Abstract
Objectives
To review the opportunities and possibilities for advancing oncology nursing competencies in genetic/genomics through the illustration of case scenarios in clinical care.
Data Sources
Literature; research reports.
Conclusions
Oncology nurses have the potential to influence whether or not cutting edge research discoveries are utilized at the bedside. Clinical integration of genetic/genomic information has the potential to optimize health outcomes and lengthen patient lives.
Implications for Nursing Practice
Oncology nurses need to include genetics/genomics in their practice in order to impact quality patient care today and for the future.
Keywords: Competency, Genetics, Genomics, Oncology Nursing Education
Genetic and genomic scientific advances have rapidly illuminated mechanisms of cancer etiology, with implications for risk assessment, diagnostic approaches, treatment design, and application of targeted interventions. Results from these advances provide the foundational knowledge of cancer at the level of the gene and have begun to revolutionize oncology care, with data acquisition from ongoing research expected to significantly influence cancer risk management, care and management options. Table 1 provides a list of research initiatives and web sites to obtain further information on the advances taking place today.1 Oncology nurses have a responsibility to serve as translators of this complex information to individuals and their families. Now, more than ever, oncology nurses must understand the fundamental principles of the biology of cancer to be competent in utilizing genetics and genomics in oncology nursing practice.2
Table 1.
Research Initiatives1
| INITIATIVE | FOR MORE INFORMATION |
|---|---|
| Biomarkers Consortium | http://www.biomarkersconsortium.org |
| Cancer Genetic Markers of Susceptibility (CGEMS) project | http://cgems.cancer.gov |
| Cancer Genome Anatomy Project (CGAP) | http://cgap.nci.nih.gov |
| Cancer Genome Atlas (TCGA) | http://cancergenome.nih.gov |
| Cancer Genome Project (CGP) | http://www.sanger.ac.uk/genetics/CGP |
| Catalog of Published Genome Wide Association Studies | http://www.genome.gov/26525384 |
| Encyclopedia of DNA Elements Project (ENCODE) | http://www.genome.gov/10005107 |
| Evaluation of Genomic Applications In Practice and Prevention | http://www.egappreviews.org |
| Genomics Applications in Practice and Prevention Network (GAPPNet™) | http://www.cdc.gov/genomics/translation/GAPPNet/index.htm/ |
| Initiative for Chemical Genetics | http://ocg.cancer.gov/programs/icg.asp |
| Microarray in Node-Negative Disease May Avoid Chemotherapy (MIND) Clinical Trial | http://www.cancer.gov/clinicaltrials/EORTC-10041 |
| National Cancer Institute Cancer Family Registries | http://epi.grants.cancer.gov/CFR |
| Pharmacogenomics Knowledge Base | http://www.pharmgkb.org |
| PhenX Toolkit | http://www.phenxtoolkit.org |
| TAILORx Clinical Trial | http://www.cancer.gov/clinicaltrials/digestpage/TAILORx |
| Therapeutically Applicable Research | http://ocg.cancer.gov/programs/target.asp |
Relevance of Genetics and Genomics to Oncology Care
The utilization of genetics and genomics in oncology nursing practice is relevant to all oncology nurses, regardless of role, setting, specialty, or population. Cancer genetics and genomics provides the scientific basis for understanding the process of carcinogenesis with implications for identifying those at risk; for those diagnosed with cancer; and for those undergoing treatment for cancer (see Figure 1). Oncology nurses have the potential to influence whether or not cutting edge research discoveries are utilized at the bedside. Clinical integration of genetic/genomic information has the potential to make a difference in the quality and/or length of patient lives through improvements in or optimization of health outcomes
Figure 1.
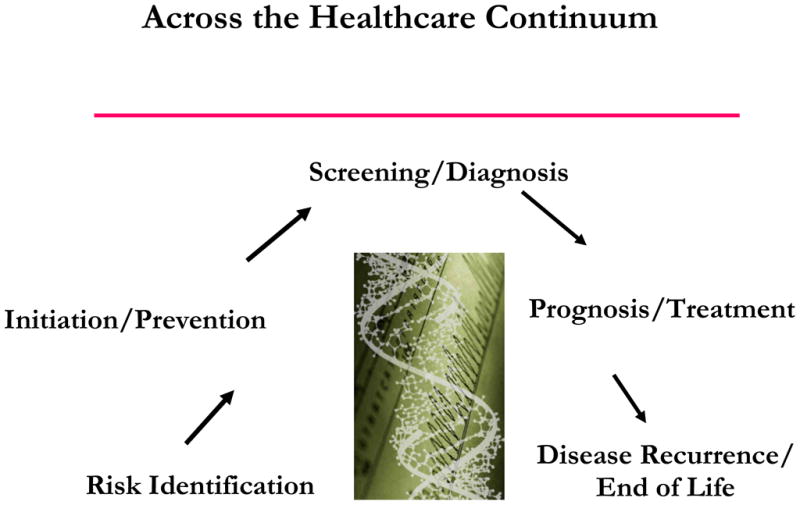
Genetic Influences
Exciting discoveries about the influences of genetic and genomic variations on the risk and development of disease is occurring for many common diseases including cardiovascular, diabetes, and mental health disorders (See http://www.genome.gov/26525384). 3,4 However, clinical integration of these discoveries is limited by the lack of a genetic/genomically informed and competent workforce, limited educational resources, lack of sufficient clinical decision support tools (i.e., pharmacogenomic test interpretation), and inadequate documentation/communication of data in medical records.
Oncology nurses have an extraordinary opportunity to be leaders in creating a model of care for integration of genetics and genomics that considers each of these gaps. Through such leadership, oncology nurses can create a shared vision of what constitutes the scope of practice required for all nursing practice specialties in this arena to help actualize the promise and potential of personalized genetic/genomic-based healthcare.
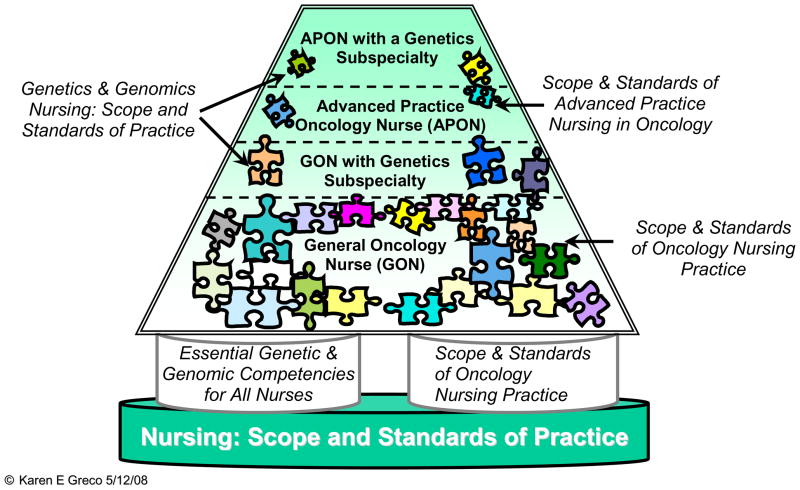
Scope of Oncology Nursing Practice
The scope of oncology nursing practice is defined through multiple mechanisms including the scope and standards of practice published by the American Nurses Association5 and by individual state practice acts. Further refinement occurs through specialty nursing organizations. For example, the Oncology Nursing Society (ONS) defines the scope of practice for oncology nurses6,7 and the International Society of Nurses in Genetics, Inc., defines practice related to genetics and genomics nursing.8 Building on the foundational understanding of practice, competencies provide an additional framework to guide nursing practice and education designed to improve health outcomes for clients. To date, the essential genetics/genomics competencies for all nurses have been endorsed by 49 professional nursing organizations, including ONS (see Table 2).9,10 As such, it is now expected that all levels of oncology nurses will incorporate genetics/genomics as a foundation to their practice (see Figure 211).
Table 2.
Essentials of Genetic and Genomic Nursing: Competencies, Curricula Guidelines, and Outcome9
| Professional Responsibilities Domain |
| Recognize when one’s own attitudes and values related to genetic and genomic science may affect care provided to clients. |
| Advocate for clients’ access to desired genetic/genomic services and/or resources including support groups. |
| Examine competency of practice on a regular basis, identifying areas of strength, as well as areas in which professional development related to genetics and genomics would be beneficial. |
| Incorporate genetic and genomic technologies and information into registered nurse practice. |
| Demonstrate in practice the importance of tailoring genetic and genomic information and services to clients based on their culture, religion, knowledge level, literacy, and preferred language. |
| Advocate for the rights of all clients for autonomous, informed genetic- and genomic-related decision-making and voluntary action. |
| Professional Practice Domain |
| Nursing Assessment: Applying/Integrating Genetic and Genomic Knowledge |
| Demonstrates an understanding of the relationship of genetics and genomics to health, prevention, screening, diagnostics, prognostics, selection of treatment, and monitoring of treatment effectiveness. |
| Demonstrates ability to elicit a minimum of three generation family health history information. |
| Constructs a pedigree from collected family history information using standardized symbols and terminology. |
| Collects personal, health, and developmental histories that consider genetic, environmental, and genomic influences and risks. |
| Conducts comprehensive health and physical assessments which incorporate knowledge about genetic, environmental, and genomic influences and risk factors. |
| Critically analyzes the history and physical assessment findings for genetic, environmental, and genomic influences and risk factors. |
| Assesses clients’ knowledge, perceptions, and responses to genetic and genomic information. |
| Develops a plan of care that incorporates genetic and genomic assessment information. |
| Identification |
| Identifies clients who may benefit from specific genetic and genomic information and/or services based on assessment data. |
| Identifies credible, accurate, appropriate, and current genetic and genomic information, resources, services, and/or technologies specific to given clients. |
| Identifies ethical, ethnic/ancestral, cultural, religious, legal, fiscal, and societal issues related to genetic and genomic information and technologies. |
| Defines issues that undermine the rights of all clients for autonomous, informed genetic- and genomic-related decision-making and voluntary action. |
| Referral Activities |
| Facilitates referrals for specialized genetic and genomic services for clients as needed. |
| Provision of Education, Care, and Support |
| Provides clients with interpretation of selective genetic and genomic information or services. |
| Provides clients with credible, accurate, appropriate, and current genetic and genomic information, resources, services, and/or technologies that facilitate decision-making. |
Uses health promotion/disease prevention practices that:
|
| Uses genetic- and genomic-based interventions and information to improve clients’ outcomes. |
| Collaborates with healthcare providers in providing genetic and genomic health care. |
| Collaborates with insurance providers/payers to facilitate reimbursement for genetic and genomic healthcare services. |
| Performs interventions/treatments appropriate to clients’ genetic and genomic healthcare needs. |
| Evaluates impact and effectiveness of genetic and genomic technology, information, interventions, and treatments on clients’ outcome. |
Figure 2.
Levels of Oncology Nursing Practice in Genetics and Genomics
The current scope of oncology nursing practice is outlined in a model that includes educational preparation, experience, specialty, roles, and responsibilities to differentiate four practice levels: the general oncology nurse (GON), the general oncology nurse with a subspecialty in genetics, the Advanced Practice Oncology Nurse (APON), and the Advanced Practice Oncology Nurse with a genetics subspecialty. A basic foundation in genetics and genomics is necessary for nurses practicing at each of these levels.11
Competencies
The Essentials of Genetic and Genomic Nursing: Competencies, Curricula Guidelines, and Outcome Indicators, established by consensus, apply to all registered nurses.9 This resource assists the academic and continuing education nurse community to prepare the nursing workforce in genetics/genomics and provide a platform to build tools needed to achieve this goal. Guidance in curriculum design and course development is provided, enhanced by the addition of outcome indicators that consist of competency-specific areas of knowledge and clinical performance indicators. The following case scenarios illustrate the relevancy, opportunities, and possibilities for advancing oncology nursing competency in genetics/genomics and thus impacting quality patient care today and for the future.
Scenario: Cancer risk-assessment: preimplantation diagnosis
Kate’s mother, Ann, is undergoing treatment for breast cancer. As part of her work-up, Ann received genetic education and counseling, chose to undergo genetic testing, and was found to have a BRCA1 mutation. Kate was quite concerned about not only her mother when she heard the news, but also about her own risk of developing cancer so she also had genetic testing, which revealed that she did indeed have a BRCA1 mutation. This result was of most importance to Kate, as she and her husband were just starting the process of in-vitro fertilization, and they were concerned about whether or not she could pass the BRCA1 mutation onto a future child. When Kate accompanied her mother to the clinic for chemotherapy, she asked the oncology nurse about the possibility of a preimplantation genetic diagnosis (PGD), expressing interest in such testing if it was available. The nurse felt very uncomfortable discussing this subject with Kate because she recognized that she personally had limited knowledge about the availability of PGD and she also had ethical concerns about using PGD for cancer risk determination. She was aware of someone who could perhaps assist Kate in finding the answers to her questions and referred Kate to this resource.
In this scenario, the clinic oncology nurse has an opportunity to use genetic and genomic knowledge and skills to provide assistance to Kate and Ann. Essential nursing competencies that could make a difference to health outcomes might include:
Recognizes when one’s own attitudes and values related to genetic and genomic science may affect care provided to clients
Advocates for the rights of all clients for autonomous, informed genetic- and genomic- related decision-making and voluntary action
Assesses clients’ knowledge, perceptions, and responses to genetic and genomic information
Identifies ethical, ethnic/ancestral, cultural, religious, legal, fiscal, and societal issues related to genetic and genomic information and technologies
Facilitates referrals for specialized genetic and genomic services for individuals as needed.
Review of the competencies listed in Table 2 may elucidate additional competencies that could apply in this situation. See Vadaparampil et al12 and Sagi et al13 for more information about preimplantation genetic diagnosis.
Scenario: Cancer risk-assessment: newborn screening and/or direct to consumer genetic testing
Jeremy was recently diagnosed with lymphoma and was being seen in the surgical clinic for a pre-operative evaluation. He was to have a lymph node removed as part of his preparation for a vaccine treatment. Jeremy’s wife is pregnant and he shares with the surgical oncology nurse that they have already named their soon to be born daughter, Lauren. He asks the surgical oncology nurse about whether or not he knows if any tests that assess risk for cancer are included in newborn screening testing and whether or not the sample taken for this testing is stored for future use. Jeremy would like to have information about Lauren’s risk for cancer earlier in her life. He hopes that if she has this information, she will have the opportunity to make better life decisions (i.e., better diet, earlier cancer screening) so that she will not have to experience what he is now going through. He also states that if newborn screening doesn’t include what he’s looking for, perhaps he’ll check out the direct to consumer tests (DCT) he has been hearing about. The nurse responds that he is not up to date on newborn screening testing but is willing to get in touch with the couples’ OB/GYN physician to clarify what information is available and determine what happens to the child’s sample when testing is completed. Additionally, because he is also unfamiliar with DCT, he decides to look on the internet for information that might be of help to Jeremy. He has heard that there may be issues related to clinical utility and validity of genetic test results and wants to read more about DCT before he discusses this information with Jeremy.
Essential nursing competencies that could make a difference to health outcomes in this scenario might include:
Examine competency of practice on a regular basis, identifying areas of strength, as well as areas in which professional development related to genetics and genomics would be beneficial
Identifies credible, accurate, appropriate, and current genetic and genomic information, resources, services, and/or technologies specific to given clients
Provides clients with credible, accurate, appropriate, and current genetic and genomic information, resources, services, and/or technologies that facilitate decision-making
Collaborates with healthcare providers in providing genetic and genomic healthcare
Refer to the competency listing in Table 2 to select additional competencies that could also apply in this scenario, and read about the utilization of genetic/genomic information in lymphoma care,14 the Institute of Medicine meeting on newborn screening report15, other screening of newborns and children,16 genomic medicine in children,17 and DTC genetic testing.18
Scenario: Genetic testing for identification of hereditary colon cancer diagnosis and treatment identification
Ken is being admitted to the hospital. During a routine colonoscopy he was found to have colon cancer and he is now being admitted for surgery. As part of the admission process, the in-patient oncology nurse asks about Ken’s family history. Ken mentions that his father, several of his aunts, and a few cousins have had cancer at early ages and that his father died at age 55 from colon cancer. The oncology nurse continues to collect family history details and suspects that Ken’s family may have a hereditary susceptibility to cancer. She remembers an announcement of a recent report on the Centers for Disease Control and Prevention (CDC) web site (http://www.cdc.gov/genomics/update/current.htm ) that provided recommendations for genetic testing in newly diagnosed individuals with colon cancer and shares that information with Ken’s doctor. The doctor then discusses with the nurse information about microsatellite instability (MSI) testing and immunohistochemical (IHC) testing of the tumor tissue upon surgical resection and also KRAS testing to assist in Ken’s treatment decisions. They discussed the implications of genetic evaluation for Ken and his family. If Ken is found to have a mutation that has contributed to his risk for colon cancer, his relatives might also benefit from having genetic testing. Relatives inheriting this mutation would benefit from colonoscopy screening at a younger age.
Essential nursing competencies for the oncology nurse in this situation that could make a difference to health outcomes might include:
Incorporates genetic and genomic technologies and information into registered nurse practice
Demonstrates ability to elicit a minimum of three-generation family health history information
Constructs a pedigree from collected family history information using standardized symbols and terminology
Collects personal health, and developmental histories that consider genetic, environmental, and genomic influences and risks
Identifies clients who may benefit from specific genetic and genomic information and/or services based on assessment data
Uses genetic- and genomic- based interventions and information to improve clients’ outcomes
Refer to the competency listing in Table 2 to select additional competencies that could also apply in this scenario. See the EGAPP Recommendation Statement19 and article by Markowitz and Bertagnoli20 for more information.
Scenario: Genetic testing for melanoma treatment selection
Stacy, an elderly Asian lady, was being being seen in a Cancer Center to receive follow-up information from the melanoma biomarker testing performed to faciliate treatment decisions. Stacy speaks fairly good English but sometimes interrupts the oncology research nurse for further clarification as she explains the type of biomarkers evaluated, the meaning of genetic changes, and how when certain genetic changes are present in the tumor (i.e., the oncogene BRAF21), there are medications that have been found to work best for those clients (i.e., PLX403221). Stacy said she previously had a genetic test done at a local pharmacy for a medication she took when she had a blood clot, so she understands what the nurse is saying. But Stacy was concerned about whether the cost of this new targeted drug would be paid for by her insurance. The research nurse assesses Stacy’s understanding of the genetic test results and the treatment plan and assists her with investigating insurance coverage.
Essential nursing competencies for the oncology nurse in this scenario that could make a difference to health outcomes might include:
Demonstrate in practice the importance of tailoring genetic and genomic information and services to clients based on their culture, religion, knowledge level, and literacy, and preferred language
Demonstrates an understanding of the relationship of genetics and genomics to health, prevention, screening, diagnsotics, prognostics, selection of treatment, and monitoring of treatment effectiveness
Develops a plan of care that incorporates genetic and genomic assessment information
Provides clients with interpretation of selective genetic and genomic information or services
Collaborates with insurance providers/payers to faciliate reimbursement for genetic and genomic healthcare services
Refer to the competency listing in Table 2 to select additional competencies you think could also apply in this scenario. See Wellbrock and Hurlstone21 for information about targeted melanoma treatments; and more about personalized interventions at http://oba.od.nih.gov/oba/SACGHS/reports/SACGHS_PGx_report.pdf.
Implications for Practice, Education, and Research
These scenarios illustrate some currently available healthcare implications of genetic and genomic discoveries. The potential benefits to individuals and their families can best be realized if oncology nurses are aware of, prepared for, and able to competently adopt options for personalized healthcare into their practice. This will require a commitment by the nurse to become adequately educated and knowledgeable about the relevancy of genetic/genomic information for every patient. Nursing research that evaluates the effectiveness of nursing competency in making a difference in quality such as improvements in or optimizing of health outcomes and length of our patient’s lives is a key component in assuring that this revolution in oncology care is actualized.1
Conclusion
Oncology nurses have a wonderful opportunity to create the optimal care model for implementation and utilization of emerging genetic/genomic science that will make a difference in outcomes for patients and their families. The Essentials of Genetic and Genomic Nursing 9 provides guidance for clinical integration. The case scenarios described illustrate the relevancy, opportunities, and possibilities for advancing oncology nursing competency and thus impacting quality patient care today and for the future. Just as the unfolding stories continuously unravel, so too will the options for improving healthcare illuminated by genetic/genomic research continue to expand.22 This necessitates that informed and competent oncology nurses become intimately involved in policy decisions regarding types of service delivery and access; privacy and confidentially of genetic/genomic information; reimbursement for personalized healthcare; and creation of educational resources. Only then will the ability to appropriately and responsibly integrate these discoveries into practice to optimize health outcomes be achieved.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Conley Y. Research: making a difference in practice. In: Calzone K, Masny A, Jenkins J, editors. Genetics and Genomics in Oncology Nursing Practice. Pittsburgh, PA: Oncology Nursing Society; 2010. pp. 305–316. [Google Scholar]
- 2.Calzone K, Masny A, Jenkins J. Genetics and Genomics in Oncology Nursing Practice. Pittsburgh, PA: Oncology Nursing Society; 2010. [Google Scholar]
- 3.Kirk M, Tonkin E. Understanding the role of genetics and genomics in health 1: background. Nurs Times. 2009;105:18–22. [PubMed] [Google Scholar]
- 4.Kirk M, Tonkin E. Understanding the role of genetics and genomics in health 2: implications for practice. Nurs Times. 2009;105:19–23. [PubMed] [Google Scholar]
- 5.American Nurses Association . Nursing: Scope and standards of practice. Washington, DC: Author; 2004. [Google Scholar]
- 6.Brant JM, Wickham R, editors. Statement on the scope and standards of oncology nursing practice. Pittsburgh, PA: Oncology Nursing Society; 2004. [Google Scholar]
- 7.Jacobs L, editor. Statement on the scope and standards of advanced practice nursing in oncology. 3. Pittsburgh, PA: Oncology Nursing Society; 2003. [Google Scholar]
- 8.International Society of Nurses in Genetics and the American Nurses Association. Genetics and genomics nursing: Scope and standards of nursing practice. Silver Spring, MD: American Nurses Association; 2006. [Google Scholar]
- 9.Consensus Panel on Genetic/Genomic Nursing Competencies. Essentials of genetic and genomic nursing: competencies, curricula guidelines, and outcome indicators. 2. Silver Spring, MD: American Nurses Association; 2009. [Google Scholar]
- 10.Jenkins J, Calzone K. Establishing the essential nursing competencies for genetics and genomics. J Nurs Scholarsh. 2007;39(1):10–16. doi: 10.1111/j.1547-5069.2007.00137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calzone K, Greco K. The scope of cancer genetics and genomics nursing practice. In: Calzone K, Masny A, Jenkins J, editors. Genetics and Genomics in Oncology Nursing Practice. Pittsburgh, PA: Oncology Nursing Society; 2010. pp. 3–12. [Google Scholar]
- 12.Vadaparampil S, Quinn G, Knapp C, Maol T, Friedman S. Factors associated with preimplantation genetic diagnosis acceptance among women concerned about hereditary breast and ovarian cancer. Genet Med. 2009;11(10):757–765. doi: 10.1097/GIM.0b013e3181b3f451. [DOI] [PubMed] [Google Scholar]
- 13.Sagi M, Weinberg N, Eilat A, et al. Preimplantation genetic diagnosis for BRCA1/2-a novel clinical experience. Prenat Diagn. 2009;29:508–513. doi: 10.1002/pd.2232. [DOI] [PubMed] [Google Scholar]
- 14.Calzone K, Lea D, Masny A. Non-Hodgkin’s lymphoma as an exemplar of the effects of genetics and genomics. J Nurs Scholarsh. 2006;38(4):335–343. doi: 10.1111/j.1547-5069.2006.00124.x. [DOI] [PubMed] [Google Scholar]
- 15. [Accessed August 31, 2010];Challenges and opportunites in using newborn screening samples for translational research: A workshop. 2010 http://www.iom.edu/Activities/Research/GenomicBasedResearch/2010-MAY-24.aspx. [PubMed]
- 16.Calonge N, Green N, Rinalso P, et al. Committee report: Method for evaluating conditions nominated for population-based screening of newborns and children. Genet Med. 2010;12(3):153–159. doi: 10.1097/GIM.0b013e3181d2af04. [DOI] [PubMed] [Google Scholar]
- 17.Haga S, Terry S. Ensuring the safe use of genomic medicine in children. Clin Pediatr. 2009;48(7):703–708. doi: 10.1177/0009922809335736. [DOI] [PubMed] [Google Scholar]
- 18.Tabor H, Kelley M. Challenges in the use of direct to consumer personal genome testing in children. Am J Bioeth. 2009;9(6–7):32–34. doi: 10.1080/15265160902893916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evaluation of genomic applications in practice and prevention (EGAPP) working group. Recommendations from the EGAPP working group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med. 2009;11(1):35–41. doi: 10.1097/GIM.0b013e31818fa2ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Markowitz S, Bertagnolli M. Molecular basis of colorectal cancer. N Engl J Med. 2009;361(25):2449–2460. doi: 10.1056/NEJMra0804588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wellbrock C, Hurlstone A. BRAF as a therapeutic target in melanoma. Biochem Pharmacol. 2010;80:561–567. doi: 10.1016/j.bcp.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 22.Collins F. The Language of Life. New York, NY: HarperCollins; 2010. [Google Scholar]