Abstract
OBJECTIVES
To examine caregiver burden over time among caregivers of patients with advanced chronic disease.
DESIGN
Observational cohort with interviews over 12 months.
PARTICIPANTS
Caregivers of 179 community-living persons age ≥ 60 years with advanced cancer, heart failure (HF), or chronic obstructive pulmonary disease (COPD).
MEASUREMENTS
Caregiver burden assessed using a short-form of the Zarit Burden Inventory (ZBI) to measure psychosocial distress.
RESULTS
At baseline, the median caregiver burden was 5 (interquartile range [IQR 1,11]), which indicates that the caregiver endorsed having at least 2 of 10 distressing concerns at least some of the time. Only 10% reported no burden. Although scores increased modestly over time, the association between time and burden was not significant in longitudinal multivariable analysis. High burden was associated with caregivers’ need for more help with daily tasks (odds ratio [OR] = 23.13, 95% confidence interval [CI] = 5.94, 90.06) and desire for greater communication with the patient (OR = 2.53, 95% CI = 1.16, 5.53). The longitudinal multivariable analysis did not yield evidence of associations of burden with patient sociodemographic or health characteristics.
CONCLUSION
Caregiver burden was common among caregivers of patients with cancer, HF, and COPD. High burden was associated with the caregiver’s report of need for greater help with daily tasks but not with objective measures of the patient’s need for assistance, such as symptoms or functional status, suggesting that burden may be a measure of the caregiver’s ability to adapt to the caregiving role.
Keywords: caregiver burden, advanced illness, social support, communication
INTRODUCTION
As physicians prepare to care for an older population of patients with chronic disease, assessing caregiver burden and understanding caregiver needs are increasingly important components of comprehensive clinical care.1 Caregiver burden refers to the physical, financial, and psychosocial hardships of caring for a loved one, usually a family member, struggling with a medical condition.2 Many families caring for terminally ill older adults report making major life changes and personal sacrifices to care for their relative.3, 4 Furthermore, caregiver burden has been identified as a risk factor for worsening caregiver physical and psychological health,5–8 worsening health-related quality of life,9 compromised immunity10, 11 and mortality.12 The psychological strain of caregiving and its association with negative health outcomes have been documented in caregivers from multiple nationalities and diverse cultures.13–15
Most research on caregiver burden has examined selected populations, primarily caregivers of patients with dementia16 and patients at the end of life.3, 17 Comparison of results across studies examining single populations such as caregivers of patients with heart failure (HF)18, 19 and chronic obstructive pulmonary disease (COPD)20 suggest there may be differences in caregiver burden across disease. However, in the absence of direct comparisons within a single study, it is difficult to know whether these are true differences or whether they result from differences in methods across the individual studies. Additionally, there has been more limited examination of caregiver, as compared to patient, characteristics that are associated with burden. There has also been limited evaluation of change in caregiver burden over time, with potentially conflicting results. Whereas one study of spouses of patients with Parkinson’s disease demonstrated increasing burden over time,21 a study of caregivers for patients with Alzheimer’s disease found coping strategies and depressive symptoms to be stable over time.22
The purpose of this study was to assess changes over time in caregiver burden of patients with advanced cancer, HF, or COPD and to examine characteristics of caregivers and patients associated with caregiver burden.
METHODS
Participants
Study participants were members of a longitudinal cohort study designed to examine as its primary outcome changes in preferences among older persons with advanced illness.23 Participants were recruited from 6 cardiology, 4 oncology, and 3 pulmonary outpatient practices in the greater New Haven area; outpatient clinics at two Veterans Affairs hospitals; and inpatient clinics at a university teaching hospital, community hospital, and Veterans Affairs hospital.24 Sequential medical records of patients 60 years or older at these sites with a primary diagnosis of cancer, HF, and COPD were reviewed to identify patients with advanced illness, defined using Connecticut Hospice (Summary guidelines for initiation of advanced care. Branford: Connecticut Hospice; 1996) or Study to Understand Prognoses and Preferences of Outcomes and Risks of Treatment (SUPPORT) criteria.25, 26 Participants eligible by chart review completed a telephone screen for the additional inclusion criterion of assistance with ≥ 1 instrumental activity of daily living (IADL),27 selected to improve the identification of persons with advanced illness.28 The screen also assessed participants for exclusion criteria, including impaired cognition as determined by the EXIT, a test for executive functioning,29 and the Short Portable Mental Status Questionnaire;30 and part time residence in Connecticut. Participants were asked to identify as their primary caregiver the person who provided the most help with their IADLs. Screening and enrollment were stratified according to diagnosis. The Human Investigation Committees of all participating hospitals approved the study protocol. All caregivers and patients provided written informed consent.
A total of 548 patients were identified by chart review. Of these, 30 were not contacted because their physician did not provide permission, 24 died before the telephone screen, 6 could not be reached, and 19 declined the telephone screen. Of those completing the telephone screen, 108 were excluded because they did not require help with IADLs, 76 were cognitively impaired, and 6 were not full-time residents of Connecticut. Of the 279 eligible participants, 51 refused participation and 2 died before enrollment, resulting in 226 enrolled patients. Of the 226 patients enrolled, 47 did not have participating caregivers: 33 patients did not provide permission for their caregiver to be contacted, 9 patients had only a paid/formal caregiver, 15 caregivers declined participation and 10 patients did not have participating caregivers for two reasons. An additional 14 caregivers were excluded from the cross-sectional analysis because they were interviewed with an earlier version of the questionnaire that did not include the caregiver burden scale. However, their follow up data was complete and thus they were included in the longitudinal analysis.
Data Collection
Patients and caregivers were interviewed separately in their homes at least every 4 months for 12 months or until the patient became too sick to participate or died. Patients and caregivers were interviewed immediately if the patient’s health declined significantly, defined as a decline in ability to perform one or more activities of daily living (ADL),31 a hospitalization lasting more than one week, hospital discharge to a nursing home or rehabilitation facility, or the introduction of hospice care.
The outcome variable, caregiver burden, was assessed in terms of the caregiver’s psychological and emotional strain using a 10-item subset of the Zarit Burden Inventory (ZBI).32 The full ZBI scale consists of 40 questions originally designed to evaluate five broad aspects of caregiver burden in caregivers of patients with dementia.2 The subscale used in this report consists of the 10 questions measuring psychosocial distress answered on a 5-point Likert scale with “never,” “rarely,” “sometimes,” “often,” and “always” corresponding to scores of 0 to 4 and summed to give a total score ranging from 0–40. The subscale includes items such as; “I feel that my relative makes requests of me that are over and above what he/she needs,” “Because of my involvement with my relative, I don’t have enough time for myself”, and “I feel stressed between trying to give to my relative as well as to other responsibilities.” This subscale has been demonstrated to have high internal consistency (Cronbach alpha = 0.94).5
Because burden scores were not normally distributed, we used the median and interquartile range to describe the distribution of scores. However, in order to compare the average level of burden of caregivers in the current study with burden of caregivers in previous studies, we characterized burden using mean and standard deviation, as this was the only description of average burden available in most previous studies. For analytical purposes, we created a dichotomous variable of high burden, defined as a score of greater than the median, versus low burden. This approach has been used previously33 because the ZBI score does not have either a theoretically34 or empirically35 defined threshold for high burden.
Descriptive and analytical variables included patient and caregiver socio-demographic and health characteristics and caregiver psychosocial characteristics. The patient socio-demographic variables included age, education, gender, race, marital status, and living arrangements. Health status variables included self-rated health;36 symptoms, measured using a modified version of the Edmonton symptom scale;37 number of hospitalizations in the six months prior to study enrollment; utilization of hospice services at any time after enrollment (used in longitudinal analysis only); functional status measured in terms of ADLs31 and IADLs;27 and depression, measured using the 2-item PRIME-MD (Primary Care Evaluation of Mental Disorders) instrument.38
The caregiver socio-demographic variables included age, education, gender, race, marital status, living arrangements, adequacy of monthly income39 and the caregiver’s relationship to the patient. The health variable was the caregiver’s self-rated health. The psychosocial variables included prior experience caring for a terminally ill relative; social support assessed using questions from the Established Populations for the Epidemiological Studies of the Elderly project41 which included the following questions: “Could you use more help with daily tasks,” and “Could you use more emotional support than you receive;” concerns about the course of illness which were assessed with a 5-point Likert scale (“strongly agree,” “agree,” “neither agree nor disagree,” “disagree,” “strongly disagree,” and “don’t know”) and consisted of the following questions: “I am concerned that my relative’s life will be inappropriately prolonged by the use of machines,” “I am concerned about my relative having other uncomfortable symptoms, such as fatigue, nausea, or shortness of breath,” and “I am concerned that, if my relative has these symptoms, they will not be adequately controlled”; and communication concerns, which included the following questions: “I would like to talk with my relative more about his/her illness” and “I would like to talk with the doctor more about my relative’s illness”.
Statistical Analysis
Frequencies and proportions and means and standard deviations were used to describe the patient and caregiver characteristics of the cohort as a whole and as stratified by patient diagnosis. All binary and ordinal variables were categorized at clinically meaningful cut points. Associations between patient and caregiver characteristics and patient diagnosis were examined in cross-sectional bivariate analyses using the chi-square test for categorical variables and the F-test for continuous variables. The Kruskal-Wallis test was used to examine the significance of the association between caregiver burden scores and patient diagnosis.
We described changes in caregiver burden scores over time by presenting median and interquartile range (IQR) for the entire cohort and stratified by patient diagnosis at baseline and the interview occurring closest to 4, 8, 12 months following baseline. In order to explore the effect of patient drop-out secondary to declining health and death on caregiver burden, we examined median burden scores at the initial and 12-month interview for caregivers of patients who completed study participation and at the initial and final interview for caregivers of patients who died during follow up. This analysis included caregiver burden scores for 14 caregivers who completed interviews when the patient was too sick to participate in an interview prior to his/her death. The analysis excluded 15 caregivers whose patients died before a second interview could be performed, 1 caregiver who died before a second interview could be performed, and 6 caregivers who either they or the patient declined to complete a follow-up interview.
The relationships between patient and caregiver characteristics with the dichotomous caregiver burden variable (high burden versus low burden) at baseline were examined in bivariate cross-sectional analysis using the chi-square test or F-test, as appropriate. The variables associated with caregiver burden at a significance level of p < .20 were examined in bivariate longitudinal analysis, in which data from all patient and caregiver interviews were included, using mixed effects models. The variables associated with caregiver burden in longitudinal analysis at a significance level of p < .10 were included in a multivariable mixed effects logistic regression model having a random intercept, and odds ratios with 95% confidence intervals are reported for these variables. Correlations among these variables were examined cross-sectionally using the Spearman rank correlation coefficient. When pairs of variables demonstrated correlation with a Spearman’s rho > 0.4, a single variable was selected for inclusion in the model. SAS version 9.2 (SAS Institute, Cary, NC) was used for all analyses.
RESULTS
Caregiver and Patient Populations
Characteristics of the 179 caregivers are summarized in Table 1. Of the total caregiver cohort, 56% were the patient’s spouse, 25% child, 13% other relative, and 6% friend. Overall, the majority of caregivers reported themselves to be in good or excellent health and to have sufficient help with daily tasks and sufficient emotional support. Concerns about communication were high; 39% reported wanting to talk with their relative more about his/her illness. A lower proportion of caregivers of patients with heart failure reported having experience caring for a sick relative (53%) than did caregivers of patients with cancer (75%) or COPD (69%). A higher proportion of caregivers of patients with heart failure reported needing more help with daily tasks (23%) as compared to caregivers of patients with cancer (9%) or COPD (11%).
Table 1.
Description of Caregivers and Patients
| Total (n = 179) | Cancer (n=68) | COPD (n=64) | HF (n=47) | P- value | |
|---|---|---|---|---|---|
| Caregiver characteristics | |||||
| Age, mean +/− SD | 62+/−14 | 60+/−14 | 63+/−15 | 62+/−14 | 0.60 |
| Education, years, mean +/− SD | 13+/−3 | 13+/−3 | 12+/−3 | 13+/−3 | 0.19 |
| Female, % | 78 | 78 | 77 | 81 | 0.86 |
| White, % | 92 | 93 | 94 | 89 | 0.68 |
| Married, n % | 78 | 77 | 78 | 79 | 0.95 |
| Not enough/just enough money, % | 45 | 42 | 43 | 51 | 0.62 |
| Self-rated health, fair/poor, % | 18 | 10 | 23 | 21 | 0.11 |
| Relationship to patient,% | 0.51 | ||||
| Spouse, husband, wife | 56 | 54 | 55 | 60 | |
| Child, daughter, son | 27 | 25 | 27 | 32 | |
| Other, relative, friend, paid caregiver | 17 | 21 | 19 | 9 | |
| Prior experience caring for ill person, % | 67 | 75 | 69 | 53 | 0.05 |
| More help with daily tasks needed, some/a lot,% | 13 | 9 | 11 | 23 | 0.06 |
| More emotional support needed, some/a lot,% | 17 | 15 | 16 | 23 | 0.53 |
| I would like to talk to the patient more, agree/strongly agree% | 39 | 50 | 34 | 30 | 0.06 |
| I would like to talk to the doctor more, agree/strongly agree% | 35 | 37 | 38 | 28 | 0.50 |
| Caregiver burden, median (IQ range)* | 5 (1–11) | 4(1–10) | 4(2–9) | 8 (1–15) | 0.36 |
| Patient characteristics | |||||
| Age, mean +/− SD | 73 +/−7 | 72+/−7 | 73+/−7 | 75+/−8 | 0.03 |
| Education, years, mean +/−SD | 12+/−3 | 12+/−3 | 11+/−3 | 12+/−3 | 0.07 |
| Female,% | 41 | 44 | 45 | 32 | 0.31 |
| White, % | 91 | 93 | 94 | 85 | 0.24 |
| Married, % | 61 | 62 | 59 | 62 | 0.95 |
| Just enough/not enough money, % | 58 | 54 | 61 | 58 | 0.68 |
| Lives alone, % | 20 | 16 | 22 | 21 | 0.67 |
| ≥1 ADL disablities, % | 39 | 32 | 48 | 34 | 0.13 |
| ≥3 IADL disability, % | 78 | 68 | 81 | 87 | 0.03 |
| ≥ 2 hospitalizations in previous year, % | 47 | 32 | 50 | 64 | <0.01 |
| Self-rated health, fair/poor,% | 67 | 53 | 81 | 66 | <0.01 |
| Physical discomfort, moderate/severe,% | 39 | 42 | 42 | 30 | 0.31 |
| Depression,% | 50 | 47 | 61 | 38 | 0.05 |
COPD = Chronic obstructive pulmonary disease, HF = Heart failure; ADL = activity of daily living; IADL = Instrumental activity of daily living
CG burden as measured by a short form of the Zarit Burden Inventory with scores ranging from 0–40 (higher scores indicate higher burden)
Characteristics of the 179 patients are also summarized in Table 1. The majority of patients reported ≥ 3 IADL disabilities (78%) and fair or poor self-rated health (67%), and 50% reported depression. A higher proportion of patients with HF reported greater than 2 hospitalizations in the previous year (64%) as compared with patients with COPD (50%) and cancer (32%). A higher proportion of patients with COPD reported their health to be fair or poor (81%) as compared to patients with cancer (53%) and HF (66%).
Description of Caregiver Burden at Baseline and over 12 Months
At baseline, the median caregiver burden (on a 0–40 scale) was 5 (interquartile range [IQR 1,11]), which indicates that the caregiver endorsed having at least 2 of the 10 concerns included in the scale. For example, a score of 5 can reflect the reporting of one concern occurring “always” and a second occurring “rarely” or the reporting of one concern occurring “sometimes” and a second occurring “frequently.” Only 10% reported no burden. The mean (m) caregiver burden score was 7.12 and the standard deviation (SD) was 7.2. Caregiver burden scales of this magnitude have been reported in caregivers of patients with dementia (m = 7.56, SD = 7.8434), and terminal cancer receiving palliative care using the full length ZBI with scores ranging from 0–88 (m =18.3, SD = 11.641, and m = 18.5, SD = 11.033).
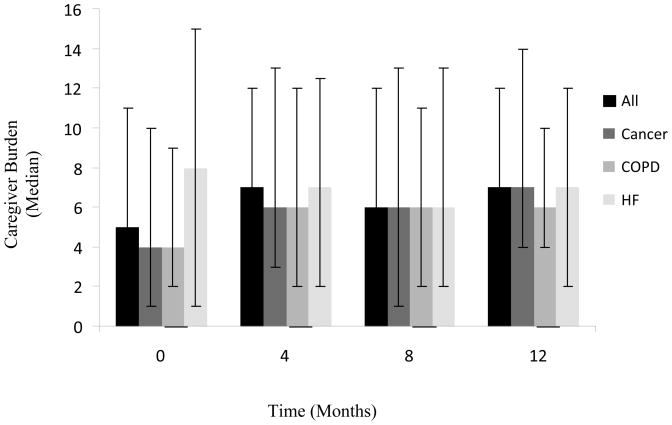
Over 12 months, there was little change in caregiver burden overall. Whereas burden increased slightly among caregivers of patients with COPD and cancer, it decreased among caregivers of patients with HF (Figure 1). Among caregivers of the patients who completed a full year of study participation, the initial caregiver burden score was 4 (IQR 1, 12) and the final score was 6 (IQR 2, 12). Among caregivers of the patients who died or became too sick to complete the full year, the initial score was 6 (IQR 3, 10) and the final score was 7 (IQR 3, 14).
Figure 1. Longitudinal Description of Caregiver Burden by Patient Diagnosis.
The figure shows the median caregiver burden score and interquartile range measured at baseline (time 0), 4 month, 8 month, and 12 month follow up. Caregiver burden was assessed during an in person interview with the caregiver using a 10 item short-form of the Zarit Burden Inventory scored on a 5 point Likert scale with total scores ranging from 1 – 40. The total sample size at base line was 179 caregivers (cancer 68, COPD 64, HF 47), 4 months was 165 (cancer 54, COPD 63, HF 48), 8 months was 137 (cancer 41, COPD 57, HF 39) and 12 months was 113 (cancer 27, COPD 51, HF 35).
Caregiver and Patient Characteristics in Association with Caregiver Burden
In bivariate cross-sectional analysis, the patient’s report of moderate to severe physical discomfort was the only patient characteristic significantly associated with high burden (Table 2). A larger proportion of caregivers of patients who had a diagnosis of HF, greater IADL disability, depression, and moderate to severe shortness of breath reported high caregiver burden when compared to caregivers of patients without these characteristics, however these differences did not reach statistical significance. Additional patient characteristics examined were not associated with caregiver burden (age, gender, race, education, marital status, self-rated health, number of hospitalizations in the six months prior to study enrollment, ADL disability, and living alone.) In contrast, a number of caregiver psychosocial and demographic characteristics were associated with high burden, as were several caregiver concerns. The large majority of caregivers who reported needing more help with daily tasks reported a high burden (88%), as compared to 40% of caregivers who did not need more help (p<0.001). Likewise, nearly all caregivers who reported a need for more emotional support reported high burden (97%) as compared to 36% of caregivers who did not need more support (p<0.001). The caregivers’ desire for more communication with their relative and with their relative’s doctor, as well as female gender of the caregiver, were significantly associated with high caregiver burden. A greater proportion of caregivers with the relationship to the patient of child as compared to those with the relationship of spouse or other reported higher burden, as did caregivers with not enough or just enough money as compared to caregivers with more than enough money, but these relationships did not reach statistical significance. A greater proportion of caregivers who were concerned their loved one’s life would be inappropriately prolonged by machines and who were concerned their loved one’s symptoms would not be well controlled reported high burden as compared to those who did not have this concerns, but these relationships did not reach statistical significance (Table 2).
Table 2.
Bivariate Associations between Patient and Caregiver Characteristics and High Caregiver Burden in Cross-Sectional Analysis
| Patient Characteristics | High Burden % (n=84) | P Value |
|---|---|---|
| Diagnosis | 0.13 | |
| Cancer, (n = 68) | 43 | |
| COPD, (n = 64) | 42 | |
| HF, (n = 47) | 60 | |
| IADL disabilities | 0.18 | |
| ≥3, (n = 139) | 50 | |
| <3, (n = 40) | 38 | |
| Physical discomfort | 0.03 | |
| Moderate/severe, (n = 70) | 57 | |
| None/mild, (n = 109) | 40 | |
| Shortness of breath | 0.16 | |
| Moderate/severe, (n=67) | 54 | |
| None/mild, (n=112) | 43 | |
| Depression | 0.12 | |
| Present, (n=89) | 53 | |
| Absent, (n=90) | 41 | |
| Caregiver characteristics | ||
| Gender | 0.05 | |
| Female, (n = 140) | 51 | |
| Male, (n = 39) | 33 | |
| Income | 0.08 | |
| Not enough/just enough money, (n = 78) | 55 | |
| More than enough money, n = 96) | 42 | |
| Relationship to patient | 0.07 | |
| Spouse, husband, wife, (n = 100) | 45 | |
| Child, daughter, son, (n = 49) | 59 | |
| Other, (n = 30) | 33 | |
| More help with daily tasks needed | <0.001 | |
| Yes, ( = 24) | 88 | |
| No, (n = 154) | 40 | |
| More emotional support needed | <0.001 | |
| Yes, (n = 30) | 97 | |
| No, (n = 144) | 36 | |
| “I am concerned that symptoms will not be controlled” | 0.09 | |
| Strongly agree/agree, (n = 70) | 56 | |
| Neither agree nor disagree/disagree/strongly disagree, (n =109) | 43 | |
| “I am concerned the patient’s life will be inappropriately prolonged” | ||
| Strongly agree/agree, (n=44) | 57 | 0.13 |
| Neither agree nor disagree/disagree/strongly disagree (n=135) | 44 | |
| “I would like to talk to the patient about his/her illness more” | 0.03 | |
| Strongly agree/agree, (n = 70) | 57 | |
| Neither agree nor disagree/disagree/strongly disagree, (n =109) | 40 | |
| “I would like to talk to the doctor about the patient’s illness more” | 0.03 | |
| Strongly agree/agree, (n = 62) | 58 | |
| Neither agree nor disagree/disagree/strongly disagree, (n =117) | 41 | |
COPD = Chronic Obstructive Pulmonary Disease; HF = Heart Failure
In longitudinal multivariable analysis, the need for more help with daily tasks remained the variable most strongly associated with high caregiver burden. Because this variable was highly correlated with the need for greater emotional support, the latter was not included in the multivariable model. In addition, caregiver’s desire for more communication with the patient remained statistically significantly associated with high caregiver burden. This variable was highly correlated with desire for more communication with the patient’s doctor, so that the latter was not included in the model. Time in the study and caregivers’ relationship to the patient of child, as compared to spouse or other, were significantly associated with high burden in bivariate longitudinal analysis; however, these factors did not retain their significance in multivariable analysis. Patients’ reports of shortness of breath, physical discomfort, and depression, patient enrollment in hospice, and caregiver concerns about prolonging the patient’s life with machines had elevated odds ratios but the results did not reach statistical significance (Table 3). The relationships seen in cross-sectional analysis between diagnosis, caregiver gender, caregiver income, caregiver concerns that the patient’s symptoms would not be controlled, patient IADL disability and caregiver burden were not confirmed in longitudinal analysis.
Table 3.
Patient and Caregiver Characteristics Associated with Caregiver Burden in Longitudinal Bivariate and Multivariable Analysis
| Variables | Biavariate Odds Ratio (95% CI) | Multivariable Odds Ratio (95% CI) |
|---|---|---|
| Caregiver characteristics | ||
| Relationship to patient of child | 3.95 (1.09, 14.36) | 2.84 (0.78, 10.34) |
| More help with daily tasks needed | 30.63 (7.79, 120.50) | 23.13 (5.94, 90.06) |
| Concerns about prolonging life with machines | 2.25 (0.87, 5.82) | 2.03 (0.74, 5.59) |
| Desire to talk with relative more | 2.72 (1.32, 5.63) | 2.53 (1.16, 5.53) |
| Patient characteristics | ||
| Shortness of breath | 2.04 (0.88, 4.73) | 1.53 (0.63, 3.74) |
| Physical discomfort, moderate/severe | 1.92 (0.97, 3.79) | 1.47 (0.70, 3.07) |
| Depression | 2.06 (0.98, 4.32) | 1.49 (0.68, 3.29) |
| Enrolled in Hospice | 7.70 (0.98, 60.70) | 5.35 (0.62, 46.03) |
| Time (months) | 1.08 (1.01, 1.15) | 1.05 (0.98, 1.13) |
DISCUSSION
In this population of caregivers of older adults with advanced cancer, COPD, and HF, the great majority of caregivers reported caregiver burden measured in terms of psychosocial distress. Although caregivers for patients with HF reported higher burden at baseline than caregivers for patients with cancer and COPD, this difference did not reach statistical significance, and there was no longitudinal relationship between patient diagnosis and burden. Overall, level of burden showed only minimal change over time, and the relationship between time and burden did not remain significant in multivariable analysis. Caregiver characteristics were more strongly associated with high burden than were patient characteristics. In longitudinal analysis, the caregiver’s need for more help with daily tasks demonstrated the strongest association with high caregiver burden.
The level of caregiver burden found in this study was similar across different patient diagnoses and comparable to the level of burden previously documented among caregivers of patients with dementia34 and terminal cancer.33, 41 These findings suggest that caregiver burden may not be disease-specific but may be a universal phenomenon of caring for older adults with chronic illnesses.
Prior literature examining the relationship between patient characteristics and caregiver burden has yielded mixed results. A comprehensive review of caregiver burden among caregivers for patients with dementia concluded that patient variables were not particularly strong predictors of caregiver outcomes.42 However, one small study of caregivers of older adult patients with chronic illness found an association between activities of care performed by the caregiver and caregiver burden.43 A second small study of caregiver burden in caregivers of patients with terminal cancer receiving home palliative care was associated with patient psychological status.44 These latter studies analyzed association as correlations between patient characteristics and burden measured using continuous scales, which, in contrast to the conservative approach of evaluating caregiver burden as a dichotomous outcome used in the present study, may have increased the likelihood of finding associations.
The association of the caregivers’ objective need for social support and concerns about communication with high burden provide quantitative evidence consistent with the findings of qualitative studies on caregivers of patients with cancer,45 HF,18 and COPD,46 indicating that limited social support,45 social isolation,46 lack of professional communication with clinicians, and concerns about the future of the patient18 are important aspects of caregiver psychological wellbeing and possible sources of emotional strain. In a study of recently bereaved caregivers, informal social support was directly related to better caregiver physical and mental health.47
The need for increased social support was included in the study as a measure of caregivers’ objective requirements for more help with their caregiving tasks, in contrast to the caregiver burden scale, which was developed as a measure of the subjective emotional strain associated with those tasks. Given the strong high association between these measures, it could be argued that these are, instead, assessments of the same phenomenon. Several additional results of this study support the notion that the measure of need for social support, rather than reflecting an objective assessment of need, is assessing the subjective construct of the caregivers’ ability to cope with their caregiving role. First, caregiver burden was not strongly associated with patients’ functional disability, a measure of patients’ need for direct assistance from caregivers. Second, caregiver burden changed very little over the one-year course of the study, despite the advancing illness of the patients. Finally, caregiver burden was higher, albeit non-significantly, among caregivers of patients who received hospice services and presumably were therefore receiving an increased amount of formal caregiving services to relieve their burden. Taken together, these results suggest that the strain of caregiving may be determined to a large extent by the caregiver’s psychological response to their role, rather than by the objective tasks they perform to care for their relative. This conclusion is supported by a number of studies that have found a relationship between caregivers’ personality attributes and/or coping strategies and caregiver burden.16,21,22
These findings have several implications for the clinical care of patients with advanced illness and their families. The level and frequency of caregiver burden suggest that caregiver burden is important to assess in caregivers of older adult patients with advanced illnesses, regardless of specific diagnosis. The strong association between the caregivers’ perceived need for social support and high burden indicate that it may be possible to capture levels of burden by simply asking caregivers about their need for social and emotional support. The lack of association between burden and patient characteristics suggests that more work is necessary to understand fully the aspects of caregiving that contribute to caregivers’ sense of burden and need for greater assistance. However, the association between high caregiver burden and caregivers’ desire for more communication illustrates that unmet communication needs is one such aspect. It has been suggested that physicians who engage families in difficult conversations and demonstrate empathy for family emotions may relieve psychological stress on caretakers.1 To the extent that burden appears to be a function of the caregiver’s ability to adapt, rather than the caregiving needs of the patient, interventions aimed at helping the caregiver cope with his/her role may help reduce burden and improve caregiver outcomes. A review of psychosocial interventions aimed at caregivers concluded that they had small but significant effects on caregiver burden, depression, and anxiety.48 Improved understanding about factors that affect caregivers’ ability to adapt and cope may aid in developing interventions with even greater efficacy.
This study has several limitations. Several caregiver characteristics that have previously been found to be associated with caregiver burden were not measured in this study, such as the caregiver’s functional status, depression, and cognition,16 or the quality of the relationship between caregiver and patient.20 Because the study cohort included few caregivers of minority ethnic/racial status, whose burden has been shown to differ systematically from that of White caregivers, the results may have limited generalizability.49 The one-year study period reflects only a brief portion in the course of patients’ entire illness trajectories. Because we studied caregivers of patients with advanced illness, a substantial proportion did not complete participation, because of the death or worsening health of the patient. Although this drop-out was unavoidable, it created the potential for bias in the measurement of burden over time if caregivers with the greatest burden were more likely to fail to complete the study. However, although the initial burden scores were slightly higher for caregivers who did not complete participation compared to those who did, the final burden scores were similar, providing some evidence that burden did not rise substantially prior to the caregiver leaving the study. Lastly, the ZBI scale does not have an a priori defined threshold for high burden34 because cut-off scores35 are not sufficiently specific or sensitive. Thus it is unknown if the caregivers in the high burden group were at increased risk for adverse.
In conclusion, caregiver burden, assessed in terms of psychosocial distress, was common among caregivers of patients with cancer, HF, and COPD. High burden was associated with the caregiver’s report of need for greater help with daily tasks but not with factors affecting the patient’s need for assistance, such as symptoms or functional status, suggesting that burden may be a measure of the caregiver’s ability to adapt to the caregiving role.
Acknowledgments
American Federation of Aging Research, Medical Student Training in Aging Award, P30 AG21342 from the Claude D. Pepper Older Americans Independence Center at Yale University and R01 AG19769 from the National Institute on Aging. Dr Fried is supported by grant K24 AGAG028443 from the National Institute on Aging.
Sponsors’ role: The sponsors had no role in the design, methods, subject recruitment, data collection, or analysis and preparation of the paper.
Funding sources: American Federation of Aging Research, Medical Student Training in Aging Award, P30 AG21342 from the Claude D. Pepper Older Americans Independence Center at Yale University and R01 AG19769 from the National Institute on Aging. Dr Fried is supported by grant K24 AGAG028443 from the National Institute on Aging.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
Study concept and design: KG, TF
Acquisition of subjects and data: TF
Analysis and interpretation of data: KG, PHVN, JOL, TF
Preparation of manuscript: KG, TF
Editing of manuscript: PHVN, JOL, TF
References
- 1.Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: “they don’t know what they don’t know”. JAMA. 2004;291:483–491. doi: 10.1001/jama.291.4.483. [DOI] [PubMed] [Google Scholar]
- 2.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 3.Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families. SUPPORT investigators study to understand prognoses and preferences for outcomes and risks of treatment. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 4.Emanuel EJ, Fairclough DL, Slutsman J, et al. Understanding economic and other burdens of terminal illness: The experience of patients and their caregivers. Ann Intern Med. 2000;132:451–459. doi: 10.7326/0003-4819-132-6-200003210-00005. [DOI] [PubMed] [Google Scholar]
- 5.Beery LC, Prigerson HG, Bierhals AJ, et al. Traumatic grief, depression and caregiving in elderly spouses of the terminally ill. Omega: Int Manage Sci. 1997;35:261–279. [Google Scholar]
- 6.Anthony-Bergstone CR, Zarit SH, Gatz M. Symptoms of psychological distress among caregivers of dementia patients. Psychol Aging. 1988;3:245–248. doi: 10.1037//0882-7974.3.3.245. [DOI] [PubMed] [Google Scholar]
- 7.Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 8.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 9.Burton LC, Newsom JT, Schulz R, et al. Preventive health behaviors among spousal caregivers. Prev Med. 1997;26:162–169. doi: 10.1006/pmed.1996.0129. [DOI] [PubMed] [Google Scholar]
- 10.Kiecolt-Glaser JK, Dura JR, Speicher CE, et al. Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosom Med. 1991;53:345–362. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- 11.von Kanel R, Dimsdale JE, Mills PJ, et al. Effect of Alzheimer caregiving stress and age on frailty markers interleukin-6, C-reactive protein, and D-dimer. J Gerontol A Biol Sci Med Sci. 2006;61:963–969. doi: 10.1093/gerona/61.9.963. [DOI] [PubMed] [Google Scholar]
- 12.Schulz R, Beach SR. Caregiving as a risk factor for mortality: The caregiver health effects study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 13.Uwakwe R, Modebe I. Disability and care-giving in old age in a Nigerian community. Niger J Clin Pract. 2007;10:58–65. [PubMed] [Google Scholar]
- 14.Andrieu S, Balardy L, Gillette-Guyonnet S, et al. Burden experienced by informal caregivers assisting Alzheimer’s patients in the REAL.FR study. Rev Med Interne. 2003;3:351s–359s. doi: 10.1016/s0248-8663(03)80695-1. [DOI] [PubMed] [Google Scholar]
- 15.Ho SC, Chan A, Woo J, et al. Impact of caregiving on health and quality of life: A comparative population-based study of caregivers for elderly persons and noncaregivers. J Gerontol A Biol Sci Med Sci. 2009;64:873–879. doi: 10.1093/gerona/glp034. [DOI] [PubMed] [Google Scholar]
- 16.Schulz R, Martire LM. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12:240–249. [PubMed] [Google Scholar]
- 17.McCorkle R, Pasacreta JV. Enhancing caregiver outcomes in palliative care. Cancer Control. 2001;8:36–45. doi: 10.1177/107327480100800106. [DOI] [PubMed] [Google Scholar]
- 18.Aldred H, Gott M, Gariballa S. Advanced heart failure: Impact on older patients and informal carers. J Adv Nurs. 2005;49:116–124. doi: 10.1111/j.1365-2648.2004.03271.x. [DOI] [PubMed] [Google Scholar]
- 19.Hooley PJ, Butler G, Howlett JG. The relationship of quality of life, depression, and caregiver burden in outpatients with congestive heart failure. Congest Heart Fail. 2005;11:303–310. doi: 10.1111/j.1527-5299.2005.03620.x. [DOI] [PubMed] [Google Scholar]
- 20.Pinto RA, Holanda MA, Medeiros MM, et al. Assessment of the burden of caregiving for patients with chronic obstructive pulmonary disease. Respir Med. 2007;101:2402–2408. doi: 10.1016/j.rmed.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 21.Lyons KS, Stewart BJ, Archbold PG, et al. Optimism, pessimism, mutuality, and gender: predicting 10-year role strain in Parkinson’s Disease spouses. Gerontologist. 2009;49:378–387. doi: 10.1093/geront/gnp046. [DOI] [PubMed] [Google Scholar]
- 22.Powers DV, Gallagher-Thompson D, Kraemer HC. Coping and depression in Alzheimer’s caregivers: Longitudinal evidence of stability. J Gerontol Series B Psychol Sci Soc Sci. 2002;57:205–211. doi: 10.1093/geronb/57.3.p205. [DOI] [PubMed] [Google Scholar]
- 23.Fried TR, Byers AL, Gallo WT, et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med. 2006;166:890–895. doi: 10.1001/archinte.166.8.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fried TR, Bradley EH, Towle VR. Assessment of patient preferences: Integrating treatments and outcomes. J Gerontol B Psychol Sci Soc Sci. 2002;57:S348–S354. doi: 10.1093/geronb/57.6.s348. [DOI] [PubMed] [Google Scholar]
- 25.Murphy DJ, Knaus WA, Lynn J. Study population in SUPPORT: Patients (as defined by disease categories and mortality projections), surrogates, and physicians. J Clin Epidemiol. 1990;43:11S–28S. doi: 10.1016/0895-4356(90)90213-9. [DOI] [PubMed] [Google Scholar]
- 26.Knaus WA, Harrell FE, Jr, Lynn J, et al. The SUPPORT prognostic model. objective estimates of survival for seriously ill hospitalized adults. study to understand prognoses and preferences for outcomes and risks of treatments. Ann Intern Med. 1995;122:191–203. doi: 10.7326/0003-4819-122-3-199502010-00007. [DOI] [PubMed] [Google Scholar]
- 27.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 28.Inouye SK, Peduzzi PN, Robison JT, et al. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–1193. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 29.Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: The executive interview. J Am Geriatr Soc. 1992;40:1221–1226. doi: 10.1111/j.1532-5415.1992.tb03646.x. [DOI] [PubMed] [Google Scholar]
- 30.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 31.Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged. the index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 32.Schulz R, Williamson GM. The measurement of caregiver outcomes in Alzheimer disease research. Alzheimer Dis Assoc Disord. 1997;6:117–124. [PubMed] [Google Scholar]
- 33.Higginson IJ, Gao W. Caregiver assessment of patients with advanced cancer: Concordance with patients, effect of burden and positivity. Health Qual Life Outcomes. 2008;6:42. doi: 10.1186/1477-7525-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Rourke N, Tuokko HA. Psychometric properties of an abridged version of the Zarit burden interview within a representative Canadian caregiver sample. Gerontologist. 2003;43:121–127. doi: 10.1093/geront/43.1.121. [DOI] [PubMed] [Google Scholar]
- 35.Bedard M, Molloy DW, Squire L, et al. The Zarit burden interview: A new short version and screening version. Gerontologist. 2001;41:652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- 36.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 37.Walke LM, Gallo WT, Tinetti M, et al. The burden of symptoms among community-dwelling older persons with advanced chronic disease. Arch Intern Med. 2004;164:2321–2324. doi: 10.1001/archinte.164.21.2321. [DOI] [PubMed] [Google Scholar]
- 38.Whooley MA, Avins AL, Miranda J, et al. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pearlin LI, Lieberman MA, Menaghan EG, et al. The stress process. J Health Soc Behav. 1981;22:337–356. [PubMed] [Google Scholar]
- 40.Mendes de Leon CF, Gold DT, Glass TA, et al. Disability as a function of social networks and support in elderly African Americans and whites: The Duke EPESE 1986--1992. J Gerontol B Psychol Sci Soc Sci. 2001;56:S179–S190. doi: 10.1093/geronb/56.3.s179. [DOI] [PubMed] [Google Scholar]
- 41.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: Results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170:1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dunkin J, Anderson-Hanley C. Dementia caregiver burden: A review of the literature and guidelines for assessment and intervention. Neurology. 1998;51:S53–S60. doi: 10.1212/wnl.51.1_suppl_1.s53. [DOI] [PubMed] [Google Scholar]
- 43.Faison KJ, Faria SH, Frank D. Caregivers of chronically ill elderly: Perceived burden. J Community Health Nurs. 1999;16:243–253. doi: 10.1207/S15327655JCHN1604_4. [DOI] [PubMed] [Google Scholar]
- 44.Harding R, Higginson IJ, Donaldson N. The relationship between patient characteristics and carer psychological status in home palliative cancer care. Support Care Cancer. 2003;11:638–643. doi: 10.1007/s00520-003-0500-6. [DOI] [PubMed] [Google Scholar]
- 45.Payne S, Smith P, Dean S. Identifying the concerns of informal carers in palliative care. Palliat Med. 1999;13:37–44. doi: 10.1191/026921699673763725. [DOI] [PubMed] [Google Scholar]
- 46.Bergs D. “The hidden client”--women caring for husbands with COPD: Their experience of quality of life. J Clin Nurs. 2002;11:613–621. doi: 10.1046/j.1365-2702.2002.00651.x. [DOI] [PubMed] [Google Scholar]
- 47.Williams SW, Williams CS, Zimmerman S, et al. Emotional and physical health of informal caregivers of residents at the end of life: The role of social support. J Gerontol B Psychol Sci Soc Sci. 2008;63:S171–S183. doi: 10.1093/geronb/63.3.s171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martire LM, Lustig AP, Schulz R, et al. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychol. 2004;23:599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- 49.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) Gerontologist. 2002;42:237–72. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]