Abstract
Excess maternal weight has been negatively associated with breastfeeding. We examined correlates of breastfeeding initiation and intensity in a racially diverse sample of overweight and obese women. This paper presents a secondary analysis of data from 450 women enrolled in a postpartum weight loss intervention (Active Mothers Postpartum [AMP]). Sociodemographic measures and body mass index (BMI), collected at 6 weeks postpartum, were examined for associations with breastfeeding initiation and lactation score (a measure combining duration and exclusivity of breastfeeding until 12 months postpartum). Data were collected September 2004–April 2007. In multivariable analyses, BMI was negatively associated with both initiation of breastfeeding (OR: .96; CI: .92–.99) and lactation score (β −0.22; P = 0.01). Education and infant gestational age were additional correlates of initiation, while race, working full-time, smoking, parity, and gestational age were additional correlates of lactation score. Some racial differences in these correlates were noted, but were not statistically significant. Belief that breastfeeding could aid postpartum weight loss was initially high, but unrelated to breastfeeding initiation or intensity. Maintenance of this belief over time, however, was associated with lower lactation scores. BMI was negatively correlated with breastfeeding initiation and intensity. Among overweight and obese women, unrealistic expectations regarding the effect of breastfeeding on weight loss may negatively impact breastfeeding duration. In general, overweight and obese women may need additional encouragement to initiate breastfeeding and to continue breastfeeding during the infant’s first year.
Keywords: Breastfeeding, Overweight, Obesity, Postpartum, Initiation, Lactation
Introduction
Breastfeeding is the preferred mode of infant feeding [1–3] and is associated with important health benefits for both mother and child [1–4]. The American Academy of Pediatrics [1] and the World Health Organization [2] recommend exclusive breastfeeding through 6 months postpartum and continued breastfeeding through at least the first year of life. Breastfeeding is a Healthy People 2010 priority [5], and the US Preventive Services Task Force recently recommended intervention before, around and after childbirth to encourage and support the practice [6].
Age, white race, and education have been positively associated with breastfeeding [7–11], while smoking [8, 11, 12], cesarean versus vaginal delivery [8, 13], and preterm birth [11] have been negatively associated. Breastfeeding initiation and duration is also lower among overweight and obese women [14–16]. While there have been some inconsistent findings, most studies show that obese women breastfeed for shorter durations than normal weight women, even after adjustment for covariates [17].
The objective of this paper is to examine the effect of increasing body mass index on breastfeeding in a sample comprised exclusively of overweight and obese women. We further examine other correlates of breastfeeding within this sample, and whether there are differences in these correlates by race. Finally, we investigate whether beliefs about the effect of lactation on weight loss influence these overweight and obese women’s breastfeeding behaviors.
Subjects and Methods
Participants
We conducted a secondary analysis of data collected from participants in Active Mothers Postpartum (AMP), a behavioral intervention to promote weight loss in overweight and obese postpartum women [18]. Results from the larger trial have been published elsewhere [19]. Participants (n = 450) were recruited from September 2004 through April 2006 from the three largest obstetric clinics in Durham, North Carolina, and through posters in grocery stores, smaller obstetrics clinics, and libraries. English-speaking women ≥18 years of age and with a measured BMI ≥25 kg/m2 at 6 weeks postpartum were eligible. In accordance with Duke Institutional Review Board approval, informed consent was obtained prior to any data collection.
Measures
Four hundred fifty women completed the baseline assessments at 6 weeks postpartum. Sociodemographic information included: age, race, education, marital status, parity, and plans to work outside the home at 6 months postpartum. Health- and pregnancy-related data included smoking status, the Edinburgh Postnatal Depression Scale [20] (score of>12 categorized as “postpartum depression” [21]), vaginal versus cesarean delivery, infant gestational age (weeks), self-reported prepregnancy weight and gestational weight gain, and current breastfeeding status (full breastfeeding, breastfeeding and formula feeding [mixed feeding], or formula feeding only).
Measured height and weight were obtained at 6 weeks postpartum using a Seca portable stadiometer and a Tanita BWB-800 scale, with participants in street clothing with shoes removed. Due to the high correlation (Pearson’s r = 0.92; P = <.0001) between BMI derived from self-reported pre-pregnancy weight and BMI derived from weight measured at 6 weeks postpartum, and the greater reliability of the latter, we used the measured BMI at 6 weeks postpartum as the indicator of overall maternal weight status.
A total of 385 women completed the follow-up at 12 months postpartum. Women were again asked how they were currently feeding their baby, and formula feeding women were asked if they had ever breastfed. All women currently or ever breastfeeding completed a detailed recall of how the baby was fed during each month of life—full breastfeeding, mixed feeding, or formula feeding only. Full breastfeeding was defined as infant receiving only breast milk, not any formula or other milk. Introduction of juice, other fluids or solid foods was not recorded.
Figure 1 describes inclusion in the analysis samples. Initiation of breastfeeding was derived from the more detailed data available at 12 months, with all women currently or ever breastfeeding categorized as initiating breastfeeding. For those lost to follow-up (n = 65), their response at 6 weeks postpartum was used to define initiation, with full (n = 14) or mixed (n = 22) breastfeeding categorized as initiating breastfeeding. No data on whether formula feeders at 6 weeks postpartum (n = 29) had ever breastfed was available.
Fig. 1.
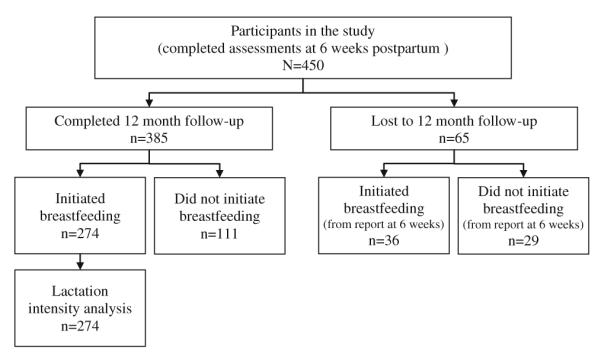
Inclusion in the analysis samples
Amount of breastfeeding was summarized by a lactation score, a measure of breastfeeding “intensity” combining the duration and exclusivity of breastfeeding [22]. This score was derived from the detailed monthly feeding data collected at the 12 month follow-up. A value was assigned for each month—0 if formula fed, 1 if mixed, and 2 if fully breastfed. The resulting score has a possible range of 0–24, and more explanatory power than a simple measure of duration. Intensity was only addressed in those who initiated breastfeeding; i.e., respondents with a lactation score of 0 (never breastfed) were not included in the intensity analysis.
All women at baseline and 12 month follow-up were asked about their beliefs regarding lactation and weight loss: “on a scale from 1 to 7, where 1 is certain not to happen and 7 is certain to happen, to what extent do you think breastfeeding will help women lose weight?” Women who reported ever having breastfed at 12 month follow-up (n = 274) also responded to a list of possible reasons for breastfeeding.
Statistical Analyses
We examined initiation of breastfeeding for the total sample (n = 450), and lactation score among those who initiated breastfeeding and completed the detailed breastfeeding recall at 12 months postpartum (n = 274). Proportions initiating breastfeeding by relevant categories of each sociodemographic and health-related characteristic were calculated, and the chi-square test used to identify associations between these variables and breastfeeding initiation. For the purposes of presentation in these bivariate analyses, BMI was categorized as overweight (25.0–29.9), obesity class 1 (30.0–34.9), obesity class II (35.0–39.9), or obesity class III (40+) [23], and gestational weight gain was classified according to Institute of Medicine (IOM) recommendations for appropriate gestational weight gain according to prepregnancy BMI [24]. Mean lactation scores were calculated by relevant categories for each variable, and Student’s t-test and ANOVA used to test bivariate associations between these characteristics and lactation score.
Multivariable logistic and linear regression were used to assess the sociodemographic and health-related variables as predictors of breastfeeding initiation and lactation score. To control for any possible effect of intervention participation, trial arm was included as a control variable in the model for lactation score. Education was collected in categories and entered as dummy variables into the models. Age, parity, gestational age, gestational weight gain, and BMI were entered as continuous variables.
Racial differences were first examined in separate models for blacks and whites. Any variable with a P-value ≤ .05 in the stratified models was tested for statistical significance by introducing an interaction term with race into the original combined model. Pearson’s r was used to explore simple correlations between baseline weight loss outcome expectancies and the initiation and intensity of breastfeeding. Responses at 12 months and the change over time (i.e., response at 12 months minus response at 6 weeks) were calculated, and tested for correlation with lactation score.
For all analyses, a P-value ≤ .05 was used to indicate statistically significant associations. Analysis was performed using SAS 8.2 (Cary, NC).
Results
Comparing women who completed the 12 month follow-up with those who did not, we found no statistically significant differences in age group, race, work outside the home, parity, BMI category, or intervention arm. Women who were unmarried, were smokers, and had less education were somewhat less likely to have completed the follow-up, though these differences were not significant after controlling for the other sociodemographic covariates (data not shown).
Baseline characteristics of the sample are presented in Table 1. The mean BMI was 33 (±6.4) and a high proportion of the women were black. Most had a college or graduate degree, were married, and planned to return to work full-time. There were few smokers, and the proportion having cesarean delivery was high.
Table 1.
Sample characteristics
| Variable | Total (n = 450) % (n) |
|---|---|
| Age (mean [SD]) | 30.9 (5.6) |
| 18–24 | 14.2 (64) |
| 25–34 | 55.8 (251) |
| 35+ | 30.0 (135) |
| Race | |
| White/other | 54.9 (247) |
| Black | 45.1 (203) |
| Education | |
| High school graduate or less | 45.1 (203) |
| College degree | 33.3 (150) |
| Postgraduate degree | 21.6 (97) |
| Marital status | |
| Single | 31.3 (141) |
| Married | 68.7 (309) |
| Plan to work outside home (at 6 mo pp) | |
| Not work outside the home | 19.2 (86) |
| Parttime | 18.0 (81) |
| Fulltime | 62.8 (282) |
| Parity | |
| 1 | 41.1 (185) |
| 2 | 36.0 (162) |
| 3+ | 22.9 (103) |
| Current smoking | |
| Yes | 5.8 (26) |
| Postpartum depression | |
| Yes | 8.7 (39) |
| Delivery type | |
| Vaginal | 61.9 (274) |
| Cesarean section | 38.2 (169) |
| Gestational age (weeks; mean [SD]) | 38.4 (2.1) |
| Preterm birth (<37 weeks) | 11.6 (52) |
| Gestational weight gain (kg; mean [SD])[24] | 14.9 (8.7) |
| Under IOM recommendations | 19.6 (88) |
| Within IOM recommendations | 20.8 (93) |
| Above IOM recommendations | 59.6 (267) |
| Body mass index (kg/m2; mean [SD]) [23] | 33.0 (6.4) |
| 25–29.9 (overweight) | 40.0 (180) |
| 30–34.9 (obese class I) | 31.3 (141) |
| 35–39.9 (obese class II) | 15.6 (70) |
| 40+ (obese class III) | 13.1 (59) |
| Initiation of breastfeeding | |
| Never breastfed | 31.1 (140) |
| Breastfed | 68.9 (310) |
| Duration of breastfeeding (months [1–12]; mean [SD])a |
7.2 (4.0) |
| Lactation score (intensity [1–24]; mean [SD])a |
12.4 (7.8) |
Among breastfeeders only; measured at 12 month follow-up
Sixty-nine percent of participants initiated breastfeeding. Among those who breastfed, the mean duration of breastfeeding was 7.2 months (±4.0), and the mean lactation score was 12.4 (±7.8). Figure 2 details the proportions fully breastfeeding or mixed feeding in each of the 12 months postpartum (among those who completed the 12 month follow-up, n = 385).
Fig. 2.
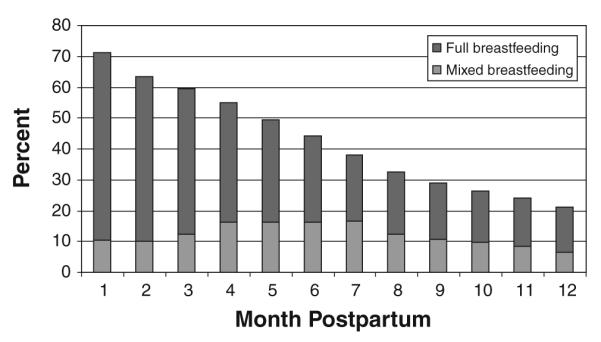
Breastfeeding in the first year postpartum. Percent fully breastfeeding or combining with formula (mixed feeding) by month among those completing the 12-month survey (n = 385)
Bivariate relationships are presented in Table 2. Women who were older, more educated, married, and non-smokers were more likely to breastfeed and have higher lactation scores. Black women were less likely to initiate breastfeeding and had lower lactation scores than women of other races. Women with preterm births and fewer children were less likely to initiate breastfeeding, and women working full-time had lower lactation scores.
Table 2.
Bivariate relationships between predictor variables and breastfeeding initiation and lactation score
| Variable | Initiation of breastfeeding (n = 450) |
Lactation score* (n = 274) |
||
|---|---|---|---|---|
| % | P-value** | Mean (SD) | P-value** | |
| Age | ||||
| 18–24 | 45.3 | <0.0001 | 8.2 (6.5) | 0.02 |
| 25–34 | 74.5 | 13.0 (7.8) | ||
| 35+ | 69.6 | 12.3 (8.0) | ||
| Race | ||||
| White/other | 76.5 | 0.0001 | 14.0 (7.9) | <0.0001 |
| Black | 59.6 | 9.8 (6.9) | ||
| Education | ||||
| High school graduate or less | 59.1 | <0.0001 | 10.5 (7.9) | 0.003 |
| College degree | 70.0 | 12.7 (7.7) | ||
| Postgraduate degree | 87.6 | 14.5 (7.5) | ||
| Marital status | ||||
| Single | 53.2 | <0.0001 | 9.1 (6.3) | 0.0001 |
| Married | 76.1 | 13.4 (8.0) | ||
| Plan to work outside home (at 6 mo pp) | ||||
| Not work outside the home | 76.7 | 0.14 | 16.1 (7.9) | <0.0001 |
| Parttime | 71.6 | 13.5 (8.7) | ||
| Fulltime | 66.0 | 10.8 (7.0) | ||
| Parity | ||||
| 1 | 68.1 | 0.03 | 11.3 (7.9) | 0.16 |
| 2 | 63.6 | 12.8 (7.9) | ||
| 3+ | 78.6 | 13.6 (7.6) | ||
| Current smoking | ||||
| No | 70.5 | 0.003 | 12.6 (7.8) | 0.007 |
| Yes | 42.3 | 5.6 (5.3) | ||
| Postpartum depression | ||||
| No | 69.6 | 0.30 | 12.4 (7.8) | 0.66 |
| Yes | 61.5 | 11.6 (8.4) | ||
| Delivery type | ||||
| Vaginal | 70.8 | 0.21 | 12.6 (7.9) | 0.48 |
| Cesarean section | 65.1 | 11.9 (7.7) | ||
| Preterm birth (<37 weeks) | ||||
| No | 71.3 | 0.005 | 12.6 (7.8) | 0.12 |
| Yes | 51.9 | 9.6 (8.4) | ||
| Gestational weight gain [24] | ||||
| Under IOM recommendations | 65.9 | 0.56 | 11.8 (7.5) | 0.52 |
| Within IOM recommendations | 73.1 | 13.4 (8.0) | ||
| Above IOM recommendations | 68.5 | 12.2 (7.9) | ||
| Body mass index (kg/m2) [23] | ||||
| 25–29.9 (overweight) | 75.0 | 0.003 | 14.0 (7.9) | 0.004 |
| 30–34.9 (obese class I) | 72.3 | 10.9 (7.6) | ||
| 35–39.9 (obese class II) | 60.0 | 13.1 (7.9) | ||
| 40+ (obese class III) | 52.5 | 9.1 (6.8) | ||
Significant P-values in bold
Range = 1–24
Chi-square test for differences in proportions; ANOVA and t-tests for differences in means
Body mass index was negatively correlated with both initiation of breastfeeding and lactation score. Figure 3 presents breastfeeding by weight category at initiation and at 6 and 12 months postpartum.
Fig. 3.
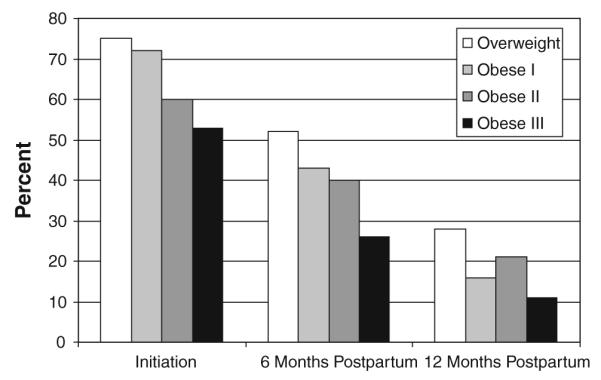
Breastfeeding by BMI group. Initiation of breastfeeding (n = 450), and percent continuing to breastfeed at 6 and 12 months among those completing the 12-month survey (n = 385)
In multivariable models (Table 3), education, gestational age and BMI remained significant predictors of breastfeeding initiation. For every unit increase in BMI, the relative odds of initiating breastfeeding were reduced by 4% (OR: .96; CI: .92–.99). Among those who initiated breastfeeding, black race, working full-time, parity, smoking, gestational age and BMI all had significant effects on lactation score. Each unit increase in BMI reduced the lactation score by 0.22 (P = 0.01).
Table 3.
Multivariable analysis: predictors of breastfeeding initiation (logistic regression) and lactation score (linear regression)
| Variable | Initiation of Breastfeeding (n = 450) |
Lactation score (n = 274) |
||
|---|---|---|---|---|
| Adjusted odds ratio |
Confidence interval |
Effect size | P-value | |
| Age (years) | 1.01 | (0.96, 1.06) | 0.02 | 0.83 |
| Racea | ||||
| Black | 0.81 | (0.46, 1.42) | −3.13 | 0.006 |
| Educationb | ||||
| College degree | 1.27 | (0.72, 2.23) | 1.20 | 0.31 |
| Postgraduate degree | 2.77 | (1.26, 6.08) | 2.11 | 0.12 |
| Marital statusc | ||||
| Married | 1.38 | (0.78, 2.45) | −1.01 | 0.44 |
| Plan to work outside home (at 6 mo pp)d | ||||
| Parttime | 0.69 | (0.31, 1.54) | −1.49 | 0.30 |
| Fulltime | 0.60 | (0.33, 1.21) | −4.26 | 0.0005 |
| Parity | 1.30 | (0.94, 1.81) | 1.85 | 0.006 |
| Current smokinge | ||||
| Yes | 0.45 | (0.18, 1.14) | −7.06 | 0.008 |
| Postpartum depressiong | ||||
| Yes | 0.77 | (0.36, 1.67) | −1.44 | 0.42 |
| Delivery typef | ||||
| Cesarean section | 0.78 | (0.48, 1.25) | −0.69 | 0.47 |
| Gestational age (weeks) | 1.12 | (1.01, 1.25) | 0.65 | 0.002 |
| Gestational weight gain (kg) | 1.01 | (0.97, 1.02) | −0.0004 | 0.99 |
| Body mass index (kg/m2) | 0.96 | (0.92, 0.99) | −0.22 | 0.01 |
| Intervention arm | 0.14 | 0.87 | ||
| Intercept (R-square) | 16.7 | (0.24) | ||
Significant P-values in bold
Reference categories: all other races;
high school graduate or less;
single;
do not plan to work outside the home;
nonsmoker;
vaginal delivery;
not depressed
The separate analyses for blacks and whites suggested tendencies toward racial differences—for example, increasing education had a significant positive effect on lactation score for black women, although this was not found in the overall sample or in the stratified model for whites. In models including interaction terms between race and these covariates, however, none of the interaction terms were significant at the .05 level (data not shown).
Among ever breastfeeders at 12 months (n = 274), the third most commonly endorsed reason for breastfeeding was that it would help the mother lose weight (n = 202). Other common reasons for breastfeeding were to benefit the health of the baby (n = 268), to bond with the baby (n = 234), to reduce feeding costs (n = 190), and convenience (n = 178). As for whether breastfeeding would help with weight loss, 37% of women at baseline answered “7” (“certain to happen”) and 80% answered 5 or higher. However, this variable was not significantly correlated with either breastfeeding initiation or lactation score (data not shown).
Belief that breastfeeding would enhance weight loss decreased from 6 weeks to 12 months postpartum, at which time 27% responded “7” and 69% responded 5 or higher. This measure at 12 months was negatively correlated with lactation score (Pearson’s r = −0.13, P = .04), as was the change in beliefs over time (Pearson’s r = −0.16; P = 0.009). There were no significant correlations between change in beliefs and BMI or weight change from baseline to follow-up, although heavier women were less likely to lose weight in this period (data not shown).
Discussion
Within this sample of overweight and obese women, BMI was negatively associated with breastfeeding initiation and intensity. In multivariable analysis, for every 5 units increase in BMI (e.g., every increase in BMI category—overweight to obese class I, class I to class II, etc.) the odds of initiating breastfeeding were reduced by ~20%, and the lactation score was reduced by about 1.1. A drop of this size in lactation score represents more than a month of breastfeeding lost, or more than a month of mixed feeding instead of full breastfeeding.
Bivariate relationships between initiation and duration of breastfeeding and age, race, education, marital status, fulltime work, parity, smoking, and infant gestational age mirrored those in the general population [7–11]. Associations between initiation and several demographic predictors were mitigated after adjusting for education, as has been found elsewhere [25, 26]. Also consistent with previous studies [25, 27, 28], gestational age remained positively associated with both outcomes and full-time work remained negatively associated with intensity after adjustment for covariates. Smokers were only half as likely as non-smokers to initiate breastfeeding in the multivariable model; that this effect was not statistically significant is likely due to the small number of smokers in the sample (n = 26). The effect of smoking on intensity, however, was large enough to be statistically significant, even among the small number of breastfeeders who smoked [28]. Neither postpartum depression nor cesarean delivery were associated with breastfeeding.
Racial Differences in Predictors of Breastfeeding
There were no statistically significant racial differences in the predictors of breastfeeding. However, low educational attainment may be more of a barrier to breastfeeding intensity for blacks than for whites. Though the interaction effect of race with education on lactation score was sizable, it did not achieve statistical significance (β 3.60, P = 0.09 for college; β 2.94, P = 0.24 for postgraduate). Thus, although breastfeeding predictors did not differ statistically by race, overweight and obese African-American women with the lowest levels of education may be at particularly high risk for early breastfeeding cessation.
Our findings can be compared to those of Kugyelka et al. [29] and Liu et al. [30] who found no effect of BMI on initiation or duration of breastfeeding in stratified analyses including only black women. In our similar stratified analyses, we found no effect of BMI on initiation among black women but did find an effect on intensity (β −0.26; P = 0.02, adjusted for covariates). This effect was not significantly different from that among whites, however, when tested using an interaction term for race*BMI in the model including the entire sample (β −0.09; P = 0.58).
Breastfeeding and Weight Loss for Overweight Women
Breastfeeding can promote postpartum weight loss, particularly when continued for at least 6 months [31, 32]. The women in our sample were familiar with this idea, but beliefs related to breastfeeding and weight loss at baseline were not associated with breastfeeding initiation or intensity. Interestingly, expectations regarding weight loss decreased overall from baseline to follow-up, while both higher expectations at 12 months and increasing expectations over time were associated with lower lactation scores. It may be that women with more experience breastfeeding (e.g., higher lactation scores) reduced their expectations of weight loss to realistic levels, but it may also be that women with persistent, unrealistically high expectations for postpartum weight loss gave up on lactation earlier. Future research should explore this possibility in greater detail.
Limitations of the Study
The question “have you ever breastfed your baby” was not asked among formula feeders at baseline. Some women (n = 29) may have initiated breastfeeding but stopped by 6 weeks postpartum, making the crude initiation rate conservative. This may also have impacted the intensity analysis; however, both breastfeeders and formula feeders were lost to follow-up, and we found no systematic differences between those who completed follow-up and those who did not. The breastfeeding measure we used did not account for supplementation with juice or water. However, the lactation score summarizes breastfeeding intensity without utilizing such information, and is appropriate to the present analysis, since the outcome of interest is duration and exclusivity of breastfeeding behavior, and not volume of lactation. Also, the breastfeeding measures are based on recall at 12 month follow-up—however, recall methods are standard practice for national surveillance [33] and breastfeeding recall has been shown to be valid up to 3 years postpartum [34].
The proportion of women who initiated breastfeeding was slightly larger than has been reported in other samples of overweight and obese women. Women in this study participated in a 9-month behavioral intervention trial, although it is not clear how this might make them different in their breastfeeding behavior from those who did not enroll. Although research participants tend to be more educated than the general population, our participants were racially and sociodemographically diverse. Further, it should be noted that women enrolling in a weight loss trial may be more interested in losing weight, and therefore more sensitive to a perceived lack of weight loss over time. If so, they may be more likely than other women to stop breastfeeding if they experience little postpartum weight loss. This possibility should be considered when interpreting the association between beliefs about lactation and weight loss and the duration of breastfeeding in this group.
The measure of overall body weight status used for these analyses was the more reliable, measured BMI, which was collected 6 weeks postpartum, rather than the self-reported prepregnancy weight. These measures were highly correlated in our sample, however, and since weight tends to be under-reported generally [35] and particularly by overweight persons [36–38], a measured weight is preferred when available. Further, we tested the multivariable models using prepregnancy BMI as the indicator of weight status and achieved similar results. This may limit comparison to other studies, however, as many do not have a measured weight available to use as the indicator of weight status.
Implications for Clinical Practice
Overweight women may have problems initiating breastfeeding due to large breasts, which can make positioning and latching on more difficult [39], and are more likely to experience delayed lactogenesis (milk “coming in”) [40–42]. Obese women are also more likely to experience delivery complications that are independently associated with delayed lactogenesis, including prolonged labor and cesarean delivery [13, 43, 44]. Further, obesity is an independent predictor of diminished prolactin response, which can impact the establishment of successful lactation and lead to diminished lactation performance in the short term [45]. Accordingly, obese women are more likely to discontinue breastfeeding within only a few weeks of delivery [16, 46].
Providers often do not realize that these women are less likely to breastfeed successfully nor do they counsel overweight women differently because of their weight [47]. Recent evidence has shown that interventions to encourage and support breastfeeding can positively affect breastfeeding uptake and duration [6, 48, 49], and resources are available to inform practitioners about the special needs and concerns of overweight and obese women [50–52]. Our study also shows, as with the general population [53,54], that overweight and obese mothers who are black or have a high school or less than high school education are at particularly high risk of early breastfeeding cessation.
Finally, overweight and obese breastfeeding women expecting to lose weight postpartum may be frustrated if this weight loss is not realized, and this may impact their commitment to sustained breastfeeding. In these cases, a likely barrier to weight reduction is excess caloric intake, which itself promotes weight retention but also offsets the energy deficit produced by lactation [55, 56]. These women need continued counseling to manage their expectations around the effect of breastfeeding on weight loss, and can be advised to reduce their overall caloric intake to promote moderate and sustainable weight reduction: reducing energy intake by 500 kilocalories per day in overweight, fully breastfeeding women has been shown to produce an average weight loss of 0.5 kg per week without affecting lactation or infant growth [56]. Moreover, the potential negative impact of beliefs about breastfeeding and weight loss requires further study, as it may represent a previously unrecognized, modifiable risk factor for reduced breastfeeding among overweight and obese women. The most commonly cited reason for breastfeeding in this group was the health of baby, and emphasizing this point is likely the best way to encourage breastfeeding among overweight women.
Conclusion
BMI was negatively correlated with both initiation and intensity of breastfeeding in this sample of overweight and obese women. These women did not appear to have additional unique risk factors for reduced breastfeeding, although overweight mothers who are black and less educated may be an especially high-risk group. Overweight and obese women may become discouraged if they don’t experience weight loss during breastfeeding, and should be counseled to manage their weight loss expectations and to moderate their overall caloric intake to support postpartum weight loss. In general, overweight and obese women may need additional encouragement to consider breastfeeding and to continue breastfeeding during the infant’s first year.
Acknowledgments
This work was supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIH; R01 DK064986). The original trial through which these data were collected is registered with ClinicalTrials.gov (NCT00212251).
Footnotes
Conflicts of interest The authors have no conflicts of interest to disclose.
Contributor Information
Katrina M. Krause, Department of Community and Family Medicine, Duke University Medical Center, Box 104006, Durham, NC 27710, USA
Cheryl A. Lovelady, Department of Nutrition, University of North Carolina at Greensboro, Greensboro, NC, USA
Truls Østbye, Department of Community and Family Medicine, Duke University Medical Center, Box 104006, Durham, NC 27710, USA.
References
- 1.American Academy of Pediatrics. Work Group on Breastfeeding Breastfeeding and the use of human milk. Pediatrics. 1997;100(6):1035–1039. doi: 10.1542/peds.100.6.1035. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Global strategy for infant and young child feeding. World Health Organization; Geneva: 2003. [Google Scholar]
- 3.James DC, Dobson B, American Dietetic Association Position of the American Dietetic Association: Promoting and supporting breastfeeding. Journal of the American Dietetic Association. 2005;105(5):810–818. doi: 10.1016/j.jada.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 4.Ip S, Chung M, Raman G, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evidence Report/Technology Assessment (Full Rep) 2007;153:1–186. [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health, Human Services U.S. Government Printing Office; Washington, DC: Healthy people 2010: Understanding and improving health. (2nd ed.) 2000
- 6.US Preventive Services Task Force Agency for Healthcare Research and Quality: Guide to Clinical Preventive Services. Available at: http://www.ahrq.gov/clinic/uspstfix.htm. See also (specific breastfeeding recommendation) http://www.ahrq.gov/clinic/uspstf/uspsbrfd.htm.
- 7.Ryan AS, Wenjun Z, Acosta A. Breastfeeding continues to increase into the new millennium. Pediatrics. 2002;110(6):1103–1109. doi: 10.1542/peds.110.6.1103. [DOI] [PubMed] [Google Scholar]
- 8.Ahluwalia IB, Morrow B, Hsia J, Grummer-Strawn LM. Who is breast-feeding? Recent trends from the pregnancy risk assessment and monitoring system. Journal of Pediatrics. 2003;142(5):486–491. doi: 10.1067/mpd.2003.199. [DOI] [PubMed] [Google Scholar]
- 9.McDowell MA, Wang C-Y, Kennedy-Stephenson J. NCHS data briefs, no 5. National Center for Health Statistics; Hyattsville, MD: 2008. Breastfeeding in the United States: Findings from the National Health and Nutrition Examination Surveys 1999–2006. [PubMed] [Google Scholar]
- 10.Li R, Darling N, Maurice E, Barker L, Grummer-Strawn LM. Breastfeeding rates in the United States by characteristics of the child, mother, or family: The 2002 national immunization survey. Pediatrics. 2005;115(1):e31–e37. doi: 10.1542/peds.2004-0481. (Epub 2004 Dec 3) [DOI] [PubMed] [Google Scholar]
- 11.Li R, Ogden C, Ballew C, Gillespie C, Grummer-Strawn L. Prevalence of exclusive breastfeeding among US infants: The third national health and nutrition examination survey (Phase II, 1991–1994) American Journal of Public Health. 2002;92(7):1107–1110. doi: 10.2105/ajph.92.7.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amir LH, Donath SM. Does maternal smoking have a negative physiological effect on breastfeeding? The epidemiological evidence. Birth. 2002;29(2):112–123. doi: 10.1046/j.1523-536x.2002.00152.x. [DOI] [PubMed] [Google Scholar]
- 13.Dewey KG. Maternal and fetal stress are associated with impaired lactogenesis in humans. Journal of Nutrition. 2001;131(11):3012S–3015S. doi: 10.1093/jn/131.11.3012S. [DOI] [PubMed] [Google Scholar]
- 14.Hilson JA, Rasmussen KM, Kjolhede CL. Maternal obesity and breast-feeding success in a rural population of white women. American Journal of Clinical Nutrition. 1997;66(6):1371–1378. doi: 10.1093/ajcn/66.6.1371. [DOI] [PubMed] [Google Scholar]
- 15.Li R, Jewell S, Grummer-Strawn L. Maternal obesity and breast-feeding practices. American Journal of Clinical Nutrition. 2003;77(4):931–936. doi: 10.1093/ajcn/77.4.931. [DOI] [PubMed] [Google Scholar]
- 16.Baker JL, Michaelsen KF, Sørensen TI, Rasmussen KM. High prepregnant body mass index is associated with early termination of full and any breastfeeding in Danish women. American Journal of Clinical Nutrition. 2007;86(2):404–411. doi: 10.1093/ajcn/86.2.404. [DOI] [PubMed] [Google Scholar]
- 17.Amir LH, Donath S. A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth. 2007;7:9. doi: 10.1186/1471-2393-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Østbye T, Krause KM, Brouwer RJN, et al. Active Mothers Postpartum (AMP): Rationale, design, and baseline characteristics. Journal of Womens Health (Larchmt) 2008;17(10):1567–1575. doi: 10.1089/jwh.2007.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Østbye T, Krause KM, Lovelady CA, et al. Active Mothers Postpartum (AMP): A randomized controlled weight loss intervention trial. American Journal of Preventive Medicine. 2009;37(3):173–180. doi: 10.1016/j.amepre.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 21.Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry. 1990;157:288–290. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
- 22.Ohlin A, Rössner S. Maternal body weight development after pregnancy. International Journal of Obesity. 1990;14(2):159–173. [PubMed] [Google Scholar]
- 23.National Heart, Lung and Blood Institute (NHLBI) Obesity Education Initiative Expert Panel . NIH publication no.98-4083. National Institutes of Health; Sep, 1998. Clinical guidelines onthe identification, evaluation, and treatment of overweight and obesity in adults. 1998. [Google Scholar]
- 24.Institute of Medicine . Weight gain during pregnancy: Reexamining the guidelines. National Academies Press; Washington, D.C.: 2009. [PubMed] [Google Scholar]
- 25.Hendricks K, Briefel R, Novak T, Ziegler P. Maternal and child characteristics associated with infant and toddler feeding practices. Journal of the American Dietetic Association. 2006;106(1 Suppl 1):S135–S148. doi: 10.1016/j.jada.2005.09.035. [DOI] [PubMed] [Google Scholar]
- 26.Heck KE, Braveman P, Cubbin C, Chávez GF, Kiely JL. Socioeconomic status and breastfeeding initiation among California mothers. Public Health Reports. 2006;121(1):51–59. doi: 10.1177/003335490612100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Donath SM, Amir LH. Effect of gestation on initiation and duration of breastfeeding. Archives of Disease in Childhood: Fetal and Neonatal. 2008;93(6):F448–F450. doi: 10.1136/adc.2007.133215. (Epub 2008 May 1) [DOI] [PubMed] [Google Scholar]
- 28.Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of breastfeeding duration: Evidence from a cohort study. Pediatrics. 2006;117(4):e646–e655. doi: 10.1542/peds.2005-1991. [DOI] [PubMed] [Google Scholar]
- 29.Kugyelka JG, Rasmussen KM, Frongillo EA. Maternal obesity is negatively associated with breastfeeding success among hispanic but not black women. Journal of Nutrition. 2004;134(7):1746–1753. doi: 10.1093/jn/134.7.1746. [DOI] [PubMed] [Google Scholar]
- 30.Liu J, Smith MG, Dobre MA, Ferguson JE. Maternal obesity and breast-feeding practices among white and black women. Obesity (Silver Spring) 2009 Jun 11; doi: 10.1038/oby.2009.182. 2009. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Dewey KG. Impact of breastfeeding on maternal nutritional status. Advances in Experimental Medicine and Biology. 2004;554:91–100. doi: 10.1007/978-1-4757-4242-8_9. [DOI] [PubMed] [Google Scholar]
- 32.Baker JL, Gamborg M, Heitmann BL, Lissner L, Sørensen TI, Rasmussen KM. Breastfeeding reduces postpartum weight retention. American Journal of Clinical Nutrition. 2008;88(6):1543–1551. doi: 10.3945/ajcn.2008.26379. [DOI] [PubMed] [Google Scholar]
- 33.Grummer-Strawn LM, Li R. US national surveillance of breastfeeding behavior. Journal of Human lactation. 2000;16(4):283–290. doi: 10.1177/089033440001600403. [DOI] [PubMed] [Google Scholar]
- 34.Li R, Scanlon KS, Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews. 2005;63(4):103–110. doi: 10.1111/j.1753-4887.2005.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 35.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: A systematic review. Obesity Reviews. 2007;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 36.Nawaz H, Chan W, Abdulrahman M, Larson D, Katz DL. Self-reported weight and height: Implications for obesity research. American Journal of Preventive Medicine. 2001;20(4):294–298. doi: 10.1016/s0749-3797(01)00293-8. [DOI] [PubMed] [Google Scholar]
- 37.Elgar FJ, Stewart JM. Validity of self-report screening for overweight and obesity. Evidence from the Canadian community health survey. Canadian Journal of Public Health. 2008;99(5):423–427. doi: 10.1007/BF03405254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shields M, Gorber SC, Tremblay MS. Estimates of obesity based on self-report versus direct measures. Health Reports. 2008;19(2):61–76. [PubMed] [Google Scholar]
- 39.Chapman DJ, Pérez-Escamilla R. Identification of risk factors for delayed onset of lactation. Journal of the American Dietetic Association. 1999;99(4):450–454. doi: 10.1016/S0002-8223(99)00109-1. [DOI] [PubMed] [Google Scholar]
- 40.Hilson JA, Rasmussen KM, Kjolhede CL. High prepregnant body mass index is associated with poor lactation outcomes among white, rural women independent of psychosocial and demographic correlates. Journal of Human Lactation. 2004;20(1):18–29. doi: 10.1177/0890334403261345. [DOI] [PubMed] [Google Scholar]
- 41.Lovelady CA. Is maternal obesity a cause of poor lactation performance. Nutrition Reviews. 2005;63(10):352–355. doi: 10.1111/j.1753-4887.2005.tb00113.x. [DOI] [PubMed] [Google Scholar]
- 42.Dewey KG, Nommsen-Rivers LA, Heinig MJ, Cohen RJ. Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics. 2003;112(3 Pt 1):607–619. doi: 10.1542/peds.112.3.607. [DOI] [PubMed] [Google Scholar]
- 43.Linné Y. Effects of obesity on women’s reproduction and complications during pregnancy. Obesity Reviews. 2004;5(3):137–143. doi: 10.1111/j.1467-789X.2004.00147.x. [DOI] [PubMed] [Google Scholar]
- 44.Rasmussen KM. Association of maternal obesity before conception with poor lactation performance. Annual Review of Nutrition. 2007;27:103–121. doi: 10.1146/annurev.nutr.27.061406.093738. [DOI] [PubMed] [Google Scholar]
- 45.Rasmussen KM, Kjolhede CL. Prepregnant overweight and obesity diminish the prolactin response to suckling in the first week postpartum. Pediatrics. 2004;113(5):e465–e471. doi: 10.1542/peds.113.5.e465. [DOI] [PubMed] [Google Scholar]
- 46.Donath SM, Amir LH. Maternal obesity and initiation and duration of breastfeeding: Data from the longitudinal study of Australian children. Maternal and Child Nutrition. 2008;4(3):163–170. doi: 10.1111/j.1740-8709.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rasmussen KM, Lee VE, Ledkovsky TB, Kjolhede CL. A description of lactation counseling practices that are used with obese mothers. Journal of Human Lactation. 2006;22(3):322–327. doi: 10.1177/0890334406290177. [DOI] [PubMed] [Google Scholar]
- 48.Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database Systematic Reviews. 2007;1:CD001141. doi: 10.1002/14651858.CD001141.pub3. [DOI] [PubMed] [Google Scholar]
- 49.Labarere J, Gelbert-Baudino N, Ayral AS, et al. Efficacy of breastfeeding support provided by trained clinicians during an early, routine, preventive visit: A prospective, randomized, open trial of 226 mother-infant pairs. Pediatrics. 2005;115(2):e139–e146. doi: 10.1542/peds.2004-1362. [DOI] [PubMed] [Google Scholar]
- 50.Jevitt C, Hernandez I, Groër M. Lactation complicated by overweight and obesity: Supporting the mother and newborn. Journal of Midwifery Womens Health. 2007;52(6):606–613. doi: 10.1016/j.jmwh.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 51.Walker M. Breastfeeding management for the clinician: Using the evidence. Jones and Bartlett Publishers; Sudbury, MA: 2006. Influence of the maternal anatomy and physiology on lactation; pp. 51–82. [Google Scholar]
- 52.Mok E, Multon C, Piguel L, et al. Decreased full breastfeeding, altered practices, perceptions, and infant weight change of prepregnant obese women: A need for extra support. Pediatrics. 2008;121(5):e1319–e1324. doi: 10.1542/peds.2007-2747. [DOI] [PubMed] [Google Scholar]
- 53.Centers for Disease Control, Prevention (CDC) Racial and socioeconomic disparities in breastfeeding—United States, 2004. MMWR Morbidity and Mortality Weekly Report. 2006;55(12):335–339. [PubMed] [Google Scholar]
- 54.Centers for Disease Control, Prevention (CDC) Breastfeeding trends and updated national health objectives for exclusive breastfeeding—United States, birth years 2000–2004. MMWR Morbidity and Mortality Weekly Report. 2007;56(30):760–763. [PubMed] [Google Scholar]
- 55.Winkvist A, Rasmussen KM. Impact of lactation on maternal body weight and body composition. Journal of Mammary Gland Biology Neoplasia. 1999;4(3):309–318. doi: 10.1023/a:1018706131168. [DOI] [PubMed] [Google Scholar]
- 56.Lovelady CA, Garner KE, Moreno KL, Williams JP. The effect of weight loss in overweight, lactating women on the growth of their infants. New England Journal of Medicine. 2000;342(7):449–453. doi: 10.1056/NEJM200002173420701. [DOI] [PubMed] [Google Scholar]


