Abstract
Purpose
To perform a reliable non-invasive detection of the fetal achondroplasia using maternal plasma.
Methods
We developed a quantitative fluorescent-polymerase chain reaction (QF-PCR) method suitable for detection of the FGFR3 mutation (G1138A) causing achondroplasia. This method was applied in a non-invasive detection of the fetal achondroplasia using circulating fetal-DNA (cf-DNA) in maternal plasma. Maternal plasmas were obtained at 27 weeks of gestational age from women carrying an achondroplasia fetus or a normal fetus.
Results
Two percent or less achondroplasia DNA was reliably detected by QF-PCR. In a woman carrying a normal fetus, analysis of cf-DNA showed only one peak of the wild-type G allele. In a woman expected an achondroplasia fetus, analysis of cf-DNA showed the two peaks of wild-type G allele and mutant-type A allele and accurately detected the fetal achondroplasia.
Conclusions
The non-invasive method using maternal plasma and QF-PCR may be useful for diagnosis of the fetal achondroplasia.
Keywords: Achondroplasia, Non-invasive prenatal diagnosis, Maternal plasma, QF-PCR
Introduction
Achondroplasia is the most common form of dwarfism in humans. It results from an autosomal dominant mutation in the fibroblast growth factor receptor 3 gene (FGFR3). The majority of cases appear to be de novo mutations. In about 98% of cases, a G to A point mutation at nucleotide 1138 of the FGFR3 gene (G1138A) causes a glycine to arginine substitution [1–4].
Achondroplasia is generally detected by abnormal prenatal ultrasound findings in the third trimester of pregnancy. It is then confirmed by molecular genetic testing of fetal genomic DNA obtained by percutaneous umbilical blood sampling (PUBS). These invasive procedures present a small but significant risk for both the fetus and mother. Therefore, non-invasive procedures using circulating fetal DNA (cf-DNA) in maternal plasma have been studied for the detection of the fetal achondroplasia mutation and improved via applications of various molecular methods.
Using polymerase chain reaction (PCR) and restriction fragment length polymorphism analysis (RFLP), Saito et al. were able to detect the FGFR3 mutation in the plasma of a woman carrying a fetus suspected of having achondroplasia [5]. Since this report, the FGFR3 mutation was detected in maternal plasma by molecular methods such as size fractionation method, touchdown PCR-RFLP and matrix-assisted laser desorption/ionization time of flight mass spectrometry (MALDI-TOF MS) [6, 7]. However, these methods required a large volume of maternal blood and additional size fractionation process. Therefore, we considered a method to detect the fetal achondroplasia with a small volume of maternal blood without size fractionation process and developed a modified method that combined RFLP with a quantitative fluorescence-PCR (QF-PCR). Here we present data showing that a modified QF-PCR can be performed on a small quantity of achondroplasia DNA and this method can be used to confidently detect the fetal achondroplasia in maternal plasma.
Materials and methods
Sample collection and processing
All samples used in this study were collected under an appropriate IRB approval of the Ethics Committee at Cheil General Hospital (#CGH-IRBGR-2009–10) and written informed consent was obtained for this study. To establish a QF-PCR method for detection of the FGFR3 mutation in a small quantity of achondroplasia DNA, peripheral bloods were obtained from a female carrier of the mutant A-allele (n = 1) and a non-pregnant female blood donor (n = 1). Achondroplasia genomic DNA and normal genomic DNA was extracted using a QIAamp blood DNA kit (Qiagen, USA). DNA concentration was measured using ND-1000 Spectrophotometer (NanoDrop Technologies, Inc., USA) and adjusted to 10 ng/μL using deionized water. The lower limit of detection as well the inter-assay precision was determined using 1-in-2 dilution steps and five replicates. To determine the usefulness of this method in real maternal plasma, maternal peripheral bloods were obtained at 27 weeks of gestational age from a normal healthy pregnant woman expecting an achondroplasia fetus (n = 1) and a normal healthy pregnant woman carrying a normal fetus (n = 1). Immediately after blood sampling, the maternal plasma was separated from the whole blood by centrifugation at 2,500 g for 10 min. Recovered plasma was then centrifuged for an additional 10 min at 16,000 g to remove cell debris and other small molecular particles. The cf-DNA was extracted from 0.5 mL maternal plasma using a commercially available QIAamp DSP Virus Kit (QIAGEN, Germany). Fetal bloods were obtained by PUBS to verify QF-PCR results of the cf-DNA in maternal plasma. Fetal and maternal genomic DNA was extracted using a QIAamp blood DNA kit (Qiagen, USA) from the buffy-coats of the fetal and maternal blood samples.
QF-PCR method for detection of achondroplasia
PCR was used to amplify the FGFR3 polymorphic region. The primer set for PCR was as follows: forward: 5′-AGGAGCTGGTGGAGGCTGA-3′, reverse: 5′- GGAGATCTTGTGCACGGTGG-3′. The reverse primer was labeled with 6-carboxyfluorescein. The PCR reaction solution contained 10 pM primers, 0.25 mM dNTPs, 1.5 mM MgCl2, 1 X buffer, 0.25 U Taq polymerase, and 1 μL mixed genomic DNA or 5 μL of cf-DNA per 20 μL of total reaction volume. PCR conditions included pre-denaturation at 95°C for 5 min, 30 cycles of 95°C for 30 sec, 68°C for 15 sec, 72°C for 30 sec, and a final extension at 72°C for 10 min.
Restriction digestion was used to distinguish the alleles in the FGFR3 polymorphic region. The PCR products (5 μL) were added to a 1 X restriction enzyme buffer that contained bovine serum albumin and 1 U of SfcI restriction enzyme (New England Biolabs, USA). The final reaction volume was adjusted to 15 μL using deionized water. These mixtures were incubated overnight at 37°C. After restriction enzyme digestion, the mixtures were purified using a PCR purification kit (BIONEER, Korea). They were analyzed on an Applied Biosystems 3100 Avant genetic analyzer (Applied Biosystems Inc., USA) using the Pop-4 polymer and GeneScan-500 ROX size standard (Applied Biosystems Inc., USA).
QF-PCR results were confirmed by direct sequencing. After PCR amplification using unlabeled fluorescence primer, PCR products were purified using a PCR purification kit (BIONEER, Korea) and sequenced using a PRISM BigDye Terminator Cycle Sequencing Kit (Applied Biosystems Inc., USA) and a reverse primer. Sequencing products were analyzed using a PRISM 3100 Genetic Analyzer (Applied Biosystems Inc., USA) and electropherogram traces were interpreted with Genescan software version 3.7 (Applied Biosystems Inc., USA). Corresponding genotypes were assigned using Genotyper software version 3.7 (Applied Biosystems Inc., USA).
Statistical analysis
Allelic ratios in all dilution steps were calculated as follows: peak height of mutant-type A allele/peak height of wild-type G allele. The inter-assay precision was presented as coefficient of variation (CV). Statistical analysis was performed using Microsoft Excel.
Results
In QF-PCR of achondroplasia genomic DNA, mutant-type A allele and wild-type G allele were presented as 107-bp and 161-bp fragment, respectively. Table 1 presents peak height of each allele and allelic ratio according to dilution factor of achondroplasia genomic DNA. The CV was less than 10% in both of the two alleles and was less than 15% in allelic ratios. Peak height of wild-type G allele was not different among the dilution factors. However, peak height of mutant-type A allele and allelic ratio were reduced in a dilution factor-dependent manner. Moreover, QF-PCR reliably detected the mutant-type A allele in 2% or less achondroplasia DNA (dilution factor: 1/64). However, direct sequencing could not detect the fetal achondroplasia mutation in these dilution factors (data not shown).
Table 1.
QF-PCR results of achondroplasia genomic DNA according to dilution factor
| Dilution factor | Peak height of G allele | Peak height of A allele | Allelic Ratio | |||
|---|---|---|---|---|---|---|
| Mean ± SD | CV (%) | Mean ± SD | CV (%) | Mean ± SD | CV (%) | |
| 1 | 3729.0 ± 237.9 | 6.3 | 3704.4 ± 238.1 | 6.4 | 0.99 ± 0.09 | 9.5 |
| 1/2 | 3691.8 ± 253.5 | 6.8 | 3667.2 ± 249.4 | 6.8 | 0.99 ± 0.09 | 9.5 |
| 1/4 | 3665.4 ± 284.3 | 7.8 | 3603.4 ± 238.1 | 6.6 | 0.98 ± 0.10 | 10.2 |
| 1/8 | 3677.4 ± 280.9 | 7.6 | 3153.4 ± 286.8 | 9.0 | 0.84 ± 0.09 | 10.7 |
| 1/16 | 3741.2 ± 287.9 | 7.7 | 2808.4 ± 244.5 | 8.7 | 0.71 ± 0.07 | 9.8 |
| 1/32 | 3671.6 ± 300.9 | 8.2 | 1652.8 ± 161.0 | 9.7 | 0.45 ± 0.05 | 11.9 |
| 1/64 | 3629.2 ± 293.0 | 8.1 | 848.4 ± 84.4 | 9.9 | 0.23 ± 0.03 | 14.5 |
| 0 | 3751.1 ± 221.4 | 5.9 | 0 | – | 0 | – |
CV coefficient of variation, SD standard deviation
Dilution factor was determined according to 1-in-2 dilution steps of achondroplasia genomic DNA and normal female genomic DNA. Allelic ratio was calculated as peak height of mutant-type A allele/peak height of wild-type G allele
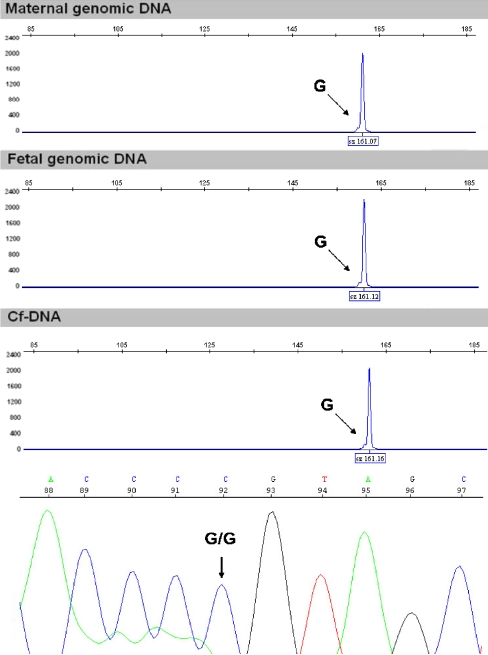
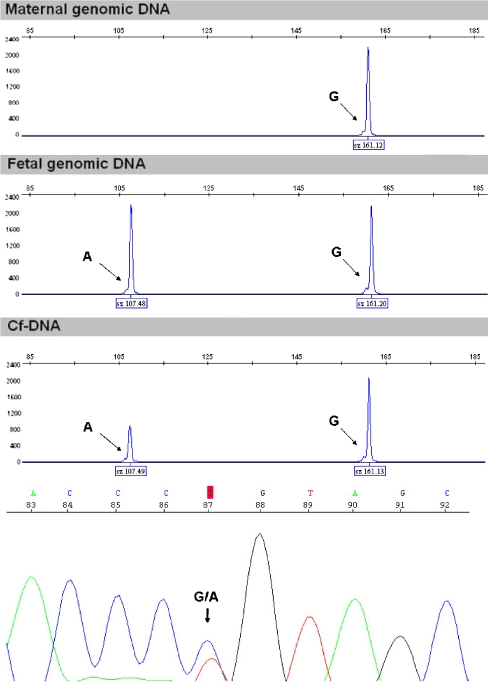
Figure 1 shows the QF-PCR results in a pregnant woman with a normal fetus. All samples including maternal genomic DNA, fetal genomic DNA and cf-DNA showed only one peak of the wild-type G allele. Figure 2 shows the QF-PCR results in a pregnant woman expecting an achondroplasia fetus. Maternal genomic DNA showed only one peak for the 161-bp fragment representing the wild-type G allele. The fetal genomic DNA and cf-DNA showed two peaks including a 107-bp fragment representing the mutant-type A allele and a 161-bp fragment representing the wild-type G allele. Allelic ratios in fetal genomic DNA and cf-DNA were 0.99 ± 0.05 (CV: 5.1%) and 0.41 ± 0.05 (CV: 12.2%), respectively. QF-PCR results of cf-DNA were confirmed by direct sequencing and produced identical results (Figs. 1 and 2).
Fig. 1.
QF-PCR results in a pregnant woman with a normal fetus (n = 1). Maternal genomic DNA, fetal genomic DNA and cf-DNA showed only one peak for the 161-bp fragment representing the wild-type G allele of the FGFR3 mutation (G1138A). QF-PCR result of cf-DNA was confirmed by direct sequencing
Fig. 2.
QF-PCR results in a pregnant woman with an achondroplasia fetus (n = 1). Maternal genomic DNA showed only one peak for the 161-bp fragment representing the wild-type G allele of the FGFR3 mutation (G1138A). However, the fetal genomic DNA and cf-DNA accurately showed two peaks including a 107-bp fragment representing the mutant-type A allele and a 161-bp fragment representing the wild-type G allele of the FGFR3 mutation (G1138A). QF-PCR result of cf-DNA was confirmed by direct sequencing
Discussion
Following the detection of cf-DNA in maternal plasma [8], maternal plasma is being widely used as a new material in non-invasive prenatal diagnostics research. Especially, it is considered as a material for diagnosing single gene disorders, because the cf-DNA in maternal plasma have the potential to provide for non-invasive prenatal diagnosis of single gene disorders in which the mother does not have genomic alterations in the target sequence [5, 9].
In previous reports, the fetal mutant fragment in the FGFR3 G1138A polymorphic region was detected by non-invasive method using the maternal plasma at the third trimester of pregnancy (more than 30 weeks of gestational age) [5–7]. Especially, Li et al. emphasized a size fractionation method to increase the quantity of cf-DNA in maternal plasma. Although this approach required a large volume of maternal plasma and additional process such as agarose gel electrophoresis and re-extraction of DNA from the agarose section, analysis of size fractionated cf-DNA successfully detected the fetal FGFR3 mutation using touchdown PCR-RFLP and MOLDI-TOF MS.
In this study, we extracted cf-DNA using a DSP viral kit from a small volume of the maternal plasma at the second trimester of pregnancy (27 weeks of gestational age) and then successfully detected a FGFR3 mutation of fetus in the maternal plasma using QF-PCR combined with restriction enzyme analysis. Our data demonstrate that the extraction of cf-DNA using a DSP virus kit, along with the high sensitivity of QF-PCR, may lead to the successful detection of fetal achondroplasia in maternal plasma at the second trimester of pregnancy.
Recent findings have shown that the length of most fetal DNA fragments is found to be <300 bp [6, 7, 10] and an extraction system optimized for viral DNA is favoring small-size DNA fragments [11–13]. Rijnders et al. were able to detect fetal DNA at 5 weeks of gestation using the Ultrasens Virus Kit [11] and Clausen et al. reported that the DSP Virus Kit gave a higher yield of cf-DNA than of circulating total DNA in maternal plasma [12]. Moreover, in a workshop report about cf-DNA, Legler et al. reported that using the DSP Virus Kit was an optimal method for extracting a high yield of cf-DNA from total plasma [13]. We therefore designed this study based on these previous reports and were able to extract the cf-DNA using a small amount of maternal plasma.
The introduction of fluorescence based PCR such as real-time PCR and QF-PCR to detect fetal DNA from maternal plasma are increasing the number of potential applications in non-invasive prenatal diagnostic research. Among them, QF-PCR is now commonly employed in routine clinical practice and is often employed as an initial diagnostic method for aneuploidy detection. However, it needs the fetal genomic DNA isolated by invasive procedures such as amniocentesis, chorionic villus sampling and PUBS [14–16]. In the non-invasive prenatal diagnostic studies using QF-PCR, González-González et al. successfully performed a detection of fetal sex and a diagnosis of Huntington’s disease [17, 18]. We were also able to detect the fetal achondroplasia via QF-PCR using cf-DNA in maternal plasma at the second trimester of pregnancy. This data indicates that the high sensitivity of this technique may provide the ability for the detection of a small quantity of cf-DNA in maternal plasma.
To the best of our knowledge, this is the first study to detect a G1138A mutation in the FGFR3 by QF-PCR using cf-DNA in maternal plasma. Our data indicates that QF-PCR using cf-DNA in maternal plasma may be effective for the non-invasive prenatal diagnosis of achondroplasia. However, there are limitations as follows; First, negative results were controlled by an invasive test because no control for the presence of fetal DNA was included in this approach. In addition, the level of accuracy could not compare with the level of accuracy when using invasive procedures due to the lack of larger clinical trials reporting the sensitivity and specificity of this novel diagnostic procedure. Our results therefore need to be confirmed by further studies in a larger cohort.
Conclusions
The use of this technique may prove useful in the non-invasive prenatal diagnosis of achondroplasia, as well as other autosomal dominant disorders caused by single gene point mutation.
Acknowledgements
The study was supported by a research grant of the Life Insurance Philanthropy Foundation.
Footnotes
Capsule Non-invasive diagnosis of the fetal achondroplasia is possible using maternal plasma and QF-PCR.
Contributor Information
Jae Hyug Yang, Phone: +82-2-2000-7683, FAX: +82-2-2278-4574.
Hyun Mee Ryu, Phone: +82-2-2000-7683, FAX: +82-2-2278-4574, Email: hmryu@yahoo.com.
References
- 1.Shiang R, Thompson LM, Zhu YZ, Church DM, Fielder TJ, Bocian M, et al. Mutations in the transmembrane domain of FGFR3 cause the most common genetic form of dwarfism, achondroplasia. Cell. 1994;78:335–42. doi: 10.1016/0092-8674(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 2.Bellus GA, Hefferon TW, Ortiz de Luna RI, Hecht JT, Horton WA, Machado M, et al. Achondroplasia is defined by recurrent G380R mutations of FGFR3. Am J Hum Genet. 1995;56:368–73. [PMC free article] [PubMed] [Google Scholar]
- 3.Rousseau F, Bonaventure J, Legeai-Mallet L, Pelet A, Rozet JM, Maroteaux P, et al. Mutations of the fibroblast growth factor receptor-3 gene in achondroplasia. Horm Res. 1996;45:108–10. doi: 10.1159/000184768. [DOI] [PubMed] [Google Scholar]
- 4.Trujillo-Tiebas MJ, Fenollar-Cortés M, Lorda-Sánchez I, Díaz-Recasens J, Carrillo Redondo A, Ramos-Corrales C, et al. Prenatal diagnosis of skeletal dysplasia due to FGFR3 gene mutations: a 9-year experience: prenatal diagnosis in FGFR3 gene. J Assist Reprod Genet. 2009;26:455–60. doi: 10.1007/s10815-009-9339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saito H, Sekizawa A, Morimoto T, Suzuki M, Yanaihara T. Prenatal DNA diagnosis of a single-gene disorder from maternal plasma. Lancet. 2000;356:1170. doi: 10.1016/S0140-6736(00)02767-7. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Holzgreve W, Page-Christiaens GC, Gille JJ, Hahn S. Improved prenatal detection of a fetal point mutation for achondroplasia by the use of size-fractionated circulatory DNA in maternal plasma-case report. Prenat Diagn. 2004;24:896–8. doi: 10.1002/pd.1030. [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Page-Christiaens GC, Gille JJ, Holzgreve W, Hahn S. Non-invasive prenatal detection of achondroplasia in size-fractionated cell-free DNA by MALDI-TOF MS assay. Prenat Diagn. 2007;27:11–7. doi: 10.1002/pd.1608. [DOI] [PubMed] [Google Scholar]
- 8.Lo YM, Corbetta N, Chamberlain PF, Rai V, Sargent IL, Redman CW, et al. Presence of fetal DNA in maternal plasma and serum. Lancet. 1997;350:485–7. doi: 10.1016/S0140-6736(97)02174-0. [DOI] [PubMed] [Google Scholar]
- 9.Chiu RW, Lau TK, Leung TN, Chow KC, Chui DH, Lo YM. Prenatal exclusion of beta thalassaemia major by examination of maternal plasma. Lancet. 2002;360:998–1000. doi: 10.1016/S0140-6736(02)11086-5. [DOI] [PubMed] [Google Scholar]
- 10.Chan KC, Zhang J, Hui AB, Wong N, Lau TK, Leung TN, et al. Size distributions of maternal and fetal DNA in maternal plasma. Clin Chem. 2004;50:88–92. doi: 10.1373/clinchem.2003.024893. [DOI] [PubMed] [Google Scholar]
- 11.Rijnders RJ, Luijt RB, Peters ED, Goeree JK, Schoot CE, Ploos Van Amstel JK, et al. Earliest gestational age for fetal sexing in cell-free maternal plasma. Prenat Diagn. 2003;23:1042–4. doi: 10.1002/pd.750. [DOI] [PubMed] [Google Scholar]
- 12.Clausen FB, Krog GR, Rieneck K, Nielsen LK, Lundquist R, Finning K, et al. Reliable test for prenatal prediction of fetal RhD type using plasma from RhD negative women. Prenat Diagn. 2005;25:1040–4. doi: 10.1002/pd.1248. [DOI] [PubMed] [Google Scholar]
- 13.Legler TJ, Liu Z, Mavrou A, Finning K, Hromadnikova I, Galbiati S, et al. Workshop report on the extraction of foetal DNA from maternal plasma. Prenat Diagn. 2007;27:824–9. doi: 10.1002/pd.1783. [DOI] [PubMed] [Google Scholar]
- 14.Cirigliano V, Ejarque M, Cañadas MP, Lloveras E, Plaja A, Perez MM, et al. Clinical application of multiplex quantitative fluorescent polymerase chain reaction (QF-PCR) for the rapid prenatal detection of common chromosome aneuploidies. Mol Hum Reprod. 2001;7:1001–6. doi: 10.1093/molehr/7.10.1001. [DOI] [PubMed] [Google Scholar]
- 15.Pertl B, Kopp S, Kroisel PM, Tului L, Brambati B, Adinolfi M. Rapid detection of chromosome aneuploidies by quantitative fluorescence PCR: first application on 247 chorionic villus samples. J Med Genet. 1999;36:300–3. [PMC free article] [PubMed] [Google Scholar]
- 16.Schmidt W, Jenderny J, Hecher K, Hackelöer BJ, Kerber S, Kochhan L, et al. Detection of aneuploidy in chromosomes X, Y, 13, 18 and 21 by QF-PCR in 662 selected pregnancies at risk. Mol Hum Reprod. 2000;6:855–60. doi: 10.1093/molehr/6.9.855. [DOI] [PubMed] [Google Scholar]
- 17.González-González C, Garcia-Hoyos M, Trujillo-Tiebas MJ, Lorda-Sanchez I, Alba MR, Infantes F, et al. Application of fetal DNA detection in maternal plasma: a prenatal diagnosis unit experience. J Histochem Cytochem. 2005;53:307–14. doi: 10.1369/jhc.4A6400.2005. [DOI] [PubMed] [Google Scholar]
- 18.González-González MC, Garcia-Hoyos M, Trujillo-Tiebas MJ, Bustamante Aragonés A, Rodriguez de Alba M, Diego Alvarez D, et al. Improvement in strategies for the non-invasive prenatal diagnosis of Huntington disease. J Assist Reprod Genet. 2008;25:477–81. doi: 10.1007/s10815-008-9256-8. [DOI] [PMC free article] [PubMed] [Google Scholar]