Abstract
Objectives
Hispanics have less favorable cardiovascular risk profiles relative to other groups, although little is known regarding variability in risk profiles according to country of origin. Our goal was to examine the association of cardiovascular risk factors with country of origin and acculturation in a cohort of middle-aged Hispanic women.
Design
Cross-sectional study.
Setting
Baseline data for participants at the New Jersey Site of the Study of Women’s Health Across the Nation (SWAN).
Participants
419 women (142 non-Hispanic Whites, 277 Hispanic ethnicity: Central American (n=29), South American (n=106), Puerto Rican (n=56), Dominican (n=42) and Cuban (n=44).) aged 42–52.
Main Outcome Measures
BMI, smoking, blood pressure, lipid profiles, and presence of hypertension, hyperlipidemia, diabetes and metabolic syndrome were compared using univariate and multivariable models.
Results
LDL and HDL varied significantly across Hispanic subgroups (overall p ≤ 0.05). Prevalence of metabolic syndrome was greatest in Puerto Rican women (48.2% versus 40.0%, 35.0%, 13.9% and 29.3% in Central American, South American, Dominican and Cuban women, respectively, p=0.016). Central American women were least likely to smoke (p< 0.05 vs. Puerto Rican, Cuban and South American). Prevalence of hypertension and diabetes were similar across groups. Differences in lipids and metabolic syndrome were not explained by acculturation, financial strain, education, physical activity, smoking or dietary fat intake.
Conclusions
There is significant heterogeneity in cardiovascular risk status among middle-aged Puerto Rican, Cuban, Dominican, Central American and South American women, not explained by acculturation or socioeconomic indicators. These differences may be important for targeting screening and preventive interventions.
Keywords: Cardiovascular Risk Factors, Hispanics, Women, Acculturation
Introduction
Hispanics are the fastest growing demographic subgroup in the US, and will constitute 25% of the US population by 2050 (1). In general, Hispanics in the US have higher prevalence of cardiovascular risk factors than do non-Hispanic whites, particularly obesity and diabetes. (2, 3) Paradoxically, some studies have reported lower coronary heart disease and total cardiovascular disease rates among US Hispanics compared with other ethnic groups (4, 5). However, others demonstrating higher all cause (6) and coronary heart disease mortality in Hispanics (7, 8) have challenged the existence of a “Hispanic paradox”.
Reasons for elevated risk factor prevalence among Hispanics remain unclear. Acculturation to a more sedentary western lifestyle has been suggested as a factor related to the elevated rates of obesity and diabetes (9–11), and access to medical care has been shown to be lower among Hispanics compared with other ethnic groups in the US (12). Our current understanding is limited by the lack of data regarding variation in cardiovascular risk factors among Hispanic subgroups. The term Hispanic refers to a heterogeneous group consisting of persons with ancestries from a number of countries of origin. Despite heterogeneity of socioeconomic status and culture, few studies have described risk factor prevalence among ethnic subgroups of Hispanics (13). Such information would facilitate the targeting of preventive public health interventions. The New Jersey cohort of the Study of Women’s Health Across the Nation (SWAN) provided the opportunity to examine variations in cardiovascular risk factors among Hispanic women in relation to country of origin and measures of acculturation.
Methods
This cross-sectional study includes baseline data for women enrolled at the Newark, NJ site of the SWAN, a multicenter, multiethnic community-based longitudinal study designed to characterize biological and psychosocial changes during the menopausal transition (14). Briefly, SWAN enrolled a total of 3,302 women from 1996 to 1997 at seven sites: Boston MA, Chicago IL, Detroit MI, Los Angeles and Oakland CA, Newark NJ, and Pittsburgh PA. Each site recruited Caucasian women and women from one other race-ethnic background. The NJ site is the only site that specifically targeted enrollment of Hispanic women. At enrollment, women were required to have an intact uterus and at least one ovary, were not pregnant or breastfeeding, and were between 42–52 years of age. All participants were still menstruating, and women using oral contraceptives or hormone replacement therapy within the previous three months were excluded.
The Newark site recruited Hispanic and Caucasian women from Hudson County, NJ using random digit dialing and snowball sampling (14). Census tracts containing higher than average densities of Hispanic households were over sampled. A total of 420 women (142 Caucasian, 278 Hispanic) were enrolled. Women were asked to designate their primary race-ethnicity. Women were eligible for enrollment at the NJ site if they designated Puerto Rican, Mexican or Mexican American, Dominican, Central American, Cuban or Cuban American, South American, Spanish, or other Hispanic, or Caucasian/white non-Hispanic (European descent). This study was approved by the institutional review board of the New Jersey Medical School and all women signed informed consent prior to participation.
A fasting blood draw was targeted to the early follicular phase of the menstrual cycle (days two to five). All samples were maintained at 4° C until separated and then were frozen at −80° C and shipped on dry ice to a central laboratory. Standard cardiovascular risk factors were assayed at the Medical Research Laboratories, (Lexington, Kentucky, USA) which is certified by the National Heart Lung and Blood Institute, Centers for Disease Control Part III program (15). LDL was calculated using the Friedewald equation (16) excluding women with triglycerides > 4.52 mmol/L (400 mg/dL). The HOMA insulin resistance index was calculated as (fasting insulin × fasting glucose)/22.5(17). C-reactive protein was quantified with an ultrasensitive rate-immunonephelometric method (hs-CRP on a BN 100, Dade-Behring).
Blood pressure was measured in the right arm with the participant seated following at least five minutes of rest. Two sequential values were averaged. Height and weight were measured without shoes with participants wearing light clothing. Waist circumference was measured over undergarments or light clothing. Body mass index was calculated as weight (kg) divided by height (m), squared.
Diabetes was defined as a fasting blood glucose level ≥ 6.993 mmol/L (126 mg/dL) or self-reported use of insulin. The metabolic syndrome was defined according to the Adult Treatment Panel III criteria (18, 19) as having at least three of the following metabolic abnormalities: 1.) blood pressure > 130/85 or self-reported use of antihypertensive medications, 2.) HDL cholesterol < 1.295 mmol/L (50 mg/dL), 3.) triglycerides ≥ 1.695 mmol/L (150 mg/dL), 4.) Fasting glucose ≥ 5.55 mmol/L (100 mg/dL)and/or diabetes, and 5.) Waist circumference ≥ 88 cm.
Dietary data were obtained through an interviewer-administered modification of the 1995 Block Food frequency questionnaire(20). Based on examination of The Hispanic Health and Nutrition Examination Data (HHANES), nine items were added to capture nutrient intake among Hispanic participants. Frequency and portion size was asked for each food. Physical activity was assessed by self-report with an adapted version of the Kaiser Physical Activity Survey, which is based on the Baecke questionnaire (21, 22). Smoking history was assessed by self-report.
Demographic data were obtained by self-report using standard questionnaires. Level of acculturation was ascertained from four questions regarding the language in which women usually think, read or speak, talk to their friends, and listen to the radio or watch television (23). Responses to each were coded as 0=only Spanish, 1=Spanish more often than English, 2=English equal to Spanish, 3=English more often than Spanish, or 4=only English. The mean responses for these 4 questions was then calculated and used to create a categorical variable (0=low, 1–2=mid, ≥3=high acculturation). The question regarding household income was frequently unanswered or missing. Therefore, as an indicator of economic status, we utilized a three level variable that describes a perception of economic (financial) strain, "how hard is it to pay for basics", (very hard, somewhat hard, not very hard).
Statistical Methods
Demographic, behavioral, and cardiovascular risk factor variables were compared between non-Hispanic Whites and all Hispanics combined using the chi-square test for categorical variables and t-test for normally distributed continuous variables and Wilcoxon Rank Sum test for non-normally distributed continuous variables. Differences among Hispanic subgroups were assessed using chi-square for categorical variables, ANOVA for normally distributed continuous variables and Kruskall Wallis test for non-normally distributed continuous variables. When the overall difference across Hispanic subgroups was significant (p<0.05), post-hoc tests were performed with adjustment for multiple comparisons. As the primary purpose of our study was to examine differences in CVD risk factor levels among Hispanic ethnicities, the multivariable analyses focused only on the Hispanic’s. P-values were examined for overall differences across the five Hispanic subgroups, with Puerto Ricans as the referent group based on their significantly higher level of acculturation relative to the other groups in this cohort. Linear regression was used to examine differences in CVD risk factors by Hispanic subgroup after adjusting for age, acculturation, percent dietary fat intake, alcohol consumption, socioeconomic status (defined by difficulty paying for basics), and smoking status, with additional models also adjusting for BMI. The odds ratios for metabolic syndrome for each ethnic group relative to PR was calculated using logistic regression adjusted for the covariates noted above. Analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, North Carolina).
Results
No women identified themselves as Spanish or Other Hispanic, and the one woman identifying herself as Mexican American was excluded, leaving 419 of the total 420 for analyses (Table 1). Mean ages of all groups were similar. The proportion of women reporting education beyond high school was higher in Non-Hispanic Whites compared with all Hispanics combined, fewer Non-Hispanic Whites reported that it was very hard to pay for basics, and Non-Hispanic whites were more physically active.
Table I.
Demographic and Behavioral Characteristics in Caucasians and Hispanics by Ethnicity, SWAN New Jersey Site.
| Variable | Puerto Ricans N=56 |
Cubans N=44 |
Dominicans N=42 |
Central Americans N=29 |
South Americans N=106 |
Caucasians N=142 |
p-values for differences across groups | ||
|---|---|---|---|---|---|---|---|---|---|
| Non-Hispanic White vs. Hispanic† |
Among Hispanics† |
Post-Hoc Comparisons* |
|||||||
| Age, years (Mean,SD) | 46.4 (3.1) | 46.7 (3.0) | 45.4 (2.6) | 47.4 (2.9) | 46.3 (2.5) | 46.2 (2.8) | 0.71 | 0.05 | |
| Education, % > high school | 21.2 | 39.3 | 23.1 | 23.1 | 29.7 | 74.8 | <0.001 | 0.29 | |
| Acculturation: | PR v. D PR v. CA PR v. SA |
||||||||
| %Low | 50.0 | 65.9 | 81.0 | 93.1 | 76.0 | 0 | <0.001 | <0.001 | |
| %Medium | 28.6 | 31.8 | 14.3 | 6.9 | 19.2 | 2.9 | |||
| %High | 21.4 | 2.3 | 4.8 | 0 | 4.8 | 97.1 | |||
| Hard to pay for basics | |||||||||
| %Very Hard | 25.0 | 18.2 | 35.7 | 37.9 | 23.8 | 8.5 | <0.001 | 0.52 | |
| %Somewhat Hard | 55.4 | 59.1 | 50.0 | 44.8 | 66.0 | 38.7 | |||
| %Not Very Hard | 19.6 | 22.7 | 14.3 | 17.2 | 15.2 | 52.8 | |||
| Physical Activity Score | |||||||||
| % <6.25 | 38.9 | 39.5 | 35.7 | 34.6 | 37.5 | 26.1 | <0.001 | 0.96 | |
| % 6.25–7.6 | 42.6 | 37.2 | 42.9 | 34.6 | 35.6 | 22.5 | |||
| % ≥7.65 | 18.5 | 23.3 | 21.4 | 30.8 | 26.9 | 51.5 | |||
| Alcohol Intake | |||||||||
| %Non-drinkers | 44.6 | 52.3 | 50.0 | 69.0 | 49.1 | 40.4 | 0.001 | 0.64 | |
| %17.9 kcal/day | 23.2 | 13.6 | 11.9 | 17.2 | 16.0 | 19.2 | |||
| %18.0–37.1 kcal/day | 17.9 | 18.2 | 26.2 | 10.3 | 21.7 | 13.5 | |||
| %>37.1 kcal/day | 14.3 | 15.9 | 11.9 | 3.5 | 13.2 | 27.0 | |||
| Percent kcal from fat (SD) | 35.2 (9.2) | 32.8 (6.9) | 33.9 (6.8) | 32.5 (5.9) | 32.5 (6.0) | 33.6 (8.0) | 0.75 | 0.17 | |
| % Current Smokers | 26.8 | 25.0 | 12.8 | 0 | 14.4 | 22.7 | 0.15 | 0.01 | PR v. CA CA v. Cu |
Post-hoc pairwise comparisons with p<0.05;
p-values for chi-square or ANOVA
Among Hispanic subgroups, education and the proportions reporting difficulty paying for basics were similar. Acculturation was substantially higher among Puerto Ricans than other Hispanic groups. Prevalence of current smoking was significantly lower among Central Americans compared with Puerto Ricans or Cubans. Level of physical activity was similar across the Hispanic groups.
In agreement with previous studies, non-Hispanic Whites had more favorable cardiovascular risk profiles compared with Hispanics, with higher mean HDL cholesterol, lower blood pressure and triglycerides, and lower prevalence of diabetes, fasting insulin, HOMA index, and lower BMI (Table II).
Table II.
Mean (SD) and Prevalence of Cardiovascular Disease Risk Factors in Hispanics by Ethnicity and in Caucasians, SWAN New Jersey Sit
| Variable Mean (SD) or Median (IQ range) |
Puerto Ricans N=56 |
Cubans N=44 |
Dominicans N=42 |
Central Americans N=29 |
South Americans N=106 |
Caucasians N=142 |
p-values for differences across groups | ||
|---|---|---|---|---|---|---|---|---|---|
| Non- Hispanic White vs. Hispanic† |
Among Hispanics† |
Post-Hoc Comparisons‡ |
|||||||
| Systolic BP, mmHg | 123.7(12.2) | 125.3 (11.5) | 122.9 (12.3) | 125.7 (9.4) | 121.7 (10.2) | 120.6 (11.5) | 0.02 | 0.28 | |
| Diastolic BP, mmHg | 82.4 (6.1) | 82.0 (7.4) | 81.3 (8.1) | 83.4 (7.2) | 81.8 (7.1) | 78.5 (7.6) | <0.001 | 0.77 | |
| LDL Cholesterol, mmol/L | 2.83 (0.69) | 3.29 (0.69) | 3.28 (0.73) | 3.18 (0.69) | 3.13 (0.73) | 3.10 (0.81) | 0.82 | 0.02 | PR vs. Cu |
| HDL Cholesterol, mmol/L | 1.23 (0.27) | 1.22 (0.26) | 1.37 (0.30) | 1.37 (0.38) | 1.28 (0.31) | 1.42 (0.38) | <0.001 | 0.05 | |
| Triglycerides, mmol/L* | 1.51 (0.89–2.14) | 1.33 (0.88–1.62) | 0.94 (0.76–1.37) | 1.18 (0.97–1.77) | 1.44 (1.05–2.06) | 1.11(0.75–1.59) | 0.003 | 0.006 | PR vs. D D v. SA |
| % with Diabetes | 13.5 | 9.8 | 5.9 | 8.3 | 15.6 | 3.3 | 0.004 | 0.56 | |
| Glucose, mmol/L* | 5.22 (4.61–9.10) | 5.11 (4.77–5.49) | 5.05 (4.77–5.66) | 5.30 (4.66–5.99) | 4.99 (4.66–5.83) | 4.94 (4.72–5.38) | 0.07 | 0.98 | |
| Insulin, ρmol/L | 119.5 (65.3–186.1) | 77.1 (57.6–102.8) | 72.2 (46.5–111.8) | 72.2 (52.8–142.4) | 89.6 (52.1–143.8) | 66.7 (43.1–125.7) | 0.003 | 0.07 | |
| HOMA | 3.9 (2.0–6.0) | 2.7 (1.8–3.5) | 2.4 (1.5–3.8) | 2.4 (1.7, 4.8) | 2.8 (1.6, 5.2) | 2.1 (1.3–4.1) | 0.002 | 0.14 | |
| Body Mass Index, kg/m2 | 30.3 (5.9) | 30.4 (7.5) | 28.2 (5.8) | 29.4 (5.0) | 29.1 (5.6) | 27.7 (6.5) | 0.008 | 0.34 | |
| Waist Circumference, cm | 91.1 (14.3) | 90.3 (16.8) | 86.2 (13.7) | 89.2 (8.8) | 86.8 (13.7) | 86.9 (17.9) | 0.37 | 0.27 | |
For variables that were not normally distributed, medians and interquartile ranges are presented.
p-values for chi-square, ANOVA or Kruskall-Wallis test
Post-hoc pairwise comparisons with p<0.05
Among Hispanic women, LDL and HDL levels varied significantly, with post-hoc testing showing significantly lower LDL among Puerto Rican compared with Cuban women. Triglycerides also varied across Hispanic groups, with Dominicans significantly lower than either Puerto Ricans or South Americans. The prevalence of diabetes among Hispanics ranged from 5.9% to 15.6% although differences were not statistically significant. Glucose levels and HOMA index were similar across groups. Prevalence of metabolic syndrome was highest among Puerto Rican women and lowest among Dominican women, for whom prevalence was one third to one half that among other Hispanic groups (Overall p for differences = 0.0016). These differences primarily reflect differences in the proportions with low HDL, high triglycerides, and high waist circumference (Figure 1). After adjustment for age, education, SES (difficulty paying for basics), acculturation, percent dietary fat intake, alcohol consumption and smoking status, Puerto Ricans remained most likely to have the metabolic syndrome, although the difference was statistically significant only for the comparisons with Dominicans (OR; 95% confidence interval: 0.13; 0.03 to 0.5).
Figure 1.
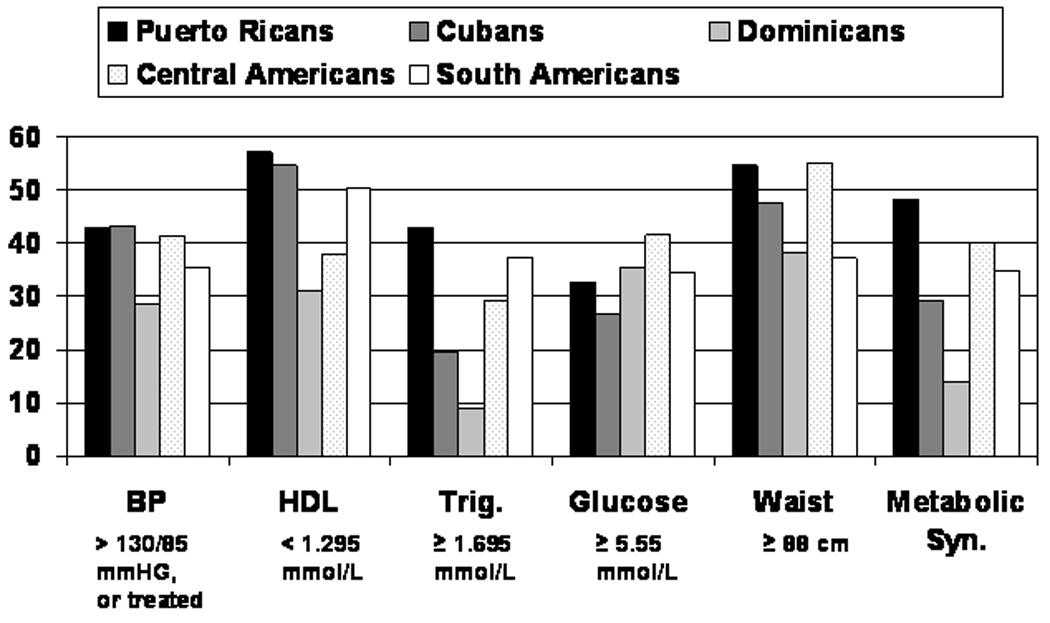
Prevalence of Metabolic Syndrome and its Components by Country of Origin.
Differences in cardiovascular risk factors among Hispanic groups were further evaluated in linear regression models adjusted for age, education, financial status, acculturation, dietary fat intake, alcohol consumption, smoking status, and BMI, with Puerto Rican considered the referent. Additional models were also adjusted for BMI (Table III). After adjustment, Puerto Rican women had significantly lower LDL cholesterol levels than Cubans, Dominicans, or South Americans. A similar pattern was observed for Puerto Rican compared with Central American women although the difference was not statistically significant after adjustment for BMI. In adjusted models, HDL was significantly higher among Dominican or Central American women compared with Puerto Rican women and BMI was significantly lower among Dominican or South American women compared to Puerto Rican women. Triglyceride levels were lower in Dominican compared with Puerto Rican women, although adjustment for BMI attenuated the association. Blood pressure measures, waist circumference, and glucose levels were not significantly different in Puerto Ricans compared with any of the other ethnic groups after adjustment.
Table III.
Multivariable-Adjusted Linear Regression Beta Estimates (95% Confidence Interval) for CVD Risk Factor Differences among Hispanic Sub-groups, SWAN New Jersey Site
| Variable | Puerto Ricans | Cubans | Dominicans | Central Americans |
South Americans |
|---|---|---|---|---|---|
| Systolic Blood Pressure, mmHg | |||||
| Model 1* | Ref | 1.9 (−2.9, 6.7) | 2.0 (−3.1, 7.1) | 3.5 (−2.3, 9.3) | −0.3 (−4.4, 3.7) |
| Model2 † | Ref | 2.1 (−2.5, 6.7) | 3.9 (−1.1, 8.8) | 4.6 (−1.0, 10.1) | 0.9 (−3.1, 4.8) |
| Diastolic Blood Pressure, | |||||
| Model 1 | Ref | −0.3 (−3.5, 2.8) | −0.6 (−3.9, 2.7) | 1.1 (−2.7, 4.8) | −0.3 (−3.0, 2.3) |
| Model2 | Ref | −0.3 (−3.3, 2.8) | 0.3 (−3.0, 3.5) | 1.5 (−2.1, 5.2) | 0.2 (−2.4, 2.8) |
| LDL, mg/dl | |||||
| Model 1 | Ref | 15.7 (3.1, 28.2) | 20.5 (7.1, 33.9) | 15.2 (0.01, 30.5) | 12.4 (1.8, 23.1) |
| Model 2 | Ref | 15.7 (3.1, 28.3) | 20.7 (7.0, 34.3) | 15.3 (−0.01, 30.6) | 12.5 (1.7, 23.4) |
| HDL, mg/dl | |||||
| Model 1 | Ref | −0.6 (−5.5, 4.3) | 7.7 (2.5, 12.9) | 8.2 (2.3, 14.1) | 3.1 (−1.1, 7.2) |
| Model 2 | Ref | −0.7 (−5.5, 4.1) | 6.3 (1.2, 11.4) | 7.4 (1.6, 13.1) | 2.2 (−1.9, 6.3) |
| Log Triglycerides, mg/dl | |||||
| Model 1 | Ref | −0.1 (−0.3, 0.2) | −0.3 (−0.6, −0.02) | −0.1 (−0.4, 0.2) | 0.004 (−0.2, 0.2) |
| Model 2 | Ref | −0.1 (−0.3, 0.2) | −0.2 (−0.5, 0.06) | −0.1 (−0.4, 0.2) | 0.1 (−0.1, 0.3) |
| Log Glucose, mg/dl | |||||
| Model 1 | Ref | −0.03 (−0.2, 0.1) | −0.03 (−0.2, 0.1) | −0.02 (−0.2, 0.1) | 0.004 (−0.1, 0.1) |
| Model 2 | Ref | −0.03 (−0.1, 0.1) | 0.002 (−0.1, 0.1) | 0.0004 (−0.1, 0.1) | 0.02 (−0.1, 0.1) |
| Body Mass Index, kg/m2 | |||||
| Model 1 | Ref | −0.3 (−2.8, 2.2) | −3.4 (−6.1, −0.7) | −1.9 (−4.9, 1.1) | −2.2 (−4.3, − 0.1) |
| Model 2 | Ref | ---- | ---- | ---- | ---- |
Model 1 adjusted for age, education, SES (difficulty paying for basics), acculturation, % dietary fat intake, alcohol consumption, and smoking status.
Model 2 adjusted for Model 1 plus BMI.
Discussion
This is one of the first studies to examine differences in cardiovascular risk factors among subgroups of Hispanic women selected from the same geographic area. Hispanic women represent a heterogeneous group with respect to cardiovascular risk factor prevalence, with Puerto Rican women at somewhat higher risk.
Diabetes and metabolic syndrome are the risk factors most consistently shown to be more prevalent among Hispanics compared with non-Hispanic Whites (2). In our cohort, Puerto Rican women were most likely to have metabolic syndrome. Dominican women were 80 percent less likely and Cuban women were 60% less likely to have metabolic syndrome than were Puerto Ricans. In the Multi-Ethnic Study of Atherosclerosis (MESA) cohort, Dominican American men and women were also less likely to have metabolic syndrome than were Puerto Ricans (13).
More recent data from MESA also demonstrate significant differences in the risk profiles of Hispanic subgroups (13). Our findings of lower LDL, higher BMI, insulin and higher prevalence of smoking among Puerto Rican women compared with Cuban Americans are consistent with the patterns observed for these groups in the larger MESA study (13). The similarity of these findings is of interest given that the SWAN cohort is on average over 10 years older than the MESA cohort, and that all women in the present analysis were recruited from the same geographical area. This implies that the ethnic subgroup differences may not be explained by regional or environmental differences.
In HHANES, Cuban American women had lower prevalence of hypertension compared with Puerto Rican or Mexican American women (24). Cuban American women in HHANES had lower rates of overweight, and hypercholesterolemia, while Puerto Rican women were more likely to smoke than were other Hispanic groups. These differences may be attributable to age differences of the cohorts. For example, in the HHANES sample, the mean age for Cuban American women was two years less and that for Puerto Rican women was 10 years less than the corresponding means in our sample(24).
In our sample, differences across subgroups of Hispanics were not explained by differences in acculturation, lifestyle factors or body size. This is consistent with a study of Mexican Americans and Central Americans living in California, that reported that acculturation was not associated with obesity in women (12).
Some prior studies have shown that Hispanics may be unaware of their cardiovascular risk status. The Centers for Disease Control and Prevention have reported that only 42% of Mexican Americans were aware of having elevated cholesterol levels, compared with 66% of non-Hispanic Whites (25, 26). In HHANES, despite lower prevalence of hypertension, Cuban American women were more likely to be aware of their hypertension status compared with Puerto Rican or Mexican American women (24). In this SWAN Newark, NJ cohort, nearly 90% of women reported having their blood pressure screened in the past 2 years, regardless of race/ethnicity. There were differences in the proportions who reported having cholesterol checked in the previous two years, ranging from 91% for Cuban women to 78% among Dominican women and 73% among Central/ South American women. Others have reported that awareness of overweight or obesity status is low among Hispanics, when self-perceptions are compared with actual anthropometric measures (27, 28). Finally, only 27% of Hispanic women compared with 55% of non-Hispanic White females have been reported to indicate awareness that heart disease is a major health problem for women (2, 29).
The present study is limited by its cross-sectional design, and small sample size among subgroups. However, this community-based sample provides the opportunity to describe a group of relatively low socioeconomic status women who have been rarely studied. Because the group of Hispanic women is heterogeneous with respect to country of origin, we were able to explore variability in the prevalence of cardiovascular risk across ethnic subgroups residing in the same geographic area. Given the lack of data on this topic, these data provide useful information which highlights the need to further explore reasons for the variations in cardiovascular risk among Hispanic women. Additional studies are required to confirm whether these results are generalizable to Hispanic women from other geographic areas or to larger samples.
We demonstrate that among middle aged Hispanic women in the SWAN New Jersey cohort, prevalence of cardiovascular risk factors varies by country of origin. Our results suggest that among Hispanic American women the development of effective prevention strategies may need to be tailored specifically for women from different countries of origin. The evolution of these risk factor profiles by country of origin will be of further interest as the SWAN New Jersey cohort traverses the menopause.
Acknowledgments/ Funding Sources
The Study of Women's Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants NR004061; AG012535, AG012531, AG012539, AG012546, AG012553, AG012554, AG012495). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH or the NIH.
Clinical Centers: University of Michigan, Ann Arbor - MaryFran Sowers, PI; Massachusetts General Hospital, Boston, MA - Robert Neer, PI 1994 – 1999; Joel Finkelstein, PI 1999- present; Rush University, Rush University Medical Center, Chicago, IL - Lynda Powell, PI; University of California, Davis/Kaiser - Ellen Gold, PI; University of California, Los Angeles - Gail Greendale, PI; University of Medicine and Dentistry - New Jersey Medical School, Newark –Gerson Weiss, PI 1994 – 2004; Nanette Santoro, PI 2004 – present; and the University of Pittsburgh, Pittsburgh, PA - Karen Matthews, PI.
NIH Program Office: National Institute on Aging, Bethesda, MD - Marcia Ory 1994 – 2001; Sherry Sherman 1994 – present; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory: University of Michigan, Ann Arbor - Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center: New England Research Institutes, Watertown, MA - Sonja McKinlay, PI 1995 – 2001; University of Pittsburgh, Pittsburgh, PA – Kim Sutton-Tyrrell, PI 2001 – present.
Steering Committee: Chris Gallagher, Chair
Susan Johnson, Chair
We thank the study staff at each site and all the women who participated in SWAN.
References
- 1.Rameriz R, de la Cruz G. The Hispanic population in the United States: March 2002. 2002 (US Census Bureau) [Google Scholar]
- 2.Davidson JA, Kannel WB, Lopez-Candales A, et al. Avoiding the looming Latino/Hispanic cardiovascular health crisis: a call to action. Ethn Dis. 2007;17(3):568–573. [PubMed] [Google Scholar]
- 3.Slattery ML, Sweeney C, Edwards S, et al. Physical activity patterns and obesity in Hispanic and non-Hispanic white women. Med Sci Sports Exerc. 2006;38(1):33–41. doi: 10.1249/01.mss.0000183202.09681.2a. [DOI] [PubMed] [Google Scholar]
- 4.Liao Y, Cooper RS, Cao G, Kaufman JS, Long AE, McGee DL. Mortality from coronary heart disease and cardiovascular disease among adult U.S. Hispanics: findings from the National Health Interview Survey (1986 to 1994) J Am Coll Cardiol. 1997;30(5):1200–1205. doi: 10.1016/s0735-1097(97)00278-7. [DOI] [PubMed] [Google Scholar]
- 5.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 6.Hunt KJ, Williams K, Resendez RG, Hazuda HP, Haffner SM, Stern MP. All-cause and cardiovascular mortality among diabetic participants in the San Antonio Heart Study: evidence against the "Hispanic Paradox". Diabetes Care. 2002;25(9):1557–1563. doi: 10.2337/diacare.25.9.1557. [DOI] [PubMed] [Google Scholar]
- 7.CDC, Prevention CfDCa. Disparities in Premature Deaths from Heart Disease--50 States and the District of Columbia, 2001. Morbidity and Mortality Weekly Report. 2004;53:121–125. [PubMed] [Google Scholar]
- 8.Pandey DK, Labarthe DR, Goff DC, Chan W, Nichaman MZ. Community-wide coronary heart disease mortality in Mexican Americans equals or exceeds that in non-Hispanic whites: the Corpus Christi Heart Project. Am J Med. 2001;110(2):81–87. doi: 10.1016/s0002-9343(00)00667-7. [DOI] [PubMed] [Google Scholar]
- 9.Evans M. Hispanic care worsens. But progress made in healthcare for blacks: report. Mod Healthc. 2006;36(4):17. [PubMed] [Google Scholar]
- 10.Khan LK, Sobal J, Martorell R. Acculturation, socioeconomic status, and obesity in Mexican Americans, Cuban Americans, and Puerto Ricans. Int J Obes Relat Metab Disord. 1997;21(2):91–96. doi: 10.1038/sj.ijo.0800367. [DOI] [PubMed] [Google Scholar]
- 11.Stern MP, Rosenthal M, Haffner SM, Hazuda HP, Franco LJ. Sex difference in the effects of sociocultural status on diabetes and cardiovascular risk factors in Mexican Americans. The San Antonio Heart Study. Am J Epidemiol. 1984;120(6):834–851. doi: 10.1093/oxfordjournals.aje.a113956. [DOI] [PubMed] [Google Scholar]
- 12.Bowie JV, Juon HS, Cho J, Rodriguez EM. Factors associated with overweight and obesity among Mexican Americans and Central Americans: results from the 2001 California Health Interview Survey. Prev Chronic Dis. 2007;4(1):A10. [PMC free article] [PubMed] [Google Scholar]
- 13.Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167(8):962–969. doi: 10.1093/aje/kwm402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sowers M, Crawford S, Sternfeld B, et al. Design, survey sampling and recruitment methods of SWAN: A multi-center, multi-ethnic, community-based cohort study of women and the menopausal transition. In: RA L JW, R M JK, editors. Menopause: Biology and Pathobiology. Academic Press; 2000. [Google Scholar]
- 15.Sutton-Tyrrell K, Wildman RP, Matthews KA, et al. Sex-hormone-binding globulin and the free androgen index are related to cardiovascular risk factors in multiethnic premenopausal and perimenopausal women enrolled in the Study of Women Across the Nation (SWAN) Circulation. 2005;111(10):1242–1249. doi: 10.1161/01.CIR.0000157697.54255.CE. [DOI] [PubMed] [Google Scholar]
- 16.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 17.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 18.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109(3):433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 20.Huang MH, Schocken M, Block G, et al. Variation in nutrient intakes by ethnicity: results from the Study of Women's Health Across the Nation (SWAN) Menopause. 2002;9(5):309–319. doi: 10.1097/00042192-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 22.Sternfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med. 1999;28(3):313–323. doi: 10.1006/pmed.1998.0470. [DOI] [PubMed] [Google Scholar]
- 23.Marin G. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1978;2:1860. doi: 10.1177/0739986314526697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crespo CJ, Loria CM, Burt VL. Hypertension and other cardiovascular disease risk factors among Mexican Americans, Cuban Americans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey. Public Health Rep. 1996 111 Suppl 2:7–10. [PMC free article] [PubMed] [Google Scholar]
- 25.CDC. Disparities in screening for and awareness of high blood cholesterol--United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54(5):117–119. [PubMed] [Google Scholar]
- 26.Census UBot, editor. Census UBot. The Hispanic Population in the United States: March 2002. Washington, D.C: 2003. [Google Scholar]
- 27.Burroughs VJ, Nonas C, Sweeney CT, et al. Self-reported Comorbidities Among Self-described Overweight African-American and Hispanic Adults in the United States: Results of a National Survey. Obesity (Silver Spring) 2008;16(6):1400–1406. doi: 10.1038/oby.2008.61. [DOI] [PubMed] [Google Scholar]
- 28.Bennett GG, Wolin KY. Satisfied or unaware? Racial differences in perceived weight status. Int J Behav Nutr Phys Act. 2006;3:40. doi: 10.1186/1479-5868-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women's awareness of heart disease: an American Heart Association national study. Circulation. 2004;109(5):573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]


