Abstract
Objectives
Isoflurane preconditioning has been shown to protect endothelial cells against lipopolysaccharide and cytokines-induced injury. This study was designed to determine whether isoflurane preconditioning increased endothelial cell tolerance to ischemia.
Methods
Bovine pulmonary arterial endothelial cells were exposed or not exposed to various concentrations of isoflurane for 1 hr. After a 30-min isoflurane-free period, cells were subjected to oxygen-glucose deprivation (OGD) for 3 hr and reoxygenation for 1 hr. Lactate dehydrogenase (LDH) release from cells was used to measure cell injury. In some experiments, various protein kinase C (PKC) inhibitors and ATP-sensitive potassium channel (KATP channel) inhibitors were present from 30 min before isoflurane treatment to the end of isoflurane treatment.
Key findings
Isoflurane preconditioning dose-dependently decreased the OGD-induced LDH release. This protection was inhibited by 2 μM chelerythrine, a general PKC inhibitor, or 10 μM GÖ6976, an inhibitor for the conventional PKCs. This protection also was inhibited by 0.3 μM glybenclamide, a general KATP channel inhibitor, and 500 μM 5-hydroxydecanoate, a mitochondrial KATP channel blocker. In addition, pretreatment with 100 μM diazoxide, a KATP channel activator, for 1 hr also reduced OGD-induced endothelial cell injury. This diazoxide-induced protection was inhibited by chelerythrine.
Conclusions
Our results suggest that isoflurane preconditioning induces endothelial protection against in vitro simulated ischemia. This protection may be mediated at least in part by conventional PKCs and mitochondrial KATP channels. Our results also indicate that PKCs may be downstream of KATP channels in causing endothelial protection.
Keywords: endothelial cells, isoflurane, mitochondrial KATP channel, preconditioning, protein kinase C
Introduction
Endothelial cells line blood vessels in all organs and systems. They form a unique barrier to prevent free access of chemicals and cells in the blood to the vascular smooth muscle cells and parenchymal cells in organs. Also, endothelial cells release various molecules, such as nitric oxide and endothelin, to affect the functions of other cells.[1,2] Thus, maintaining structural and functional integrity of endothelial cells is critical under physiological and pathophysiological conditions. However, many insults can threaten this integrity. For example, ischemia can injure endothelial cells.
Preconditioning is a phenomenon in which a prior exposure to short episodes of ischemia or other stimuli can induce ischemic tolerance. Since the concept “preconditioning” was introduced in 1986,[3] numerous studies have shown that preconditioning is a promising approach to reduce ischemic injury in various organs.[4,5] Although many stimuli can induce a preconditioning effect, the use of a relatively safe agent to induce preconditioning effects represents a potentially useful approach to provide organ protection in clinical practice. It has been shown that commonly used volatile anesthetics, such as isoflurane, can induce a preconditioning effect against ischemia in many organs including brain and heart.[6,7] Isoflurane preconditioning also reduces inflammation-induced endothelial injury.[8] Application of sevoflurane, another volatile anesthetic used in clinical practice, during the period from 15 min before ischemia to 5 min after the onset of reperfusion improved the functions of endothelial cells in human forearm arteries after a 15-min forearm ischemia.[9] Thus, we hypothesize that preconditioning with volatile anesthetics can reduce ischemic injury of endothelial cells. To test this hypothesis, we used bovine pulmonary arterial endothelial cells (BPAECs) and subjected them to oxygen-glucose deprivation (OGD), a condition to simulate ischemia in vitro. Since protein kinase C (PKC) and ATP-sensitive potassium channels (KATP channels) are implicated to be involved in isoflurane preconditioning-induced protection in many organs and cell types,[7,10,11] we tested the role of PKC and KATP channels in the isoflurane preconditioning-induced endothelial protection. Despite numerous studies on preconditioning-induced protection of various organs and tissues since 1986, very few studies have been focused on preconditioning-induced protection of endothelial cells. Our study was designed not only to determine whether isoflurane could induce a preconditioning effect against in vitro simulated ischemia/reperfusion in endothelial cells but also to reveal mechanisms for this protection.
Materials and Methods
Materials
Isoflurane was purchased from Abbott Laboratories (North Chicago, IL). Chelerythrine chloride was obtained from Biomol (Plymouth Meeting, PA). Other chemicals were obtained from Sigma-Aldrich (St Louis, MO), unless specified in the text.
Cell culture
BPAECs were isolated and characterized as we described before.[12,13] The cells were cultured in a T75 flask containing 12 ml of culture media composed of Dulbecco's Modified Eagle's Medium (DMEM) (containing 1,000 mg/l D-glucose, L-glutamine and pyridoxine HCl), 110 mg/l sodium pyruvate, 10% heat inactivated fetal bovine serum, 90 μg/ml thymidine, 100 U/ml penicillin and 100 μg/ml streptomycin. The cells were kept in a humidified atmosphere containing 95% air-5% CO2 at 37°C. Culture medium was changed three times per week. Cells were sub-cultured when they were 70 – 80% confluent. The cells between passage 8 and 20 were used in the experiments.
Isoflurane and oxygen-glucose deprivation exposure
The cells were placed into 6-well plates at a density of 5 × 103cells/ml (2 ml/well) and cultured overnight (about 17 hr). Glucose-free buffer contained 154 mM NaCl, 5.6 mM KCl, 3.6 mM NaHCO3, 3.6 mM CaCl2 and 5.0 mM HEPES. Glucose was added to make glucose containing buffer that contained 4.5 g/l glucose. Isoflurane was delivered by air through an agent specific vaporizer. The glucose containing buffer was pregassed with isoflurane for 10 min. This isoflurane containing buffer was added to the cells. The cells were immediately placed into an air-tight chamber and this chamber was gassed with isoflurane containing air for 10 min. The anesthetic concentrations in the outlet gases were monitored by a Datex™ infrared analyzer (Capnomac, Helsinki, Finland) and the target isoflurane concentrations were reached in < 2 min. After closure of the inlet and outlet of the chamber, the chamber was then placed in an incubator for 1 hr at 37°C. Cells were then removed from the chamber and placed in the incubator for 30 min at 37°C before they were subjected to OGD.
OGD buffer was prepared by bubbling the glucose-free buffer with 100% N2 for 30 min. Cells in control group were washed with and incubated in glucose containing buffer in a humidified atmosphere of 95% air-5% CO2 at 37°C. OGD condition to cells was created by washing cells with OGD buffer three times and then placing cells in this OGD buffer. These plates were then placed in an air-tight chamber gassed with 100% N2 for 10 min. The oxygen content in the outlet of the chamber was monitored with a Datex™ infrared analyzer and was below 2% at ~3 min after the onset of gassing. The inlet and outlet of the chamber were closed and the chamber was kept at 37°C for 3 hr. After the oxygen content in the chamber at the end of incubation was confirmed to be < 2%, the chamber was opened and glucose was added to the incubation solutions to make the final concentration of glucose at 4.5 g/l. In a separate preliminary experiment, the O2 partial pressure in the incubation solutions during the OGD exposure was measured to be < 10 mmHg. The cells were kept in glucose containing solution in air for 1 hr at 37°C. The incubation buffer and cells were then used for assay of lactate dehydrogenase (LDH) activity.
Application of chemicals
KATP channel blockers (0.3 μM glybenclamide or 500 μM 5-hydroxydecanoate) or PKC inhibitors (2 μM chelerythrine chloride or 10 μM GÖ6976) were added to the cells at 30 min before the exposure to 3% isoflurane for 1 hr. After the incubation (total incubation time with these inhibitors was 1.5 hr), the solutions were replaced with fresh glucose containing buffers without these reagents. The solutions in the control, OGD only or isoflurane preconditioning plus OGD groups in the same set of experiments were also changed in the same way. In another set of experiments, a mitochondrial KATP channel activator (100 μM diazoxide) was applied for 1 hr in the presence or absence of 2 μM chelerythrine chloride. After a 30-min drug free-period, these cells were also exposed to a 3-hr OGD followed with a 1-hr simulated reperfusion.
Lactate dehydrogenase activity assay
LDH activity was determined using LDH cytotoxicity detection kit (Clontech Laboratory, La Jolla, CA). Briefly, the incubation solution was centrifuged at 13,000 rpm for 10 min and the cell-free supernatant was transferred to 96-well plates. A 100-μl supernatant was incubated with the same amount of reaction mixture. LDH activity was determined by a colorimetric assay. The absorbance of samples was measured at 492 nm with the reference wavelength of 655 nm in a spectrophotometry (Bio-Rad Laboratories, Hercules, CA). Background absorbance from the cell-free buffer solution was subtracted from all absorbance measurements. After removal of the buffer from 6-well plates, 0.5% triton X-100 lysing solution was applied to the remaining cells. The percentage of LDH released to incubation buffer in total LDH was calculated: 100*spontaneously released LDH in the buffer/(spontaneously released LDH in the buffer + intracellular LDH released by triton X-100).
Statistical Analyses
Data are expressed as mean ± S.D. (n ≥ 26 for each experimental condition). One-way analysis of variance followed by the Tukey test for post hoc analysis was performed for normally distributed data. One-way analysis of variance on ranks followed by the Dunn's test for post hoc analysis was performed for non-normally distributed data. A P value < 0.05 was considered statistically significant.
Results
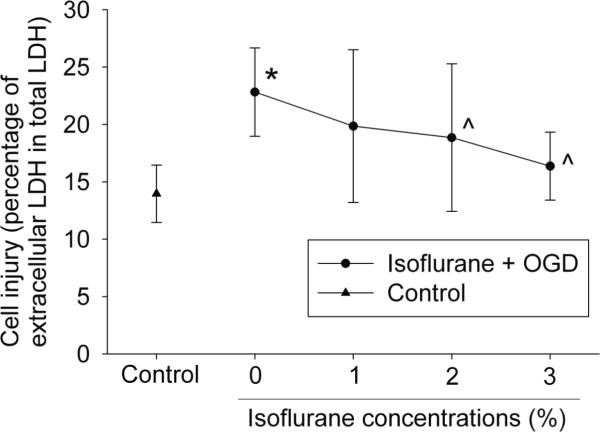
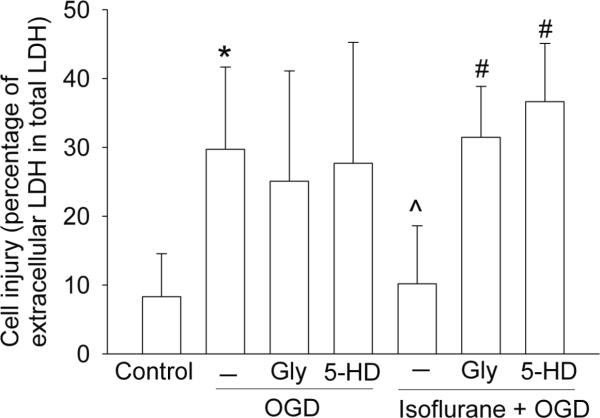
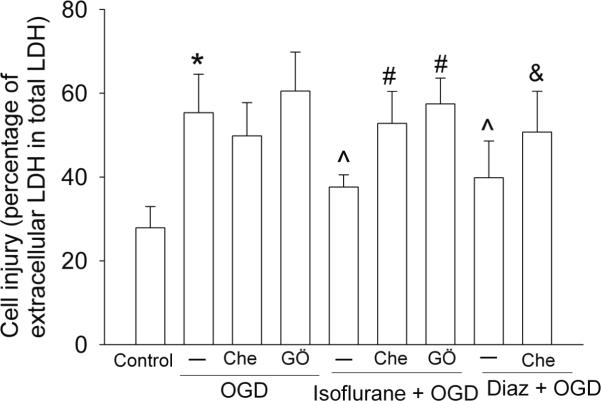
The 3-hr OGD and 1-hr simulated reperfusion significantly increased LDH release from BPAECs (Fig. 1), suggesting that this condition caused injury of these cells. This injury was significantly attenuated by pretreatment with 2% or 3% isoflurane (Fig. 1). The attenuation of cell injury caused by 3% isoflurane pretreatment was inhibited by glybenclamide, a general KATP channel inhibitor, and by 5-hydroxydecanoate, a mitochondrial KATP channel blocker; whereas glybenclamide and 5-hydroxydecanoate did not affect the LDH release under the OGD and simulated reperfusion condition alone (Fig. 2). Similarly, the 3% isoflurane pretreatment-induced attenuation of cell injury was inhibited by chelerythrine, a general PKC inhibitor, and 10 μM GÖ6976, an inhibitor for the conventional PKCs. These two PKC inhibitors did not affect the LDH release caused by the OGD and simulated reperfusion alone (Fig. 3). Pretreatment with diazoxide, a KATP channel activator, also reduced the OGD and simulated reperfusion-induced LDH release. This diazoxide-induced protection was inhibited by chelerythrine (Fig. 3). Of note, the LDH release under the OGD and simulated reperfusion only condition in figure 3 was higher than that presented in figures 1 or 2. This difference may be due to different batches of cells used to generate results for these figures. In supporting this possibility, LDH release under control condition in figure 3 was higher than that presented in figures 1 and 2.
Fig. 1. Isoflurane preconditioning effect.
Bovine pulmonary arterial endothelial cells were pretreated with various concentrations of isoflurane for 1 hr and then were exposed or not exposed to a 3-hr oxygen-glucose deprivation (OGD). Results are means ± S.D. (n = 29 – 34). * P < 0.05 compared with control. ^ P < 0.05 compared with OGD only. Statistic analysis was performed by one-way analysis of variance. LDH: lactate dehydrogenase.
Fig. 2. Involvement of mitochondrial KATP channels in isoflurane preconditioning effect.
Bovine pulmonary arterial endothelial cells were pretreated with or without 3% isoflurane for 1 hr in the presence or absence of 0.3 μM glybenclamide (Gly) or 500 μM 5-hydroxydecanoate (5-HD) and then were exposed or not exposed to a 3-hr oxygen-glucose deprivation (OGD). Results are mean ± S.D. (n = 26 – 30). * P < 0.05 compared with control. ^ P < 0.05 compared with OGD only. # P < 0.05 compared with isoflurane preconditioning + OGD. Statistic analysis was performed by one-way analysis of variance on ranks. LDH: lactate dehydrogenase.
Fig. 3. Involvement of protein kinase C in isoflurane preconditioning effect.
Bovine pulmonary arterial endothelial cells were pretreated with or without 3% isoflurane for 1 hr in the presence or absence of 2 μM chelerythrine (Che) or 10 μM GÖ6976 (GÖ) or were pretreated with 100 μM diazoxide (Diaz) for 1 hr in the presence or absence of 2 μM chelerythrine. The cells were then subjected to a 3-hr oxygen-glucose deprivation (OGD). Results are mean ± S.D. (n = 29 – 30). * P < 0.05 compared with control. ^ P < 0.05 compared with OGD only. # P < 0.05 compared with isoflurane preconditioning + OGD. & P < 0.05 compared with Diaz + OGD. Statistic analysis was performed by one-way analysis of variance. LDH: lactate dehydrogenase.
Discussion
Isoflurane preconditioning has been shown to reduce cytokine-induced endothelial cell injury.[8] We showed in this study that isoflurane preconditioning concentration-dependently decreased the OGD-induced endothelial cell injury. These results suggest that isoflurane preconditioning can induce ischemic tolerance in endothelial cells. Consistent with this suggestion, a previous study showed that sevoflurane improved endothelial functions after ischemia.[9] However, sevoflurane was present throughout the period from 15 min before to 5 min after a 15-min ischemia. It is difficult to determine the contribution of sevoflurane preconditioning-induced protection to the overall improvement of endothelial functions after the ischemia.
In our study, the isoflurane preconditioning-induced endothelial cell protection was abolished by glybenclamide, a general KATP channel blocker,[14] and 5-hydroxydecanoate, a mitochondrial KATP channel blocker.[14,15] These results suggest that mitochondrial KATP channels are involved in this isoflurane preconditioning-induced protection. Consistent with this idea, diazoxide, a mitochondrial KATP channel activator,[16] also induced a preconditioning effect. In addition, previous studies have suggested the involvement of the mitochondrial KATP channels in the volatile anesthetic preconditioning-induced protection in the heart and brain.[11,17]
At least 11 isozymes of PKC have been identified. They are classified into three groups: conventional PKCs (α, βI, βII, and γ), novel PKCs (δ, ε, η, and θ), and atypical PKCs (ζ and ι/λ).[18] We showed here that the isoflurane preconditioning-induced endothelial cell protection was abolished by chelerythrine, a general PKC inhibitor, and GÖ6976, an inhibitor for the conventional PKCs.[19,20] These results suggest the involvement of the conventional PKCs in this isoflurane preconditioning effect. Consistent with this suggestion, we and others have shown that volatile anesthetics including isoflurane can activate the conventional PKCs.[21–23] Also, PKC has been shown to be involved in isoflurane preconditioning-induced cardioprotection and neuroprotection.[10,24]
KATP channels including the mitochondrial KATP channels have been considered as a putative end-effector in organ protection induced by ischemic or anesthetic preconditioning.[10] Activation of mitochondrial KATP channels reduces ischemia-induced Ca++ influx into the mitochondria and the subsequent mitochondrial swelling.[25] Activation of these channels may also restore mitochondrial membrane potential and ATP production [reviewed in.[10,25]] In addition, activation of mitochondrial KATP channels can produce signaling molecules, such as free radicals that can then activate PKC.[26–28] Thus, the mitochondrial KATP channels are also signaling molecules. Here, we showed that the protection induced by diazoxide was abolished by chelerythrine, a PKC inhibitor.[29] These results suggest that the mitochondrial KATP channels may be a molecule upstream of PKC to induce endothelial protection. These results, along with the findings that suggest the involvement of the conventional PKCs and mitochondrial KATP channels in the isoflurane preconditioning-induced protection, indicate that the conventional PKCs may be a molecule downstream of the mitochondrial KATP channels to mediate the isoflurane preconditioning-induced endothelial protection.
Our findings may have a broad implication. Endothelial cells are ubiquitous in all organs and tissues. They play a critical role in maintaining vasculature functional integrity and normal coagulation status. Endothelial cells are a physical barrier to prevent free access of chemicals and cells in the blood to the vascular smooth muscle cells and parenchymal cells of organs. Thus, it is critically important to maintain the functions and structural integrity of endothelial cells under physiological and pathophysiological conditions. Our results suggest that specific activators for the conventional PKCs or mitochondrial KATP channels may be used for this purpose. This protection of endothelial cells may reduce organ injury under various pathological conditions, such as ischemia.
Conclusions
Pre-exposure of endothelial cells to isoflurane dose-dependently reduced endothelial cell injury after in vitro simulated ischemia and reperfusion. This effect may be mediated at least partially by the mitochondrial KATP channels and conventional PKCs. It appears that PKCs may be signaling molecules downstream of the mitochondrial KATP channels in causing endothelial protection.
Acknowledgments
Funding This study was supported by grants (GM065211 to Z Zuo) from the National Institutes of Health, Bethesda, Maryland, by a grant from the International Anesthesia Research Society (2007 Frontiers in Anesthesia Research Award to Z Zuo), by a Grant-in-Aid from the American Heart Association Mid-Atlantic Affiliate (0755450U to Z Zuo) and the Department of Anesthesiology, University of Virginia.
Footnotes
Conflict of interest The authors declare that they have no conflicts of interest to disclose.
References
- 1.Nathan C, Xie QW. Nitric oxide synthases: roles, tolls, and controls. Cell. 1994;78:915–8. doi: 10.1016/0092-8674(94)90266-6. [DOI] [PubMed] [Google Scholar]
- 2.Cheng YS, et al. Stress-induced cardiac insufficiency relating to abnormal leptin and FKBP12.6 is ameliorated by CPU0213, an endothelin receptor antagonist, which is not affected by the CYP3A suppressing effect of erythromycin. J Pharm Pharmacol. 2009;61:569–76. doi: 10.1211/jpp/61.05.0004. [DOI] [PubMed] [Google Scholar]
- 3.Murry CE, et al. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74:1124–36. doi: 10.1161/01.cir.74.5.1124. [DOI] [PubMed] [Google Scholar]
- 4.Dirnagl U, et al. Ischemic tolerance and endogenous neuroprotection. Trends Neurosci. 2003;26:248–54. doi: 10.1016/S0166-2236(03)00071-7. [DOI] [PubMed] [Google Scholar]
- 5.Ferrari R, et al. Ischemic preconditioning, myocardial stunning, and hibernation: basic aspects. American Heart Journal. 1999;138:S61–8. doi: 10.1016/s0002-8703(99)70322-4. [DOI] [PubMed] [Google Scholar]
- 6.Zheng S, Zuo Z. Isoflurane preconditioning induces neuroprotection against ischemia via activation of p38 mitogen-activated protein kinase. Molecular Pharmacology. 2004;65:1172–1180. doi: 10.1124/mol.65.5.1172. [DOI] [PubMed] [Google Scholar]
- 7.Obal D, et al. Role of protein kinase C-epsilon (PKCepsilon) in isoflurane-induced cardioprotection. Br J Anaesth. 2005;94:166–73. doi: 10.1093/bja/aei022. [DOI] [PubMed] [Google Scholar]
- 8.de Klaver MJM, MD, et al. Isoflurane Pretreatment Inhibits Cytokine-induced Cell Death in Cultured Rat Smooth Muscle Cells and Human Endothelial Cells. Anesthesiology. 2002;97(1):24–32. doi: 10.1097/00000542-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Lucchinetti E, et al. Sevoflurane inhalation at sedative concentrations provides endothelial protection against ischemia-reperfusion injury in humans. Anesthesiology. 2007;106:262–8. doi: 10.1097/00000542-200702000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Zaugg M, et al. Anaesthetics and cardiac preconditioning. Part I. Signalling and cytoprotective mechanisms. Br J Anaesth. 2003;91:551–65. doi: 10.1093/bja/aeg205. [DOI] [PubMed] [Google Scholar]
- 11.Kehl F, et al. Sevoflurane-induced preconditioning of rat brain in vitro and the role of KATP channels. Brain Res. 2004;1021:76–81. doi: 10.1016/j.brainres.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 12.Zuo Z, Johns RA. Inhalational anesthetics up-regulate constitutive and lipopolysaccharide-induced inducible nitric oxide synthase expression and activity. Molecular Pharmacology. 1997;52:606–612. doi: 10.1124/mol.52.4.606. [DOI] [PubMed] [Google Scholar]
- 13.Wu X, et al. Statin post-treatment provides protection against simulated ischemia in bovine pulmonary arterial endothelial cells. European Journal of Pharmacology. 2010;636:114–20. doi: 10.1016/j.ejphar.2010.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sato T, et al. Selective pharmacological agents implicate mitochondrial but not sarcolemmal K(ATP) channels in ischemic cardioprotection. Circulation. 2000;101:2418–23. doi: 10.1161/01.cir.101.20.2418. [DOI] [PubMed] [Google Scholar]
- 15.Lim YJ, et al. Morphine preconditions purkinje cells against cell death under in vitro simulated ischemia-reperfusion conditions. Anesthesiology. 2004;100:562–8. doi: 10.1097/00000542-200403000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Roseborough G, et al. The mitochondrial K-ATP channel opener, diazoxide, prevents ischemia-reperfusion injury in the rabbit spinal cord. Am J Pathol. 2006;168:1443–51. doi: 10.2353/ajpath.2006.050569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Obal D, et al. The influence of mitochondrial KATP-channels in the cardioprotection of preconditioning and postconditioning by sevoflurane in the rat in vivo. Anesth Analg. 2005;101:1252–60. doi: 10.1213/01.ANE.0000181336.96511.32. [DOI] [PubMed] [Google Scholar]
- 18.Way KJ, et al. Identification of PKC-isoform-specific biological actions using pharmacological approaches. Trends in Pharmacological Sciences. 2000;21:181–7. doi: 10.1016/s0165-6147(00)01468-1. [DOI] [PubMed] [Google Scholar]
- 19.Davis KE, et al. Multiple signaling pathways regulate cell surface expression and activity of the excitatory amino acid carrier 1 subtype of Glu transporter in C6 glioma. Journal of Neuroscience. 1998;18:2475–85. doi: 10.1523/JNEUROSCI.18-07-02475.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonzalez M, et al. Phorbol myristate acetate-dependent interaction of protein kinase C alpha and the neuronal glutamate transporter EAAC1. Journal of Neuroscience. 2003;23:5589–5593. doi: 10.1523/JNEUROSCI.23-13-05589.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang Y, Zuo Z. Isoflurane induces a protein kinase C alpha-dependent increase in cell surface protein level and activity of glutamate transporter type 3. Molecular Pharmacology. 2005;67:1522–1533. doi: 10.1124/mol.104.007443. [DOI] [PubMed] [Google Scholar]
- 22.Huang Y, et al. Critical Role of Serine 465 in Isoflurane-induced Increase of Cell-surface Redistribution and Activity of Glutamate Transporter Type 3. J Biol Chem. 2006;281:38133–8. doi: 10.1074/jbc.M603885200. [DOI] [PubMed] [Google Scholar]
- 23.Hemmings HC, Adamo AI. Effects of halothane and propofol on purified brain protein kinase C activation. Anesthesiology. 1994;81:147–55. doi: 10.1097/00000542-199407000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Xu X, et al. Isoflurane preconditioning reduces mouse microglial activation and injury induced by lipopolysaccharide and interferon-gamma. Neuroscience. 2008;154:1002–8. doi: 10.1016/j.neuroscience.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grover GJ, Garlid KD. ATP-Sensitive potassium channels: a review of their cardioprotective pharmacology. J Mol Cell Cardiol. 2000;32:677–95. doi: 10.1006/jmcc.2000.1111. [DOI] [PubMed] [Google Scholar]
- 26.McPherson BC, Yao Z. Morphine Mimics Preconditioning via Free Radical Signals and Mitochondrial K(ATP) Channels in Myocytes. Circulation. 2001;103:290–295. doi: 10.1161/01.cir.103.2.290. [DOI] [PubMed] [Google Scholar]
- 27.Gopalakrishna R, Anderson WB. Ca2+− and phospholipid-independent activation of protein kinase C by selective oxidative modification of the regulatory domain. Proc Natl Acad Sci U S A. 1989;86:6758–62. doi: 10.1073/pnas.86.17.6758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jabr RI, Cole WC. Alterations in electrical activity and membrane currents induced by intracellular oxygen-derived free radical stress in guinea pig ventricular myocytes. Circ Res. 1993;72:1229–44. doi: 10.1161/01.res.72.6.1229. [DOI] [PubMed] [Google Scholar]
- 29.Herbert JM, et al. Chelerythrine is a potent and specific inhibitor of protein kinase C. Biochem Biophys Res Commun. 1990;172:993–9. doi: 10.1016/0006-291x(90)91544-3. [DOI] [PubMed] [Google Scholar]