Abstract
Objectives
This study aimed to examine the longitudinal association between decline in cognitive function and risk of elder self-neglect in a community-dwelling population.
Design
Prospective population-based study
Setting
Geographically-defined community in Chicago.
Participants
Community-dwelling subjects reported to the social services agency from 1993–2005 for self-neglect who also participated in the Chicago Health Aging Project (CHAP). Of the 5,519 participants in the Chicago Health Aging Project, 1,017 were reported to social services agency for suspected elder self-neglect from 1993–2005.
Measurements
Reported elder self-neglect was identified by social services agency. The primary predictor was decline in cognitive function assessed using the Mini-Mental State Examination (MMSE), the Symbol Digit Modalities Test (Executive Function), and both immediate and delayed recall of the East Boston Memory Test (Episodic Memory). An index of global cognitive function scores was derived by averaging z-scores of all tests. Outcome of interest was elder self-neglect. Logistic and linear regression models were used to assess these longitudinal associations.
Results
After adjusting for potential confounding factors, decline in global cognitive function, MMSE or episodic memory was not independently associated with increased risk of reported and confirmed elder self-neglect. Decline in executive function was associated with increased risk of reported and confirmed elder self-neglect. Decline in global cognitive function was associated with increased risk of greater self-neglect severity (PE=0.76, SE=0.31, p=0.014).
Conclusion
Decline in executive function was associated with increased risk of reported and confirmed elder self-neglect. Decline in global cognitive function was associated with increased risk of greater self-neglect severity.
Keywords: self-neglect, decline in cognitive function, aging, population-based study
INTRODUCTION
Elder self-neglect is a common and important public health issue across all sociodemographic and socioeconomic strata in the US. Elder self-neglect has great relevance not only to health care professional and social services agency, but also to public health professionals, community organizations and other relevant disciplines. Evidence suggests that there are about 1.2 million cases of elder self-neglect annually in the US (1). A recent study suggests that elder self-neglect reported to social services agency was associated with increased risk of mortality, and there is a gradient relation between greater self-neglect severity and higher risk for mortality (2). Moreover, evidence indicates that reports of elder self-neglect to social services agencies are rising (3). As our aging population increases, elder elder self-neglect will likely become an even more pervasive public health issue.
The National Centers on Elder Abuse defines elder self-neglect as “…as the behavior of an elderly person that threatens his/her own health and safety. Self-neglect generally manifests itself in an older person as a refusal or failure to provide himself/herself with adequate food, water, clothing, shelter, personal hygiene, medication (when indicated), and safety precautions” (4). There have been a number of conceptual frameworks postulated for the syndrome of elder self-neglect (5–8).
This study follows the conceptual framework derived by Dyer and colleagues (5) from a cohort of elder self-neglect cases reported to social services agencies. This conceptual framework represents a synthesis of elder self-neglect and is used by public health workers, clinicians and researchers to better understand the issues of elder self-neglect (9–14). In this conceptual framework, the common elements include: medical comorbidities (e.g., diabetes, cancer, cerebrovascular disease, cardiovascular disease, etc), depression, cognitive impairment, executive dysfunction, physical function impairment, lack of social network and social support. The central hypothesis of this framework suggests that increased burden of medical commorbidities compounded by psychological distress may exacerbate the impairment in cognitive function and physical function which in turn lead to elder self-neglect. In this model, impairment in cognitive function represents one of the central factors associated with worsening vulnerability in the syndrome of elder self-neglect. In addition, decline in cognitive function combined with physical disability, lack of social network and inadequate support services magnify the inadequate ability for self-protection, leading to the syndrome of elder self-neglect.
Lower levels of cognition function have been associated with increased morbidity and mortality (15–22). In addition, prior research suggest that cognitive impairment is associated with increased risk of elder self-neglect (23–25). There is a great paucity in our current understanding regarding the longitudinal association between declines in different domains of cognitive function with the risk of elder self-neglect. Furthermore, most prior research has categorized self-neglect dichotomously as "self-neglect" or "no self-neglect". However, self-neglect, like many other geriatric syndromes, occurs along a continuum, rather than in two discrete categories (26). We are not aware of any study that has examined the longitudinal association between decline in cognitive function and risk of greater self-neglect severity.
In this longitudinal study, we aim to expand the prior literature in two ways by examining: 1) the relationship between decline in cognitive function and the risk of self-neglect; and 2) the relationship between decline in cognitive function and the risk of greater self-neglect severity within a prospective population-based cohort. We hypothesized that decline in cognitive function is associated with increased risk of reported and confirmed elder self-neglect. In addition, we hypothesized that there is a linear relation between decline in cognitive function with greater self-neglect severity.
METHODS
Setting
Chicago Health and Aging Project (CHAP) is a study begun in 1993 that examines risk factors for Alzheimer’s disease and cognitive decline. Its participants include residents of three adjacent neighborhoods on the south side of Chicago: Morgan Park, Washington Heights and Beverly. More in depth details of the study design of CHAP have been previously published (27;28).Of the 7,813 age-eligible residents identified through a complete census of these areas, 6,158 (78.9%) were enrolled and administered a baseline interview. Data collection occurred in cycles, each lasting three years, with each cycle ending as the succeeding cycle began. Each cycle consisted of in-person interviews of subjects in the participants’ homes.
Participants
In the current study, participants were enrolled between 1993 and 2005 and had repeated cognitive function measures (N=5,519) prior to the report of elder self-neglect to social services agency. From this cohort, we identified a subset of participants (N=1,017) who were reported to social services agency for suspected elder self-neglect. Suspected cases of elder self-neglect were reported by friends, neighbors, family, social workers, city workers, health care professionals, and others. The reports were usually triggered by concerns for the health and safety of the older adult in their home environment, which would initiate a number of different services to help the affected person. CHAP and social services data were matched using variables of date of birth, sex, race, home telephone number and exact home address. All CHAP participants received structured, standardized in-person interviews that included assessment of health history and detailed assessment of cognitive function. Written informed consent was obtained, and the study was approved by the Institutional Review Board at Rush University Medical Center.
Reporting and Assessment of Self-Neglect
Elder self-neglect in this study was based on all suspected cases reported to social services agency. When a case was reported, case workers performed a home assessment, which assessed the deficits in the domains of personal hygiene and grooming, household and environmental hazards, health needs and overall home safety concerns. The level of severity was rated by case workers based on their concerns for the client’s personal health and safety issues, with the maximum cumulative score of 45. Confirmed elder self-neglect in this study was defined as anyone with a score of 1 or greater (N=862). The elder self-neglect severity referred to the scores 1 to 45, with higher score within this range indicating greater levels of elder self-neglect severity. The detail of this measure has been previously described (9;29;30). Available information from the social services agency internal report (31) showed that this measure was tested using the Kappa Statistic Algorithm (32), and all variables had inter-rater reliability coefficients great than 0.70. In addition, the internal consistencies of the items were high with Cronbach’s alpha of 0.95 (9). Both face and content validity were evaluated using qualitative data from case managers and agency administrators. In addition, external validity of the measure was assessed as a continuous variable and was shown to predict higher health care utilization (31) and increased risk of premature mortality (2).
Assessment of Cognitive Function
A battery of four different cognitive function tests was administered. The Mini-Mental State Examination (MMSE) is a widely used, 30-items measure of dementia severity (33). It has previously been used in epidemiologic studies (34) and is a component of the Consortium to Establish a Registry for Alzheimer's Disease (CERAD) protocol (35). Episodic memory was assessed using summarized scores of both immediate and delayed recall of brief stories in the East Boston Memory Test (36). Executive Function was assessed using the oral version of the Symbol Digit Modalities Test (37), which calls for rapid perceptual comparisons.
To assess global cognitive function with minimal floor and ceiling artifacts, we constructed a summary measure for global cognition based on all 4 tests. Individual test scores were summarized by first transforming a person's score on each individual test to a z-score, which was based on the mean and standard deviation of the distribution of the scores of all participants on that test, and then averaging z scores across tests to yield a composite score for global cognitive function. This procedure has the advantage of increasing power by reducing random variability present within tests, as well as reducing floor and ceiling effects of particular tests. In addition, it produces a composite score that is approximately normally distributed.
Covariates
Demographic variables used in analyses were age, sex, race and levels of education. Self-report of hypertension, diabetes mellitus, stroke, cardiovascular disease, hip fracture, cancer, Parkinson’s disease and thyroid disease were collected. Physical function was assessed using the Katz Index of Activities of Daily Living (Katz ADL), which measured limitations in an individual’s ability to perform basic self-care tasks (38). Physical function was also assessed by direct performance testing, which provided a comprehensive objective and detailed assessment of certain abilities (39). Symptoms of depression were measured using a modified version (40) of the Center for the Epidemiological Study of Depression Scale (CES-D: range 0–10) (41). Social networks was summarized as the total the number of children, relatives, and friends seen at least monthly (42)
Analytic Approach
Descriptive characteristics were provided for the reported and un-reported elder self-neglect groups. Our outcomes of interest were reported self-neglect, confirmed self-neglect, and self-neglect severity. Our predictor of interest was decline in cognitive function. For change in cognitive function measures, we summarized the differences in cognitive function scores (global cognitive function, MMSE, Executive Function, Episodic Memory), which were uniformly assessed during the CHAP interviews. For participants with elder self-neglect, we summarized the differences between first available cognitive function measure to the most immediate cognitive function measure prior to the reporting of elder self-neglect. For participants without elder self-neglect, we summarized the differences between the first available cognitive function measure to the most immediate assessment prior to the end of year 2005, as that was the last available date of self-neglect data.
Logistic regression models were used to analyze the relationship between decline in cognitive function and risk of elder self-neglect. We used a series of models to consider the relationship between decline in cognitive function and elder self-neglect, taking into consideration the potential confounders as guided by the conceptual framework. In our core model (Model A), we included age, sex, race, education to estimate the association of decline in cognitive function and risk of elder self-neglect outcomes. In addition, we added to the prior model the health-related variables of physical function and common medical comorbidities of hypertension, myocardial infarction, stroke, shingles, Parkinson’s disease, hip fracture, cancer, thyroid disease, and diabetes (Model B). Finally, models were repeated controlling for additional psychological and social factors of depressive symptomatology and social network (Model C).
We repeated the models A–C for confirmed elder self-neglect. Lastly, we used linear regression to examine the association between decline in cognitive function and elder self-neglect severity and repeated Models A–C. Odds Ratio (OR), 95% Confidence Interval (CI), Standardized-Parameter Estimates (PE), Standard Error (SE) and P values were reported for the regression models. Analyses were carried out using SAS®, Version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Baseline Characteristics
There were a total of 5,519 CHAP participants in this study and 1,017 participants were identified by social services agency for suspected elder self-neglect. The mean age of the total cohort was 72.8 years (standard deviation [SD] = 6.1 years), with approximately 61% of them being women and 64% being black older adults. The median MMSE was 28.0 (Inter-quartile range 3.0) and the median global cognitive function was 0.35 (Inter-quartile range 0.88) for the total cohort. The median decline in global cognitive function score was −0.16 (Inter-quartile range 0.82) for those with elder self-neglect and −0.15 (Inter-quartile range 0.72) for those without elder self-neglect (Table 1). Results for decline in MMSE, Executive Function, and Episodic Memory function were detailed in Table 1.
Table 1.
Cognitive Function Measures Between Elders with and without Self-Neglect
| Self-Neglect (N=1017) | No Self-Neglect (N=4502) | |
|---|---|---|
| Global Cognitive Function, mean, (SD) | −0.05 (0.75) | 0.27 (0.73) |
| Global Cognitive Function, median (IQR) | 0.08 (0.93) | 0.41 (0.83) |
| Global Cognitive Function Change, mean (SD) | −0.29 (0.79) | −0.27 (0.76) |
| Global Cognitive Function Change, median (IQR) | −0.19 (0.81) | −0.15 (0.72) |
| MMSE, mean, (SD) | 25.6 (4.4) | 26.7 (4.2) |
| MMSE, Median, (IQR) | 27.0 (4.0) | 28.0 (3.0) |
| MMSE Change, mean (SD) | −2.0 (5.5) | −1.8 (5.1) |
| MMSE Change, Median, (IQR) | −1.0 (5.0) | −1.0 (4.0) |
| Executive Function, mean, (SD) | 23.4 (12.7) | 30.9 (14.1) |
| Executive Function, median, (IQR) | 23.0 (18.0) | 32.0 (20.0) |
| Executive Function Change mean (SD) | −3.9 (10.1) | −4.2 (12.1) |
| Executive Function Change, median, (IQR) | −3.0 (11.0) | −3.0 (13.0) |
| Episodic Memory, mean (SD) | −0.01 (0.88) | 0.26 (0.84) |
| Episodic Memory, median (IQR) | 0.12 (1.13) | 0.43 (0.97) |
| Episodic Memory Change, mean (SD) | −0.23 (0.98) | −0.19 (0.93) |
| Episodic Memory Change, median (IQR) | −0.17 (1.16) | −0.03 (0.99) |
Normal Ranges for the Cognitive Function Score:
Global Cognitive Function: Range (−3.49 – 1.66)
MMSE, Range (0–30)
Executive Function, Range (0–75); Episodic Memory, Range (−2.69 – 1.42)
Decline in Global Cognitive Function and Risk of Elder Self-Neglect
In the initial logistic regression model adjusting for age, sex, race and education, we found that decline in global cognitive function was not independently associated with reported elder self-neglect (OR, 1.01, 95%CI, 0.92–1.11) (Table 2, Model A). After adding physical function, hypertension, diabetes, stroke, cancer, thyroid disease, and myocardial infarction to the model (Model B), the association did not significantly change. In the last model (Model C), after adjusting for psychosocial measures of depressive symptomatology and social network, decline in global cognitive function was not independently associated with increased risk of reported elder self-neglect (OR, 0.99, 95%CI, 0.89–1.09). For confirmed elder self-neglect, the associations were similar (Table 3)
Table 2.
Decline in Cognitive Function and Risk of Reported Self-Neglect Outcomes
| Global Cognitive Function | |||
|---|---|---|---|
| Odds Ratio (95% CI) for Self-Neglect Outcomes | |||
| Model A | Model B | Model C | |
| Sociodemographic | |||
| Age | 1.06 (1.05–1.07) | 1.05 (1.04–1.07) | 1.06 (1.04–1.07) |
| Men | 0.78 (0.67–0.89) | 0.84 (0.72–0.98) | 0.84 (0.72–0.98) |
| Black | 5.04 (4.09–6.19) | 4.86 (3.91–6.03) | 4.92 (3.95–6.13) |
| Education | 0.95 (0.93–0.97) | 0.96 (0.84–0.98) | 0.96 (0.94–0.98) |
| Health Related | |||
| Medical Conditions | 1.10 (1.01–1.20) | 1.09 (1.00–1.19) | |
| Physical Function | 0.95 (0.93–0.97) | 0.96 (0.93–0.98) | |
| Psychosocial | |||
| Depressive Symptoms | 1.04 (1.00–1.08) | ||
| Social Network | 1.00 (0.93–0.98) | ||
| Decline in Global Cognition | 1.01 (0.92–1.11) | 0.99 (0.90–1.09) | 0.99 (0.89–1.09) |
| Mini-Mental State Examination (MMSE) | |||
| Odds Ratio (95% CI) for Self-Neglect Outcomes | |||
| Model A | Model B | Model C | |
| Sociodemographic | |||
| Age | 1.07 (1.05–1.08) | 1.06 (1.05–1.08) | 1.06 (1.05–1.08) |
| Men | 0.75 (0.64–0.87) | 0.80 (0.68–0.94) | 0.80 (0.68–0.95) |
| Black | 4.98 (4.02–6.17) | 4.87 (3.89–6.08) | 4.86 (3.87–6.09) |
| Education | 0.96 (0.93–0.98) | 0.97 (0.94–0.99) | 0.97 (0.94–0.99) |
| Health Related | |||
| Medical Conditions | 1.09 (1.00–1.19) | 1.08 (0.99–1.19) | |
| Physical Function | 0.95 (0.93–0.97) | 0.95 (0.93–0.98) | |
| Psychosocial | |||
| Depressive Symptoms | 1.05 (1.01–1.09) | ||
| Social Network | 0.99 (0.98–1.01) | ||
| MMSE | 0.99 (0.98–1.01) | 0.99 (0.98–1.01) | 0.99 (0.98–1.04) |
| Executive Function | |||
| Odds Ratio (95% CI) for Self-Neglect Outcomes | |||
| Model A | Model B | Model C | |
| Sociodemographic | |||
| Age | 1.07 (1.06–1.09) | 1.06 (1.05–1.08) | 1.06 (1.05–1.08) |
| Men | 0.75 (0.64–0.87) | 0.82 (0.69–0.96) | 0.82 (0.69–1.97) |
| Black | 5.17 (4.15–6.43) | 4.89 (3.89–6.15) | 4.84 (3.84–6.08) |
| Education | 0.94 (0.92–0.96) | 0.95 (0.93–0.98) | 0.95 (0.93–0.98) |
| Health Related | |||
| Medical Conditions | 1.09 (1.00–1.21) | 1.09 (0.99–1.19) | |
| Physical Function | 0.94 (0.92–0.96) | 0.94 (0.92–0.97) | |
| Psychosocial | |||
| Depressive Symptoms | 1.03 (0.99–1.08) | ||
| Social Network | 0.99 (0.98–1.01) | ||
| Decline in Executive Function | 1.01 (0.99–1.01) | 1.01 (1.00–1.01)* | 1.01 (1.00–1.01)* |
| Episodic Memory | |||
| Odds Ratio (95% CI) for Self-Neglect Outcomes | |||
| Model A | Model B | Model C | |
| Sociodemographic | |||
| Age | 1.06 (1.05–1.07) | 1.06 (1.04–1.07) | 1.06 (1.04–1.07) |
| Men | 0.76 (0.65–0.88) | 0.82 (0.69–0.96) | 0.82 (0.69–0.96) |
| Black | 5.09 (4.13–6.28) | 4.96 (3.98–6.18) | 5.02 (4.02–6.27) |
| Education | 0.95 (0.93–0.97) | 0.96 (0.94–0.99) | 0.96 (0.94–0.99) |
| Health Related | |||
| Medical Conditions | 1.12 (1.02–1.22) | 1.11 (1.01–1.21) | |
| Physical Function | 0.96 (0.93–0.98) | 0.96 (0.94–0.98) | |
| Psychosocial | |||
| Depressive Symptoms | 1.04 (0.99–1.08) | ||
| Social Network | 0.99 (0.99–1.01) | ||
| Decline in Episodic Memory | 1.00 (0.93–1.08) | 0.99 (0.91–1.07) | 0.98 (0.90–1.06) |
P < 0.05
Table 3.
Decline in Cognitive Function and Risk of Confirmed Elder Self-Neglect
| Models | Odds Ratio | 95% CI | P value | |
|---|---|---|---|---|
| Global Cognitive Function | A | 1.03 | 0.93–1.14 | 0.58 |
| B | 1.01 | 0.91–1.12 | 0.87 | |
| C | 1.01 | 0.91–1.13 | 0.83 | |
| MMSE | A | 1.00 | 0.99–1.02 | 0.98 |
| B | 1.00 | 0.98–1.02 | 0.88 | |
| C | 1.00 | 0.98–1.02 | 0.68 | |
| Executive Function | A | 1.01 | 1.00–1.01 | 0.06 |
| B | 1.01 | 1.00–1.02 | 0.03 | |
| C | 1.01 | 1.00–1.02 | 0.02 | |
| Episodic Memory | A | 0.99 | 0.92–1.08 | 0.95 |
| B | 0.98 | 0.89–1.07 | 0.63 | |
| C | 0.98 | 0.89–1.07 | 0.61 |
Models: A: Adjusted for age, sex, race, education
B: Adjusted for A + cognitive function, hypertension, diabetes, stroke, cancer, thyroid disease, coronary artery disease
C: Adjusted for B + depressive symptomatology, social network
Decline in Specific Domains of Cognitive Function and Risk of Elder Self-Neglect
Next, we examined the decline in specific domains of cognitive function and the risk of reported elder self-neglect. After adjusting for same above confounders, decline in MMSE score (Table 2, Model C) was not independently associated with increased risk of reported elder self-neglect (OR, 0.99, 95%CI, 0.98–1.04). Decline in episodic memory scores was also not independently associated with increased risk of reported elder self-neglect (OR, 0.98, 95% CI, 0.90–1.06). For confirmed self-neglect, decline in MMSE or episodic memory were not independently associated with increased risk of confirmed elder self-neglect (Table 3, Model C). Decline in executive function scores was independently associated with increased risk of reported elder self-neglect (OR, 1.01, 95%CI, 1.00–1.01) and confirmed elder self-neglect (OR, 1.01, 95% CI, 1.00–1.02).
Self-Neglect Severity and Cognitive Function
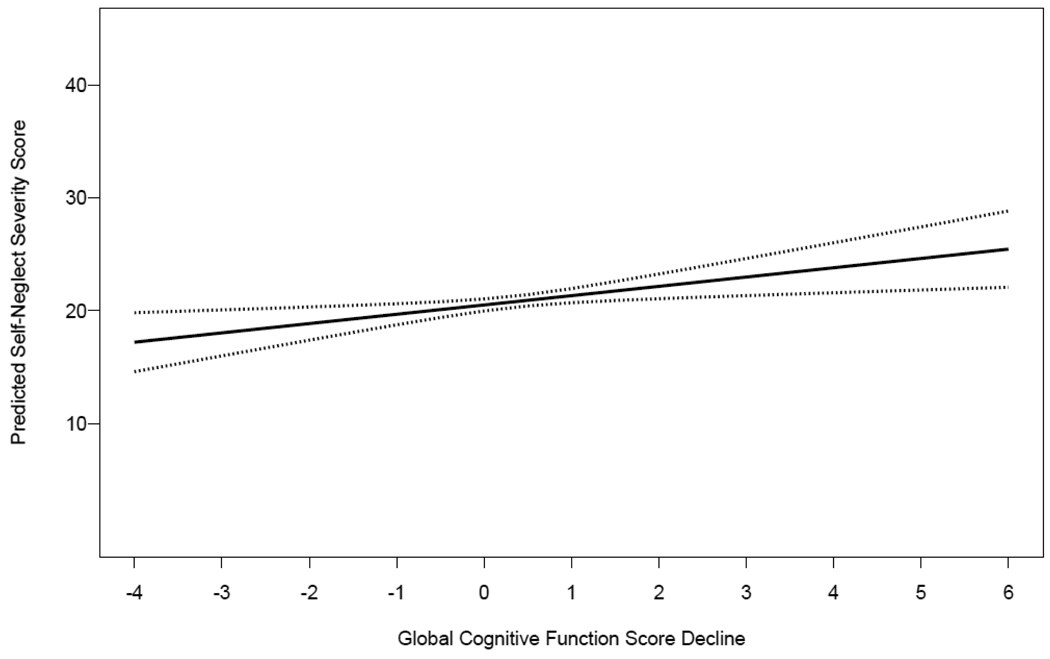
To measure the relations between decline in cognitive function and greater elder self-neglect severity, an initial linear regression model adjusting for age, sex, race and education was created with elder self-neglect severity as the outcome (Table 4, Model A). The coefficient representing the association of elder self-neglect severity and global cognitive function testing was 0.79 (p=0.006), suggesting a statistically significant association between decline in global cognitive function and greater severities of elder self-neglect. However, the association was quite small: after adjustment for the covariates, decline in cognitive function accounted for about 1% of the variability in the composite measure of elder self-neglect severity (increase in adjusted R2 = .015). After adding physical function and medical comorbidities of hypertension, diabetes, stroke, cancer, thyroid disease, and myocardial infarction to the model (Model B), the association remained statistically significant. In the last model (Model C), after adjusting for depressive symptomatology and social network, the coefficient changed minimally and remained statistically significant (Coefficient = 0.76, p=0.014). Figure 1 graphically represents the greater decline in global cognitive function, the higher the risk of greater self-neglect severity in the fully-adjusted model.
Table 4.
Greater Decline in Physical Function and Greater Self-Neglect Severity
| Models | Parameter Estimates | Standard Errors | P value | |
|---|---|---|---|---|
| Global Cognitive Function | A | 0.79 | 0.29 | 0.006 |
| B | 0.67 | 0.31 | 0.028 | |
| C | 0.76 | 0.31 | 0.014 | |
| MMSE | A | 0.09 | 0.04 | 0.042 |
| B | 0.07 | 0.05 | 0.138 | |
| C | 0.07 | 0.05 | 0.155 | |
| Executive Function | A | 0.02 | 0.02 | 0.464 |
| B | 0.02 | 0.03 | 0.409 | |
| C | 0.02 | 0.03 | 0.364 | |
| Episodic Memory | A | 0.53 | 0.24 | 0.028 |
| B | 0.39 | 0.25 | 0.116 | |
| C | 0.45 | 0.25 | 0.077 |
Note: Self-Neglect Severity represents a 1 point increase on the scale of 1–45.
Models: A: Adjusted for age, sex, race, education B: Adjusted for A + cognitive function, hypertension, diabetes, stroke, cancer, thyroid disease, coronary artery disease C: Adjusted for B + depressive symptomatology, social networ
Figure 1. Decline in Global Cognitive Function and Self-Neglect Severity.
Figure 1 demonstrates the association between the decline in global cognitive function score and the predicted self-neglect severity score with the 95% confidence intervals. The overall trend of association between decline in MMSE, executive function and episodic memory and self-neglect severity were not statistically significant.
Note:
Y-Axis: (Predicted Self-Neglect Severity Score) with higher score indicate greater self-neglect severity.
X-Axis: (Global Cognitive Function Score Decline) with higher score indicate the greater decline in the levels of global cognitive function levels.
For the specific domains of cognitive function, in the core models, the decline in MMSE (Coefficient=0.09, p=0.042 and Adjusted R2=0.015) and episodic memory (Coefficient= 0.53, p=0.028 and adjusted R2=0.015) were associated with increased risk of greater self-neglect severity (Table 4: Model A). However, after consideration of health related variable and psychosocial factors, decline in MMSE or episodic memory was not significantly associated with increased risk of greater self-neglect severity.
DISCUSSION
In this prospective population-based study of 5,519 older adults from an urban geographically-defined community, we found that decline in global cognitive function, MMSE or episodic memory was not independently associated with increased risk of elder self-neglect. Decline in executive function was associated with increased risk of elder self-neglect. Decline in the global cognitive function was associated with increased risk of greater self-neglect severity. However, the strength of these associations for self-neglect severity was relatively small accounting for a fraction of variability.
Our findings expand the results of other cross-sectional studies of elder self-neglect and cognitive function. Lachs at al. matched the Connecticut Social Services Agency data to Established Populations for the Epidemiological Studies of the Elderly (EPESE) and found 126 cases of elder self-neglect. In this study (23), cognition was measured using the Pfeiffer Short Portable Mental Status Questionnaire and the authors found that scores ≥ 4 errors out of 10 was significantly associated with elder self-neglect. In a study (24) of 47 cases of elder self-neglect presented to medical center for clinical geriatric comprehensive assessment, author found higher prevalence of dementia (MMSE < 24) (51% vs. 30%, p=0.03). A recent study of a clinical population by Tierney et al (25) conducted more detailed neuropsychological testing on cognitively impaired self-neglectors who lived alone. In their study, cognitive impairment was defined as score of < 131 on the Dementia Rating Scale. MMSE scores in this study also did not predict harmful outcomes among elders who self-neglected themselves. In addition, the authors found that increased risk for harmful outcomes in elder with self-neglect were associated with impairment in recognition memory (HR 0.94, 95% CI, 0.90–0.98), executive function (HR, 1.01, 95% CI, 1.00–1.02) and conceptualization (HR 0.89, 95% CI, 0.81–0.98).
Prior cross-sectional study also suggested the association between lower levels of cognitive function and greater self-neglect severity. Dong and colleagues (30) found that lower levels of global cognitive function (Coefficient = −0.008, p=0.013), perceptual speed (Coefficient = −0.013, p=0.002), or episodic memory (Coefficient = −0.008, p=0.01) was associated with increased risk of greater self-neglect severity. However, the strength of these associations was also quite small. After adjusting for the potential confounders, self-neglect accounted for less than 1% variability in the composite measures of global cognition.
Our present study specifically tested one of the key factors preceding the syndrome of elder self-neglect: decline in cognitive function. Under Dyer’s framework, medical comorbidities, depression, and physical impairment all exacerbate the impairment in cognitive function and specifically executive function, leading to the syndrome of elder self-neglect. In addition, this conceptual framework considered extrinsic issues such as sociodemographic characteristics that may potentially exacerbate the lack of social network. In our present study, after consideration of extensive number of potential contributing factors, decline in executive function remained to be independently associated with elder self-neglect. Executive function is often referred to as frontal lobe function, includes the planning, initiation, organization, self-awareness and execution of tasks. Improved understanding of the relationship between elder self-neglect and levels of executive function could contribute to the causal mechanism to self-neglect. Our study did not provide evidence supporting decline in global cognitive function, MMSE or episodic memory as independent risk factors for elder self-neglect. Future longitudinal studies of other cognitive domains are needed to further explore and validate this framework.
Our findings expand on the results of other studies of self-neglect and cognitive function in a number of different ways. First, our study is the largest population-based study to examine the longitudinal association between cognitive function and elder self-neglect; demonstrating a significant association between decline in executive function and risk of elder self-neglect. The study population is racially/ethnically and socioeconomically diverse and has been well characterized for more than 15 years, which contribute to the potential generalizability of our study findings.
Second, the present study further expands our existing knowledge about association of the specific domains of cognition (executive function and episodic memory) and risk of self-neglect. Future studies are needed to expand more detailed testing of attention/calculation, orientation, memory, language, abstraction and perception. Improved understanding of the relationship between elder self-neglect and these specific cognitive domains could contribute to better understand the causal mechanism to self-neglect.
Third, our study is also the first longitudinal population-based study able to examine the decline in cognitive function with elder self-neglect as a continuum of severity, complementing most prior studies which defined self-neglect as categorically measured (yes or no). Improved understand of the potential gradient associations would contribute to our understanding to the potential causal association between cognitive function and elder self-neglect.
Fourth, even though the present study found a significant statistical association between declines in global cognition with greater self-neglect severity, the strength of association is relatively weak, accounting for only a fraction of variability in self-neglect severity. This finding contrasts with prior studies and set the ground work for future examination of the temporal relations between changes in comprehensively measured cognitive domains and greater self-neglect severity in different populations.
Lastly, MMSE is a commonly used screening test for health care professional and social services agencies and is often used to evaluate older adults to determine the degree of vulnerability and severity of self-neglect. In our study, we did not find any statistically significant association between MMSE and elder self-neglect. This could have potentially important practice implications for health care professionals and social services organization in using MMSE as the only means to screen, detect and manage cases of self-neglect across different severities. Comprehensive cognitive testing and its sub-domains may be warranted to assist professionals in working with older adults with varying severities of self-neglect.
Our study also has a number of limitations. First, self-neglect was not ascertained uniformly for all members of the population, but only for participants referred to the social services agency because someone suspected problems. Self-neglect is under-reported, although the precise rate of under-reporting is unknown. Future study is needed to uniformly collect self-neglect measures in representative population to rigorously examine these associations.
Second, cognitive measures were limited to brief assessments of episodic memory and executive function and the MMSE. Further study need to focus on more comprehensive measure of domains of cognitive function and risk of elder self-neglect. Third, although this study examined cognitive function decline as the predictor of elder self-neglect, it is conceivable that cognitive function decline is an outcome of elder self-neglect. Our cohort did not have sufficient repeated measures of cognitive function after the elder self-neglect report to examine these relationships.
Fourth, this study could not examine the relation between the decline in cognitive function and specific indicators/behaviors of elder self-neglect. Prior study by McDermott and colleagues (McDermott, 2008) suggest that the precise understanding of elder self-neglect phenotypes could further contribute to a clearer conceptual framework for elder self-neglect. Fifth, there are likely to be additional factors (substance abuse, schizophrenia, personality disorders, social support, and etc) not considered in our analyses, which may account for these findings. However, this study sets the foundation for future study of elder self-neglect to fully examine these causal mechanisms.
Conclusion
We conclude that decline in executive function was associated with increased risk of reported or confirmed self-neglect. Although decline in global cognitive function was associated with increased risk of greater self-neglect severity, the association was quite small; accounting for only a fraction of variability. Future longitudinal investigations are needed to explore the potential causal mechanisms between decline in cognitive function and specific phenotypes of elder self-neglect. Future studies will also be necessary to adequately determine the temporal relationships between racial/ethnic and gender differences between the decline in cognitive function and elder self-neglect in the general population.
ACKNOWLEDGMENTS
The authors wish to thank Ms Ann Marie Lane for community development and oversight of project coordination, Ms. Michelle Bos, Ms. Holly Hadden, Mr. Flavio LaMorticella, and Ms. Jennifer Tarpey for coordination of the study. We further thank ZhaoTai Cui, MS, for statistical programming; George Dombrowski, MS, and Todd Beck, MS for data management support.
This work was supported by National Institute on Aging grant (R01 AG11101), Paul B. Beeson Career Development Award in Aging (K23 AG030944), The Starr Foundation, American Federation for Aging Research, John A. Hartford Foundation and The Atlantic Philanthropies.
Sponsor’s Role: None
Footnotes
Conflict of Interest
Drs Dong, Wilson, Simon, Mendes de Leon, Rajan, and Evans declare no conflict of interest.
Author Contributions
Drs. Dong, Wilson, Simon, Mendes de Leon, Rajan and Evans were responsible for the conception and design as well as analysis and interpretation of data. All these authors were involved in the drafting of the manuscript, critical revision of the manuscript and statistical analysis of the manuscript.
REFERENCES
- 1.National Center on Elder Abuse. The National Elder Abuse Incidence Study. Washington, DC: American Public Human Services Association; 1998
- 2.Dong X, Simon M, Mendes de Leon C, et al. Elder Self-neglect and abuse and mortality risk in a community-dwelling population. JAMA. 2009;302:517–526. doi: 10.1001/jama.2009.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Teaster PB. A response to abuse of vulnerable adults: The 2000 survey of state adult protective service. 2002 http://www.ncea.aoa.gov/ncearoot/Main_Site/pdf/research/apsreport030703.pdf 1-16-2006.
- 4.National Center on ELder Abuse Website. NCEA: the basics. 2006 http://elderabusecenter.org/pdf/research/apsreport030703.pdf 6-20-2006.
- 5.Dyer CB, Goodwin JS, Pickens-Pace S, et al. Self-neglect among the elderly: a model based on more than 500 patients seen by a geriatric medicine team. Am J Public Health. 2007;97:1671–1676. doi: 10.2105/AJPH.2006.097113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orem DE. Nursing: Concepts of Practice. 4th edn ed. St Louis, Missouri: Mosby; 1991. [Google Scholar]
- 7.Choi NG, Kim J, Asseff J. Self-neglect and neglect of vulnerable older adults: reexamination of etiology. J Gerontol Soc Work. 2009;52:171–187. doi: 10.1080/01634370802609239. [DOI] [PubMed] [Google Scholar]
- 8.Iris M, Ridings JW, Conrad KJ. The development of a conceptual model for understanding elder self-neglect. Gerontologist. 2010;50:303–315. doi: 10.1093/geront/gnp125. Epub 2009 Sep 2. [DOI] [PubMed] [Google Scholar]
- 9.Dong X, Wilson RS, Mendes de Leon CF, et al. Self-neglect and cognitive function among community-dwelling older persons. Int J Geriatr Psychiatry. 2010;25:798–806. doi: 10.1002/gps.2420. [DOI] [PubMed] [Google Scholar]
- 10.Dyer CB, Franzini L, Watson M, et al. Future Research: A Prospective Longitudinal Study of Elder Self-Neglect. J Am Geriatr Soc. 2008;56:S261–S265. doi: 10.1111/j.1532-5415.2008.01978.x. [DOI] [PubMed] [Google Scholar]
- 11.Paveza G, Vandeweerd C, Laumann E. Elder self-neglect: A discussion of a social typology. J Am Geriatr Soc. 2008;56:S271–S275. doi: 10.1111/j.1532-5415.2008.01980.x. [DOI] [PubMed] [Google Scholar]
- 12.McDermott S. The devil is in the details: self-neglect in Australia. J Elder Abuse Negl. 2008;20:231–250. doi: 10.1080/08946560801973077. [DOI] [PubMed] [Google Scholar]
- 13.Naik AD, Burnett J, Pickens-Pace S, et al. Impairment in Instrumental Activities of Daily Living and the Geriatric Syndrome of Self-Neglect. Gerontologist. 2008;48:388–393. doi: 10.1093/geront/48.3.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pickens S, Naik AD, Burnett J, et al. The utility of the Kohlman evaluation of living skills test is associated with substantiated cases of elder self-neglect. J Am Acad Nurse Pract. 2007;19:137–142. doi: 10.1111/j.1745-7599.2007.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bennett DA, Schneider JA, Bienias JL, et al. Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology. 2005;64:834–841. doi: 10.1212/01.WNL.0000152982.47274.9E. [DOI] [PubMed] [Google Scholar]
- 16.Wilson RS, Bennett DA, Bienias JL, et al. Cognitive activity and incident AD in a population-based sample of older persons. Neurology. 2002;59:1910–1914. doi: 10.1212/01.wnl.0000036905.59156.a1. [DOI] [PubMed] [Google Scholar]
- 17.Kelman HR, Thomas C, Kennedy GJ, et al. Cognitive impairment and mortality in older community residents. Am J Public Health. 1994;84:1255–1260. doi: 10.2105/ajph.84.8.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arfken CL, Lichtenberg PA, Tancer ME. Cognitive impairment and depression predict mortality in medically ill older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M152–M156. doi: 10.1093/gerona/54.3.m152. [DOI] [PubMed] [Google Scholar]
- 19.Ostbye T, Hill G, Steenhuis R. Mortality in elderly Canadians with and without dementia: A 5-year follow-up. Neurology. 1999;53:521–526. doi: 10.1212/wnl.53.3.521. [DOI] [PubMed] [Google Scholar]
- 20.Smits CH, Deeg DJ, Kriegsman DM, et al. Cognitive functioning and health as determinants of mortality in an older population. Am J Epidemiol. 1999;150:978–986. doi: 10.1093/oxfordjournals.aje.a010107. [DOI] [PubMed] [Google Scholar]
- 21.Hui JS, Wilson RS, Bennett DA, et al. Rate of cognitive decline and mortality in Alzheimer's disease. Neurology. 2003;61:1356–1361. doi: 10.1212/01.wnl.0000094327.68399.59. [DOI] [PubMed] [Google Scholar]
- 22.van Gelder BM, Tijhuis MA, Kalmijn S, et al. Decline in cognitive functioning is associated with a higher mortality risk. Neuroepidemiology. 2007;28:93–100. doi: 10.1159/000098552. [DOI] [PubMed] [Google Scholar]
- 23.Abrams RC, Lachs M, McAvay G, et al. Predictors of self-neglect in community-dwelling elders. Am J Psychiatry. 2002;159:1724–1730. doi: 10.1176/appi.ajp.159.10.1724. [DOI] [PubMed] [Google Scholar]
- 24.Dyer CB, Pavlik VN, Murphy KP, et al. The high prevalence of depression and dementia in elder abuse or neglect. J Am Geriatr Soc. 2000;48:205–208. doi: 10.1111/j.1532-5415.2000.tb03913.x. [DOI] [PubMed] [Google Scholar]
- 25.Tierney MC, Snow WG, Charles J, et al. Neuropsychological predictors of self-neglect in cognitively impaired older people who live alone. Am J Geriatr Psychiatry. 2007;15:140–148. doi: 10.1097/01.JGP.0000230661.32735.c0. [DOI] [PubMed] [Google Scholar]
- 26.Dong X, Gorbien M. Decision-Making Capacity: The Core of Self-Neglect. J Elder Abuse Negl. 2005;17:19–36. doi: 10.1300/j084v17n03_02. [DOI] [PubMed] [Google Scholar]
- 27.Bienias JL, Beckett LA, Bennett DA, et al. Design of the Chicago Health and Aging Project (CHAP) J Alzheimers Dis. 2003;5:349–355. doi: 10.3233/jad-2003-5501. [DOI] [PubMed] [Google Scholar]
- 28.Evans DA, Bennett DA, Wilson RS, et al. Incidence of Alzheimer disease in a biracial urban community: Relation to apolipoprotein E allele status. Arch Neurol. 2003;60:185–189. doi: 10.1001/archneur.60.2.185. [DOI] [PubMed] [Google Scholar]
- 29.Dong X, Simon MA, Evans DA. Cross-sectional study of the characteristics of reported elder self-neglect in a community-dwelling population: Findings from a population-based cohort. Gerontology. 2009 doi: 10.1159/000243164. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dong X, Mendes de Leon CF, Evans DA. Is greater self-neglect severity associated with lower levels of physical function? J Aging Health. 2009;21:596–610. doi: 10.1177/0898264309333323. [DOI] [PubMed] [Google Scholar]
- 31.Illinois Department on Aging. Illinois Department on Aging; 1989. Determination of Need Revision Final Report Volume I. [Google Scholar]
- 32.Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971;76:378–382. [Google Scholar]
- 33.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 34.Folstein M, Anthony JC, Parhad I, et al. The meaning of cognitive impairment in the elderly. J Am Geriatr Soc. 1985;33:228–235. doi: 10.1111/j.1532-5415.1985.tb07109.x. [DOI] [PubMed] [Google Scholar]
- 35.Welsh KA, Butters N, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part V. A normative study of the neuropsychological battery. Neurology. 1994;44:609–614. doi: 10.1212/wnl.44.4.609. [DOI] [PubMed] [Google Scholar]
- 36.Albert M, Smith LA, Scherr PA, et al. Use of brief cognitive tests to identify individuals in the community with clinically diagnosed Alzheimer's disease. Int J Neurosci. 1991;57:167–178. doi: 10.3109/00207459109150691. [DOI] [PubMed] [Google Scholar]
- 37.Smith A. Symbol Digit Modalities Test Manual-Revised. Los Angeles: Western Psychological; 1984. [Google Scholar]
- 38.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 39.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 40.Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 41.Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 42.Cornoni-Huntley J, Brock DB, Ostfeld A, et al. Washington, D.C.: US Department of Health and Human Services; Established Populations for Epidemiological Studies of the Elderly Resource Data Book. 1986 (Rep. No. NIH Publication No. 86-2443)