Abstract
Objective
To examine the self-administered Clinical Cultural Competency Questionnaire (CCCQ) and assess the perceived level of cultural competence of students in Xavier University of Louisiana College of Pharmacy to guide curriculum development within the 4-year academic program.
Methods
The CCCQ was administrated to each class of pharmacy students during spring 2009. Exploratory factor analysis with principal components and varimax rotation was conducted to build the constructs explaining the factors measuring students' self-assessment of cultural competence.
Results
Nine factors, including 46 items extracted from the CCCQ and explaining 79% of the total variance, were found as the best fit to measure students' self-assessment of cultural competence.
Conclusions
The CCCQ was found to be a practical, valid, and reliable self-assessment instrument to measure the perceived level of pharmacy students' knowledge, skills, attitudes, and encounters in cross-cultural environments. The questionnaire allowed the identification of students' needs for training in cultural competence and the development of a curriculum tailored to satisfy those needs.
Keywords: cultural competence, curriculum, self-assessment, survey, minority students
INTRODUCTION
Cultural competence has emerged as an important strategy to respond to the multicultural, multiracial, and multilingual needs of a growing diverse population in the United States, and to reduce disparities in health and health care.1 Although policies are in place that mandate culturally and linguistically competent health care, and several national organizations and accreditation bodies require the inclusion of training in cultural competence in continuing education and academic programs,2 several studies show that health professionals still are not prepared to interact adequately with the diverse cultures in our nation's patient populations.3 The Accreditation Council for Pharmacy Education's (ACPE's) revised standards includes Guideline 9.1: “The college or school must ensure that the curriculum addresses patient safety, cultural competence, health literacy, health care disparities, and competencies needed to work as a member of or on an interprofessional team.”4
To satisfy this academic standard at Xavier University of Louisiana College of Pharmacy, a reliable and practical instrument was needed for students to use to self-assess their perceived cultural competencies. The instrument would be used: (1) to evaluate students' needs for training in cultural competence; (2) as a baseline measure with which to compare perceived change over time in the competencies developed during the academic program; and (3) as a tool to compare students' perceptions of their level of cultural competency (self-assessment) with their performance in the real world (peer, patient, staff, and teachers' feedback, and evaluations). Also, data collected from students over time would be useful to examine differences in perceptions over the entire academic program, such as different classes in the same academic year or the same cohort over the complete curriculum, and as feedback for curriculum development and improvement.5
Cultural competence assessment falls into 4 categories: evaluation of the cultural competencies of the individual; evaluation of the implementation of cultural competence in the organization; evaluation of the delivery of culturally competent services and programs; and evaluation of curriculum, education, and training programs in cultural competence. In a review of the status of assessment of cultural competence, South-Paul and Like concluded that the lack of a standard definition and reliable indicators of cultural competence impede the ability to measure the impact of culturally competent provider behaviors on the outcomes of care.6 From a meta analysis of the medical education literature, much variance was found in the way researchers assess cross-cultural education, and a mixed-methods approach was recommended for evaluation and assessments, including self-assessment of perceived level of competencies, and the assessment of performance.2 Mixed methods would include pre- post-tests, role playing, portfolios, standardized patients, pharmacy practice experiences, objective structured clinical examinations, and patients' evaluations. A self-assessment strategy applied systematically and sequentially throughout the pharmacy curriculum would provide opportunities for students to monitor their own progress and give faculty members insight on students' strengths and weaknesses.7 This self-assessment could be used as an important source of data for a comprehensive assessment of the academic program.8
An extensive number of instruments have been developed for self-assessment of cultural competence in health professions;9 some of them are validated and widely used measures of cultural competence, and others are used in cultural competence training.10 A review of the most widely used measures revealed important limitations to their application in this study including: restriction to a specific specialty or profession; inherent restrictions and biases11; abbreviated length that would not provide enough information for curriculum development; extensive length prohibiting ease of application in an academic environment; and environmental adaptability problems. These results emphasized the need to define a valid self-administrated measure, that is applicable to all health professionals and that can be used to evaluate training or assess perceived level of cultural competence.12
None of the tools found in the literature review were developed specifically for pharmacy students; therefore, it was necessary to identify the most relevant tools and perform a validation process to measure the reliability and consistency of the constructs. The objective of this study was to examine one of the selected tools, the self-administered Clinical Cultural Competency Questionnaire (CCCQ), as the standard measure to be used in Xavier University of Louisiana, College of Pharmacy, to assess the students' perceived level of cultural competence and to guide curriculum development within the 4-year academic program.
METHODS
From the literature review, we identified 2 tools that were relevant to our needs, so permission was requested and granted to use and adapt them. The first, the CCCQ, is a 63-item measure developed to assess physicians' provision of culturally competent health care to diverse patient populations.13 Responses to the questionnaire can be used as a needs assessment to assist in planning cultural diversity educational interventions. The Migrant-friendly Hospitals project14 translated the CCCQ into 6 languages and used it to measure the effectiveness of training in cultural competence in 9 hospitals in Europe, with reliability coefficients reported as higher than 0.8.15
The second tool, the California Brief Multicultural Competency Scale (CBMCS), is a 21-item scale measuring self-reported multicultural competence in mental health services providers.16 This scale was developed as a single brief instrument combining 4 of the more predominant measures of multicultural counseling competence: the Cross-Cultural Counseling Inventory-Revised (CCCI-R); the Multicultural Counseling Awareness Scale: Form B (MCAS: B); the Multicultural Awareness Knowledge Skills Scale (MAKSS); and the Multicultural Competency and Training Survey (MCCTS). The CBMCS was validated using the Multicultural Counseling Inventory (MCI) and was found to be a reliable instrument (coefficient alpha for the subscales ranged from 0.75 to 0.90) with a strong theoretical foundation.
Although the 2 questionnaires were considered suitable to our needs, neither had been validated with pharmacy students. Additionally, the CCCQ was too long to apply in an educational setting, and the CBMCS was too short to evaluate training needs. We combined both questionnaires in a new self-assessment tool to administer to our sample population of students. Data collected was used to validate the questionnaires and to select the more representative items using statistical analysis. The expected result was to have a shorter, combined and validated measure that could be applied at baseline and follow-up assessments over the 4-years of the pharmacy program. Items were included in the same order of the original measures, and organized into 2 parts. The first part included the 63 items defined in the 4 domains in the CCCQ (knowledge with 16 items; skills with 15 items; attitudes with 20 items; and encounters with 12 items). The second part included the 21-items defined in the CBMSC, which were edited to eliminate the restricted application to mental health providers.
During the review of the CCCQ, no modifications were made to the items; however, a new item was created in the skills domain: S16 “dealing with cross-cultural conflicts relating to the informed consent.” The practice of obtaining informed consent in a culturally sensitive manner is difficult because of the regulations, laws, and ethical codes involved when administering medical treatment or conducting research.17 Many conflicts result from cultural differences regarding respect, autonomy, and privacy issues involved in informed consent, and family involvement in the selection of treatment and final decision-making.
After obtaining institutional review board approval, the combined instrument was completed by all pharmacy students enrolled during the 2009 spring semester. Completion of the instrument was considered to be implicit consent for participation. Four hundred sixty-seven of 493 pharmacy students completed the assessment (response rate of 94.7%). Of these students, 32.3% were in the first year of the program; 31.5% were in the second year; 15% were in the third year; and 21.2% were in the fourth (final) year. Students self-identified their race/ethnicity as follows: 48% African American, 30% Asian American, 17% White, and 5% Other (eg, Hispanic/Latino, biracial, multiracial, unknown). Forty-three percent (201) of the respondents spoke a language other than English, with Vietnamese being the most common language (125), followed by Spanish (20), and French (12). Most of the respondents (85.9%) reported having received training in cultural competence during the academic program, at conferences, or through personal readings. Results from individual respondents were kept confidential, and only aggregate summaries were used for reporting results. Although we initially considered the length of the combined tool to be an issue for its application, the importance of completing the assessment was explained to the students, and they were willing to participate. Respondents rated the average time to fill out the survey instrument (21 minutes) as a “moderate” amount; the high response rate confirmed this result.
Exploratory factor analysis with principal components and varimax rotation was used to aggregate the different items supporting the construct of the 4 domains measuring students' cultural competence (knowledge, skills, attitudes, and encounters). Factor analysis is one of the most used techniques of data reduction in social science.18 It is commonly used to discover predominant patterns or underlying relationships (factors) among a large number of variables/items when there is no prior theory about the factor structure of the data, such as in the case of the CCCQ, and to delete items that do not exhibit a large-enough relationship with other items. The method consists of the extraction of factors with eigenvalues over 1.0 to aggregate the different items according to their factor loadings (structure coefficients); this is according to how much weight is assigned to the factor.19 An eigenvalue is the amount of variance accounted for in each factor, which can be expressed as a percent of the total variance. During the process, the factors are identified by looking at the covariance or correlation among the observed variables and then determining how much of the variance is explained by those common factors. To simplify interpreting the factors obtained in the original results, the covariance matrix is rotated; varimax rotation is most frequently used for this.
The appropriateness of using factor analysis was evaluated through 2 tests20: (1) the Bartlett Test statistic for sphericity, which tests the hypothesis that the correlation matrix is an identity matrix (if the test statistic is large and the associated significance level is small, it is appropriate to use factor analysis), and (2) the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy, which is an index to compare the observed correlation coefficients to the partial correlation coefficients (KMO below 0.5 is unacceptable for factor analysis19).
Following the methodology, the criteria to define the validity of the resulting constructs was determined by: (1) computing the total variance explained; (2) extracting the minimum eigenvalue > 1; (3) eliminating items that did not produce a high structure coefficient (loads ≥ 0.55), that is, failed to load significantly on any factor (convergent validity); (4) eliminating items that showed high cross loading (> 0.35), that is, loaded significantly on more than 1 factor (discriminant validity); and (5) eliminating items with low extraction communality (h2 < 0.50). Additionally, Cronbach's alpha coefficients were calculated to measure internal consistency of the constructs. During the reliability analysis, the following also were verified: (1) whether the corrected item-total correlation (item discrimination) was > 0.20; (2) whether the elimination of an item caused the alpha to increase; (3) whether a reduced range of responses was observed in an item; and, (4) whether item means were extreme. SPSS, version 11.0.1 (SPSS Inc, Chicago, IL) was used to carry out the data analyses.
RESULTS
The results obtained in the application of the CCCQ are reported below. Results about the application of the CBMCS and the profile of Xavier College of Pharmacy students in cultural competence will be reported separately.
Final exploratory factor analysis procedure resulted in the selection of 9 factors explaining 78.7% of the variance and grouping 46 of the 64 items included in the CCCQ. The number of factors was determined by extracting the minimum eigenvalues > 1. According to the criteria defined, 18 items were eliminated either because they did not have a high structure coefficient (≥ 0.55) or because they showed cross-loadings with other factors (≥ 0.35). All extracted items had extraction communality of h2 > 0.5 and corrected item-total correlation > 0.20. No items were eliminated during the reliability analysis because they caused the alpha to increase, had a reduced range of responses, or showed extreme means.
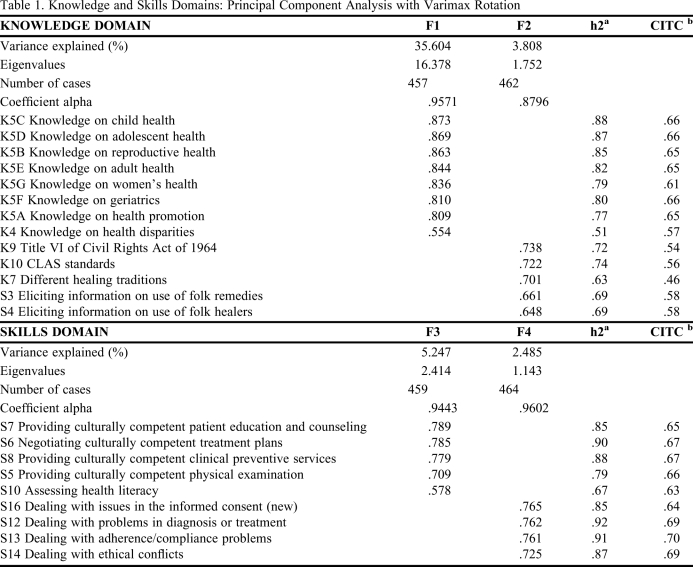
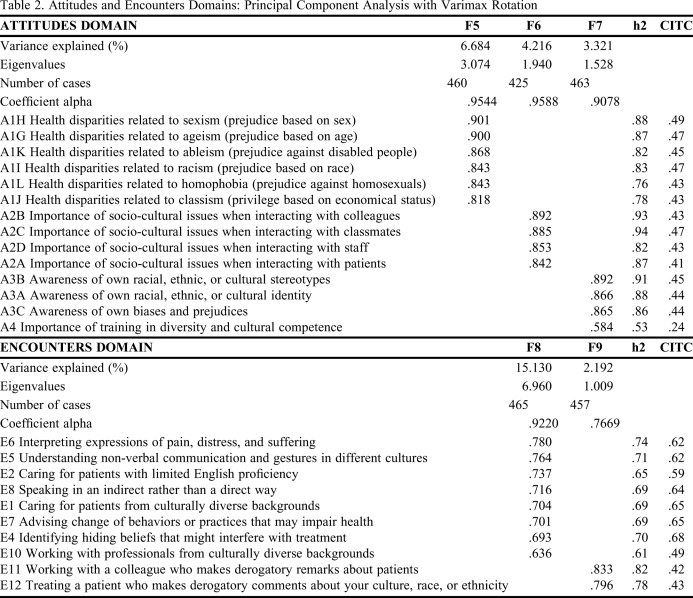
Tables 1and 2 summarize the factors found as the best fit to explain the 4 domains measuring cultural competence: knowledge, skills, attitudes, and encounters. Items are presented according to the domain and factor to which they belong and in descending order of their factor loadings within each factor. Because factors are generated based only on the coefficient loadings, the interpretation of their meanings and the names assigned are based on the variables included and the variance explained. Following is the analysis of the factors explaining each of the domains.
Table 1.
Knowledge and Skills Domains: Principal Component Analysis with Varimax Rotation
Abbreviations: h2 = communality extraction; CITC = corrected item-total correlation; F1 = Addressing Population Health Issues; F2 = Understanding the Context of Care; F3 = Providing Culturally Responsive and Effective Services; F4 = Managing Cross-Cultural Clinical Challenges.
Table 2.
Attitudes and Encounters Domains: Principal Component Analysis with Varimax Rotation
Abbreviations: h2 = communality extraction; CITC = corrected item-total correlation; F5 = Recognizing Disparities-Related Discrimination; F6 = Improving Interpersonal and Intercultural Interactions; F7 = Engaging in Self-Reflection; F8 = Increasing Comfort During Cross-Cultural Clinical Encounters; F9 = Coping With Aggressiveness and Bias
Knowledge Domain
The Knowledge domain measures students' self-assessment of their knowledge about different issues related to cultural competence. The following 2 factors included 11 of the 16 items in the CCCQ and explained 39.4% of the total variance.
Addressing Population Health Issues (F1).
Factor 1, Addressing Population Health Issues, groups 8 items related to knowledge of sociocultural issues in diverse populations, such as age and gender, health disparities experienced by diverse racial and ethnic groups, and health promotion. This factor is interpreted as the need to learn about developmental changes across one's lifespan; the influence of life cycles on physical characteristics, behaviors, attitudes, and health risks in different populations; and the changes in health promotion strategies and health disparities over the lifespan. Developmental factors across the lifespan influence the way people communicate and form relationships with others.23
Understanding the Context of Care (F2).
The second factor, Understanding the Context of Care, groups 3 items related to knowledge of regulations, standards, and healing traditions (K7, K9, and K10) and 2 items from the Skills domain (S3 and S4), both related to eliciting patients' information about use of folk remedies, folk healers, and other alternative modalities. The Title VI of the Civil Rights Act of 1964 prohibits discrimination based on race, color, and national origin, and the Office of Minority Health's National Standards for Culturally and Linguistically Appropriate Services call for the provision of health care compatible with cultural health beliefs, practices, and preferred language.21
Skills Domain
The Skills domain measures students' self-assessment of their skills in dealing with socio-cultural issues in patient care. The following 2 factors included 9 of the 16 items in the CCCQ and explained 7.7% of the total variance:
Providing Culturally Responsive and Effective Services (F3).
The third factor, Providing Culturally Responsive and Effective Services, groups 5 items related to providing culturally-sensitive services along the continuum of health: eliciting prevention, education, and counseling; assessing health literacy; performing physical examinations and diagnosis; and prescribing and negotiating treatment plans. Culturally sensitive services are services that consider the person as a whole, including the sociopolitical and cross-cultural issues, and are tailored to an increasingly diverse racial, linguistic, and cultural population. Included are interpreter services as well as language and culturally appropriate health educational materials.
Managing Cross-Cultural Clinical Challenges (F4).
Factor 4, Managing Cross-Cultural Clinical Challenges, groups 4 items related to professional challenges in multicultural encounters, specifically when dealing with conflicts related to the explanation and signature of informed consent; understanding diagnosis and treatment; adherence and compliance; and professional ethics. This factor is interpreted as the skills to handle conflict and build consent during patient-provider encounters.
Attitudes Domain
The Attitudes domain measures students' awareness of their own culture, biases, and prejudices, and the importance given to health disparities, and to receiving training in cultural competence. The following 3 factors included 14 of the 20 items in the CCCQ and explained 14.2% of the total variance:
Recognizing Disparities-Related Discrimination (F5).
The fifth factor, Recognizing Disparities-Related Discrimination, groups 6 items related to the importance given to different forms of discrimination and prejudice that contribute to health disparities: ageism, sexism, racism, classism, ableism, and homophobia. Several studies have raised awareness of provider bias and discrimination in medical decision-making.22
Improving Interpersonal and Intercultural Interactions (F6).
Factor 6, Improving Interpersonal and Intercultural Interactions, groups 4 items related to the importance of sociocultural issues in interactions with patients, colleagues, residents/students, and staff members.
Engaging in Self-Reflection (F7).
Included in factor 7, Engaging in Self-Reflection, are 4 items related to identity self-awareness, stereotypes, biases, and prejudices, and to the importance given to training in cultural diversity and multicultural health care. This factor incorporates the need for health care providers to identify, reflect upon, understand, and control or eliminate their biases and prejudices, specially those identified in the Recognizing Disparities-Related Discrimination factor (F5).
Encounters Domain
The Encounters domain measures students' degree of comfort in dealing with different cross-cultural situations. The following 2 factors included 10 of the 12 items in the CCCQ and explained 17.3% of the total variance:
Increasing Comfort During Cross-Cultural Clinical Encounters (F8).
Included in factor 8, Increasing Comfort During Cross-Cultural Clinical Encounters, are 8 items related to comfort with different cross-cultural communications issues during the patient encounter. This factor can be interpreted as the abilities students should have to break out of their comfort zone, understand how communication can break down, establish rapport, and adjust the communication to a comfortable level for everyone involved. Rapport means a mutually and comfortable relationship based on trust and safety.23
Coping With Aggressiveness and Bias (F9).
Under factor 9, Coping With Aggressiveness and Bias, are 2 items related to working with colleagues or patients who make derogatory remarks about specific population groups, including one's own. These behaviors from colleagues or patients hurt people's feelings and challenge the multicultural encounters. Aggressiveness is an ineffective communication, used intentionally or unintentionally to humiliate, blame and embarrass others.
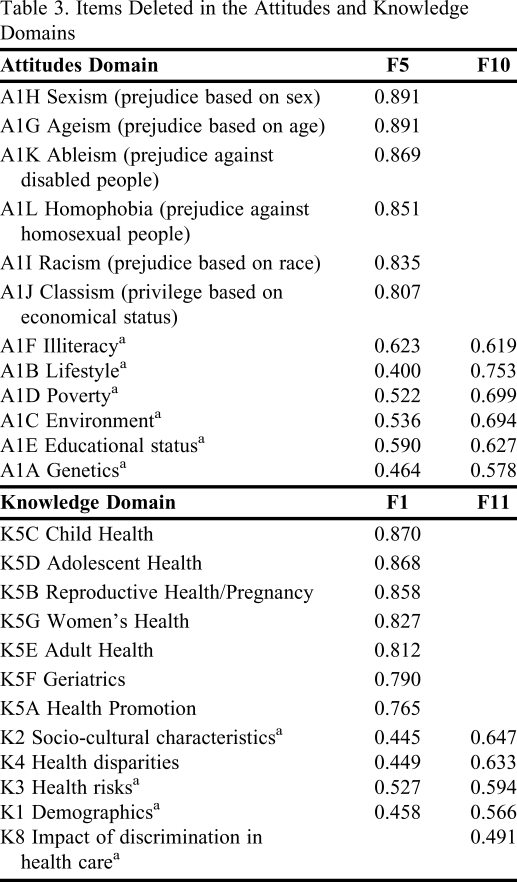
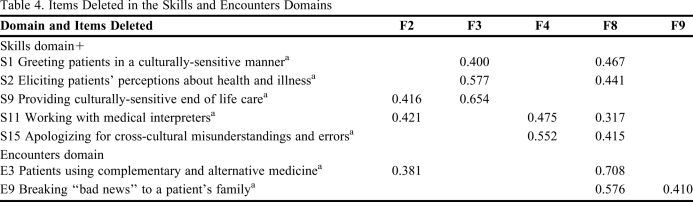
Items Eliminated During the Process
As defined in the methodology, 18 items were deleted during the analysis because of low factor loadings (0.55) or high cross loading with other factors (greater than 0.35). The initial factor analysis, without removing any items, resulted in 11 factors explaining 76.7% of the variance. Table 3 shows the main findings in the cross loadings of these items in the Attitudes and Knowledge domains.
Table 3.
Items Deleted in the Attitudes and Knowledge Domains
Abbreviations: F1 = Addressing Population Health Issues; F5 = Recognizing Disparities-Related Discrimination; F10 = Social Determinants of Health; F11 = Socio-demographic Characteristics
a Item deleted during the process.
In the Attitudes domain, 6 items related to the contribution of important social determinants of health to health disparities (illiteracy, lifestyle, poverty, environment, educational status, and genetics) grouped together, but had to be deleted because they all were cross loaded with F5 (see F10, Table 3). In the Knowledge domain, 5 items related to knowledge of diverse racial and ethnic populations were deleted. Initially, they grouped in an additional factor (F11, Table 3), 4 of them with high cross-loading coefficients with the factor Addressing Population Health Issues (F1), and 1 (K8) with a low coefficient. After deleting these items, one by one, the item health disparities (K4) grouped with F1, and was kept in the final arrangement.
Table 4 shows the main cross loadings of items in the Skills and Encounters domains. Data show that many of these items where cross loaded with the factor Increasing Comfort During Cross-Cultural Clinical Encounters (F8). Although the items S1, S2, and S9 grouped in the factor Providing Culturally Responsive and Effective Services (F3), they were cross loaded with other factors and had to be removed. Also, S9, S11, and E3 grouped in the factor Understanding the Context of Care (F2).
Table 4.
Items Deleted in the Skills and Encounters Domains
Abbreviations: F2 = Understanding the Context of Care; F3 = Providing Culturally Responsive and Effective Services; F4 = Managing Cross-Cultural Clinical Challenges; F8 = Increasing Comfort During Cross-Cultural Clinical Encounters; F9 = Coping With Aggressiveness and Bias
a Item deleted during the process
The item Knowledge About Ethnopharmacology (K6) grouped in the factor Addressing Population Health Issues (F1) and in the factor Understanding the Context of Care (F2), but in both with low coefficients (0.462 and 0.513, respectively) so it was deleted. This item refers to the knowledge and understanding of variations in medication responses in diverse racial and ethnic populations.
DISCUSSION
Not surprisingly, the factors found as the best fit could be grouped into the 4 domains used to measure competencies: knowledge, skills, attitudes, and encounters. Although this is an exploratory factor analysis, the factors were expected to group following the domains defined in the structure of the questionnaire. These domains concur with the domains defined in 2 widely used models for developing cultural competence: The Multidimensional Model of Cultural Competence,24 and the Culturally Competent Model of Care.25 Both of these models are based in the traditional Bloom's domains of educational activities (cognitive, affective, and psychomotor), and follow the competency-based model of knowledge, skills, and attitudes (KSA). They have been adapted and used to implement cultural competence at Xavier, College of Pharmacy.
Knowledge Domain
The factor Addressing Population Health Issues (F1) confirms the guiding principle and standard for cultural competence education that recommends using a broad and inclusive definition of culture and diversity that includes other characteristics, instead of being restricted to the common emphasis on race and ethnicity.26 Although the items related to demographics (K1), sociocultural characteristics (K2), and health risks (K3) had to be removed during the analysis, the fact that they initially grouped in this factor indicates that these topics should be embedded as important components when working with issues related to health disparities and diverse population groups.
Curiously, the factor Understanding the Context of Care (F2) is the only one that contains items from 2 different domains: 3 items from the Knowledge domain and 2 from the Skills domain grouped under this factor. This result could indicate that the items (S3 and S4) “eliciting” information on the patients' use of folk remedies and healers and other alternative modalities require more knowledge about non-Western medicine and complementary and alternative medicine. Definitely, medical and pharmacy students need to learn first about the different folk remedies and practices and open their minds to a more holistic view of health and medicine before eliciting information and caring for patients using these modalities. Culturally competent patient-centered care requires a wider perspective, including biomedicine and other healing traditions such as alternative, complementary, and integrative medicine.27 An advance toward this goal is the South Central Foundation/Alaska Native Medical Center and its Traditional Healing Program,28 which is a major training site for physicians to learn about the healing practices of Alaska Natives as well as for traditional healers to receive formal training and be hired for paid staff positions in a primary care/hospital setting. A similar successful project is the Healthy House, funded by the California Endowment Foundation, which has implemented a certificate program where physicians and shamans work together, observe each other, and demonstrate and discuss their different healing techniques.29 The fact that items related to patients' use of alternative modalities grouped with items related to regulations and standards could be a call for regulations fostering the right to receive health care that is compatible with different healing traditions and the use of complementary and alternative medicine; care that goes beyond the hospital and medical world of diagnoses, medications, treatment, and prognosis.30
Because CLAS standards call for health care delivery that is sensitive to cultural beliefs, practices and language, it is understandable that the items Providing culturally-sensitive end of life care (S9) and Working with medical interpreters (S11) initially grouped in this factor, but that the item Patients using complementary and alternative medicine (E3) also was initially included in this factor (Table 4) reinforces the previous suggestion of extending the CLAS standards to a more holistic concept of “health.” A study to inform how 5 selected national sites are bringing to life, redefining, and informing the reach of CLAS standards concluded that “for the CLAS standards to fully achieve their purpose, the very culture, definition, and design of ‘health care' delivery warrants vigorous examination.”28 This wider definition of health requires systemic changes within the social and legal structures of the health care system to include understanding of patient-provider cultural differences and explanatory models of disease/illness and negotiation of mutually desired goals for care.31
The fact that the item Knowledge About Ethnopharmacology (K6) initially grouped in the 2 factors in the Knowledge domain (F1and F2) and had to be removed, brings into consideration recent efforts in pharmacology and medicine to address unequal or inappropriate medication use by diverse populations. A comprehensive review of studies on medication use in United States reported important disparities in the access, prescriptions, and adherence to medications for African Americans, Hispanics and Asian Americans, and recommended health care planners, advocates, clinicians, and health care organizations to improve prescribing and using medications in a diverse society.32 This result indicates that the variations in medication use and responses in diverse populations also should be considered when working with issues related to health disparities and diverse population groups.
Skills Domain
The items included in the 2 factors in the Skills domain are focused on the different steps along the continuum of health, from patient education and counseling, to prevention, physical examination and diagnosis, to treatment plans negotiation and adherence. In a multicultural environment, conflicts are anticipated to arise along the health care continuum. Misunderstandings, miscommunications, and ethical issues are common causes of failure in diagnosis and treatment plans. Failure to consider diversity factors (gender, age, sexual orientation, race, ethnicity, language, physical ability, social status, among others) when developing health services for a diverse population may result in inaccurate diagnoses, inappropriate treatment plans, malpractices and law suits, and loss of trust. Assertive communication skills in negotiation and conflict resolution and addressing patients' health literacy are keys to obtaining agreement and providing effective interventions.
Attitudes Domain
The 3 factors in the Attitudes domain deal with issues related to discrimination, intercultural interactions and self-reflection. The factor Recognizing Disparities-Related Discrimination (F5) is interpreted as the need to acknowledge that stigma and discrimination exist in the health system, instead of denying it and considering it as something from the past. Cultural competence involves understanding different perspectives of vulnerability and discrimination and a commitment to equity and a social justice. Strong evidence has been found for the relationship between some types of discrimination and health outcomes,33 supporting the need to address stigma and discrimination in an effort to eliminate inequalities in health,34 and to include these topics in education.35 Results in Table 3 show that definitely there is a connection between the Social Determinants of Health (F10) such as illiteracy, lifestyle, poverty, environment, education, and genetics and the different forms of discrimination and prejudice such as sexism, ageism, ableism, homophobia, racism, and classism. The impact of contextual discrimination in health disparities may be mitigated with educational and workforce development activities to foster self-reflection and elimination of personal biases and stereotypes, issues that are included in the factor Engaging in Self-Reflection (F7) in this domain. Training in these topics is the key to moving beyond mere awareness of the impact of biases and recognizing and breaking stereotypes. Sensitivity, a sincere desire, and great humility are the requirements to control and perhaps eliminate personal biases and prejudices.25
Complementing the Attitudes domain is the factor Improving Interpersonal and Intercultural Interactions (F6). Effective communication and workplace interactions are usually found as relevant factors in social sciences. Getting along well with people from different disciplines (such as physicians and pharmacists), with different levels of expertise (such as providers, staff, and students), and having different roles (such as professionals, healers, and patients) contributes to better interactions and a sound crosscultural collaboration environment.
Encounters Domain
Several studies3 have determined that physicians lack the information and skills to understand the multicultural encounter and effectively bridge potential differences. Students need to be able to identify and respond adequately to aggressiveness, bias, and cultural miscommunications caused by differences in habits, values, and communication styles; concepts of time, individualism; and contact and physical space. Aggressive communication shows a lack of respect for others that eventually breaks trust and relationships and jeopardizes health outcomes.23 Items in this factor go beyond approaches that reduce the definition of cultural competence to issues related to cross-cultural communication.
Tables 1 and 2 show the reliability coefficients (Cronbach's alpha) obtained to measure the internal consistency of the factors. Alphas ≥ 0.80 are considered an appropriate level of reliability for research instruments.36 Cronbach's alpha was 0.96 for the sum scale, meaning that it may be considered a reliable measure. Internal consistency reliability coefficients for each factor consistently ranged above 0.85, except for the factor Coping with Aggressiveness and Bias (F9), which had a value of 0.77. This factor included only 2 items and had the lowest eigenvalue (1.009) and variance explained (2.19%). Factors with 3 or fewer items should be considered weak.37 The scree test showed that this factor has a relatively minimal contribution to the scale. When removing the 2 items in this factor, the other 8 factors were not affected, and the change in the total variance explained was not important (decreased to 78.5); therefore, we concluded that it was not necessary to retain this factor.
The minimum structure coefficient obtained was in the item health disparities (K4) with a factor loading of 0.554. This item also showed the minimum communality (h2 = 0.51). Although Costello and Osborne consider item communalities 0.8 or greater as “high,” they found that the more common magnitudes in the social sciences are low to moderate communalities of 0.4 to 0.7 and suggested reviewing items with communality of less than 0.4.37 This item was retained because of its importance in cultural competence, because it satisfied the criteria defined in the methodology (factor load, communality, and CITC value), and because there would be no impact on the scale mean, scale variance, or scale alpha if the item were deleted. Results obtained with the Bartlett Test statistic for sphericity and the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy show that the chi-square (19267.73), associated significance level (0 .000) , and KMO obtained (0.931) allow the use of factor analysis as the statistical technique in this study.
To determine the sample size in principal component analysis, some statisticians recommend looking at the number of cases (N), while others recommend the use of the cases-to-items ratio. A revision of published literature38 found that the common practice in factor analysis is to have cases-to-items ratios ranging from 5:1 to 10:1, and that the number of items, the number of cases, and the cases-to-items ratio had a larger effect when the component loadings were smaller. After analyses were conducted, the number of cases in this study (N = 467) and the cases-to-items ratio (7.3:1) were determined to be adequate for the number of factors extracted (9), the number of items included in those factors (46), and the component loadings finally obtained in this study (> 0.55.)
Based upon the results of this study, other colleges and schools of pharmacy working on the development of curriculum in cultural competence may wish to apply the shorter version of the CCCQ identified in this study (Tables 1 and 2), and to use confirmatory factor analysis to determine if the data conform to the same factor structure found in this study. The CCCQ may also be applicable to different health professions (such as medicine and nursing) and levels of practice (students, residents, and providers). In this case, the full version of the CCCQ may be given and confirmatory factor analysis applied to the results to validate the constructs found in this study.
Limitations of This Study
Although this study provided an opportunity to examine the main constructs of cultural competence to measure cultural competence in pharmacy students, there are some limitations. One important limitation is lack of validation of the measure against other measures available in the field. The CCCQ has been applied to staff members in different hospitals to evaluate the effectiveness of training, but the results are not applicable to this study.15 During the literature review, the California Brief Multicultural Competence Scale16 was identified as a validated and reliable measure of cultural competence at the individual level and was considered suitable to our needs. Unfortunately, the CBMCS is restricted to measure multicultural competence of providers of mental health services and requires further adaptation and validation prior to its use with pharmacy students. We already have applied the CBMCS to the same group of participants and are using the results to validate the CCCQ (manuscript in process). Both measures together will allow us to validate the measurement instruments, assess needs, and develop tailored curriculum content for Xavier College of Pharmacy.
Other limitations are related to the distribution of the sample population and the sample size. More than 75% of the students participating in this study were African and Asian Americans. Although they represent the population characteristics of Xavier University of Louisiana, a historically black university, results could be different with a more diverse population. Although the sample size is considered adequate, more third- and fourth-year participants would strengthen the results. This is a pilot project and the limitations will be accounted for in later applications and validations of the CCCQ and also the CBMCS in the same setting, Xavier College of Pharmacy students.
CONCLUSIONS
The CCCQ is reliable for pharmacy students' self-assessment of their perceived levels of cultural competence. The final number of items derived from the factor analysis is adequate to evaluate students' needs of training in each of the domains defined in this study: knowledge, skills, attitudes, and encounters, which follow the more widely used models of cultural competence. Although results in this study could be different if the factor loadings limits were changed, removing the 18 items that showed low coefficients or high cross loads with other factors resulted in a reliable and practical final arrangement that facilitates the application of the CCCQ in the academic environment. Final constructs contribute to the discussion of the definition of cultural competence and to the growing body of tools available for self-assessment of cultural competence.
ACKNOWLEDGMENTS
The authors would like to express our deep appreciation to Dr. Robert Like for granting authorization to use and modify the Clinical Cultural Competency Questionnaire and for improving this manuscript through his edits and comments. The authors also acknowledge the students who completed the survey instruments, the faculty members who authorized the application of the instrument, and the Institutional Review Board who approved the research. The authors report no conflict of interest in the conduct of this study or the preparation of this manuscript.
REFERENCES
- 1. Goode TD, Dunne C. Policy Brief 1: Rationale for Cultural Competence in Primary Care. National Center for Cultural Competence (NCCC), Washington, DC: Georgetown University Center for Child and Human Development; 2003. http://www11.georgetown.
- 2.Gates M, Bradley KD. Measuring cross-cultural competence in medical education: A review of curricular effectiveness and attitudinal studies. Paper presented at: Annual meeting of the American Educational Research Association. April 12-18, 2009; San Diego, CA. [Google Scholar]
- 3.Betancourt JR, Weissman JS, Kim MK. Resident physicians' preparedness to provide cross-cultural care: implications for clinical care and medical education policy. Commonwealth Fund. 2007;58(10):1362–1365. [Google Scholar]
- 4. Accreditation Council for Pharmacy Education (ACPE). Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed September 1, 2010.
- 5.Scott DM, Friesner DL, Miller DR. Pharmacy students' perceptions of their preparedness to provide pharmaceutical care. Am J Pharm Educ. 2010;74(1) doi: 10.5688/aj740108. Article 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.South-Paul JE, Like RC. Cultural competence for the health workforce. In: Holmes DE, editor. From Education to Regulation: Dynamic Challenges for the Health Workforce. Washington, DC: Association of Academic Health Centers; 2008. pp. 123–152. [Google Scholar]
- 7.Abate MA, Stamatakis MK, Haggett RR. Excellence in curriculum development and assessment. Am J Pharm Educ. 2003;67(3) Article 89. [Google Scholar]
- 8.Boyce EG. Finding and using readily available sources of assessment data. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205102. Article 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. University of Michigan, Program for Multicultural Health. Tools for assessing cultural competence. http://www.med.umich.edu/Multicultural/ccp/Assessments.doc. Accessed September 1, 2010.
- 10.Dunn TW, Smith TB, Montoya JA. Multicultural competency instrumentation: a review and analysis of reliability generalization. J Counse Dev. 2006;84(Fall):471–482. [Google Scholar]
- 11.Kumas-Tan Z, Beagan B, Loppie C, MacLeod A, Frank B. Measures of cultural competence: examining hidden assumptions. Acad Med. 2007;82(6):548–557. doi: 10.1097/ACM.0b013e3180555a2d. [DOI] [PubMed] [Google Scholar]
- 12.Gozu A, Beach MC, Price EG, et al. Self-administered instruments to measure cultural competence of health professionals: a systematic review. Teach Learn Med. 2007;19(2):180–190. doi: 10.1080/10401330701333654. [DOI] [PubMed] [Google Scholar]
- 13. Like RC. Clinical Cultural Competency Questionnaire (CCCQ). Center for Healthy Families and Cultural Diversity, Department of Family Medicine, UMDNJ-Robert Wood Johnson Medical School. Aetna Foundation-Funded Cultural Competency/Quality Improvement Study, 2001. http://www.umdnj.edu/fmedweb/chfcd/aetna_foundation.htm. Accessed September 1, 2010.
- 14. The Migrant Friendly Hospitals Project (MFH), sponsored by the European Commission, DG Health and Consumer Protection (SANCO). http://www.mfh-eu.net/public/home.htm. Accessed September 1, 2010.
- 15.Krajic K, Straßmayr C, Karl-Trummer U. Improving ethnocultural competence of hospital staff by training: experiences from the European ‘Migrant-friendly Hospitals' project. Divers Health Soc Care. 2005;2(4):279–290. [Google Scholar]
- 16.Gamst G, Dana RH, Der-Karabetian A, Aragon M, et al. Cultural competency revised: the California brief multicultural competence scale. Meas Eval Counsel Dev. 2004;37(3):163–183. [Google Scholar]
- 17.Del Carmen MG, Joffe S. Informed consent for medical treatment and research: a review. Oncologist. 2005;10(8):636–641. doi: 10.1634/theoncologist.10-8-636. [DOI] [PubMed] [Google Scholar]
- 18.Babbie E. The Practice of Social Research. 12th edition. Belmont, CA: Wadsworth Publishing Company; 2009. 530. [Google Scholar]
- 19.Norusis MJ. SPSS 13.0 Guide to Data Analysis. Upper Saddle River, NJ: Prentice Hall; 2005. 648. [Google Scholar]
- 20.Leech N, Barrett K, Morgan GA. SPSS for Intermediate Statistics: Use and Interpretation. 3rd ed. Mahwah, NJ: Lawrence Eribaum Associates; 2007. 288. [Google Scholar]
- 21. Office of Minority Health (OMH). National Standards for Culturally and Linguistically Appropriate Services in Health Care: FINAL REPORT. Washington, DC: Department of Health and Human Services (DHHS);2001:132. http://raceandhealth.hhs.gov/assets/pdf/checked/finalreport.pdf. Accessed September 1, 2010.
- 22. Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1497553/pdf/12815076.pdf Accessed September 1, 2010.
- 23.Antai-Otong D. Nurse-Client Communication: A Life Span Approach. Sudbury, MA: Jones and Bartlett Publishers; 2007. 251. [Google Scholar]
- 24.Sue DW. Multidimensional facets of cultural competence. Couns Psychol. 2001;29(6):790–821. [Google Scholar]
- 25.Campinha-Bacote J. The Process of Cultural Competence in the Delivery of Healthcare Services: The Journey Continues. 5th ed. Cincinnati, OH: Transcultural Care. [DOI] [PubMed] [Google Scholar]
- 26.Gilbert J. Woodland, CA: The California Endowment; 2003. Principles and Recommended Standards for Cultural Competence Education of Health Care Professionals. 93. [Google Scholar]
- 27. National Center for Complementary and Alternative Medicine (NCCAM), National Institutes of Health (NIH), US Department of Health and Human Services. http://nccam.nih.gov/. Accessed September 1, 2010.
- 28. Putsch R, SenGupta I, Sampson A, Tervalon M. Reflections on the CLAS Standards: Best Practices, Innovations and Horizons. The Cross Cultural Health Care Program, Office of Public Health and Science. Seattle, Washington: Office of Minority Health; 2003:93. http://www.xculture.org/files/CLAS.Standards.Report.pdf.pdf. Accessed September 1, 2010.
- 29. Goode T, Sockalingam S, Lopez-Snyder L. Bridging the Cultural Divide in Health Care Settings: The Essential Role of Cultural Broker Programs. Washington, DC: National Center for Cultural Competence, Georgetown University Center for Child and Human Development, 2003. http://www11.georgetown.edu/research/gucchd/nccc/documents/Cultural_Broker_Guide_English.pdf Accessed September 1, 2010.
- 30.Wintz S, Cooper E. Schaumburg, IL: Association of Professional Chaplains; 2003. Learning Module Cultural and Spiritual Sensitivity: A Quick Guide to Cultures and Spiritual Traditions, Teaching Notes. 101. [Google Scholar]
- 31.Kagawa-Singer M, Kassim-Lakha S. A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes. Acad Med. 2003;78(6):577–587. doi: 10.1097/00001888-200306000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Levy R, Like RC, Shabsin H. Origins and Strategies for Addressing Ethnic and Racial Disparities in Pharmaceutical Therapy: The Health-Care System, the Provider, and the Patient. Washington, DC: National Minority Quality Forum; 2009. [Google Scholar]
- 33.Harris R, Tobias M, Jeffreys M, Waldegrave K, Karlsen S, Nazroo J. Racism and health: the relationship between experience of racial discrimination and health in New Zealand. Soc Sci Med. 2006;63(6):1428–1441. doi: 10.1016/j.socscimed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 34.Stuber J, Meyer L, Link B. Stigma, prejudice, discrimination, and health. Soc Sci Med. 2008;67(3):351–357. doi: 10.1016/j.socscimed.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Porter CP, Barbee E. Race and racism in nursing research: past, present, and future. Ann Rev Nurs Res. 2004;22(9):37. [PubMed] [Google Scholar]
- 36.Raubenheimer JE. An item selection procedure to maximize scale reliability and validity. S Afr J Ind Psychol. 2004;30(4):59–64. [Google Scholar]
- 37.Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1–9. [Google Scholar]
- 38.Osborne JW, Costello AB. Sample size and subject to item ratio in principal components analysis. Pract Assess Res Eval. 2004;9 article 11. [Google Scholar]