Abstract
In 2006, the CDC released a revised Field Triage Decision Scheme. It is unknown how this modified scheme will affect the number of patients identified by EMS for transport to a trauma center.
Objective
To determine the change in the number of patients transported by EMS who meet the 2006 scheme, compared to the 1999 scheme, and to determine how the scheme change would affect under- and over-triage rates.
Methods
EMS providers in charge of care for injured adult patients transported to a regional trauma center in three mid-sized cities were interviewed immediately after completing transport. All injured patients were included, regardless of severity. The interview included patient demographics, vital signs, apparent anatomic injury, and the mechanism of injury. Included patients were then followed through hospital discharge. The 1999 and 2006 scheme criteria were each retrospectively applied to the collected data. The number of patients identified by the two schemes was determined. Patients were considered to have needed a trauma center if they had non-orthopedic surgery within 24 hours, ICU admission, or died. Data were analyzed using descriptive statistics including 95% confidence intervals.
Results
EMS interviews were conducted for 11,892 patients and outcome data was unavailable for one patient. Average patient age was 48 years; 51% were men. Providers reported bringing 54% of the enrolled patients to the trauma center based on their local trauma protocol. 12% of enrolled patients were identified as needing a trauma center based on medical record review. Use of the 2006 scheme would have resulted in 1,423 fewer patients (12%; 95% CI:11-13%) being identified as needing a trauma center by EMS providers (40%; 95%CI:39-41% versus 28%; 95%CI:27-29%). 1,344 of those patients did not actually need the resources of a trauma center (94%). 78 (6%) of those patients actually needed the resources of a trauma center and would have been under-triaged.
Conclusion
Use of the 2006 Field Triage Decision Scheme would have resulted in a significant decrease in the number of patients identified as needing the resources of a trauma center. These changes reduced over-triage while causing a small increase in the number of patients who would have been under-triaged.
Keywords: Wounds and Injury, Triage, Emergency Medical Services, Emergency Medical Technicians
Introduction
The American College of Surgeons first described criteria for EMS providers to identify patients who needed the resources of a trauma center in 1987.1 These field triage criteria were designed to help EMS providers identify patients who needed the specialized resources of a trauma center. For patients who meet the criteria it was recommended that the patient be transported directly from the scene of their injury to the trauma center even if a closer non-trauma center hospital was bypassed. Over the years the criteria have been revised and included in each subsequent publication of the American College of Surgeons Committee on Trauma “Resources for Optimal Care of the Injured Patient”. In 2006, the American College of Surgeons partnered with the Centers for Disease Control and Prevention to revise the Field Triage Decision Scheme. These recently released guidelines were published in the Resources for Optimal Care of the Injured Patient 2006 and in the Morbidity and Mortality Weekly Report.2, 3
The 2006 revision was developed by a nationally representative, multi-disciplinary, expert panel and each step of the Field Triage Decision Scheme was revised using the best available science and consensus opinion.3 Examples of the revisions included: removing the Revised Trauma Score from the physiologic criteria and adding crushed, degloved, and mangled extremities to the anatomic criteria. The most significant changes were made to the mechanism of injury criteria and the special considerations criteria.
Based on the scope of these changes it is clear that they will have an affect on the number of patients who are transported to a trauma center. However, the magnitude of their affect is unknown. It is hoped that these changes will reduce over-triage while reducing or holding-steady under-triage rates. The objective of this study was to determine the number of patients who would be affected by these changes to the Field Triage Decision Scheme and to determine its affect on under- and over-triage.
Methods
A two-year prospective observational study was conducted at large tertiary care hospitals which were also the regional trauma centers in three midsized cities: Milwaukee, WI; Rochester, NY; and Royal Oak, MI. All three hospitals were state-designated level 1 regional trauma centers, two of which were also verified as Level 1 Trauma Centers by the American College of Surgeons. Included in the study was any adult patient (age 18 years and older) with a traumatic mechanism of injury, regardless of injury severity, transported to a study hospital by an EMS provider (either by ground ambulance or helicopter) from the scene of their injury. Included patients may have requested transport to the study hospital or the EMS providers may have selected it based on their local trauma triage protocols. That is only some of the patients included in this study were identified by the EMS providers as having to be transported to a trauma center by their trauma protocols, while the remainder of the patients were injured patients who were brought to the study hospital because it was a tertiary care hospital. The local EMS agencies used trauma protocols which were locally modified versions of the American College of Surgeons Field Triage Decision Scheme and varied by site. For the purposes of this study, traumatic mechanism of injury was defined as: motor vehicle crash, motorcycle crash, fall, pedestrian or bicyclist struck, or assault. Patients were excluded if they were not transported by EMS, were transferred by EMS from another receiving facility, or if the EMS providers did not see the scene of the injury.
EMS providers in charge of patient care were interviewed upon arrival at the emergency department (ED). The interview was conducted when interview staff were available, which was typically between 7am and 11pm, or providers could complete the interview via a paper survey instrument when an interviewer was unavailable. Missed patients were tracked and basic demographic information was captured to identify any biases in captured subjects.
The interview included: patient demographics, initial vital signs, co-morbidities, apparent anatomic injury, and mechanism of injury. Specifically the interview captured information on each component of the Field Triage Decision Scheme. For any component that required measurement the provider was asked to give their estimation rather than stating if the criteria was met. For example, rather than stating if intrusion into a vehicle’s passenger compartment was greater then 12 inches the provider was asked to estimate “how many inches of intrusion were there in the passenger compartment” and where the intrusion was located (e.g., driver side or passenger side).
After the interview was completed, a research assistant monitored the patients’ progress through the hospital via medical records to determine when they were discharged from the ED, or if admitted, when they were discharged from the hospital. Once the patient was discharged the research assistant reviewed the patient’s medical records to determine if the patient should be classified as needing the resources of a trauma center. Need for the resources of a trauma center was explicitly defined using a composite measure which included: whether or not the patient had urgent non-orthopedic surgery within 24 hours of ED arrival, were admitted to the intensive care unit, and/or died prior to discharge. This was selected as the primary outcome because it represents actual trauma center resource use and has been described in previous research.6 Injury Severity Score was also obtained as a secondary outcome using the ICD-9 codes documented in the patients medical record and previously described methodology.4, 5
At all three sites the medical record review was conducted by the research coordinator using a structured data collection instrument. At two sites this position was held by two different people so a total of 5 non-physicians abstracted the outcome data. Prior to abstracting the data the research coordinator and the site investigator, who was a physician, independently reviewed the same 10 charts. If there were discrepancies in the abstraction an additional 5 charts were reviewed. This process continued until there was 100% agreement on the data abstraction between the research coordinator and the physician site investigator. The research coordinator subsequently abstracted data independently and the physician was available for questions. Monthly conference calls were held with all of the investigators and coordinators to discuss the study and issues or questions regarding data abstraction. The study was approved by all three institutions’ Institutional Review Boards.
Data Analysis
The 1999 and 2006 schemes were each retrospectively applied to the data collected during the EMS provider interview. That is, we determined for each patient if they would have met any of the criteria of either scheme. The number of patients identified by each scheme was determined and descriptive statistics were calculated. We then calculated the number of patients who would have been over- or under-triaged using each scheme and calculated the change in the rate of under- and over-triage that would have resulted from using the 2006 scheme rather than the 1999 scheme.
Results
A total of 11,892 interviews were conducted. One case was missing outcome information and had to be excluded from the under- and over-triage analysis. The average patient age was 48.0 years ± 21.8, 51% were men, and in 54% of the cases EMS reported they brought the patient to the trauma center based on local trauma protocol. The remaining patients requested to be brought to that particular hospital or were taken there for some other reason.
Using the 1999 scheme would have identified 4,772 patients (40%; 95%CI: 39%-41%) for transport to the trauma center, while using the 2006 scheme would have identified 3,349 patients (28%; 95%CI: 27%-29%) for transport to the trauma center. Figure 1 demonstrates the number of patients identified as needing a trauma center at each step of the 1999 and 2006 schemes. The specific anatomic criteria attained by patients for both schemes is shown in Table 1 and the specific mechanism of injury criteria attained by patients for both schemes is shown in Table 2. Overall, use of the 2006 scheme would have identified 1,423 (12%; 95%CI: 11%-13%) fewer patients for transport to a trauma center. Of those patients, 1,344 (94%) did not need the resources of a trauma center, but 78 (6%) patients needed the resources of a trauma center and would have been under-triaged. Outcome information was not available for 1 patient so trauma center need could not be determined. In Table 3 we show the accuracy rate for each scheme. The sensitivity of the 2006 criteria was 72% (95%CI 69% - 74%) and the specificity was 77% (95%CI: 77% - 78%). The sensitivity of the 1999 criteria was 77% (95%CI 75% - 79%) and the specificity was 65% (95%CI: 64% - 66%).
Figure 1.
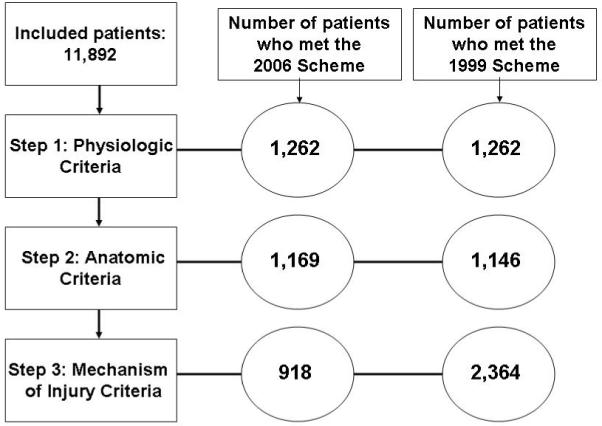
The number of patients who were identified by each step of the Scheme
Table 1.
Comparison of Patients Achieving the 1999 Anatomic Criteria vs. the 2006 Anatomic Criteria
| 1999 SCHEME | CRITERIA | 2006 SCHEME | ||
|---|---|---|---|---|
| # of Patients |
Status in 1999 | Status in 2006 | # of Patients |
|
| 700 | Included | Penetrating injuries | Included | 700 |
| 26 | Included | Flail chest | Included | 26 |
| 136 | Included | 2 or more proximal long bone fractures |
Included | 136 |
| 205 | Included | Pelvic fracture | Included | 205 |
| 3 | Included | Open and depressed skull fracture | Changed to: open OR depressed |
82 |
| 67 | Included | Paralysis | Included | 67 |
| 9 | Included | Amputation | Included | 9 |
| 3 | Included | Major burns | Removed | --- |
| 39 | Included | Burns with trauma | Removed | --- |
| --- | Not Included | Crush, degloved or mangled extremities |
Included | not collected |
Table 2.
Comparison of Patients Achieving the 1999 Mechanism of Injury Criteria vs. the 2006 Mechanism of Injury Criteria
| 1999 SCHEME | CRITERIA | 2006 SCHEME | ||
|---|---|---|---|---|
| # of Patients |
Included in 1999 | Included in 2006 | # of Patients |
|
| 38 | Included | Ejection from automobile | Included | 37 |
| 25 | Included | Death in the same passenger compartment |
Included | 25 |
| 202 | Included | Intrusion >12 inches | Changed to: >12in patient side, >18in other sides |
142 |
| --- | Not included | Vehicle telemetry data | Included | not available |
| 105 | Included | Extrication time >20 minutes | Removed | --- |
| 524 | Included | Rollover | Removed | --- |
| 970 | Included | Initial speed >40 mph | Removed | --- |
| 457 | Included | Deformity >20 inches | Removed | --- |
| 36 | Included | Fall >20 feet | Included | 35 |
| 314 | Included | Auto-pedestrian/bicycle >5 mph | Changed to: >20 mph | 155 |
| 180 | Included | Pedestrian thrown or run over | Included | 176 |
| 387 | Included | Motorcycle crash >20 mph or separation of rider from bike |
Removed: separation of rider from bike |
306 |
Table 3.
1999 and 2006 Field Triage Decision Schemes Compared for Triage Accuracy Using a Composite measure as the Gold Standard for Trauma Center Need
| Needed Resources of a Trauma Center | ||
|---|---|---|
| Yes | No | |
| 1999 Criteria | ||
| Positive | 1,054 (8.9%) | 3,717 (31.2%) |
| Negative | 310 (2.6%) | 6,810 (57.2%) |
| 2006 Criteria | ||
| Positive | 976 (8.2%) | 2,373 (20.0%) |
| Negative | 388 (3.3%) | 8,154 (68.6%) |
Highlighted boxes indicate triage scheme was accurate
Composite measure included having non-orthopedic surgery within 24 hours, ICU admission, or death
Previous literature has used Injury Severity Score greater than 15 as an indicator of trauma center need. Table 4 illustrates that using Injury Severity Score as a measure for trauma center need would have reduced the calculated accuracy rate for both schemes, but the finding that the 2006 scheme slightly increases under-triage and greatly reduces over-triage was still seen.
Table 4.
1999 and 2006 Field Triage Decision Schemes Compared for Triage Accuracy Using Injury Severity Score as the Outcome
| ISS>15 | ||
|---|---|---|
| Yes | No | |
| 1999 Criteria | ||
| Positive | 709 (6.0%) | 4,062 (34.1%) |
| Negative | 398 (3.3%) | 6,722 (56.5%) |
| 2006 Criteria | ||
| Positive | 622 (5.2%) | 2,727 (22.9%) |
| Negative | 485 (4.1%) | 8,057 (67.8%) |
Highlighted boxes indicate triage scheme was accurate
Discussion
Our study is the first to directly compare the 1999 version of the Field Triage Decision Scheme to the newly released 2006 Scheme. We found that the 2006 scheme changes will likely lead to fewer patients being identified for transport to a trauma center. This reduction will primarily reduce over-triage, but will cause a small increase in under-triage.
The 1999 scheme would have incorrectly triaged 34% of patients, while the 2006 scheme would have incorrectly triaged 23% of patients. While ideally, these guidelines would result in no under- or over-triage, that is impossible. An acceptable rate of under- and over- triage has not been determined, but the Resources for Optimal Care of the Injured Patient 2006 document suggests that a 5% rate of under-triage is acceptable, and an acceptable over-triage rate is 25% to 50%.2 Our data demonstrate that either triage scheme meets these stated goals, but clearly the 2006 scheme improves accuracy and is an important advance. It is also important to note that not meeting the Field Triage Decision Scheme criteria does not mean a patient will not receive care but will instead be transported to a closer hospital that in an inclusive trauma system would simply be a lower level trauma center (i.e., a level III or IV trauma center).
Any discussion of triage accuracy must consider the outcome that is being used as a gold standard. The Resources for Optimal Care of the Injured Patient 2006 document suggests using Injury Severity Score as a measure of trauma center need.2 However, there is no universally accepted gold standard for trauma center need and there are studies which have shown the identified accuracy of Field Triage Decision Scheme changes depending on how trauma center need is defined.6 We chose to use a composite measure as our outcome, but acknowledge that our findings would be slightly modified if we used an injury severity score greater than 15 as our outcome.
When a severely injured patient is not identified (i.e., under-triaged) that patient may be taken to a non-trauma center or a lower level trauma center and this can have negative patient effects by increasing their risk of morbidity and mortality. This was demonstrated by MacKenzie et al who found that transport of severely injured patients to a trauma center reduced mortality.7 Therefore, even this slight increase in under-triage that resulted from using the 2006 scheme has negative implications for patient outcome. On the other hand, over-triage can have negative patient effects and negative system effects. The patient effects are related to potential safety issues related to mode of transport. These patients are more likely to be transported by helicopter or by a ground ambulance traveling with lights and siren. Both of these modes of transport are associated with an increased crash risk.8-10 There are also several system affects. Ambulance out of service times will be increased because of the increased transport times that result from by-passing closer hospitals. By-passing closer hospitals may also have negative economic consequences for the by-passed hospital. Finally, more patients being transported to the trauma center may contribute to emergency department crowding at the trauma center. Communities need to weigh the risks associated with under-triage against those associated with over-triage.
There are limited data supporting the Field Triage Decision Scheme in general.3, 6 The Field Triage Decision Scheme has been modified at regular intervals since its inception in 1987 using the best available evidence and expert opinion, but more evidence is needed to continue the refinement of this valuable tool and improve its accuracy. The majority of changes between the 1999 scheme and the 2006 scheme were to the mechanism of injury criteria. These criteria have long been debated and their utility questioned.3, 11 Consideration should be given to using new technologies for determining the forces that were sustained by an injured patient such as automatic crash notification to further improve knowledge of the injury event, which may lead to better resource need predictions.12
Limitations
Our data collection form had two limitations. Due to an oversight on our data collection form, we did not collect information on crushed, degloved and mangled extremities, which may have resulted in our under-estimating the number of patients who met the 2006 scheme. We also were not able to determine if penetrating injuries were proximal to the knee or elbow; only that there was a penetrating injury. This may have lead to an over-estimation of patients who met both the 1999 and 2006 scheme, since we considered any penetrating injury to meet the criteria regardless of location.
This study was not able to look at a community based sample. We instead studied the broad spectrum of injured patients brought to a single large tertiary care hospital in each community that was also the regional trauma center. By using these centers we were able to ensure that the care provided and resources available at the study hospitals were relatively standardized but it is possible that patients brought to these hospitals who were not identified by local trauma protocols were different from injured patients that are brought to other hospitals. We did conduct random interviews of providers to determine the characteristics of injured patients brought to other facilities and we did not find any obvious differences in their characteristics.
A fundamental limitation of any triage study is the use of a validated outcome measure, which doesn’t exist for trauma triage. Our outcome measure (urgent non-orthopedic surgery within 24 hours of ED arrival, admission to the intensive care unit, and/or death prior to discharge), represents a best consensus of the literature.6
Conclusion
Use of the 2006 Field Triage Decision Scheme would have resulted in a significant decrease in the number of patients identified as needing a trauma center. These changes reduced over-triage while causing only a small increase in the number of patients who would be under-triaged.
Acknowledgments
Funding: This project was supported by grant: 5R49CE001010 from the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC. Dr. Shah is supported by the Paul B. Beeson Career Development Award (NIA 1K23AG028942).
Footnotes
The authors have no financial conflicts of interest to report.
Presented: Society for Academic Emergency Medicine Annual Meeting, New Orleans, LA; May 2009
References
- 1.Mackersie RC. History of Trauma Field Triage Development and the American College of Surgeons Criteria. Vol. 10. Informa Healthcare; 2006. pp. 287–294. [DOI] [PubMed] [Google Scholar]
- 2.Committee on Trauma American College of Surgeons . Resources for Optimal Care of the Injured Patient 2006. American College of Surgeons; Chicago, IL: 2006. [Google Scholar]
- 3.Sasser SM, Hunt RC, Sullivent EE, et al. Guidelines for field triage of injured patients. Recommendations of the National Expert Panel on Field Triage. MMWR Recomm Rep. 2009 Jan 23;58(RR-1):1–35. [PubMed] [Google Scholar]
- 4.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989 Apr;27(4):412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Rutledge R. Injury severity and probability of survival assessment in trauma patients using a predictive hierarchical network model derived from ICD-9 codes. J Trauma. 1995 Apr;38(4):590–597. doi: 10.1097/00005373-199504000-00022. discussion 597-601. [DOI] [PubMed] [Google Scholar]
- 6.Lerner EB. Studies evaluating current field triage: 1966-2005. Prehosp Emerg Care. 2006 Jul-Sep;10(3):303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 7.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 8.Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of Fatal Ambulance Crashes in the United States: an 11-Year Retrospective Analsysis. Prehospital Emergency Care. 2001;5(3):261–269. doi: 10.1080/10903120190939751. [DOI] [PubMed] [Google Scholar]
- 9.Rhee KJ, Holmes EM, 3rd, Moecke HP, Thomas FO. A comparison of emergency medical helicopter accident rates in the United States and the Federal Republic of Germany. Aviat Space Environ Med. 1990 Aug;61(8):750–752. [PubMed] [Google Scholar]
- 10.Saunders CE, Heye CJ. Ambulance collisions in an urban environment. Prehosp Disaster Med. 1994 Apr-Jun;9(2):118–124. doi: 10.1017/s1049023x00041017. [DOI] [PubMed] [Google Scholar]
- 11.Brasel KJ, Nirula R. What mechanism justifies abdominal evaluation in motor vehicle crashes? J Trauma. 2005 Nov;59(5):1057–1061. doi: 10.1097/01.ta.0000187798.37920.4c. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Injury Prevention and Control . Recommendations from the Expert Panel: Advanced Automatic Collision Notification and Triage of the Injured Patient. Centers for Disease Control and Prvention; Atlanta, GA: 2008. [Google Scholar]


