Abstract
Objective
To develop and implement a medication therapy management (MTM) curriculum and assess students' skills and attitudes after the provision of MTM services to faculty and staff members.
Design
Third-year students enrolled in a pharmaceutical care laboratory course received lectures and participated in MTM activities in preparation for an MTM encounter. Students conduced MTM sessions with university faculty and staff members, providing comprehensive medication review, blood pressure checks, and optional blood glucose and cholesterol (total cholesterol and HDL) screenings.
Assessment
A faculty-developed rubric was used to evaluate students' ability to explain MTM to the participant and address medication-related problems. Students' responses on pre- and post-encounter survey instruments showed their confidence to provide MTM services, communicate with participants and other health care providers, and provide point-of-care screening services had increased.
Conclusion
Incorporating MTM into an existing laboratory course increased students' confidence and perceived ability to provide MTM services.
Keywords: medication therapy management, medication review, patient-centered care
INTRODUCTION
The Joint Commission of Pharmacy Practitioners' Vision of Pharmacy Practice 2015 states that pharmacists should be proficient in medication therapy management (MTM) and be advocates for the promotion of patient wellness.1 MTM services are patient-centered encounters that result in the optimization of medication therapy, improved patient outcomes, and cost-savings.1 Real-time meetings between a pharmacist and patient are designed to improve collaboration among the health care continuum, enhance communication, and empower patients through education.2 Real-life MTM encounters improve students' confidence in providing MTM services.3 The American Pharmacists' Association, in collaboration with the National Association of Chain Drug Stores Foundation, has identified 5 core elements of MTM: conducting a medication therapy review, providing patients with a personal medication record and medication action plan, recognizing whether intervention or referrals are needed, and documenting services provided.2
The Institute of Medicine has stated that health care should be safe, effective, and patient-centered, and has encouraged patients to be active participants in the health care process to assist in the prevention of medication-related problems.4 Medication-related problems are a significant public health issue. A 2001 study estimated that more than 1.5 million preventable medication-related adverse events occur each year in the United States, accounting for an excess of $177 billion in medication-related morbidity and mortality.5
As MTM opportunities expand within the profession of pharmacy, future pharmacists must have the knowledge, skills, and abilities to provide these services. The American Association of Colleges of Pharmacy (AACP) Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Educational Outcomes has defined criteria for providing patient-centered and population-based care that optimizes medication therapy. The CAPE outcomes state that PharmD graduates should be able to provide exemplary patient-centered care, which includes the ability to obtain, interpret, and evaluate patient information; determine the presence of a disease or medical condition; assess the need for treatment and/or referral; and identify patient-specific factors that affect health, pharmacotherapy, and/or disease management.6 Standards 2007 describes the use of innovative instructional methodologies to foster the development of critical-thinking and problem-solving skills in students and emphasizes the importance of actual student-patient interaction to develop these skills.1
This article describes how third-year pharmacy students provided MTM services to faculty and staff members of North Dakota State University through an innovative MTM curriculum. Three objectives were developed and designed around the highest levels of Bloom's Taxonomy of learning.7 Students would demonstrate the ability to perform a comprehensive medication review effectively and interpret findings to identify medication-related problems; demonstrate the ability to document an MTM encounter; and feel confident to integrate the core elements of MTM, clinical knowledge, and communication skills to effectively provide MTM.
DESIGN
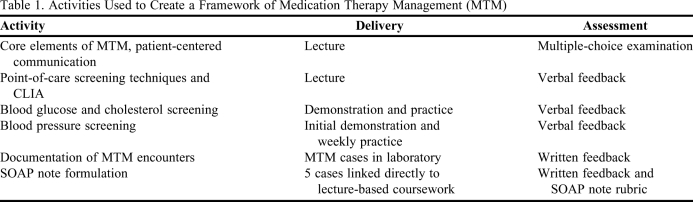
Medication therapy management activities were integrated into the Pharmaceutical Care Laboratory IV course to teach third-year pharmacy students the skills necessary to provide MTM services during an actual patient encounter (Table 1). Students received lectures focused on the core elements of MTM, patient-centered communication, and techniques used for point-of-care screenings. Paper-based MTM cases were used during weekly laboratory activities, and students practiced point-of-care testing through peer screening. Five pharmacist faculty members and 1 pharmacy resident served as preceptors for the encounters and evaluated students' performance. These individuals were practicing pharmacists with experience providing MTM and disease state management services.
Table 1.
Activities Used to Create a Framework of Medication Therapy Management (MTM)
Abbreviations: MTM = Medication Therapy Management; CLIA = Clinical Laboratory Improvement Amendments; SOAP = Subjective, objective, assessment, and plan
Brochures and e-mails were sent inviting 2,205 faculty and staff members at North Dakota State University to schedule an MTM encounter with a precepted pharmacy student that would include a comprehensive medication review, blood pressure check, and optional blood glucose and cholesterol (total cholesterol and HDL) screenings. The first 45 eligible respondents were selected to participate in the project, resulting in a 2:1 student-to-participant ratio. To be eligible, respondents had to have been taking 3 or more prescription medications. To comply with the Health Insurance Privacy and Accountability Act policies participants' names and dates of birth were not collected.8
The class was randomly divided into groups of 2 students and a participant was randomly assigned to each group. Students received their participant's health information 1 week prior to their scheduled encounter to allow the students time to review the participant's health history, identify drug-related problems, and perform searches for clinical information if necessary. Students also were encouraged to review course lecture notes and national treatment guidelines to assist in the evaluation and preparation of their case. During this time, precepting faculty members were available to meet with students to discuss specific cases. Students used a health information form to develop a personal medication record prior to the encounter. The template used was a pocket-sized guide developed by the North Dakota Pharmacists Association and included the name and strength of each medication, directions for use, and the prescriber.
The encounters were held in 2 private consultation rooms within the laboratory and students were given 1 hour to interview the participant, perform 2 blood pressure readings, and conduct optional blood glucose and cholesterol screenings. Each participant was given a PMR as a comprehensive record of their medications, including prescription and nonprescription medications, herbal products, and dietary supplements. When the medication record was complete, it was given to the participant to use to manage their medications. Students performed a comprehensive medication review with the participant in which they reviewed participant-specific information, evaluated medication therapies, and developed a plan to resolve any medication-related issues. Pharmacy students identified and managed drug therapy problems for participants, including addressing medication dosing issues, discussing possible adverse effects, and providing cost-containment strategies for medications.
Students also assisted the participant with the formulation of a medication action plan, which included a list of actions for the participant to take toward self-management of his/her health and a place to record progress. Students used the medication action plan template from the American Pharmacists' Association MTM Core Elements Toolbox.9
During the encounter, faculty members used a specially designed rubric to evaluate each student's interviewing techniques, verbal and nonverbal communication skills, and ability to conduct a complete evaluation of past medical history and current complaints. After the encounter, each student wrote a summary of the visit in the form of a subjective, objective, assessment, and plan (SOAP) note which was assessed by faculty members using a second rubric. If prescriber approval was needed before a recommended change could be made, students formulated a written recommendation that included their findings and justification. All recommendations were reviewed and cosigned by precepting faculty members prior to the students communicating with the prescriber. After the MTM encounters, students presented their results in small groups to increase peer exposure to the impact of MTM. The North Dakota State University Institutional Review Board approved the informed consent document and survey instruments used in this study.
EVALUATION AND ASSESSMENT
Eighty-five students performed MTM encounters. Students were evaluated on their interviewing techniques, verbal and nonverbal communication skills, and ability to conduct a complete evaluation of past medical history, medication-related problems, and current complaints. A faculty-developed rubric was used to evaluate each student during the encounter. Students scored an average of 18.5 out of 20 possible points (92.9%).
Students also were evaluated on their ability to document their MTM encounter. A faculty- developed rubric was used to evaluate students' documentation of subjective and objective information, assessment of medication-related problems, plan of therapy, and the updated list of medications. Each of these focus areas were graded using a Likert scale and the descriptors missing, poor, incomplete, and excellent. Students scored an average of 14.6 out of 15 possible points (97.5%).
Faculty members reviewed all student-identified drug-therapy problems, none of which required faculty members' intervention during the patient encounter. Student recommendations were classified as dose too low or high, needs additional or is receiving unnecessary drug therapy, adverse drug reaction, needs different drug, noncompliance, and cost-containment. Students identified 85 drug therapy problems for the 45 participants. Of these recommendations, 14 were communicated to the participant's prescriber. In addition to identifying drug-therapy problems, students also recommended lifestyle modifications to 29 of the participants.
Students recommended additional drug therapy for 28 participants. Of these, 13 were recommendations for immunization updates. Students identified 12 cost-containment interventions, 11 of which were communicated to the prescriber. Cost-containment interventions included recommendations to change to a generic alternative, a combination medication, or splitting of tablets. Students identified 20 cases of noncompliance. Of these, inappropriate administration technique was the most common issue. Most administration problems were a result of the participant's incorrect timing of the administration. After evaluating specific participant information, students identified 11 participants who needed an additional medication, or a change to a more effective medication.
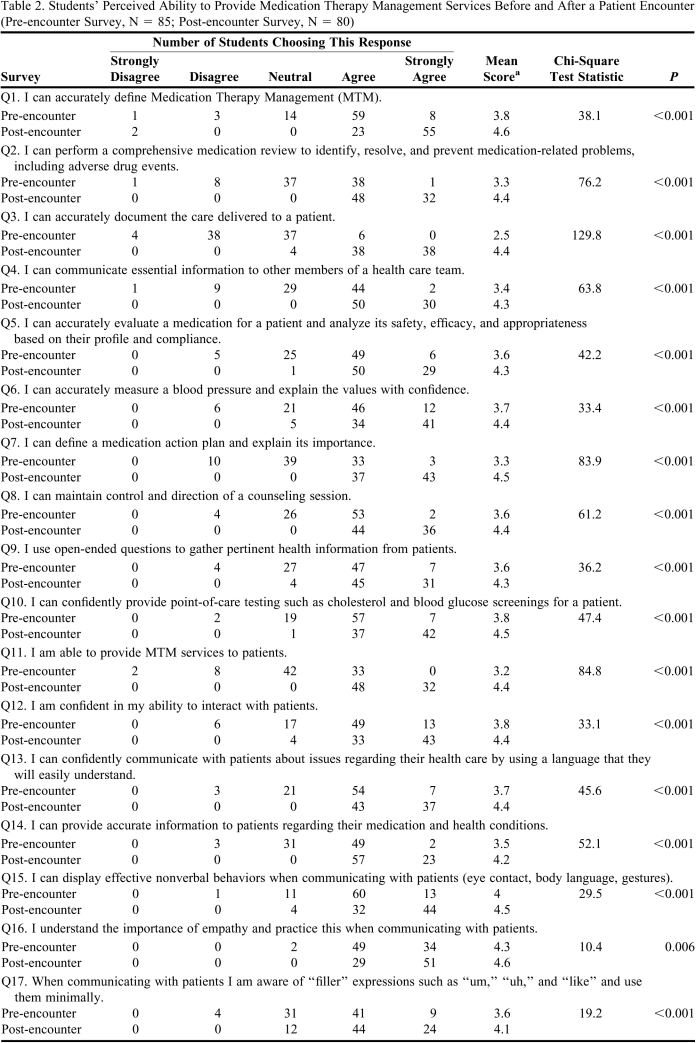
Faculty-developed pre-encounter and post-encounter survey instruments were used to assess students' confidence and perception of their ability to provide MTM services as defined in the learning objectives. The surveys were administered online using a 5-point Likert scale and participation was anonymous and voluntary. The pre-encounter survey instrument was administered after the lectures and paper-based MTM cases were completed, but prior to the actual patient encounter. The post-encounter survey instrument was administered upon completion of the project, after the small group case presentations. The post-encounter survey instrument contained all of the items in the pre-encounter survey plus 7 additional items that allowed students to rate the grading procedures, participant feedback, and the effect the project had on their ability to work with the participants.
Eighty-five students (100%) completed the pre-encounter survey instrument, and 80 students (94.1%) completed the post-encounter survey instrument. Results were analyzed using a chi-square test under the null hypothesis that the distribution of pre- and post-encounter responses would be the same (Table 2). Rejecting the null of homogeneity suggests that the intervention changed students' perceived MTM competencies.
Table 2.
Students' Perceived Ability to Provide Medication Therapy Management Services Before and After a Patient Encounter (Pre-encounter Survey, N = 85; Post-encounter Survey, N = 80)
Abbreviations: MTM = Medication Therapy Management
aResponses based on a scale of 1 to 5 on which 1 = strongly disagree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree.
Each survey item correlated with a significant increase in students' perceived ability to perform MTM services after the encounter (p < 0.05). The number of students who strongly agreed they could provide MTM services increased after the participant encounter (Table 2). Students' perceived ability to document patient care, perform a comprehensive medication review, and evaluate appropriateness of medications based on a specific case also increased. An increased number of students strongly agreed they were confident in their ability to provide point-of-care testing such as blood pressure, cholesterol, and blood glucose screenings.
After the MTM encounter, students' perceived ability to communicate effectively increased. The number of students who strongly agreed they could communicate information with other health care professionals, use open-ended questions to gather health information, and display proper nonverbal communication skills while interacting with participants also increased, as did students' understanding of the importance of practicing empathy when communicating with patients.
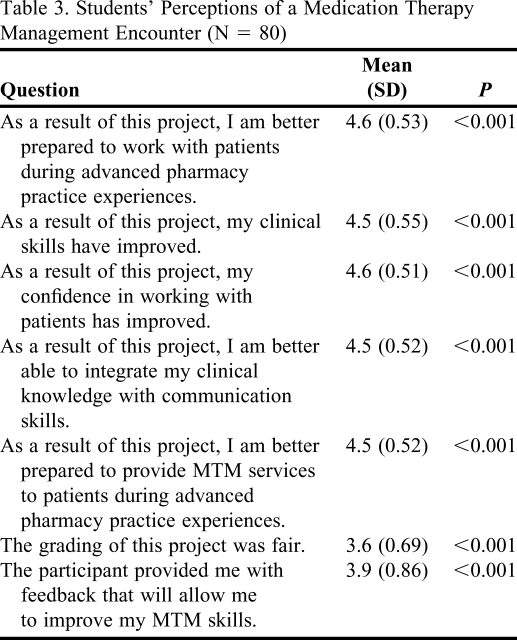
Results of the post-encounter survey were analyzed using a univariate t test under the null of “neutral” responses (score 3 of 5), and all results were significant with a p value < 0.05 (Table 3). Students reported that the MTM encounters increased their confidence to work with participants, improved their clinical skills, and prepared them to perform MTM services.
Table 3.
Students' Perceptions of a Medication Therapy Management Encounter (N = 80)
Abbreviations: MTM = Medication Therapy Management
Scale: 1 = strongly agree; 2 = disagree; 3 = neutral; 4 = agree; 5 = strongly agree
An anonymous and voluntary survey instrument was distributed to all faculty and staff participants immediately after the MTM encounters. Thirty of the 45 participants (67%) completed the survey instrument. One hundred percent of the participants agreed that their encounter was valuable to their health and that they would be interested in returning for an additional encounter if the services were offered again the following year.
DISCUSSION
As MTM opportunities expand within the profession of pharmacy, future pharmacists must have the knowledge, skills, and abilities to provide these services. Medication therapy management was integrated into a preexisting laboratory course required in the professional pharmacy curriculum. Students critically analyzed their participant's health information, using educational coursework and national treatment guidelines to develop a patient-centered plan of care.
The Accreditation Council for Pharmacy Education (ACPE) recommends the use of actual student-patient interaction to develop critical-thinking and problem-solving skills.2 Based on evidence that pharmacy students prefer actual patients over standardized patients,10 faculty members developed the MTM curriculum to include real, non-simulated, non-standardized patients. We used actual patient MTM encounters to assist students in developing the skills and knowledge necessary to become proficient in MTM, and advocates for the promotion of patient wellness. Furthermore, students conducted the MTM encounters in an authentic working environment.
Surveys evaluated students' perceived ability to provide MTM services prior to and after an MTM encounter with a non-standardized, non-simulated patient. Students' skills in providing the core elements of MTM during an encounter and their documentation were evaluated using faculty-developed rubrics. After completion of the MTM component of the curriculum, assessment revealed students felt prepared to provide MTM services. Students' confidence to integrate the core elements of MTM, clinical knowledge, and communication skills increased after the MTM encounter. These results indicated students can improve confidence and perceived ability through actual student-patient interactions. Evaluation of students' provision and documentation of MTM services indicated that the learning objectives for the MTM curriculum were met.
Participants reported that the MTM services were successful and valuable to their health, and all surveyed participants stated they would be interested in a follow-up visit. Future curricular development could include an additional comprehensive medication review and a follow-up visit later in the semester to evaluate recommendations made and progress towards self-management. With the addition of a follow-up visit, students would see the impact of MTM on patient care. Follow-up also would provide an opportunity for students to build patient relationships. Additional pharmacy services that could be offered include bone density screening, immunization administration, fasting lipid panels, and hemoglobin A1C screenings. This follow-up would increase student exposure to patient-centered care, point-of-care testing devices, and provide additional opportunities to evaluate and discuss test results.
Potential limitations included the participant population used, adherence to HIPAA, and the encounter space. The participants recruited from campus were healthy, knowledgeable, and educated about their medications and disease states. Also, they may have been more likely to rate the encounters positively because this was the first time MTM services were offered. Recruiting participants from off campus may have resulted in a patient population with more complex disease states and medication regimens. There was no blinding, and faculty members may have been looking for positive results as they evaluated students. This may have been a potential source of bias. Also, adherence to HIPAA regulations was difficult through the use of campus resources such as e-mail and campus mail. Finally, encounters took place in the pharmaceutical care laboratory; however, the laboratory had only 2 consultation rooms, limiting the number of encounters that could occur simultaneously. Increasing the number of private rooms available for encounters would decrease the total amount of time needed for MTM encounters.
SUMMARY
Incorporating MTM into an existing laboratory course resulted in student learning and an increase in students' confidence and perceived ability to provide MTM services. After the MTM encounter, students felt confident to provide MTM services, perform point-of-care testing, and communicate with participants and other health care providers.
ACKNOWLEDGEMENTS
The authors acknowledge the North Dakota State University Department of Pharmacy Practice for providing a grant to defer the costs associated with the project. The authors thank faculty members Alicia Fitz, PharmD, Renae Lien, PharmD, and Amy Werremeyer, PharmD, for precepting participant encounters. The authors thank Dan Freisner, PhD, Associate Dean of Student Affairs, for his assistance with data analysis.
REFERENCES
- 1. Accreditation Council for Pharmacy Education (ACPE). Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Chicago, Illinois. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed October 27, 2010.
- 2.American Pharmacists Association. National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service (version 2.0) J Am Pharm Assoc. 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 3.Kuhn C, Powell PH, Sterrett JJ. Elective course on medication therapy management services. Am J Pharm Educ. 2010;74(3) doi: 10.5688/aj740340. Article 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine. To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [Google Scholar]
- 5.Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc. 2001;41(2):192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- 6. The AACP Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Educational Outcomes. 2004 Educational Outcomes. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf Accessed October 27, 2010.
- 7.Castle A. Demonstrating critical evaluation skills using Bloom's taxonomy. Int J Ther Rehabil. 2003;10(8):369–373. [Google Scholar]
- 8. Department of Health & Human Services Office of the Secretary. Standards for Privacy of Individually Identifiable Health Information (45 CFR parts 160 and 164). http://www.hhs.gov/ocr/privacy/hipaa/understanding/summary/guidanceallsections.pdf Accessed October 27, 2010.
- 9. American Pharmacists Association MTM Core Elements Toolkit. MTM Medication Action Plan. http://www.pharmacist.com/AM/Template.cfm?Section=Pharmacists&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=118&ContentID=18972 Accessed October 27, 2010.
- 10.Gallimore C, George AK, Brown MC. Pharmacy students' preferences for various types of simulated patients. Am J Pharm Educ. 2008;72(1) doi: 10.5688/aj720104. Article 4. [DOI] [PMC free article] [PubMed] [Google Scholar]