating how pharmacy educators can play a key role in providing graduate public health education for rural states.
North Dakota State University is a land-grant institution located in a geographically large, predominantly rural state. Fifty of North Dakota's 53 counties contain medically underserved areas, and a disproportionately large elderly population lives outside of its major metropolitan areas of Fargo, Grand Forks, Bismarck, and Minot.10-14 The prevalence of chronic conditions, particularly type 2 diabetes, is relatively high in North Dakota, especially in rural areas, and this trend is expected to increase in the future.14,15
Similar to most other rural areas in the United States, North Dakota continues to experience a shortage of medical (and nonmedical) public health providers. Consequently, rural public health providers typically assume duties outside of their primary training and often work collaboratively with other public health professionals who do not share their training, professional standards, and/or legal requirements. As a result, different disciplines must work cooperatively to provide health care.
The North Dakota Department of Health has stated openly its desire to proactively cross train health care personnel to fill multiple roles as dictated by the needs of its communities. The interprofessional nature and widespread acceptance of the MPH degree makes it a natural choice for educational programming in this context. However, of the 125 accredited MPH programs in the United States, the majority are located in the eastern United States, and none exist in the rural midwestern states of North Dakota, South Dakota, Montana, and Wyoming.16
The College of Pharmacy, Nursing, and Allied Sciences is a major academic unit of North Dakota State University. The mission of the college is to educate students, advance research, and provide professional services in pharmacy, nursing, and allied sciences. The college seeks to accomplish this mission with an interprofessional team approach to patient care, education, and research, as well as through developing health care professionals to meet the health care needs of the state, region, nation, and world. In 2008, the college initiated a strategic planning process. The department of pharmacy practice identified the development of an MPH graduate program as an interprofessional opportunity to advance the research and scholarship mission of the college and support the role of the pharmacist in rural and public health.
The department of pharmacy practice desired to lead the MPH program for a variety of reasons. The MPH degree is a graduate-level, health-related professional degree, drawing practitioners from the fields of pharmacy, nursing, medicine, and allied sciences, as well as other related disciplines. The college has extensive experience in providing effective management and administrative oversight for health-related degree programs that require an accreditation process and accreditation standards. Also, an MPH program under the direction of the pharmacy practice department supports and expands our role in educating PharmD students to “promote health improvement, wellness, and disease prevention in cooperation with patients, communities, at-risk populations, and other members of an interprofessional team of health care providers” as outlined in the Accreditation Council for Pharmacy Education (ACPE) Standard 12.17 The MPH degree program will require working collaboratively and cooperatively with the North Dakota state health officer, who provides regulatory oversight on a variety of public health issues. The department of pharmacy practice has established a close relationship with this individual, working in collaboration to develop the MPH program to fit the needs of a rural state. Also, adequate funding for the MPH degree program is crucial to ensure its financial viability. The department of pharmacy practice has negotiated an agreement with the State Board of Higher Education to levy a differential tuition that is higher than the standard graduate tuition at the university. A comparison of tuition and fee expenses with those of other accredited MPH programs suggests that the per-credit cost of North Dakota State University's MPH program is still comparable to (or less than) most other programs despite the differential tuition. Graduates who hold both a clinical (PharmD) and a public health practice (MPH) degree, and have acquired the skills therein, would be uniquely qualified to provide optimum health care services and be beneficial to the future of public health.18 Implementing the MPH program in stages is the university's intent, first with a small group of part-time students, and later expanding the program to include all other qualified applicants. To assess the demand for the MPH program among this initial target market, an informal survey of the university's first-year pharmacy students (N = 85) was conducted (further details are available upon request). Of the 67 respondents, approximately 30% indicated interest in pursuing a PharmD/MPH dual degree option. This finding is supported by a study in which a majority of pharmacy students found public health courses to be extremely appealing and believed that establishing a public health program provided an opportunity to make a difference and be engaged in the community.19
CURRICULUM DESIGNED TO ADDRESS SPECIFIC NEEDS
The needs of North Dakota dictated that public health educational programming exhibit several unique characteristics. It had to be practical and focus on disease state management, health disparities, emergency preparedness, and related activities of interest to public health practitioners and policymakers in North Dakota and other rural states. All students had to be educated in an interprofessional manner in a number of core competencies (including, but not limited to leadership, cultural diversity, communication and informatics, professionalism, and program planning) that are not typically covered in traditional public health graduate coursework. This training would ensure that public health personnel (who may initially be trained in a variety of fields, including medicine, pharmacy, nursing, management, human development, and sociology) can work together effectively to provide comprehensive team-based health care services and formulate and enact public health policies. Additionally, the educational programming had to be flexible enough to serve the needs of the variety of constituents working, or planning to work, in the field of public health. Some of these individuals have no formal public health training and might wish to complete an entire sequence of MPH coursework, while others might desire a shorter certificate program, with credits eventually applied towards the MPH degree. A third group might already hold an MPH degree, yet be interested in additional public health coursework focused on new professional content areas not covered in their original degree program. To meet these needs, a unique program was designed that contains specific tracks of specialization, each of which could be completed as a standalone certificate program. The MPH degree can be earned later in its entirety by completing the core coursework. The length of time it takes to earn the MPH degree must be reasonable and the courses easily accessible. The MPH degree requires completion of 42 semester credit hours (a standard for MPH program accreditation),20 and can be completed in approximately 2 years with minimal prerequisite work. The ultimate goal is to offer the entire program (certificate and MPH) onsite and via distance education, thereby making it accessible to residents across the state as well as to students in other states.
According to the Council on Education in Public Health (CEPH) guidelines, the goals and primary learning objectives of an MPH program center on preparing individuals to carry out broad public health functions in local, state, national, and international settings.20 To accomplish this, our MPH curriculum was based on the Association of Schools of Public Health (ASPH) Core Competency Model.21 This model incorporates CEPH competency requirements in 5 discipline-specific areas (biostatistics, epidemiology, environmental health science, health policy and management, and social and behavioral sciences) to constitute the core curriculum. The core curriculum is intended to give all students a strong set of fundamental skills that are necessary for careers in public health. Because it is required for all students, the core curriculum is interprofessional in nature with students from multiple disciplines interacting with and learning from one another.
In addition to the core curriculum, ASPH recommends 7 additional areas of crosscutting competencies: leadership, communication and informatics, diversity and culture, public health biology, professionalism, program planning, and systems thinking.21 These competencies do not comprise individual courses, rather they are included in existing courses throughout the curriculum so that all public health personnel (who may be trained in a variety of fields) can work together effectively to provide comprehensive, team-based, health care services and to formulate and enact public health policies. Thus, all of the crosscutting competencies are interprofessional in nature and are required attributes for public health practice, regardless of the area of specialization (Figure 1).21
Figure 1.
Association of Schools of Public Health1 Core Competency Model for the masters of public health degree. 1Used with permission from Association of Schools of Public Health.
A steering committee, consisting of representatives from a wide variety of disciplines across campus, worked collaboratively to design the MPH and certificate curriculum. Disciplines represented on the steering committee included pharmacy, nursing, statistics, microbiology, veterinary science, emergency management, sociology, food safety, and health, nutrition, and exercise science. The resulting coursework capitalizes on the strengths of multiple departments and programs within the university.
SPECIFICS OF THE CURRICULUM
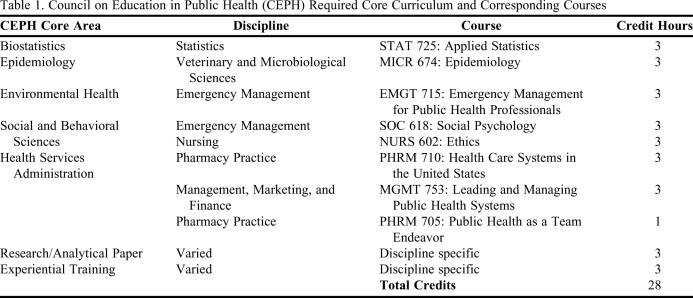
The specific core courses identified by the MPH steering committee were chosen intentionally to address the practical needs of public health practitioners and are taught by faculty members in an array of disciplines (Table 1). An additional consideration in choosing the specific core courses was a department's demonstrated willingness (through current and past faculty allocations and course offerings) to commit resources to offer the course(s) on a regular basis, or at the request of the MPH program director. As a result, pharmacy students would receive a strong set of core skills that are necessary not only for careers in public health, and are delivered in an appropriate interprofessional fashion.
Table 1.
Council on Education in Public Health (CEPH) Required Core Curriculum and Corresponding Courses
To satisfy both CEPH and the university's graduate school guidelines, students would have to complete a research/analytical paper (3 credits) related to public health as well as a public health-based experiential work requirement (ie, a practicum, internship, or residency) for 3 credits. Most theses in public health revolve around creating needs assessments, searching for funding sources, and program planning, while the experiential training focuses on implementing such projects. The MPH director is responsible for working with students to set up research paper committees and to assist students who cannot find experiential assignments on their own.
The Council on Education for Public Health allows for prior professional degrees to offset a limited number of credits in the MPH degree curriculum which is consistent with our degree program in that we allow PharmD students (and others) to count up to 9 credit hours (twice) towards both programs. Thus, 1 or more APPEs conceivably could count towards both the PharmD and the MPH degree provided the APPEs are in a public health setting.
Students also would have to complete a minimum of 15 credits of course work in an area of specialization. Students who did not wish to obtain a degree, or who already had a degree in public health, but wished to add to their credentials, could pursue 1 of these tracks as a certificate program. A student wishing to pursue a track would have to be approved by faculty members in that discipline, to ensure the student has an adequate background and is capable of successful work. The MPH director then would assign the student to an advisor from that discipline to assist in choosing appropriate course work. In addition, advisors would mentor students as they completed their research paper and experiential work and grade their work/progress. The program has 7 available specialization tracks, including pharmaceutical disease state management.
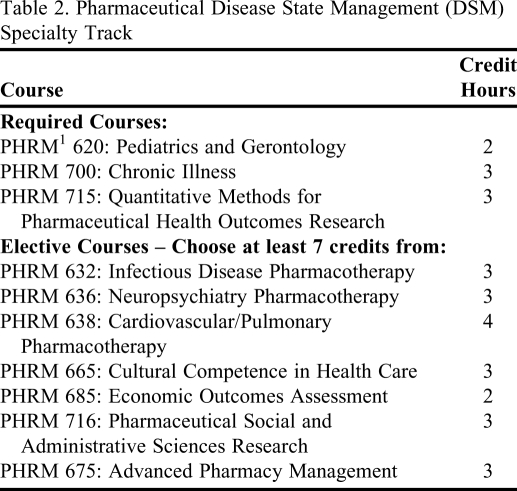
The courses available for the pharmaceutical disease state management track are listed in Table 2. Several criteria guided the selection of these courses. First, they cover a wide range of chronic conditions which use pharmaceutical care extensively. Second, to encourage pharmacy students to enroll in the program (whether to complete the MPH degree program in its entirety or a certificate program), the courses were chosen to give students the ability to count up to 9 credits towards both their PharmD and MPH degrees, as allowed by the university's graduate school. CEPH also allows for prior professional-degreed courses to offset some of the credits in the MPH curriculum. Finally, to enhance the research competencies of pharmacy students, several new courses in social and behavioral pharmacy methods and outcomes research were developed (Table 2). Consequently, students would gain significant exposure to interprofessional public health principles in the core courses and develop their DSM and research abilities in the disease state management track.
Table 2.
Pharmaceutical Disease State Management (DSM) Specialty Track
1PHRM denotes courses offered by the Pharmacy Practice Department. Any course labeled 600 and higher signifies a graduate level course.
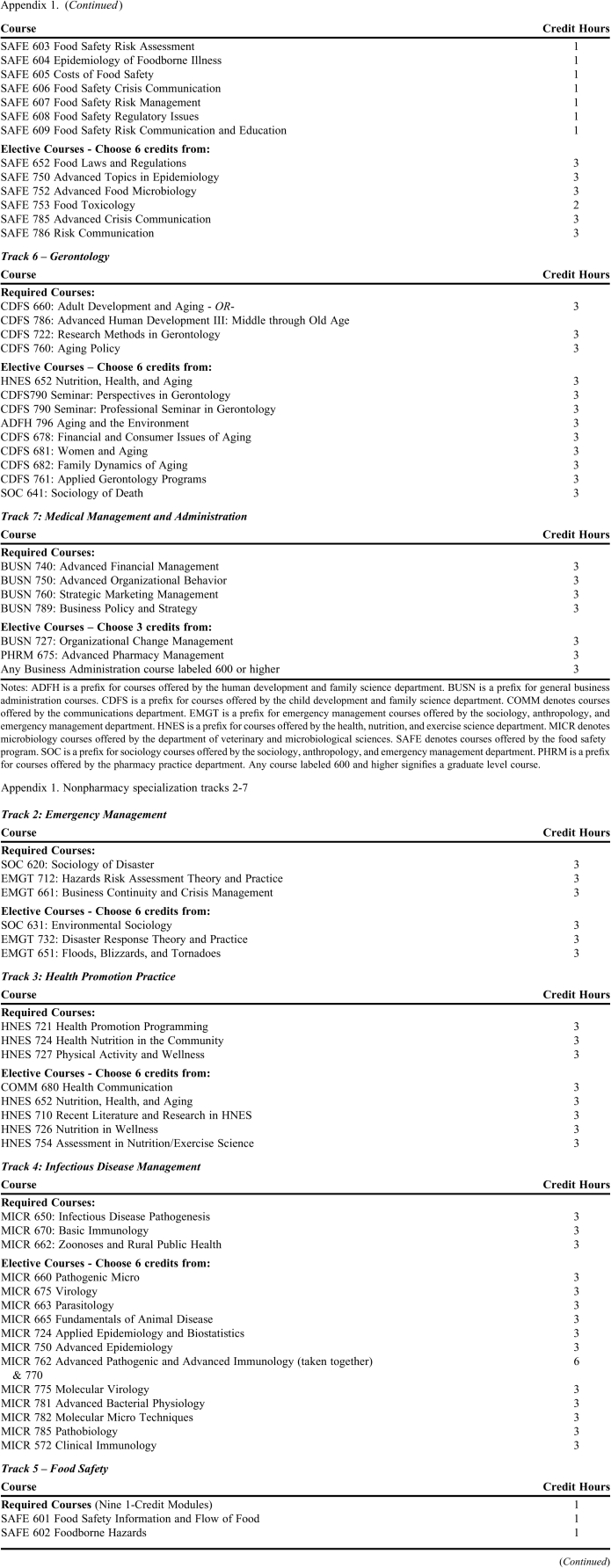
Other specialization tracks included emergency management, health promotion practice, infectious disease management, food safety, gerontology, and medical management and administration. All of the tracks share a similar format with 8 or 9 required credits, plus 6 or 7 elective credits within the specialization. The full set of courses for each of these tracks is shown in Appendix 1. PharmD students (and pharmacists) would be eligible to choose a nonpharmacy specialty track after meeting a minimum number of prerequisites, if any. As an example, pharmacy students pursuing the medical management and administration track (Appendix 1) would be required to complete additional, advanced undergraduate coursework in finance, marketing accounting, and management (consistent with what would be expected for admission into a typical master of business administration program) prior to completing this track. The steering committee decided to limit the initial program to a relatively small number of tracks to simplify the initial approval process through the university.
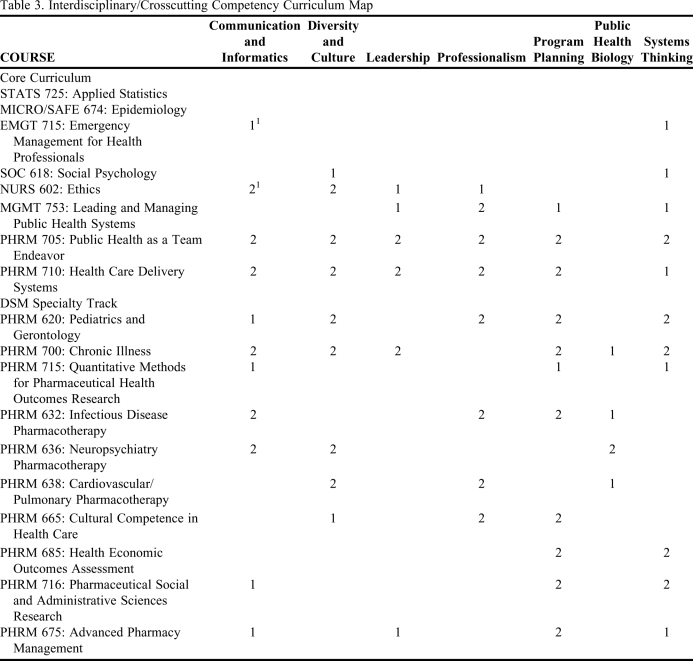
All courses within the core and specialty tracks were mapped to CEPH competency requirements and the ASPH interprofessional crosscutting competencies. An abbreviated curriculum map depicting the crosscutting competencies mapped to the core curriculum and the DSM track is outlined in Table 3. Other specialization tracks have similar mappings which were approved by the MPH steering committee and are available from the author. Consistent with university policies, instruction in all MPH courses will be assessed formatively and summatively using standard university course and instructor evaluation forms. As mentioned previously, the MPH program will seek CEPH accreditation. To prepare for the accreditation visit, an assessment plan will be developed to ensure that students meet expected student outcomes, and that the program is tied to curricular and program assessment criteria. Both formative and summative evaluation techniques and internal (student, faculty members) and external (employer, alumni surveys) criteria will be used. A benefit to seeking accreditation for this MPH program is the past experience of the department of pharmacy practice in obtaining successful accreditation for the PharmD program. Typically, the time from initial application to CEPH and the accreditation decision is 3 years, so our goal is to attain accreditation status by fall 2015.20
Table 3.
Interdisciplinary/Crosscutting Competency Curriculum Map
1 = Major focus in course; 2 = Minor focus in course
SUGGESTIONS FOR OTHER PROGRAMS
The program outlined in this manuscript offers several suggestions for colleges of pharmacy expanding the depth and breadth of their public health curricula. Resources in a university setting are scarce even in the best of economic times. Similarly, if an institution does not have a standalone public health program, the interprofessional nature of public health may lead to academic “turf wars” over who oversees the program. The MPH program outlined in this manuscript may be useful in addressing both of these challenges. By sharing responsibility for the core coursework and the tracks, it is possible to provide a rigorous, but expansive public health curriculum of interest to a variety of student backgrounds. Moreover, because many departments across a college campus typically offer a small handful of public health courses, many of the resources necessary to implement a program of this nature are already in place. What remains is to organize them into a consistent and coherent framework. While this program is administered through the college's pharmacy practice department, there is no particular reason why another participating department could not provide administrative coordination instead. Other pharmacy programs may find it expedient to cede the administrative responsibilities to other departments (perhaps those in an independent school, college, or department of public health), and simply offer a track in pharmaceutical disease state management.
This case study also offers several cautionary suggestions to institutions seeking to implement similar public health education initiatives. A program such as that described here cannot exist without being accredited by CEPH or an equivalent agency. Accreditation is the leverage the program director has to ensure that courses are offered on a timely basis, and that the program receives the resources it needs to function appropriately. With the number of participating departments involved, it is inevitable that the accreditation leverage will need to be applied. At the same time, it is important to recognize that building a program worthy of CEPH accreditation is a costly, time-consuming process. As identified in the CEPH accreditation manual, the process takes several years, and the fees and implementation costs can exceed several hundred thousand dollars, especially if 1 or more new permanent faculty lines are necessary to offer key program coursework.22 Our program proposal includes several additional faculty lines, and has a proposed budget of approximately $1.2 million, much of which will be financed through differential tuition. To reduce the immediate impact of the program on the university budget, new faculty lines will be assigned based on the expected contribution of an academic unit to the MPH program (ie, programs that are expected to develop new core courses would receive priority in new faculty line allocation compared to other contributing academic units) and will be phased in gradually over the first few years of the program's existence. For programs that do not require new faculty lines (and/or that cannot generate revenue streams via program fees), program costs may (out of necessity) be a fraction of this amount. Another caution is to identify carefully and limit the number of specialization tracks, especially as the program itself negotiates the approval process. This is important for 2 reasons. In most higher education institutions, each of the courses, whether new or existing, receives scrutiny during the approval process. Each track added to the proposal disproportionately increases that scrutiny. Also, initiating such a program requires a high degree of collaboration and participation across departments sponsoring the tracks and the core coursework. Every department must have a detailed understanding of its role in the program, and the commitment (financial, personnel, or otherwise) required for that role. The program and its students will be impacted adversely, for instance, if a department reneges on its commitment to offer a core course, a track course, or both. The content of each of the tracks should be chosen wisely. Due to different prerequisites, the subject matter in some tracks and/or ease of completion may be more popular with some students than others. Tracks must be chosen in accordance with both current and available resources, as well as the potential size of the student population seeking the training, and the needs of the communities being served by MPH graduates. Efforts must be taken so that student enrollment in a given track does not overburden the departments sponsoring those tracks. The same is true for the faculty members advising student papers and/or experiential work. While some institutions might use student enrollments as a criteria in allocating resources and allocating new faculty lines, this is not universally true. In those cases, other means must be used to ensure that the program's faculty members are not overburdened.
SUMMARY
The rural land-grant mission of North Dakota State University College of Pharmacy, Nursing, and Allied Sciences makes it uniquely qualified to offer rural health care educational programming. No other MPH degree programs are offered and taught specifically by faculty members from North Dakota institutions of higher education. The MPH degree described in this manuscript allows practitioners to advance in their careers and take a leadership role to advance the public's health. The MPH is a graduate-level professional degree providing students with skills that are both technical and interprofessional in nature. Thus, students will increase the depth and breadth of their knowledge base, which will increase their employment opportunities and allow them to move into new areas of practice. As the name suggests, the MPH degree provides students with the skills to improve the health of the public, which is a fundamental contribution to the community.
ACKNOWLEDGMENTS
We thank members of the MPH planning committee who devoted time and effort in developing the proposal and curriculum. We thank Howard Anderson, Jr. and Charles Peterson for their valuable comments which improved this manuscript.
Appendix 1. Nonpharmacy specialization tracks 2-7
REFERENCES
- 1. Confronting the Public Health Workforce Crisis. Association of Schools of Public Health Policy Brief; 2008. http://www.asph.org/UserFiles/WorkforceShortage2010Final.pdf. Accessed September 22, 2010.
- 2.Cranor CW, Bunting BA, Christensen DB. The Asheville project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc. 2003;43(2):173–184. doi: 10.1331/108658003321480713. [DOI] [PubMed] [Google Scholar]
- 3.Crawford SY. Pharmacists' roles in health promotion and disease prevention. Am J Pharm Educ. 2005;69(4) Article 73. [Google Scholar]
- 4.Friesner D, Scott DM. Exploring the formation of patient satisfaction in rural community telepharmacies. J Am Pharm Assoc. 2009;49(4):48–57. doi: 10.1331/JAPhA.2009.08110. [DOI] [PubMed] [Google Scholar]
- 5.Traynor AP, Sorensen TD, Larson T. The main street pharmacy: becoming an endangered species. Rural MN J. 2007;2(1):83–100. [Google Scholar]
- 6.Whitten P, Love B. Patient and provider satisfaction with the use of telemedicine: overview and rationale for cautious enthusiasm. J Post Grad Med. 2005;51(4):294–300. [PubMed] [Google Scholar]
- 7.Fincham JE. Global public health and the academy. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700114. Article 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fincham JE. Public health, pharmacy, and the prevention education center. Am J Pharm Educ. 2007;71(5) doi: 10.5688/aj7105104. Article 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friesner DL, Miller D, Scott DM, Naughton CA, Albano CB. Rural public health education as a pharmacist-led team endeavor. J Am Pharm Assoc. 2010;50(2):207–213. doi: 10.1331/JAPhA.2010.09175. [DOI] [PubMed] [Google Scholar]
- 10. Center for Rural Health. Rural Health Facts. 2006. www.ruralhealth.und.edu. Accessed November 11, 2010.
- 11. US Census Bureau. North Dakota Percent of Population Age 65 and Older, 2000. www.census.gov. Assessed November 11, 2010.
- 12. Center for Rural Health. North Dakota Medically Underserved Areas/Populations, 2008. http://www.ruralhealth.und.edu. Accessed November 11, 2010.
- 13. Rathge R. The Economic Impact of the Senior Population on a State's Economy: The Case of North Dakota, 2007. http://www.ndsu.nodak.edu/sdc/publications/reports/2007EconImpactSeniorPop.pdf. Accessed September 22, 2010.
- 14. North Dakota Health Care Review, Inc. North Dakota Diabetes Surveillance Report, 2000. www.health.state.nd.us. Accessed November 11, 2010.
- 15. Centers for Disease Control. County Level Estimates of Diagnosed Diabetes – Percentage of Adults in North Dakota by Natural Breaks. 2005. http://www.cdc.gov. Accessed November 11, 2010.
- 16. CEPH. Schools of public health and public health programs accredited by the council on education for public health. http://www.ceph.org/pdf/Master_List.pdf. Accessed November 29, 2010.
- 17. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, 2006. http://www.acpe-accredit.org/standards/default.asp. Accessed November 11, 2010.
- 18.Crismon ML, Albright FS, Canney DJ, et al. The role of dual-degree programs in colleges and schools of pharmacy: the report of the 2008-2009 Research and Graduate Affairs Committee. Am J Pharm Educ. 2009;73(8) doi: 10.5688/aj7308s06. Article S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah B, Rahim H, Yin H, Bhavsar J. Pharmacy students' attitudes toward a required public health course and developing a public health program. Am J Pharm Educ. 2009;73(7):134. doi: 10.5688/aj7307134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. CEPH. Accreditation Criteria: Schools of Public Health. 2005. http://www.ceph.org/pg_accreditation_criteria.htm. Accessed November 29, 2010.
- 21.Calhoun JG, Ramiah K, Weist EM, Shortell SM. Development of a core competency model for the master of public health degree. Am J Public Health. 2008;98(9):1598–1607. doi: 10.2105/AJPH.2007.117978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Society of Health-System Pharmacists. ASHP statement on the role of health-system pharmacists in public health. Am J Health-Syst Pharm. 2008;65(5):462–467. doi: 10.2146/ajhp070399. [DOI] [PubMed] [Google Scholar]