Abstract
BACKGROUND
About one-quarter of rehospitalized Medicare patients are admitted to hospitals different from their original. The extent to which this practice is related to for-profit hospital status, and impacts payments and mortality, is unknown.
OBJECTIVE
To describe and examine predictors of and payments for rehospitalization to a different hospital within 30 days among Medicare beneficiaries in for-profit and in not-for-profit/public hospitals.
DESIGN
Retrospective cohort study.
SETTING
Medicare fee-for-service hospitals throughout the United States.
PARTICIPANTS
Random 5% national sample of Medicare beneficiaries with acute-care rehospitalizations within 30-days of discharge, 2005–2006 (N=74,564).
MEASUREMENTS
30-day rehospitalizations to different hospitals; total payments/mortality over subsequent 30-days. Multivariate logistic and quantile regression models included index hospital for-profit status, discharge counts, geographic region, rural-urban commuting area, and teaching status; and patient sociodemographics, disabled status, comorbidities, and a measure of risk-adjustment.
RESULTS
22% (16,622) of the sample was rehospitalized to a different hospital. Factors associated with increased risk for rehospitalization to a different hospital included being hospitalized within a for-profit, major medical school-affiliated, or low volume index hospital, and having a Medicare-defined disability. When compared to those rehospitalized to the same hospital, patients rehospitalized to different hospitals had significantly higher adjusted 30-day total payments (median additional $1,308/patient, p-value<0.001), but no significant differences in 30-day mortality, regardless of index hospital for-profit status.
LIMITATIONS
The analysis lacked detailed clinical data, and did not assess specific provider practice motivations or the role of patient choice.
CONCLUSIONS
Rehospitalizations to different hospitals are common among Medicare beneficiaries, more likely among those initially hospitalized at a for-profit hospital, and related to increased overall payments without improved mortality.
INTRODUCTION
Rehospitalization within the first 30 days of discharge affects 1 in 5 hospitalized Medicare fee-for-service beneficiaries and accounts for approximately $17.4 billion in payments annually (1). Although most patients are rehospitalized within the same hospital from which they were discharged, at least 1 in 4 is rehospitalized to a different hospital (1). This holds true even if the patient originates from a high-volume center (1). Information exchange between hospitals is hampered by the lack of a universal medical record (2), and health care professionals are often unaware of critical information gathered in another facility (3). As such, rehospitalizations to different hospitals may result in the duplication of costly tests, procedures, and treatments. It may also delay appropriate diagnoses or treatments, leading to increased payments and mortality.
A multitude of patient and hospital factors may drive these diversions to different hospitals. Rehospitalizations to different hospitals may be planned, driven by patient choice, or made necessary by a high hospital census or the need for expertise unavailable at the original hospital. However, it is also well-established that non-medical (e.g., patient race/ethnicity) and financial factors (e.g., lack of insurance) can influence provider decisions to triage patients to other hospitals for admission (4–9). Furthermore, in the case of rehospitalization, the original hospital understands the patient’s needs and likely would be able to project his/her future care costs. In particular, for-profit hospitals may have a financial incentive to divert known high-cost patients with impending rehospitalization to different facilities as a means of minimizing costs and increasing profits (4, 10). However, objective evidence of this practice has not been offered. Given the sizable influence that for-profit hospitals exert in certain US regions (11, 12), it is vital that for-profit rehospitalization practices be further defined.
As the Centers for Medicare and Medicaid Services and other federal entities contemplate the precise enactment of the new Hospital Readmissions Reduction Program (legislation contained within the recent healthcare reform to reduce 30-day Medicare rehospitalizations through hospital-based payment penalties beginning in 2012) (13–18), it is important to obtain knowledge on how for-profit status affects rehospitalizations to different hospitals and how this practice, in turn, impacts overall payments and mortality. Unless carefully monitored, a payment policy targeting rehospitalizations has the potential to incentivize diversions to other facilities (14). Therefore, to inform the national discussion on payment reform, we utilized a nationally representative 5% random sample of Medicare beneficiaries from 2005–2006 to examine 1) the prevalence and predictors of rehospitalization to different hospitals, and 2) how rehospitalization to a different hospital impacts 30-day Medicare payments and mortality in for-profit and in not-for-profit/public hospitals.
METHODS
Design Overview
We used Medicare data to identify a cohort of beneficiaries with acute care rehospitalizations within 30 days of an acute care (i.e., hospital) discharge between January 1, 2005 and November 31, 2006. Medicare fee-for-service claims are longitudinal, and are a well-accepted standard for identifying sites of acute care and total payments over time for care reimbursed through the Medicare system (1, 14). Medicare data were also used to assess index hospital characteristics, including for-profit status, and baseline sociodemographic and comorbidity characteristics of eligible beneficiaries. This allowed us to examine predictors of and payments for rehospitalization to a different hospital within 30 days among Medicare beneficiaries in for-profit and in not-for-profit/public hospitals.
Prior to examining/conducting any specific data or analyses, we developed the study objective, analysis protocol, and table outlines. This a priori analysis protocol remained unaltered throughout the research process, except for the addition of extra comorbidity measures and hospital discharge volume strata requested by peer-reviewers. Although no hypotheses about the relationships between hospital status and outcomes were specified a priori, our analytic plan was constructed on the theory that beneficiaries rehospitalized to different hospitals may experience differences in their payment or mortality outcomes due to poor care coordination and information flow between hospitals, and that certain types of hospitals (i.e., for-profits) may have additional incentives to divert certain populations to different hospitals for their care. The University of Wisconsin Institutional Review Board approved this study with a waiver of consent.
Data Sources
We obtained demographic/enrollment data and institution/physician/supplier claims for a 5% random national sample of 2004, 2005, and 2006 Medicare beneficiaries from the Centers for Medicare and Medicaid Services Chronic Condition Data Warehouse [CCW] (19). Details regarding the random sampling procedures utilized by the CCW in its construction of this sample can be found at http://ccwdata.org (20). Linked annual Medicare provider of services files containing hospital characteristics were also obtained for 2004–2006 from the CCW. Medicare beneficiaries who had non-continuous Part A and B enrollment (for reasons other than death), or received railroad retirement benefits or care through a Medicare health maintenance organization were excluded.
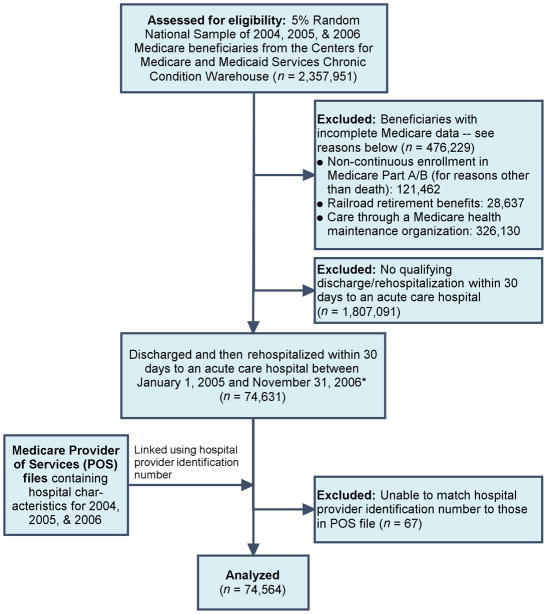
We examined this dataset to identify subjects who were discharged and then rehospitalized within 30 days to acute care hospitals from January 1, 2005 to November 31, 2006. Data from 2004 were used to calculate baseline risk adjustment scores, and therefore, were not used to identify qualifying hospitalizations. Using criteria for rehospitalization published by Jencks et al. (1), we defined a qualifying acute care hospitalization as any acute care stay contained within the inpatient Medicare claims that was not within a hospital specialty unit, not within an inpatient rehabilitation, long-term care, or critical access hospital, and not for a primary rehabilitation diagnosis (DRG-462). Additionally, to exclude hospital-to-hospital transfers, all rehospitalizations to different hospitals occurring on the same day as discharge from the index hospital were excluded. Same-day rehospitalizations to index facilities were included. For subjects with more than one qualifying hospitalization-rehospitalization dyad, only the first chronologically was included. Final sample size was 74,564 (see study flow diagram, figure 1).
Figure 1. Study Flow Diagram.
* For beneficiaries with more than one qualifying hospitalization-rehospitalization dyad, only the first chronologically was included
Variables
All patient-level variables were created using information available within the Medicare data. We determined whether subjects were rehospitalized to the same or a different acute care hospital as the index hospitalization by comparing the facility identification number for each acute stay. Total payments for all Medicare claims for 30 days, starting at the date of rehospitalization, were calculated. Claims which extended beyond the 30-day timeframe were broken into per-diem rates and only the cost for the first 30 days was included. We identified patients who died within 30 days of rehospitalization using dates of rehospitalization in the inpatient file and dates of death within the demographic/enrollment file. Using admission/discharge dates on acute care facility claims, we also calculated the index hospitalization length of stay. Age at rehospitalization, gender, race/ethnicity, Medicaid enrollment, and disabled status were obtained directly from the Medicare data for all patients. Race/ethnicity was split into categories of White, Black, and Other based upon the beneficiary race code contained within the Medicare data, and was included because race/ethnicity has been shown to impact 30-day rehospitalization risk (21, 22). The Centers for Medicare and Medicaid Services (CMS) utilizes a risk adjustment model called the CMS-hierarchical condition category (CMS-HCC) score to predict Medicare payments and to adjust Medicare capitation payments on the basis of case-mix. This system utilizes ICD-9-CM codes gathered from both inpatient and outpatient encounters from the prior year to assign the beneficiary to specific “condition categories” which are clinically- and cost-similar. CMS utilized 3,000 specific ICD-9-CM codes to define the 70 condition categories included in the measure. Comorbidity is reflected by allowing a beneficiary to belong to multiple condition categories. Beneficiary demographic adjusters are also included (i.e., age, gender, Medicaid status, disabled status) in the creation of the final CMS-HCC score (average score = 1.0). The final CMS-HCC model has an expenditure prediction R2 statistic of 9.8%. (23). We calculated each subject’s CMS-HCC score for the 12 months prior to the rehospitalization date. This calculation included all outpatient and inpatient claims over the 12 months of interest, including the index hospitalization. These CMS-HCC scores were included within models as comprehensive risk adjustment measures (23). Furthermore, we identified comorbid conditions by incorporating information from the index hospitalization, all hospitalizations during the year prior to the rehospitalization, and all physician claims during the year prior to the rehospitalization using methods proposed by Elixhauser et al. (24). Of the conditions identified, we included the 10 comorbidities most often present in our sample (i.e., hypertension, fluid and electrolyte disorders, congestive heart failure, chronic pulmonary disease, deficiency anemias, diabetes-uncomplicated, valvular disease, hypothyroidism, peripheral vascular disorders, cardiac arrhythmias) and created an indicator variable of ‘other comorbidity’ to denote the presence of pulmonary circulation disorders, other neurological disorders, diabetes-complicated, renal failure, metastatic cancer, solid tumor without metastasis, coagulopathy, obesity, weight loss, psychoses, or depression (all of which occurred at lower frequencies within the sample). These variables were included within our analyses to provide an additional control for the effect of comorbidity. The most common reasons for index hospitalization and rehospitalization were categorized using the Agency for Healthcare Research and Quality’s (AHRQ) Clinical Classifications Software (25), a tool for clustering patient diagnoses and procedures (using ICD-9-CM codes) into a manageable number of clinically meaningful categories. For this analysis, we clustered diagnoses into the 285 AHRQ-pre-defined, mutually exclusive, ‘single-level’ diagnostic categories (26).
Facility characteristics were also obtained from the Medicare files. We determined the index hospital’s for-profit status, medical school affiliation (i.e., major, minor [limited/graduate], and none), and Centers for Medicare and Medicaid Services geographic billing region from the provider of services file corresponding to the patient’s index hospitalization date (27). We used acute care facility claims over the full 3-year period to determine average annual Medicare discharge number for each hospital within the 5% sample. Each average was then multiplied by 20 to estimate the total average annual discharge count (23) and to categorize hospitals as having >10,000 annual discharges, 6,001–10,000 annual discharges, 1,000–6,000 annual discharges, and <1,000 annual discharges. A census tract-based measure of rural/urban status used by the US Department of Agriculture, the Rural/Urban Commuting Area code (28), was generated for each index hospital and clustered into categories of “urban core areas,” “suburban areas,” “large town areas,” and “small town/isolated rural areas” (29).
We obtained all of our variables from Medicare data. Medicare fee-for-service claims are longitudinal, and are a well-accepted standard for identifying sites of acute care, length of stay, and total payments over time for care reimbursed through the Medicare system (1, 14, 30). Medicare claims are also a well-accepted approach for assessing mortality (30–32). We had no missing information for subjects’ age, gender, Medicaid status, or disability status, or for index hospital Medicare billing region. Less than 1% of our sample was missing race/ethnicity, or index hospital for-profit status, medical school affiliation, or rural urban commuting area code data. Information on subjects’ baseline comorbidities was collected from diagnoses recorded in Medicare claims. It is not possible to assess the extent to which this comorbidity information was missing.
Analysis
Multivariable logistic regression was used to determine the relationship between explanatory variables and readmission to a different hospital. Since our outcomes were common, it would have been inappropriate to estimate relative risks from the odds ratios resulting from these multivariable logistic regression models. Therefore, we used methods published by Kleinman (33) and Localio (34) to calculate adjusted risk ratios, predicted probabilities, and 95% confidence intervals from these models on the basis of marginal standardization (33, 34). The same analytic technique was utilized to determine the relationship between 30-day mortality from the date of rehospitalization and readmission to the same or different hospital, overall and stratified by index hospital for-profit status. To better assess inherently skewed payment data, we used quantile regression (35) to calculate adjusted predicted percentile payments for 30 days from the date of rehospitalization for readmissions to same or different hospitals, overall and stratified by index hospital for-profit status. Because the impact of rehospitalization to a same or to a different facility may differ across the distribution of payments, and because such differences may be intrinsically interesting, we estimate these differential impacts at the 10th, 50th, and 90th percentiles of the conditional distributions, thus permitting these effects to be separately examined for patients at low, median, and high ends of the payment spectrum.
All analyses were pre-specified and were performed using SAS 9.2 (Cary, NC) (36) and STATA 11 (College Station, TX) (37). Significance was assessed at the 5% level. We used chi-squared tests to analyze differences in the frequencies of hospital and beneficiary characteristics between non-profit/public and for-profit hospitals. To account for clustering within hospitals, models utilized robust estimates of the variance. Ninety-five percent confidence intervals for the payment models were estimated using bootstrap techniques to replicate analyses 1,000 times (38, 39). Models included: 1) index hospital for-profit status, medical school affiliation, Rural/Urban Commuting Area code, Centers for Medicare and Medicaid Services geographic region, and average annual discharge count grouping, and 2) patient age, gender, race, Medicaid status, disabled status, comorbidities, index hospitalization length of stay, and Hierarchical Condition Category score.
Role of the Funding Sources
The UW Health Innovation Program provided assistance with Institutional Review Board application, Medicare data management, variable creation, and manuscript formatting. No other funding source had a role in the design or conduct; data collection, management, analysis or interpretation; or preparation, review or approval of the manuscript. The authors do not have any potential conflicts of interest.
RESULTS
Sample Characteristics
3,879 index hospitals and 3,905 readmission (second) hospitals were represented within the analysis. These hospitals each contributed an average of 19 beneficiaries (range 1 to 251) to the analysis. Patients tended to be rehospitalized within hospitals of the same and/or similar type. For example, patients rehospitalized within a non-profit/public hospital were most often initially hospitalized within a non-profit/public hospital, and patients rehospitalized within a for-profit hospital were most often initially hospitalized within a for-profit hospital (Appendix Table 1).
Appendix Table 1.
Characteristics of Index and Rehospitalization Hospitals, 2005–2006
| First (Index) Hospital Characteristics (N = 3,879) | Second (Rehospitalization) Hospital Characteristics (N = 3,905) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| For-Profit Status |
Total Discharge Count Category |
Medical School Affiliation |
Rural Urban Commuting Area Code |
||||||||||
| Non-Profit/Public (N = 3133) | For-Profit (N = 772) | >10,000 Annual Discharges (N = 211) | 6,001–10,000 Annual Discharges (N = 472) | 1,000–6,000 Annual Discharges (N = 2186) | <1,000 Annual Discharges (N = 1036) | None (N = 2750) | Minor (N = 697) | Major(N = 457) | Urban core area (N = 2360) | Suburban area (N = 169) | Large town area (N = 730) | Small town and isolated rural area (N = 584) | |
| For-Profit Status | |||||||||||||
| Non-Profit/Public | 95.0 | 24.2 | 91.5 | 87.7 | 79.1 | 79.9 | 78.3 | 86.1 | 89.9 | 80.1 | 82.8 | 84.0 | 82.5 |
| For-Profit | 5.0 | 75.8 | 8.5 | 12.3 | 21.0 | 20.1 | 21.8 | 13.9 | 10.1 | 19.9 | 17.2 | 16.0 | 17.5 |
| Total discharge count category | |||||||||||||
| >10,000 annual discharges | 9.9 | 5.8 | 77.7 | 4.5 | 5.0 | 6.0 | 6.9 | 10.8 | 19.9 | 11.3 | 10.7 | 4.7 | 6.3 |
| 6,001 – 10,000 annual discharges | 17.8 | 12.7 | 7.1 | 85.0 | 6.1 | 10.0 | 13.5 | 22.2 | 27.8 | 22.8 | 10.7 | 8.8 | 5.7 |
| 1,000 – 6,000 annual discharges | 53.9 | 64.1 | 14.2 | 9.3 | 87.3 | 19.4 | 58.7 | 52.7 | 44.0 | 54.5 | 53.9 | 68.8 | 45.4 |
| <1,000 annual discharges | 18.5 | 17.4 | 1.0 | 1.3 | 1.6 | 64.6 | 20.9 | 14.4 | 8.3 | 11.5 | 24.9 | 17.8 | 42.6 |
| Medical school affiliation | |||||||||||||
| None | 62.8 | 76.9 | 35.6 | 50.4 | 68.6 | 72.4 | 87.4 | 13.2 | 14.7 | 57.5 | 76.9 | 77.4 | 80.3 |
| Minor | 21.0 | 14.4 | 26.1 | 26.5 | 19.2 | 16.2 | 6.7 | 80.2 | 5.5 | 22.7 | 10.1 | 17.0 | 13.0 |
| Major | 16.2 | 8.7 | 38.4 | 23.1 | 12.2 | 11.4 | 6.0 | 6.6 | 79.9 | 19.8 | 13.0 | 5.6 | 6.7 |
| Rural Urban Commuting Area Code | |||||||||||||
| Urban core area | 64.9 | 70.7 | 92.9 | 90.2 | 63.6 | 54.2 | 58.6 | 78.7 | 91.4 | 96.7 | 26.6 | 14.5 | 17.8 |
| Suburban area | 3.7 | 3.7 | 1.0 | 1.1 | 4.0 | 4.8 | 4.7 | 1.5 | 1.3 | 0.7 | 70.4 | 0.4 | 0.7 |
| Large town area | 18.4 | 15.1 | 5.2 | 7.9 | 22.0 | 16.0 | 21.0 | 13.5 | 4.2 | 2.0 | 2.4 | 83.3 | 3.9 |
| Small town and isolated rural area | 13.1 | 10.5 | 1.0 | 0.9 | 10.4 | 25.0 | 15.7 | 6.3 | 3.1 | 0.7 | 0.6 | 1.8 | 77.6 |
Values represent percentages unless otherwise specified
Hospital and patient characteristics differed depending upon the for-profit status of the index hospital facility (Table 1). For-profit index hospitals were slightly more likely to be located in suburban areas and to be of lower volume, and were less likely to have medical school affiliations.
Table 1.
Characteristics of Medicare Beneficiaries with 30-Day Rehospitalizations and Their Sites of Index Hospitalization, 2005–2006 (N=74,564)
| Characteristic* | Overall† (N=74,564) | For-Profit Status of Index Hospital |
|
|---|---|---|---|
| Non- Profit/Public† (N=63,957) | For-Profit† (N=10,607) | ||
| Index hospital characteristics | |||
| Average annual discharge count (SD) | 7,115 (5,455) | 7,441 (5,453) | 5,150 (5,038) |
| >10,000 annual discharges | 22.2 | 24.6 | 8.0 |
| 6,001 – 10,000 annual discharges | 26.9 | 28.2 | 19.2 |
| 1,000 – 6,000 annual discharges | 46.7 | 43.6 | 65.9 |
| <1,000 annual discharges | 4.2 | 3.7 | 6.9 |
| Medical school affiliation | |||
| None | 54.9 | 51.1 | 77.9 |
| Minor | 22.5 | 24.0 | 13.7 |
| Major | 22.6 | 25.0 | 8.4 |
| Rural Urban Commuting Area Code for index hospital | |||
| Urban core area | 80.5 | 80.9 | 78.0 |
| Suburban area | 2.2 | 1.9 | 3.8 |
| Large town area | 12.6 | 12.7 | 12.3 |
| Small town and isolated rural area | 4.7 | 4.6 | 5.9 |
| Patient sociodemographic characteristics | |||
| Average age in years (SD) | 76 (12) | 77 (12) | 76 (13) |
| <65 years | 12.2 | 11.9 | 13.9 |
| 65–69 years | 8.5 | 8.5 | 8.8 |
| 70–74 years | 15.4 | 15.4 | 15.4 |
| 75–79 years | 19.0 | 19.1 | 18.9 |
| 80–84 years | 19.7 | 19.8 | 19.1 |
| ≥85 years | 25.1 | 25.3 | 24.1 |
| Gender | |||
| Male | 40.1 | 40.0 | 40.4 |
| Female | 59.9 | 60.0 | 59.6 |
| Race | |||
| White | 84.7 | 85.2 | 81.6 |
| Black | 11.3 | 11.2 | 11.9 |
| Other | 4.0 | 3.6 | 6.5 |
| Medicaid | |||
| No | 76.8 | 77.7 | 71.7 |
| Yes | 23.2 | 22.4 | 28.3 |
| Disabled | |||
| No | 89.4 | 89.7 | 87.6 |
| Yes | 10.6 | 10.3 | 12.4 |
| Patient prior medical history | |||
| HCC score prior to rehospitalization date (SD) | 2.05 (1.2) | 2.05 (1.2) | 2.04 (1.3) |
| 1st quartile (mean = 0.81) | 25.0 | 24.9 | 25.7 |
| 2nd quartile (mean = 1.44) | 25.0 | 25.0 | 25.2 |
| 3rd quartile (mean = 2.18) | 25.0 | 25.1 | 24.6 |
| 4th quartile (mean = 3.76) | 25.0 | 25.1 | 24.5 |
| Comorbidities | |||
| Hypertension | 75.4 | 75.3 | 76.0 |
| Fluid and electrolyte disorders | 36.7 | 36.6 | 37.5 |
| Congestive heart failure | 32.5 | 32.3 | 34.0 |
| Chronic pulmonary disease | 33.1 | 32.8 | 35.1 |
| Deficiency anemias | 28.3 | 28.3 | 28.6 |
| Diabetes, uncomplicated | 22.4 | 22.3 | 23.2 |
| Valvular disease | 16.8 | 17.0 | 15.6 |
| Hypothyroidism | 16.2 | 16.2 | 16.2 |
| Peripheral vascular disorders | 14.2 | 14.2 | 14.5 |
| Cardiac arrythmias | 36.9 | 37.0 | 36.3 |
| Other comorbidity | 61.8 | 61.9 | 61.5 |
| Index hospitalization | |||
| Length of stay in days (SD) | 6 (7) | 6 (7) | 6 (6) |
| 1–2 days | 23.6 | 23.6 | 23.9 |
| 3–4 days | 27.7 | 27.8 | 27.1 |
| 5–6 days | 17.6 | 17.6 | 17.4 |
| 7 or more days | 31.1 | 31.0 | 31.6 |
| Readmission hospital facility | |||
| Same as index facility | 77.7 | 78.6 | 72.5 |
| Different than index facility | 22.3 | 21.4 | 27.5 |
| Mortality from rehospitalization date | |||
| 30 days | 12.8 | 12.9 | 12.2 |
| Total payments from rehospitalization date | |||
| 30-day mean (SD) | 15,106 (12,137) | 15,137 (12,126) | 14,917 (12,203) |
| 30-day median [IQR] | 11,611 [7,212, 19,134] | 11,649 [7,240, 19,203] | 11,334 [7,032, 18,786] |
Abbreviations: SD=Standard deviation; HCC=Hierarchical Condition Category Score created through the Centers for Medicare and Medicaid Services; IQR=Interquartile range
Race data was missing for 68 subjects within the sample, index hospital for-profit status and medical school affiliation was missing for 3 subjects, and index hospital rural urban commuting area code was missing for 476 subjects.
Values represent percentages unless otherwise specified
Fourteen percent (10,607) of sample patients had their index hospitalization within a for-profit facility. These patients were slightly younger and more apt to be non-white, disabled, and on Medicaid than patients with index hospitalizations in not-for-profit/public facilities. These patients were also slightly more likely to have diagnoses of congestive heart failure and chronic pulmonary disease and slightly less likely to have valvular disease than patients with index hospitalizations in not-for-profit/public facilities. Other comorbidities did not differ by for-profit index hospital status. Gender mix, average Hierarchical Condition Category scores, and index hospitalization lengths of stay did not meaningfully differ by index hospital for-profit status. Unadjusted 30-day mortality and median total payments from the date of rehospitalization also did not differ between these groups. However, 28% of patients initially hospitalized in for-profit hospitals were rehospitalized to a different facility than their index hospital, compared to 21% of patients originating from non-profit/public hospitals (p-value <0.001).
Predictors for Rehospitalization to a Different Hospital
Table 2 shows adjusted risk ratios and corresponding predicted probabilities for the association of each variable within the predictive model to rehospitalization to a different hospital. After adjustment for geographic region and all other characteristics listed, the top four factors most related to the risk of rehospitalization to a different facility included being initially admitted to a for-profit index hospital (17% increased risk, p-value <0.001), being initially admitted to a lower volume index hospital (those with <1,000 annual discharges had 221% increased risk, p-value <0.001), being initially admitted to a hospital with a major medical school affiliation (18% increased risk, p-value <0.001) and being disabled (21% increased risk, p-value <0.001).
Table 2.
Predictors for Rehospitalization to a Different Hospital Facility for Medicare Beneficiaries with 30-Day Rehospitalizations, 2005–2006 (N=74,564)
| Characteristic* | Predictors for Rehospitalization to a Different Hospital (N=74,564) |
||
|---|---|---|---|
| Adjusted† Risk Ratio (95% CI) | P-Value | Predicted† Probability (95% CI) | |
| Index hospital characteristics | |||
| Hospital type | |||
| Non-profit/Public | 1.00 | (Reference) | 21.7 (21.4, 22) |
| For profit | 1.17 (1.13, 1.21) | <0.001 | 25.4 (24.5, 26.2) |
| Total discharge count category | |||
| >10,000 annual discharges | 1.00 | (Reference) | 18.2 (17.6, 18.8) |
| 6,001 – 10,000 annual discharges | 1.08 (1.03, 1.13) | <0.001 | 19.7 (19.1, 20.2) |
| 1,000 – 6,000 annual discharges | 1.34 (1.28, 1.39) | <0.001 | 24.3 (23.8, 24.8) |
| <1,000 annual discharges | 2.21 (2.07, 2.34) | <0.001 | 40.2 (38.2, 42.1) |
| Medical school affiliation | |||
| None | 1.00 | (Reference) | 21.3 (20.9, 21.7) |
| Minor | 1.03 (0.99, 1.07) | 0.090 | 21.9 (21.3, 22.6) |
| Major | 1.18 (1.14, 1.22) | <0.001 | 25.1 (24.4, 25.8) |
| Rural Urban Commuting Area Code for index hospital | |||
| Urban core area | 1.00 | (Reference) | 23.1 (22.8, 23.5) |
| Suburban area | 0.99 (0.9, 1.07) | 0.74 | 22.8 (20.8, 24.8) |
| Large town area | 0.77 (0.74, 0.81) | <0.001 | 17.9 (17.1, 18.6) |
| Small town and isolated rural area | 0.85 (0.79, 0.91) | <0.001 | 19.8 (18.4, 21.1) |
| Patient sociodemographic characteristics | |||
| Average age in years | |||
| <65 years | 1.00 | (Reference) | 22.9 (20.9, 25) |
| 65–69 years | 1.03 (0.92, 1.14) | 0.57 | 23.7 (22.6, 24.8) |
| 70–74 years | 1.06 (0.95, 1.17) | 0.27 | 24.3 (23.5, 25.2) |
| 75–79 years | 1.04 (0.93, 1.15) | 0.45 | 23.9 (23.1, 24.6) |
| 80–84 years | 0.93 (0.83, 1.03) | 0.182 | 21.3 (20.6, 22.1) |
| ≥85 years | 0.85 (0.76, 0.94) | 0.003 | 19.5 (18.9, 20.2) |
| Gender | |||
| Male | 1.00 | (Reference) | 23.1 (22.7, 23.6) |
| Female | 0.93 (0.91, 0.96) | <0.001 | 21.6 (21.2, 22) |
| Race | |||
| White | 1.00 | (Reference) | 22.1 (21.8, 22.4) |
| Black | 1.02 (0.98, 1.07) | 0.29 | 22.6 (21.7, 23.5) |
| Other | 1.10 (1.03, 1.18) | 0.005 | 24.3 (22.8, 25.9) |
| Medicaid | |||
| No | 1.00 | (Reference) | 22.2 (21.8, 22.5) |
| Yes | 1.01 (0.97, 1.04) | 0.60 | 22.4 (21.7, 23.1) |
| Disabled | |||
| No | 1.00 | (Reference) | 21.7 (21.3, 22.1) |
| Yes | 1.21 (1.09, 1.34) | <0.001 | 26.4 (24.0, 28.7) |
| Patient prior medical history | |||
| HCC score prior to rehospitalization date | |||
| 1st quartile (lowest) | 1.00 | (Reference) | 23.6 (22.9, 24.3) |
| 2nd quartile | 0.95 (0.91, 0.98) | 0.005 | 22.3 (21.7, 23.0) |
| 3rd quartile | 0.93 (0.89, 0.97) | 0.001 | 21.9 (21.3, 22.5) |
| 4th quartile (highest) | 0.89 (0.85, 0.94) | <0.001 | 21.1 (20.4, 21.7) |
| Comorbidities | |||
| Hypertension | 1.02 (0.98, 1.05) | 0.33 | 22.3 (22.0, 22.7) |
| Fluid and electrolyte disorders | 0.98 (0.95, 1.01) | 0.125 | 21.9 (21.4, 22.4) |
| Congestive heart failure | 1.00 (0.97, 1.04) | 0.81 | 22.3 (21.7, 22.9) |
| Chronic pulmonary disease | 0.92 (0.89, 0.95) | <0.001 | 21.0 (20.5, 21.6) |
| Deficiency anemias | 0.92 (0.89, 0.95) | <0.001 | 21.0 (20.4, 21.6) |
| Diabetes, uncomplicated | 1.00 (0.97, 1.03) | 1.00 | 22.2 (21.6, 22.9) |
| Valvular disease | 1.04 (1.00, 1.08) | 0.047 | 23.0 (22.2, 23.7) |
| Hypothyroidism | 0.98 (0.95, 1.02) | 0.35 | 21.9 (21.2, 22.7) |
| Peripheral vascular disorders | 0.98 (0.94, 1.02) | 0.30 | 21.8 (21.0, 22.7) |
| Cardiac arrythmias | 1.05 (1.02, 1.08) | 0.002 | 22.9 (22.4, 23.5) |
| Other comorbidity | 1.08 (1.05, 1.11) | <0.001 | 22.9 (22.5, 23.3) |
| Index hospitalization | |||
| Length of stay in days | |||
| 1–2 days | 1.00 | (Reference) | 24.1 (23.5, 24.8) |
| 3–4 days | 0.89 (0.86, 0.92) | <0.001 | 21.5 (21.0, 22.1) |
| 5–6 days | 0.90 (0.86, 0.94) | <0.001 | 21.7 (21.0, 22.4) |
| 7 or more days | 0.90 (0.87, 0.93) | <0.001 | 21.7 (21.2, 22.3) |
Abbreviations: CI=Confidence interval; HCC=Hierarchical Condition Category Score created through the Centers for Medicare and Medicaid Services
Race data was missing for 68 subjects within the sample; index hospital for-profit status and medical school affiliation was missing for 3 subjects; and index hospital rural urban commuting area code was missing for 476 subjects.
All characteristics were included in multivariate logistic regression models and adjusted for Centers for Medicare and Medicaid Services geographic billing region to produce the adjusted risk ratios (using methods by Kleinman et al.) and adjusted predicted probabilities shown.
A number of other factors were statistically significantly associated with rehospitalization to a different hospital, but, in general, these effects were smaller than the four listed above. Non-white/non-black (i.e., other race) patients were slightly more likely to be rehospitalized in a different hospital. Factors which slightly decreased this risk included being initially admitted to an index hospital in a large town or in a small town/isolated rural area, being 85 years or older, being female, and having a higher Hierarchical Condition Category score (i.e., being sicker) or a longer index hospital length of stay.
Reasons for Rehospitalization
Table 3 shows the top 10 most common reasons for index hospitalization for patients rehospitalized to the same hospital and the top 10 most common reasons for index hospitalization for patients rehospitalized to a different hospital. The top 2 most common rehospitalization reasons are also listed for each index reason. Notably, the ‘most common’ rehospitalization reason in each category was often the same as the index hospitalization reason.
Table 3.
Most Frequent Reasons for Rehospitalization According to the Reason for the Index Hospitalization, for Patients Rehospitalized at Same and at Different Hospitals, 2005–2006 (N=74,564)*
| Reasons for the Index Hospitalization, by Rehospitalization Site | Proportion of All Index Hospitalizations, by Site% (n) | Proportion of All 30-Day Rehospitalizations, by Site % (n) | Most Common Reasons for Rehospitalization, By Rehospitalization Site |
|
|---|---|---|---|---|
| Most Frequent (%) | 2nd Most Frequent (%) | |||
| Rehospitalized to the Same Hospital (N = 57,942) | N = 57,942 % (n) | |||
| Congestive Heart Failure (nonhypertensive) | 6.4 (3698) | 6.8 (3941) | Congestive Heart Failure (34) | Pneumonia (5) |
| Pneumonia (non-tuberculous) | 5.9 (3425) | 5.4 (3122) | Pneumonia (20) | Congestive Heart Failure (8) |
| Coronary Atherosclerosis and Other Heart Disease | 4.8 (2767) | 3.8 (2203) | Coronary Atherosclerosis (33) | Complications of Surgical Procedures or Medical Care (7) |
| Cardiac Dysrhythmias | 3.7 (2135) | 3.5 (2026) | Cardiac Dysrhythmias (26) | Congestive Heart Failure (10) |
| Chronic Obstructive Pulmonary Disease | 3.5 (2041) | 2.7 (1576) | Chronic Obstructive Pulmonary Disease (31) | Pneumonia (12) |
| Acute Myocardial Infarction | 3.4 (1971) | 1.0 (1131) | Coronary Atherosclerosis (19) | Congestive Heart Failure (15) |
| Acute Cerebrovascular Disease | 2.7 (1578) | 2.3 (1347) | Acute Cerebrovascular Disease (19) | Septicemia (5) |
| Fracture of Neck of Femur (Hip) | 2.6 (1531) | 0.9 (537) | Complication of Device; Implant or Graft (9) | Complications of Surgical Procedures or Medical Care (7) |
| Urinary Tract Infections | 2.5 (1434) | 2.5 (1421) | Urinary Tract Infection (12) | Pneumonia (7) |
| Septicemia | 2.3 (1333) | 3.8 (2190) | Septicemia (18) | Pneumonia (6) |
| Rehospitalized to a Different Hospital(N = 16,622) | N = 16,622% (n) | |||
| Congestive Heart Failure (nonhypertensive) | 5.7 (939) | 6.6 (1090) | Congestive Heart Failure (29) | Coronary Atherosclerosis (8) |
| Coronary Atherosclerosis and Other Heart Disease | 5.6 (932) | 5.4 (895) | Coronary Atherosclerosis (28) | Congestive Heart Failure (8) |
| Pneumonia (non-tuberculous) | 4.8 (792) | 4.8 (796) | Pneumonia (17) | Congestive Heart Failure (7) |
| Acute Myocardial Infarction | 4.0 (661) | 2.5 (420) | Coronary Atherosclerosis (18) | Acute Myocardial Infarction (16) |
| Cardiac Dysrhythmias | 3.7 (606) | 3.7 (613) | Cardiac Dysrhythmias (26) | Congestive Heart Failure (9) |
| Acute Cerebrovascular Disease | 3.4 (571) | 2.8 (461) | Acute Cerebrovascular Disease (20) | Aspiration Pneumonitis (5) |
| Fracture of Neck of Femur (Hip) | 2.4 (405) | 1.1 (178) | Septicemia (7) | Urinary Tract Infection (6) |
| Chronic Obstructive Pulmonary Disease | 2.4 (396) | 1.9 (314) | Chronic Obstructive Pulmonary Disease (21) | Pneumonia (11) |
| Osteoarthritis | 2.4 (391) | 0.4 (66) | Complications of Surgical Procedures or Medical Care (8) | Complication of Device; Implant or Graft (8) |
| Nonspecific Chest Pain | 2.1 (347) | 1.7 (281) | Coronary Atherosclerosis (27) | Nonspecific Chest Pain (7) |
Primary diagnoses for the index hospitalization are listed by decreasing proportion of index hospitalization in each rehospitalization category (same hospital versus different hospital). The primary diagnosis groups for both the index hospitalization and the rehospitalization were created using Clinical Classification software (Agency for Healthcare Research and Quality, 2003). Specific diagnosis levels within each diagnostic group include Single-Level Clinical Classification System levels of 108 for Congestive Heart Failure, 122 for Pneumonia, 101 for Coronary Atherosclerosis, 106 for Cardiac Dysrhythmias, 127 for Chronic Obstructive Pulmonary Disease, 100 for Acute Myocardial Infarction, 109 for Acute Cerebrovascular Disease, 226 for Fracture of Neck of Femur, 159 for Urinary Tract Infections, 2 for Septicemia, 203 for Osteoarthritis, 102 for Nonspecific Chest Pain, 237 for Complication of Device; Implant or Graft, 238 for Complications of Surgical Procedures or Medical Care, and 129 for Aspiration Pneumonitis.
30-Day Medicare Payments
Table 4 shows adjusted predicted payments for 30 days from the date of rehospitalization by same or different rehospitalization facility for patients at the low end (10%), median (50%), and high end (90%) of the cost-spectrum. Overall, rehospitalization to a different hospital was associated with a statistically significant increase in adjusted total 30-day payments at the 50% and 90% payment spectrum levels. The increase in adjusted 30-day payments at the median for rehospitalization to a different hospital was $1,308/patient. This pattern of significantly increased adjusted 30-day payments was maintained whether a patient had an index hospitalization in a for-profit hospital or in a not-for-profit/public hospital.
Table 4.
Predicted Total 30-Day Payments from the Date of Rehospitalization by Same or Different Rehospitalization Facility, Overall and Stratified by Index Hospital For-Profit Status (N = 74,564)
| Characteristic | Predicted Total 30-Day Payments* per Patient in US Dollars |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 10% | Difference (95% CI) | P- Value | 50% | Difference (95% CI) | P- Value | 90% | Difference (95% CI) | P- Value | |
| OVERALL MODEL | |||||||||
| Rehospitalized in same facility | 5,326 | (Ref.) | 12,167 | (Ref.) | 31,378 | (Ref.) | |||
| Rehospitalized in different facility | 5,412 | +87 (+2, +171) | 0.044 | 13,475 | +1308 (+1096, +1520) | <0.001 | 35,560 | +4182 (+3555, +4810) | <0.001 |
| STRATIFIED MODELS | |||||||||
| Not-for-profit/Public index hospital patients only | |||||||||
| Rehospitalized in same facility | 5,082 | (Ref.) | 11,860 | (Ref.) | 31,156 | (Ref.) | |||
| Rehospitalized in different facility | 5,137 | +56 (−40, +151) | 0.25 | 13,189 | +1329 (+1089, +1569) | <0.001 | 35,380 | +4225 (+3529, +4921) | <0.001 |
| For-profit index hospital patients only | |||||||||
| Rehospitalized in same facility | 5,721 | (Ref.) | 13,532 | (Ref.) | 32,269 | (Ref.) | |||
| Rehospitalized in different facility | 5,843 | +123 (−94, +339) | 0.27 | 14,627 | +1095 (+569, +1622) | <0.001 | 36,143 | +3874 (+2448, +5300) | <0.001 |
Abbreviations: Ref=Reference; CI=Confidence Interval
Quantile regression model producing predicted percentiles of total payments from the date of rehospitalization to 30-days after rehospitalization by rehospitalization facility (same or different), overall and stratified by index hospital for-profit status, controlled for patient characteristics of age, gender, race, Medicaid and disability status, comorbidities (hypertension, fluid and electrolyte disorders, congestive heart failure, chronic pulmonary disease, deficiency anemias, diabetes-uncomplicated, valvular disease, hypothyroidism, peripheral vascular disorders, cardiac arrythmias, and an indicator denoting the presence of other comorbidity), index hospital length of stay and Center for Medicare and Medicaid Service’s Hierarchical Condition Category Score; and Index hospital characteristics of annual discharge number, teaching status, for-profit status (omitted in stratified models), billing region and rural-urban community area code. 95% Confidence intervals were bootstrapped using 1000 analytic repetitions.
30-Day Mortality
Table 5 shows adjusted risk ratios and corresponding predicted probabilities for mortality 30 days from the date of rehospitalization by same or different rehospitalization facility. Patients rehospitalized to the same and different hospitals exhibited no significant differences in adjusted 30-day mortality. This pattern held true regardless of index hospital for-profit status.
Table 5.
30-Day Mortality from the Date of Rehospitalization by Same or Different Rehospitalization Facility, Overall and Stratified by Index Hospital For-Profit Status (N = 74,564)
| Characteristic | 30-Day Mortality |
||
|---|---|---|---|
| Adjusted* Risk Ratio (95% CI) | P-Value | Predicted* Probability (95% CI) | |
| OVERALL MODEL | |||
| Rehospitalized in same facility | 1.00 | (Reference) | 12.7 (12.5, 13.0) |
| Rehospitalized in different facility | 1.01 (0.96, 1.06) | 0.68 | 12.9 (12.3, 13.4) |
| STRATIFIED MODELS | |||
| Not-for-profit/Public index hospital patients only | |||
| Rehospitalized in same facility | 1.00 | (Reference) | 12.9 (12.6, 13.1) |
| Rehospitalized in different facility | 1.01 (0.96, 1.06) | 0.77 | 13.0 (12.4, 13.5) |
| For-profit index hospital patients only | |||
| Rehospitalized in same facility | 1.00 | (Reference) | 12.1 (11.4, 12.8) |
| Rehospitalized in different facility | 1.01 (0.90, 1.13) | 0.81 | 12.3 (11.1, 13.5) |
Abbreviation: CI=Confidence interval
Logistic regression models producing adjusted risk ratios (using methods by Kleinman et al.) and adjusted predicted probabilities for death within 30 days of rehospitalization by rehospitalization facility (same or different), overall and by index hospital for-profit status controlled for patient characteristics of age, gender, race, Medicaid and disability status, comorbidities (hypertension, fluid and electrolyte disorders, congestive heart failure, chronic pulmonary disease, deficiency anemias, diabetes-uncomplicated, valvular disease, hypothyroidism, peripheral vascular disorders, cardiac arrythmias, and an indicator denoting the presence of other comorbidity), index hospital length of stay and Center for Medicare and Medicaid Service’s Hierarchical Condition Category Score; and Index hospital characteristics of annual discharge number, teaching status, for-profit status (omitted in stratified models), billing region and rural-urban community area code.
DISCUSSION
In summary, we demonstrated that Medicare rehospitalizations to different hospitals were common in 2005–2006, and were most strongly predicted by index hospital traits (i.e., for-profit status, major medical school affiliation, and volume) and patient disability. These factors outweighed the effects of age and disease considerably. Patients with rehospitalizations to different hospitals had higher total 30-day payments, but no differences in 30-day mortality, when compared to their counterparts rehospitalized to the same hospitals. These findings raise concerns that select patients with imminent rehospitalizations are being diverted to different hospitals for reasons other than disease severity at a cost to the Medicare program and without 30-day mortality benefit.
The higher payments incurred by Medicare patients rehospitalized in different hospitals may be explained, in part, by the fundamental lack of US health system interconnectivity. In most modern health care transitions, the patient/caregiver navigates alone amongst a multitude of settings (40). Physicians and other team members commonly restrict practice to single settings (41) and active care coordination is often absent (41). No universal medical record exists to inform medical teams at different hospitals of a new patient’s previous medical history or treatments (2). The discharge summary, a hospital’s primary discharge-communication tool, is frequently of poor quality and often unavailable during the early post-hospital period (3). This lack of communication and coordination may result in delayed medical treatments and in the duplication of costly diagnostic tests, procedures, and therapies; especially considering our finding that reasons for rehospitalization frequently mirror those of the original hospital stay. This inefficiency of care may have negative implications for the health of both the Medicare patient and system (42). Additional research examining the impact of poor inter-facility communication, and incentives to encourage improved inter-facility communication/coordination are needed.
The factors which most strongly predict rehospitalization to different hospitals are remarkable in their predominantly non-medical/non-disease severity nature. Previous studies have shown that non-medical and patient financial factors influence provider decisions to triage patients to other hospitals (4–9). However, this is the first study to specifically consider rehospitalizations, and the first to assess how hospital-specific factors influence this practice (English-language PUBMED search to January 2010).
We can speculate regarding possible explanations for the pre-eminence of these predictors in patient diversion. First, hospitals with low volume often lack access to specific medical expertise that would allow them to have the confidence to manage the most complex of rehospitalized patients (43–46). This lack of expertise/confidence may result in a greater number of patient diversions. Hospitals with major medical school affiliations may encounter high demand for services and high censuses which necessitate patient diversions (47, 48). However, in the cases of index hospital for-profit status and disabled patients, the reasons for patient diversions are less clear. During a rehospitalization, the original/index hospital likely understands the patient’s needs in depth, and as a result, may be able to project future costs/needs to some degree. It is possible that certain facilities could use this information to be selective in their rehospitalizations, more frequently diverting “less-desirable” patients for readmission elsewhere (4, 10). Additional research is needed to better understand the patient, clinical, and system motivations underlying patient diversion.
Our findings should be considered in light of the forthcoming enactment of the new Medicare rehospitalization payment reforms (the Hospital Readmissions Reduction Program) (13–18). These reforms would aim to reduce 30-day rehospitalizations by monetarily penalizing hospitals with rehospitalization rates significantly above the national average (13, 14, 18). However, in such a system, a hospital may have incentive to divert less-desirable patients to other facilities for their care, especially at the point of index admission or just beyond the 30-day rehospitalization timeframe. Our findings suggest that some diversions/loss of continuity may increase Medicare payments, and may disproportionately affect the disabled. Additional research is needed on patient diversions outside of the 30-day rehospitalization timeframe before any definitive policy recommendations can be made.
Our study is limited by our use of Medicare data, which provides excellent measures of payments and rehospitalizations, but is limited in its ability to provide detailed insight into specific practice motivations. Although this approach provides important data on predictors for rehospitalizations to different hospitals, it cannot assess whether or not a diversion was in the patient’s best interest and is inherently limited in its measures of geographic proximity, primary care involvement, and detailed clinical information. However, the weak predictive role of disease-specific factors may suggest that non-medical patient and hospital factors play a major role in this diversion decision. Like many studies of readmission, this study cannot be applied to non-Medicare populations. Furthermore, we are unable to comment upon the role of patient choice. It is possible that transient/migratory populations and/or patient dissatisfaction with an index hospital may cause the patient to actively choose to be rehospitalized elsewhere. Although studies have previously shown that non-acutely ill patients clearly exert their preferences when choosing a hospital for an elective procedure (49), it is likely that acutely ill patients needing emergent rehospitalization have much less time or ability to exercise choice (49–51). These issues are in great need for additional study.
In conclusion, rehospitalizations to different hospitals are common, are most strongly predicted by non-disease factors, and are related to increased Medicare payments without improved 30-day mortality. Further study of how transitional care, inter-facility communication, and care coordination impact costs and quality of care is needed.
Acknowledgments
Financial Support: Funding for this project was provided by the University of Wisconsin (UW) Hartford Center of Excellence in Geriatrics and the UW Health Innovation Program. Dr. Kind is supported by a K-L2 through the NIH grant 1KL2RR025012-01 [Institutional Clinical and Translational Science Award (UW-Madison) 1UL1RR025011 (KL2) program of the National Center for Research Resources, National Institute of Health]. Additional support was provided by the Health Innovation Program and the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UW ICTR), grant 1UL1RR025011 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources, National Institutes of Health. The UW Health Innovation Program provided assistance with IRB application, Medicare data management, variable creation and manuscript formatting. No other funding source had a role in the design or conduct; data collection, management, analysis or interpretation; or preparation, review or approval of the manuscript.
Special thanks to UW Health Innovation Program staff Robert Purvis for data management and variable creation and to Colleen Brown for manuscript formatting.
Footnotes
Protocol: Available to interested readers by contacting Dr. Kind at ajk@medicine.wisc.edu
Statistical Code: Available to interested readers by contacting Dr. Kind at ajk@medicine.wisc.edu
Data: Available for purchase through the Centers for Medicare and Medicaid Services’ Chronic Condition Data Warehouse website at http://ccwdata.org/index.php
The authors do not have any potential conflicts of interest.
Publisher's Disclaimer: This is the prepublication, author-produced version of a manuscript accepted for publication in Annals of Internal Medicine. This version does not include post-acceptance editing and formatting. The American College of Physicians, the publisher of Annals of Internal Medicine, is not responsible for the content or presentation of the author-produced acceptedz version of the manuscript or any version that a third party derives from it. Readers who wish to access the definitive published version of this manuscript and any ancillary material related to this manuscript (e.g., correspondence, corrections, editorials, linked articles) should go to www.annals.org or to the print issue in which the article appears. Those who cite this manuscript should cite the published version, as it is the official version of record.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Goldsmith J, Blumenthal D, Rishel W. Federal health information policy: a case of arrested development. Health Aff (Millwood) 2003;22:44–55. doi: 10.1377/hlthaff.22.4.44. [DOI] [PubMed] [Google Scholar]
- 3.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care. JAMA. 2007;297:831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- 4.Cram P, Pham HH, Bayman L, Vaughan-Sarrazin MS. Insurance status of patients admitted to specialty cardiac and competing general hospitals: are accusations of cherry picking justified? Med Care. 2008;46:467–475. doi: 10.1097/MLR.0b013e31816c43d9. [DOI] [PubMed] [Google Scholar]
- 5.Koval KJ, Tingey CW, Spratt KF. Are patients being transferred to level-I trauma centers for reasons other than medical necessity? J Bone Joint Surg Am. 2006;88:2124–2132. doi: 10.2106/JBJS.F.00245. [DOI] [PubMed] [Google Scholar]
- 6.Nathens AB, Maier RV, Copass MK, Jurkovich GJ. Payer status: The unspoken triage criterion. J Trauma. 2001;50:776–783. doi: 10.1097/00005373-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a level-I trauma center. J Bone Joint Surg Am. 2007;89:2625–2631. doi: 10.2106/JBJS.F.01499. [DOI] [PubMed] [Google Scholar]
- 8.Berman L, Rosenthal MS, Moss RL. The paradoxical effect of medical insurance on delivery of surgical care for infants with congenital anomalies. J Pediatr Surg. 2010;45:38–43. doi: 10.1016/j.jpedsurg.2009.10.006. discussion 44. [DOI] [PubMed] [Google Scholar]
- 9.Smedley BD, Stith AY, Nelson AR. Washington, D.C: Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, The National Academies Press; 2003. [August 12, 2010]. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Accessed at http://www.nap.edu/openbook.php?record_id=12875&page=1. [PubMed] [Google Scholar]
- 10.Casalino LP, Devers KJ, Brewster LR. Focused factories? Physician-owned specialty facilities. Health Aff (Millwood) 2003;22:56–67. doi: 10.1377/hlthaff.22.6.56. [DOI] [PubMed] [Google Scholar]
- 11.Kessler DP, McClellan MB. The effects of hospital ownership on medical productivity. Rand J Econ. 2002;33:488–506. [PubMed] [Google Scholar]
- 12.Duggan M. Hospital market structure and the behavior of not-for-profit hospitals. Rand J Econ. 2002;33:433–446. [PubMed] [Google Scholar]
- 13.Patient Protection and Affordable Care Act, H.R. 3590, Sec. 3025 (2010).
- 14.Medicare Payment Advisory Commission. Promoting Greater Efficiency in Medicare. Washington, D.C: MedPAC; 2007. [Google Scholar]
- 15.Medicare Payment Advisory Commission. A Path to Bundled Payment Around a Hospitalization. Washington, D.C: MedPAC; 2008. [Google Scholar]
- 16.Medicare Payment Advisory Commission. Improving Incentives in the Medicare Program. Washington, D.C: MedPAC; 2009. [Google Scholar]
- 17.Department of Health and Human Services. 42 CFR Parts 411, 412, 413, 422, and 489. Washington, D.C: Centers for Medicare and Medicaid Services; 2008. [Google Scholar]
- 18.Bhalla R, Kalkut G. Could Medicare readmission policy exacerbate health care system inequity? Ann Intern Med. 2010;152:114–117. doi: 10.7326/0003-4819-152-2-201001190-00185. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Medicare & Medicaid Services. Chronic Condition Data Warehouse (CCW) home page. West Des Moines, IA: Buccaneer Computer Systems and Service, Inc; 2009. [March 9, 2009]. Accessed at http://ccwdata.org. [Google Scholar]
- 20.Centers for Medicare & Medicaid Services. Chronic Condition Data Warehouse User Manual, version 1.6. West Des Moines, IA: Buccaneer Computer Systems and Service, Inc; 2010. [August 12, 2010]. Accessed at http://ccwdata.org/downloads/CCW_UserManual.pdf. [Google Scholar]
- 21.Kind AJH, Smith MA, Frytak JR, Finch MD. Bouncing back: patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. J Am Geriatr Soc. 2007;55:365–373. doi: 10.1111/j.1532-5415.2007.01091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kind AJ, Smith MA, Liou JI, Pandhi N, Frytak JR, Finch MD. Discharge destination’s effect on bounce-back risk in Black, White, and Hispanic acute ischemic stroke patients. Arch Phys Med Rehabil. 2010;91:189–195. doi: 10.1016/j.apmr.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pope GC, Kautter J, Ellis RP, Ash AS, Ayanian JZ, Lezzoni LI, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25:119–141. [PMC free article] [PubMed] [Google Scholar]
- 24.Elixhauser A, Steiner C, Harris DR, Coffey RN. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Clinical Classifications Software (ICD-9-CM): Summary and Downloading Information [Computer program] Rockville, MD: Agency for Healthcare Research and Quality; 2003. [Google Scholar]
- 26.Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) 2010 User’s Guide. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [August 12, 2010]. Accessed at http://www.hcup-us.ahrq.gov/toolssoftware/ccs/CCSUsersGuide.pdf. [Google Scholar]
- 27.Sharma G, Fletcher KE, Zhang D, Kuo YF, Freeman JL, Goodwin JS. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. JAMA. 2009;301:1671–1680. doi: 10.1001/jama.2009.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Economic Research Service, United States Department of Agriculture. Measuring Rurality: Rural-Urban Commuting Area Codes. Washington, D.C: United States Department of Agriculture Economic Research Service; [March 9, 2010]. Accessed at http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/ [Google Scholar]
- 29.Washington State Department of Health. A four-tier consolidation of the RUCA system at the sub-county level. Olympia, WA: Washington State Department of Health; [March 9, 2010]. Accessed at http://www.doh.wa.gov/data/Guidelines/RuralUrban2.htm#fourtier. [Google Scholar]
- 30.Yuan Z, Cooper GS, Einstadter D, Cebul RD, Rimm AA. The association between hospital type and mortality and length of stay: a study of 16.9 million hospitalized Medicare beneficiaries. Med Care. 2000;38:231–245. doi: 10.1097/00005650-200002000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Peterson ED, Jollis JG, Bebchuk JD, Delong ER, Muhlbaier LH, Mark DB, et al. Changes in mortality after myocardial revascularization in the elderly - the national Medicare experience. Ann Intern Med. 1994;121:919–927. doi: 10.7326/0003-4819-121-12-199412150-00003. [DOI] [PubMed] [Google Scholar]
- 32.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 33.Kleinman LC, Norton EC. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44:288–302. doi: 10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Localio AR, Margolis DJ, Berlin JA. Relative risks and confidence intervals were easily computed indirectly from multivariable logistic regression. J Clin Epidemiol. 2007;60:874–882. doi: 10.1016/j.jclinepi.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 35.Greene W. Econometric analysis. 3. Englewood Cliffs, NJ: Prentice Hall; 1997. [Google Scholar]
- 36.SAS Statistical Software [Computer program]. Version 9.2. Cary, NC: SAS Institute; 2009. [Google Scholar]
- 37.Stata Statistical Software [Computer program]. Version 11.0. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- 38.Efron B. 1977 Rietz lecture - Bootstrap methods: Another look at the jackknife. Ann Stat. 1979;7:1–26. [Google Scholar]
- 39.Carpenter J, Bithell J. Bootstrap confidence intervals: when, which, what? A practical guide for medical statisticians. Stat Med. 2000;19:1141–1164. doi: 10.1002/(sici)1097-0258(20000515)19:9<1141::aid-sim479>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 40.Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–536. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 41.Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 42.Fisher ES, McClellan MB, Bertko J, Lieberman SM, Lee JJ, Lewis JL, et al. Fostering accountable health care: Moving forward in Medicare. Health Aff (Millwood) 2009;28:w219–231. doi: 10.1377/hlthaff.28.2.w219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Billingsley KG, Morris AM, Dominitz JA, Matthews B, Dobie S, Barlow W, et al. Surgeon and hospital characteristics as predictors of major adverse outcomes following colon cancer surgery - Understanding the volume-outcome relationship. Arch Surg. 2007;142:23–31. doi: 10.1001/archsurg.142.1.23. [DOI] [PubMed] [Google Scholar]
- 44.Elixhauser A, Steiner C, Fraser I. Volume thresholds and hospital characteristics in the United States. Health Aff (Millwood) 2003;22:167–177. doi: 10.1377/hlthaff.22.2.167. [DOI] [PubMed] [Google Scholar]
- 45.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 46.Sosa JA, Bowman HM, Gordon TA, Bass EB, Yeo CJ, Lillemoe KD, et al. Importance of hospital volume in the overall management of pancreatic cancer. Ann Surg. 1998;228:429–436. doi: 10.1097/00000658-199809000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weiss SJ, Derlet R, Arndahl J, Ernst AA, Richards J, Fernandez-Frankelton M, et al. Estimating the degree of emergency department overcrowding in academic medical centers: Results of the national ED overcrowding study (NEDOCS) Acad Emerg Med. 2004;11:38–50. doi: 10.1197/j.aem.2003.07.017. [DOI] [PubMed] [Google Scholar]
- 48.Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20:402–405. doi: 10.1136/emj.20.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luft HS, Garnick DW, Mark DH, Peltzman DJ, Phibbs CS, Lichtenberg E, et al. Does quality influence choice of hospital? JAMA. 1990;263:2899–2906. [PubMed] [Google Scholar]
- 50.Mukamel DB, Weimer DL, Mushlin AI. Interpreting market share changes as evidence for effectiveness of quality report cards. Med Care. 2007;45:1227–1232. doi: 10.1097/MLR.0b013e31812f56bb. [DOI] [PubMed] [Google Scholar]
- 51.Kolstad JT, Chernew ME. Quality and consumer decision making in the market for health insurance and health care services. Med Care Res Rev. 2009;66:28S–52S. doi: 10.1177/1077558708325887. [DOI] [PubMed] [Google Scholar]