Abstract
Objective
Most smoking cessation studies use long-term abstinence as their primary outcome measure. Recent research suggests that long-term abstinence may be an insensitive index of important smoking cessation mechanisms. The goal of the current study is to examine the effects of five smoking cessation pharmacotherapies using Shiffman et al.'s (2006) approach of examining the effect of smoking cessation medications on three process markers of cessation or smoking cessation “milestones”: initial abstinence, lapse, and the lapse-relapse transition.
Method
The current study (N = 1504, 58% female, 84% Caucasian) examines the effect of five smoking cessation pharmacotherapy treatments vs. placebo (bupropion, nicotine lozenge, nicotine patch, bupropion + lozenge, patch + lozenge) on Shiffman et al.'s smoking cessation milestones over 8 weeks following a quit attempt.
Results
Results show that all five medication conditions decreased rates of failure to achieve initial abstinence and most (with the exception of the nicotine lozenge) decreased lapse risk, however only the nicotine patch and bupropion + lozenge conditions affected the lapse-relapse transition.
Conclusions
These findings demonstrate that medications are effective at aiding initial abstinence and decreasing lapse risk, but generally do not decrease relapse risk following a lapse. The analysis of cessation milestones sheds light on important impediments to long-term smoking abstinence, suggests potential mechanisms of action of smoking cessation pharmacotherapies, and identifies targets for future treatment development.
Much smoking cessation research has used long-term abstinence to evaluate the efficacy of cessation treatments. Recently, Shiffman and colleagues (2006) introduced the notion that successful cessation may be viewed as being dependent upon several component events that they term “milestones.” These include: ability to stop smoking (achieve short-term abstinence), avoid a lapse (smoking on a single day), and if a lapse occurs, avoid a relapse (a return to daily smoking; Shiffman et al., 2006). Parsing the multicomponential process of smoking cessation into meaningful subunits may provide insight into the process of cessation and relapse, and provide guidance for the development and administration of smoking cessation treatments. The current study evaluates the effects of five smoking cessation pharmacotherapy treatments on smoking cessation milestones.
The majority of smoking cessation research has focused on a single type of outcome, long-term abstinence, defined as the absence of smoking within a period of one week prior to a distant follow-up time point (e.g., at 6-months after a quit attempt; Hughes et al., 2003). Recent research suggests that this type of outcome reflects an amalgam of different cessation events or processes (Piasecki, Fiore, McCarthy, & Baker, 2002; Piasecki, 2006; Shiffman et al., 2006) that are rarely explored in cessation studies. For example, most studies do not establish whether participants were able to quit (i.e., abstain from smoking for at least 24 hours) during a cessation attempt. In addition, many studies do not separate out those smokers who lapsed and then returned to abstinence from those who lapsed and then reverted to regular smoking (i.e., relapsed). Thus, long-term abstinence, as it has been measured, may be an insensitive outcome by which to measure relations between cessation treatments and cessation processes (Piasecki et al., 2002; Piasecki, 2006; Shiffman et al., 2006).
Smoking Cessation Milestones
As noted above, Shiffman et al. (2006) suggest three discriminable smoking cessation events: achieving initial abstinence, lapsing, and the lapse-relapse transition. They argue that these “milestones” may reflect the influence of different causal processes that might be differentially sensitive to treatments. In support of this hypothesis, Shiffman et al. found that the high-dose nicotine patch had a larger effect on the transition from lapse to relapse than on other milestones (although being on the active high-dose patch treatment was associated with achievement of all milestones).
The aim of the current research is to characterize the effects of different smoking cessation pharmacotherapies on smoking cessation milestones. While Shiffman et al. (2006) contributed to our understanding of how one treatment affects abstinence outcomes, their work had limitations. First, it examined only one investigational treatment (high-dose nicotine patch). The current work examines five pharmacotherapy treatments, several of which are in widespread use. If milestones reflect different causal influences, and treatments vary in mechanisms, treatments may differ in their relations with milestones. For instance, this research tests two combination pharmacotherapies that have been shown to be significantly more effective than monotherapies in producing long-term abstinence (Piper et al., 2009; Smith et al., 2009). The current research will allow us to conduct relatively fine grained analyses regarding the source of any added benefit of combination pharmacotherapies (e.g., higher initial cessation, lower lapse rates). Second, Shiffman et al. examined smoking cessation milestones for a relatively brief interval after the quit attempt (5 weeks). Some cessation processes (e.g., the resolution of a lapse) may unfold over an extended period of time; a longer period of study may yield more informative results. Third, the Shiffman et al. study had fairly high drop-out (21% before treatment; 28% during treatment).
Treatment and Prediction of Cessation Milestones
The current study uses the Shiffman et al. (2006) paradigm to evaluate treatment effects on cessation milestones in individuals receiving one of five pharmacotherapy treatments vs. placebo: the nicotine patch, the nicotine lozenge, bupropion, bupropion + nicotine lozenge or nicotine patch + nicotine lozenge. These pharmacotherapies might produce different effects on the milestones, in part, because of differences in dosing parameters and therapeutic mechanism. Bupropion is started one week prior to the quit date to reach a therapeutic dose of the drug before the quit attempt (Hurt et al., 1997). Nicotine replacement therapies (NRTs) are generally started on the quit day. Therefore, while any of the medications might increase initial cessation, bupropion might produce higher rates of initial abstinence than NRTs because individuals initiate quit attempts with therapeutic levels of drug in the body. As Shiffman et al. (2006) noted, lapsing is often associated with exposure to smoking cues (Caggiula et al., 2001; Caggiula et al., 2002; Conklin, 2006; Conklin, Robin, Perkins, Salkeld, & McClernon, 2008; McCarthy, Piasecki, Fiore, & Baker, 2006; Shiffman, 2006). This suggests that PRN medications (e.g., the nicotine lozenge) might show strong effects on lapsing since they could be taken during high risk situations (e.g., during a stressful event). Finally, non-PRN pharmacotherapies are purported to work by reducing the rewarding properties of cigarettes (West, Baker, Cappelleri, & Bushmakin, 2008). This hypothesis is consistent with the Shiffman et al. (2006) finding that the high-dose nicotine patch was effective at reducing the risk of transition from lapse to relapse. The simple dosing parameters of non-PRN treatments may promote adherent use and more consistent therapeutic levels of drug when lapses occur. In sum, non-PRN pharmacotherapies (i.e., bupropion; nicotine patch) could decrease the risk of transition from lapse to relapse more effectively than do other agents.
Combination pharmacotherapies produce greater long-term abstinence rates than do monotherapies in head-to-head comparisons (Fiore et al., 2008; Piper et al., 2007; Smith et al., 2009). In this study, the combination pharmacotherapies comprise both PRN and non-PRN administration schedules, increasing the likelihood that the combinations may significantly affect all milestones. Further, the combinations might be superior to monotherapies by producing higher doses of the therapeutic agent (the nicotine patch + lozenge) or delivering multiple agents (bupropion + lozenge). Therefore, the combination treatments may be effective at boosting success rates at each milestone.
In sum, we hypothesized that, compared to placebo: 1) bupropion will increase initial abstinence rates; 2) the nicotine lozenge will reduce lapse risk; 3) bupropion and nicotine patch will reduce relapse risk following a lapse; and 4) combination pharmacotherapies (bupropion + lozenge, patch + lozenge) will produce beneficial effects relative to the monotherapies at each of the milestones (e.g., increase initial abstinence rates, reduce lapse risk and reduce relapse risk following a lapse).
Method
Participants
Participants were 1504 smokers (58% female, 83% Caucasian; see Table 1 for demographics) from Southeastern WI, participating in clinical trial (Piper et al., 2009). Participants were recruited via TV, radio and newspaper advertisements, flyers, and media coverage. Inclusion criteria included smoking greater than nine cigarettes per day for the past 6 months and being motivated to quit smoking. Exclusion criteria included medical contraindications to study medications, including heavy alcohol consumption (six drinks per day on six or seven days of the week), history of seizure, schizophrenia, psychosis, an eating disorder, or bipolar disorder. In addition, participants could not be pregnant or breast-feeding and must have agreed to use adequate contraception. All participants were treated ethically. This study was approved by the University of Wisconsin Heath Sciences Institutional Review Board.
Table 1.
Demographics and Descriptive Statistics
| Measure | ||
|---|---|---|
| Gender | % Female | 58.2 |
| Education | % <High School | 5.6 |
| % High School | 23.6 | |
| % Some College | 48.4 | |
| % ≥ College | 21.9 | |
| Marital Status | % Married/Live-in Partner/ Widowed | 56.8 |
| % Divorced/Separated | 24.2 | |
| % Never Married | 18.6 | |
| Race | % Caucasian | 83.9 |
| % African American | 13.6 | |
| % Other | 2.5 | |
| Age | M (SD) | 44.7 (11.1) |
| Cigarettes per Day | M (SD) | 21.4 (8.9) |
| # of Previous Quit Attempts | M (SD) | 5.7 (9.7) |
| Fagerström Test for Nicotine | M (SD) | 5.4 (2.1) |
| Dependence | ||
Procedure
Potential participants called into a central office to complete a phone screen. Those eligible were invited to an information session where they provided written, informed consent. Next, participants attended a screening visit where they were evaluated for possible exclusion criteria based on a medical history screening, vital signs measurements (blood pressure over 160 systolic and/or 100 diastolic), and a carbon monoxide (CO) breath test. Additionally, participants completed several demographic, smoking history, and tobacco dependence questionnaires (e.g., the FTND; Heatherton, Kozlowski, Frecker, & Fagerstrom, 1991). If participants met inclusion criteria, they completed two baseline sessions. During the first baseline session, participants completed additional assessments (e.g., a social network interview). At the second baseline session, participants came to the clinic after abstaining from cigarettes overnight in order to conduct medical assessments (e.g., serum lipid profiles, carotid intima media ultrasound, hemoglobin A1C).
Upon successful completion of the baseline assessment sessions, participants were randomized in a double-blinded fashion blocked on gender and race (white/non-white). In addition to pharmacotherapy, all participants received 6 one-on-one counseling sessions based on the PHS guideline (e.g., decreasing smoking cues, increasing social support for non-smoking, Fiore et al., 2000) lasting 10-20 minutes. Study staff who provided counseling and conducted study sessions were bachelor-level, trained case managers supervised by a licensed clinical psychologist. Counselors were blind to placebo condition status (e.g., active patch vs. placebo patch), but not to medication type (e.g., bupropion vs. patch). Sessions occurred during 7 weeks with the first counseling session occurring 1 week before the quit day and the subsequent 5 occurring on the quit day and a 1-, 2-, 4, and 8-weeks post quit.
The baseline visits occurred between 8 and 15 days pre-quit. Study visits occurred 1 week pre-quit, on the quit day, and 1-, 2-, 4- and 8-weeks post quit.
Treatment
Participants were randomized to one of six treatment conditions: 1) bupropion SR (150 mg, bid for 9 weeks total: 1 week pre-quit and 8 weeks post-quit); 2) nicotine lozenge (recommended use of nine 2 or 4 mg lozenges per day, based on appropriate dose for dependence level per package instructions, for 12 weeks post-quit); 3) nicotine patch (24-hour patch; 21, 14, and 7mg; titrated down over 8 weeks post-quit); 4) nicotine patch + nicotine lozenge combination therapy; 5) bupropion SR + nicotine lozenge combination therapy; or 6) placebo. Use instructions were consistent with the FDA approved package insert instructions and lozenge use instructions were the same when it was used as either a monotherapy or in a combination therapy condition. Those in the placebo condition were randomly assigned to one of five placebo conditions that matched the active treatments, with 1/5th of participants receiving each condition (e.g., placebo bupropion, lozenge, patch, patch + lozenge and bupropion + lozenge). There were no statistically significant differences between the active and placebo treatment groups on age, cigarettes smoked per day, FTND score, baseline CO level, gender, marital status, race, Hispanic origin, or education. Consistent with the FDA package instructions, participants on nicotine replacement products such as lozenge and patch were instructed not to smoke while using nicotine replacement therapy (e.g., to remove the nicotine patch before smoking a cigarette).
Smoking status
Smoking status was collected using a smoking calendar whereby, at each contact, participants reported on their smoking each day since the last contact using time-line follow-back (Brigham et al., 2008; Sobell, Sobell, Leo, & Cancilla, 1988). This differs from Shiffman et al., 2006 in that Shiffman et al. used ecological momentary assessment (EMA) to collect daily smoking data. However, the timeline follow-back procedure appears to be highly sensitive to whether or not people smoke (such as lapsing or relapsing), even though it is not as sensitive to fine grained patterns of smoking as is the EMA method (Lewis-Esquerre, Colby, Tevyaw, Eaton, Kahler, & Monti, 2005; Shiffman, 2009). Seven-day point-prevalence abstinence (“Have you smoked at all, even a puff, in the last seven days?”) was assessed during the 8-week visit. Self-reports of smoking status were confirmed by a CO rating (<10 ppm). Follow-up interviewers were blind to treatment condition.
Data Analysis
Outcome variables
Three of the outcome variables were computed using the smoking calendar data. Participants were coded as having achieved initial abstinence if an individual reported smoking zero cigarettes on one or more days during the first 14 days of the study.1 The lapse variable was computed using only those individuals who achieved initial abstinence and was defined as the number of days between the first day where the participant smoked zero cigarettes and the first day where he or she smoked any amount (Shiffman et al., 2006). If individuals did not lapse, their lapse variable indicated the time from their quit day until the end of the 8-week follow-up period. If individuals withdrew from the study before lapsing, their lapse variable indicated the number of days from the quit day until the withdrawal date. Finally, the relapse variable was computed for all individuals who lapsed. The relapse variable was defined as the number of days from the lapse day until relapse day (the first of seven consecutive days of smoking; Shiffman et al., 2006). If individuals lapsed but did not relapse, their relapse variable indicated the number of days from their lapse date until the end of the 8 week follow-up period. If they lapsed but withdrew from the study before relapsing, their relapse variable indicated the number of days from their lapse date until their withdrawal date. The results of these analyses were compared to CO-confirmed 7-day point-prevalence abstinence at 8 weeks post target quit date. It should be noted that the post-prevalence abstinence results were reported in the main outcome paper from this dataset (Piper et al., 2009). This study had an a priori power of 0.88 to detect a clinically significant improvement in point-prevalence abstinence rates of 12%.
Tests of milestones
Analyses of initial abstinence were conducted using logistic regression. Failure to achieve initial cessation was coded as “1” and achieving initial cessation was coded as “0”. Thus, odds ratios below one indicate variables that improved rates of achievement of initial abstinence. Analyses of lapse and relapse were conducted using Cox proportional hazards regression survival analysis2. Because proportional hazards regression results are interpreted as the risk of having an event (e.g., lapse) over time, results will be discussed in terms of lapse risk and lapse-relapse risk (the risk of a relapse following a lapse). Individuals were censored from the analysis at the time of their last contact (e.g., their withdrawal date) if they did not have an event (e.g., lapse); all other participants who did not have an event were censored at the end of the follow-up period (8 weeks). In all of the survival analyses having an event (e.g., lapse, relapse) was coded as “0”; hazard ratios below one are interpreted as beneficial for cessation.
We used an 8-week follow-up period because all treatments lasted at least 8 weeks post-quit (the lozenge treatment lasted 12 weeks). This time point captures the longest time period at which intra-treatment data were gathered for all active treatments. Because the goal of this research is to understand how medications influence the milestones, we will not report milestone outcomes after the medication had been discontinued. In support of this decision, when we examined the effect of the medication conditions on smoking cessation milestones during the 6-month follow-up period, the pattern of results was similar, though the effects were somewhat weaker.
Interactions with time
To test the Cox proportional hazards assumption and to determine whether the effect of treatment varied throughout the quit attempt, we examined interactions with time for the survival analyses. We computed the interaction between treatment condition and a variable representing time (e.g., Bupropion X days-to-lapse). Only significant interactions with time will be reported.
Differential efficacy of pharmacotherapy treatments
All active medication conditions were compared with the placebo condition for each milestone. In addition, based on a priori hypotheses that the combination pharmacotherapies would be superior to the monotherapies, we conducted planned comparisons between a composite variable coding all the monotherapies and a composite variable coding the combination treatments with the monotherapy condition as the reference group for each milestone. In addition, we compared the combination treatments with one another, with the bupropion + lozenge condition as the reference group.
Results
Achievement of milestones
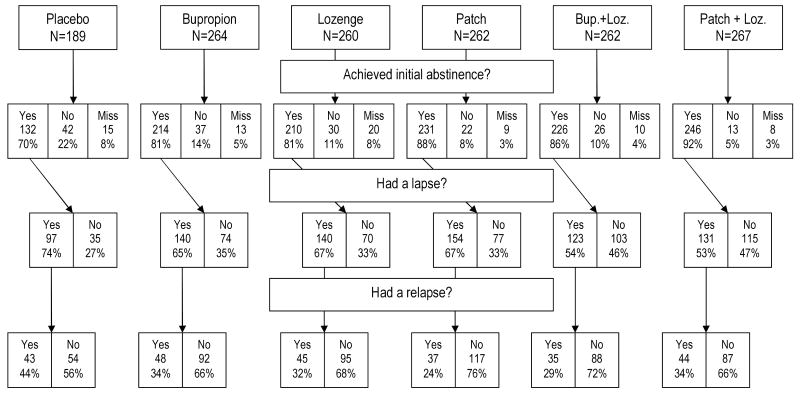
Of the 1504 smokers enrolled in the study, 1429 had complete calendar data for the first 14 days. Of those 1429, 1259 (88.1%) achieved initial abstinence (M days to initial abstinence = .71, SD = 2.23, median=0, mode=0). Of the 1259 who achieved initial abstinence, 785 (62.4%) had a lapse (M = 11.54 days, SD = 14.63; median = 5 days, mode = 1 day). Of those 785 who lapsed, 252 (32.1%) relapsed (days to relapse M = 21.66, SD = 17.04, median=17, mode=2; number of days from lapse to relapse M = 7.49, SD = 7.80, median=6, mode=0). As reported in Piper et al., 2009, number and percentage rates of withdrawal from the study by treatment group during the treatment period were: 9 (3% for patch), 17 (7%) for lozenge, 6 (2%) for patch + lozenge, 9(6%) for bupropion, 9 (3%) for bupropion + lozenge, 13 (7%) for placebo. Progression through the milestones by treatment condition is detailed in Figure 1.
Figure 1.
Progression through smoking cessation milestones by treatment condition.
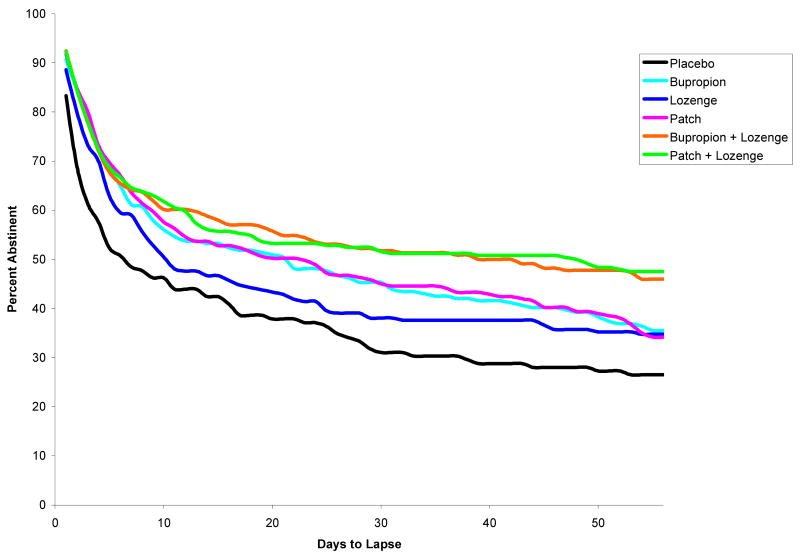
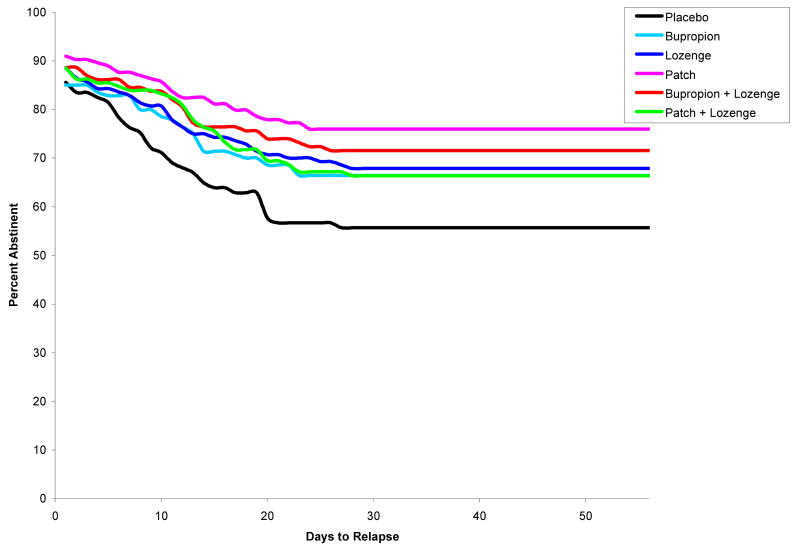
Treatment
Treatment was dummy-coded for analysis. The comparison group was a combined group of all of the placebo conditions. Dummy-coded treatment variables were entered together as a set into the models for each of the outcomes. The results for each medication will be discussed separately (see Table 2 for hazard ratios, p-values and confidence intervals; see Figure 2 for lapse survival curves; see Figure 3 for relapse survival curves)3.
Table 2.
| Medication | Failure to Reach Initial Abstinence (n=1429) |
Lapsec (n=1259) |
Relapsed (n=785) |
8 Week Point-Prevalence Abstinence (N=1504) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | p | 95% CI |
HR | p | 95% CI |
HR | p | 95% CI |
OR | p | 95% CI |
|
| Bupropion | .54* | .02 | .33-.89 | .74* | .02 | .57-.96 | .76 | .18 | .50-1.14 | .64* | .03 | .43-.96 |
| Lozenge | .45* | .002 | .27-.75 | .80 | .10 | .62-1.04 | .68 | .08 | .45-1.04 | .64* | .03 | .43-.95 |
| Patch | .30* | <.001 | .17-.52 | .74* | .02 | .58-.96 | .52* | .003 | .33-.80 | .54* | .002 | .36-.79 |
| Bupropion + Lozenge | .36* | <.001 | .21-.62 | .58* | <.001 | .45-.76 | .59* | .02 | .38-.92 | .43* | <.001 | .29-.63 |
| Patch + Lozenge | .17* | <.001 | .09-.32 | .57* | <.001 | .44-.75 | .71 | .11 | .47-1.08 | .38* | <.001 | .25-.56 |
Note. OR = Odds Ratio; HR = Hazards Ration; CI = Confidence Interval
All significant effects remained significant after applying a Holm alpha correction for multiple comparisons, with the exception of the bupropion + lozenge condition predicting the lapse-relapse transition.
All HRs and ORs refer to comparisons between medication and placebo.
Excludes individuals who did not achieve initial abstinence.
Excludes individuals who did not lapse.
Figure 2.
Days to lapse by treatment condition.
Figure 3.
Days from lapse to relapse by treatment condition.
Bupropion
Relative to placebo, bupropion reduced rates of failure to achieve initial abstinence, and decreased lapse risk. Bupropion did not predict lapse-relapse risk. Bupropion reduced point-prevalence smoking rates relative to placebo.
Nicotine Lozenge
Relative to placebo, the nicotine lozenge reduced rates of failure to achieve initial abstinence. Nicotine lozenge did not significantly decrease lapse risk nor did it predict lapse-relapse risk. The nicotine lozenge reduced point-prevalence smoking rates relative to placebo.
Nicotine Patch
Relative to placebo, the nicotine patch reduced rates of failure to achieve initial abstinence, decreased lapse risk and lapse-relapse risk. There was a significant interaction between nicotine patch and time to lapse such that nicotine patch was less effective at preventing lapse later in the follow-up period (HR = 5.11, 95% CI = 1.001-1.01). The nicotine patch reduced point-prevalence smoking rates relative to placebo.
Bupropion + Lozenge
Relative to placebo, bupropion + lozenge reduced rates of failure to achieve initial abstinence, and decreased lapse risk and lapse-relapse risk. Bupropion + lozenge decreased point-prevalence smoking rates relative to placebo.
Patch + Lozenge
Relative to placebo, patch + lozenge reduced rates of failure to achieve initial abstinence, and decreased lapse risk. Patch + lozenge did not predict lapse-relapse risk. Patch + lozenge decreased point-prevalence smoking rates relative to placebo.
Differential Efficacy of Pharmacotherapy Treatments.
Initial Abstinence
The combination treatments produced significantly lower rates of failure to achieve initial abstinence than did the monotherapies (OR = .61, 95% CI = .41-.90). Patch + lozenge produced significantly lower rates of failure to achieve initial abstinence than did the bupropion + lozenge (OR= .46, 95% CI = .23-.92).
Lapse
The combination treatments produced lower lapse risk than did the monotherapies (HR = .76, 95% CI = .65-.89), but did not differ from one another (p>.05).
Relapse
The combination treatments and monotherapies did not differ in reducing lapse-relapse risk (p>.05), and did not differ from one another (p>.05).
Point-prevalence abstinence
The combination treatments yielded lower point-prevalence smoking rates than did the monotherapies (OR = .66, 95% CI = .53-.83), but did not differ from one another (p>.05).
Discussion
The guiding hypothesis of this study is that examination of meaningful components of the cessation process, or milestones (i.e., establishing initial abstinence, lapsing, and relapsing), can illuminate how treatments influence the transition from regular smoking to long-term abstinence. As was reported previously (Piper et al., 2009), all tested medications increased 8-week point-prevalence abstinence rates when compared to placebo, with combination treatments producing significantly higher abstinence rates than did the monotherapies. The examination of cessation milestones revealed important information about the how these various medications resulted in these net effects on point-prevalence abstinence.
All the pharmacotherapy treatments increased the likelihood of initial cessation. As predicted, the combination therapies were particularly effective at producing high initial abstinence rates. The patch + lozenge combination was especially effective, producing initial abstinence rates that were significantly higher than those produced by the nicotine lozenge alone, bupropion alone, and the bupropion + lozenge combination. It was predicted that bupropion would produce the highest abstinence rates. However, while bupropion did increase initial abstinence relative to placebo treatment, it was far from the most effective agent. This may be because individuals were allowed 14 days to achieve initial abstinence, making the prequit administration of bupropion less important. On the other hand, nicotine replacement may be more effective than bupropion at reducing risk factors for early cessation failure such as craving and withdrawal.
Most smoking cessation medications were effective in reducing lapse risk following cessation, but the combination treatments tended to be more effective than the monotherapies (see Table 2). Contrary to predictions, the nicotine lozenge alone did not reduce lapse risk at 8 weeks post-quit. This could be due to adherence. Perhaps, as found in other studies of PRN nicotine replacement therapies (Fortmann & Killen, 1995; Glover et al., 1996; Goldstein, Niaura, Follick, & Abrams, 1989), few participants took enough lozenges to reach a therapeutic dose. It is important to note that the nicotine lozenge did boost the efficacy of bupropion and the nicotine patch when taken in combination (Table 2). Also, while the nicotine lozenge demonstrated significant increases in 8-week point-prevalence abstinence relative to placebo, it appears to exert these effects by increasing initial abstinence rates, not by decreasing risks of lapse or relapse.
While the cessation medications, on the whole, did influence initial cessation and lapse risk, few of them were significantly associated with the risk of relapse following a lapse. Only the nicotine patch and the bupropion + lozenge combination reduced relapse risk following a lapse during the 8-week treatment period. Bupropion alone, lozenge alone and the patch + lozenge combination treatment did not affect the lapse-relapse transition. The finding that the medications produced relatively weak effects on relapse risk after a lapse was surprising given that Shiffman et al., (2006) found that this was the milestone most affected by high-dose nicotine patch. A comparison of the effect sizes in the two studies illustrates the differences in findings. In Shiffman et al, those on the high-dose nicotine patch were 1.3 times more likely to achieve initial abstinence, whereas in our study those in the medication conditions were 1.85 (bupropion)-5.8 times (patch + lozenge) more likely to achieve initial abstinence than were those on placebo. The medications in the current study showed similar effect sizes to the Shiffman et al. study with respect to reducing lapse risk (Shiffman et al. 1.60 vs. 1.25 [lozenge]-1.75 [patch + lozenge] in our study), but smaller effects with regard to lapse-relapse transition. In the Shiffman et al., study, those taking placebo were 4.8 times more likely to relapse following a lapse than were those on the high-dose nicotine patch, whereas in our study those on placebo were 1.31 (bupropion) – 1.92 (patch) times more likely to relapse than were those in the active medication conditions. Therefore, in the present research the five medications exerted relatively large effects on attainment of initial abstinence, and more modest effects on preventing relapse.
Differences in the pattern of results in the two studies could be due to multiple factors. For example, differences in duration of the follow-up period analyzed might have affected the results. It is also possible that the high dose nicotine patch is particularly effective in reducing lapse-relapse progression. Also, an absence of statistically significant effects on relapse rates in the present study can be attributed, in part, to low statistical power, since only lapsers were available for such analyses However, an examination of effect sizes shows that the interventions all exerted larger effects on the early, initial abstinence mark than on the later outcomes (e.g., the lapse-relapse latency).
It is important to note that, when we examined effects over 6 months post-quit (rather than 8 weeks), the pattern of results was similar, but the effects were weaker. For instance, prediction of lapse remained significant for all treatment conditions, but none of the treatment conditions was associated with the risk of a relapse following a lapse. Thus, across both durations of follow-up, the general pattern of results is consistent with earlier suggestions that the beneficial effects of cessation medications tend to be manifested early in the course of treatment (e.g., in facilitating the initial achievement of abstinence; see Hughes, Gust, Keenan, Fenwick, & Healey, 1989; Hughes & Callas, 2006; Piasecki et al., 2002), and that once treatment has ended, treatment effects abate (Medioni, Berlin, & Mallet, 2005).
Implications for Treatment
The above findings have relevance for smoking cessation treatment. Our data suggest that early cessation success may provide a highly informative surrogate outcome for evaluating cessation medications, one that permits efficient, early evaluation of treatments and that permits treatment adjustment based upon initial effects (e.g., in accordance with a sequential multiple assignment randomized trial design in which treatment is altered if an individual does not achieve initial abstinence; Murphy, 2005). The present findings also underscore the need to develop treatments that more effectively reduce relapse likelihood following a lapse.
Limitations and Future Directions
The method of examining milestones for only individuals who reached a previous milestone may introduce bias in the data when comparing across conditions. For example, if one medication were particularly good at helping smokers achieve initial abstinence, then the smokers entered into the lapse analyses in this condition may differ in important ways from those entered into that analysis for the placebo condition. Therefore, after the initial cessation analysis, it is possible that the treatments were not being compared using a level playing field. For instance, the nicotine patch + lozenge condition may have had relatively weak effects on relapse because it was so effective in preventing lapses: i.e., only the most vulnerable individuals lapsed with this treatment and therefore they were especially susceptible to eventual, full relapse. This problem makes it difficult to compare treatments on the later milestones and reduces the strength of inferences from such inter-treatment contrasts. Also, adherence to medications may have been an issue for analyses of later time points, particularly after participants began to lapse. This may have been compounded by the package instructions for nicotine replacement therapies that told patients not to smoke while using these medications, which may have encouraged discontinuation of medication use. We had limited ability to assess adherence in this research because medication adherence data were collected only at visits, and these occurred infrequently at later time-points. Also, the current research examined only a subset of cessation medications; it will be important to use milestones to examine additional medications such as varenicline. One additional limitation is that some smoking measures (e.g., relapse date) were not individually verified using biochemical confirmation. However, point prevalence reports of smoking were consistently validated by CO assays, and relapse status (among those who lapsed) evaluated at 6 months was correlated with CO-confirmed point-prevalence abstinence r=.51, p <.001.
Summary and Conclusions
This research yielded the following findings. (1) Smoking cessation medications are quite effective at promoting initial abstinence and reducing lapse risk, but the evidence is weaker that they prevent a transition from lapse to relapse. (2) The combination pharmacotherapies tested tended to be superior to the monotherapies in boosting attainment of initial abstinence and prevention of lapse. The nicotine patch + lozenge was superior to bupropion + lozenge in producing initial abstinence.
A final observation is that an examination of milestones did afford useful information that could not be inferred from point-prevalence abstinence rates per se. For instance, these analyses revealed that large differences in point-prevalence abstinence observed at 8 weeks post-quit can be attributed, in good part, to effects on initial cessation that occur within two weeks of the quit attempt (see Figure 1). Conversely, treatments that differ greatly on 8 week point-prevalence abstinence are essentially equivalent in terms of protecting against lapse-relapse progression. Therefore, the results presented in this paper, as well as those produced by Shiffman et al., (2006) support the utility of this more comprehensive approach to understanding the process of relapse and identifying where in this process treatments are exerting their effects.
Acknowledgments
This research was conducted at the University of Wisconsin-Madison and was supported by grant #P50 DA019706 from NIH/NIDA; by grant #M01 RR03186 from the General Clinical Research Centers Program of the National Center for Research Resources, NIH; by an Institutional Clinical and Translational Science Award (UW-Madison; KL2 Grant # 1KL2RR025012-01); and by grant #s 1K05CA139871 and K08DA025041 from the NIH. Medication was provided to participants at no cost under a research agreement with GlaxoSmithKline (GSK); no part of this manuscript was written or edited by anyone employed by GSK.
Footnotes
In the Shiffman et al. (2006) study, participants were given the entire length of the study (5 weeks) to achieve initial abstinence. However, because of the longer length of our study, we chose to limit the period for quitting to 2 weeks so as not to count fortuitous causes of abstinence for reasons such as hospitalization, international plane flights, etc.
We also conducted Kaplan-Meier survival analyses. Because the results did not differ we will only report the Cox proportional hazards regression results.
Data analyses were conducted with and without controlling for gender and nicotine dependence (FTND score). The results did not change when covariates were entered. The unadjusted results are reported in Table 2.
The authors are solely responsible for the analyses, content, and writing of this article. The authors have full control of all primary data, and they agree to allow the journal to review the data if requested.
We declare that this research complies with the current laws of the United States of America. All participants gave written informed consent, and the study was approved by the Institutional Review Board.
References
- Brigham J, Lessov-Schlaggar CN, Javitz HS, McElroy M, Krasnow R, Swan GE. Reliability of adult retrospective recall of lifetime tobacco use. Nicotine & Tobacco Research. 2008;10:287–299. doi: 10.1080/14622200701825718. [DOI] [PubMed] [Google Scholar]
- Caggiula AR, Donny EC, Chaudhri N, Perkins KA, Evans-Martin FF, Sved AF. Importance of nonpharmacological factors in nicotine self-administration. Physiology & Behavior. 2002;77:683–7. doi: 10.1016/s0031-9384(02)00918-6. [DOI] [PubMed] [Google Scholar]
- Caggiula AR, Donny EC, White AR, Chaudhri N, Booth S, Gharib MA, et al. Cue dependency of nicotine self-administration and smoking. Pharmacology Biochemistry & Behavior. 2001;70:515–30. doi: 10.1016/s0091-3057(01)00676-1. [DOI] [PubMed] [Google Scholar]
- Conklin CA. Environments as cues to smoke: implications for human extinction-based research and treatment. Experimental & Clinical Psychopharmacology. 2006;14:12–19. doi: 10.1037/1064-1297.14.1.12. [DOI] [PubMed] [Google Scholar]
- Conklin CA, Robin N, Perkins KA, Salkeld RP, McClernon FJ. Proximal versus distal cues to smoke: the effects of environments on smokers' cue-reactivity. Experimental & Clinical Psychopharmacology. 2008;16:207–214. doi: 10.1037/1064-1297.16.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, et al. Clinical Practice Guideline. Rockville, MD: U.S.: Department of Health and Human Services. Public Health Service; May, 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- Fortmann SP, Killen JD. Nicotine gum and self-help behavioral treatment for smoking relapse prevention: Results from a trial using population-based recruitment. Journal of Consulting and Clinical Psychology. 1995;63:460–468. doi: 10.1037//0022-006x.63.3.460. [DOI] [PubMed] [Google Scholar]
- Glover ED, Sachs DPL, Stitzer ML, Rennard SI, Wadland WC, Pomerleau OF, Nowak RT, Daughton DM, Glover PN, Hughes JR, Gross J. Smoking cessation in highly dependent smokers with 4mg nicotine polacrilex. American Journal of Health Behavior. 1996;20:319–332. [Google Scholar]
- Goldstein MG, Niaura R, Follick MJ, Abrams DB. Effects of behavioral skills training and schedule of nicotine gum administration on smoking cessation. American Journal of Psychiatry. 1989;146:56–60. doi: 10.1176/ajp.146.1.56. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Callas PW. Errors in interpreting abstinence curves in studies of smoking cessation. Nicotine & Tobacco Research. 2006;8:7–12. doi: 10.1080/14622200500431635. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Gust SW, Keenan RM, Fenwick JW, Healy ML. Nicotine vs placebo gum in general practice. The Journal of the American Medical Association. 1989;261:1300–1305. [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine & Tobacco Research. 2003;5:13–25. [PubMed] [Google Scholar]
- Hurt RD, Sachs DPL, Glover ED, Offord KP, Johnston JA, Dale LC, et al. A comparison of sustained release bupropion and placebo for smoking cessation. New England Journal of Medicine. 1997;337:1195–1202. doi: 10.1056/NEJM199710233371703. [DOI] [PubMed] [Google Scholar]
- Lewis-Esquerre JM, Colby SM, Tevyaw TO, Eaton CA, Kahler CW, Monti PM. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug and Alcohol Dependence. 2005;79:33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- McCarthy DE, Piasecki TM, Fiore MC, Baker TB. Life before and after quitting smoking: An electronic diary study. Journal of Abnormal Psychology. 2006;115:454–466. doi: 10.1037/0021-843X.115.3.454. [DOI] [PubMed] [Google Scholar]
- Medioni J, Berlin I, Mallet A. Increased risk of relapse after stopping nicotine replacement therapies: a mathematical modeling approach. Addiction. 2005;100:247–254. doi: 10.1111/j.1360-0443.2004.00961.x. [DOI] [PubMed] [Google Scholar]
- Murphy SA. An experimental design for the development of adaptive treatment strategies. Statistics in Medicine. 2005;24:1455–81. doi: 10.1002/sim.2022. [DOI] [PubMed] [Google Scholar]
- Piasecki TM. Relapse to smoking. Clinical Psychology Review. 2006;26:196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, McCarthy DE, Baker TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction. 2002;97:1093–1108. doi: 10.1046/j.1360-0443.2002.00216.x. [DOI] [PubMed] [Google Scholar]
- Piper ME, Federman EB, McCarthy DE, Bolt DM, Smith SS, Fiore MC, et al. Efficacy of bupropion alone and in combination with nicotine gum. Nicotine & Tobacco Research. 2007;9:947–954. doi: 10.1080/14622200701540820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fiore MC, Jorenby DE, Fraser DE, et al. A randomized placebo-controlled clinical trial of five smoking cessation pharmacotherapies. Archives of General Psychiatry. 2009;66:1253–1262. doi: 10.1001/archgenpsychiatry.2009.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S. Reflections on smoking relapse research. Drug and Alcohol Review. 2006;25:15–20. doi: 10.1080/09595230500459479. [DOI] [PubMed] [Google Scholar]
- Shiffman S. How Many Cigarettes Did You Smoke? Assessing Cigarette Consumption by Global Report, Time-Line Follow-Back, and Ecological Momentary Assessment. Health Psychology. 2009;28:519–526. doi: 10.1037/a0015197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Gnys M, Richards TJ, Paty JA, Hickcox M, Kassel JD. Temptations to smoke after quitting: A comparison of lapsers and maintainers. Health Psychology. 1996;15:455–461. doi: 10.1037//0278-6133.15.6.455. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Sharf DM, Shadel WG, Gwaltney CJ, Dang Q, Paton SM, et al. Analyzing milestones in smoking cessation: Illustration in a nicotine patch trial in adult Smokers. Journal of Consulting and Clinical Psychology. 2006;74:276–285. doi: 10.1037/0022-006X.74.2.276. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. British Journal of Addiction. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- West R, Baker CL, Cappelleri JC, Bushmakin AG. Effect of varenicline and bupropion SR on craving, withdrawal symptoms and the rewarding effects of smoking during a quit attempt. Psychopharmacology. 2008;197:371–377. doi: 10.1007/s00213-007-1041-3. [DOI] [PubMed] [Google Scholar]