Abstract
Background
Hispanics have much higher cirrhosis mortality rates than non-Hispanic Blacks and Whites. Although heavy alcohol use and hepatitis C virus (HCV) infection are two major risk factors for cirrhosis, no studies have systematically assessed the contribution of alcohol- and HCV-related cirrhosis deaths to the total cirrhosis mortality for Hispanics as a whole and its variations across Hispanic subgroups. To fill this gap, the current study presents the latest data on total cirrhosis mortality as well as its component alcohol- and HCV-related cirrhosis mortality for all Hispanics and for Hispanic subgroups.
Methods
The multiple-cause approach was used to analyze data from the U.S. Multiple Cause of Death Data Files for 28,432 Hispanics and 168,856 non-Hispanic Whites (as a comparison group) who died with cirrhosis as the underlying or a contributing cause during 2000–2004. Four major Hispanic subgroups were defined by national origin or ancestry, including Mexicans, Puerto Ricans, Cubans, and Other Hispanics. The cirrhosis deaths were divided into four distinctive cause-of-death categories: alcohol-related, HCV-related, both alcohol- and HCV-related, and neither alcohol- nor HCV-related. Age-adjusted total cirrhosis death rates and percentage shares of the cause-specific categories were compared across Hispanic subgroups and non-Hispanic Whites.
Results
Compared with non-Hispanic Whites, all Hispanic subgroups except Cubans had much higher cirrhosis mortality. The age-adjusted total cirrhosis death rates were twice as high for Puerto Ricans and Mexicans as for non-Hispanic Whites. Alcohol-related and HCV-related cirrhosis death rates also were higher for most Hispanic subgroups than for non-Hispanic Whites.
Conclusions
Heavy alcohol use and hepatitis C viral infection are two important factors contributing to the high cirrhosis mortality among Hispanics. However, their relative contributions to total cirrhosis mortality varied by gender and Hispanic subgroup. This information is useful for targeted prevention and intervention efforts to address the excessive cirrhosis mortality in the Hispanic population.
Keywords: Ethnic Groups, Female, Health Status Disparities, Male, Risk Factors
INTRODUCTION
As the fastest growing ethnic group in the United States, the Hispanic population is an increasingly visible and important demographic group. In 2004, the number of Hispanics in the United States was approximately 41.3 million (14.1 percent of US population) (Miniño et al., 2007); by 2050, this number is expected to increase to 132.8 million (30 percent of US population) (Bureau of the Census, 2008).
While Hispanics have a mortality advantage compared with non-Hispanics with respect to all-cause death and some major causes of death, such as coronary heart diseases and certain cancers, they have a disadvantage with respect to several specific causes of death, including liver cirrhosis, diabetes, human immunodeficiency virus (HIV) disease, and homicide (Centers for Disease Control and Prevention, 2004).
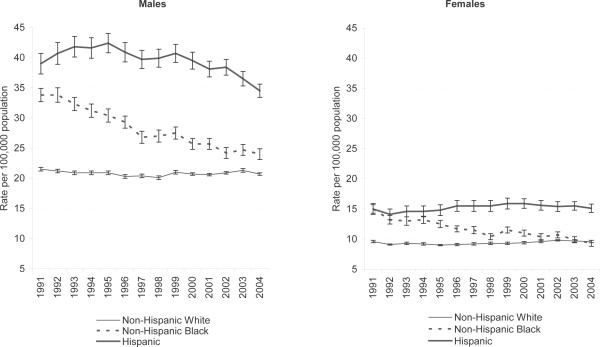
Liver cirrhosis is an especially serious public health problem for the Hispanic population in the United States. In 2004, cirrhosis was the 6th leading cause of death for Hispanics, but only the 12th leading cause of death for the total population in the United States (Heron, 2007). Compared with non-Hispanic Whites and Blacks, Hispanics have consistently shown the highest cirrhosis death rates for both males and females since the early 1990s, when comprehensive information on Hispanic origin first became available on death records (Stinson et al., 2001; Yoon and Yi, 2007) (See Figure 1).
Figure 1.
Age-adjusted death rates from all liver cirrhosis based on multiple-cause for “Non-Hispanic White,” “Non-Hispanic Black,” and “Hispanic” by sex: United States, 1991–2004. Vertical bars represent 95 percent confidence intervals.
Data Source: Multiple Cause of Death data files, 1991–2004 (National Center for Health Statistics).
Today, alcohol abuse and hepatitis C virus (HCV) infection are known as two major causes of chronic liver disease in the United States. Since the seminal work of Pearl, Alcohol and Longevity published in 1926, extensive scientific research has firmly established the association between alcohol consumption and cirrhosis risk. This connection is so robust that in the 1950s researchers began using cirrhosis mortality as an indicator of alcohol problems in populations. Cirrhosis mortality rates also have been used as a benchmark for evaluating the preventive impact of policies aimed at reducing alcohol consumption (Bruun et al., 1975; Edwards et al., 1994).
While the overall cirrhosis mortality rate has been declining during the last three decades (Yoon and Yi, 2007), HCV mortality rates, highly associated with cirrhosis, have been increasing since the 1990s (Kim, 2002; Vong and Bell, 2004; Wise et al., 2008). Up to 20 percent of individuals infected with HCV develop cirrhosis over a 20–30 year period (Seeff, 2002; Tong et al., 1995). Heavy alcohol use is among the most important factors influencing disease outcome in chronic HCV, exacerbating fibrosis progression in the liver, which is a precursor to cirrhosis (Poynard et al., 1997; Tong et al., 1995), and causing premature hospitalization and death (Chen et al., 2007; Jamal and Morgan, 2003).
The HCV literature indicates that Hispanics have a higher prevalence of anti-HCV antibodies than non-Hispanic Whites (Alter et al., 1999; Armstrong et al., 2006; Yen et al., 2003). Moreover, Hispanic patients with HCV infection have a faster fibrosis progression rate than non-Hispanic patients (Bonacini et al., 2001; Verma et al., 2006). Consequently, Hispanics are at higher risk for HCV-related cirrhosis death than non-Hispanic Whites and Blacks (Vong and Bell, 2004; Wise et al., 2008).
Although Hispanics are often considered a single ethnic group, they are in fact heterogeneous in terms of socioeconomic status (Ramirez and Cruz, 2002), health risk behaviors (Marks et al., 1990), drinking patterns (Black and Markides, 1993; Caetano, 1988; Canino, 1994; Gilbert and Cervantes, 1986; Johnson et al., 1998; Rogers, 1991), and alcohol abuse and dependence (Caeteno et al., 2008), all of which vary by country of origin. The three largest Hispanic subgroups are Mexicans, Puerto Ricans, and Cubans (65.9, 9.2, and 3.9 percent of all Hispanics, respectively), with the remaining 21 percent of Hispanics in the United States coming from all other Latin American and Caribbean countries (Miniño et al., 2007).
The heterogeneity among Hispanic subgroups generally has been ignored in mortality studies as data normally have been aggregated. Only a few studies have examined cirrhosis mortality by disaggregating Hispanic subgroups. Based on mortality data from 15 states for 1979 to 1981, Rosenwaike (1987) reported that the age-adjusted cirrhosis death rate varied across foreign-born Hispanic subgroups. Using more complete national mortality data for 2000–2004, Yoon and Yi (2007) confirmed the diverse cirrhosis mortality rates among Hispanic subgroups.
To date, there have been no national data that systematically assess the role of alcohol use and HCV infection in the excessive cirrhosis mortality of the Hispanic population and its subpopulations. Therefore, the objective of our study was to present the latest data for Hispanics on total cirrhosis mortality as well as its component alcohol- and HCV-related cirrhosis mortality and to disaggregate these data for Hispanic subgroups. To this end, we analyzed national mortality data for 2000–2004 using a multiple-cause approach. This approach included deaths for which cirrhosis was recorded as either the underlying cause or a contributing cause of death, allowing us to capture the full scope of cirrhosis mortality and its relatedness to alcohol use and HCV infection. All data are presented with non-Hispanic Whites as a comparison group.
MATERIALS AND METHODS
Data
Mortality data were taken from the Multiple Cause of Death public-use data file for 2000 to 2004 provided by the National Center for Health Statistics. The Multiple Cause of Death data include information from all resident death certificates filed each year in the 50 states and the District of Columbia. To increase the reliability of the analysis results, data for the 5-year period were pooled to calculate annual averages.
In the Multiple Cause of Death data, causes of death were classified according to the International Classification of Diseases, Tenth Revision (ICD-10). Each death record includes codes for one underlying cause and up to 20 contributing causes of death. For the current study, we included deaths for which cirrhosis was listed either as the underlying cause or as one of the contributing causes. The ICD-10 codes used in the current study are listed in Table 1. Following the National Institute on Alcohol Abuse and Alcoholism's surveillance report on liver cirrhosis mortality (Yoon and Yi, 2007), the ICD-10 codes used to identify all liver cirrhosis deaths are K70, K73, K74, K76.0 and K76.6. Among these codes, K70 indicates alcoholic liver cirrhosis. ICD-10 codes for HCV are B17.1 and B18.2. Based on the cirrhosis codes, a total of 28,432 Hispanics who resided in the United States at the time of their death during 2000–2004 were identified and included in the analysis. According to the U.S. Standard Certificate of Death, decedent's Hispanic origin is filled by funeral directors based on information given by the informant, and the definition of origin includes “ancestry, nationality, and lineage” (National Center for Health Statistics, 2003). The Hispanic decedents were divided into four major subgroups for the analysis: Mexicans (n=18,151; 63.8 percent), Puerto Ricans (n=3,863; 13.6 percent), Cubans (n=1,214; 4.3 percent), and Other Hispanics (n=5,204; 18.3 percent). The Other Hispanics category included “Central and South Americans” (n=1,683) and “Other and Unknown Hispanics” (n=3,521). These two groups can be identified separately in the mortality data. However, Dominicans were moved from the “Central and South Americans” to “Other Hispanics” in the population data from the Current Population Survey (CPS) since 2003. This change in categorization of the denominator data made it necessary to collapse the two groups in our study. Hispanics were not further broken down by race in our analysis, since over 98.6 percent of all Hispanics were identified as Whites in the death certificates. As a comparison group, 168,856 non-Hispanic White cirrhosis deaths during the same period were also included in the analysis.
Table 1.
ICD-10 Codes for HCV and Liver Cirrhosis
| Hepatitis C Infection | |
| B17.1 | Acute hepatitis C |
| B18.2 | Chronic viral hepatitis C |
| Liver Cirrhosis | |
| Alcohol-related cirrhosis | |
| K70.0 | Alcoholic fatty liver |
| K70.1 | Alcoholic hepatitis |
| K70.2 | Alcoholic fibrosis and sclerosis of liver |
| K70.3 | Alcoholic cirrhosis of liver |
| K70.9 | Alcoholic liver disease, unspecified |
| K70.4 | Alcoholic hepatic failure |
| Specified liver cirrhosis without mention of alcohol | |
| K73.0 | Chronic persistent hepatitis, not elsewhere classified (n.e.c.) |
| K73.1 | Chronic lobular hepatitis, n.e.c. |
| K73.2 | Chronic active hepatitis, n.e.c. |
| K73.8 | Other chronic hepatitis, n.e.c. |
| K73.9 | Chronic hepatitis, unspecified |
| K74.3 | Primary biliary cirrhosis |
| K74.4 | Secondary biliary cirrhosis |
| K74.5 | Biliary cirrhosis, unspecified |
| K76.0 | Fatty (change of) liver, n.e.c.a |
| K76.6 | Portal hypertensiona |
| Unspecified liver cirrhosis without mention of alcohol | |
| K74.0 | Hepatic fibrosis |
| K74.2 | Hepatic fibrosis with hepatic sclerosis |
| K74.6 | Other and unspecified cirrhosis of liver |
| K74.1 | Hepatic sclerosis |
Categorization by the National Institute on Alcohol Abuse and Alcoholism (Yoon and Yi, 2007). K76.0 is not defined as liver cirrhosis by the National Center for Health Statistics.
Source: International Classification of Diseases and Related Health Problems, Tenth Revision. Geneva,
Switzerland: World Health Organization, 1992.
The population data used as the denominators to calculate death rates were taken from estimates based on the CPS prepared by the U.S. Census Bureau for National Center for Health Statistics (Arias et al., 2003; Hoyert et al., 2006; Kochanek et al., 2004; Miniño et al., 2002; Miniño et al., 2007). This is the only source that includes Hispanic subgroup population data. Information on Hispanic origin on the CPS was determined on the basis of a question that asked for self-identification of the person's origin or descent. The definition of Hispanic origin was similar to that in the mortality data as described above (Bureau of Labor Statistics, 1997). The CPS population estimates were adjusted to resident Hispanic population control totals (i.e., the year 2000-based population estimates for the respective subpopulations in the United States for July 1 of each year).
Analysis
The analysis is primarily descriptive. Mortality rates were calculated as the number of deaths per 100,000 population. In order to compare mortality across subpopulation groups in a manner uninfluenced by differences in the subpopulation age structures, these rates were adjusted (or standardized) by age using the direct standardization method. The age-adjustment involved two steps. First, age-specific death rates for a subpopulation group were calculated for 8 age categories: 0–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85+ years. Second, the age-specific rates were weighted by the Year 2000 U.S. population distribution (as the age standard) and summed up as the age-adjusted rate for the respective subpopulation group. All age-adjusted death rates were calculated by sex and five racial/ethnic groups: Mexican, Puerto Rican, Cuban, Other Hispanics, and non-Hispanic White (as the comparison group). In most cases, the 5-year annual average of each descriptive statistic was used to ensure the reliability of the results by minimizing random fluctuations over time. However, since population estimates for Hispanic subgroups are derived from the CPS, the death rates calculated are subject to survey sampling variability in the denominator as well as random variability in the numerator. Therefore, 95 percent confidence intervals were calculated using standard errors for age-specific and age-adjusted rates derived from formula recommended by the National Center for Health Statistics (Miniño et al., 2007). In accordance with the National Center for Health Statistics formula (1, p.115), standard errors of age-adjusted death rates (R') were calculated as follows:
where
Psi = age-specific standard population for the ith age group from the U.S. standard population age distribution
Ps = total U.S. standard population (all age combined)
Ri = age-specific rate for the ith age group
Di = number of deaths for the ith age group
a = parameter derived from the CPS data for each year and varying depending on the subgroup of interest
b = parameter derived from the CPS data for each year and varying depending on the subgroup of interest
Pi = number of population for the ith age group
Furthermore, calculated age-adjusted rates were deemed unreliable if their relative standard error (i.e., standard error divided by its respective age-adjusted rate and multiplied by 100) was 23 percent or more (Miniño et al., 2007, p.115).
Taking a multiple-cause approach, cirrhosis death rates were calculated based on the underlying cause as well as contributing causes. To assess the relatedness of cirrhosis deaths to alcohol use, the age-adjusted alcohol-related cirrhosis death rate as well as its percentage share in the total age-adjusted cirrhosis death rate were calculated. Similarly, the relatedness of cirrhosis deaths to HCV was determined by the age-adjusted rate and percentage share of deaths with a co-occurring HCV infection in the total age-adjusted cirrhosis death rate. Percentage shares of alcohol-related and HCV-related liver cirrhosis death rates were derived by dividing the age-adjusted death rates for each type of cirrhosis by the age-adjusted death rate for all liver cirrhosis. The 95 percent confidence intervals for the percentage shares were calculated according to the formula recommended by Kegler (2007).
It should be noted that, when making comparisons, the ranking of a cause-specific cirrhosis death rate for a subpopulation group is not necessarily consistent with the ranking of its percentage share. This is because the death rates are absolute values, whereas percentage shares are relative within each subpopulation group. Consequently, one cause-specific cirrhosis category can have a low rate but a high percentage share, depending on its denominator—the all-cirrhosis death rate of the respective subpopulation group.
RESULTS
Liver cirrhosis mortality among Hispanic subgroups
As shown in Table 2, during 2000–2004, the annual average number of deaths from all types of liver cirrhosis (as either the underlying cause or a contributing cause) was 5,686 for Hispanics, corresponding to a rate of 25.70/100,000, and 33,771 for non-Hispanic Whites, corresponding to a rate of 14.98/100,000. Thus, the annual average age-adjusted death rate from all liver cirrhosis was higher for Hispanics as a whole than for non-Hispanic Whites. The same was true when males and females were analyzed separately.
Table 2.
Five-Year Annual Average Number of Deaths, Median Age at Death, and Annual Average of Age-Adjusted Death Rates from All Liver Cirrhosis, Alcohol- and HCV-Related Cirrhosis Among Hispanic Subgroups and Non-Hispanic Whites by Sex, United States, 2000–2004
| 5-year Annual Average Number of Deaths | Median Age at Death (Years) | Age-Adjusted Death Rates (Number of Deaths per 100,000 Population) and95% Confidence Intervals (CI) |
|||||
|---|---|---|---|---|---|---|---|
| All Cirrhosis | Alcohol-Related Cirrhosis | HCV-Related Cirrhosis | Both Alcohol- and HCV-Related Cirrhosisa | Neither Alcohol- Nor HCV-Related Cirrhosis | |||
| (1) | (2) | (3) | (4) | (5) | |||
| Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | Rate (95% CI) | |||
| Both Sexes | |||||||
| Hispanic | 5,686 | 56 | 25.70 (25.41, 25.99) | 9.50 (9.33, 9.68) | 3.30 (3.20, 3.41) | 0.97 (0.92, 1.03) | 13.86 (13.63, 14.09) |
| Mexican | 3,630 | 55 | 28.79 (28.36, 29.21) | 11.11 (10.86, 11.37) | 3.16 (3.02, 3.30) | 1.07 (1.00, 1.15) | 15.59 (15.25, 15.92) |
| Puerto Rican | 772 | 55 | 31.66 (30.62, 32.70) | 9.78 (9.22, 10.34) | 5.77 (5.36, 6.19) | 1.37 (1.17, 1.57) | 17.49 (16.68, 18.29) |
| Cuban | 243 | 69 | 12.01 (11.31, 12.70) | 2.69 (2.34, 3.04) | 2.20 (1.90, 2.50) | 0.25b (0.14, 0.37) | 7.37 (6.85, 7.88) |
| Other Hispanic | 1,041 | 55 | 21.34 (20.71, 21.97) | 7.92 (7.58, 8.27) | 2.76 (2.54, 2.98) | 0.74 (0.64, 0.84) | 11.40 (10.91, 11.88) |
| Non-Hispanic White | 33,771 | 60 | 14.98 (14.91, 15.05) | 5.47 (5.42, 5.51) | 1.46 (1.44, 1.49) | 0.49 (0.48, 0.50) | 8.54 (8.49, 8.59) |
| Male | |||||||
| Hispanic | 4,027 | 54 | 37.03 (36.53, 37.52) | 16.95 (16.61, 17.29) | 4.61 (4.43, 4.79) | 1.70 (1.59, 1.80) | 17.16 (16.79, 17.54) |
| Mexican | 2,601 | 53 | 40.41 (39.68, 41.13) | 19.47 (18.97, 19.96) | 4.28 (4.05, 4.50) | 1.83 (1.69, 1.98) | 18.50 (17.99, 19.00) |
| Puerto Rican | 563 | 54 | 49.31 (47.39, 51.23) | 17.97 (16.82, 19.12) | 9.16 (8.39, 9.92) | 2.46b (2.07, 2.85) | 24.65 (23.29, 26.00) |
| Cuban | 149 | 66 | 16.41 (15.20, 17.62) | 4.95 (4.28, 5.63) | 2.49 (2.02, 2.97) | 0.44b (0.23, 0.66) | 9.41 (8.56, 10.26) |
| Other Hispanic | 714 | 52 | 31.50 (30.33, 32.66) | 14.76 (14.01, 15.51) | 3.94 (3.56, 4.33) | 1.35 (1.15, 1.54) | 14.14 (13.56, 14.72) |
| Non-Hispanic White | 21,887 | 58 | 20.91 (20.80, 21.03) | 8.34 (8.27, 8.42) | 2.13 (2.09, 2.17) | 0.78 (0.76, 0.81) | 11.22 (11.15, 11.30) |
| Female | |||||||
| Hispanic | 1,659 | 65 | 15.31 (14.99, 15.63) | 2.83 (2.70, 2.97) | 2.02 (1.90, 2.14) | 0.29 (0.24, 0.33) | 10.74 (10.46, 11.02) |
| Mexican | 1,029 | 64 | 17.52 (17.03, 18.00) | 3.22 (3.03, 3.42) | 1.99 (1.82, 2.15) | 0.31 (0.25, 0.36) | 12.61 (12.21, 13.02) |
| Puerto Rican | 209 | 60 | 16.83 (15.77, 17.89) | 3.07 (2.64, 3.49) | 2.80 (2.39, 3.20) | 0.44b (0.29, 0.59) | 11.41 (10.78, 12.03) |
| Cuban | 94 | 74 | 7.86 (7.12, 8.61) | 0.53 (0.32, 0.75) | 1.89 (1.52, 2.26) | 0.05b (0.00, 0.13) | 5.49 (5.17, 5.82) |
| Other Hispanic | 327 | 65 | 13.34 (12.66, 14.02) | 2.65 (2.38, 2.91) | 1.74 (1.49, 1.98) | 0.23b (0.17, 0.30) | 9.19 (8.82, 9.56) |
| Non-Hispanic White | 11,884 | 66 | 9.67 (9.59, 9.74) | 2.84 (2.79, 2.88) | 0.83 (0.81, 0.85) | 0.21 (0.19, 0.22) | 6.20 (6.15, 6.25) |
The overlapping portion of (2) and (3).
Rate unreliable because the relative standard error (i.e., standard error divided by its respective age-adjusted rate and multiplied by 100) is 23 percent or more (Miniño et al., 2007).
Data source: Multiple Cause of Death data files, 2000–2004 (National Center for Health Statistics).
Among Hispanics, the rate of deaths from all cirrhosis varied greatly across subgroups. Compared with non-Hispanic Whites (20.91/100,000 and 9.67/100,000 for males and females, respectively), the rate was substantially higher for Puerto Ricans (49.31/100,000 and 16.83/100,000, respectively), Mexicans (40.41/100,000 and 17.52/100,000, respectively) and Other Hispanics (31.50/100,000 and 13.34/100,000, respectively), and lower for Cubans (16.41/100,000 and 7.86/100,000, respectively). The rate for males was consistently more than twice the rate for females for all Hispanic subgroups as well as for non-Hispanic Whites. Furthermore, the median age at death was younger for Puerto Ricans (54 and 60 years for males and females, respectively), Mexicans (53 and 64, respectively) and Other Hispanics (52 and 65, respectively) and much older for Cubans (66 and 74, respectively) compared with non-Hispanic Whites (58 and 66, respectively).
Alcohol-related and HCV-related liver cirrhosis mortality among Hispanic subgroups
Table 2 also shows age-adjusted death rates from alcohol-related and HCV-related cirrhosis. Table 3 shows the relatedness of cirrhosis mortality to alcohol use and HCV as indicated by percentage shares of alcohol- and HCV-related cirrhosis death rates in the total cirrhosis death rates. These data indicate that, in general, the prevalence and share of alcohol-related cirrhosis are higher than that for HCV-related cirrhosis. For both sexes combined, the share of alcohol-related cirrhosis death rates was about three times the share of HCV-related cirrhosis death rates for Hispanics (37.0 vs. 12.8 percent), and this difference was even greater among non-Hispanic Whites (36.5 vs. 9.7 percent). However, considerable variation existed in the alcohol-relatedness and HCV-relatedness across gender and Hispanic subgroups.
Table 3.
Percentage Share (%) of Alcohol-Related and HCV-Related Liver Cirrhosis Among All Liver Cirrhosis Deaths by Sex and Hispanic Subgroup, United States, 2000–2004
| Alcohol-Related Cirrhosis | HCV-Related Cirrhosis | Both Alcohol- and HCV- Related Cirrhosisa | Neither Alcohol- Nor HCV-Related Cirrhosis | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Percent (95% CI) | Percent (95% CI) | Percent (95% CI) | Percent (95% CI) | |
| Both Sexes | ||||
| Hispanic | 37.0 (36.2, 37.8) | 12.8 (12.4, 13.3) | 3.8 (3.5, 4.0) | 53.9 (52.8, 55.0) |
| Mexican | 38.6 (37.5, 39.7) | 11.0 (10.5, 11.5) | 3.7 (3.4, 4.0) | 54.2 (52.8, 55.6) |
| Puerto Rican | 30.9 (28.9, 33.0) | 18.2 (16.8, 19.7) | 4.3 (3.7, 5.0) | 55.2 (52.2, 58.5) |
| Cuban | 22.4 (19.4, 25.9) | 18.3 (15.8, 21.2) | 2.1b (1.3, 3.3) | 61.4 (56.0, 67.2) |
| Other Hispanic | 37.1 (35.2, 39.1) | 12.9 (11.9, 14.1) | 3.5 (3.0, 4.0) | 53.4 (50.7, 56.3) |
| Non-Hispanic White | 36.5 (36.2, 36.8) | 9.7 (9.6, 9.9) | 3.3 (3.1, 3.4) | 57.0 (56.6, 57.5) |
| Male | ||||
| Hispanic | 45.8 (44.7, 46.9) | 12.4 (12.0, 13.0) | 4.6 (4.3, 4.9) | 46.3 (45.2, 47.5) |
| Mexican | 48.2 (46.7, 49.7) | 10.6 (10.0, 11.2) | 4.5 (4.2, 4.9) | 45.8 (44.3, 47.3) |
| Puerto Rican | 36.4 (33.8, 39.3) | 18.6 (16.9, 20.4) | 5.0b (4.2, 5.9) | 50.0 (46.7, 53.5) |
| Cuban | 30.2 (25.8, 35.3) | 15.2 (12.4, 18.6) | 2.7b (1.6, 4.4) | 57.3(51.1, 64.4) |
| Other Hispanic | 46.9 (44.0, 49.9) | 12.5 (11.2, 13.9) | 4.3 (3.7, 5.0) | 44.9 (42.5, 47.4) |
| Non-Hispanic White | 39.9 (39.5, 40.3) | 10.2 (10.0, 10.4) | 3.7 (3.6, 3.8) | 53.7 (53.2, 54.1) |
| Female | ||||
| Hispanic | 18.5 (17.5, 19.5) | 13.2 (12.4, 14.0) | 1.9 (1.7, 2.2) | 70.2 (67.9, 72.5) |
| Mexican | 18.4 (17.2, 19.7) | 11.4 (10.4, 12.3) | 1.8 (1.5, 2.1) | 72.0 (69.0, 75.0) |
| Puerto Rican | 18.2 (15.6, 21.3) | 16.6 (14.2, 19.5) | 2.6b (1.8, 3.8) | 67.8 (62.4, 73.7) |
| Cuban | 6.7 (4.4, 10.2) | 24.0 (19.3, 29.9) | 0.6b (0.1, 3.1) | 69.8 (62.4, 78.2) |
| Other Hispanic | 19.9 (17.7, 22.3) | 13.0 (11.3, 15.1) | 1.7b (1.3, 2.2) | 68.9 (64.5, 73.6) |
| Non-Hispanic White | 29.4 (28.9, 29.8) | 8.6 (8.4, 8.8) | 2.2 (2.0, 2.4) | 64.1 (63.3, 64.9) |
The overlapping portion of (1) and (2).
Based on unreliable estimate of rate (see note in Table 2).
Data source: Multiple Cause of Death data files, 2000–2004 (National Center for Health Statistics).
Males
Among males, the age-adjusted death rate of alcohol-related cirrhosis for Hispanics as a whole (16.95/100,000) was about twice the rate for non-Hispanic Whites (8.34/100,000) (Table 2). Furthermore, except for Cuban males (4.95/100,000), the age-adjusted death rate of alcohol-related cirrhosis was higher for the Hispanic subgroups (19.47/100,000, 17.97/100,000, and 14.76/100,000 for Mexicans, Puerto Ricans, and Other Hispanics, respectively) than for non-Hispanic White males. The percentage share of alcohol-related cirrhosis death rate also was higher for Hispanic males as a whole (45.8 percent) than for non-Hispanic White males (39.9 percent). Among the Hispanic subgroups, however, the share of alcohol-related cirrhosis death rate was only higher for Mexican males (48.2 percent) and Other Hispanic males (46.9 percent) than for non-Hispanic White males (Table 3).
For HCV-related cirrhosis, the death rate among Hispanic males as a whole was more than twice as high (4.61/100,000) as that for non-Hispanic White males (2.13/100,000) (Table 2). As with the alcohol-related cirrhosis death rate, the HCV-related cirrhosis death rate varied greatly among Hispanic subgroups. It was highest for Puerto Rican males (9.16/100,000), which was more than four times the rate for non-Hispanic White males (2.13/100,000), more than three times that for Cuban males (2.49/100,000), and more than two times of that for Mexican (4.28/100,000) and Other Hispanic males (3.94/100,000). Consequently, Puerto Rican males had the highest share of HCV-related cirrhosis (18.6 percent) among all male subgroups (Table 3).
The cirrhosis death rate related to both alcohol and HCV was relatively low at 1.70/100,000 for Hispanic males as a whole. Nevertheless, this was two times the rate for non-Hispanic White males (0.78/100,000). There seemed to be a fair amount of variation in this rate across the Hispanic subgroup, but comparisons could not be made with certainty due to the unreliability of the estimated rate for some subgroups.
Females
In contrast to males, females had a much lower age-adjusted death rate of alcohol-related cirrhosis, which was about the same for Hispanic and non-Hispanic White females (2.83/100,000 and 2.84/100,000, respectively). Among the Hispanic subgroups, however, the rate varied in a similar pattern to that in the male subgroups, with the highest rate found among Mexican females (3.22/100,000), followed by Puerto Ricans (3.07/100,000), Other Hispanics (2.65/100,000), and Cubans (0.53/100,000). Also, in contrast to males, the share of alcohol-related cirrhosis death rate was lower for Hispanic females (18.5 percent) than for Non-Hispanic White females (29.4 percent). There was little variation among the subgroups of Hispanic females, except that Cuban females had a considerably smaller share of any alcohol-related cirrhosis deaths (6.7 percent) than other Hispanic female subgroups (ranging from 18.2 to 19.9 percent).
The age-adjusted death rate of HCV-related cirrhosis for Hispanic females as a whole (2.02/100,000) was about 2.4 times that for non-Hispanic Whites (0.83/100,000), with relatively small variations within Hispanic subgroups. The percentage share of HCV-related cirrhosis death rate was higher for Hispanic females (13.2 percent) than for non-Hispanic White females (8.6 percent). Among the subgroups, Cuban females displayed the highest (24.0 percent) and Mexican females the lowest share (11.4 percent) of HCV-related cirrhosis deaths.
The cirrhosis death rate related to both alcohol and HCV was low for Hispanic and non-Hispanic females (0.29/100,000 and 0.21/100,000, respectively). Moreover, its percentage share also was low and similar for Hispanic and non-Hispanic females. Again, comparisons across Hispanic subgroups could not be made with certainty due to unreliability of some estimates.
It should be noted from Table 3 that, although alcohol and HCV are two well-known etiological factors for cirrhosis deaths, a substantial proportion of the total cirrhosis death rates were due to neither alcohol- nor HCV-related cirrhosis (i.e., unknown etiological factors). The percentage share of this “residual” category was 3 percentage points lower for Hispanics than for non-Hispanic Whites. Further breaking down by gender and Hispanic subgroup revealed a greater variability of this category. For instance, the percentage share of this “residual” category was 7.4 percentage points lower for Hispanic males than for non-Hispanic White males. The percentage share of this category varied even more across Hispanic subgroups, ranging from 44.9 to 57.3 percent in males and from 64.1 to 72.0 percent in females.
DISCUSSION
From 2000 through 2004, cirrhosis was the underlying or a contributing cause of death for 28,432 (or 5,686 per year) Hispanics in the United States. Compared with non-Hispanic Whites, all Hispanic subgroups, except Cubans, were at much higher risk for cirrhosis mortality. In particular, Puerto Ricans and Mexicans were about twice as likely to die from cirrhosis as non-Hispanic Whites. These results confirm findings of mortality differentials among Hispanic subgroups in an earlier study by Rosenwaike (1987).
More detailed analyses found that among males, the high rate of alcohol-related cirrhosis deaths among Hispanics accounted for a large part of the cirrhosis mortality disparities. Except for Cuban males, Hispanic males had alcohol-related cirrhosis mortality rates that were twice as high as the rate among non-Hispanic White males. In contrast, there were no substantial differences in alcohol-related cirrhosis mortality rates between most Hispanic and non-Hispanic White females (again, Cuban females were an exception with a much lower rate). These mortality patterns are consistent with previous findings on the total alcohol intake and drinking patterns of Hispanics and non-Hispanics. Stinson and colleagues (Stinson et al., 1998) reported that there were no differences in average daily ethanol consumption between Hispanic and non-Hispanic males. However, Hispanic males were more likely to be engaged in weekend binge drinking. From a life course perspective, Jackson and colleagues (Jackson et al., 1998) showed that Hispanic males developed heavy drinking patterns later in life but sustained these patterns for longer periods of time than did White males. Among the Hispanic subgroups, Mexican males exhibited a higher prevalence of heavy alcohol use and alcohol dependence than non-Hispanic White males, whereas Cuban males showed a lower prevalence (Caetano et al., 2008; Johnson et al., 1998).
In the Hispanic community, heavy drinking and drunkenness is primarily a male activity, whereas abstention and infrequent light drinking is the common pattern for women (Caetano, 1988; Canino, 1994; Gilbert and Cervantes, 1986). Nevertheless, differences in consumption patterns exist among Hispanic female subgroups, with Mexican and Puerto Rican women more likely than Cuban women to consume larger amounts of alcohol (Black and Markides, 1993; Rogers, 1991).
Our results also indicate that HCV infection also contributes to the high Hispanic cirrhosis mortality. The proportion of HCV infection in liver cirrhosis deaths was higher for all of the four Hispanic subgroups than for non-Hispanic Whites. Among Hispanic subgroups, Puerto Ricans had the highest co-occurring HCV infection among cirrhosis deaths in both males and females. This may be associated with the high rates of HIV infection and illicit drug use among Puerto Ricans. According to a National Research Council's report on emerging issues in Hispanic health (National Research Council, 2002), HIV infection is the third leading cause of death for Puerto Ricans. Puerto Ricans also have a higher prevalence of illicit drug use than other Hispanic subgroups (Johnson et al., 1998). Previous research indicates that many people are infected with both HCV and HIV due to injection drug use (Wise et al., 2008), and coinfection with HIV is an important prognostic factor exacerbating the course of HCV infection (Graham et al., 2001).
Despite the growing concern about the HCV epidemic (Armstrong et al., 2000), our data suggest that alcohol played a more important role than HCV infection in the development of liver cirrhosis among Hispanics. For instance, the percentage share of alcohol-related cirrhosis among cirrhosis deaths was substantially greater than that of HCV-related cirrhosis for all demographic subgroups, except Cuban females. The contribution of alcohol involvement relative to HCV infection in all cirrhosis deaths generally was greater among males than females, especially among Mexican, Other Hispanic and non-Hispanic White males.
While the differences between Hispanic subgroups in the percentage shares of co-occurring alcohol- and HCV-related cirrhosis death rate were not particularly striking, they should be noted because individuals with this comorbidity are at increased risk of early death. Previous research has found that in the presence of heavy alcohol use, HCV accelerates premature deaths from cirrhosis (Chen et al., 2007).
Our results on the percentage share of the “residual” category (i.e., neither alcohol- nor HCV-related cirrhosis) indicated that alcohol and HCV played more important roles in cirrhosis mortality among males than among females, among Hispanic males than among non-Hispanic White males, and among Mexican males than among Cuban males. However, overall, only about half of cirrhosis deaths were related to alcohol or HCV in this study. As an effort to explore etiological factors other than alcohol and HCV, we examined non-alcoholic fatty liver disease (NAFLD), which is regarded as hepatic manifestation of metabolic syndrome. Histologically, NAFLD is a spectrum ranging from benign hepatic steatosis to steatohepatitis, fibrosis, and cirrhosis (Alazmi et al., 2006). With the dramatic increase in the prevalence of obesity, NAFLD has become one of the most common chronic liver diseases (Lazo and Clark, 2008). Previous studies also indicated that Hispanics (especially Mexican Americans) have a higher prevalence of NAFLD than non-Hispanic Whites (Browning et al., 2004; Clark, 2006; Weston et al., 2005). According to the recently released ICD-10-CM (NCHS, 2010, p.634), we used two ICD-10 codes—K76.0 (Change of fatty liver, not elsewhere classified) and K75.8 (Other specified inflammatory liver diseases, a category for nonalcoholic steatohepatitis [NASH]), as a direct measure for NAFLD. We identified 6,226 deaths (or 1,245 per year) from NAFLD-related cirrhosis (not related to either alcohol or HCV). Contrary to what was expected, the prevalence of NAFLD-related cirrhosis was substantially lower than that of alcohol- and HCV-related cirrhosis across the board. Overall, age-adjusted death rates from NAFLD were 0.52 and 0.51 per 100,000 population for Hispanics and non-Hispanic Whites, respectively. Among Hispanics, Mexicans showed higher age-adjusted death rates from NAFLD cirrhosis than non-Hispanic Whites (0.63 versus 0.51). While the relative contribution of NAFLD cirrhosis to the total cirrhosis death rate was generally low, it was greater for non-Hispanic Whites (3.4 percent) than for all Hispanic subgroups (ranging from 1.1 to 2.2 percent). The low prevalence of NAFLD-related cirrhosis deaths could be partly due to the under-reporting on the death certificate because NAFLD is difficult to determine since steatosis may disappear as cirrhosis develops (McCullough, 2002). Future research is needed to identify etiological factors that account for the cirrhosis mortality that is neither alcohol- nor HCV-related.
Our findings revealed that Cubans had remarkably lower cirrhosis mortality rates than the rest of the Hispanic subgroups as well as non-Hispanic Whites. This may be due to their distinctive features documented in the literature. A large majority of Cubans are foreign-born (Hajat et al., 2000). The early emigrants are mostly political refugees from upper and middle classes and had experienced high-quality health care even before their arrival to the United States (Diaz-Briquets, 1991). Compared with other Hispanics, Cubans are more likely to have private health insurance (Escarce and Kapur, 2006). They are less likely to have obesity (Diaz-Briquets, 1991; Escarce et al., 2006; Morales et al., 2002) and more likely to drink alcohol in moderation (Black and Markides, 1993; Caetano et al., 2008; Diaz-Briquets, 1991; Johnson et al., 1998; Marks et al., 1990; Rogers, 1991). However, we were unable to examine these factors due to the lack of information on such factors in death certificates.
To our knowledge, the current study is the only one in recent years that presents cirrhosis mortality data for Hispanic population subgroups in the United States. Our study also is unique in that it examined the contributions of both heavy alcohol use and HCV infection to the high cirrhosis mortality among Hispanics. This is much-needed information for addressing disparity issues in Hispanic health. The findings presented here extend our understanding of cirrhosis mortality differentials among Hispanic subgroups. Previous research has shown excess cirrhosis mortality for Hispanics as a whole. Our study unmasked the wide subgroup variations in the rates and relative contributions of major etiological factors (i.e., alcohol and HCV) for cirrhosis mortality among the Hispanic population. The results provide basic epidemiologic data to develop public heath strategies targeting risk factors unique to each Hispanic subgroup, such as heavy alcohol use among Mexican and Puerto Rican males to reduce their high alcoholic cirrhosis mortality and HCV infection among Puerto Ricans to reduce their high HCV-related cirrhosis mortality.
There are several limitations to this study. First, identification of Hispanic ethnicity in mortality data has some sources of error. Differences exist in reporting Hispanic origin on death certificates and on censuses and the Current Population Surveys (Miniño et al., 2007), which were used as the denominator in computing age-adjusted death rates in the current study. The ratio of death estimates from Current Population Surveys to death certificates for Hispanics was found to be 1.05, indicating a 5-percent net underreport of Hispanic origin on death certificates (Miniño et al., 2007, p.107). Second, alcohol-related and HCV-related cirrhosis deaths could be underestimated because of underreporting of alcohol-relatedness and inadequate identification of HCV infection on death certificates. This may in part explain the relatively large residual proportion of liver cirrhosis deaths that are yet to be accounted for. Previous research has indicated that a large portion of the unspecified cirrhosis deaths were in fact alcohol-related (Parrish et al., 1993). Moreover, the detection of HCV has not been comprehensive for various reasons (Manos et al., 2008; Wu et al., 2005). Third, data from death certificates lack information on etiological factors other than alcohol and HCV. Although we attempted to examine the etiological role of NAFLD, the low prevalence of it did not add much to the explanation of the Hispanic cirrhosis mortality. As mentioned earlier, underreporting in the death certificates also may be responsible for the low NAFLD-related cirrhosis death rates. Finally, genetic and environmental risk factors play important roles in ethnic differences in alcohol metabolism and subsequent liver injury (Day, 2006; Kemmer and Neff, 2008; Reuben, 2008; Zakhari and Li, 2007). Future studies analyzing the excessive cirrhosis mortality among Hispanics, especially Hispanic males, should take these factors into consideration.
ACKNOWLEDGMENT
The authors thank Dr. Raul Caetano for his helpful comments on an earlier version of this paper. The authors also wish to thank the two anonymous reviewers for their helpful comments.
This article is based on a study conducted under the Alcohol Epidemiologic Data System project funded by the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health through Contract No.HHSN267200800023C to CSR, Incorporated. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of the sponsoring agency or the Federal Government.
REFERENCES
- Alazmi WM, Regev A, Molina EG, Schiff ER. Predictors of cirrhosis in Hispanic patients with Nonalcoholic Steatohepatitis. Dig Dis Sci. 2006;51:1725–1729. doi: 10.1007/s10620-005-9065-1. [DOI] [PubMed] [Google Scholar]
- Alter MJ, Kruszon-Moran D, Nainan OV, McQuillan GM, Gao F, Moyer LA, Kaslow RA. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556–562. doi: 10.1056/NEJM199908193410802. [DOI] [PubMed] [Google Scholar]
- Arias E, Anderson RN, Kung HC, Murphy SL, Kochanek KD. Deaths: Final Data for 2001. National Vital Statistics Report. No. 3. Vol. 52. National Center for Health Statistics; Hyattsville, MD: 2003. [PubMed] [Google Scholar]
- Armstrong GL, Alter MJ, McQuillan GM, Margolis HS. The past incidence of hepatitis C virus infection: Implications for the future burden of chronic liver disease in the United States. Hepatology. 2000;31:777–782. doi: 10.1002/hep.510310332. [DOI] [PubMed] [Google Scholar]
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med. 2006;144:705–714. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Black SA, Markides KS. Acculturation and alcohol consumption in Puerto Rican, Cuban-American and Mexican-American women in the United States. Am J Public Health. 1993;83:890–893. doi: 10.2105/ajph.83.6.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonacini M, Groshen S, Y MC, Govindarajan S, Lindsay KL. Chronic Hepatitis C in ethnic minority patients evaluated in Los Angeles County. Am J Gastroenterol. 2001;96:2438–2341. doi: 10.1111/j.1572-0241.2001.04050.x. [DOI] [PubMed] [Google Scholar]
- Browning JD, Szczepaniak LS, Dobbins R, Nurembert P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in urban population in the United States: Impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- Bruun K, Edwards G, Lumio M. Alcohol Control Policies in Public Health Perspective. Finnish Foundation for Alcohol Studies; Helsinki: 1975. [Google Scholar]
- Bureau of the Census. US Department of Commerce . An older and more diverse nation by midcentury. U.S. Census Bureau News. Bureau of the Census; Washington, DC: 2008. [Accessed February 19, 2010]. [U.S. Census Bureau Web site]. August 14, 2008. Available at: http://www.census.gov/Press-Release/www/releases/archives/population/012496.html. [Google Scholar]
- Bureau of Labor Statistics [Accessed February 24, 2010];Current Population Survey. Basic Monthly Survey. Interviewer's Manual. 1997 Available at: http://www.bls.census.gov/cps/intmanc3.htm#C3O.
- Caetano R. Alcohol use among Hispanic groups in the United States. Am J Drug Alcohol Abuse. 1988;14:293–308. doi: 10.3109/00952998809001552. [DOI] [PubMed] [Google Scholar]
- Caetano R, Ramisetty-Mikler S, Rodriguez LA. The Hispanic Americans Baseline Alcohol Survey (HABLAS): Rates and predictors of alcohol abuse and dependence across Hispanic national groups. J Stud Alcohol Drugs. 2008;69:441–448. doi: 10.15288/jsad.2008.69.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G. Alcohol use and misuse among Hispanic women: Selected factors, processes, and studies. Int J Addict. 1994;29:1083–1100. doi: 10.3109/10826089409047930. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Hispanic disparities experienced by Hispanics – United States. MMWR. 2004;53:935–937. [PubMed] [Google Scholar]
- Chen CM, Yoon YH, Yi H, Lucas DL. Alcohol and hepatitis C mortality among males and females in the United States: a life table analysis. Alcohol Clin Exp Res. 2007;31:285–292. doi: 10.1111/j.1530-0277.2006.00304.x. [DOI] [PubMed] [Google Scholar]
- Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol. 2006;40:S5–S10. doi: 10.1097/01.mcg.0000168638.84840.ff. [DOI] [PubMed] [Google Scholar]
- Day CP. Genes or environment to determine alcoholic liver disease and non-alcoholic fatty liver disease. Liver International. 2006;26:1021–1028. doi: 10.1111/j.1478-3231.2006.01323.x. [DOI] [PubMed] [Google Scholar]
- Diaz-Briquets S. In: Mortality patterns of Cubans in the United States, in Mortality of Hispanic Populations. Rosenwaike I, editor. Greenwood Press; Westport, Connecticut: 1991. pp. 111–129. [Google Scholar]
- Edwards G, Anderson P, Babor TF, Casswell S, Ferrence R, Giesbrecht N, Godfrey C, Holder HD, Lemmens P, Makela K, Midanik LT, Norstrom T, Osterberg E, Romelsjo A, Room R, Simpura J, Skog OJ. Alcohol Policy and the Public Good. Oxford University Press; New York: 1994. [PubMed] [Google Scholar]
- Escarce JJ, Kapur K. Access to and quality of health care. In: Tienda M, Mitchell F, editors. Hispanics and the Future of America. Committee on Transforming our Common Destiny, National Research Council. The National Academies Press; Washington, DC: 2006. pp. 410–446. [PubMed] [Google Scholar]
- Escarce JJ, Morales LS, Rumbaut RG. The health status and health behaviors of Hispanics. In: Tienda M, Mitchell F, editors. Hispanics and the Future of America. Committee on Transforming Our Common Destiny, National Research Council. The National Academies Press; Washington, DC: 2006. pp. 362–409. [Google Scholar]
- Gilbert MJ, Cervantes RC. Patterns and practices of alcohol use among Mexican-Americans: A comprehensive review. Hisp J Behav Sci. 1986;8:1–60. [Google Scholar]
- Graham CS, Baden LR, Yu E, Mrus JM, Carnie J, Heeren T, Kaziel MJ. Influence of human immunodeficiency virus infection on the course of hepatitis C virus infection: a meta analysis. Clin Infect Dis. 2001;33:562–569. doi: 10.1086/321909. [DOI] [PubMed] [Google Scholar]
- Hajat A, Lucas JB, Kington R. Health Outcomes Among Hispanic Subgroups: Data From the National Health Interview Survey, 1992–95. National Center for Health Statistics; Hyattsville, Maryland: 2000. (Advance data from vital and health statistics; no.310) (DHHS publication no. (PHS) 2000-1250) [PubMed] [Google Scholar]
- Heron MP. Deaths: Leading Causes for 2004. National Vital Statistics Report. No. 5. Vol. 56. National Center for Health Statistics; Hyattsville, MD: 2007. [PubMed] [Google Scholar]
- Hoyert DL, Heron MP, Murphy SL, Kung H-C. Deaths: Final Data for 2003. National Vital Statistics Report. No. 13. Vol. 54. National Center for Health Statistics; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- Jamal MM, Morgan TR. Liver disease in alcohol and hepatitis C. Best Pract Res Clin Gastroenterol. 2003;17:649–662. doi: 10.1016/s1521-6918(03)00018-0. [DOI] [PubMed] [Google Scholar]
- Jackson JS, Williams DR, Gomberg ESL. Aging and alcohol use and abuse among African Americans: A life-course perspective. In: Gomberg ESL, Hegedus AM, Zucker RA, editors. Alcohol Problems and Aging, NIAAA Research Monograph No. 33. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 1998. pp. 63–87. [Google Scholar]
- Johnson RA, Larison C, Gerstein DR, Greenblatt J. Prevalence of Substance Use Among Racial and Ethnic Subgroups in the United States 1991–1993. Substance Abuse and Mental Health Services Administration; Rockville, MD: 1998. [Google Scholar]
- Kegler SR. Applying the compound Poisson process model to the reporting of injury-related mortality rates. Epidemiol Perspect Innov. 2007;4:1–9. doi: 10.1186/1742-5573-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemmer N, Neff GW. Ethnic variations in chronic liver diseases. Dig Dis Sci. 2008;53:1339–1344. doi: 10.1007/s10620-007-9992-0. [DOI] [PubMed] [Google Scholar]
- Kim WR. The burden of hepatitis C in the United States. Hepatology. 2002;36(Suppl):S30–S34. doi: 10.1053/jhep.2002.36791. [DOI] [PubMed] [Google Scholar]
- Kochanek KD, Murphy SL, Anderson RN, Scott C. Deaths: Final Data for 2002. National Vital Statistics Report. No. 5. Vol. 53. National Center for Health Statistics; Hyattsville, MD: 2004. [PubMed] [Google Scholar]
- Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: a global perspective. Semin Liver Dis. 2008;28:339–350. doi: 10.1055/s-0028-1091978. [DOI] [PubMed] [Google Scholar]
- Manos MM, Leyden WA, Murphy RC, Terrault N, Bell BP. Limitations of conventionally derived chronic liver disease mortality rates: Results of a comprehensive assessment. Hepatology. 2008;47:1150–1157. doi: 10.1002/hep.22181. [DOI] [PubMed] [Google Scholar]
- Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: Findings from HHANES, 1982–84. Am J Pubic Health. 1990;80(Suppl):S20–S26. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough AJ. Update on nonalcoholic fatty liver disease. J Clin Gastroenterol. 2002;34:255–262. doi: 10.1097/00004836-200203000-00013. [DOI] [PubMed] [Google Scholar]
- Miniño AM, Arias E, Kochanek KD, Murphy SL, Smith BL. Deaths: Final Data for 2000. National Vital Statistics Report. No. 15. Vol. 50. National Center for Health Statistics; Hyattsville, MD: 2002. [PubMed] [Google Scholar]
- Miniño AM, Heron MP, Murphy SL, Kochanek KD. Deaths: Final Data for 2004. National Vital Statistics Report. No. 19. Vol. 55. National Center for Health Statistics; Hyattsville, MD: 2007. [PubMed] [Google Scholar]
- Morales LS, Marielena L, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13:477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics [Accessed February 24, 2010];U.S. Standard Certificate of Death. 2003 Available at: http://www.cdc.gov/nchs/data/dvs/DEATH11-03final-ACC.pdf.
- National Center for Health Statistics [Accessed June 22, 2010];2010 Update of ICD–10–CM. 2010 Tabular List. Available at: http://www.cdc.gov/nchs/icd/icd10cm.htm#10update.
- National Research Council, Committee on Population . In: Emerging Issues in Hispanic Health: Summary of a Workshop. Iannotta JG, editor. National Academies Press; Washington, D.C.: 2002. [Accessed February 19, 2010]. [The National Academies Press Web site]. Available at: www.nap.edu/catalog/10485.html. [PubMed] [Google Scholar]
- Parrish KM, Dufour MC, Stinson FS, Harford TC. Average daily alcohol consumption during adult life among decedents with and without cirrhosis: The 1986 National Mortality Followback Survey. J Stud Alcohol. 1993;54:450–456. doi: 10.15288/jsa.1993.54.450. [DOI] [PubMed] [Google Scholar]
- Pearl R. Alcohol and Longevity. Alfred A. Knopf; New York: 1926. [Google Scholar]
- Poynard T, Becossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825–832. doi: 10.1016/s0140-6736(96)07642-8. [DOI] [PubMed] [Google Scholar]
- Ramirez RR, Cruz GP. The Hispanic Population in the United States: March 2002, Current Population Reports P20–545. Bureau of the Census; Washington, DC: 2002. [Google Scholar]
- Rogers RG. In: Health-related lifestyles among Cubans, Mexican-Americans, and Puerto-Ricans in the United States, in Mortality of Hispanic Populations. Rosenwaike I, editor. Greenwood Press; Westport, Connecticut: 1991. pp. 145–160. [Google Scholar]
- Rosenwaike I. Mortality differentials among persons born in Cuba, Mexico, and Puerto Rico residing in the United States, 1979–91. Am J Public Health. 1987;77:603–606. doi: 10.2105/ajph.77.5.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reuben A. Alcohol and the Liver. Curr Opin in Gastroenterol. 2008;24:328–338. doi: 10.1097/MOG.0b013e3282fbceca. [DOI] [PubMed] [Google Scholar]
- Seeff LB. Natural history of chronic hepatitis C. Hepatology. 2002;36(Suppl):S35–S46. doi: 10.1053/jhep.2002.36806. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res. 2001;25:1181–1187. [PubMed] [Google Scholar]
- Stinson FS, Yi H, Grant BF, Chou P, Dawson DA, Pickering R. U.S. Alcohol Epidemiologic Data Reference Manual. Vol. 6, Drinking in the United States: Main Findings from the National Longitudinal Alcohol Epidemiologic Survey (NLAES) National Institute on Alcohol Abuse and Alcoholism, Division of Biometry and Epidemiology, Alcohol Epidemiologic Data system; Bethesda, MD: 1998. [Google Scholar]
- Tong MJ, el-Farra NS, Reikes AR, Co RL. Clinical outcomes after transfusion-associated hepatitis C. N Engl J Med. 1995;332:1463–1466. doi: 10.1056/NEJM199506013322202. [DOI] [PubMed] [Google Scholar]
- Verma S, Bonacini M, Govindarajan S, Kanel G, Lindsay KL, Redeker A. More advanced hepatic fibrosis in Hispanics with chronic hepatitis C infection: role of patient demographics, hepatic necroinflammation, and steatosis. Am J Gastroenterol. 2006;101:1817–1823. doi: 10.1111/j.1572-0241.2006.00682.x. [DOI] [PubMed] [Google Scholar]
- Vong S, Bell BP. Chronic liver disease mortality in the United States, 1990–1998. Hepatology. 2004;39:476–483. doi: 10.1002/hep.20049. [DOI] [PubMed] [Google Scholar]
- Weston SR, Leyden W, Murphy R, Bass NM, Bell BP, Manos MM, Terrault NA. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Hepatology. 2005;41:372–379. doi: 10.1002/hep.20554. [DOI] [PubMed] [Google Scholar]
- Wise M, Bialek S, Finelli L, Bell BP, Sorvillo F. Changing trends in Hepatitis C-related mortality in the United States, 1995–2004. Hepatology. 2008;47:1128–1135. doi: 10.1002/hep.22165. [DOI] [PubMed] [Google Scholar]
- World Health Organization . International Classification of Diseases and Related Health Problems, Tenth Revision. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- Wu C, Chang HG, McNutt LA, Smith PF. Estimating the mortality rate of hepatitis C using multiple data sources. Epidemiol Infect. 2005;133:121–125. doi: 10.1017/s0950268804003103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen T, Keefee EB, Ahmed A. The epidemiology of hepatitis C virus infection. J Clin Gastroenterol. 2003;36:47–53. doi: 10.1097/00004836-200301000-00015. [DOI] [PubMed] [Google Scholar]
- Yoon YH, Yi H. National Institute on Alcohol Abuse and Alcoholism, Division of Epidemiology and Prevention Research, Alcohol Epidemiologic Data System; Bethesda, MD: 2007. Surveillance Report #79: Liver Cirrhosis Mortality in the United States, 1970–2004. [Google Scholar]
- Zakhari S, Li T-K. Determinants of alcohol use and abuse: Impact of quantity and frequency patterns on liver disease. Hepatology. 2007;46:2032–2039. doi: 10.1002/hep.22010. [DOI] [PubMed] [Google Scholar]