Abstract
This study examined whether improvement in parents’ depression was linked with changes in their children’s depressive symptoms and functioning. Participants were 223 parents and children ranging in age from 7–17 years old (Mean=12.13, SD=2.31); 126 parents were in treatment for depression and 97 parents were nondepressed. Children were evaluated six times over two years. Changes in parents’ depressive symptoms predicted changes in children’s depressive symptoms over and above the effect of time; children’s symptoms significantly predicted parents’ symptoms. Trajectories of children’s depressive symptoms differed significantly for children of remitted versus nonremitted depressed parents, and these differences were significantly predicted by their parents’ level of depression. The relation between parents’ and children’s depressive symptoms was partially mediated by parental acceptance.
Depression is a common psychiatric disorder in adults that presents a great cost to society in terms of dysfunctional interpersonal relationships (e.g., parenting), reduced work productivity, and increased utilization of medical and mental health services (Murray & Lopez, 1996). In adults, the population incidence of depressive disorders in a given year is 9.5% (Kessler, Chiu, Demler, & Walters, 2005b); lifetime prevalence rates are about 18% (Kessler et al., 2005a), with the highest rates in women during the years they are bearing and raising children (Heneghan, Silver, Westbrook, Bauman, & Stein, 1998; Kessler, 2003).
Offspring of depressed parents are at significantly greater risk of developing depression and other psychiatric disorders, cognitive and medical difficulties, and impaired academic and social functioning compared to offspring of nondepressed parents (Beardslee, Versage, & Gladstone, 1998; Goodman & Gotlib, 1999; Hay et al., 2001; Kramer et al., 1998; Lieb Isensee, Hofler, Pfister, & Wittchen, 2002). Moreover, depressive disorders among high-risk offspring continue into adulthood (Weissman et al., 2006a) and across multiple generations (Weissman et al., 2005). Increased risk to offspring of depressed parents has been reported in infants through adolescents, boys and girls, and for both depressed mothers and fathers (Beardslee et al., 1998; Connell & Goodman, 2002; Goodman & Gotlib, 1999; Kane & Garber, 2004).
Fortunately, depression in adults is treatable. Various interventions have been found to be efficacious in reducing depression in adults including pharmacotherapy, cognitive, behavioral, and interpersonal psychotherapies (Dimidjian et al., 2006; Hollon, Thase, & Markowitz, 2002; Weissman, Markowitz, & Klerman, 2000). In general, about 60–70% of depressed patients show a reduction in symptoms and impairment with treatment (Hollon et al., 2002). Thus, although parental depression is a highly significant predictor of psychopathology in children, depression can be treated successfully. A logical next question is: When parents recover from a depressive episode, is there also change in their children’s symptoms and functioning?
The present study examined whether reductions in parents’ depression were associated with improvement in their children’s depressive symptoms, functioning, and competence. That is, do positive changes in parents’ depression “trickle down” to their offspring? The answer to this question has serious and important policy implications for “raising healthy children.” For example, many depressed individuals either do not seek or have access to adequate clinical services (Hirschfeld et al., 1997; Newman et al., 1996). The possibility that ameliorating parents’ depression might benefit their children could motivate parents to get treatment as well as convince policy makers to make treatment of depression more available. Conversely, if remission of parents’ depression is not linked with significant improvement in their children, then more direct, child- or family-focused interventions that augment parents’ treatment might be needed to facilitate healthy development in these at-risk children.
A small but growing literature has been examining the relation between improvements in parents’ depression and their children’s psychopathology (Gunlicks & Weissman, 2008). In samples of children ranging in age from 4 to 18 years old, studies (Bryne et al., 2006; Modell et al., 2001; Timko, Cronkite, Berg, & Moos, 2002; Weissman et al., 2006b) have found that decreases in parents’ depression were associated with better child functioning, although other studies (Lee & Gotlib, 1989, 1991; Verduyn, Barroclough, Roberts, Tarrier, & Harrington, 2003) have not found a significant effect of depressed parents’ treatment or remission on their children’s adaptation. Limitations of these studies served as a guide to the present investigation.
Most studies have included only one (Alpern & Lyons-Ruth, 1993; Billings & Moos, 1986; Byrne et al., 2006; Cox et al., 1987; Lee & Gotlib, 1989, 1991; Modell et al., 2001; Weissman et al., 2006b) or two (Verdeli et al., 2004; Verduyn et al., 2003) follow-up points. Only one study to date (Pilowsky et al., 2008) has examined the relation between changes in parents’ and children’s symptoms across multiple time points. Rather, most studies simply have compared outcomes in offspring of depressed parents as a function of treatment (e.g., Verduyn et al., 2003) or remission status (e.g., Billings & Moos, 1986; Byrne et al., 2006; Cox, Puckering, Pound, & Mills, 1987); a few studies have reported correlations between parents’ and children’s symptoms (e.g., Billings & Moos, 1983; Modell et al., 2001).
Second, whereas several studies included a nondepressed “normal” comparison group (Alpern & Lyons-Ruth, 1993; Billings & Moos, 1986; Cox et al., 1987; Lee & Gotlib, 1989), others have not (e.g., Pilowsky et al., 2008; Weissman et al., 2006b). Although offspring of remitted depressed parents show improved adjustment, they typically continue to function worse compared to children of nondepressed controls (e.g., Cox et al., 1987; Lee & Gotlib, 1991). Including a nondepressed comparison group is important for determining (a) whether children of remitted parents who improve actually “normalize” (i.e., reach a level of functioning comparable to children whose parents have never been depressed), and (b) if observed changes are simply a function of time and maturation or are indeed related to improvements in parents’ depression.
Third, some researchers (e.g., Lee & Gotlib, 1991; Timko et al., 2002) have speculated that the effects of improvements in parental depression on children’s adjustment may be delayed, but only one study has tested a lagged effect (Pilowsky et al., 2008). Fourth, the idea that the changes in parents’ and children’s symptoms may be bidirectional has been noted (e.g., Dodge, 1990; Verduyn et al., 2003), but only one study has examined this (Pilowsky et al., 2008). Fifth, sample sizes have been small to moderate (mean = 127 participants); sixth, some samples have included multiple children from the same family (e.g., Byrne et al., 2006). Seventh, in several studies (e.g., Billings & Moos, 1986; Byrne et al., 2006; Modell et al., 2001; Timko et al., 2002) depressed parents were the primary informant about their children’s symptoms. Although whether or not depressed parents have distorted views of their children’s symptom remains debatable (Conrad & Hammen, 1989; Fergusson, Lynskey, & Horwood, 1993), using different informants reduces the potential problem of shared method variance.
Finally, several mechanisms have been suggested to explain the cross-generational transmission of depression (Goodman & Gotlib, 1999). In particular, rejection, hostility, withdrawal, and over control have been observed in depressed parents (e.g., Gelfand & Teti, 1990; Lovejoy, Graczyk, O’Hare, & Neuman, 2000); such problematic parenting may partially explain the relation between parental depression and psychopathology in their children (Bifulco et al., 2002). Is the reverse also true? That is, are improvements in parental depression linked with changes in parenting behavior and in children’s symptoms? Specific mechanisms explaining the relation between changes in parents’ depression and children’s adjustment have been suggested (e.g., Byrne et al., 2006; Lee & Gotlib, 1991) and tested (e.g., Billings & Moos, 1986; Timko et al., 2002). Timko et al. showed that family dysfunction contributed to the prediction of children’s outcomes over and above parents’ depression. Whether family factors mediate the link between changes in parents’ and children’s depression remains to be studied.
Thus, although some evidence exists of significant associations between remission of parents’ depression and improvements in their children’s outcomes, questions persist about the strength, direction, and underlying causes of this relation. The current study built on this literature by (a) exploring individual trajectories of depressive symptoms in parents and children and the relation between these trajectories, (b) testing lagged effects, (c) examining bidirectional relations between parents’ and children’s symptoms, (d) examining changes in symptoms and behaviors in nonremitted depressed, remitted, and nondepressed parents, (e) testing whether improvement in parenting mediated changes in the relation between parents’ and children’s depressive symptoms, and (f) exploring the trajectories of functioning and perceived competence of offspring of nonremitted depressed, remitted, and nondepressed parents. In addition, this study addressed methodological weaknesses of prior studies by including a nondepressed comparison group, using different informants about parents’ depression and children’s symptoms, having a moderate size sample of 226 parents, including only one child per family, and conducting multiple follow-up assessments post baseline across 22 months.
Consistent with the goals of this special issue on the healthy development of children, this study (a) measured child outcomes related to adaptation and functioning, (b) focused on the family context, (c) addressed the amelioration or prevention of child problems through reducing depression in parents, and (d) identified a potential mechanism of change (e.g., parenting), which could be a more direct target of intervention. The following hypotheses were addressed: (1) There will be a significant association between changes in parents’ and children’s depressive symptoms over time. We examined whether this association was significant when lagged by one assessment point and whether it was bidirectional. (2) Trajectories of change in children’s depressive symptoms will differ significantly among offspring of nonremitted depressed, remitted, and nondepressed parents. Changes in children’s symptoms in these groups will be predicted by parents’ depressive symptoms. (3) Trajectories of parenting will differ for nonremitted depressed, remitted, and nondepressed parents. Changes in parenting will mediate the relation between changes in parents’ and children’s depressive symptoms. (4) Trajectories of adaptive functioning and perceived competence will differ among offspring of nonremitted depressed, remitted, and nondepressed parents.
METHOD
Participants
Participants were 226 dyads of one parent and one child per family. The high-risk group consisted of 129 families in which a parent was receiving treatment for a current Major Depressive Disorder (MDD) as defined in the Diagnostic and Statistical Manual of Mental Disorders (4th edition; American Psychiatric Association, 1994), and scored 14 or greater on the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1967). Exclusion criteria included a lifetime diagnosis in parents of any psychotic or paranoid disorder, organic brain syndrome, mental retardation, or bipolar I or II, or a current or primary diagnosis of substance abuse or dependence, obsessive-compulsive disorder, eating disorder, certain personality disorders (antisocial, borderline, schizotypal), or unwillingness to participate in treatment for depression.
The comparison group (low risk) included 97 families with parents who were lifetime-free of mood disorders, psychotic disorders, organic brain syndromes, or personality disorders, and during the child’s life were free of adjustment disorders, anxiety disorders, substance abuse/dependence, psychotherapy longer than eight sessions, and psychotropic medication use.
Child participants were between 7 and 17 years old (Mean = 12.39, SD = 2.31). Only one child per family was included. In families with multiple children, the child closest to age 12 participated. Exclusion criteria were a developmental disability or a chronic medical condition. Children lived with the target parent at least half the time. For nondepressed families, the enrolled child was selected to be similar in age, gender, and race to a high-risk child. The overall sample was 54.6% female, 69.6% Caucasian, 21.6% African-American, 1% Asian, and 6.9% multi-racial. High- and low-risk children did not differ significantly in children’s age, gender, ethnicity/race, or parents’ age or gender (see Table 1); the index of socioeconomic status, parent education, differed significantly between the groups and was controlled in all analyses.
Table 1.
Demographic characteristics and parents’ baseline depressive symptom scores
| CHILDREN | High-Risk N = 129 | Low-Risk N = 97 |
|---|---|---|
| Age [Mean (SD)] | 12.02 (2.41) | 12.76 (2.26) |
| Girls [N (%)] | 68 (52.7%) | 54 (55.1%) |
| Ethnicity/Race [N (%)] | ||
| White, non-Hispanic | 90 (69.8%) | 68 (69.4%) |
| African-American | 27 (20.9%) | 22 (22.4%) |
| Asian | 2 (1.5%) | 1 (1.0%) |
| Multi-racial | 10 (7.8%) | 6 (6.1%) |
| PARENTS | Depressed N = 129 | Nondepressed N = 97 |
| Female [N (%)] | 95 (73.5%) | 77 (77.5%) |
| Age [Mean (SD)] | 41.32 (6.8) | 44.48 (5.0) |
| Parent Education [Mean (SD)]* | 14.71 (14.71) | 15.48 (15.45) |
| BDI-II [Mean (SD)] | 25.77 (11.69) | 1.91 (2.48) |
| HRSD [Mean (SD)] | 21.30 (5.77) | 1.25 (2.30) |
p < .05; SD = Standard Deviation; BDI-II = Beck Depression Inventory, second edition; HRSD = Hamilton Rating Scale for Depression
Procedure
Participants were obtained from three different cities in the southeast, northeast, and northwest United States. Depressed parents were recruited from clinics when they first presented for treatment. These parents received standard, evidence-based treatments including medication and/or cognitive behavioral therapy from experienced psychiatrists, psychologists, social workers, or psychiatric nurses. Recruitment of comparison families involved advertisements, coordination with local schools, health maintenance organizations, and community agencies. These parents were initially screened over the phone, and if eligible, then were scheduled for an evaluation to further assess eligibility criteria.
Assessments of high-risk children were conducted by different evaluators than those treating and assessing the parent. Child evaluations occurred at the beginning of the parents’ treatment and at parents’ mid- and post-treatment (4 months) and then at 6-month intervals (i.e., 10, 16, and 22 months post intake). Low-risk children were assessed within two weeks after the parent evaluation and then also followed at these multiple points across time.
Measures
Parents’ Psychopathology
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First et al., 1997) was used to evaluate psychopathology in parents. A randomly selected subset of taped interviews was used to assess inter-rater reliability, yielding kappa coefficients ≥ .80.
Hamilton Rating Scale for Depression (HRSD; Hamilton, 1967) is an interview-based measure of the severity of depression. The 17-item version used here yields scores ranging from 0 to 52; higher scores indicate greater severity. The HRSD has high inter-rater reliability (i.e., ≥ .84). Intra-class correlation in this study was .96.
Beck Depression Inventory, Second Edition (BDI-II; Beck et al., 1996; Beck, Steer, & Garbin, 1988) is a 21-item self-report measure rated on a scale ranging from 0 (absence of symptoms) to 3 (most severe level of the symptom). Scores can range from 0 to 63; higher scores indicate more depression. Coefficient alpha in this sample was ≥ .91 at all time points.
Children’s Depressive Symptoms, Functioning, Perceived Competence
The Children’s Depression Inventory (CDI; Kovacs, 1992) is a 27-item self-report measure of children’s symptoms of depression rated on a 3-point scale. Total scores can range from 0 to 54, with higher scores indicating more depression. Coefficient alpha for the CDI in this sample was ≥ .84 at all time points.
The Child and Adolescent Functional Assessment Scale (CAFAS; Hodges, 1997) measures functional impairment in children in five domains (role performance, behavior toward others/self, moods/self-harm, thinking, and substance use). Each item is assigned an impairment score ranging from “Minimal or No Impairment” to “Severe;” higher scores indicate worse functioning. Reliability and validity of the CAFAS are well-established and have been found to be good (Bates, 2001).
The Self-Perception Profile for Children (SPPC; Harter, 1985) assesses children’s perceptions of their competence in several domains (e.g., academic, social, appearance, behavior). Responses are scored on a 4-point scale. Lower scores indicate poorer perceived competence. Internal consistencies for the subscales were .89 or higher at all time points.
Parenting was measured with the Children’s Report of Parent Behavior Inventory (CRPBI; Schaefer, 1965), which contains 24 items yielding 3 factors: acceptance, psychological control, and monitoring/knowledge. Children completed the measure about the target depressed parent by reporting on the similarity between the item and the parent’s behavior using a 3-point scale (0 = like, 1 = somewhat like, 2 = not like). Higher scores indicated more of the particular parenting behaviors. In the current sample, internal consistency across all time points was α ≥ .90 for acceptance, α ≥ .77 for psychological control, α ≥ .84 for monitoring/knowledge.
Data Analysis Plan
Growth curve analyses were used to examine the intercepts and slopes and to test both linear and curvilinear trends. In these analyses, multilevel modeling techniques were used, accounting for the nesting of time within person. Outcome variables were regressed on TIME, allowing for differences between subjects in linear slope, and TIME*TIME, allowing for differences in a curvilinear (quadratic) trend. These trends then can become dependent variables, which may be predicted by between-subjects variables (e.g., differences between parent groups). For analyses examining differences among slopes across three parent groups (i.e., nonremitted, remitted, nondepressed), dummy coded variables were used to estimate group intercepts and slopes and to test for differences among those parameter estimates. To examine whether another time-varying covariate explained (i.e., mediated) group differences in slopes over time, models including and then not including the covariates were estimated. Mediation was judged to be present if the covariate showed a significant association with the dependent variable, and the association between the dependent variable and the slope estimates decreased when the time-varying covariate was included in the model. Differences in these slope estimates (with and without the mediator in the model) were examined with the Sobel test, using the standard error equation provided by Clogg, Petkova, and Shihadeh (1992), and recommended by MacKinnon, Lockwood, Hoffman, West, and Sheets (2002).
RESULTS
Children’s Depressive Symptoms, Functioning, and Perceived Competence
Multivariate analyses of covariance (MANCOVAs) and analyses of covariance (ANCOVAs) with parent education as the covariate were used to compare high- and low-risk offspring on the CDI, CAFAS, and SPPC. At baseline, offspring of depressed parents had significantly higher levels of depressive symptoms, worse functioning in several domains, and lower perceived competence than low-risk children (see Table 2).
Table 2.
Depressive symptoms, functioning, perceived competence, and parenting among offspring of depressed and nondepressed comparison parents at baseline
| Offspring of Depressed N = 129 | Offspring of Nondepressed N = 97 | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | F | |
| Child Depression Inventory (CDI) | 7.87 (6.19) | 4.82 (4.43) | 506.68*** |
| CAFAS – Functioning | a12.605*** | ||
| Role Performance | 8.53 (8.37) | 2.11 (4.11) | 33.87*** |
| Behavior toward others | 5.09 (6.79) | 1.13 (3.18) | 18.53*** |
| Moods/Emotions/Self-harm | 8.62 (8.43) | 1.13 (3.18) | 46.31*** |
| Substance Use | 1.47 (5.32) | .85 (4.05) | 2.00 |
| Thinking | .43 (2.43) | .00 (.0) | 3.69~ |
| Total Score | 24.22 (23.37) | 5.21 (8.60) | b32.48*** |
| Perceived Competence | a 2.14~ | ||
| Academic Competence | 3.05 (0.74) | 3.36 (0.55) | 5.97* |
| Social Competence | 3.19 (0.61) | 3.34 (0.53) | 2.94~ |
| Appearance | 2.98 (0.75) | 3.19 (0.61) | 3.61~ |
| Behavioral Competence | 3.14 (0.67) | 3.41 (0.54) | 6.92** |
| CRPBI - Parenting | a4.60** | ||
| Acceptance/Support | 24.89 (4.71) | 26.26 (3.97) | 4.68* |
| Psychological Control | 13.04 (3.37) | 11.72 (2.90) | 6.89** |
| Monitoring/Knowledge | 12.62 (2.51) | 13.68 (1.91) | 10.27** |
p < 10;
p < .05;
p < .01;
p < .001;
Overall F from the MANCOVA;
based on ANCOVA with parent education as the covariate. CAFAS = Child and Adolescent Functional Assessment Scale; CRPBI = Children’s Report of Parent Behavior Inventory
Trajectories of Change in Parents’ and Children’s Depressive Symptoms over Time
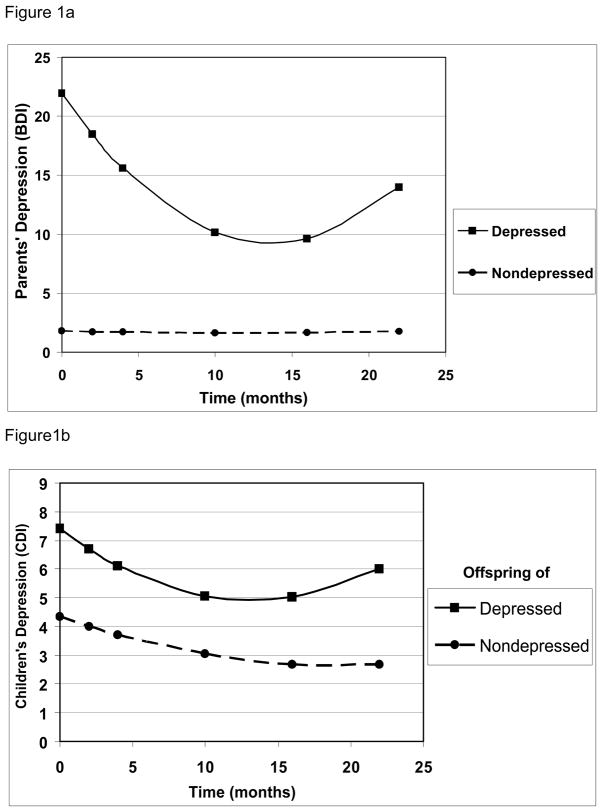
Growth curve analyses revealed that depressed parents had a significant linear and curvilinear slope on the BDI-II, indicating a significant decline and then an increase; the slope for the nondepressed parents remained low and flat (see Figure 1a). Children of depressed parents (i.e., high-risk) also showed significant linear and curvilinear trajectories for their depressive symptoms; these effects were not significant for the low-risk children (see Figure 1b). Thus, the patterns of change in depressive symptoms were similar for parents and children.
Figure 1.
Figure 1a. Trajectories of Parents’ Depressive Symptoms on the BDI-II for Nondepressed and Depressed Parents
Figure 1b. Trajectories of Children’s Depressive Symptoms on the CDI for Offspring of Nondepressed and Depressed Parents
Relation between the Trajectories of Parents’ and Children’s Depressive Symptoms
Were parents’ depressive symptoms (BDI-II) a significant time varying covariate predicting children’s depressive symptoms (CDI)? To address this question, we examined whether the estimate of the coefficient corresponding to TIME (i.e., number of months from baseline) decreased in magnitude and statistical significance with the addition of the BDI-II as the time dependent covariate, and whether the regression coefficient for the BDI-II was significant. We then analyzed whether changes in parents’ BDI-II scores predicted changes in children’s CDI scores by regressing parents’ symptoms on children’s CDIs using random regression models.
When parents’ BDI-II scores were included in the model as a time-dependent covariate, they significantly predicted children’s CDI scores (b = 0.061, p<.001). Further, the association between TIME and CDI scores decreased from −0.301 (p < .001) to −0.203 (p<.001), which was significant (z = 10.10, p<.001). The association between TIME*TIME and CDI scores decreased from 0.011(p<.001) to 0.007 (p<.001), which also was significant (z = 8.42, p<.001).
Reverse direction
Were children’s depressive symptoms (CDI scores) a significant time varying covariate of parents’ depressive symptoms? When children’s CDIs were included in the model as a time dependent covariate, they significantly predicted parents’ BDI-II scores (b=0.253, p<.001). The association between TIME and BDI-II scores was reduced from −1.040 (p<.0001) to −0.982 (p<.0001), which was a significant decrease (z = 3.12, p<.001). Similarly, the association between TIME*TIME and BDI-II scores was reduced from 0.038 (p<.0001) to 0.036 (p<.0001); this small decrease was significant (z = 2.62, p<.001). Overall these findings indicate that changes in parents’ depressive symptoms significantly predicted changes in children’s depressive symptoms over and above the simple effect of time, and similarly, children’s symptoms significantly predicted parents’ symptoms beyond the effect of time.
Lagged effects
Next, we conducted a similar set of analyses to examine the relation between the trajectories of parents’ and children’s depressive symptoms when the predictor was lagged by one assessment point. That is, did parents’ level of depressive symptoms at the prior assessment predict subsequent changes in children’s depressive symptom trajectories? When the time-lagged parent BDI-II scores were included in the model as the time-dependent covariate, the prediction to children’s CDI scores was nonsignificant (b = 0.031, p=.10). The association between TIME and CDI scores decreased from −0.301, (p<.001) to −0.060 (p=.51), which was significant (z = 14.21, p<.001). The association between TIME*TIME and CDI scores decreased from 0.011 (p<.001) to 0.003 (p<.42), which also was significant (z = 13.05, p<.001).
We again tested the reverse model. Analyses of time-lagged CDIs as a time-dependent covariate yielded a nonsignificant trend to predict parents’ BDI-IIs (b = 0.124, p=.06). The association between TIME and BDI-IIs decreased from −1.040 (p<.001) to −0.756 (p<.001), which was significant (z = 10.35, p<.001). The association between TIME*TIME and CDI scores decreased from 0.038 (p<.001) to 0.025 (p<.001), which also was significant (z=12.12, p<.001).
Trajectories of Depressive Symptoms in Parents and Children for Not Remitted Depressed, Remitted, and Nondepressed Comparison Groups
Are the trajectories of change in children’s outcomes different for those whose parents’ depression remitted versus did not remit by the end of the four months of treatment? Remission was defined as no longer being in a Major Depressive Episode and having a HRSD score of less than 12 at the end of treatment assessment (4 months). This resulted in the following groups: Remitted Depressed (Rem; n= 65), Not Remitted, still Depressed (NRD; n = 64), and the Nondepressed Comparison group (NDC; n=97). The Rem and NRD groups did not differ significantly with regard to any child or parent demographic characteristics (i.e., age, gender, race), or in the type of treatment the depressed parent received [χ2 (df=3) = 0.698, p=.874.].
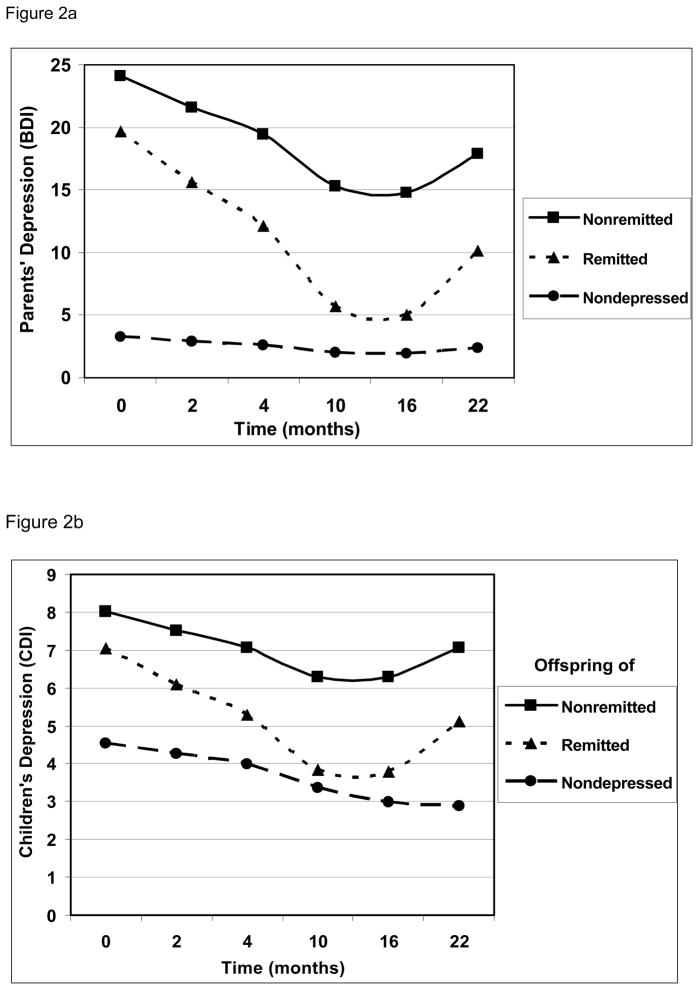
The three groups were significantly different from each other on parents’ depressive symptoms (BDI-II) in their intercepts and linear and quadratic slopes (see Table 3 and Figure 2a). Regarding children’s depressive symptoms (CDI), offspring of nondepressed parents (low-risk) had a significantly lower intercept than both high-risk groups, which did not differ significantly from each other. The trajectories of offspring of remitted and nondepressed parents were significantly different, with the remitted group showing significant linear and quadratic trends, indicating that they had a steeper drop and a greater increase compared to low-risk children (see Figure 2b). The two high-risk groups also were significantly different from each other such that there was a sharper linear decrease in children’s depressive symptoms for offspring of remitted compared to nonremitted depressed parents.
Table 3.
Growth coefficients for Parents’ (BDI-II) and Children’s (CDI) Depressive Symptoms for the Nondepressed, Remitted, and Not Remitted Depressed Parent groups.
| Measures | Groups | Intercept | Linear Change | Quadratic Change |
|---|---|---|---|---|
| Parent’s BDI-II Scores | ||||
| Nondepressed | 2.756a | −0.124a | 0.004a | |
| Remitted | 19.933b | −2.241b | 0.082b | |
| Not Remitted | 23.875c | −1.410c | 0.052c | |
| Children’s CDI Scores | ||||
| Nondepressed | 4.443a | −0.182a | 0.005a | |
| Remitted | 7.320b | −0.526b | 0.020b | |
| Not Remitted | 7.106b | −0.256a | 0.011ab |
Vertical values (columns) with different superscripts are significantly different between groups p<.05. BDI-II = Beck Depression Inventory, second edition; CDI = Children’s Depression Inventory
Figure 2.
Figure 2a. Trajectories of Parent’s Depressive Symptoms on the BDI-II for Nondepressed, Remitted, and Nonremitted Depressed Parents
Figure 2b. Trajectories of Children’s Depressive Symptoms on the CDI for Offspring of Nondepressed, Remitted, and Nonremitted Depressed Parents
Relation of the Trajectories of Depressive Symptoms in Parents and Children across Time for Not Remitted Depressed, Remitted, and Nondepressed Comparison Groups
Our analytic strategy here modeled Time (linear, quadratic) as predictors of change in children’s depressive symptoms, and tested for the effects of Parent Group (Not Remitted Depressed, Remitted, and Nondepressed) by including Time by Group interactions. These interaction terms quantified the degree to which the groups differed in their growth parameters (i.e., linear and quadratic change). To test whether change in parents’ depressive symptoms (BDI-II) predicted change in children’s depressive symptoms (CDI) over and above the effect of Time, we ran the aforementioned random regression models again and included parents’ BDI-II as a time-varying covariate (Table 4). The reduction in these interaction terms quantified the degree to which the effect of Time on changes in child CDIs was mediated by change in parents’ BDI-IIs (Baron & Kenny 1986). Mediation was tested by conducting a modified Sobel test using the standard error estimate (Clogg et al., 1992; MacKinnon et al., 2002).
Table 4.
Regression analyses of the linear (Time x Group) and curvilinear (Time x Time x Group) trajectories on the BDI-II, CDI, CAFAS, CRPBI, and Perceived Competence
| Parent’s BDI-II | Children’s CDI | CAFAS-Total | ||||
|---|---|---|---|---|---|---|
| Regression Analyses | beta | t | beta | t | beta | t |
| Intercept | 2.756 | 3.34*** | 4.443 | 8.22*** | 8.139 | 3.83*** |
| −0.108 | −0.66 | −0.260 | −2.32* | −0.834 | −1.72~ | |
| Remitted | 17.177 | 13.14*** | 2.877 | 3.33** | 16.888 | 4.88*** |
| Nonremitted | 21.118 | 15.6*** | 2.663 | 3.01** | 13.624 | 3.86*** |
| Time | −0.124 | −0.91 | −0.182 | −2.50* | −0.034 | −0.38 |
| Time X Remitted | −2.117 | −9.33*** | −0.344 | −2.89** | −0.239 | −1.57 |
| Time X Not Remitted | −1.286 | −5.55*** | −0.073 | −0.60 | 0.074 | 0.50 |
| Time X Time | 0.004 | 0.75 | 0.005 | 1.60 | -- | -- |
| Time X Time X Remitted | 0.078 | 7.74*** | 0.015 | 2.77** | -- | -- |
| Time X Time X NRD | 0.048 | 4.66*** | 0.006 | 1.08 | -- | -- |
| CRPBI (Parenting) | Acceptance | Psychol Control | Monitor/Knowledge | |||
|---|---|---|---|---|---|---|
| Regression Analyses | beta | t | beta | t | beta | t |
| Intercept | 26.446 | 59.87*** | 12.127 | 58.77*** | 13.194 | 56.19*** |
| 0.106 | 1.01 | 0.048 | 1.21 | −0.074 | −1.56 | |
| Remitted | −0.811 | −1.15 | 0.450 | 1.42 | −0.591 | −1.65~ |
| Nonremitted | −1.614 | −2.22* | 1.051 | 3.23 ** | −0.220 | −0.60 |
| Time | 0.048 | 0.85 | 0.272 | 6.06*** | −0.346 | −6.56*** |
| Time X Remitted | 0.121 | 1.30 | −0.246 | −3.34*** | 0.142 | 1.64 |
| Time X Not Remitted | −0.018 | −0.19 | −0.358 | −4.79*** | 0.266 | 3.03 ** |
| Time X Time | −0.001 | −0.21 | −0.009 | −4.70*** | 0.012 | 5.09*** |
| Time X Time X Remitted | −0.009 | −2.11* | 0.009 | 2.64** | −0.005 | −1.19 |
| Time X Time X NRD | −0.002 | −0.54 | 0.013 | 3.85*** | −0.008 | −2.00* |
| Competence | Social | Academic | Appearance | Behavior | ||||
|---|---|---|---|---|---|---|---|---|
| beta | t | beta | t | beta | t | beta | t | |
| Intercept | 3.423 | 64.41*** | 3.395 | 60.05*** | 3.302 | 51.32*** | 3.407 | 54.7*** |
| 0.002 | 0.15 | 0.040 | 3.08** | 0.001 | 0.06 | 0.031 | 2.19* | |
| Remitted | −0.140 | −1.66~ | −0.215 | −2.38* | −0.281 | −2.73** | −0.190 | −1.91~ |
| Not remitted | −0.158 | −1.81~ | −0.165 | −1.76~ | −0.180 | −1.69~ | −0.294 | −2.86** |
| Time | 0.007 | 2.36* | 0.003 | 0.94 | 0.001 | 0.2 | 0.003 | 0.40 |
| Time X Remitted | −0.003 | −0.64 | 0.009 | 2.11* | 0.010 | 2.01* | 0.024 | 1.99* |
| Time X NRD | −0.011 | −2.30* | −0.001 | −0.12 | −0.002 | −0.39 | 0.028 | 2.26* |
| Time X Time | -- | -- | -- | -- | -- | -- | 0.000 | -0.17 |
| Time X Time X Rem | -- | -- | -- | -- | -- | -- | -0.001 | -1.42 |
| Time X Time X NRD | -- | -- | -- | -- | -- | -- | -0.001 | -2.45* |
p < .10;
p < .05;
p < .01;
p < .001; BDI-II = Beck Depression Inventory; CDI = Children’s Depression Inventory; CAFAS = Child and Adolescent Functioning Scale; CRPBI = Children’s Report of Parent Behavior Inventory; Psychol = Psychological; Rem = Remitted Group; NRD = Not Remitted Depressed Group
Prior to the BDI-II being added to the model, the linear slope difference in children’s depressive symptoms between the Nondepressed (ND) and Remitted (Rem) groups was −.3436 (p<.01); after the BDI-II was added, it was −.2095 (p=.10), which was a significant reduction (z = 4.97 , p<.001). The linear slope difference between the ND and Not Remitted Depressed (NRD) groups was −.0733 (p=.55). After parents’ BDI-II scores were added, the linear slope difference was .0487 (p=.69), which was not significant (z = 0.91, p>.05). The linear slope difference between the Rem and NRD groups was −.2848 (p<.05); after the BDI-II was added it was −.2655 (p<.05), which was a not a significant reduction (z = 0.71, p>.05).
The quadratic slope difference between the ND and Rem groups was .0145 (p<.01); after the BDI-II was added the quadratic slope was .0102 (p=.06), which was a significant reduction (z = 4.30, p<.001). The quadratic slope difference between the ND and NRD groups was .0058, (p=.12); after the BDI-II was added, it was .0015 (p=.69), which was a significant reduction (z = 4.30, p<.001). The quadratic slope difference between the Rem and NRD groups was .0091, (p=.12); after the BDI was added, it was .0088 (p=.13), which was not significant (z = 0.30, p>.05). Thus, children of remitted and nondepressed parents differed in their linear and quadratic slopes, and these differences in slope were significantly predicted by parents’ BDI-IIs.
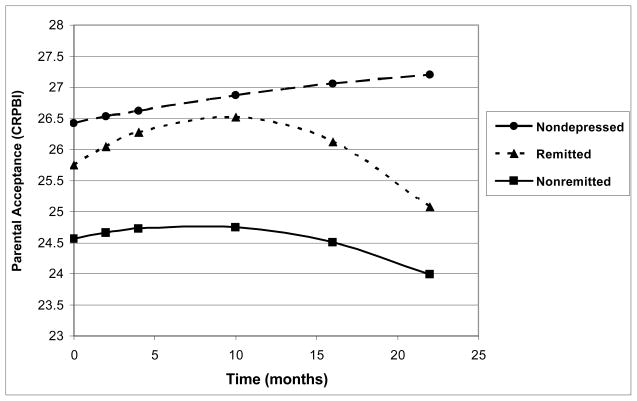
Trajectories of Parenting for Not Remitted Depressed, Remitted, and Nondepressed Groups
The next analyses compared the trajectories of the parenting variables for the three parent groups. The groups differed significantly on the trajectory of the parental acceptance subscale, with the ND group having a higher intercept than the NRD group. No differences were seen for this variable on the linear trend. The Rem group had a more negative quadratic trend than the ND group, indicating a faster increase in parental acceptance from the onset of treatment to the first follow-up, and then a faster decrease at the later assessments (Figure 3).
Figure 3.
Trajectories of Children’s Report of Parental Acceptance (CRPBI) for Nondepressed, Remitted, and Nonremitted Depressed Parents
With regard to psychological autonomy, the group difference on the intercepts was due to the ND group having a significantly lower intercept than the NRD group (see Table 4). The linear trends also differed, with the ND group having a positive slope that differed from the relatively flat slope of the Rem group and the negative slope of the NRD group. These latter slopes did not differ significantly from each other. The quadratic trends differed such that the ND group had a downward-bending curve, which differed from the flat trajectory of the Rem group and the upward-bending curve of the NRD group.
In terms of parental monitoring/knowledge, the three groups did not differ significantly on their intercepts (Table 4). The NRD group differed from the other two groups on their linear and quadratic trends such that the NRD group showed a slight drop in parental monitoring/knowledge whereas in the other two groups monitoring/knowledge decreased at a faster linear pace. Regarding the quadratic, for the NRD group levels of parental monitoring/knowledge started high and stayed high, whereas the ND and Rem groups showed a stronger positive quadratic change. That is, after an initial decrease, the NDC and Rem groups’ levels of monitoring/knowledge began to increase again.
Parenting as a Mediator of the Relation between the Trajectories of Parents’ and Children’s Depressive Symptoms
To assess whether the parenting variables mediated the relation between changes in parents’ and children’s depressive symptoms, we conducted the following analyses. In earlier analyses, we estimated the association between the BDI-II measured as a time-varying covariate and children’s CDIs. In the next analyses, we included each of the three parenting subscales (in separate analyses) as an additional time-varying covariate. Following Baron and Kenny (1986), the decrease in association between the BDI-II and CDI scores would be consistent with mediation, which can be quantified by the Sobel test. When parental acceptance was added to the model, the relation between BDI-II and CDI scores was significantly diminished (z = 5.25, p<.001), suggesting mediation. No significant change in the association between the BDI-II and CDI was found, however, when either psychological control (z = −0.763, p>.05) or parental monitoring/knowledge (z = 1.79, p>.05) were added to the model.
Trajectories of Change in Functioning and Perceived Competence for Offspring of Not Remitted Depressed, Remitted, and Nondepressed Parents
Offspring of depressed parents (both Rem and NRD) differed significantly from children of the ND group in their intercepts and linear slopes of functioning as measured by the CAFAS (see Table 4). Children whose parents’ depression remitted showed a decline in CAFAS scores indicating improved functioning, whereas children of the not remitted depressed group showed an increase in CAFAS scores, and this difference was significant. Children of the ND parents had a near-zero slope, which did not differ from either of high risk group.
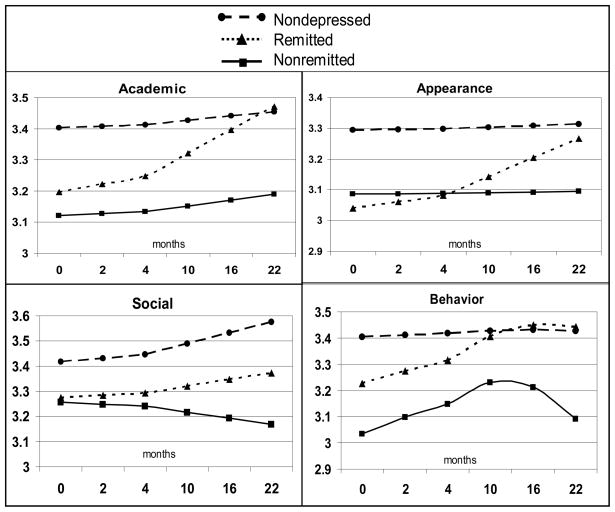
Results from modeling changes in children’s perceived competencies are presented in Table 4 and Figure 4. For perceived social competence, the groups did not differ significantly in their intercepts, but a significant linear effect was found. Children of NRD parents showed a decreasing trajectory in contrast to the increasing trajectories of children of ND and Rem parents. Analyses of children’s perceived academic competence and perceived appearance yielded similar patterns to each other. The groups were not significantly different on intercepts, but there was a significant linear effect. Offspring of Rem parents showed a significantly increasing trajectory in their perceived academic competence and perceived appearance compared to children of ND and NRD parents.
Figure 4.
Trajectories of Children’s Perceived Academic, Social, Appearance, and Behavioral Competence for Children of Nondepressed, Remitted, and Nonremitted Depressed Parents
Finally, change in children’s perceived behavioral competence scores showed a significant curvilinear effect. Children of ND parents had lower intercepts than did children of NRD and Rem parents. In terms of linear growth, children of ND parents appeared to remain steady, whereas children of NRD and Rem parents showed an increase in perceived behavioral competence over time. The significant quadratic effect indicated that children of ND parents showed a zero slope, whereas children of NRD parents showed a significant downward curve (i.e., worsening) over time.
DISCUSSION
This prospective study used knowledge from basic research on the development of adaptive and maladaptive behavior within the family context, combined with evidence from clinical science, to inform us about the possible prevention of psychopathology and promotion of well-being in at-risk youth. These results have important implications for the further construction of programs aimed at reducing children’s maladjustment and enhancing their mental health, and for the implementation of policies that facilitate their dissemination.
First, replicating basic descriptive research (Beardslee et al., 1998; Goodman & Gotlib, 1999), we found that offspring of depressed parents had higher levels of depressive symptoms, lower functioning across multiple domains, and lower perceived competence compared to children of nondepressed parents. Thus, we confirmed the first premise of the study that parental depression provides a context in which child psychopathology may develop and persist. Second, on average, parents receiving treatment for MDD showed a significantly declining linear trajectory in their depressive symptoms, and then an increase again over time. Given that depressed parents were not randomly assigned to treatment versus no treatment, however, we cannot conclude that the observed changes in depression were due to treatment per se. Rather, those individuals who improved may have done so even without intervention.
Nevertheless, the fact that depressed parents’ symptoms significantly changed over time provided an opportunity to examine whether the trajectories of parents’ and children’s depressive symptoms were associated. Indeed, offspring of depressed parents showed a similar pattern of significant linear and curvilinear trajectories of their depressive symptoms. That is, both parents’ and children’s depressive symptoms decreased and then subsequently increased over time. This finding is particularly noteworthy given that the reports about parents’ and children’s depressive symptoms were independent. Additionally, parents’ depressive symptoms significantly predicted children’s symptoms over and above the effect of time. That is, changes in children’s symptoms were significantly related to parents’ concurrent depression levels.
To examine the temporal relation between changes in parents’ and children’s depressive symptoms, we conducted the same analyses, but used parents’ depression scores from the prior assessment (e.g., at months 4, 10, and 16) to predict children’s depressive symptoms (e.g., at months 10, 16, and 22). Here we found a nonsignificant trend for parents’ depression to predict children’s depressive symptoms at the subsequent evaluation, and parents’ depressive symptoms significantly reduced the effect of time on children’s symptoms. Thus, similar to the findings of Pilowsky et al. (2008) the present study showed that the temporal relation between parents’ and children’s depressive symptoms was similar to, but less potent than, the concurrent relation. Overall, these findings suggest that changes in parents’ concurrent or prior depressive symptoms may contribute to changes in their children’s depressive symptoms over time.
Two alternative explanations for these findings are possible, however. First, the significant relation between parents’ and children’s depressive symptoms might be due to child effects. Indeed, children’s depressive symptoms significantly predicted parents’ concurrent depression scores and produced a significant reduction in the effect of time. The lagged analyses revealed a nonsignificant trend for children’s depressive symptoms to predict parents’ symptoms at the subsequent evaluation, and again the effect of time was significantly reduced. Thus, changes in parents’ depressive symptoms may be partially explained by changes in their children’s symptoms. Such child effects have been observed in other studies of parental depression (e.g., Hammen, Burge, & Stansbury, 1990; Radke-Yarrow, Nottelman, Belmont & Walsh, 1993) and suggest a possible reciprocal and likely transactional model of the relation between parents’ and children’s depression. Sameroff (2000) has asserted that examining only the influence of parents on children ignores the dynamic, transactional nature of family relationships, and that children may influence the environment (i.e., parents) as much as they are influenced by it.
Another possible explanation of the significant relation between parents’ and children’s depressive symptoms is that some third variable influenced both. For example, a common genetic vulnerability, shared life stressors, or some combination of these factors also could contribute to changes in depressive symptoms in both parents and children. Although we can eliminate the simple confound of shared method variance because different informants reported about their own depressive symptoms, we cannot rule out the substantive possibility that a third variable accounted for the observed covariation. Nevertheless, these three explanations are not mutually exclusive and likely all contribute to the dynamic relations between changes in parents’ and children’s depressive symptoms across time.
Given that not all depressed parents improved with treatment, we had the opportunity to compare the outcomes of offspring of parents whose depression remitted versus continued. Although other studies have contrasted children of remitted versus nonremitted depressed parents (e.g., Billings & Moos, 1986; Byrne et al., 2006; Cox et al., 1987), or have examined child outcomes in relation to the timing of mothers’ depression remission status (Pilowsky et al., 2008), this is the first multiple assessment, longitudinal study to examine the relations between the trajectories of parents’ and children’s depressive symptoms for parents whose depression remitted or did not remit compared to nondepressed control parents. Not surprisingly, at baseline children of nondepressed parents had significantly lower levels of depressive symptoms than offspring of both remitted and not remitted depressed parents, which were not significantly different from each other. Children of parents whose depression remitted had a steeper drop in their depressive symptoms than offspring of both nonremitted and nondepressed parents, as well as a greater subsequent increase compared to low-risk youth.
Even more interesting was that changes in parent’s depressive symptoms significantly predicted changes in their children’s depressive symptoms. In particular, differences between children of nondepressed versus remitted parents in the trajectories of their own depressive symptoms over time were partially explained by parents’ level of depressive symptoms. Similar to their parents, children of remitted patients showed a decline and then increase in their own depressive symptoms over time. These parallel patterns are consistent with the perspective that parental depression may affect children’s adjustment both positively and negatively. Thus, although decreasing parents’ depression is an important clinical goal, helping these parents maintain these gains also is critical. Sustaining positive outcomes for high-risk children may require additional interventions that specifically target the malleable mechanisms that underlie the covariation between parents’ and children’s symptoms.
One such mechanism examined in the present study was parenting behaviors, specifically acceptance, psychological control, and monitoring/knowledge. Consistent with the literature (Garber, 2005; Lovejoy et al., 2000), we found that depressed parents were significantly less accepting, more psychologically controlling, and monitored less than nondepressed parents. Moreover, the trajectories of parental acceptance differed such that remitted parents showed a greater increase in parental acceptance and then a faster decline compared to nondepressed parents. Furthermore, the relation between parents’ and children’s depressive symptoms diminished significantly when parental acceptance was added to the model, indicating that such parental acceptance partially mediated this relation. That is, decreases in parents’ depressive symptoms were associated with improvement in parental acceptance and decreases in children’s symptoms. Parental acceptance has been linked with constructs such as attachment (Bowlby, 1980) and nurturance (Maccoby & Martin, 1983), and is associated with less depression in youth (Barber, Stolz, & Olsen, 2005). One translational implication of this finding is that augmenting depressed parents’ treatment with interventions aimed at increasing parents’ support and acceptance of their children may be one way to prevent or reduce depressive symptoms in their at-risk offspring (Compas et al., in press).
Several factors may explain the lack of improvement in psychological control in both remitted and nonremitted depressed parents. First, parenting behaviors characterized by ‘‘control attempts that intrude into the psychological and emotional development of the child’’ (Barber, 1996, p. 3296) may be more ingrained in depressed parents and therefore may take longer to change. Second, reducing parents’ depression may not be sufficient to affect parents’ tendencies toward such controlling behaviors. Third, changes in this parenting behavior may be more subtle and therefore more difficult for children to detect. Nevertheless, consistent with other studies (e.g., Brennan, Le Brocque, & Hammen, 2003), this investigation found that depressed parents were more psychologically controlling than nondepressed parents.
Group differences were found in the trajectories for parental monitoring/knowledge, but this parenting dimension did not explain the relation between parents’ and children’s depressive symptoms. One reason for this may be that parental monitoring/knowledge tends to be associated with children’s externalizing problems rather than internalizing symptoms (e.g., Barber, 1996). Thus, parental monitoring likely has less of an impact on the extent and trajectories of children’s depressive symptoms.
Finally, remission of parental depression also was linked with improvements in children’s functioning in multiple domains. Whereas offspring of parents whose depression did not remit continued to have high levels of social and academic impairment, children of remitted parents showed significantly better functioning over time, although they did not reach the same level of adaptation as offspring of nondepressed parents. Thus, decreasing parents’ depression might contribute to better functioning in their children, but more may need to be done (e.g., assist with parenting; intervene directly with the children) for them to reach the level of functioning found in children of nondepressed parents.
With regard to perceived competence, offspring of remitted parents showed increasing trajectories across domains, and over time reached levels of perceived academic and behavioral competence comparable to children of nondepressed parents. In contrast, children of parents whose depression did not remit showed little change in their academic competence and perceived appearance, and had decreasing trajectories in their perceived social and behavioral competence. Thus, remission of parental depression was linked with both decreases in children’s own depressive symptoms and more positive functioning and competence.
Limitations
First, as noted earlier, because parents were not randomly assigned to treatment versus no treatment, we cannot conclude that intervention caused the changes in parents’ depression or in children’s symptoms and functioning. Second, although parents received different types of treatment (i.e., medications, therapy), the current study cannot determine the differential efficacy of these interventions in relation to children’s outcomes. Third, although a typical length of treatment for depression in adults is about 4 months (Hollon et al., 2002), longer treatment might have resulted in even more depressed parents remitting. Fourth, we cannot establish that remission of parental depression per se produced improvement in children’s depressive symptoms, functioning, and competence because possible third variables (e.g., genes, stress) cannot be ruled out. We can state with confidence, however, that improvements in parents’ depression were significantly associated with lower levels of children’s depressive symptoms, greater parental acceptance, better functioning, and greater perceived competence.
Several methodological improvements also are recommended: (1) Although the parenting dimensions studied here have been shown to be related to children’s adaptation (Barber, 1996), other aspects of parenting (e.g., Baumrind, 1978; Steinberg, 2001) also should be explored in relation to parent and child depression. (2) The use of additional informants (e.g., the other parent) and methods (e.g., behavioral observation) would provide a more comprehensive assessment of parenting. Nevertheless, children’s perceptions of their parents’ behavior may be as important in relation to their levels of distress and well-being as parents’ actual behaviors. (3) In contrast to many of the studies that have examined the relation between parents’ and children’s depression (see Gunlicks & Weissman, 2008 for a review), the present investigation included both mothers and fathers. The relatively small number of participating fathers, however, limited our power to compare the results for mothers and fathers separately. (4) Although most children lived with the depressed parent, some lived in shared custody situations. Future research with larger samples should explore whether the amount of time children spend with their depressed parent moderates the relation between parents’ and children’s depression. (5) The current study focused on differences in the trajectories of children’s symptoms and functioning. Changes in children’s diagnoses of depression and other disorders (e.g., anxiety) also should be explored. (6) The precise time interval during which the link between parents’ and children’s depressive symptoms is strongest is not yet known, but likely is shorter than the six-month time frame used in the current study.
Raising Healthy Children: Implications for Policy and Practice
The translational implications of this prospective study advance our understanding of factors within the family context that may affect children’s adjustment, and suggest possible interventions and policies for reducing mental health problems and enhancing children’s well-being. First, we recommend that community agencies (e.g., schools, churches, health care settings) provide parents with information that not only can parental depression negatively impact children, but also that a reduction in parents’ depression may have positive effects on their children’s development. Second, efficacious treatments need to be made more acceptable (i.e., less stigmatized) and accessible to depressed parents for the sake of their own health and that of their children. Educating depressed parents about the possible benefits of intervention is only worthwhile if such treatments are available to them.
Third, clinicians working with depressed patients should routinely inquire about whether they have children, how their children are doing, and the quality of their relationship with them. Similarly, clinicians working with depressed children should assess the extent of depression in the parents. Indeed, interventions aimed at treating (Brent et al., 1998) or preventing (Garber et al., 2009) depression in youth tend to be less effective when a parent is currently depressed. Given that children’s psychopathology can affect parents’ mental health as well as the reverse (e.g., Pardini, 2008), getting needed services to both children and parents may benefit each.
Supplementary interventions for offspring of depressed parents could include individual treatments with the child or family-focused therapies that target improving the parent-child relationship. Studies that test the efficacy of interventions explicitly aimed at increasing depressed parents’ warmth and support of their children can further inform us about the role of such parenting behaviors in reducing children’s depressive symptoms and enhancing their adaptive functioning. Similarly, efforts to assist depressed parents to be less controlling should be a focus of parenting interventions, especially given that this aspect of parenting does not appear to change significantly when parents’ depression remits.
Although the current study cannot determine conclusively whether treatment or even remission of parental depression is either necessary or sufficient for producing healthy children, it does highlight the kinds of studies that could address this. For example, we propose a 2 by 2 design in which depressed parents are randomized to treatment A or not A, and their children are randomized to intervention B or not B. The nature of treatment A for parents would be based on what has been shown to be most effective in treating depressed adults (Hollon et al., 2002). Similarly, intervention B could teach children the kinds of cognitive and social skills found to prevent depression in youth (e.g., Garber et al., 2009; Gillham, Reivich, Jaycox, & Seligman, 1995), or could include both parenting skills and coping skills for the children (e.g., Compas et al., in press). Such an investigation would allow us to translate the basic descriptive data produced in the current study into interventions that could have real world effects on children’s healthy development.
Table 5.
Growth Coefficients for Measures of Children’s Functioning, Perceived Competence, and Parenting for the Nondepressed, Remitted, and Not Remitted Depressed Parent Groups
| Measures | Groups | Intercept | Linear Change | Quadratic Change |
| CAFAS – Total | Nondepressed | 8.139a | −0.034ab | -- |
| Remitted | 25.028b | −0.273b | -- | |
| Not Remitted | 21.764b | 0.040a | -- | |
| Perceived Competence | ||||
| Academic | Nondepressed | 3.395a | 0.003a | -- |
| Remitted | 3.180a | 0.012b | -- | |
| Not Remitted | 3.231a | 0.002a | -- | |
| Social | Nondepressed | 3.423a | 0.007a | -- |
| Remitted | 3.283a | 0.004a | -- | |
| Not Remitted | 3.265a | −0.004b | -- | |
| Appearance | Nondepressed | 3.302a | 0.001a | -- |
| Remitted | 3.021a | 0.011b | -- | |
| Not Remitted | 3.122a | −0.001a | -- | |
| Behavior | Nondepressed | 3.407a | 0.003a | 0.000a |
| Remitted | 3.217a | 0.027b | −0.001a | |
| Not Remitted | 3.113b | 0.031b | −0.001b | |
| CRPBI - Parenting | ||||
| Acceptance/Support | Nondepressed | 26.446a | 0.048a | −0.001a |
| Remitted | 25.634a | 0.170a | −0.009b | |
| Not Remitted | 24.831b | 0.030a | −0.003ab | |
| Psychological Control | Nondepressed | 12.127a | 0.272a | −0.009a |
| Remitted | 12.577ab | 0.026b | −0.001b | |
| Not Remitted | 13.178b | −0.086b | 0.003b | |
| Monitoring/Knowledge | Nondepressed | 13.194a | −0.346a | 0.012a |
| Remitted | 12.603a | −0.204a | 0.007a | |
| Not Remitted | 12.974a | −0.080b | 0.004b |
Vertical values (i.e., columns) with different superscripts are significantly different p<.05. CAFAS = Child and Adolescent Functioning Scale; CRPBI = Children’s Report of Parent Behavior Inventory
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01MH57822, R01MH57834, R01MH057977). Garber was supported in part by an Independent Scientist Award (K02 MH66249) during completion of this work. We would like to thank the parents and children who participated in this study. We also would like to acknowledge Steven Hollon, Robert DeRubeis, Richard Shelton, Jay Amsterdam, Sona Dimidjian, Neil Jacobson, Laurel Duncan, Margaret Lovett, Cynthia Flynn, Russell Hanford, Virginia Burks, Tory Creed, and Editha Nottelmann for their support of this project.
Contributor Information
Judy Garber, Department of Psychology and Human Development, Vanderbilt University
Jeff A. Ciesla, Department of Psychology, Kent State University
Elizabeth McCauley, Department of Psychiatry and Behavioral Sciences, University of Washington/Psychiatry and Behavioral Medicine, Seattle Children's Hospital
Guy Diamond, Department of Psychiatry, University of Pennsylvania, Children’s Hospital of Philadelphia
Kelly A. Schloredt, Psychiatry and Behavioral Medicine, Seattle Children’s Hospital
References
- Alpern L, Lyons-Ruth K. Preschool children at social risk: Chronicity and timing of maternal depression symptoms at school and at home. Development and Psychopathology. 1993;5:371–387. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Barber BK. Parental psychological control: Revisiting a neglected construct. Child Development. 1996;67:3296–3319. [PubMed] [Google Scholar]
- Barber BK, Stolz HE, Olsen JA. Parental support, psychological control, and behavioral control: Assessing relevance across time, method, and culture. Monographs of the Society for Research in Child Development. 2005;70(4) doi: 10.1111/j.1540-5834.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bates MP. The Child and Adolescent Functional Assessment Scale (CAFAS): Review and current status. Clinical Child and Family Psychology Review. 2001;4:63–84. doi: 10.1023/a:1009528727345. [DOI] [PubMed] [Google Scholar]
- Baumrind D. Parental disciplinary patterns and social competence in children. Youth and Society. 1978;9:239–276. [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Bifulco AT, Moran PM, Ball C, Jacobs C, Bains R, Bunn A, Cavagin J. Child adversity, parental vulnerability and disorder: Examination of inter-generational transmission of risk. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2002;43:1075–1086. doi: 10.1111/1469-7610.00234. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Comparison of depressed and nondepressed parents: A social-environmental perspective. Journal of Abnormal Child Psychology. 1983;11:463–485. doi: 10.1007/BF00917076. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Children of parents with unipolar depression: A controlled 1-year follow-up. Journal of Abnormal Child Psychology. 1986;14:149–166. doi: 10.1007/BF00917230. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 3. Loss: Sadness and depression. New York: Basic Books; 1980. [Google Scholar]
- Brennan PA, Le Brocque R, Hammen C. Maternal depression, parent-child relationships, and resilient outcomes in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1469–1477. doi: 10.1097/00004583-200312000-00014. [DOI] [PubMed] [Google Scholar]
- Brent DA, Kolko D, Birmaher B, et al. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Byrne C, Browne G, Roberts J, et al. Changes in children’s behavior and costs for service use associated with parents’ response to treatment for dysthymia. Journal of the American Academy of Child Adolescent Psychiatry. 2006;45:239–246. doi: 10.1097/01.chi.0000190351.13818.d7. [DOI] [PubMed] [Google Scholar]
- Clogg CC, Petkova E, Shihadeh ES. Statistical methods for analyzing collapsibility in regression models. Journal of Educational Statistics. 1992;17:51–74. [Google Scholar]
- Compas BE, Forehand R, Keller G, Champion JE, Rakow A, Reeslund KL, et al. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0016930. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Conrad M, Hammen C. Role of maternal depression in perceptions of child maladjustment. Journal of Consulting and Clinical Psychology. 1989;57:663–667. doi: 10.1037//0022-006x.57.5.663. [DOI] [PubMed] [Google Scholar]
- Cox AD, Puckering C, Pound A, Mills M. The impact of maternal depression in young children. Journal of Child Psychology and Psychiatry. 1987;28:917–928. doi: 10.1111/j.1469-7610.1987.tb00679.x. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dodge KA. Developmental psychopathology in children of depressed mothers. Developmental Psychology. 1990;26:3–6. [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. Journal of Abnormal Child Psychology. 1993;21:245–269. doi: 10.1007/BF00917534. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbons M, Williams JBW. User’s guide for the Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Garber J. Depression and the family. In: Hudson JL, Rapee RM, editors. Psychopathology and the family. Oxford, UK: Elsevier; 2005. pp. 227–283. [Google Scholar]
- Garber J, Clarke G, Weersing VR, Beardslee WR, Brent D, Gladstone T, Debar L, et al. Prevention of depression in at-risk adolescents: A randomized controlled trial. Journal of the American Medical Association. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:329–353. [Google Scholar]
- Gillham JE, Reivich KJ, Jaycox LH, Seligman MEP. Prevention of depressive symptoms in school children: Two-year follow-up. Psychological Science. 1995;6:343–351. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gunlicks ML, Weissman MM. Change in child psychopathology with improvement in parental depression: A systematic review. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:379–389. doi: 10.1097/CHI.0b013e3181640805. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Development of a Rating Scale for Primary Depressive Illness. British Journal of Social and Clinical Psychology. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Hammen C, Burge D, Stansbury K. Relationship of mother and child variables to child outcomes in a high-risk sample. A causal modeling analysis. Developmental Psychology. 1990;26:24–30. [Google Scholar]
- Harter S. Manual for the Self-Perception Profile for Children: Revision of the Perceived Competence Scale for Children. Denver, CO: University of Denver; 1985. [Google Scholar]
- Heneghan AM, Silver EJ, Westbrook L, Bauman LJ, Stein REK. Depressive symptoms in mothers with young children: Who is at risk? Pediatrics. 1998;102:1394–1400. doi: 10.1542/peds.102.6.1394. [DOI] [PubMed] [Google Scholar]
- Hirschfeld R, Keller M, Panico S, Arons B, Barlow D, Davidoff F, et al. The National Depressive and Manic-Depressive Association consensus statement on the under treatment of depression. Journal of the American Medical Association. 1997;277:333–340. [PubMed] [Google Scholar]
- Hodges K. CAFAS manual for training coordinators, clinical administrators, and data managers. Ann Arbor, MI: Author; 1997. [Google Scholar]
- Hollon SD, Thase ME, Markowitz JC. Treatment and prevention of depression. Psychological Science in the Public Interest. 2002;3:1–39. doi: 10.1111/1529-1006.00008. [DOI] [PubMed] [Google Scholar]
- Kane PP, Garber J. The relation between fathers’ depression and children’s externalizing and internalizing symptoms and conflict: A meta-analysis. Clinical Psychology Review. 2004;24:339–360. doi: 10.1016/j.cpr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. Journal of Affective Disorders. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005a;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005b;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory Manual. North Tonawanda, NY: Multi Health Systems, Inc; 1992. [Google Scholar]
- Kramer RA, Warner V, Olfson M, Ebanks CM, Chaput F, Weissman MM. General medical problems among the offspring of depressed parents: A 10-year follow–up. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:602–611. doi: 10.1097/00004583-199806000-00010. [DOI] [PubMed] [Google Scholar]
- Lee CM, Gotlib IH. Maternal depression and child adjustment: A longitudinal analysis. Journal of Abnormal Psychology. 1989;98:78–85. doi: 10.1037//0021-843x.98.1.78. [DOI] [PubMed] [Google Scholar]
- Lee CM, Gotlib IH. Adjustment of children of depressed mothers: a 10-month follow–up. Journal of Abnormal Psychology. 1991;100:473–477. doi: 10.1037//0021-843x.100.4.473. [DOI] [PubMed] [Google Scholar]
- Lieb R, Isensee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Maccoby EE, Martin JA. Socialization in the context of the family: Parent-child interaction. In: Hetherington EM, editor. Handbook of child psychology, Vol. 4. Socialization, personality, and social development. 4. New York: Wiley; 1983. pp. 1–101. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modell JD, Modell JG, Wallander J, Hodgens B, Duke L, Wisely D. Maternal ratings of child behavior improve with treatment of maternal depression. Family Medicine. 2001;33:691–695. [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: Prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. Journal of Consulting and Clinical Psychology. 1996;64:552–562. [PubMed] [Google Scholar]
- Pardini DA. Novel insights into longstanding theories of bidirectional parent–child influences: Introduction to the special section. Journal of Abnormal Child Psychology. 2008;36:627–631. doi: 10.1007/s10802-008-9231-y. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Talati A, Tang M, Hughes CW, Garber J, et al. Children of depressed mothers a year after the initiation of maternal treatment: Findings from STAR*D–Child. American Journal of Psychiatry. 2008;165:1136–1147. doi: 10.1176/appi.ajp.2008.07081286. [DOI] [PubMed] [Google Scholar]
- Radke-Yarrow M, Nottelman E, Belmont B, Welsh JB. Affective interactions of depressed and non-depressed mothers and children. Journal of Abnormal Child Psychology. 1993;21:683–695. doi: 10.1007/BF00916450. [DOI] [PubMed] [Google Scholar]
- Sameroff AJ. Developmental systems and psychopathology. Development and Psychopathology. 2000;12:297–312. doi: 10.1017/s0954579400003035. [DOI] [PubMed] [Google Scholar]
- Schaefer ES. Children’s reports of parental behavior: An inventory. Child Development. 1965;36:413–424. [PubMed] [Google Scholar]
- Steinberg L. Autonomy, conflict, and harmony in the family context. In: Feldman SS, Elliot GR, editors. At the threshold: The developing adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 255–276. [Google Scholar]
- Steinberg L. We know some things: Parent-adolescent relations in retrospect and prospect. Journal of Research on Adolescence. 2001;11:1–19. [Google Scholar]
- Timko C, Cronkite RC, Berg EA, Moos RH. Children of parents with unipolar depression: a comparison of stably remitted, partially remitted, and nonremitted parents and nondepressed controls. Child Psychiatry and Human Development. 2002;32:165–185. doi: 10.1023/a:1017924421229. [DOI] [PubMed] [Google Scholar]
- Verdeli H, Ferro T, Wickramaratne P, Greenwald S, Blanco C, Weissman MM. Treatment of depressed mothers of depressed children: pilot study of feasibility. Depression and Anxiety. 2004;19:51–58. doi: 10.1002/da.10139. [DOI] [PubMed] [Google Scholar]
- Verduyn C, Barrowclough C, Roberts J, Tarrier N, Harrington R. Maternal depression and child behavior problems: Randomized placebo controlled trial of a cognitive-behavioral group intervention. British Journal of Psychiatry. 2003;183:342–348. doi: 10.1192/bjp.183.4.342. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, Klerman GL. Comprehensive guide to interpersonal psychotherapy. New York: Basic Books; 2000. [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: A STAR*D-Child report. Journal of the American Medical Association. 2006b;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. American Journal of Psychiatry. 2006a;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Verdeli H, Pilowsky DJ, et al. Families at high and low risk for depression: A 3–generation study. Archives of General Psychiatry. 2005;62:29–36. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]