Abstract
Objectives
1) To develop stages of change measures for advance care planning (ACP), conceptualized as a group of interrelated but separate behaviors. 2) To use these measures to characterize older persons’ engagement in and factors associated with readiness to participate in ACP.
Design
Observational cohort study.
Setting
Community.
Participants
Persons age ≥ 65 recruited from physician offices and a senior center.
Measurements
Stages of change for six ACP behaviors: completion of a living will and health care proxy, communication with loved ones regarding use of life-sustaining treatments and quantity versus quality of life (QOL), and communication with physicians about these same issues.
Results
Readiness to participate in ACP varied widely across behaviors. Whereas between approximately 50–60% of participants were in the action or maintenance stage for communicating with loved ones and completing a living will, 40% were in the precontemplation stage for communicating with loved ones about quantity versus QOL, and 70–75% were in the precontemplation stage for communicating with physicians. Participants were frequently in different stages for the different behaviors. Relatively few sociodemographic, health, or psychosocial factors were associated with stages of change for completing a living will, but a broader range of factors was associated with stages of change for communication with loved ones about quantity versus QOL.
Conclusion
Older persons show a range of readiness to engage in different aspects of ACP. Individualized assessment and interventions targeted to stage of behavior change for each component of ACP may be an effective strategy to increase participation in ACP.
Keywords: advance care planning, health behavior, end-of-life care
INTRODUCTION
The concept of the steps needed to accomplish advance care planning (ACP) is evolving. Traditionally, the goal of ACP has been to promote patient decision-making autonomy, by having individuals pre-specify the care they wish to receive if they become unable to participate in treatment decision-making and/or the person who will make decisions regarding their care. The means of achieving this goal has been through the completion of advance directive (AD) documents, including living wills and durable powers of attorney for health care. The original intent was that these documents were to be completed only after individuals deliberated about and clarified their goals of care and communicated with their loved ones and clinicians. However, these additional steps frequently do not accompany the completion of ADs.1–4 Moreover, it has been argued that these steps represent not merely the means to promote patient autonomy, but serve as important goals for ACP in and of themselves.5 As a result, there is a growing consensus that the components of ACP should include as distinct processes the facilitation of communication among patients, their potential surrogate decision-makers, and physicians; and a consideration of patients’ goals of care.5–7
The concept of how individuals engage in ACP is also evolving. Traditional interventions have focused on the provision of standardized information and forms to patients and their surrogates.8, 9 However, it is increasingly recognized that ACP may best be understood as a health behavior, for which individuals have highly varied motivation, barriers and facilitators, and self-efficacy regarding their participation.10, 11 It has been proposed that the most effective interventions to increase participation in ACP would provide tailored information according to participants’ readiness for engagement.8
The Transtheoretical Model (TTM) provides a useful framework for considering ACP as a process of behavior change. It characterizes behavior change over time through five distinct Stages of Change. These stages include precontemplation (no intention to change behavior in the near future), contemplation (thinking about changing behavior in the near future), preparation (commitment to changing behavior soon), action (a recent change in behavior), and maintenance (ongoing behavior change). As the organizing construct for the TTM, stages of change, when combined with additional behavior change constructs, including decisional balance, efficacy, and processes of change, serves as the basis for interventions tailored to the needs of an individual.12 Such tailored interventions have been found effective for a range of health behavior changes.12, 13 The application of a stages-of-change model to ACP was first described by Pearlman, et al,14 who utilized the concept of stages of change in an intervention that was demonstrated to increase rates of completion of advance directives.15 There are three existing measures for evaluating stages of change in ACP. Two consider only the completion of ADs, 16, 17 and the second asks about multiple components of ACP (communication with surrogates and physicians, and completion of ADs) in a single item.18 Several studies have recently proposed the application of a stages-of-change model to ACP considered as consisting of multiple discrete steps,11, 19 but no measures currently exist to measure engagement in ACP in this way.
The purpose of this study was to bring together the concepts of ACP as a group of inter-related but separate healthcare behaviors. Its specific aims were: 1) to develop measures for the stages of change for these behaviors; 2) to use these measures to characterize older persons’ engagement in ACP and to examine the relationship among the stages across different behaviors; 3) to examine sociodemographic and health characteristics associated with stages of change.
METHODS
Measurement development
Measurement development began with identification of the set of behaviors that best characterizes current conceptions of ACP. This identification was accomplished through a literature review of expert opinion commentaries on ACP supplemented by the conduct of focus groups to understand older persons’ experiences with these behaviors.11 The literature review revealed a broad range of proposed objectives for ACP3, 5–7, 20 and the processes that best accomplish these objectives.2, 3, 5, 6, 20–23 Because several papers suggested a large number of potential objectives and processes that would yield an impractical number of behaviors, the literature review sought to identify a smaller set of shared objectives and processes. Even with this smaller set, several complex behaviors were identified that could be conceptualized as a series of separate behaviors versus a single behavior composed of a number of discrete steps. In this case, when a decision needed to be made regarding “lumping” versus “splitting,” the guiding principle was whether the individual step was regarded in the literature as being in and of itself sufficient to accomplish a necessary part of ACP.
Participants
Participants were age 65 years and older recruited from two primary care practices and one senior center. These sites were purposefully selected in order to provide access to a group of older persons with diversity in race, socioeconomic status, and health status. In the primary care practices, letters were sent to sequential persons age ≥ 65 who were screened by their physician as not having a diagnosis of dementia. Persons who agreed (92% and 88% in the two practices) underwent a telephone screen to determine exclusion criteria, which included: non-English speaker (7% and 2%), hearing loss precluding participation in interview (7% and 1%), nursing home resident (0% and 1%), acute episode of illness (8% and 4%), and cognitive impairment, defined as <2/3 recall on a test of short-term memory (7% and <1%). Among eligible participants, 83% and 80% completed interviews. In the senior center, volunteers were solicited for participation. All of the persons who volunteered were eligible for participation and completed interviews.
Data collection
Participants were interviewed in person by trained research assistants. In addition to the items measuring ACP behaviors, the interview included measures of sociodemographic status (age, ethnicity, race, education, sufficiency of monthly income,24 marital status, and household composition) and health status (self-rated health;25 quality of life, assessed using a single-item global measure: “How would you rate your overall quality of life?;” chronic conditions; instrumental activities of daily living;26 depression27). In the absence of available instruments in the literature, the survey also included items developed for the purposes of this study to assess participants’ life experiences with life-threatening illness and decision-making (“Have you ever had to make a medical decision for someone who was dying?”), participation in activities to prepare for the future other than ACP, and knowledge regarding advance directives. The knowledge scale consisted of 15 true-false questions addressing basic facts regarding the purpose of and mechanisms of completing health care proxies and living wills, including such items as: “If a person’s doctor believes a person should undergo a treatment, then that person needs to undergo it, even if he does not want to.” and “The best place to keep a living will is in a safety deposit box.” The full set of items is included in the Appendix.
Analysis
Univariate statistics were used to describe the study population and characterize the stages of change for the ACP behaviors. Characteristics associated with stages of change for two of the individual behaviors representing different aspects of ACP were examined in bivariate analysis using the chi-square test for categorical variables and analysis of variance for continuous variables.
RESULTS
Development of items to assess stage of change for ACP behaviors
Traditionally, the objective of ACP has been to allow patients to specify the healthcare they would want to receive in a time of decisional incapacity. A review of the literature revealed that the objective(s) of ACP have been greatly expanded. A number of objectives appeared repeatedly in commentaries reviewing the purpose of ACP. These included: a) improving communication among patients, surrogates, and clinicians;4,5,7,20,21,22,23 b) helping patients to clarify their broad goals of care;4,5,6,7,20,21,23 c) preparing patients and surrogates for the difficulties they may face at the end of life;3,6 d) decreasing family member/surrogate burden.5,7,20 There was disagreement regarding the role of ADs. While some authors argued that, because of their limitations, they should be abandoned, other authors argued that they had a continuing role.
We elected to focus on those objectives for ACP for which there were corresponding clearly identifiable and broadly applicable behaviors. The objectives of preparing patients and surrogates and decreasing burden appeared to depend upon understanding the needs of individual patients and family members and tailoring behaviors to these needs, so that these objectives were not included. We therefore focused on the objectives of clarifying patients’ goals of care, improving patient-surrogate communication, and fostering the completion of ADs. We elected to include the latter despite their controversy because our focus groups revealed that this was the aspect of ACP most familiar to older persons. We combined goals of care clarification and patient-surrogate communication into a single objective, because patients’ views regarding goals of care are a critical aspect of their communication with their surrogates. The challenge to the assessment of patients’ clarification of goals is that this is a complex task, ideally encompassing patients’ values as they relate to the acceptability of diminishing states of health, the trade-offs between the benefits and burdens of interventions, and the likelihood of different health outcomes. However, the focus groups suggested that many older persons may not be familiar with one or more of these concepts. Because the goal of this study was to assess whether patients had engaged in values clarification, rather than actually engaging patients in this process, we simplified the notion of clarification of goals to include the most fundamental concepts most likely to be familiar to a diverse group of older persons. These included whether they had considered their attitudes toward the use of life-sustaining treatment and toward the trade-offs between quality and quantity of life. The behaviors corresponding to these ACP objectives were therefore: a) completion of a living will; b) completion of a health care proxy; c) communication between patient and loved ones regarding patients’ views about the use of life-sustaining treatment; d) communication between patient and loved ones regarding patients’ views about quality versus quantity of life; e) communication between patient and clinicians regarding patients’ views about the use of life-sustaining treatment; f) communication between patient and clinicians regarding patients’ views about quality versus quantity of life.
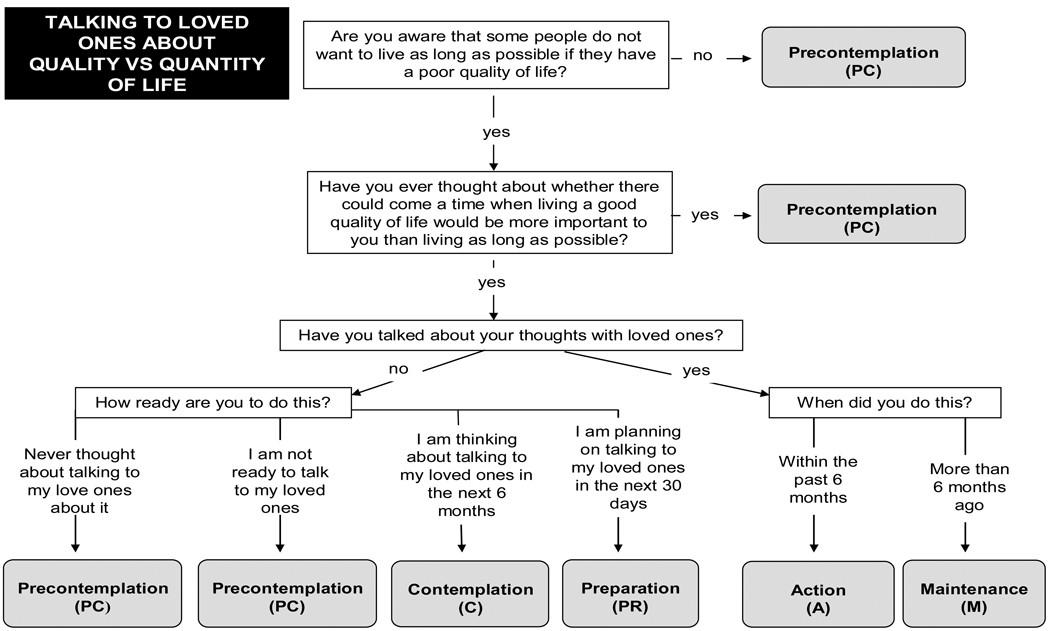
For each of these behaviors, patients were asked to choose from a fixed set of responses to indicate if they: a) had participated in the activity greater than six months ago (maintenance), b) had participated in the activity within the past six months (action), c) were planning to complete the activity within the next 30 days (preparation); d) were thinking about completing the activity in the next six months (contemplation); e) had not thought about or were not ready to participate in the activity (precontemplation). For the behaviors of communicating with loved ones and with clinicians, which represented behaviors consisting of several steps, participants could be in the precontemplation stage for a number of different reasons, including lack of awareness of life-sustaining treatments or of potential trade-offs between quantity and quality of life, never having thought about these issues, lack of readiness to talk about these issues, or having thought about these issues but lack of readiness to discuss them. Participants who indicated that they were not ready to participate in the behavior were asked about each of these reasons. The algorithm for asking about the behaviors of living will completion and communicating with loved ones about quality versus quantity of life are provided in Figure 1. The algorithms for the other behaviors followed similar logic.
Figure 1.
Staging algorithms for living will completion and communication with loved ones about quality versus quantity of life.
Description of participants and their ACP behaviors
A description of the participants is provided in Table 1. Completion of preparations for the future other than ACP ranged from 8% of participants having pre-paid for their funeral to 84% having told someone where their important papers are. The distribution of stages of change varied widely across behaviors. Whereas between approximately 50–60% of participants were in the action or maintenance stages for communicating with loved ones and completing a living will, 40% were also in the precontemplation stage for communicating with loved ones about quantity versus quality of life. Only 34% were in the action or maintenance stages for completing a health care proxy, and only 5–10% were in these stages for communicating with physicians (Table 2).
Table 1.
Description of the 304 participants
| Characteristic | Value |
|---|---|
| Age, mean years (SD) | 75 (7.1) |
| Female, % | 73 |
| Non-white ethnicity, % | 26 |
| Greater than high school education, % | 73 |
| Married, % | 46 |
| Lives alone, % | 43 |
| Chronic diseases, mean number (SD) | 3.8 (2.2) |
| ≥ 1 IADL disability, % | 20 |
| Self-rated health fair/poor, % | 22 |
| Quality of life fair/poor, % | 17 |
| AD knowledge, % correct, median (IQR)* | 73 (60, 87) |
| Preparations for the future, % | |
| Move to location with more help | 23 |
| Teach someone to do things around house | 26 |
| Long-term care insurance | 24 |
| Told someone location important papers | 84 |
| Prepared will | 70 |
| Prepared funeral arrangements | 48 |
| Pre-paid funeral | 8 |
| Purchased cemetery plot/cremation | 49 |
| Preparations, mean number (SD) | 3.3 (1.6) |
IADL = instrumental activities of daily living AD = advance directives IQR = interquartile range
AD knowledge assessed with 15 true-false questions. See Appendix for the questions.
Table 2.
Proportion of Participants at Each Stage of Change for ACP behaviors
| PC | C | PR | A/M | |
|---|---|---|---|---|
| N (%)* |
||||
| Completing a living will | 79 (26) | 55 (18) | 15 (5) | 155 (51) |
| Completing a health care proxy | 110 (36) | 62 (20) | 26 (9) | 104 (34) |
| Communicating with loved ones about life-sustaining treatment | 78 (26) | 26 (9) | 15 (5) | 180 (59) |
| Communicating with clinicians about life-sustaining treatment | 208 (68) | 47 (15) | 13 (4) | 29 (10) |
| Communicating with loved ones about quality versus quantity of life | 122 (40) | 30 (10) | 8 (3) | 143 (47) |
| Communicating with clinicians about quality versus quantity of life | 225 (74) | 53 (17) | 5 (2) | 16 (5) |
PC = pre-contemplation; C = contemplation; PR = preparation; A = action; M = maintenance
Percentages do not add up to 100% due to missing data.
We compared individual participants’ stage of change for each of two behaviors. This revealed that participants were frequently in different stages for different behaviors. For example, even when action and maintenance stages were combined, 45% of participants were in a different stage for completing a living will as compared to communicating with loved ones about quality versus quantity of life, and 51% of participants were in a different stage for completing a health care proxy as compared to communicating with loved ones about life-sustaining treatment. There was no consistent ordering when participants were in different stages for a given behavior. For example, whereas 25% of participants were in a later stage for communication with loved ones about life-sustaining treatment as compared to living will completion, 16% were in an earlier stage. The only exception was for the behaviors of completing a living will and a health care proxy; of the participants completing a living will, all but one had also completed a health care proxy.
When factors associated with stages of change for completing a living will were examined, being non-white and never having made a medical decision for someone who was dying were associated with being in earlier stages of readiness, although the latter failed to reach statistical significance (Table 3). Those who were in later stages had greater knowledge regarding living wills and advance directives compared to participants in earlier stages, and they had participated in a greater number of other preparations for the future. Age, gender, education, and health status were not associated with stage of readiness for living will completion in this community-dwelling population. In contrast, when factors associated with stages of change for communication with loved ones regarding quality versus quantity of life, all of these factors were associated with stage of readiness, as was having had to make a medical decision for someone who was dying (Table 4).
Table 3.
Factors Associated with Living Will Completion
| PC | C | PR | A/M | ||
|---|---|---|---|---|---|
| Percent | P-value | ||||
| Ethnicity | <.001 | ||||
| White | 21 | 17 | 3 | 60 | |
| Non-white | 41 | 21 | 11 | 26 | |
| Made a medical decision | .07 | ||||
| Yes | 21 | 13 | 7 | 59 | |
| No | 29 | 21 | 4 | 46 | |
| AD Knowledge* | 58 | 67 | 64 | 77 | <.001 |
| Preparation for the future† | 2.5 | 2.9 | 3.1 | 3.9 | <.001 |
PC = pre-contemplation; C = contemplation; PR = preparation; A = action; M = maintenance; AD = advance directive
AD knowledge assessed with 15 true-false questions. Results reported as % of items answered correctly.
Count of activities other than advance care planning participant had completed to plan for the future, as listed in Table 1.
Table 4.
Factors Associated With Communication With Loved Ones Regarding Quality Versus Quantity Of Life
| PC | C | PR | A/M | ||
|---|---|---|---|---|---|
| Percent | P-value | ||||
| Age | .02 | ||||
| 65–74 | 31 | 12 | 3 | 54 | |
| 75–84 | 50 | 8 | 3 | 39 | |
| 85+ | 55 | 5 | 0 | 40 | |
| Gender | .05 | ||||
| Male | 35 | 5 | 5 | 55 | |
| Female | 42 | 12 | 2 | 44 | |
| Ethnicity | <.001 | ||||
| White | 34 | 10 | 2 | 54 | |
| Non-white | 59 | 10 | 4 | 27u | |
| Marital status | .002 | ||||
| Married | 30 | 9 | 2 | 59 | |
| Other | 49 | 11 | 3 | 37 | |
| Education | <.001 | ||||
| High school or less | 58 | 8 | 4 | 30 | |
| More than high school | 29 | 11 | 2 | 58 | |
| Self-rated health | .05 | ||||
| Excellent/VG/Good | 37 | 11 | 3 | 49 | |
| Fair/Poor | 54 | 6 | 0 | 40 | |
| Made a medical decision | .001 | ||||
| Yes | 29 | 8 | 6 | 58 | |
| No | 47 | 11 | 1 | 41 | |
| AD Knowledge* | 61 | 70 | 60 | 77 | <.001 |
| Preparation for the future† | 2.9 | 3.3 | 2.1 | 3.7 | <.001 |
PC = pre-contemplation; C = contemplation; PR = preparation; A = action; M = maintenance; AD = advance directive
AD knowledge assessed with 15 true-false questions. Results reported as % of items answered correctly.
Count of activities other than advance care planning participant had completed to plan for the future, as listed in Table 1.
DISCUSSION
Conceptualizing ACP as a set of inter-related health behaviors provides a foundation for model-based health behavior change intervention development. Current thinking about advance care planning reveals it to be composed of behaviors including clarification of values; communication among patients, surrogates, and clinicians; and completion of written directives. In this cohort of older community-dwelling persons recruited from physician offices and senior centers, there was a full spectrum of readiness to participate, or stages of change, for each of these behaviors. Stages of change varied widely across the behaviors, and individual participants were frequently in different stages of readiness for the different behaviors, without evidence of ordering or sequential completion. Only a small proportion of participants had communicated with their physicians regarding their values and preferences. Relatively few sociodemographic, health, or psychosocial factors were associated with stages of change for completing a living will, but a broader range of factors was associated with stages of change for communication with loved ones about values.
The proportion of older persons in this study who were in the action/maintenance stage for living will completion and health care proxy designation was substantially higher than the proportion reported to have completed advance directives (living will and/or durable power of attorney for health care) in the control groups of multiple randomized controlled trials.9 However, in a representative national sample of family members of people who had died, the rate of advance directive completion among the decedents was 71%,28 and a second recent study utilizing a national sample found, in a national sample of adults 60 years of age or older found that, among decedents who required decision making at the end of life but lacked decision-making capacity, 68% had an advance directive.29 Although it is possible that these directives were completed close to death, which would then account for the high prevalence of directives, several studies, including the present one, have failed to find an association between severity of illness and advance directive completion. It is therefore unclear what accounts for the disparate range of completion rates across these studies.
The additional behaviors related to communication examined in this study have only recently been a separately measured part of the advance care planning process and, therefore, little is known about the prevalence of participation in them. Given the sizeable proportion of participants in the later stages of behavior change for the majority of behaviors, the large number of participants in the precontemplation stage for communication with their physicians was striking. These findings are consistent with several other studies demonstrating low rates of communication between patients with individual diseases and physicians regarding end-of-life care and multiple barriers to this communication.30, 31 These low rates highlight the lost opportunity in the portion of the (now defunct) House of Representative’s health care reform bill that would have provided incentives for promoting patient-physician communication.32 However, the fact that participants were in the earliest stage of readiness for this communication suggests that physician incentives may be insufficient to address these low rates. Intervention efforts to increase rates of communication will also need to focus on the most fundamental aspects of this behavior from the patient’s perspective, including addressing older persons’ awareness of the need for and increasing their awareness of the positive aspects of this communication.
One previous study found ACP to consist of a series of sequential steps, in which individuals were most likely to have thought about their wishes regarding life-sustaining treatment, with a sizeable subset moving on to discuss their wishes with family members and smaller subsets discussing their wishes with physicians and documenting their wishes in an AD.19 The results of the current study, in contrast, suggest that communication with loved ones about values and advance directive completion are not sequential activities, but are rather behaviors for which individuals may be in any combination of readiness to participate or stage of change. Such a model of ACP is supported by studies demonstrating that there are different sets of both barriers to and facilitators of participation in the different behaviors.10, 11 This model of ACP suggests that interventions designed to promote ACP need to assess and target stage of change for each of the behaviors individually. It also supports the feasibility of stage-tailored interventions. To the extent that facilitators of behavior change are also shared across behaviors, it may be possible to build upon the motivations an individual has for completing one aspect of ACP to support their participation in those remaining.
The associations between patient characteristics and stages of change for the different ACP behaviors both provide external validation for the measures and provide new insights into ACP as a health behavior. In the current study, non-white ethnicity was strongly associated with stages of change for living will completion, similar to the findings in a number of previous studies examining the dichotomous outcome of having versus not having a living will.33–35 The current study extends these findings by demonstrating that non-white participants were not only more likely not to have completed a living will but also more likely to be in the earliest stages of readiness to participate in the process. The current study failed to find an association between health status, measured in terms of both self-rated health and number of comorbid conditions, and stage of change for AD completion. This lack of association between health and ADs has also been previously demonstrated.36, 37 Much less is known about factors associated with other aspects of ACP. The results of the current study demonstrate that, as compared to living will completion, communication with loved ones about values regarding quantity versus quality of life is associated with a broader range of an individual’s health and psychosocial characteristics. It is also associated with their experiences with their own and with others’ serious illness. The association between stage of change and knowledge regarding ADs supports the notion that participants use certain processes of change, including gathering information, to move through the stages of readiness.11
Both living will completion and communication were associated with individuals’ participation in other, non-health-related, activities related to end-of-life preparation. This finding suggests that the predisposition to participate in ACP is, at least in part, related to the importance placed on and willingness to plan for the end of life. It also suggests the potential utility of approaches to promote ACP based on bringing together ACP with other advance planning activities outside of the medical realm. For example, older persons cite their lawyers as a source of information regarding and prompt for completing advance directives,38 suggesting that certain components of ACP might be promoted as part of estate planning. Although not routinely done, the results raise the possibility of incorporating ACP as a part of funeral planning or purchasing of long-term care insurance, which represent times at which individuals may be more receptive to the difficult task of thinking about the healthcare they wish to receive or forgo at the end of life.
The study has a number of limitations. First, because of the many models that exist for ACP, there is likely to be disagreement regarding the precise set of behaviors that define the process of ACP. Until there are more data examining the relationship between these behaviors and improved patient outcomes, determining which behaviors should be included as part of ACP will be the subject of debate. The behaviors utilized in this study were not meant to be definitive; rather, they were chosen as a set that appeared to be representative of the existing literature. Second, we assessed participants’ engagement in these behaviors in a simplified fashion. In order to ensure that participants would understand what was meant by a consideration of goals, we asked them about only the most fundamental aspects of this process, thereby potentially overestimating their engagement in these behaviors. Third, although we included participants regardless of their health status in order to examine participation in ACP among a broad cross-section of older persons, it could be argued that it is most relevant to examine ACP engagement among persons who are at greater risk of decisional incapacity. Finally, the study was restricted to ACP as it pertained to treatment decision-making for physical, and not mental, health.
ACP can be conceptualized as a group of related health care behaviors. This study demonstrates the variability in readiness to participate, or stages of change, for these different behaviors, among a cohort of older, community-living persons. It also illustrates that these persons are frequently in different stages for the different behaviors. Individualized assessment and interventions targeted to the stage of behavior change for each component of ACP may be an effective strategy to increase older persons’ participation in ACP.
ACKNOWLEDGMENTS
Supported by grants R01 AG19769 and K24 AG28443 from the National Institute on Aging and the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG21342 NIH/NIA).
Sponsors’ role: The sponsors had no role in the design, methods, subject recruitment, data collection, or analysis and preparation of the paper.
APPENDIX: Advance Directive Knowledge Items
I have the right to refuse a medical treatment, even if that treatment might keep me alive longer.
If my doctor believes I should undergo a treatment, then I need to undergo it, even if I do not want to.
A living will is a document saying I would not want to be kept alive on machines if I was in a terminal state or permanently unconscious.
A living will is a document saying I would not want to be kept alive on machines if I was a burden on my loved ones.
A living will is a document saying I would not want to be kept alive on machines if I had a poor quality of life.
If I have filled out a will to say how I want my property divided, I do not have to complete a living will.
A health care proxy or representative is someone who would make medical decisions on my behalf if I were not able to make my own decisions.
A health care proxy or representative is someone who would make medical decisions on my behalf even if I were able to make my own decisions.
A person named as my power of attorney is someone who could make any medical decision on my behalf if I were not able to make my own decisions.
A living will is legal only if it is drawn up by a lawyer.
A health care proxy or representative is legal only if it is drawn up by a lawyer.
Once I signed a living will, I could not change my mind about how I would want to be treated.
Once I named a health care proxy or representative, I could not change my mind and name someone else.
The best place to keep a living will is in a safety deposit box.
My doctor would not need a copy of my living will.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions:
Study concept and design: TRF, CR, MR
Acquisition of subjects and data: TRF, JRO, LI
Analysis and interpretation of data: TRF, CR. MR, AP, JRO, LI
Preparation of manuscript: TRF
Editing of manuscript: CR, MR, AP, JRO, LI
REFERENCES
- 1.Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep. 2004;34:30–42. [PubMed] [Google Scholar]
- 2.Lynn J. Why I don't have a living will. Law Med Health Care. 1991;19:101–104. doi: 10.1111/j.1748-720x.1991.tb01803.x. [DOI] [PubMed] [Google Scholar]
- 3.Perkins HS. Controlling death: The false promise of advance directives. Ann Intern Med. 2007;147:51–57. doi: 10.7326/0003-4819-147-1-200707030-00008. [DOI] [PubMed] [Google Scholar]
- 4.Brett AS. Limitations of listing specific medical interventions in advance directives. JAMA. 1991;266:825–828. [PubMed] [Google Scholar]
- 5.Kolarik RC, Arnold RM, Fischer GS, et al. Objectives for advance care planning. J Pall Med. 2002;5:697–704. doi: 10.1089/109662102320880516. [DOI] [PubMed] [Google Scholar]
- 6.Gillick MR. A broader role for advance medical planning. Ann Intern Med. 1995;123:621–624. doi: 10.7326/0003-4819-123-8-199510150-00009. [DOI] [PubMed] [Google Scholar]
- 7.Hammes BJ. What does it take to help adults successfully plan for future medical decisions? J Palliat Med. 2001;4:453–456. doi: 10.1089/109662101753381584. [DOI] [PubMed] [Google Scholar]
- 8.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: What do we need for success? J Am Geriatr Soc. 2007;55:277–283. doi: 10.1111/j.1532-5415.2007.01065.x. [DOI] [PubMed] [Google Scholar]
- 9.Bravo G, Dubois M-F, Wagneur B. Assessing the effectiveness of interventions to promote advance directives among older adults: A systematic review and multi-level analysis. Soc Sci Med. 2008;67:1122. doi: 10.1016/j.socscimed.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Schickedanz AD, Schillinger D, Landefeld CS, et al. A clinical framework for improving the advance care planning process: Start with patients' self-identified barriers. J Am Geriatr Soc. 2009;57:31–39. doi: 10.1111/j.1532-5415.2008.02093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fried TR, Bullock K, Iannone L, et al. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc. 2009;57:1547–1555. doi: 10.1111/j.1532-5415.2009.02396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prochaska JO, Redding CA, Evers KE. The Transtheoretical Model and Stages of Change. In: Glanz K, Rimer BK, Viswanath KV, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4th edition. San Francisco: Jossey-Bass; 2008. pp. 170–222. [Google Scholar]
- 13.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 14.Pearlman RA, Cole WG, Patrick DL, et al. Advance care planning: Eliciting patient preferences for life-sustaining treatment. Patient Educ Couns. 1995;26:353–361. doi: 10.1016/0738-3991(95)00739-m. [DOI] [PubMed] [Google Scholar]
- 15.Pearlman RA, Starks H, Cain KC, et al. Improvements in advance care planning in the Veterans Affairs System: Results of a multifaceted intervention. Arch Intern Med. 2005;165:667–674. doi: 10.1001/archinte.165.6.667. [DOI] [PubMed] [Google Scholar]
- 16.Medvene LJ, Base M, Patrick R, et al. Advance directives: Assessing stage of change and decisional balance in a community-based educational program. J Appl Soc Psychol. 2007;37:2298–2318. [Google Scholar]
- 17.Jezewski MA, Finnell DS, Wu YW, et al. Psychometric testing of four transtheoretical model questionnaires for the behavior, completing health care proxies. Res Nurs Health. 2009;32:606–620. doi: 10.1002/nur.20352. [DOI] [PubMed] [Google Scholar]
- 18. [Accessed September 3, 2009];REAP: Readiness to engage in advance care planning. http://www.promotingexcellence.org/i4a/pages/Index.cfm?pageID=3836.
- 19.Sudore RL, Schickedanz AD, Landefeld CS, et al. Engagement in multiple steps of the advance care planning process: A descriptive study of diverse older adults. J Am Geriatr Soc. 2008;56:1006–1013. doi: 10.1111/j.1532-5415.2008.01701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Winzelberg GS, Hanson LC, Tulsky JA. Beyond autonomy: Diversifying end-of-life decision-making approaches to serve patients and families. J Am Geriatr Soc. 2005;53:1046–1050. doi: 10.1111/j.1532-5415.2005.53317.x. [DOI] [PubMed] [Google Scholar]
- 21.Hammes BJ. Update on Respecting Choices four years on. Innovations in End-of-Life Care. 2003;5 www.edc.org/lastacts.
- 22.Lo B, Steinbrook R. Resuscitating advance directives. Arch Intern Med. 2004;164:1501–1506. doi: 10.1001/archinte.164.14.1501. [DOI] [PubMed] [Google Scholar]
- 23.Loewy EH. Ethical considerations in executing and implementing advance directives. Arch Intern Med. 1998;158:321–324. doi: 10.1001/archinte.158.4.321. [DOI] [PubMed] [Google Scholar]
- 24.Pearlin LI, Lieberman MA, Menaghan EG, et al. The stress process. J Health Soc Behav. 1981;22:337–356. [PubMed] [Google Scholar]
- 25.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 26.Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 27.Whooley MA, Avins AL, Miranda J, et al. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teno JM, Gruneir A, Schwartz Z, et al. Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc. 2007;55:189–194. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]
- 29.Silveira MJ, Kim SYH, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362:1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curtis JR, Patrick DL, Caldwell ES, et al. Why don't patients and physicians talk about end-of-life care? Barriers to communication for patients with acquired immunodeficiency syndrome and their primary care clinicians. Arch Intern Med. 2000;160:1690–1696. doi: 10.1001/archinte.160.11.1690. [DOI] [PubMed] [Google Scholar]
- 31.Knauft E, Nielsen EL, Engelberg RA, et al. Barriers and facilitators to end-of-life care communication for patients with COPD. Chest. 2005;127:2188–2196. doi: 10.1378/chest.127.6.2188. [DOI] [PubMed] [Google Scholar]
- 32.America’s Affordable Health Choices Act of 2009 as introduced. 2009 [Google Scholar]
- 33.Baker ME. Economic, political and ethnic influences on end-of-life decision-making: a decade in review. J Health Soc Policy. 2002;14:27–39. doi: 10.1300/J045v14n03_02. [DOI] [PubMed] [Google Scholar]
- 34.Bullock K. Promoting advance directives among African Americans: A faith-based model. J Palliat Med. 2006;9:183–195. doi: 10.1089/jpm.2006.9.183. [DOI] [PubMed] [Google Scholar]
- 35.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc. 2008;56:1953–1958. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gordon NP, Shade SB. Advance directives are more likely among seniors asked about end-of-life care preferences. Arch Intern Med. 1999;159:701–704. doi: 10.1001/archinte.159.7.701. [DOI] [PubMed] [Google Scholar]
- 37.Freer JP, Eubanks M, Parker B, et al. Advance directives: ambulatory patients' knowledge and perspectives. Am J Med. 2006;119:1088–1089. doi: 10.1016/j.amjmed.2006.02.028. [DOI] [PubMed] [Google Scholar]
- 38.Mansell D, Kazis L, Glantz L, et al. Roles of physicians, attorneys, and illness experience in advance directives. South Med . 1999;92:197–203. doi: 10.1097/00007611-199902000-00007. [DOI] [PubMed] [Google Scholar]