Abstract
Androgen deprivation therapy is the major treatment for advanced prostate cancer (PCa). However, it is a temporary remission, and the patients almost inevitably develop hormone refractory prostate cancer (HRPC). HRPC is almost incurable, although most HRPC cells still express androgen receptor (AR) and depend on the AR for growth, making AR a prime drug target. Here, we provide evidence that epigallocatechin-3-gallate (EGCG), the major polyphenol in green tea, is a direct antagonist of androgen action. In silico modeling and FRET-based competition assay showed that EGCG physically interacts with the ligand-binding domain of AR by replacing a high-affinity labeled ligand (IC50 0.4 μM). The functional consequence of this interaction was a decrease in AR-mediated transcriptional activation, which was due to EGCG mediated inhibition of interdomain N-C termini interaction of AR. Treatment with EGCG also repressed the transcriptional activation by a hotspot mutant AR (T877A) expressed ectopically as well as the endogenous AR mutant. As the physiological consequence of AR antagonism, EGCG repressed R1881-induced PCa cell growth. In a xenograft model, EGCG was found to inhibit AR nuclear translocation and protein expression. We also observed a significant down-regulation of androgen-regulated miRNA-21 and up-regulation of a tumor suppressor, miRNA-330, in tumors of mice treated with EGCG. Taken together, we provide evidence that EGCG functionally antagonizes androgen action at multiple levels, resulting in inhibition of PCa growth.—Siddiqui, I. A., Asim, M., Hafeez, B. B., Adhami, V. M., Tarapore, R. S., Mukhtar, H. Green tea polyphenol EGCG blunts androgen receptor function in prostate cancer.
Keywords: androgen antagonist, androgen receptor signaling, androgen-regulated miRNA, hormone-refractory prostate cancer
Prostate cancer (PCa) in men is a serious health problem worldwide and a leading cause of cancer-related deaths in the United States, ranking second to lung cancer in terms of annual mortality (1, 2). The androgen receptor (AR) plays an important role in both early and advanced stages of PCa etiology. The AR is expressed to some degree in nearly all primary PCas (3–5), and studies in both human and animal models suggest a relationship between cellular AR level in both primary and metastatic lesions and subsequent disease progression (6–8). AR, which is a member of the nuclear hormone receptor superfamily, manifests the biological action of male sex hormones, testosterone and dihydrotestosterone. AR protein has a modular structure containing the N terminus harboring transcriptional activation domains, a central DNA-binding domain (DBD), and a C-terminal ligand-binding domain (LBD). Binding of androgens to the LBD induces conformational change in the AR and subsequently results in the shuttling of the receptor to the nucleus, where it forms a homodimer that is recruited on the androgen response element (ARE) present in the regulatory element on the target genes. In doing so, AR regulates growth of prostate gland by modulating the expression of many other target genes implicated in growth and proliferation (9, 10). To block AR function, androgen ablation in conjunction with antiandrogens remains the mainstay therapy for advanced PCa. This treatment unfortunately proves ineffective, as the hormone-refractory tumor, for which no curative therapy exists, eventually emerges in a short span of 6–12 mo (11). It is noteworthy that hormone-refractory PCa (HRPC) cells remain dependent on functional AR signaling, as their growth is severely compromised if AR is depleted in cells using RNAi or ribozyme (12–14). This makes AR the prime drug target and AR-regulated genes potential biomarkers in the treatment and diagnosis of advanced HRPC.
Although PCa is on a sharp rise in the west, epidemiological data suggest that its incidence has been especially low in East Asian countries where green tea is a popular beverage. This low occurrence of PCa might be explained partly by the fact that oral consumption of green tea polyphenols containing epigallocatechin-3-gallate (EGCG; see structure in Fig. 1B, inset) has demonstrated remarkable chemopreventive effects in PCa experimental models. Similar chemopreventive effects of green tea consumption have been observed in a few recent human intervention studies (15, 16). EGCG has also been shown to decrease the growth of PCa cells, accompanied by the reduction of prostate-specific antigen, a well-known biomarker of PCa burden in humans (17, 18). Although previous studies have demonstrated a role of EGCG in the regulation of AR (19–22), the mechanism of the effects of EGCG is not known. Here we provide evidence that EGCG blunts AR function in PCa.
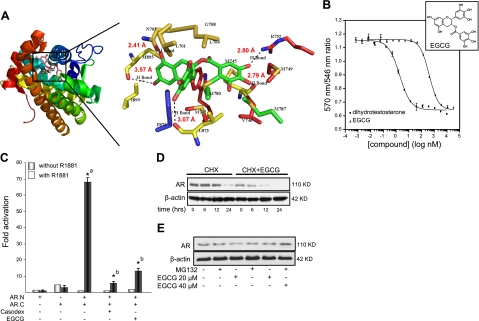
Figure 1.
A) Predicted model for EGCG binding to AR-LBD. Left panel: EGCG binds to AR-LBD in in silico molecular docking studies, using AutoDock software and 2PNU.pdb as the starting receptor. Different domains of the AR are distinguished by color. Right panel: enlarged view of boxed area in left panel, with putative binding sites in the model structure of the AR. Predicted distances of hydrogen bonds (Å) are given next to the bonds. B) EGCG competitively interacts with AR-LBD and decreases its interdomain interaction. EGCG competes with the high-affinity androgen Fluormone AL Red to physically interact with AR-LBD. Data are presented as averages ± se of two sample wells. Inset: structure of EGCG. C) AR N-C-interaction assay was performed in CV1 cells as described in Materials and Methods. Graphs represent fold of hormone induction compared with value for the non-hormone-treated group, which was set as 1. *aP < 0.01 vs. AR.N or AR.C group; *bP < 0.01 vs. AR.N+AR.C group; 1-way ANOVA followed by Tukey's HSD test. D) Effect of EGCG on AR protein turnover in LNCaP cells. Cells were treated with 40 μM EGCG and 50 μg/ml cycloheximide for the indicated time periods. AR protein levels were determined by Western blot analysis with specific antibody against AR and normalized to β-actin as loading control. E) LNCaP cells were exposed to indicated concentrations of EGCG for 48 h with or without 5 μM of MG132. AR protein levels were determined by Western blot analysis with specific antibody against AR and normalized to β-actin as loading control.
By using in silico data for AR binding to EGCG and then employing ligand competition assay, we showed that EGCG interacts competitively with the LBD of AR, validating the in silico data. This interaction resulted in the inhibition of AR-dependent transcription, and EGCG treatment also led to growth inhibition of human prostate carcinoma cells. EGCG was observed subsequently to inhibit nuclear translocation and protein expression of AR in a tumor xenograft model. We provide further evidence that microRNAs (miRNAs) that are regarded to play a role in PCa are regulated by EGCG in tumors isolated from mice. Thus, we provide evidence that EGCG possesses antiandrogenic activity that could explain the potential of green tea as a PCa chemopreventive agent.
MATERIALS AND METHODS
In silico molecular modeling study
EGCG was tested in silico for its ability to bind with the AR using the AutoDock4 software (Scripps Research Institute, La Jolla, CA, USA), utilizing 2PNU.pdb as the starting receptor docking site. The AutoDock suite of programs, which was used for the docking calculations, uses an automated docking approach that allows ligand flexibility. Default parameters (including distance-dependent dielectric constants) were used as described in the AutoDock manual. The docking modes in our study were chosen on the basis of distance between the carbonyl carbon of (−)-EGCG and the hydroxyl oxygen of the AR, and the lowest free docked energy (negative ΔG) was chosen for such a binding conformation. We also analyzed hydrogen-bond formation. In this study, we chose to use the docked free energies, since the number of rotatable bonds in AR is relatively constant, and we believe that the internal energy of the ligand should not be neglected for EGCG. It is worth mentioning that the docked free energies (or binding free energies) that one obtains might always vary depending on the precise force field parameters (charges, electrostatic treatment, etc.) in use.
Cell culture
The LNCaP and 22Rν1 cells were obtained from American Type Culture Collection (Manassas, VA, USA). The LNCaP and CV1 cells were cultured in DMEM, 22Rν1 cells were grown in RPMI 1640, and C4-2 cells were maintained in T-medium. All cells were maintained under standard cell culture conditions supplemented with 10% FBS and 1% penicillin/streptomycin at 37°C and 5% CO2 environment. EGCG dissolved in deionized water was used for the treatment of cells.
Cell viability assay
The effect of EGCG on cell viability was determined by 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazoliumbromide (MTT) assay. For the second set of experiments, cells were treated with agonistic ligand R1881 (1 nM), Casodex (0.1 μM), and the combination of R1881 (1 nM) and EGCG (10–60 μM) for 6 d. After incubation for specified times at 37°C, MTT assay was performed as described previously (23).
Transient transfection and reporter assays
Transient transfection for reporter assays was done using the standard calcium phosphate method (24) with minor modifications. LNCaP cells were seeded in 6-well dishes in DMEM supplemented with 10% hormone-depleted FBS and were transfected 16 h later with 1 μg of MMTV-Luc reporter plasmid and 50 ng of Renilla luciferase plasmid (Promega, Madison, WI, USA). After 8 h, cells were provided fresh medium and treated with R1881 (1 nM) and EGCG (10–60 μM). Cells were harvested 72 h post-transfection, and both luciferase and Renilla luciferase activities were measured using a dual luciferase assay reagent kit (Promega). For PSA-Luc reporter assay, transfection was done with an Amaxa electroporation kit (Lonza Walkersville Inc., Walkersville, MD, USA) with 2 μg of PSA-Luc reporter; after electroporation, cells were treated as above. For AR amino-terminal/carboxyl-terminal (N-C)-interaction assay, CV1 cells were transfected with pSVARN1 (N terminus of the human AR sequence aa 1–494, covering the major transactivation unit TAU1) and/or pSVARC (aa 528–910 of the human AR, covering the DBD and LBD of AR) plasmids (250 ng each), 1 μg MMTV-Luc, and 100 ng Renilla luciferase plasmid using standard calcium phosphate transfection methods and were treated as described above. For reporter assays, CV1 cells were transfected with 2 μg T877A mutant/well in a 6-well tissue culture dish using the calcium phosphate transfection method and were later treated and harvested as mentioned above.
Time-resolved fluorescence resonance energy transfer (FRET) assay
The Invitrogen method to identify AR ligands (Polarscreen Androgen Receptor Competitor Assay, Red; Invitrogen, Carlsbad, CA, USA) was used to test the ligand-binding potential of EGCG. The binding assay was followed as described earlier (25). DHT was included as the reference control competitor. Briefly, in this assay, the ligands for AR are identified by their ability to compete with and displace a high-affinity AR ligand, Fluormone AL Red, from the receptor. The binding constant of Fluormone AL Red to AR-LBD is known to be 12 nM, according to a prior study (25). Binding of agonist to the nuclear receptor causes a conformational change around helix 12 in the LBD, resulting in higher affinity for the coactivator peptide. When the terbium label on the anti-glutathione S-transferase (GST) antibody is excited at 340 nm, energy is transferred to the fluorescein label on the coactivator peptide and detected as emission at 520 nm. This assay uses AR sequences corresponding to the protein domain bearing the hinge and ligand-binding domains (aa 606–902; NP_036634) and tagged with both GST and 6× histidine (His) at the N terminus (25). Mutant rat AR-LBD bearing a threonine to alanine change corresponding to residue 877 (AR T877A) was prepared as described previously (25). The rat sequence used in this study was identical to human AR-LBD. The AR-LBD is added to the tracer Fluormone AL Red in the presence of a test compound (EGCG in our case) in a microtiter plate, and the polarization value of the tracer is measured. For this assay, the test compound does not have to be labeled fluorescently. The shift in polarization value is used to determine the relative affinity of the test compound for AR-LBD. If the test compound binds to the receptor, it will prevent the formation of the receptor/tracer complex, and the tracer will be free in solution. When the tracer is free in solution, its rotational mobility is greater than when bound to the receptor, resulting in a low polarization value. If the test compound does not bind to the receptor, it will have no effect on formation of the receptor/tracer complex, and the measured polarization value of the tracer will remain high. A purified, GST-tagged AR-LBD (1 nM) is labeled indirectly with a terbium-labeled anti-GST tag antibody (5 nM). Binding of Fluormone AL Red (1 μM solution) to AR is then measured by monitoring FRET from the terbium-labeled anti-GST tag antibody to the red fluorescent ligand, resulting in a high time-resolved FRET ratio (570-nm/546-nm fluorescent emission). Curve for the FRET ratio was fit using a sigmoidal dose-response equation with varying slope using Prism software (GraphPad Software, Inc., San Diego, CA, USA). Serial dilutions of DHT and EGCG were done in 100% DMSO at 100× the final screening concentration.
AR protein stability assay
LNCaP cells were treated with 40 μM EGCG and 50 μg/ml cycloheximide for 0, 6, 12, and 24 h, followed by the preparation of whole cell lysates. Cycloheximide was added to the medium 30 min before the addition of EGCG. AR protein levels were determined by Western blot analysis with specific antibody against AR and normalized to β-actin control.
Immunohistochemical analysis
Sections (4 μm) were cut from paraffin-embedded tumor xenograft tissues, which were obtained from a previous study (18). Immunohistochemical staining was performed using specific AR antibody at 1:50 dilution (sc-815; Santa Cruz Biotechnology, Santa Cruz, CA, USA). Antibody was replaced with either normal host serum or block, which served as negative controls. This was followed by staining with appropriate biotin-conjugated secondary antibodies (1:500 dilution); later, the sections were incubated with Vectastain ABC reagent (Vector Laboratories, Burlingame, CA, USA). The slides were developed in diaminobenzidine and counterstained with a weak solution of hematoxylin, as described previously (26). The stained slides were dehydrated and mounted in Permount (Fisher Scientific, Hampton, NH, USA) and visualized on a Zeiss-Axiophot DM HT microscope (Carl Zeiss, Jena, Germany). Images were captured with an attached camera linked to a computer.
Immunofluorescence imaging
Sections, 4–8 μm thick, were cut from frozen blocks of tumor xenograft tissues, which were obtained from a previous study (13), and mounted on superfrost plus slides. Slides were stored at −80°C until needed. Before staining, slides were warmed at room temperature for 5 min and fixed in ice-cold acetone for 15 min at 4°C, followed by washing in PBS-Tween 20. Slides were then blocked with normal serum block followed by incubation with AR antibody at 1:50 dilution (sc-815; Santa Cruz Biotechnology) in blocking buffer. After rinsing in PBS-Tween 20, slides were incubated with fluorescent-conjugated secondary antibody at 1:350 dilution in blocking buffer. Slides were then rinsed in PBS-Tween 20, and sections were mounted with ProLong Gold Antifade reagent containing DAPI (Invitrogen) and left in dark overnight. For analysis, the Nikon Eclipse Ti system (Nikon Instruments Inc., Tokyo, Japan) was used.
Real-time PCR analysis for miRNA expression
Real-time PCR-based miRNA expression profiling was performed on a real-time PCR instrument (Applied Biosystems, Foster City, CA, USA) by using the RT2 miRNA qPCR assay kit (SABiosciences, Frederick, MD, USA) by following the supplier's protocol. Briefly, RNA was extracted from the tumor tissues using TRIzol (Invitrogen), and small RNA was enriched using the RT2 qPCR miRNA isolation kit (SABiociences). This highly pure small RNA was reverse-transcribed using the RT2 miRNA first-strand kit, and the resulting cDNA was utilized in real-time PCR, performed using the primers supplied in the kit for individual miRNAs. Threshold cycle (CT) values obtained from the instrument's software were used to calculate the fold change of the respective miRNAs. ΔCT was calculated by subtracting the CT value of the housekeeping gene from that of the miRNA of interest. ΔΔCT for each miRNA was then calculated by subtracting the CT value of the control from the experiemental value. Fold change was calculated by the formula 2−ΔΔCT.
Statistical analysis
All statistical analysis was performed by using VassarStats software (Vassar College, Poughkeepsie, NY, USA). Data are expressed as means with 95% confidence intervals for all groups. Statistical significance of differences in all measurements between control and treated groups was determined by 1-way ANOVA followed by Tukey's HSD test for multiple comparisons. Student's paired t test was used for pairwise group comparisons, as needed. All statistical tests were 2-sided, and values of P < 0.05 were considered statistically significant.
RESULTS
EGCG competitively binds to the AR and disrupts interdomain (N-C) interaction
Using 2PNU.pdb as the starting receptor, 3-D structure conformation of EGCG was modeled to examine whether and how it interacts in silico using the Autodock4 software tool. 2PNU.pdb is the crystal structure of human androgen receptor ligand binding domain, as described previously (27). There are 8 polar hydrogens and 1 carbonyl oxygen on EGCG that are available for hydrogen bonding, and we observed that the majority of these actively participated in the hydrogen bonding, as evident from the hydrogen bonds (Fig. 1A, right panel, dashed lines; predicted distances 3.57, 2.41, 2.80, 2.79, and 3.07 Å). We observed that EGCG binds with a binding energy E = −8.23 kcal/mol ∼ 931 nM (Fig. 1A). EGCG interacted with the AR-LBD through 16 putative amino acid residues and 5 hydrogen bonds. Autodock scoring was based on the estimated free energy of binding and consisted of the summation of the final intermolecular energy of docking, total internal energy, and the torsional free energy of the ligand, minus the system's unbound energy.
Since EGCG inhibits the growth of LNCaP cells (23, 28), we considered the possibility that EGCG could interfere with AR functioning by competing with androgens and directly interacting with its LBD, which in turn could repress AR function. EGCG was tested for its possible binding with the purified AR-LBD in an in vitro ligand competition assay based on time-resolved FRET (TR-FRET), as described in Materials and Methods, based on a previous study (25). This setup is instrumental in identifying AR ligands based on their ability to compete and displace a labeled high-affinity androgen, Fluormone AL Red, from the AR-LBD. EGCG was found to displace Fluormone AL Red from the purified AR-LBD, resulting in a lower FRET ratio, indicating that it competed with a high-affinity labeled AR ligand and physically interacted with the AR-LBD with an IC50 of 0.4 μM (Fig. 1B). In this assay, dihydrotestosterone (DHT) was used as a control reference ligand with an estimated IC50 of 1.9 nM.
These data indicated that EGCG interacts in vitro with the purified AR-LBD, thereby serving as a specific, high-affinity competitive ligand; however, whether it is agonistic or antagonistic could not be established in such an assay. To test the functional implication of this interaction, we determined the effect of EGCG on interdomain interaction by performing a receptor reconstitution-based interdomain interaction (N-C-terminal interaction) assay in AR-null CV1 cells, which are devoid of endogenous AR. A PCa cell line with endogenous AR cannot be used to answer the question. It is known that agonist-bound AR causes interdomain interaction between the N-terminal domain and the C-terminal domain, which is required for its maximal/optimal activation (29–31). This interaction is important for AR transactivation and is promoted by agonistic ligands (30–32); conversely, AR antagonists inhibit this interaction to repress AR function. In this assay, pSVARN1, coding for the AR NH2-terminal domain, and pSVARC, coding for the AR DBD-LBD, were transfected and ectopically expressed. pSVARN1 codes for the N terminus of AR; lacking both the DBD and the C-terminal LBD, this construct is transcriptionally inactive on its own, as it cannot bind to DNA due to the lack of DBD. However, pSVARC plasmid harbors only the AR DBD and LBD, but lacks the N terminus. The pSVARC construct can bind to the DNA but, due to lack of the N-terminal transactivation domain, is not active on its own and therefore needs the pSVARN1 to become functionally active. Both of these constructs have been shown to be expressed efficiently in CV1 cells (32). Both pSVARN1 and pSVARC constructs failed to activate cognate reporter when expressed separately (Fig. 1C); similarly, no activation was observed when both were coexpressed and cells were not treated with R1881. R188-bound LBD interacted with the N-terminal domain, leading to reconstitution of functional AR, which led to a 70-fold activation of the reporter. Cotreatment of transfected cells with EGCG (10 μM) along with R1881, however, led to a very potent decrease in reporter activity, indicating that EGCG acts as an antagonist of androgen function, similar to the pharmacological inhibitor Casodex, which was used as a control.
To test the effect of EGCG binding on AR stability further, a pulse-chase experiment was performed using a translation inhibitor, cycloheximide. Treatment of LNCaP cells with cycloheximide led to a time-dependent decrease in AR protein expression, with the half-life of AR protein in the range of 12 to 18 h (Fig. 1D). Interestingly, when the cells were cotreated by cycloheximide and EGCG, the rate of AR decay was further accelerated, and the half-life of AR protein was observed to be <6 h (Fig. 1D). This finding indicates that by binding to the LBD, EGCG destabilizes AR protein levels and accelerates its degradation. Since AR protein is regulated by proteasome-mediated degradation, we wanted to confirm whether proteasome inhibitors can reverse the stability of AR protein. EGCG promoted AR protein degradation in LNCaP cells, but this was prevented by MG132 (Fig. 1E).
EGCG inhibits mutant T877A AR-mediated transactivation
Somatic missense mutations in AR have been identified in primary, recurrent, and metastatic forms of clinical PCa and cell lines (33–35). One such mutant in the LBD occurs at position 877, changing a threonine into alanine. This hotspot T877A AR mutant loses the ability to differentiate agonists from antagonists; it has been isolated from patients with clinically relapsed PCa and shows very potent transactivation in the presence of androgens (35). To test how inhibition of N-C interaction of AR modulates AR transactivation, we performed promoter reporter assays to test the influence of EGCG on AR T877A-mediated transactivation. Here, ectopically expressed T877A AR mutant was found to activate the reporter in the presence of R1881 (Fig. 2A). Treatment with EGCG (10, 20, and 40 μM) did not induce any reporter activity per se, indicating that EGCG bears no leaky agonistic activity even at high concentrations. Cotreatment of EGCG, however, repressed R1881-induced mutant AR transactivation at all three doses, indicating that EGCG can repress mutant T877A AR-mediated transactivation. Moreover, the maximal AR repression was achieved at 20 μM EGCG, and further enhancement to 40 μM did not additionally repress AR. Casodex was also found to repress R1881-induced transactivation and served as control.
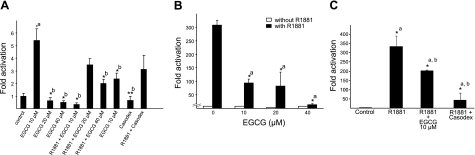
Figure 2.
EGCG inhibits hotspot AR mutant T877A-mediated transactivation. A) CV1 cells were transfected with pSG5-T877A mutant of AR (2 μg), MMTV-luc reporter (1 μg), and Renilla luc (50 ng). Graphs represent fold of hormone induction compared with value for the non-hormone-treated group, which was set as 1. *aP < 0.01 vs. control group; *bP < 0.01, **bP < 0.05 vs. R1881 group; 1-way ANOVA followed by Tukey's HSD test. B) LNCaP cells were transfected with MMTV-Luc reporter and were treated 24 h post-transfection with or without 1 nM R1881 and with indicated concenctration of EGCG. Graphs represent fold of hormone induction compared with value for the non-hormone-treated group, which was set as 1. *aP < 0.01 vs. R1881 control group; 1-way ANOVA followed by Tukey's HSD test. C) LNCaP cells were transfected with PSA promoter containing reporter and were treated 24 h post-transfection with or without 1 nM R1881 and with indicated concentration of EGCG and casodex. *aP < 0.01 vs. control group; *bP < 0.01vs. R1881 group; 1-way ANOVA followed by Tukey's HSD test.
To further validate these findings in a more physiological context, a similar reporter assay was performed in LNCaP cells that harbor endogenous T877A AR mutant. Treatment with R1881 was found to result in a robust 300-fold increase in the reporter activity (Fig. 2B), which was decreased 3-fold by cotreatment with 10 μM EGCG, and >10-fold with 40 μM EGCG, suggesting that by interacting with AR, EGCG blunts its transactivation. Finally, on a native androgen-responsive PSA-promoter-containing reporter, EGCG cotreatment led to repression of R1881-induced AR transactivation (Fig. 2C), indicating the versatility of EGCG in repressing AR function on a wide AR-specific promoter context. These effects are likely due to the efficacy of EGCG on the transactivation of the AR.
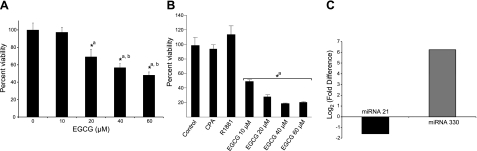
EGCG inhibits the growth of PCa cells
Since the growth of PCa cells is regulated by AR functioning, we tested how repression of AR by EGCG affects the growth of PCa cells. Hormone-refractory C4-2 cells were grown in charcoal-treated hormone-free medium, and we observed that both 40 and 60 μM doses of EGCG inhibited the growth of these cells (Fig. 3A). We also tested the effect of EGCG on the growth of androgen-independent 22Rν1 cells. These cells express multiple AR isoforms that remain constitutively active, leading to ligand-independent induction of target gene expression and cell growth (36). In line with this, in the MTT cell viability assay, the growth of these cells was not altered significantly by R1881 or partial agonist CPA (Fig. 3B); however, treatment with EGCG decreased the growth of 22Rν1 cells at all doses tested (10 to 60 μM), indicating that EGCG has a unique function in repressing AR function that represses the growth of otherwise ligand-independent 22Rν1 cells, by inhibiting AR function.
Figure 3.
EGCG antagonizes AR-positive PCa cell growth. A, B) C4-2 (A) and 22Rν1 cells (B) were treated with indicated concentrations of EGCG for 48 h, and cell viability was determined by MTT assay, as detailed in Materials and Methods. *aP < 0.01 vs. control group; *bP < 0.01vs. 20 μM EGCG group; 1-way ANOVA followed by Tukey's HSD test. C) EGCG modulated the expression of miRNAs considered to be important in PCa. Relative expression of miRNA-21 and -330 in tumor xenograft tissues isolated from animals treated with EGCG. Real-time PCR was performed for the 2 miRNAs, and fold change was calculated.
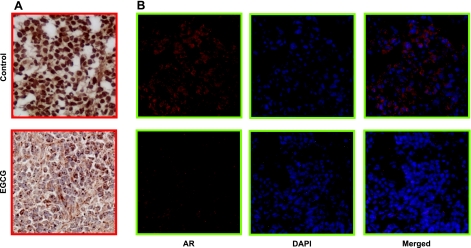
EGCG treatment decreases AR protein expression in xenograft model
We and others have earlier shown that interference with interdomain interaction of AR results in its accelerated decay (32, 37, 38). Since EGCG also interferes with this interaction, we tested how it affects AR protein stability in vivo. To examine this possibility, immunohistochemical analysis was performed to detect AR protein levels in a tumor xenograft of 22Rν1 cells established in male nude mice and treated with EGCG for 6 wk (1 mg 3×/wk, i.p.). In these experiments, vehicle-treated cells showed strong immunoreactivity for AR in both cytosol and nucleus (Fig. 4A, top panel). In contrast, PCa xenograft from mice treated with EGCG exhibited significantly less AR protein levels, which were primarily cytosolic, suggesting that EGCG, in addition to decreasing AR protein expression, sequesters it in the cytoplasm as a consequence of its nuclear exclusion (Fig. 4A, bottom panel). This is an important mechanism by which an antagonist can repress genotropic function of AR and prevent it from shuttling to the cell nucleus. To verify cytoplasmic retention of EGCG-bound AR further, we performed immunofluorescent labeling to visualize AR localization in situ in tissues isolated from the xenograft. The bright red fluorescence from AR in control cells is indicative of homogeneous distribution of AR in cytoplasm and nucleus, while the tissues isolated from animals treated with EGCG had the protein sequestered in cytoplasm, with clear blue DAPI-stained nuclei (Fig. 4B).
Figure 4.
EGCG decreases AR protein expression and its nuclear shuttling in vivo. Localization of AR in androgen-independent 22Rν1 tumor xenograft in nude mice. Photomicrographs (×300) represent immunohistochemical staining (A) and immunofluorescence staining (B) for AR in tumor xenograft.
EGCG administration modulates expression levels of miRNA in tissues isolated from xenograft model
miRNAs are 18- to 24-nt small regulatory RNAs that repress target gene expression by inhibiting either mRNA translation or target mRNA degradation. Deregulated miRNA expression has recently been reported in advanced PCa (39–41). miRNA-21 was recently demonstrated to be regulated by androgens and was shown to promote hormone-dependent and refractory PCa growth (42). We thus employed real-time RT-PCR to evaluate the expression of this miRNA in the tumor tissues isolated from our previous study (18). We observed that the tissue isolated from the animals that were treated with EGCG for 6 wk (1 mg/d 3×/wk) exhibited 1.5-fold down-regulation of miR-21 as compared to the vehicle treated controls (Fig. 3C). We further tested the expression levels of miRNA-330, which is a known tumor suppressor and induces apoptosis in PCa cells (43). We observed >6-fold induction in the levels of miR-330 in the tumor tissues isolated from animals that were treated with EGCG as compared to the untreated controls (Fig. 3C).
DISCUSSION
Our most important observation, based on multiple lines of experimentation, is that EGCG blunts AR function at multiple levels in PCa. Despite the fact that PCa cells generally become androgen refractory, they still depend on functional AR signaling, which is often overexpressed in hormone-refractory PCa, for growth, and decreasing AR levels impair their growth (44, 45). Since most clinically relapsed PCa patients develop resistance to currently available antihormone therapies, finding alternate and effective antagonists that interfere with the expression and function of AR could dramatically improve the benefits of therapeutic intervention in the treatment of hormone-refractory PCa.
In cell growth assays, EGCG has been shown to inhibit the growth and proliferation of various PCa cells through multiple mechanisms (17, 19, 23, 46, 47), with minimal effects on normal human prostate epithelial cells (PrECs). This finding developed an enthusiasm for EGCG as an anti-PCa agent. During the past decade, a number of studies demonstrated potential effects of tea polyphenols, including EGCG, through multiple mechanisms, including cell growth inhibition (48–50), induction of apoptosis (50, 51), cell cycle arrest (51), inhibition of type 2,5-α-reductase (49), and in vitro and in vivo inhibition of testosterone-mediated induction of ornithine decarboxylase (52). Based on these results alone, it is challenging to explain how EGCG serves as a more potent inhibitor of PCa growth, specifically in cells expressing functional AR (17, 53). Our results demonstrated that the beneficial effects of green tea polyphenol are associated with its antiandrogenic action. To explain its antigrowth effect on PCa cells, we found that EGCG physically interacts with the AR-LBD and competes with natural agonist DHT (IC50 0.4 μM). The cell growth assay was also in concordance with this result, and EGCG in fact abrogated the proliferative effect of strong synthetic agonist R1881 on PCa cells, and hence serves as a functional antagonist. It is important to mention here that the most widely used AR antagonists have been the steroidal drug cyproterone and the nonsteroidal drugs flutamide and bicalutamide, which are all competitive antagonists of androgen binding. Previous studies have shown that bicalutamide is a pure antagonist of wild-type and identified mutant ARs (54). The unliganded AR associates with a heat-shock protein 90 (HSP90) chaperone complex that facilitates ligand binding, with subsequent conformational changes resulting in AR homodimerization, nuclear translocation, DNA binding, and transcriptional activation (55).
Because the growth of LNCaP cells depends on functional AR signaling, and RNAi-mediated knockdown of AR had a negative effect on cellular growth, we further tested whether EGCG decreases AR protein levels in vivo. Here we observed that AR protein expression was decreased in EGCG-treated mice bearing a 22Rν1 PCa cell xenograft. AR protein levels are known to correlate positively with the degree of androgen independence (56); thus, EGCG-mediated decrease in AR protein expression could also revert androgen-independent 22Rν1 phenotype back to androgen-dependent and thereby could also help restore sensitivity to other antiandrogenic drugs. These speculations will, however, require further experimental validation.
The antiandrogenic activity of EGCG becomes evident from the results of FRET-based competition assays, where EGCG displays notable competition with a high-affinity androgenic agonist, Fluormone AL Red. A functional assay demonstrating reversal of R1881-induced transcriptional activation assay by EGCG further provides evidence for a physiological competition between androgens and EGCG. Interestingly, much higher concentrations of ECGC were required to inhibit cell growth, as compared to the micromolar amounts required to competitively bind to the AR-LBD in a cell free in vitro assay. This could be due to the less hydrophilic nature of EGCG, which impedes its free cellular uptake through the plasma membrane; therefore, bioavailability of ECGC similar to that of Casodex or R1881 could be achieved at a much higher dose. Thus, it is important to translate the dose of EGCG into cell culture or animal models to achieve effects similar to those observed in FRET-based competition assays.
The AR is a ligand-activated transcription factor that mediates the biological responses of androgens (31). In our study, we found that AR N-C interaction was blocked by 10 μM EGCG. Hence, the in vivo decrease in AR protein expression in the tumor xenograft appears to be primarily due to a decrease in AR protein stability due to interference with N-C-terminal interaction, thereby also leading to a decrease in transactivation. The major finding of the present work is that EGCG functions as a direct androgen antagonist, thereby blunting AR-dependent transcription. Our work provides an explanation for the decreased AR and PSA expression shown by previous studies (22, 52). This work therefore provides a mechanistic basis to explain how EGCG, by interfering with N-C interaction, decreases AR stability.
Decontrolled expression of various miRNAs has been reported for a variety of cancers, including cancer of the prostate gland (39–42), and various oncogenic and tumor-suppressor transcription factors have been shown to directly regulate miRNA transcription (57). Further, miRNAs have been shown to be regulated by AR (42). In light of this, we tested the expression levels of miRNA-21 in the tumor xenograft tissues of EGCG-treated and control mice. Our data suggest a noticeable inhibition of this miRNA in the EGCG-treated samples. We also looked at the expression profile of another miRNA, miRNA-330, which acts as tumor suppressor and is known to induce apoptosis of PCa cells (43). We observed >6-fold up-regulation of miR-330, a tumor-suppressor miRNA that has been shown to induce apoptosis in PCa cells, in the tissues obtained from EGCG-treated mice as compared to the untreated controls. We thus provide evidence for AR-regulated miRNAs being modulated by EGCG.
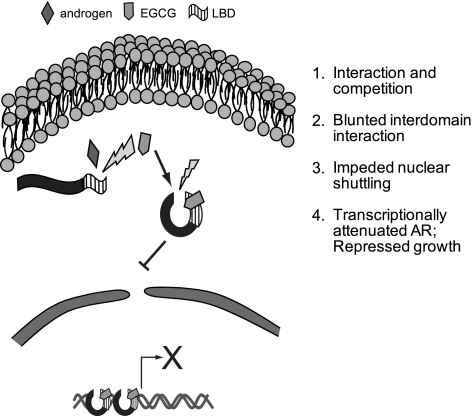
The present study is one of the first few reports demonstrating the antiandrogenic action of a plant product and the first report showing the effect of EGCG, a naturally occurring polyphenol present in green tea, in inhibiting human prostate carcinoma cell growth. We have shown that EGCG effectively inhibits the transactivation functions and expression of AR by interfering with its stability as a result of decreased interdomain interaction (Fig. 5). We also showed that EGCG is a novel antagonist of AR signaling, which can block AR-regulated gene expression and cell growth in human PCa cells. We thus suggest that EGCG could be developed as a chemotherapeutic agent against hormone-refractory PCa.
Figure 5.
Model depicting the effect of EGCG on AR-mediated signaling. EGCG could compete with natural AR agonist DHT to physically interact with the expressed AR protein. Once bound, it decreased the interdomain interaction of AR, leading to a decrease in AR protein expression and, hence, a decrease in AR transactivation functions. This resulted in decreased expression of AR target genes and thus might negatively influence the growth of PCa cells in vitro and in vivo.
Acknowledgments
The authors thank Drs. Aria Baniahmad (University of Jena, Jena, Germany), Albert Brinkmann (University of Rotterdam, Rotterdam, The Netherlands), and Zafar Nawaz (University of Miami, Miami, FL, USA) for providing plasmids used in this study. The authors thank Drs. George Thalman (Institute for Surgical Technology and Biomechanics, Bern University, Bern, Switzerland) and Randall Tibbetts (University of Wisconsin, Madison, WI, USA) for providing C4-2 and CV1 cells, respectively. The authors thank Dr. Kenneth Satyshur (Department of Bacteriology, University of Wisconsin, Madison, WI, USA) for help with in silico studies.
This work was supported by U.S. Public Health Service grants RO1CA78809, RO1CA101039, and RO1CA120451 to H.M. I.A.S. was supported by U.S. National Institutes of Health grant T32 AR 055893.
REFERENCES
- 1. Weir H. K., Thun M. J., Hankey B. F., Ries L. A., Howe H. L., Wingo P. A., Jemal A., Ward E., Anderson R. N., Edwards B. K. (2003) Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention and control. J. Natl. Cancer Inst. 95, 1276–1299 [DOI] [PubMed] [Google Scholar]
- 2. Jemal A., Siegel R., Ward E., Hao Y., Xu J., Thun M. J. (2009) Cancer statistics, 2009. CA Cancer J. Clin. 59, 225–249 [DOI] [PubMed] [Google Scholar]
- 3. Chmelar R., Buchanan G., Need E. F., Tilley W., Greenberg N. M. (2007) Androgen receptor coregulators and their involvement in the development and progression of prostate cancer. Int. J. Cancer 120, 719–733 [DOI] [PubMed] [Google Scholar]
- 4. Chodak G. W., Kranc D. M., Puy L. A., Takeda H., Johnson K., Chang C. (1992) Nuclear localization of androgen receptor in heterogeneous samples of normal, hyperplastic and neoplastic human prostate. J. Urol. 147, 798–803 [DOI] [PubMed] [Google Scholar]
- 5. Ruizeveld de Winter J. A., Janssen P. J., Sleddens H. M., Verleun-Mooijman M. C., Trapman J., Brinkmann A. O., Santerse A. B., Schroder F. H., van der Kwast T. H. (1994) Androgen receptor status in localized and locally progressive hormone refractory human prostate cancer. Am. J. Pathol. 144, 735–746 [PMC free article] [PubMed] [Google Scholar]
- 6. Chen C. D., Welsbie D. S., Tran C., Baek S. H., Chen R., Vessella R., Rosenfeld M. G., Sawyers C. L. (2004) Molecular determinants of resistance to antiandrogen therapy. Nat. Med. 10, 33–39 [DOI] [PubMed] [Google Scholar]
- 7. Ricciardelli C., Choong C. S., Buchanan G., Vivekanandan S., Neufing P., Stahl J., Marshall V. R., Horsfall D. J., Tilley W. D. (2005) Androgen receptor levels in prostate cancer epithelial and peritumoral stromal cells identify non-organ confined disease. Prostate 63, 19–28 [DOI] [PubMed] [Google Scholar]
- 8. Henshall S. M., Quinn D. I., Lee C. S., Head D. R., Golovsky D., Brenner P. C., Delprado W., Stricker P. D., Grygiel J. J., Sutherland R. L. (2001) Altered expression of androgen receptor in the malignant epithelium and adjacent stroma is associated with early relapse in prostate cancer. Cancer Res. 61, 423–427 [PubMed] [Google Scholar]
- 9. Perry J. E., Grossmann M. E., Tindall D. J. (1996) Androgen regulation of gene expression. Prostate Suppl. 6, 79–81 [PubMed] [Google Scholar]
- 10. Young C. Y., Andrews P. E., Montgomery B. T., Tindall D. J. (1992) Tissue-specific and hormonal regulation of human prostate-specific glandular kallikrein. Biochemistry 31, 818–824 [DOI] [PubMed] [Google Scholar]
- 11. Isaacs J. T. (2000) Apoptosis: translating theory to therapy for prostate cancer. J. Natl. Cancer Inst. 92, 1367–1369 [DOI] [PubMed] [Google Scholar]
- 12. Chen S., Song C. S., Lavrovsky Y., Bi B., Vellanoweth R., Chatterjee B., Roy A. K. (1998) Catalytic cleavage of the androgen receptor messenger RNA and functional inhibition of androgen receptor activity by a hammerhead ribozyme. Mol. Endocrinol. 12, 1558–1566 [DOI] [PubMed] [Google Scholar]
- 13. Haag P., Bektic J., Bartsch G., Klocker H., Eder I. E. (2005) Androgen receptor down regulation by small interference RNA induces cell growth inhibition in androgen sensitive as well as in androgen independent prostate cancer cells. J. Steroid Biochem. Mol. Biol. 96, 251–258 [DOI] [PubMed] [Google Scholar]
- 14. Liao X., Tang S., Thrasher J. B., Griebling T. L., Li B. (2005) Small-interfering RNA-induced androgen receptor silencing leads to apoptotic cell death in prostate cancer. Mol. Cancer Ther. 4, 505–515 [DOI] [PubMed] [Google Scholar]
- 15. McLarty J., Bigelow R. L., Smith M., Elmajian D., Ankem M., Cardelli J. A. (2009) Tea polyphenols decrease serum levels of prostate-specific antigen, hepatocyte growth factor, and vascular endothelial growth factor in prostate cancer patients and inhibit production of hepatocyte growth factor and vascular endothelial growth factor in vitro. Cancer Prev. Res. (Phila.) 2, 673–682 [DOI] [PubMed] [Google Scholar]
- 16. Bettuzzi S., Brausi M., Rizzi F., Castagnetti G., Peracchia G., Corti A. (2006) Chemoprevention of human prostate cancer by oral administration of green tea catechins in volunteers with high-grade prostate intraepithelial neoplasia: a preliminary report from a one-year proof-of-principle study. Cancer Res. 66, 1234–1240 [DOI] [PubMed] [Google Scholar]
- 17. Adhami V. M., Malik A., Zaman N., Sarfaraz S., Siddiqui I. A., Syed D. N., Afaq F., Pasha F. S., Saleem M., Mukhtar H. (2007) Combined inhibitory effects of green tea polyphenols and selective cyclooxygenase-2 inhibitors on the growth of human prostate cancer cells both in vitro and in vivo. Clin. Cancer Res. 13, 1611–1619 [DOI] [PubMed] [Google Scholar]
- 18. Siddiqui I. A., Zaman N., Aziz M. H., Reagan-Shaw S. R., Sarfaraz S., Adhami V. M., Ahmad N., Raisuddin S., Mukhtar H. (2006) Inhibition of CWR22Rnu1 tumor growth and PSA secretion in athymic nude mice by green and black teas. Carcinogenesis 27, 833–839 [DOI] [PubMed] [Google Scholar]
- 19. Chuu C. P., Chen R. Y., Kokontis J. M., Hiipakka R. A., Liao S. (2009) Suppression of androgen receptor signaling and prostate specific antigen expression by (-)-epigallocatechin-3-gallate in different progression stages of LNCaP prostate cancer cells. Cancer Lett. 275, 86–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Morrissey C., Brown M., O'Sullivan J., Weathered N., Watson R. W., Tenniswood M. (2007) Epigallocatechin-3-gallate and bicalutamide cause growth arrest and apoptosis in NRP-152 and NRP-154 prostate epithelial cells. Int. J. Urol. 14, 545–551 [DOI] [PubMed] [Google Scholar]
- 21. Naftalin R. J., Afzal I., Cunningham P., Halai M., Ross C., Salleh N., Milligan S. R. (2003) Interactions of androgens, green tea catechins and the antiandrogen flutamide with the external glucose-binding site of the human erythrocyte glucose transporter GLUT1. Br. J. Pharmacol. 140, 487–499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ren F., Zhang S., Mitchell S. H., Butler R., Young C. Y. (2000) Tea polyphenols down-regulate the expression of the androgen receptor in LNCaP prostate cancer cells. Oncogene 19, 1924–1932 [DOI] [PubMed] [Google Scholar]
- 23. Siddiqui I. A., Malik A., Adhami V. M., Asim M., Hafeez B. B., Sarfaraz S., Mukhtar H. (2008) Green tea polyphenol EGCG sensitizes human prostate carcinoma LNCaP cells to TRAIL-mediated apoptosis and synergistically inhibits biomarkers associated with angiogenesis and metastasis. Oncogene 27, 2055–2063 [DOI] [PubMed] [Google Scholar]
- 24. Asim M., Siddiqui I. A., Hafeez B. B., Baniahmad A., Mukhtar H. (2008) Src kinase potentiates androgen receptor transactivation function and invasion of androgen-independent prostate cancer C4-2 cells. Oncogene 27, 3596–3604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ozers M. S., Marks B. D., Gowda K., Kupcho K. R., Ervin K. M., De Rosier T., Qadir N., Eliason H. C., Riddle S. M., Shekhani M. S. (2007) The androgen receptor T877A mutant recruits LXXLL and FXXLF peptides differently than wild-type androgen receptor in a time-resolved fluorescence resonance energy transfer assay. Biochemistry 46, 683–695 [DOI] [PubMed] [Google Scholar]
- 26. Siddiqui I. A., Shukla Y., Adhami V. M., Sarfaraz S., Asim M., Hafeez B. B., Mukhtar H. (2008) Suppression of NFkappaB and its regulated gene products by oral administration of green tea polyphenols in an autochthonous mouse prostate cancer model. Pharm. Res. 25, 2135–2142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cantin L., Faucher F., Couture J. F., de Jesus-Tran K. P., Legrand P., Ciobanu L. C., Frechette Y., Labrecque R., Singh S. M., Labrie F., Breton R. (2007) Structural characterization of the human androgen receptor ligand-binding domain complexed with EM5744, a rationally designed steroidal ligand bearing a bulky chain directed toward helix 12. J. Biol. Chem. 282, 30910–30919 [DOI] [PubMed] [Google Scholar]
- 28. Hastak K., Gupta S., Ahmad N., Agarwal M. K., Agarwal M. L., Mukhtar H. (2003) Role of p53 and NF-kappaB in epigallocatechin-3-gallate-induced apoptosis of LNCaP cells. Oncogene 22, 4851–4859 [DOI] [PubMed] [Google Scholar]
- 29. Hsu C. L., Chen Y. L., Ting H. J., Lin W. J., Yang Z., Zhang Y., Wang L., Wu C. T., Chang H. C., Yeh S., Pimplikar S. W., Chang C. (2005) Androgen receptor (AR) NH2- and COOH-terminal interactions result in the differential influences on the AR-mediated transactivation and cell growth. Mol. Endocrinol. 19, 350–361 [DOI] [PubMed] [Google Scholar]
- 30. Wong C. I., Zhou Z. X., Sar M., Wilson E. M. (1993) Steroid requirement for androgen receptor dimerization and DNA binding. Modulation by intramolecular interactions between the NH2-terminal and steroid-binding domains. J. Biol. Chem. 268, 19004–19012 [PubMed] [Google Scholar]
- 31. Zhou Z. X., Lane M. V., Kemppainen J. A., French F. S., Wilson E. M. (1995) Specificity of ligand-dependent androgen receptor stabilization: receptor domain interactions influence ligand dissociation and receptor stability. Mol. Endocrinol. 9, 208–218 [DOI] [PubMed] [Google Scholar]
- 32. Khan N., Asim M., Afaq F., Abu Zaid M., Mukhtar H. (2008) A novel dietary flavonoid fisetin inhibits androgen receptor signaling and tumor growth in athymic nude mice. Cancer Res. 68, 8555–8563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Han G., Buchanan G., Ittmann M., Harris J. M., Yu X., Demayo F. J., Tilley W., Greenberg N. M. (2005) Mutation of the androgen receptor causes oncogenic transformation of the prostate. Proc. Natl. Acad. Sci. U. S. A. 102, 1151–1156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hyytinen E. R., Haapala K., Thompson J., Lappalainen I., Roiha M., Rantala I., Helin H. J., Janne O. A., Vihinen M., Palvimo J. J., Koivisto P. A. (2002) Pattern of somatic androgen receptor gene mutations in patients with hormone-refractory prostate cancer. Lab. Invest. 82, 1591–1598 [DOI] [PubMed] [Google Scholar]
- 35. Taplin M. E., Bubley G. J., Ko Y. J., Small E. J., Upton M., Rajeshkumar B., Balk S. P. (1999) Selection for androgen receptor mutations in prostate cancers treated with androgen antagonist. Cancer Res. 59, 2511–2515 [PubMed] [Google Scholar]
- 36. Dehm S. M., Schmidt L. J., Heemers H. V., Vessella R. L., Tindall D. J. (2008) Splicing of a novel androgen receptor exon generates a constitutively active androgen receptor that mediates prostate cancer therapy resistance. Cancer Res. 68, 5469–5477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Centenera M. M., Harris J. M., Tilley W. D., Butler L. M. (2008) The contribution of different androgen receptor domains to receptor dimerization and signaling. Mol. Endocrinol. 22, 2373–2382 [DOI] [PubMed] [Google Scholar]
- 38. Lee D. K., Chang C. (2003) Endocrine mechanisms of disease: Expression and degradation of androgen receptor: mechanism and clinical implication. J. Clin. Endocrinol. Metab. 88, 4043–4054 [DOI] [PubMed] [Google Scholar]
- 39. Ambs S., Prueitt R. L., Yi M., Hudson R. S., Howe T. M., Petrocca F., Wallace T. A., Liu C. G., Volinia S., Calin G. A., Yfantis H. G., Stephens R. M., Croce C. M. (2008) Genomic profiling of microRNA and messenger RNA reveals deregulated microRNA expression in prostate cancer. Cancer Res. 68, 6162–6170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ozen M., Creighton C. J., Ozdemir M., Ittmann M. (2008) Widespread deregulation of microRNA expression in human prostate cancer. Oncogene 27, 1788–1793 [DOI] [PubMed] [Google Scholar]
- 41. Porkka K. P., Pfeiffer M. J., Waltering K. K., Vessella R. L., Tammela T. L., Visakorpi T. (2007) MicroRNA expression profiling in prostate cancer. Cancer Res. 67, 6130–6135 [DOI] [PubMed] [Google Scholar]
- 42. Ribas J., Ni X., Haffner M., Wentzel E. A., Salmasi A. H., Chowdhury W. H., Kudrolli T. A., Yegnasubramanian S., Luo J., Rodriguez R., Mendell J. T., Lupold S. E. (2009) miR-21: an androgen receptor-regulated microRNA that promotes hormone-dependent and hormone-independent prostate cancer growth. Cancer Res. 69, 7165–7169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lee K. H., Chen Y. L., Yeh S. D., Hsiao M., Lin J. T., Goan Y. G., Lu P. J. (2009) MicroRNA-330 acts as tumor suppressor and induces apoptosis of prostate cancer cells through E2F1-mediated suppression of Akt phosphorylation. Oncogene 28, 3360–3370 [DOI] [PubMed] [Google Scholar]
- 44. Zhu W., Zhu D. S., Madan R. A., Gulley J. L., Figg W. D., Dahut W. L. (2009) Treatment of castration-resistant prostate cancer: updates on therapeutics targeting the androgen receptor signaling pathway. Am. J. Ther. 17, 176–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chen Y., Sawyers C. L., Scher H. I. (2008) Targeting the androgen receptor pathway in prostate cancer. Curr. Opin. Pharmacol. 8, 440–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Brusselmans K., De Schrijver E., Heyns W., Verhoeven G., Swinnen J. V. (2003) Epigallocatechin-3-gallate is a potent natural inhibitor of fatty acid synthase in intact cells and selectively induces apoptosis in prostate cancer cells. Int. J. Cancer 106, 856–862 [DOI] [PubMed] [Google Scholar]
- 47. Stuart E. C., Scandlyn M. J., Rosengren R. J. (2006) Role of epigallocatechin gallate (EGCG) in the treatment of breast and prostate cancer. Life Sci. 79, 2329–2336 [DOI] [PubMed] [Google Scholar]
- 48. Blot W. J., Chow W. H., McLaughlin J. K. (1996) Tea and cancer: a review of the epidemiological evidence. Eur. J. Cancer Prev. 5, 425–438 [PubMed] [Google Scholar]
- 49. Liao S., Hiipakka R. A. (1995) Selective inhibition of steroid 5 alpha-reductase isozymes by tea epicatechin-3-gallate and epigallocatechin-3-gallate. Biochem. Biophys. Res. Commun. 214, 833–838 [DOI] [PubMed] [Google Scholar]
- 50. Paschka A. G., Butler R., Young C. Y. (1998) Induction of apoptosis in prostate cancer cell lines by the green tea component, (-)-epigallocatechin-3-gallate. Cancer Lett. 130, 1–7 [DOI] [PubMed] [Google Scholar]
- 51. Ahmad N., Feyes D. K., Nieminen A. L., Agarwal R., Mukhtar H. (1997) Green tea constituent epigallocatechin-3-gallate and induction of apoptosis and cell cycle arrest in human carcinoma cells. J. Natl. Cancer Inst. 89, 1881–1886 [DOI] [PubMed] [Google Scholar]
- 52. Gupta S., Ahmad N., Mohan R. R., Husain M. M., Mukhtar H. (1999) Prostate cancer chemoprevention by green tea: in vitro and in vivo inhibition of testosterone-mediated induction of ornithine decarboxylase. Cancer Res. 59, 2115–2120 [PubMed] [Google Scholar]
- 53. Gupta S., Ahmad N., Nieminen A. L., Mukhtar H. (2000) Growth inhibition, cell-cycle dysregulation, and induction of apoptosis by green tea constituent (-)-epigallocatechin-3-gallate in androgen-sensitive and androgen-insensitive human prostate carcinoma cells. Toxicol. Appl. Pharmacol. 164, 82–90 [DOI] [PubMed] [Google Scholar]
- 54. Masiello D., Cheng S., Bubley G. J., Lu M. L., Balk S. P. (2002) Bicalutamide functions as an androgen receptor antagonist by assembly of a transcriptionally inactive receptor. J. Biol. Chem. 277, 26321–26326 [DOI] [PubMed] [Google Scholar]
- 55. Brinkmann A. O., Blok L. J., de Ruiter P. E., Doesburg P., Steketee K., Berrevoets C. A., Trapman J. (1999) Mechanisms of androgen receptor activation and function. J. Steroid. Biochem. Mol. Biol. 69, 307–313 [DOI] [PubMed] [Google Scholar]
- 56. Craft N., Shostak Y., Carey M., Sawyers C. L. (1999) A mechanism for hormone-independent prostate cancer through modulation of androgen receptor signaling by the HER-2/neu tyrosine kinase. Nat. Med. 5, 280–285 [DOI] [PubMed] [Google Scholar]
- 57. O'Donnell K. A., Wentzel E. A., Zeller K. I., Dang C. V., Mendell J. T. (2005) c-Myc-regulated microRNAs modulate E2F1 expression. Nature 435, 839–843 [DOI] [PubMed] [Google Scholar]