Abstract
Evidence of the effects of negative affect (NA) and sexual craving on unprotected sexual activity remains scant. We hypothesized that NA and sexual craving modify the same day association between low self-efficacy to use condoms and unprotected anal or vaginal sex, and the same-day association between alcohol use during the 3 hours prior to sexual activity and unprotected sex. We used an electronic daily diary, drawing on a sample of 125 men and women recruited from an agency serving economically disadvantaged persons living with HIV/AIDS. Casual or steady partner type designation and perceived partner HIV serostatus were also examined. Findings support the hypothesized moderating effects of high NA and sexual craving on the association between low self-efficacy and unprotected sex, and the association between alcohol use and unprotected sex. Implications are discussed.
Most people who live with HIV/AIDS are motivated to avoid infecting others with HIV; they are more likely to be inconsistent condom users rather than consistent non-users (Crepaz & Marks, 2002; Kalichman, 2000). Even when both partners in a sexual relationship are living with HIV/AIDS, condom use is strongly advocated by public health professionals given the danger of infection by a strain of HIV that is resistant to antiretroviral medications used to suppress HIV (Templeton et al., 2009), or infection with other sexually transmitted infections (Anzala et al., 2000).
Researchers have speculated that acute emotional distress contributes to inconsistent condom use (Canin, Dolcini, & Adler, 1999). People living with HIV/AIDS face profound day-to-day stress and anxiety (Schmitz & Crystal, 2000) and exhibit twice the prevalence of depression than what is observed in the general population (Ciesla & Roberts, 2001). Yet, this remains a matter of debate. Crepaz and Marks (2001) concluded, based on a meta-analysis of 34 pertinent studies, that there is little evidence to support the view that negative affective states are associated with unprotected sexual activity.
Conventional cross-sectional and longitudinal designs cannot capture acute emotional states in a way that allows investigators to examine the temporal link between these states and risky sexual episodes. Negative affect (NA), the self-reported experience of worry, anger, or other aversive hedonic states, is subject to intra-individual fluctuation (Diener & Emmons, 1984). As Kalichman and Weinhardt (2001) note, global assessments of affect that are used in cross-sectional and most longitudinal studies, “are insensitive to the co-occurrence of emotion and sexual events; negative affect that immediately precedes sexual decisions may be associated with risk practices, and these associations may only be observable at the event level (p. 301).”
If, as Kalichman and Weinhardt and others theorize, high NA is related to risk-taking behavior, one cannot assume that the relationship will manifest similarly across diverse contexts. The literature suggests that high NA is associated with increased risk-taking with respect to behaviors associated with mood enhancement, such as alcohol use and sexual activity (Cooper, Wood, Orcutt, & Albino, 2003). However, the literature also suggests that high NA is associated with risk-avoidant behavior in situations in which performance- or evaluation-related concerns are salient (Canin et al., 1999; Scott & Cervone, 2002).
Sexual Craving
Individuals who report a desire to counteract NA as a motive for having sex are more likely than others to engage in unprotected sex and more likely to report sex involving risky partners (Cooper, Shapiro, & Powers, 1998). One may infer, then, that momentary increases in NA will sometimes coincide with increased frequency and intensity of thoughts about sex (sexual craving). Sexual craving may also potentiate the association between high NA and desire to experience the mood enhancing effects of sexual activity.
Self-Efficacy
Self-efficacy is defined as confidence in one’s ability to engage in a skilled or effortful task (Bandura, 1997). Condom use self-efficacy is an established correlate of condom use behavior (Lescano, Brown, Miller, & Puster, 2007; St. Lawrence, Brasfield, Jefferson, & Alleyne, 1995). Past research using diary methods has shown that, on days when individuals report higher than their own average levels of NA, they are also more likely to report lower self-efficacy to use condoms (Kiene, Barta, Tennen, & Armeli, 2009). However, these data did not reveal a moderating effect of NA on the association between self-efficacy and unprotected sexual activity. High NA is thought to stimulate increased self-critical and exacting performance standards, thereby undermining perceived self-efficacy (Scott & Cervone, 2002).
Alcohol Use
Cooper (2006) noted that, although most cross-sectional studies find an association between alcohol use and unsafe sexual behavior, “owing to design limitations, these studies tell us little about the underlying causal relationship. Such data cannot even establish a temporal link between drinking and risky sex, a minimum condition for attributing causality to acute alcohol effects (p. 19).” A potential “third-variable” explanation for the link between drinking and unsafe sex is the propensity to engage in both alcohol use and unsafe sex as part of an effort to avoid negative emotions (Cooper et al., 2003). Cooper et al. found evidence of a longitudinal association between avoidant coping style and both drinking and unsafe sex. Their data consisted of measures collected at two time points 4.5 years apart.
To further substantiate causal inferences, one may consider whether a same-day association exists between NA and alcohol use. To this end, Mohr, Armeli, Tennen, Carney, Affleck, and Hromi (2001) conducted a diary study of alcohol users and found that on days in which relatively high NA was reported, alcohol use was greater as compared to other days.
With regard to sexually risky behavior, diary data have been inconsistent. Some studies have failed to find an association between alcohol use and unprotected sex (Leigh, Vanslyke, Hoppe, Rainey, Morrison & Gillmore, 2008). Other studies, such as Kiene et al.’s (2009) study of college students, have revealed a same-day association between alcohol use and unprotected sex with casual partners. In comparing these studies, a possible explanation is the discrepancy in the size of the sample of instances of sexual activity involving casual partners. Only 17% of sex acts (73 instances) documented in Leigh et al.’s study involved casual partners, as compared to 30% (160 instances) in Kiene et al.’s study.
Partner Type and HIV Status
Studies of people who do not self-identify as HIV-positive show that acute alcohol use increases the risk of unprotected sex with casual partners but not sex involving “steady” or committed partners (Kiene, et al., 2009; Vanable, McKirnan, Buchbinder, Bartholomew, Douglas, Judson, & MacQueen, 2004; Weinhardt & Carey, 2000). Alcohol is present at social venues and occasions where sex partners initially meet and socialize (Weinhardt & Carey, 2000). As the relationship becomes more established, alcohol use is less likely to factor in risk-related decision-making owing to the fact that people in steady relationships have, in many cases, arrived at a decision to discontinue condom use (c.f., Vanable et al., 2004). Indeed, discontinuation of condom use, for many couples, is a valued expression of trust and intimacy (Corbett, Dickson-Gomez, Hilario, & Weeks, 2009).
A quite different pattern may arise among people living with HIV/AIDS. Unprotected sex is more frequent with casual as compared to steady partners (Folch, Marks, Esteve, Zaragoza, Muñoz, & Casabona, 2006; Van Kesteren, Hospers, & Kok, 2007), particularly when the partner is perceived to be HIV-positive, and the sex act is preceded by alcohol use (Barta, Portnoy, Kiene, Tennen, Abu-Hasaballah, & Ferrer, 2008). In sexual relationships between HIV serodiscordant couples, unprotected sex may thus be less frequent in a steady relationship as compared to a casual relationship (Barta et al., 2008; Simoni, Walters, & Nero, 2000).
Contingent Relationships among Predictors
The event-level analysis of determinants of unsafe sex described here reflects a “person-oriented” rather than “variable-oriented” approach (c.f. Von Eye, Bogat, & Rhodes, 2006). That is, the goal is not to establish whether a global association exists between (for example) low self-efficacy and increased unsafe sex, but to instead examine intra-individual variation in the effects of multiple predictors bearing on the predicted probability of unsafe sex, i.e., to examine contingent relationships.
To illustrate the approach, even though there is evidence that low self-efficacy is related to unsafe sex, one may envision occasions during which a person with low self-efficacy uses condoms during sex, and occasions during which a person with high self-efficacy nonetheless engages in unsafe sex. The contingent factor in this example may be sexual partner type. The presence of contingent relationships, Von Eye et al. suggest, may help explain why event-level data and aggregate cross-sectional data are sometimes discrepant. In a study of female injection drug users living with HIV/AIDS, self-efficacy more strongly predicted unsafe sex with serodiscordant partners when partners were described as “casual” as opposed to “steady” (Latka, Metsch, Mizuno, Tobin, Mackenzie, et al. 2006). But among men living with HIV/AIDS, self-efficacy was associated with unprotected sex regardless of partner type or perceived partner serostatus (Purcell, Mizuno, Metsch, Garfein, Tobin, Knight, & Latka, 2006).
The Present Study
The present study examines the hypothesis that NA and sexual craving provide a context in which event-level associations between self-efficacy and unprotected sex acts occur, such that associations between low self-efficacy and increased sexual risk behavior differ depending on contemporaneous levels of NA and sexual craving. Alcohol use during the hours prior to sexual activity is viewed as an independent predictor of unprotected sexual activity, again in the context of varying levels of NA. Separate analyses focus on samples of sex acts involving “casual” and “steady” partners, and take into consideration the potential modifying effect of perceived partner HIV status.
Methods
Participants
Following Institutional Review Board approval, HIV seropositive participants were recruited at a community-based organization serving people living with HIV/AIDS. They were made aware of the study by means of referral. A brief eligibility interview was conducted to confirm whether participants were sexually active (defined as any sexual activity in the last 6 weeks), inconsistent condom users (defined as affirmative responses to questions tapping “any condom use” and “any instance of not using condoms” in the 6 month period prior to the study), and alcohol users (defined as any alcohol use in the last 4 weeks). HIV status was verified by inspection of test results or prescriptions for antiretroviral medications. Participants were provided with monetary incentives.
Of the participants included in the analyses, 57.4% were men and 42.6% women; 62% of participants self-identified as African American, 32.7% as “White,” and 4.8% as either Native American or Asian/Pacific Islander; 42% also self-identified as Latino or Latina. The average age reported by participants was 46, and ranged from 25 to 65 years of age. In terms of sexual orientation, 70% reported engaging exclusively in sexual activity with people of the opposite sex, 19.0% reported engaging exclusively in sexual activity with people of the same sex, and 11% reported engaging in sexual activity with people of both sexes.
Materials
Diary data was provided by participants through an Interactive Voice Response system (IVRS), a telephone-based technology that delivers questions by means of voice recording, and collects responses by means of touch-tone responses entered by participants. A toll-free number was provided to access this system, and on accessing the system, participants could choose either an English or Spanish version. The data collection system only accepted calls between the hours of 3:00 and 6:00 pm. This restriction was imposed to minimize the potential for overlapping responses to questions referring, for example, to the “last 24 hours.” Participants were asked to provide a unique ID number that was provided during training, and this ID was programmed into the IVR to ensure user authentication. Each diary entry required about 10 minutes. Participants were asked to continue completing these calls once a day for 35 continuous days.
Measures and Procedures
Prior to completing diary entries, participants completed baseline measures, including demographic information and personal history data such as age, gender, ethnicity, socio-economic status, and self-reported frequency of sexual activity during the six weeks prior to enrolling in the study. After completing these measures, participants were trained to use of the IVRS. Each participant was also issued a booklet containing the complete set of questions and response options administered by the IVRS.
Daily diary items were prefaced by stems such as “last night, from the time you completed the diary until you went to sleep,” or “today, since you woke up this morning” to assess approximate temporal sequence. Alcohol use and sexual activity were assessed for the period “last night,” anticipated self-efficacy for the period “in the next 24 hours” (and lagged so that self-efficacy “in the next 24 hours” overlapped with events reported for the period “last night”), sexual craving for the period “today,” and NA for the period “in the last two or three hours.” Additional questions, contingent on participants reporting alcohol use or sexual activity, were included to establish the recalled time of these behaviors within 1 hour of their occurrence; that is, for an event that occurred between 8:00 and 9:00 pm, participants were asked to enter the number “8” and to select the second option in response to the question “am or pm?”
Alcohol Use
During the training session, participants were familiarized with standard drink units – that is, the typical alcohol content of a 12 ounce can of beer as compared to, say, a 5 ounce glass of wine – and the booklet received by participants contained a chart providing standard drink conversions. These steps were intended to sensitize participants to the value placed on providing careful estimates. However, when completing the daily diary, participants were asked to report how many drinks they had consumed for the time period “last night” based on familiar beverages. These included 40 ounce bottles of malt liquor, with response options ranging from 1 (about one third of a bottle or less) to 5 (more than a full bottle); 12 ounce cans or bottles of beer, with an “open” response format (“how many 12 ounce cans or bottles of beer did you drink last night?”) followed by the instruction to enter the number of cans or bottles; drinks of wine, based on 5 ounce servings, followed by an open response format; and drinks of hard liquor, based on a 1.5 ounce “shot,” with an open response format.
Sexual Activity
Participants were asked to report the number of occasions in which they engaged in anal or vaginal sex for the period “last night” and the number of each of these occasions in which they used a condom “from start to finish” (for as long as there is penile contact culminating in orgasm and/or loss of erection). In these analyses, unsafe sex was defined as the difference between total and protected self-reported vaginal and anal sex acts on a given day. For each reported occasion of sexual activity, participants were asked “did this sex partner ever tell you that he or she was HIV positive?” If the response was “yes,” the variable was coded as 1; for HIV-negative partners and partners of unknown serostatus, the response was coded as 0. This dichotomous coding of “HIV-negative or unknown serostatus” is consistent with other HIV prevention research (e.g., Folch et al., 2006).
Participants were also asked to rate level of partner involvement, selecting among casual (“someone you just met”), ongoing (“someone other than your steady partner that you have sex with”) and steady (“steady partner like a boyfriend, girlfriend, husband or wife”). Members of the target community are fairly consistent in their distinction between the level of emotional intimacy and trust felt in a “casual” versus a “steady” relationship. However, there is greater variability in the degree of emotional intimacy felt toward “ongoing” partners (Singer et al., 2006). Therefore, analyses will focus on the two more reliably distinctive categories of “casual” and “steady.”
Alcohol-Involved Sexual Activity
The self-reported end-time of alcohol consumption was compared with the start-time of sexual activity. Acute alcohol use prior to sexual activity was inferred if the start- or end-time of the drinking episode fell within 3 hours prior to the reported time of onset of sexual activity. Estimated number of drinks prior to sex is based on reported number of drinks consumed divided by the total number of reported hours spent drinking.
Sexual Craving
Investigators have operationalized craving as the frequency and intensity of consummatory thoughts in a fixed time period (c.f. Eliason & Amodia, 2007, for a review). Following their example, a summed 2-item daily measure of sexual craving was developed for this study. The items, “today, how much did you think about sex?” and “today, did you feel like you really needed sex?” were scored on a “not at all” (0) to “a lot” (3) scale. Cronbach’s reliabilities, assessed on days 7, 14, 21, Day 28, were .82, .72, .81, and .85 respectively.
Anticipated Self-Efficacy to Use Condoms
A 2-item measure of self-efficacy, arrayed from “very hard” (1) to “very easy” (5) was also included. Self-efficacy was coded as “low” (below the participant’s mean value by less than half a standard deviation) or “very low” (below the participant’s mean value by at least a half a standard deviation). The stem used for self-efficacy items was “In the next 24 hours.” This was meant to tap participant’s self-predictions regarding the following day, and the items consisted of “If you were to have sex in the next 24 hours, how hard or easy would it be for you to use a condom with your partner?” and “If you were to have sex in the next 24 hours, how hard or easy would it be for you to avoid having sex with your partner if he/she did not want to use a condom?” Lagging this variable enabled us to match self-efficacy “for the next 24 hours” with sex acts reported for the period “last night.” Cronbach’s reliabilities assessed on days 7, 14, 21 and 28, were .58, .68, .74, and .71 respectively.
Negative Affect (NA)
A 3-item measure was used, consisting of adjective-based measures of moods and based on Diener and Emmon’s (1984) 5-item measure. Because affective states may change throughout the course of a day and are poorly remembered (Robinson & Clore, 2002), the participants were asked to describe NA for the period described as “the last two or three hours.” Negative affect items consisted of “sad,” “nervous or worried,” and “angry.” Response options ranged from “not at all” (0) to “very” (3). Cronbach’s reliabilities for the measure, assessed on Day 7, 14, 21 and 28, were .62, .73, .81, and .79 respectively.
Results
Missing Data
Data were obtained from 140 participants. Missing data resulted in the case-wise elimination of 15 participants. In the reduced sample, 125 participants provide a total of 2812 diary entries out of a possible total of 4375 (that is, 35 days x 125), i.e., 64% adherence to the diary protocol. A simple and standard imputation method taking the mean of the entries before and after the missing entry was employed when isolated instances of missing data occurred (Engels & Diehr, 2003). Imputation of data is justified on the basis that daily variables such as NA exhibit moderate day-to-day autocorrelation (Moberly & Watkins, 2008).
Analytic Strategy
Multilevel (random coefficient hierarchical regression) models, sometimes referred to as hierarchical linear models, may be appropriately applied to analyzing diary entries as data points nested within participants. In this case, the outcome of unsafe sex was modeled using a Poisson distribution, showing the effects of hypothesized predictors on the probability of unsafe sex acts in a fixed time interval (in this case a day). The result -- an Event Rate Ratio (ERR) – is interpreted like an Odds Ratio relative to the value of 1. To allow for inter-individual variability in the frequency of sexual activity, an offset was included that is equal to the maximum number of discrete protected or unsafe sex acts reported on a given day; in the data reported here, the maximum number of acts is 10.
The analyses described below are based on two 3-level models. The lowest level of analysis (Level 1) is comprised of diary entries, and the Level 1 equation includes partner type designation. In the first model, “casual” partner type is contrasted with both “ongoing” and “steady” partner type. In the second model, “steady” partner type is contrasted to both “casual” and “ongoing.” The two models are otherwise identical and also include, at Level 1, self-efficacy “for the next 24 hours,” alcohol use during the 3 hours prior to sex and the interaction of low self-efficacy and alcohol use. Variables at Level 1 are theorized “day-level” determinants of the outcome (unsafe sex). In other words, partner type, daily self-efficacy and alcohol use were regarded as compositional variables that distinguish among diary entries.
At Level 2, the following variables were added as cross-level moderators of Level 1 associations: (i) perceived partner HIV status (HIV-positive vs. either HIV-negative or unknown HIV status) as a moderator of the hypothesized association between partner type and rate of unsafe sex and (ii) NA and sexual craving as moderators of the hypothesized associations between self-efficacy and alcohol use on unsafe sex. Level 2 variables represent theoretical contexts in which day-level associations manifest.
At Level 3, diary entries were grouped by the participant providing the entries, to recognize the dependency of data provided by the same individual. At this level, mean levels of NA, self-efficacy and craving refer to the average ratings assigned to these variables by each participant across diary entries. These ratings were compared to the mean values provided by other participants in the same sample.
To explicate the last point, in the daily diary literature, a distinction is made between “daily” and “mean” levels of a variable (c.f. Kiene et al., 2008; Shiffman, Balabanis, Paty, Engberg, Gwaltney et al., 2000). For example, self-efficacy may fluctuate meaningfully from one day to the next. Stable differences in the mean level of self-efficacy are also likely. Hence, “daily self-efficacy” distinguishes among days within participants, and “mean self-efficacy,” derived from the average value of self-efficacy across diary entries, distinguishes among participants.
Descriptive Findings
The means and standard deviations of the daily variables were as follows: self-efficacy (M = 3.01, SD = 1.217), NA (M = .678, SD = .791), sexual craving (M = .716, SD = .862) and alcohol use prior to self-reported sexual activity (M = 5.44 drinks; SD = 4.515). This may be compared to overall drinking activity (M = 5.85 drinks, SD = 4.84); drinking was reported in 1211 diary entries (or 42% of the total) and there were 243 instances in which sexual activity and drinking occurred on the same evening. The key variables listed here are not significantly associated with one another, based on the results of a Pearson’s correlation. Participants reported a total of 725 unsafe anal or vaginal sex acts and 380 protected acts; on average, participants reporting any sexual activity on a given evening reported an average of 2.28 discrete sex acts. A total of 241 acts (about 22%) involved a partner described as “casual.”
Model for Casual Partner Type
For ease of interpretation, two models were constructed; the first contrasts sex acts involving casual partners with acts involving either “ongoing” or “serious” partners. In the Level 1 equation, casual partner type, low self-efficacy, alcohol use, and the interaction between alcohol use and low self-efficacy were each associated with predicted probability of unsafe sex acts (Table 1). Notably, and contrary to predictions, low self-efficacy was associated with a lower probability of unsafe sex at Level 1; however, when the cross-level interactions were considered, as will be discussed, the results supported the hypothesized association between low self-efficacy and increased probability of unsafe sex.
Table 1.
A multilevel model treating “unprotected anal or vaginal sex acts” as a Poisson outcome. Variables listed at Level 2 are cross-level moderators of the effects of Level 1 variables on the outcome. Mean NA, at Level 3, controls for individual differences in the average self-reported intensity of NA across days
| Level 1 |
Level 2 |
Level 3 |
B |
t (df) |
ERR |
p value |
|---|---|---|---|---|---|---|
| 0. Intercept | −3.313 | −39.277 (121) | 0.036 | 0.000 | ||
| 1. Casual | 1.505 | 6.403 (124) | 4.505 | 0.000 | ||
| HIV+ | 0.942 | 3.738 (2812) | 2.564 | 0.000 | ||
| High NA | Mean NA | −0.863 | −2.259 (2812) | 0.422 | 0.024 | |
| 2. Low SE | −1.215 | −5.535 (123) | 0.297 | 0.000 | ||
| High NA | 0.501 | 4.067 (2812) | 1.650 | 0.000 | ||
| Craving | 0.716 | 7.040 (2812) | 2.047 | 0.000 | ||
| 3. AU | 0.167 | 2.396 (123) | 1.181 | 0.018 | ||
| 4. SE x AU | 0.239 | 2.141 (2812) | 2.141 | 0.032 |
Reliability Estimates. 0 = .188; 1 = 0.117; 2 = 0.082; 3 = 0.084; 4 = 0.171
SE=self-efficacy; AU=alcohol use
Not shown: Non-significant Level 3 effects of gender, grand mean-centered sexual craving and NA; also, non-significant Level 2 effect of sexual craving on alcohol use.
Estimation: Penalized Quasi-Likelihood.
The Level 2 equation that is linked to the variable “casual partner type” includes perceived partner serostatus and NA. The association between partner type and probability of unsafe sexual activity was greater in the case of acts involving partners perceived to be HIV-positive. Unsafe sex with casual partners was less likely among individuals who reported high NA relative to other participants and on days in which high NA was reported.
Turning to the Level 2 variables linked to low self-efficacy, on days distinguished by high NA and high sexual craving but not on other days, low self-efficacy increased the probability of unsafe sex. Neither NA nor sexual craving influenced the association between alcohol use and unsafe sex, (not included in Table 1). Lastly, as predicted, additional variability was accounted for by the interaction of low self-efficacy and alcohol use.
To reiterate, when self-efficacy was especially low on a given day – with “very low” signifying a distance of at least one half of a standard deviation from the participant’s average SE - and the individual also reported strong sexual craving and high NA, the predicted probability of unsafe sex was greater than on other days. This is illustrated in Figure 1.
Figure 1.
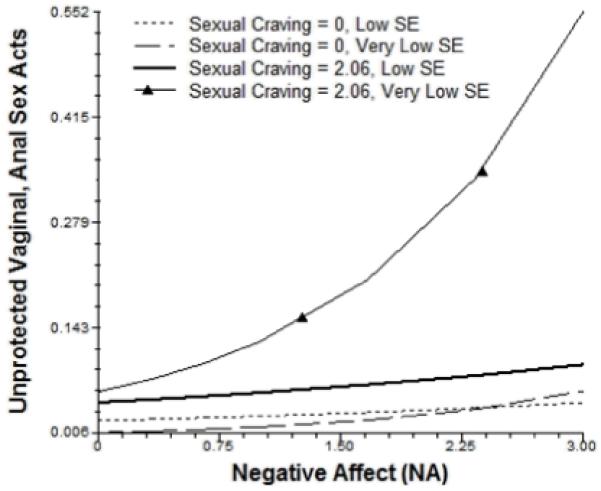
Casual Partner Type: Self-Efficacy and Sexual Craving. The effect of self-reported self-efficacy to use condoms (SE) “in the next 24 hours” on same-day frequency of unprotected anal or vaginal sex acts is most pronounced on days distinguished by both strong sexual craving and high NA. Here, the averaged upper and lower quartiles of sexual craving are shown.
Similarly, when holding craving and mean NA constant, the association between low self-efficacy and probability of unsafe sex was greater on days distinguished by high NA, and this association was stronger on days when the individual consumed alcohol prior to sexual activity (Figure 2).
Figure 2.

Casual Partner Type: Negative Affect and Alcohol Use. The effect of self-reported self-efficacy to use condoms (SE) “in the next 24 hours” on same-day frequency of unprotected anal or vaginal sex acts is most pronounced on days in which relatively strong negative affect (NA) is reported. This is particularly true on days in which participants report alcohol use in the 3 hour period prior to sexual activity.
Model for Steady Partner Type
A second model was created to examine sex acts involving steady partners (Table 2). In the Level 1 equation, steady partner type, low self-efficacy, and the interaction between alcohol use and low self-efficacy were each associated with increased probability of unsafe sex. In contrast to the model for casual partner type, alcohol use was only associated with unsafe sex on days when high NA was also reported. Individual differences in the tendency to report high NA did not affect these findings.
Table 2.
Model for steady partner type
| Level 1 |
Level 2 |
Level 3 |
B |
t (df) |
ERR |
p value |
|---|---|---|---|---|---|---|
| 0. Intercept | −3.544 | −33.303 (121) | 0.029 | 0.000 | ||
| 1. Steady | 1.851 | 10.173 (124) | 6.367 | 0.000 | ||
| High NA | Mean NA | 0.479 | 2.005 (2812) | 1.615 | 0.045 | |
| 2. Low SE | −0.984 | −4.374 (123) | 0.374 | 0.000 | ||
| High NA | 0.360 | 2.850 (2812) | 1.433 | 0.005 | ||
| Craving | 0.626 | 5.836 (2812) | 1.870 | 0.000 | ||
| 3. AU | High NA | 0.097 | 2.202 (2812) | 0.951 | 0.028 | |
| 4. SE x AU | 0.230 | 2.134 (2812) | 1.260 | 0.033 |
Reliability Estimates. 0 = .167; 1 = 0.214; 2 = 0.158; 3 = 0.109; 4 = 0.179
Apart from partner type, this model is otherwise identical to the model depicted in Table 1, depicting associations that are significant at p < .05 or lower.
SE=self-efficacy; AU=alcohol use
Not shown: Non-significant Level 3 effects of gender, grand mean-centered sexual craving and NA; also, non-significant Level 2 effect of sexual craving on alcohol use.
Estimation: Penalized Quasi-Likelihood.
Two differences emerged between this model and the model for casual partner type. First, perceived partner serostatus was not associated with unsafe sex. Second, this model showed that unsafe sex with a steady partner was more frequent on days distinguished by high NA, specifically among individuals who typically reported relatively high NA. The direction of the association was reversed in the model for casual partner type. In other respects, results for this model were similar to those found in the model for casual partner type. Low self-efficacy was associated with a greater predicted probability of unsafe sex when same-day NA and self-reported sexual craving were high.
Discussion
One purpose of this study was to examine the moderating contextual effects of sexual craving (defined as the self-reported frequency and intensity of thoughts regarding sex), and negative affective state (NA) on the association between low self-efficacy to use condoms and frequency of unsafe anal or vaginal sex acts. These variables were assessed in two separate models, one predicting sex acts with casual partners and the second predicting sex acts with steady partners. Another aim of the study was to examine the hypothesis that this complex of variables may aid in identifying the circumstances in which alcohol use prior to sex is most likely to affect the probability that the sexual activity will be unprotected. .
We found that low self-efficacy, alcohol use during the 3 hour period prior to sexual activity, and their interaction each affected the probability of unsafe vaginal or anal sex involving casual partners. The relationship between casual partner type and unsafe sex was stronger on days when the sex partner was perceived to be HIV-positive and attenuated on days distinguished by high NA; the latter finding was only evident among people who reported relatively high NA, on average, across diary entries. The association between high NA and reduced probability of unsafe sex with casual partners may be interpreted in light of data showing that people who are prone to exhibiting high NA are, in contexts in which risks are especially salient, risk averse (Maner et al., 2007).
The hypothesized association between low self-efficacy and predicted probability of unsafe sex was most strongly evidenced on days when strong sexual craving and high NA were reported. In fact, without taking into account craving and NA, low self-efficacy was associated with a lower probability of unsafe sex. This is probably because people who engage in relatively frequent sexual risk-taking may have high confidence in their ability to use condoms, even if they do not always use them.
Low self-efficacy was associated with a higher predicted probability of unsafe sex with steady partners. In contrast to the model for casual partner type, the effect of perceived partner HIV status was not significant, which may simply mean that in the context of established relationships, partner HIV status no longer figures in the event-specific prediction of unprotected sex. Also, the effect of high NA on the association between partner type and unprotected sex was positive rather than negative; speculatively, this may be viewed as consistent with the activation of a mood enhancement motive. As in the model for casual partners, this model showed that high NA and craving each increased the magnitude of association between low self-efficacy and increased probability of unprotected sex.
Regardless of partner type, high NA magnified the association between alcohol use and unprotected sex. The present findings contribute to the literature by demonstrating that the effect of increased consumption, as moderated by high NA, is associated with a higher probability of unprotected sex. Lastly, the significant (low self-efficacy) x (number of drinks consumed) interaction term was significant, indicating evenings distinguished by both low self-efficacy and alcohol use are associated with a higher predicted probability of unprotected sex.
The present findings contribute to the literature by demonstrating links that are consistent with theory but not previously validated. The moderating effects of sexual craving and high NA on the same-day association between low self-efficacy and unsafe sex are consistent with the view of Cooper et al. (2003) that an avoidant coping style may account for the observation that individuals who drink as a means of coping with NA may engage in risky sexual behavior. Cooper et al.’s line of reasoning supports two alternative conclusions. On one hand, it supports the conclusion that aversive motivation results in a spurious association between frequent alcohol use and frequent unsafe sexual activity. On the other hand, it supports the conclusion that high NA creates a momentary increased susceptibility to unsafe behavior. The present findings are consistent with the latter.
Cooper (2006) has argued cogently that the relationship between alcohol use and risky sex is complex and reflects “multiple underlying causal and noncausal processes.” Moreover, “even the causal portion of this relationship does not manifest as a main effect but as an interaction.” She noted that the existence of multiple causal models, “points to the need for diverse intervention strategies, and raises the possibility that different strategies will be optimally effective among individuals for whom different causal processes dominate (p. 22),” and that diary methods are one means by which researchers can empirically substantiate which of a wider range of causal models dominate within a given empirically distinguishable subset of a larger community and can guide the tailoring of risk reduction interventions.
This study had a number of limitations. The 64% diary adherence is lower than preferred, and it is possible that the daily data was not missing at random. A second limitation is the reliance on self-report data and hence the concern that individuals underreported or inaccurately reported daily behaviors and perceived states. The degree to which the findings generalize from a sample of people living with HIV/AIDS to the general population is unclear, and as noted in the Introduction, there is evidence to suggest that people living with HIV/AIDS, particularly those who are also suffering from profound economic disadvantage and who are heavy drinkers, are subject to psychosocial stressors that may make them uniquely vulnerable to the self-regulatory problems investigated in the present study. In addition, the diary assessment could have been used more effectively to capture participants’ perceptions of their partners’ support for, or resistance to, the use of condoms, as this is unquestionably an important predictor of condom use behavior. Finally, we did not distinguish between insertive and penetrative anal sex acts, or between sex acts based on HIV serostatus disclosure.
Despite these limitations, the findings underscore advantages of diary methods in recording dynamic intrapersonal processes. A prevailing practice among intervention specialists is to assign all members of a treatment group an equal “dosage” of material aimed at promoting (for example) self-efficacy to use condoms. Yet, if the association between self-efficacy and condom use behavior is contingent upon momentary affective states, the more effective intervention may be one that focuses on building skills to self-regulate emotions. Likewise, efforts to reduce alcohol use during sexual situations may be more effective if they also address affective states that give rise to both alcohol use and reduced self-efficacy to use condoms. Future researchers may benefit from using diary methods to better align the content of interventions to the needs of a specific target community or to the needs of individuals.
Acknowledgments
This research was supported by the National Institute on Alcohol Abuse and Alcoholism, R21AA015665-01A1. Dr. Kiene is supported by a mentored research scientist career development award from the National Institutes of Mental Health (K01 MH083536). We also acknowledge support provided by the University of Connecticut Health Center’s General Clinical Research Center, NIH M01 RR006192.
We wish to thank Dr. Ming-Hui Chen of the University of Connecticut’s Department of Statistics for his generous assistance, and also wish to thank the anonymous reviewers for their very helpful comments.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ADB
Contributor Information
William D. Barta, University of Connecticut, School of Nursing; University of Connecticut, Center for Health, Intervention, and Prevention, Storrs, CT
Howard Tennen, University of Connecticut Health Center, Department of Community Medicine, Farmington, CT.
Susan M. Kiene, Departments of Medicine and Community Health, The Warren Alpert Medical School of Brown University and Rhode Island Hospital
References
- Anzala AO, Simonsen JN, Kimani J, Ball TB, Nagelkerke NJ, Rutherford J, et al. Acute sexually transmitted infections increase human immunodeficiency virus type 1 plasma viremia, increase plasma type 2 cytokines, and decrease CD4 cell counts. Journal of Infectious Disease. 2000;182:459–466. doi: 10.1086/315733. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; NY: 1997. [Google Scholar]
- Barta W, Portnoy D, Kiene SM, Tennen H, Abu-Hasaballah KS, Ferrer R. A daily process investigation of alcohol-involved sexual risk behavior among economically disadvantaged problem drinkers living with HIV/AIDS. AIDS and Behavior. 2008;12(5):729–740. doi: 10.1007/s10461-007-9342-4. [DOI] [PubMed] [Google Scholar]
- Canin M, Dolcini M, Adler NE. Barriers to and facilitators of HIV-STD behavior change: Intrapersonal and relationship-based factors. Review of General Psychology. 1999;3(4):338–371. [Google Scholar]
- Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and the risk of depressive disorders. American Journal of Psychiatry. 2001;158:725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Current Directions in Psychological Science. 2006;15(1):19–23. [Google Scholar]
- Cooper ML, Shapiro CM, Powers AM. Motivations for sex and risky sexual behavior among adolescents and young adults: A functional perspective. Journal of Personality and Social Psychology. 1998;75(6):1528–1558. doi: 10.1037//0022-3514.75.6.1528. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Wood PK, Orcutt HK, Albino AW. Personality and predisposition to engage in risky or problem behaviors during adolescence. Journal of Personality and Social Psychology. 2003;84:390–410. doi: 10.1037//0022-3514.84.2.390. [DOI] [PubMed] [Google Scholar]
- Corbett AM, Dickson-Gomez J, Hilario H, Weeks MR. A little thing called love: Condom use in high-risk primary heterosexual relationships. Perspectives on Sexual and Reproductive Health. 2009;41(4):218–224. doi: 10.1363/4121809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. AIDS. 2002;16:135–149. doi: 10.1097/00002030-200201250-00002. [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA. The independence of positive and negative affect. Journal of Personality and Social Psychology. 1984;47:1105–1117. doi: 10.1037//0022-3514.47.5.1105. [DOI] [PubMed] [Google Scholar]
- Dingle GA, Oei TPS. Is alcohol a cofactor of HIV/AIDS? Evidence from immunological and behavioral studies. Psychological Bulletin. 1997;122:56–77. doi: 10.1037/0033-2909.122.1.56. [DOI] [PubMed] [Google Scholar]
- Eliason MJ, Amodia DS. An integral approach to drug craving. Addiction Research and Therapy. 2007;15(4):343–364. [Google Scholar]
- Engels JM, Diehr P. Imputation of missing longitudinal data: A comparison of methods. Journal of Clinical Epidemiology. 2003;56:968–976. doi: 10.1016/s0895-4356(03)00170-7. [DOI] [PubMed] [Google Scholar]
- Folch C, Marks G, Esteve A, Zaragoza K, Muñoz R, Casabona J. Factors associated with unprotected sexual intercourse with steady male, casual male, and female partners among men who have sex with men in Barcelona, Spain. AIDS Education and Prevention. 2006;18(3):227–242. doi: 10.1521/aeap.2006.18.3.227. [DOI] [PubMed] [Google Scholar]
- Kalichman SC. HIV transmission risk behaviors of men and women living with HIV-AIDS: Prevalence, predictors, and emerging clinical interventions. Clinical Psychology: Science and Practice. 2000;7:32–47. [Google Scholar]
- Kalichman SC, Weinhardt L. Negative affect and sexual risk behavior: Comment on Crepaz and Marks (2001) Health Psychology. 2001;20(4):300–301. [PubMed] [Google Scholar]
- Kiene SM, Tennen H, Armeli S. Today I’ll use a condom, but who knows about tomorrow: A daily process study of variability in predictors of condom use. Health Psychology. 2008;27(4):463–472. doi: 10.1037/0278-6133.27.4.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latka MH, Metsch LR, Mizuno Y, Tobin K, Mackenzie S, Arnsten JH, Gourevitch MN. Unprotected sex among HIV-positive injection drug-using women and their serodiscordant male partners: Role of personal and partnership influences. Journal of Acquired Immune Deficiencies Syndrome. 2006;42:222–228. doi: 10.1097/01.qai.0000214813.50045.09. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Vanslyke JG, Hoppe MJ, Rainey DT, Morrison DM, Gillmore MR. Drinking and condom use: Results from an event-based daily diary. AIDS and Behavior. 2008;12(1):104–112. doi: 10.1007/s10461-007-9216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lescano CM, Brown LK, Miller PM, Puster KL. Unsafe sex: Do feelings matter? Journal of Prevention and Intervention in the Community. 2007;33(1-2):51–62. doi: 10.1300/J005v33n01_05. [DOI] [PubMed] [Google Scholar]
- Maner JK, Richey JA, Cromer K, Mallott M, Lejeuz CW, Joiner TE, Schmidt NB. Dispositional anxiety and risk-avoidant decision-making. Personality and Individual Differences. 2007;42:665–675. [Google Scholar]
- Moberly NJ, Watkins ER. Ruminative self-focus, negative life events, and negative affect. Behaviour Research and Therapy. 2008;49(9):1034–1039. doi: 10.1016/j.brat.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr CD, Armeli S, Tennen H, Carney MA, Affleck G, Hromi A. Daily interpersonal experiences, context, and alcohol consumption: Crying in your beer and toasting good times. Journal of Personality and Social Psychology. 2001;80(3):489–500. doi: 10.1037/0022-3514.80.3.489. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Mizuno Y, Metsch LR, Garfein R, Tobin K, Knight K, Latka MH. Unprotected sexual behavior among heterosexual HIV-positive injection drug using men: Associations by partner type and partner serostatus. Journal of Urban Health. 2006;83(4):656–668. doi: 10.1007/s11524-006-9066-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson MD, Clore GL. Belief and feeling: Evidence for an accessibility model of emotional self-report. Psychological Bulletin. 2002;128:934–960. doi: 10.1037/0033-2909.128.6.934. [DOI] [PubMed] [Google Scholar]
- Schmitz MF, Crystal S. Social relations, coping, and psychological distress among persons with HIV/AIDS. Journal of Applied Social Psychology. 2000;30:665–685. [Google Scholar]
- Scott WD, Cervone D. The impact of negative affect on performance standards: Evidence for an affect-as-information mechanism. Cognitive Therapy and Research. 2002;26(1):19–37. [Google Scholar]
- Shiffman S, Balabanis M, Paty J, Engberg J, Gwaltney C, Liu K, et al. Dynamic effects of self-efficacy on smoking lapse and relapse. Health Psychology. 2000;19:315–323. doi: 10.1037//0278-6133.19.4.315. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Walters KL, Nero DK. Safer sex among HIV+ women: The role of relationships. Sex Roles. 2000;42(7/8):691–708. [Google Scholar]
- Singer MC, Erickson PI, Badiane L, Diaz R, Ortiz D, Abraham T, Nicolaysen AM. Syndemics, sex and the city: Understanding sexually transmitted diseases in social and cultural context. Social Science and Medicine. 2006;63:2010–2021. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Sage; London: 1999. [Google Scholar]
- Templeton AR, Kramer MG, Jarvis J, Kowalski J, Gange S, Schneider MF, et al. Multiple-infection and recombination in HIV-1 within a longitudinal cohort of women. Retrovirology. 2009;6:54. doi: 10.1186/1742-4690-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Kesteren NMC, Hospers HJ, Kok G. Sexual risk behavior among HIV-positive men who have sex with men: A literature review. Patient Education and Counseling. 2007;65:5–20. doi: 10.1016/j.pec.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Vanable PA, McKirnan DJ, Buchbinder SP, Bartholomew BN, Douglas JM, Judson FN, MacQueen KM. Alcohol use and high-risk sexual behavior among men who have sex with men: The effects of consumption level and partner type. Health Psychology. 2004;23:525–532. doi: 10.1037/0278-6133.23.5.525. [DOI] [PubMed] [Google Scholar]
- Von Eye A, Bogat GA, Rhodes JE. Variable-oriented and person-oriented perspectives of analysis: The example of alcohol consumption in adolescence. Journal of Adolescence. 2006;29:981–104. doi: 10.1016/j.adolescence.2006.06.007. [DOI] [PubMed] [Google Scholar]


