Abstract
PURPOSE
To utilize high-resolution spectral domain optical coherence tomography (SD-OCT) in the characterization of retinal and vitreal morphological changes overlying posterior lattice degeneration.
METHODS
A cross-sectional, retrospective analysis was performed on 13 eyes of 13 nonconsecutive subjects with posterior lattice degeneration seen at the New England Eye Center, Tufts Medical Center between October 2009 and January 2010. SD-OCT images taken through the region of lattice degeneration were qualitatively analyzed.
RESULTS
Four characteristic changes of the retina and vitreous were seen in the 13 eyes with lattice degeneration: (1) anterior/posterior U-shaped vitreous traction, (2) retinal breaks, (3) focal retinal thinning, and (4) vitreous membrane formation. The morphological appearance of vitreous traction and retinal breaks were found to be consistent with previous histological reports.
CONCLUSIONS
It is possible to image posterior lattice degeneration in many eyes using SD-OCT and to visualize the spectrum of retinal and vitreous changes throughout the area of lattice degeneration.
Keywords: Lattice degeneration, Optical Coherence Tomography
Introduction
Lattice degeneration is a common, atrophic disease of the peripheral retina affecting approximately 7–10% of the general population, with peak prevalence in the second decade.1, 2 Over the past decade, there has been little published on lattice degeneration. Much of what is understood today about it is based on clinical studies, autopsy, and electron microscopic reports dating back thirty to forty years.1–3
Lattice degeneration is clinically characterized by a sharply demarcated, oval, round, or linear areas of retinal thinning, usually located between the equator of the retina and the posterior border of the vitreous base, running nearly parallel to the ora serrata in a circumferentially oriented pattern. The lesions are typically bilateral and are more often located in the temporal region of the fundus.1–4 Histological studies characterize the features of lattice degeneration as having retinal thinning, vitreous liquefaction, vitreous adhesion at lattice margins, vascular changes, retinal pigment abnormalities, and accumulations of dense amorphous material.1 The exact etiology of lattice degeneration, however, is not well understood. Theories have suggested regional developmental absence of the internal limiting membrane with defects in the fibers of the Müller’s cells3 versus abnormal vitreoretinal traction dynamics.5
The clinical and histological findings in lattice degeneration have been described; however the spectral domain optical coherence tomography (SD-OCT) correlate of lattice degeneration has not been previously examined. Therefore, the purpose of this study is to qualitatively assess the structure of lattice degeneration using SD-OCT.
Patients and Methods
A retrospective analysis of 13 eyes of 13 patients with lattice degeneration was performed. All patients were examined on the retina service of the ophthalmology department of the New England Eye Center, Tufts Medical Center, Boston, Massachusetts between October 2009 and January 2010. Examination included Snellen best corrected visual acuity, slit-lamp examination, fundus biomicroscopy, color fundus photography, and OCT examination. None of the patients included in this study presented with symptoms related to the lattice degeneration. This study protocol was approved by the Institutional Review Board/Ethics Committee (IRB) of Tufts Medical Center and is compliant with the Health Insurance Portability and Accountability Act (HIPAA) of 1996.
This study utilized SD-OCT imaging to characterize retinal findings in lattice degeneration. OCT has been well established as an accurate imaging study of known retinal pathology through good correlation between histology of animals and humans in vivo.6–9 Precise correlation with histology is limited because histological fixation produces artifacts due to processing, tissue deformation, and shrinkage.6 OCT images provide an accurate visualization of the actual retinal architecture in vivo. Five line raster scans taken at various angles with respect to the lattice structure using SD Cirrus HD-OCT (Carl Zeiss Meditec, Dublin, CA) were analyzed. A 5-line raster scan protocol consists of 5 parallel lines, each 6mm long, comprised of 4096 A-scans, and spaced 0.25mm apart. The axial resolution in OCT imaging is inversely proportional to the bandwidth of the light source. SD-OCT devices utilize a superluminescent diode (SLD) light source at a near infrared wavelength of 820 nm with a bandwidth of 50 nm, achieving 5–8 μm axial resolution and a transverse resolution of ~15–20 μm in tissue. The SD-OCT cross-sectional images and summed voxel projections, or reconstructed en face fundus views, were correlated to color fundus photographs and evaluated for characteristic changes in the retina overlying the area of lattice degeneration.
Results
Twenty-one eyes with lattice degeneration were attempted to be imaged using the Cirrus HD-OCT retinal scanner, of which 13 eyes (62%) were included in this study. The 13 eyes consisted of 6 males and 7 females, with a mean age of 56.7 years (range, 30 – 70 years). Eight eyes were excluded from the study because (1) it could not be determined with certainty that the obtained image was directly overlying the lattice structure, (2) the images could not be obtained at all due the far peripheral location of the lattice, and (3) the image quality was too poor to be evaluated. Due to the limitations of both the SD-OCT scanner and the subject’s ability to fixate, the lattice degeneration that was examined was primarily posteriorly located lattice.
The 13 OCT images were qualitatively assessed to describe 4 characteristic changes of the retina and vitreous overlying lattice degeneration: (1) anterior/posterior U-shaped vitreous traction, (2) retinal breaks (including atrophic holes and retinal detachments) (3) focal retinal thinning, and (4) vitreous membrane formation. It was noted that even within one eye, different sites of lattice demonstrated more than one of the various characteristics stated above (Figures 1–5).
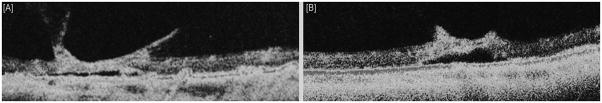
FIGURE 1. U-shaped vitreous traction.
(A, B) Anterior and posterior vitreous traction with focal retinal detachment seen on spectral domain optical coherence tomography (SD-OCT) imaging from two different eyes with lattice degeneration.
FIGURE 5. Vitreous membrane.
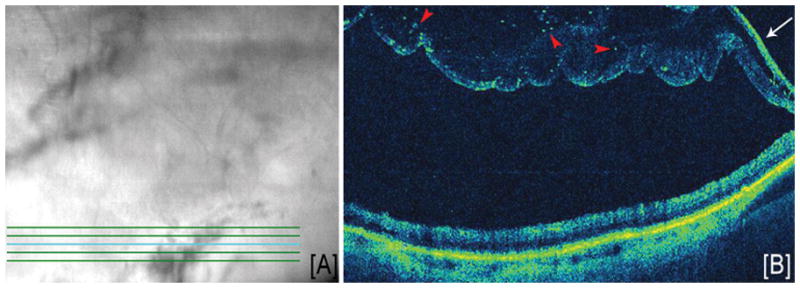
(A) Summed voxel projection generated by Cirrus HD-OCT and (B) corresponding spectral domain optical coherence tomography (SD-OCT) image from five line raster scan showing the presence of a vitreous membrane with increased reflectivity (white arrow) seen along one edge with focal reflective deposits suspended within the detached vitreous (red arrowheads).
Discussion
OCT was developed to perform a noninvasive “optical biopsy” and in that sense, the SD-OCT findings in this study demonstrated a striking correlation with previously reported histological findings of lattice degeneration. SD-OCT provides a distinct cross-sectional and three-dimensional view of the eye in vivo that is unique from the specimens examined using histological fixation. This is the first study to show that SD-OCT imaging of lattice degeneration is possible.
1. U-shaped vitreous traction
In six (46%) of the images that were examined, posterior vitreous separation was noted over the lattice structure. Anterior and posterior vitreous separation was seen with adherence over the area of lattice, giving it a U-shaped appearance (Figure 1). This appearance is consistent with the known structure of the vitreous in lattice degeneration with the vitreous gel condensed and firmly adherent to the margins of the lesion and a clear pocket of liquid vitreous over the central portion of the lesion.1, 10 One hypothesis suggests that the process behind these vitreous changes result from underlying vascular abnormalities. The retinal vasculature within the lattice structure undergoes obliterative fibrosis leading to vascular insufficiency and ischemia. First inner and then outer retinal damage occurs triggering glial cell proliferation and extension throughout the extracellular space. Eventual internal limiting membrane disruption occurs leading to dissolution of vitreoretinal attachments.1 Nevertheless, no theories have yet been proven in the pathogenesis of lattice degeneration.
All six of the images demonstrating U-shaped vitreous traction were also noted to be associated with focal retinal detachments. The retinal tissue overlying the detachments was noted to have a hyper-reflective appearance, suggesting the presence of either disruption of normal cell structure or pigment migration. Scanning electron microscopy studies demonstrate the existence of preretinal glial membranes over lattice which were stimulated from breaks in the internal limiting membrane.11 The increased reflectivity seen on SD-OCT in this study may represent this extra membrane formation. Other studies have also demonstrated neuronal degeneration causing generalized disruption of retinal layers, which could account for the irregular hyperreflectivity.1
2. Retinal Breaks
In two eyes, an atrophic retinal hole was observed. In neither of these eyes was vitreous traction seen (Figure 2). Lattice generation is known to be associated with secondary peripheral retinal atrophic holes, which are full-thickness breaks with no associated free operculum or flap and no PVD.12, 13 Atrophic holes are the most commonly seen type of retinal break, typically remain stable for years, and are rarely associated with retinal detachments. SD-OCT imaging from one other eye revealed a similar defect in retinal tissue with the presence of an atrophic hole, however one edge demonstrated vitreous traction with the presence of subretinal fluid (Figure 3). This image represents a subclinical retinal detachment since it is at least one disc diameter and associated with an atrophic hole.13, 14 This image is consistent with the understanding that retinal tears which can lead to rhegmatogenous retinal detachments are associated with PVDs.13
FIGURE 2. Atrophic retinal hole.
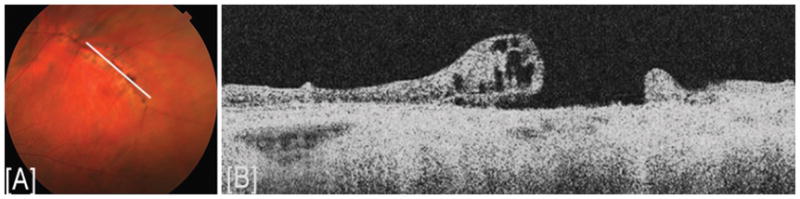
(A) Color fundus photograph and (B) spectral domain optical coherence tomography (SD-OCT) image demonstrating atrophic retinal hole with no vitreous traction.
FIGURE 3. Subclinical retinal detachment.
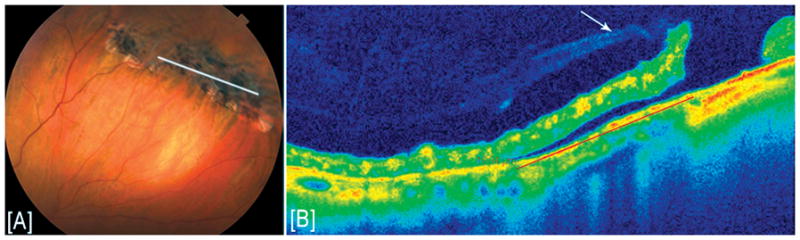
(A) Color fundus photograph and (B) spectral domain optical coherence tomography (SD-OCT) image demonstrating vitreous traction on one edge of an atrophic hole (white arrow) with subclinical retinal detachment measuring 1800 μm.
3. Retinal Thinning
In three (23%) eyes, retinal thinning was seen throughout the entire area of lattice, without clear distinction of inner and outer retinal layers (Figure 4). Within the region of thinning, it was noted that there were focal areas of increased retinal thinning, with the appearance of missing inner retinal tissue. This finding is consistent with histological reports of retinal thinning in lattice degeneration with the inner retina most severely affected as well as generalized thinning causing disruption all cell layers.1 It has also been theorized that retinal thinning eventually leads to atrophic hole formation and is not a result of tractional forces.3
FIGURE 4. Retinal thinning.
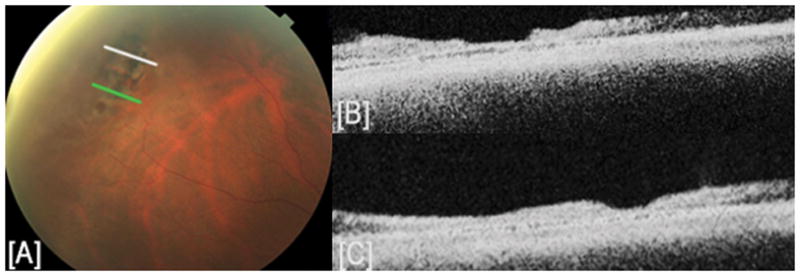
(A) Color fundus photograph and (B, C) spectral domain optical coherence tomography (SD-OCT) images represented by white and green lines respectively on fundus image. The OCT images demonstrate overall retinal thinning over the lattice degeneration with generalized disruption of all retinal layers and a central area of increased thinning with loss of inner retinal tissue.
4. Vitreous Membranes
Two (15%) SD-OCT images demonstrated vitreous separation, with a band of increased reflectivity along one edge, which may represent a vitreous membrane (Figure 5). One of these images showed numerous reflective deposits scattered within the detached vitreous, which may represent aggregates of cellular debris or hyalocytes. One histological report noted the presence of dense amorphous Periodic acid-Schiff (PAS)-positive material surrounding the lattice structure, which was thought to be extracellular products of cell breakdown and fibrosis.1
Notably, the development of lattice degeneration may be related to increased axial elongation as it is more commonly seen in myopic eyes, with up to 10% of these patients affected.1, 15 In patients with high myopia, it is an important cause of peripheral retinal degeneration and predisposes to rhegmatogenous retinal detachment, particularly at increasing degrees of myopia.4 Most retinal detachments seen in patients with lattice degeneration are secondary to tractional retinal tears following posterior vitreous detachment (PVD), and less frequently from atrophic retinal holes present within the lattice structure, except in younger patients under the age of 30.4
Based on the low incidence of retinal detachments associated with lattice degeneration, several studies demonstrated little benefit and even potential harm in prophylactic treatment of lattice.13, 16–19 This study presents SD-OCT as an ancillary imaging method that may have utility in monitoring overlying changes to the lattice structure. Patients who develop rhegmatgenous retinal detachments not related to PVDs and have peripheral retinal degeneration in the fellow eye have been noted to be at higher risk for detachment in the contralateral eye3, 20, 21; therefore SD-OCT testing could be utilized in monitoring the fellow eye for changes.
Drawbacks to this study are the retrospective design, the variable angle and location at which the SD-OCT raster scans were taken that may have altered the view of the retina, as well as the limitation to primary posterior lattice structures. In addition, not all lattice lesions in an eye were imaged. Furthermore, this study is aims to qualitatively describe the SD-OCT appearance of lattice degeneration; therefore, therapeutic implications cannot directly be made based on the images.
In conclusion, this study shows that SD-OCT evaluation of peripheral retinal lesions like lattice degeneration is possible. Considering the varying appearance of lattice between individuals and even within one eye, this descriptive analysis confirms that lattice degeneration evolves along a continuing spectrum, with the retinal and vitreal changes observed at various stages of change. This study demonstrates that SD-OCT imaging of lattice is feasible and has clinical utility in that SD-OCT imaging allows for monitoring changes overlying lattice degeneration over time.
Summary Statement.
Lattice degeneration is a common finding in the peripheral retina and represents an important risk factor for rhegmatogenous retinal detachment (RD). This study characterizes the spectral domain optical coherence tomography (SD-OCT) appearance of posterior lattice degeneration and correlates findings with previous histological reports.
Acknowledgments
Financial Support
This work was supported in part by a Research to Prevent Blindness Challenge grant to the New England Eye Center/Department of Ophthalmology -Tufts University School of Medicine, NIH contracts R01-EY11289-24, R01-EY13178-10, R01-EY013516-07, Air Force Office of Scientific Research FA9550-07-1-0101, FA9550-07-1-0014, and Massachusetts Lions Eye Research Fund.
Footnotes
Disclosures
The sponsors had no role in the design or conduct of this research.
Jay S. Duker receives research support from Carl Zeiss Meditec, Inc., Optovue Corporation, and Topcon Medical Systems, Inc. James G. Fujimoto receives royalties from intellectual property owned by M.I.T. and licensed to Carl Zeiss Meditec, Inc. and LightLabs Imaging and has stock options in Optovue Corporation.
References
- 1.Straatsma BR, Zeegen PD, Foos RY, et al. Lattice degeneration of the retina. XXX Edward Jackson Memorial Lecture. Am J Ophthalmol. 1974;77:619–49. doi: 10.1016/0002-9394(74)90525-x. [DOI] [PubMed] [Google Scholar]
- 2.Byer NE. Clinical study of lattice degeneration of the retina. Trans Am Acad Ophthalmol Otolaryngol. 1965;69:1065–81. [PubMed] [Google Scholar]
- 3.Byer NE. Lattice degeneration of the retina. Surv Ophthalmol. 1979;23:213–48. doi: 10.1016/0039-6257(79)90048-1. [DOI] [PubMed] [Google Scholar]
- 4.Tillery WV, Lucier AC. Round atrophic holes in lattice degeneration--an important cause of phakic retinal detachment. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1976;81:509–18. [PubMed] [Google Scholar]
- 5.Tolentino F, Schepens C, Freeman H. Vitreoretinal Disorders, Diagnosis and Management. Philadelphia: Saunders; 1976. pp. 340–9. [Google Scholar]
- 6.Anger EM, Unterhuber A, Hermann B, et al. Ultrahigh resolution optical coherence tomography of the monkey fovea. Identification of retinal sublayers by correlation with semithin histology sections. Exp Eye Res. 2004;78:1117–25. doi: 10.1016/j.exer.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Gloesmann M, Hermann B, Schubert C, et al. Histologic correlation of pig retina radial stratification with ultrahigh-resolution optical coherence tomography. Invest Ophthalmol Vis Sci. 2003;44:1696–703. doi: 10.1167/iovs.02-0654. [DOI] [PubMed] [Google Scholar]
- 8.Abbott CJ, McBrien NA, Grunert U, Pianta MJ. Relationship of the optical coherence tomography signal to underlying retinal histology in the tree shrew (Tupaia belangeri) Invest Ophthalmol Vis Sci. 2009;50:414–23. doi: 10.1167/iovs.07-1197. [DOI] [PubMed] [Google Scholar]
- 9.Chen TC, Cense B, Miller JW, et al. Histologic correlation of in vivo optical coherence tomography images of the human retina. Am J Ophthalmol. 2006;141:1165–8. doi: 10.1016/j.ajo.2006.01.086. [DOI] [PubMed] [Google Scholar]
- 10.Yanoff M, Duker JS. Ophthalmology. 3. Mosby, Inc; 2008. Peripheral Retinal Lesions. [Google Scholar]
- 11.Robinson MR, Streeten BW. The surface morphology of retinal breaks and lattice retinal degeneration. A scanning electron microscopic study. Ophthalmology. 1986;93:237–46. doi: 10.1016/s0161-6420(86)33759-x. [DOI] [PubMed] [Google Scholar]
- 12.Foos RY. Retinal holes. Am J Ophthalmol. 1978;86:354–8. doi: 10.1016/0002-9394(78)90239-8. [DOI] [PubMed] [Google Scholar]
- 13.Byer NE. Long-term natural history of lattice degeneration of the retina. Ophthalmology. 1989;96:1396–401. doi: 10.1016/s0161-6420(89)32713-8. discussion 401–2. [DOI] [PubMed] [Google Scholar]
- 14.Davis MD. The natural history of retinal breaks without detachment. Trans Am Ophthalmol Soc. 1973;71:343–72. [PMC free article] [PubMed] [Google Scholar]
- 15.Grossniklaus HE, Green WR. Pathologic findings in pathologic myopia. Retina. 1992;12:127–33. doi: 10.1097/00006982-199212020-00009. [DOI] [PubMed] [Google Scholar]
- 16.Robertson DM, Norton EW. Cause of failure in prophylactic treatment of retinal breaks. Mod Probl Ophthalmol. 1974;12:74–80. [PubMed] [Google Scholar]
- 17.Wilkinson C. Interventions for asymptomatic retinal breaks and lattice degeneration for preventing retinal detachment. Cochrane Database Syst Rev. 2005:CD003170. doi: 10.1002/14651858.CD003170.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson CP. Evidence-based analysis of prophylactic treatment of asymptomatic retinal breaks and lattice degeneration. Ophthalmology. 2000;107:12–5. doi: 10.1016/s0161-6420(99)00049-4. [DOI] [PubMed] [Google Scholar]
- 19.Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol. 2003;136:155–60. doi: 10.1016/s0002-9394(03)00144-2. [DOI] [PubMed] [Google Scholar]
- 20.Folk JC, Arrindell EL, Klugman MR. The fellow eye of patients with phakic lattice retinal detachment. Ophthalmology. 1989;96:72–9. doi: 10.1016/s0161-6420(89)32926-5. [DOI] [PubMed] [Google Scholar]
- 21.Gonzales CR, Gupta A, Schwartz SD, Kreiger AE. The fellow eye of patients with phakic rhegmatogenous retinal detachment from atrophic holes of lattice degeneration without posterior vitreous detachment. Br J Ophthalmol. 2004;88:1400–2. doi: 10.1136/bjo.2004.043240. [DOI] [PMC free article] [PubMed] [Google Scholar]