Abstract
Background
Social and communication impairments are core deficits and prognostic indicators of autism. We evaluated the impact of supplementing a comprehensive intervention with a curriculum targeting socially synchronous behavior on social outcomes of toddlers with autism spectrum disorders (ASD).
Methods
Fifty toddlers with ASD, ages 21 to 33 months, were randomized to one of two 6-month interventions: Interpersonal Synchrony or Non-Interpersonal Synchrony. The interventions provided identical intensity (10 hours per week in classroom), student-to-teacher ratio, schedule, home-based parent training (1.5 hours per month), parent education (38 hours), and instructional strategies, except the Interpersonal Synchrony condition provided a supplementary curriculum targeting socially engaged imitation, joint attention, and affect sharing; measures of these were primary outcomes. Assessments were conducted pre-intervention, immediately post-intervention, and, to assess maintenance, at six-month follow-up. Random effects models were used to examine differences between groups over time. Secondary analyses examined gains in expressive language and nonverbal cognition, and time effects during the intervention and follow-up periods.
Results
A significant treatment effect was found for socially engaged imitation (p=0.02), with more than doubling (17% to 42%) of imitated acts paired with eye contact in the Interpersonal Synchrony group after the intervention. This skill was generalized to unfamiliar contexts and maintained through follow-up. Similar gains were observed for initiation of joint attention and shared positive affect, but between-group differences did not reach statistical significance. A significant time effect was found for all outcomes (p<0.001); greatest change occurred during the intervention period, particularly in the Interpersonal Synchrony group.
Conclusions
This is the first ASD randomized trial involving toddlers to identify an active ingredient for enhancing socially engaged imitation. Adding social engagement targets to intervention improves short-term outcome at no additional cost to the intervention. The social, language, and cognitive gains in our participants provide evidence for plasticity of these developmental systems in toddlers with ASD. http://www.clinicaltrials.gov/ct2/show/NCT00106210?term=landa&rank=3
Keywords: Autistic Disorder, Intervention
Autism spectrum disorders (ASDs) are defined by the presence of social and communication impairments that appear early in life and persist into adulthood (Howlin, Goode, Hutton, & Rutter, 2004; Landa, Holman, & Garrett-Mayer, 2007). Yet many behaviorally-based interventions are associated with improvement in cognitive, behavioral, and language impairments for children with ASD (Rogers & Vismara, 2008), suggesting plasticity in these aspects of development, particularly when intervention is begun early (Drew et al., 2002; Harris & Handelman, 2000). Despite evidence that ASD can be diagnosed reliably in two-year olds (Chawarska, Klin, Paul, & Volkmar, 2007), only a few intervention studies, mostly with small sample sizes, have been published involving this age group, and most have relied on descriptive or quasi-experimental approaches. The present study examined the effects of a hypothesized active ingredient within a behavioral intervention targeting socially synchronous behavior on outcome measures of socially engaged imitation, joint attention, and affect sharing in 2-year-olds with ASD. These core social deficits interfere with children’s ability to establish and maintain synchronous, reciprocal engagement with others and thus, compromise prognosis.
Social and communication impairments that distinguish ASD from typical development and developmental delay include abnormality in affect expression, initiation of communication, reciprocity in interaction, social/affective signaling, joint attention, symbolic behavior, motor imitation, language understanding, and conventional use of gestures (Charman et al., 1997; Landa, Holman, & Garrett-Mayer, 2007; Rogers, Hepburn, Stackhouse, & Wehner, 2003; Wetherby, Watt, Morgan, & Shumway, 2007). These impairments, which emerge early in typical development, form a weak foundation for the ability to establish and maintain synchronous, reciprocal engagement with others. Thus, young children with ASD who elicit only infrequent, brief epochs of engagement with others limit opportunities for language and social learning. For this reason, the present study focused on effects of directly targeting socially engaged imitation, joint attention, and affect sharing.
While social impairments are central to autism, only three peer-reviewed intervention studies identified social improvements in 2-year-olds with ASD. In their descriptive study of 20 2-year-olds enrolled in a classroom-based, multi-instructional method intervention, Stahmer, Ingersoll, and Koegel (2004) identified improvements in some children’s tolerance of proximity to peers, response to others’ initiations, and engagement in reciprocal interaction after a mean of 9.7 months of intervention. In their description of a parent-mediated intervention for young children with ASD, Chandler, Christie, Newson, and Prevezer (2002) reported improved social interest in all 18 participants, but details were not provided about the magnitude of change nor how it was measured. In another parent-mediated intervention, Schertz and Odom (2007) reported improvement in two of three children’s response to others’ joint attention bids and initiation of joint attention.
Two RCTs involving very young children with ASD reported lack of social improvement. Drew and colleagues (2002) found no social gains after about one year of intervention on a parent interview measure in two groups of nearly 2-year-olds enrolled in a parent training (plus local services) or a local services only group (Drew et al., 2002). Dawson and colleagues (2009) reported a negative change in Vineland Adaptive Behavior Scales Socialization domain standard score (Sparrow, Balla, & Cicchetti, 1984) and lack of improvement in severity scores from the Autism Diagnostic Observation Schedule (ADOS; Lord, Rutter, DiLavore, & Risi, 1999) after two years of intervention in 23-month-olds receiving either the Early Denver Model (20 hours per week of 1:1 therapist-mediated in-home intervention) or local services.
The mixed evidence for social improvement in young children with ASD highlights the need for research to determine whether toddlers with ASD can show gains in core social deficit domains such as socially engaged imitation, joint attention and affect sharing, and to examine the stability of these gains post intervention. Perhaps other aspects of development, such as language and nonverbal cognition, are more plastic than social functioning in early development of children with ASD. This possibility is supported by reports of expressive language gains in both RCTs cited above (Dawson et al., 2009; Drew et al., 2002) and of modest gains in nonverbal cognition reported by Dawson and colleagues (2009).
The preliminary evidence of social and language improvement following early intervention for ASD highlights the importance of designing early therapeutic opportunities to practice joint processing of self-other experiences within social communicative exchanges. According to Mundy, Sullivan, and Mastergeorge (2009), joint processing of one’s own and others’ actions and objects of attention gives way to an automaticity that is likely fundamental to symbolic and social cognitive learning. Thus, early intervention that directly targets the development of socially engaged imitation, joint attention and affect sharing could have potent effects on later language, play and social outcomes (Bono, Daley, & Sigman, 2004; Sigman & Ruskin, 1999; Toth, Munson, Meltzoff, & Dawson, 2006).
The present RCT examined the effects of a hypothesized active intervention ingredient targeting social development in toddlers with autism. We compared two groups receiving identical intervention where one group received a supplemental social curriculum. The primary question addressed was: is there a difference in outcome measures of socially engaged imitation, joint attention, and shared positive affect in children receiving this supplementary curriculum? Secondary questions addressed were: (1) do children who receive the supplementary social curriculum show differential growth in expressive language and nonverbal cognitive functioning; and (2) do children maintain the gains established during intervention throughout a 6-month follow-up period?
Methods
This study was registered with a Data Safety and Monitoring Board at the National Institutes of Health and was approved by the Johns Hopkins Medical Institutional Review Board; all families gave written informed consent for their child’s participation.
Participants
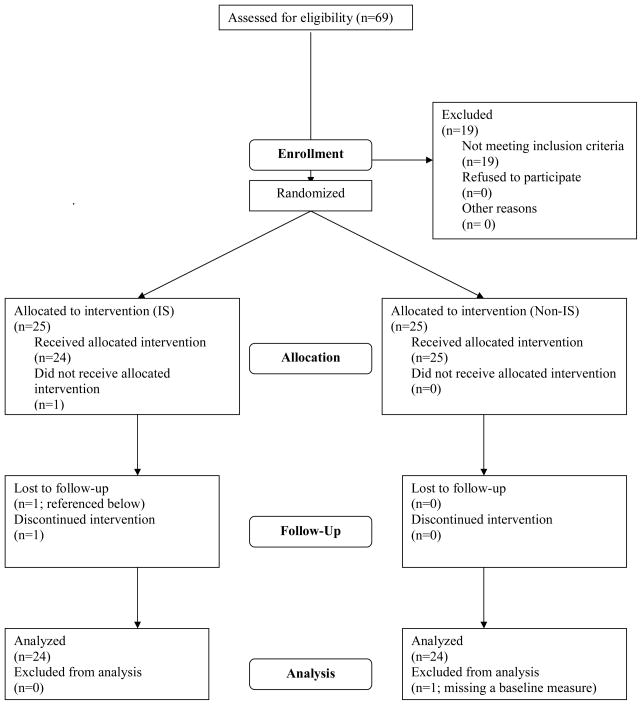
Fifty two-year-olds diagnosed with ASD were randomized to one of the two intervention conditions. A supplementary social curriculum was implemented in the Interpersonal Synchrony (IS) condition, but not within the comparison Non-Interpersonal Synchrony (Non-IS) condition. Analyses were conducted on a final sample of 48 children (IS n=24; Non-IS n=24). One child was withdrawn by his parents to enroll in a program for children with typical development and one child was missing a primary baseline variable (Figure 1).
Figure 1.
Consort table flowchart.
Participants were recruited through Kennedy Krieger Institute’s Center for Autism and Related Disorders, advocacy groups, conferences, Infants and Toddlers programs, physician’s offices, and word-of-mouth. Eligibility criteria included: meeting criteria on the ADOS for ASD or autism and receiving a diagnosis of ASD by an expert clinician; chronological age between 21 and 33 months; non-verbal mental age of at least 8 months (per Mullen Scales of Early Learning [MSEL; Mullen, 1995] Visual Reception [VR] scale); having no siblings with ASD (to avoid confounds introduced by some parents having more skills in treatment delivery within the home); primary language spoken within the home was English; and no known etiology for ASD. Inter-rater reliability of diagnosis was examined for 9 (18%) cases; agreement was 100%. Type and intensity of other interventions received by participants were documented via parent report during monthly home visits.
Prior to randomization, children were placed into matched pairs based on MSEL Receptive Language and VR T scores and ADOS Social Interaction algorithm scores. Within each pair, one child was randomly selected for the IS group. Table 1 shows that there were no group differences in socioeconomic status (Hollingshead, 1975) scores (p=0.741), proportion of non-Caucasian participants (p=0.94), or amount of outside speech-language treatment during the intervention (p=0.268) or during the follow-up period (p=0.696). There was no correlation between number of hours of outside speech-language treatment and change in MSEL Receptive or Expressive Language T score from pre- to post-test (r=−0.233, r=−0.236, respectively).
Table 1.
Subject characteristics at start of intervention for Interpersonal Synchrony (IS) and Non-Interpersonal Synchrony (Non-IS) groups
| Characteristic | IS Group (n=24) | Non-IS Group (n=25) | P value |
|---|---|---|---|
| Demographic, n (%) | |||
| Male | 20 (83.3) | 20 (80) | 1.0 |
| Caucasian | 19 (79.2) | 20 (80) | 0.94 |
| Chronological age at start of tx (mos.), M (sd) | 28.6 (2.6) | 28.9 (2.8) | 0.648 |
| Hollingshead SES score, M (sd) | 54.7 (8.7) | 53.8 (10.2) | 0.741 |
| # hrs of Speech Language tx (pre to post) | 24.45 (19.38) | 21.72 (15.95) | 0.268 |
| # hrs of Speech Language tx (post to follow-up) | 28.07 (27.01) | 24.95 (19.24) | 0.696 |
Intervention Procedures
Intervention was provided within a Kennedy Krieger classroom four days per week for 2.5 hours per day for six months. The IS and Non-IS groups received a mean (standard deviation) of 205.66 (18.63) and 196.21 (28.4) hours of classroom-based intervention, which was not significantly different (p=0.17). Student to interventionist ratio was 5:3. One interventionist was employed in both classrooms and was instructed not to discuss differences with the other interventionists.
Instructional strategies for both conditions represented a continuum of adult-imposed structure ranging from discrete trial teaching (Lovaas, 1987) to pivotal response training (Koegel et al., 1989) to routines-based interactions. Low-tech augmentative communication systems were used as needed. Visual cues (Carr, Binkoff, Kologinsky, & Eddy, 1978) and visually-based organizational strategies (Lord, Bristol, & Schopler, 1993) were provided.
Within both conditions, highly motivating intervention tasks, materials, and natural consequences were designed to elicit frequent child-initiated intentional communication and diverse object play, where interventionists followed the child’s attentional lead and provided expansions of language and play behavior. Interventionists made relevant cues (e.g., for language referents) salient through environmental arrangements, use of brief utterances, and use of linguistic mapping during child attention and engagement with objects and people.
The curriculum used within both conditions was the Assessment, Evaluation, and Programming System for Infants and Children (AEPS; Bricker, 2002), a comprehensive developmental curriculum that provides guidelines for complexity of intervention goals based on children’s individual developmental profile. While the AEPS included goals for joint attention and imitation, the IS group received many more orchestrated opportunities to respond to and initiate joint attention, imitate others during social interaction, and share positive affect, with interventionists enticing and modeling social targets, prompting as needed. More discrete breakdown of social targets than was presented within the IS than the AEPS curriculum. The IS physical learning environment presented frequent ecologically valid opportunities for initiating and responding to joint attention to proximal and distal objects, people, and events (e.g., placing thematically relevant objects or pictures on walls; creating socially enticing surprise events), and for sharing positive affect (e.g., activities involving imitation of peers and adults performing silly and engaging actions with objects).
Identical parent education classes (38 hours) focusing on strategies for enhancing child development (using simple language, imitating child’s actions with toys, establishing joint action routines), coping, behavior management strategies, and advocacy were provided in both groups. Home-based parent training sessions (1.5 hours per month for six months) focused on strategies for improving communication, adaptive, and self-regulation skills within daily living activities. Both groups received the same amount of parent training, as all cancelled sessions were rescheduled. These were modeled by the interventionist, then parents were coached while implementing the strategies with their children. Parents observed the classroom twice weekly.
Measures
Fidelity
Sixty four videotapes from a random set of sessions were coded for frequency of the following ten IS teaching behaviors: language paired with pointing gesture; hand-over-hand pointing; showing; modeling facial expression; labeling facial expression; imitation of child action; verbal label of imitated action; hand-over-hand imitation; modeling gesture; and modeling positive affect. Interventionists were videotaped on average twice during each intervention session and were blind as to whether videotaping was being conducted for purposes of coding children’s behavior or fidelity. Two trained and reliable staff, one being blind to intervention condition, coded 45 minutes of instructional activities. Significantly more IS instruction was provided by IS than Non-IS interventionists (p’s=0.047 to <0.001). Inter-observer reliability was assessed for 27% (n=17) of coded video tapes; intraclass correlation coefficients (ICC) ranged from 0.79 to 0.97.
Outcome
Children were assessed at baseline (pre-test), termination of the intervention (post-test), and at a six-month follow-up within the Autism Center’s Child Development Laboratory by a clinician blind to group membership and unfamiliar to the child.
Primary outcome variables
Initiation of joint attention (IJA) and shared positive affect (SPA) were measured using the Communication and Symbolic Behavior Scales Developmental Profile (Wetherby & Prizant, 2002), which presents communication temptations and collects a play sample using a standardized toy set. ICCs for frequency of IJA and SPA calculated on 20% (n=28) of videotaped sessions were 0.952 and 0.999, respectively.
Socially engaged imitation (SEI) was defined as proportion of imitations paired with eye contact to the examiner. SEI was coded blind to group membership or time point from videotapes of a structured imitation task, modified from that described by Rogers and colleagues (2003). Examiners modeled 15 novel facial, manual, and object manipulation movements, providing two response opportunities per movement, as children were instructed to “Do this”. ICC calculated on 15 (12%) videotapes was 0.956.
Secondary outcome variables
The MSEL Expressive Language (EL) and VR (estimate of nonverbal cognition) T scores (mean=50; sd=10) were secondary outcome variables. The MSEL is a developmental test standardized for ages 3 to 69 months.
Data Analysis
T-tests and chi-square tests assessed group comparability at baseline. Random effects models (hierarchical linear or multilevel models; Laird & Ware, 1982) were used to model each outcome over time. This longitudinal model, with a child-level random effect, permitted use of all observations available for each child while accounting for the correlation of observations within each child. The model included a factor for time (allowing growth during intervention and follow-up periods to differ), a group (IS/Non-IS) indicator, and a group by time interaction as predictors. This model allowed us to test for between-group differences at post-test and follow-up and between their growth rates. To account for chance differences between groups at pre-test and increase precision, the model also controlled for pre-test values of each outcome variable, ADOS algorithm combined Communication and Social Interaction scores (a measure of autism severity), and MSEL Receptive Language T scores. Models were estimated using xtmixed in Stata 10 (StataCorp, 2007). Effect sizes were calculated using Cohen’s d (Cohen, 1988), using the pre-test pooled standard deviation. Effect sizes reflect the regression adjustment, which controls for pre-test characteristics of the children. Significance level for all comparisons was set at p=0.05.
The effects estimated are intent-to-treat effects, which estimate the effect of assignment to the IS intervention, regardless of the amount of intervention actually received. We analyzed data from all individuals originally assigned to an intervention group, with the exception of one child in the Non-IS group who was missing a pre-intervention IJA value. Two children were missing an outcome variable at post-test or follow-up. Standard errors reflect occasional missing outcome values.
Results
Pre-intervention Equivalence of Groups
T-tests and chi-square tests revealed no between-group differences on any of the dependent variables at pre-test (p’s=0.239 to 0.924), indicating well-matched groups (see Table 1).
Main Effects of Intervention on Primary Outcome Variables
The joint tests of differences involved an overall between-group comparison for each primary outcome (SEI, IJA, SPA). A statistically significant overall main effect was found for SEI (chi-square 9.98, df=3, p=0.02; Table 2), but not for IJA (chi-square=365, df=3, p=0.30) or SPA (chi-square=2.61, df=3, p=0.46). Subsequent between-group comparisons at post-test and follow-up revealed significantly more SEI performed by the IS than Non-IS group at follow-up (p=0.01; d=0.86). Analysis of between-group differences in slopes (rates of growth) within each assessment period revealed differences in SEI growth during the intervention period (p=0.04; Table 3) but not during follow-up (p=0.24). Between-group comparisons of IJA and SPA at post-test and follow-up revealed a trend toward significance for more frequent IJA at post-test (p=.08, d=0.89) and follow-up (p=.07, d=1.56) in the IS group. Lack of significance on the joint test for IJA could be related to the significantly larger variance within the IS group for IJA at follow-up (p<0.001).
Table 2.
Outcome differences between IS and non-IS groups
| Pre-test | Post-test | Follow-up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-IS | IS | Diff. | Non-IS | IS | Diff. | Non-IS | IS | Diff. | Joint test of intervention group differences | Joint test of time effect | |
| Outcome | Mean (SD) | Mean (SD) | Effect size (p-value) | Mean (SD) | Mean (SD) | Effect size (p-value) | Mean (SD) | Mean (SD) | Effect size (p-value) | p-value | p-value |
| Primary outcomes | |||||||||||
| SEI | .25 (.24) | .17 (.19) | −.29 (.30) | .35 (.23) | .42 (.24) | .48 (.11) | .28 (.21) | .44 (.22) | .86 (.01)* | .02* | <.001* |
| IJA | 2.79 (3.62) | 2.29 (3.16) | −.04 (.89) | 5.00 (7.91) | 7.70 (9.33) | .89 (.08) | 4.42 (4.82) | 8.83 (13.22) | 1.56 (.07) | .30 | <.001* |
| SPA | 3.54 (3.56) | 2.42 (2.93) | −.41 (.31) | 5.33 (6.64) | 6.87 (7.55) | .42 (.41) | 4.96 (5.48) | 7.57 (9.76) | .81 (.27) | .46 | .01* |
| Secondary Outcomes | |||||||||||
| EL T | 25.92 (8.12) | 23.92 (5.50) | −.11 (.71) | 31.92 (13.67) | 34.08 (14.59) | .49 (.18) | 31.36 (12.12) | 34.52 (12.33) | .57 (.24) | .44 | <.001* |
| VR T | 31.12 (9.86) | 27.50 (8.27) | −.27 (.26) | 32.24 (14.07) | 36.75 (14.54) | .57 (.07) | 30.28 (16.62) | 34.44 (16.67) | .46 (.33) | .16 | <.001* |
Effect sizes in Tables 2 and 3 were calculated for each outcome by standardizing the regression-adjusted difference between IS and Non-IS groups by the pooled (IS and Non-IS) standard deviation at pre-test: SEI = 0.21; IJA = 3.33; SPA = 3.19; EL T = 6.82; VR T = 8.93. Regression incorporates adjustment for pre-test values of each outcome variable and other predictors as detailed in the text.
Table 3.
Exploratory analyses: within-group and between-group comparisons of growth rate (slopes)
| Non-IS Group | IS Group | Difference between IS and Non-IS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Pre-test to post-test | Post-test to follow-up | Change in slopes | Overall time effect | Pre-test to post-test | Post-test to follow-up | Change in slopes | Overall time effect | Pre-test to post-test | Post-test to follow-up |
| Effect size (p-value) | Effect size (p-value) | Effect size (p-value) | p-value | Effect size (p-value) | Effect size (p-value) | Effect size (p-value) | p-value | Effect size (p-value) | Effect size (p-value) | |
| Primary outcomes | ||||||||||
| SEI | .48 (.06) | −.33 (.17) | −.81 (.05)* | .13 | 1.19 (.00) | .05 (.78) | −1.14 (.01)* | <.001* | .76 (.04)* | .43 (.24) |
| IJA | .66 (.10) | −.34 (.42) | −1.00 (.05)* | .13 | 1.59 (.00) | .34 (.41) | −1.25 (.02)* | <.001* | .93 (.11) | .68 (.25) |
| SPA | .56 (.19) | −.18 (.68) | −.74 (.25) | .40 | 1.39 (.00) | .22 (.62) | −1.18 (.07) | .01* | .83 (.17) | .41 (.52) |
| Secondary outcomes | ||||||||||
| EL T | .89 (.02)* | −.10 (.73) | −.99 (.02)* | .01* | 1.49 (.00)* | −.01 (.97) | −1.50 (<.001)* | .00* | .60 (.13) | .09 (.83) |
| VR T | .20 (.44) | −.23 (.37) | −.43 (.25) | .51 | 1.04 (.00)* | −.34 (.20) | −1.37 (<.001)* | .00* | .84 (.02)* | −.10 (.78) |
Secondary Analyses
To further inform the sparse intervention literature on language, cognitive, and social growth in toddlers with ASD, we performed two sets of secondary analyses involving: (a) examination of secondary outcomes of expressive language and nonverbal cognition; and (b) examination of growth over time (slopes) on the entire sample and then within groups.
Effects of intervention on secondary outcome variables
Joint tests of differences did not reveal overall between-group differences on EL or VR T scores (chi-square=2.71, df=3, p=0.44 for EL; chi-square=5.24, df=3, p=0.16 for VR), despite moderate effect sizes at post-test of 0.57 and 0.49, respectively, and at follow-up of 0.46 and 057, respectively (Table 2). A marginal treatment effect was found for VR T score, with a trend toward higher levels of nonverbal cognition at post-test for the IS group (p=0.07; Table 2), a result of greater growth during the intervention period for the IS group (p=0.02; Table 3). However, these VR trends should be interpreted with caution due to the lack of significance of the joint test of differences (p=0.13).
Growth over time
Examining growth over time permits an understanding of the timing, rate, and direction (increasing, decreasing) of change, permitting insight into whether intervention gains were sustained after termination of the intervention. Separate joint tests of difference were conducted for each outcome to examine overall growth trends for the entire sample from pre-test to follow-up. Significant time effects were found for the full sample for all variables (p’s=0.00 to 0.01; Table 2), indicating improving performance over time.
Next, we examined growth trends of the two groups separately to better understand whether growth for each group during the intervention phase was maintained during follow-up. Table 3 examines whether slopes within the intervention and follow-up periods differed for each group. The IS group showed significant growth over time on every outcome (p’s<0.01) while the Non-IS group showed significant growth only on the EL T score (p=0.01). Further analyses compared growth during the intervention period to growth within the follow-up period within each group. For all outcomes except for SPA (p=0.07), the IS group had significantly more rapid growth in the intervention period than in the follow-up period (p’s ≤0.001). The effect sizes for the IS group’s growth during the intervention period were all over 1 and all reached significance (p<0.001). In contrast, effect sizes for the IS group’s growth during the follow-up period, while not receiving our intervention, ranged from −0.34 for VR T score to 0.34 for IJA, with none being statistically significant. The Non-IS group showed significant growth during the intervention period only for EL T score (p=0.02), with no significant growth detected on any variable during follow-up.
Discussion
To our knowledge, this is the first RCT involving two-year-olds designed to assess effects of an intervention ingredient on social development. We compared change in self-initiated socially engaged behavior in two groups receiving comparable treatments, differing only in the presence or absence of a supplementary social curriculum targeting SEI, IJA, and SPA, which are core deficits of autism. The test of SEI, IJA, and SPA outcome was stringent, reflecting generalization of these behaviors to a novel interaction context (location and materials), with an unfamiliar examiner, under unfamiliar circumstances (activity). Significant treatment effects were found for SEI at follow-up, with a trend toward significance for IJA at post-test and follow-up. Moderate effect sizes for SEI and IJA provide preliminary evidence for the efficacy of this intervention where a supplementary curriculum for social initiation and socially synchronized engagement in toddlers is overlaid on an existing group-based comprehensive intervention. A trend toward significance was found for greater improvement in the secondary variable of nonverbal cognition within the IS group during the intervention period. Trends toward significance for IJA and nonverbal cognition should be interpreted with caution since the joint tests for intervention differences was not significant for these outcomes. Secondary analyses also revealed social, cognitive, and language gains in both groups, particularly during the 6-month intervention period and within the IS group.
Our findings provide insights into the plasticity of social and communication development in toddlers with ASD. The supplementary curriculum activated development of socially engaged imitation (a greater than two-fold increase from pre- to post-test) that generalized across people, location, and interaction context. While others have reported improvements in imitation performance following targeted instruction (Ingersoll & Schreibman, 2006), this is the first study to identify a targeted treatment response involving gains in the integration of imitation with socially directed gaze. Such ability enables toddlers with ASD to liken themselves to peers while also signaling their interactive engagement. This could foster a cascade of events in which toddlers with ASD draw increasing social, play, and language learning opportunities to themselves. Future research is needed to determine whether toddlers with ASD who develop SEI learn more efficiently or implicitly within other domains of development since imitation is a vital avenue through which language and play learning occurs (Ingersoll & Schreibman, 2006; Speidel & Nelson, 1989).
The finding that both groups made significant gains over time in primary as well as secondary outcomes is of interest. The absence of more robust between-group differences is likely attributable to the similarity between the rival interventions. Instructional strategies for both interventions emphasized self-initiated communication, child choice, motivating learning materials and activities, joint action routines, natural reinforcers, and play-based learning activities. Some of these strategies are vital ingredients for development of flexible and generative language in typically developing children (Barsalou, Breazeal, & Smith, 2007; Booth & Waxman, 2002). In addition, the AEPS curriculum includes imitation and joint attention goals, albeit in less detail than in the IS curriculum. The high level of child-other engagement within the ecologically valid learning contexts of both interventions may have been sufficient to activate a high level of affect sharing and joint attention even without the additional infusion of instruction targeting joint attention and affect sharing. Indeed, Kasari et al. (2008) reported significant gains in joint attention behavior in preschoolers with ASD regardless of whether they received instruction focused on symbolic play or joint attention. Kasari et al.’s (2008) and our findings indicate that development of IJA and affect sharing may be stimulated through targeting interactions involving a joint focus of attention within motivating activities where children’s self-generated initiation is targeted. Our finding that slopes became less steep in the IS group or decreased in the Non-IS group during follow-up suggests the need for ongoing intervention targeting social development, and possibly that the community-based interventions did not sufficiently address these aspects of development. It also indicates that the IS group did not lose the skills acquired during the intervention. Further research is needed to understand more about the intervention ingredients that stimulate social development in toddlers with ASD, and to identify characteristics of children who show limited social improvement.
The gains in our participants’ expressive language and nonverbal cognitive functioning are encouraging. Since we did not include an “assess and monitor” control group, we cannot conclusively infer that these gains were effected by the overall intervention program common to both groups. However, there is indirect evidence for the intervention’s developmental impact. First, the most rapid growth in development occurred during the 6-month active intervention period.
The second source of indirect evidence is found in other published reports. In Dawson and colleagues’ (2009) RCT involving 2-year-olds with ASD receiving either 20 hours per week of 1:1 home-based Early Denver Model intervention or referral to community intervention providers, gains in MSEL EL and VR T scores for the Early Denver and community intervention groups, after one year of intervention, were nearly identical to gains observed in our IS and Non-IS groups, respectively, from pre-test through follow-up (measured 6 months after the termination of treatment) on these same variables. Although Dawson and colleagues did not include social variables comparable to those reported herein, the expressive language and nonverbal cognition results from their study and ours indicate that toddlers with ASD are able to make substantial gains in early intervention using well-defined responsive instructional strategies and developmentally-based curriculum. Furthermore, our data indicate that such gains may be effected in a relatively brief period of time. Numerous intervention studies involving preschoolers with ASD have also reported gains in nonverbal cognition and language (reviewed by Rogers & Vismara, 2008); these aspects of development may be particularly plastic and responsive to early intervention.
The present study contributes to a small body of literature focused on core deficits of communication and social functioning in young children with autism. Given the pervasive nature of imitation, joint attention and affect sharing deficits in most young children with ASD (Kasari, Freeman, & Paparella, 2006; Landa et al., 2007; Sullivan et al., 2007), and given that early social development is a major predictor of outcome for children with ASD (Charman et al., 2003; Sigman & Ruskin, 1999), there is a vital need to extend the research on which we report here. Future research should include a focus on whether and how an intervention such as the one reported here might impact parent-child interaction, and thus, mediate intervention effects.
Conclusions
This is the first RCT to identify a developmental social curriculum as an active ingredient for improving socially engaged imitation in toddlers with ASD. This effect was obtained by layering a supplementary social curriculum onto an intervention that utilized a well-defined developmental curriculum and integrated several evidence-based instructional strategies. Thus, an incremental benefit was achieved at no extra cost. The results highlight the need for future investigation of scalable early intervention models targeting core deficits of ASD and that examine factors related to generalization and maintenance of early social, communication, and cognitive skills.
Key Points.
Autism intervention studies have focused largely on children age 3 and older. No randomized controlled trials (RCTs) have shown evidence for improvement in core social deficits of autism in toddlers with ASD.
This is the first RCT involving two-year-olds with ASD to assess the efficacy of an intervention ingredient targeting core social deficits of autism.
Our findings indicate that toddlers with ASD improve in socially engaged imitation in response to a targeted curriculum and intervention activities. Significant improvements in expressive language, cognitive, and social functioning occurred in both intervention groups.
Early intervention for ASD should target social abilities as part of a comprehensive intervention program.
Acknowledgments
We wish to thank the children and parents who participated in this study. We also thank the superb staff who provided the intervention, administrative support, and data processing: Jessica Henkin, Katrina Martin, Dana Herman, James Mancini, Ashley Edmunds, Sarah Beal, Amy Knecht, Amy Falk Smith, Marguerite Adams, Allison Nelson, Dr. Michelle Sullivan, Dr. Julie Cleary, and Andrea Golloher. We also thank Dr. Laura Schreibman for training the staff on Pivotal Response Training and for her ongoing quality assurance assessments during the study. Thanks also to Ashley Faherty, Dr. David Mandell, and Dr. Jeffery Wood for their assistance in edits to this manuscript.
Funding/Support: Rebecca Landa (PI) thanks the National Institute of Mental Health (154MH066417; STudies to Advance Autism Research and Treatment) and HRSA (R40 MC 15594) for the funding to conduct this study and prepare this manuscript.
Abbreviations
- IS
Interpersonal synchrony
- IJA
Initiation of joint attention
- SEI
Socially engaged imitation
- SPA
Shared positive affect
- MSEL
Mullen Scales of Early Learning
- VR
Visual Reception
- EL
Expressive Language
Contributor Information
Rebecca J. Landa, Kennedy Krieger Institute, Center for Autism and Related Disorders Johns Hopkins University School of Medicine, Department of Psychiatry and Behavioral Sciences
Katherine C. Holman, Towson University, Department of Special Education
Allison H. O’Neill, University of Maryland School of Public Health, Department of Epidemiology and Biostatistics
Elizabeth A. Stuart, Johns Hopkins Bloomberg School of Public Health, Departments of Mental Health and Biostatistics
References
- Barsalou L, Breazeal C, Smith L. Cognition as coordinated non-cognition. Cognitive Processing. 2007;8:79–91. doi: 10.1007/s10339-007-0163-1. [DOI] [PubMed] [Google Scholar]
- Bono M, Daley T, Sigman M. Relations among joint attention, amount of intervention, and language gain in autism. Journal of Autism and Developmental Disorders. 2004;34:495–505. doi: 10.1007/s10803-004-2545-x. [DOI] [PubMed] [Google Scholar]
- Booth A, Waxman S. Object names and object functions serve as cues to categories for infants. Developmental Psychology. 2002;38:948–957. doi: 10.1037//0012-1649.38.6.948. [DOI] [PubMed] [Google Scholar]
- Bricker D. Assessment, Evaluation, and Programming System for Infants and Children: Birth to Three Years. 2. Baltimore, MD: Brookes Publishing; 2002. [Google Scholar]
- Carpenter M, Nagell K, Tomasello M. Social cognition, joint attention, and communicative competence from 9 to 15 months of age. Monographs of the Society for Research in Child Development. 1998;63:1–176. [PubMed] [Google Scholar]
- Carr EG, Binkoff JA, Kologinsky E, Eddy M. Acquisition of sign language by autistic children. I: Expressive labeling. Journal of Applied Behavior Analysis. 1978;11:489–501. doi: 10.1901/jaba.1978.11-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler S, Christie P, Newson E, Prevezer W. Developing a diagnostic and intervention package for 2- to 3-year-olds with autism: Outcomes of the frameworks for communication approach. Autism. 2002;6:47–69. doi: 10.1177/1362361302006001005. [DOI] [PubMed] [Google Scholar]
- Charman T, Baron-Cohen S, Swettenham J, Baird G, Drew A, Cox A. Predicting language outcome in infants with autism and pervasive developmental disorder. International Journal of Language and Communication and Disorders. 2003;38:265–285. doi: 10.1080/136820310000104830. [DOI] [PubMed] [Google Scholar]
- Charman T, Swettenham J, Baron-Cohen S, Cox A, Baird G, Drew A. Infants with autism: An investigation of empathy, pretend play, joint attention, and imitation. Developmental Psychology. 1997;33:781–789. doi: 10.1037//0012-1649.33.5.781. [DOI] [PubMed] [Google Scholar]
- Chawarska K, Klin A, Paul R, Volkmar F. Autism spectrum disorder in the second year: Stability and change in syndrome expression. Journal of Child Psychology and Psychiatry. 2007;48:128–138. doi: 10.1111/j.1469-7610.2006.01685.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, Donaldson A, Varley J. Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver model. Pediatrics. 2009;125:17–23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew A, Baird G, Baron-Cohen S, Cox A, Slonims V, Wheelwright S, Swettenham J, Berry B, Charman T. A pilot randomized control trial of a parent training intervention for pre-school children with autism: preliminary findings and methodological challenges. European Child & Adolescent Psychiatry. 2002;11:266–272. doi: 10.1007/s00787-002-0299-6. [DOI] [PubMed] [Google Scholar]
- Happe F, Frith U. The neuropsychology of autism. Brain: A Journal of Neurology. 1996;119:1377–1400. doi: 10.1093/brain/119.4.1377. [DOI] [PubMed] [Google Scholar]
- Harris S, Handelman J. Age and IQ at intake as predictors of placement for young children with autism: A four- to six-year follow-up. Journal of Autism and Developmental Disorders. 2000;30:137–142. doi: 10.1023/a:1005459606120. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social position. New Haven, CT: Yale University, Department of Sociology; 1975. [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45:212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Ingersoll B, Schreibman L. Teaching reciprocal imitation skills to young children with autism using a naturalistic behavioral approach: Effects on language, pretend play, and joint attention. Journal of Autism and Developmental Disorders. 2006;36:487–505. doi: 10.1007/s10803-006-0089-y. [DOI] [PubMed] [Google Scholar]
- Kaiser AP, Delaney EM. Responsive conversations: Creating opportunities for naturalistic language teaching. Young Exceptional Children Monograph Series. 2001;3:13–23. [Google Scholar]
- Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: A randomized controlled intervention study. Journal of Child Psychology and Psychiatry. 2006;47:611–620. doi: 10.1111/j.1469-7610.2005.01567.x. [DOI] [PubMed] [Google Scholar]
- Koegel R, Schreibman L, Good A, Cerniglia L, Murphy C, Koegel L. How to teach pivotal behaviors to children with autism: A training manual. Santa Barbara: University of California; 1989. [Google Scholar]
- Laird NM, Ware JH. Random effects models for longitudinal data. Biometrika. 1982;39:963–974. [PubMed] [Google Scholar]
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64:853–64. doi: 10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Lord C, Bristol M, Schopler E. Early intervention for children with autism and related disosrders. In: Schopler E, Van Bourgondien E, Bristol M, editors. Preschool issues in autism. New York: Plenum Press; 1993. pp. 199–221. [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule. Los Angeles, CA: Western Psychological Services; 1999. [Google Scholar]
- Lovaas O. Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology. 1987;55:3–9. doi: 10.1037//0022-006x.55.1.3. [DOI] [PubMed] [Google Scholar]
- McCathren R, Yoder P, Warren S. The relationship between prelinguistic vocalization and later expressive vocabulary in young children with development delay. Journal of Speech, Language, and Hearing Research. 1999;42:915–924. doi: 10.1044/jslhr.4204.915. [DOI] [PubMed] [Google Scholar]
- Mullen EM. Mullen: Scales of Early Learning. Circle Pines, MN: American Guidance Service; 1995. AGS edn. [Google Scholar]
- Mundy P, Sullivan L, Mastergeorge AM. A parallel and distributed-processing model of joint attention, social cognition and autism. Autism Research: Official Journal of the International Society for Autism Research. 2009;2:2–21. doi: 10.1002/aur.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers SJ, Vismara LA. Evidence-based comprehensive treatments for early autism. Journal of Child and Adolescent Psychiatry. 2008;37:8–38. doi: 10.1080/15374410701817808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers SJ, Hepburn SL, Stackhouse T, Wehner E. Imitation performance in toddlers with autism and those with other developmental disorders. Journal of Child Psychology and Psychiatry. 2003;44:763–781. doi: 10.1111/1469-7610.00162. [DOI] [PubMed] [Google Scholar]
- Schertz H, Odom S. Promoting joint attention in toddlers with autism: A parent-mediated developmental model. Journal of Autism and Developmental Disorders. 2007;37:1562–1575. doi: 10.1007/s10803-006-0290-z. [DOI] [PubMed] [Google Scholar]
- Sigman M, Ruskin E. Continuity and change in the social competence of children with autism, Down syndrome, and developmental delays. Monographs of the Society for Research in Child Development. 1999;64:v-114. doi: 10.1111/1540-5834.00002. [DOI] [PubMed] [Google Scholar]
- Speiel GE, Nelson KE. The many faces of imitation in language learning. New York, NY: Springer-Verlag; 1998. [Google Scholar]
- Stahmer A, Ingersoll B, Koegel R. Inclusive programming for toddlers with autism spectrum disorders: Outcomes from the Children’s Toddler School. Journal of Positive Behavior Interventions. 2004;6:67–82. [Google Scholar]
- StataCorp. Stata Statistical Software (Release 10) [computer software] College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Tomasello M, Todd J. Joint attention and lexical acquisition style. Language. 1983;4:197–211. [Google Scholar]
- Toth K, Munson J, Meltzoff A, Dawson G. Early predictors of communication development in young children with autism spectrum disorder: Joint attention, imitation, and toy play. Journal of Autism and Developmental Disorders. 2006;36:993–1005. doi: 10.1007/s10803-006-0137-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherby AM, Prizant BM. CSBS DP Manual: Communication and Symbolic Behavior Scales Developmental Profile. Baltimore, MD: Paul H Brookes Publishing Co; 2002. [Google Scholar]
- Wetherby AM, Watt N, Morgan L, Shumway S. Social communication profiles of children with autism spectrum disorders late in the second year of life. Journal of Autism and Developmental Disorders. 2007;37:960–975. doi: 10.1007/s10803-006-0237-4. [DOI] [PubMed] [Google Scholar]
- Yoder P. Predicting lexical density growth rate in young children with autism spectrum disorders. American Journal of Speech-Language Pathology. 2006;15:378–388. doi: 10.1044/1058-0360(2006/035). [DOI] [PubMed] [Google Scholar]