Abstract
Coping strategies are emerging as a predictor of treatment outcome for substance users, and may be particularly important among computerized and self-change approaches. We used data from a randomized clinical trial of a computer-based version of cognitive-behavioral therapy (CBT4CBT), in order to: (1) examine the association between observer ratings of coping skills and self-reported coping strategies; (2) evaluate whether participants assigned to the CBT4CBT program reported greater use of coping strategies compared with those not exposed to the program; and (3) examine the differential effect of coping strategies by treatment group on drug-related outcomes. Individuals (N = 77) seeking treatment for substance dependence at a community-based outpatient substance abuse treatment facility were recruited and randomized to receive treatment-as-usual (TAU), or TAU plus CBT4CBT, with the Coping Strategies Scale administered at baseline and post-treatment. Self-reported coping strategy use was strongly correlated with observer ratings on a role-play assessment of coping skills. Although no significant group differences were found across time for coping strategy use, results suggested that as coping strategy use increased, drug use decreased, and this relationship was stronger for participants who received CBT4CBT.
Keywords: Cognitive-behavioral therapy, coping strategies, coping skills, computer, substance abuse
There is strong empirical support for the use of cognitive-behavioral therapy (CBT) as a treatment for substance use disorders (Carroll & Onken, 2005; Dutra, et al., 2008; Irvin, Bowers, Dunn, & Wong, 1999). Cognitive-behavioral theories of self-control view individuals as capable of exercising influence over their own behaviors (Merbaum & Rosenbaum, 1980). A comparatively unique feature of CBT is that it emphasizes increasing the individual’s ability to cope with high-risk situations that commonly lead to relapse (Marlatt & Gordon, 1985). Thus, a main focus of CBT for substance use disorders is to teach clients strategies to cope with these high-risk situations.
There is an emerging literature on the relationship of coping strategies and substance use. Some evidence shows that individuals naturally adopt coping strategies to moderate problem drinking (King & Tucker, 2000; Sugarman & Carey, 2007). However, most of the literature in this area focuses on the use of coping strategies following substance abuse treatment.
Studies with alcohol dependent individuals provide evidence of an inverse relationship between coping strategy use and alcohol use. For example, Moser and Annis (1996) reported that maintaining abstinence during a stressful situation was predicted by total number of coping strategies used. Another study found that alcohol dependent participants who relapsed following inpatient treatment were less likely to indicate use of coping strategies in simulated problem situations (Chaney, O'Leary, & Marlatt, 1978). Similarly, in a study with heroin users, participants who were abstinent at follow-up had greater increased use of coping responses compared to participants who had lapses or relapses (Gossop, Stewart, Browne, & Marsden, 2002).
Several research studies have examined coping skills training interventions (CST), which teach individuals the use of coping skills that are thought to reduce relapse (Monti, et al., 1995; Monti, Rohsenow, Michalec, Martin, & Abrams, 1997). CST has been shown to result in shorter and less severe relapses to cocaine (Monti, et al., 1997; Rohsenow, Monti, Martin, Michalec, & Abrams, 2000). In addition, urge-specific coping skills training research found that alcohol-dependent participants who relapsed in treatment, reported less frequent use of both urge-specific and general coping skills, compared to participants who did not relapse (Monti, et al., 2001). Similarly, with cocaine using participants, urge-specific coping strategies were significantly correlated with cocaine abstinence (Rohsenow, Martin, & Monti, 2005).
A few studies have specifically examined coping strategies and substance use outcomes following CBT treatment. Litt and colleagues (2003) found that coping strategies were predictive of improved treatment outcome in alcohol dependent individuals, but both types of treatment evaluated (CBT vs. interactional) were equally successful at increasing coping strategies. In addition, a study exploring mechanisms of behavior change following treatment for marijuana dependence found that although early use of coping strategies predicted long-term outcomes, there was no significant effect for treatment condition, and coping strategy use decreased over time (Litt, Kadden, Kabela-Cormier, & Petry, 2008).
Research supports the use of computerized-assisted training in CBT for substance use disorders (Carroll, et al., 2008; Carroll, et al., 2009; Hester, Squires, & Delaney, 2005; Strecher, Shiffman, & West, 2005). The effect of participant’s use of coping strategies on treatment-related change has not been evaluated in computer-assisted therapies. This may be a particularly fruitful avenue for research in that the comparatively high level of standardization and consistency associated with computer-based approaches may facilitate clearer understandings of those relationships.
Several previous studies have assessed acquisition of coping skills through behavioral role-play measures (Carroll, Nich, Frankforter, & Bisighini, 1999; Monti, et al., 2001; Rohsenow, et al., 2004; Rohsenow, et al., 2001). Our group recently examined the acquisition of coping skills following eight weeks of computerized CBT for substance use disorders (CBT4CBT; Carroll et al., 2008). Data from this randomized clinical trial showed that quality of coping response mediated the effect of treatment on duration of abstinence (Kiluk, Nich, Babuscio, & Carroll, in press). Examining the relationship between self-reported coping and quality of coping acquisition will strengthen our understanding of these constructs.
This study is a secondary analysis of data from the same randomized clinical trial described above. The aims of this study are to: (1) examine the association between quality of observer ratings of coping skills and frequency of use of self-reported coping strategies; (2) evaluate whether participants assigned to CBT4CBT report greater use of coping strategies compared with those not exposed to the program; and (3) examine the differential effect of coping strategies by treatment group on drug-related outcomes. First, we hypothesized that self-reported use of coping strategies would be strongly correlated with independent ratings of participants’ coping skills, using a standardized role-playing measure. Second, we hypothesized that participants would report increased use of coping strategies through the course of treatment, with greater increases among those assigned to the CBT4CBT condition, given its high level of emphasis on teaching the use of coping skills. Third, we hypothesized that greater use of coping strategies would be associated with decreased substance use at the end of treatment.
Method
Participants
Participants were recruited from individuals seeking treatment at Liberation Program’s Mill Hill clinic, a community based outpatient substance abuse treatment provider in Bridgeport, CT. Participants were English-speaking adults who met DSM-IV criteria for any current substance dependence disorder, including alcohol, cocaine, opioids, or marijuana. Exclusion criteria were minimized to facilitate recruitment of a clinically representative group of individuals seeking treatment in a community setting. Thus, individuals were excluded only if (1) they had not used alcohol or illegal drugs within the past 28 days or failed to meet DSM-IV criteria for a current substance dependence disorder, (2) had an untreated psychotic disorder which precluded outpatient treatment, or (3) were unlikely to be able to complete eight weeks of outpatient treatment due to a planned move or pending court case from which incarceration was likely to be imminent. Of the 155 individuals screened for the study, 77 met inclusion/exclusion criteria, provided written informed consent, and were randomized to receive either CBT4CBT plus treatment-as-usual at the clinic, or treatment-as-usual (TAU) alone. Table 1 shows the demographic characteristics of the sample.
Table 1.
Demographic characteristics for total sample and by treatment group at baseline
| Variable | CBT4CBT | TAU | Total |
|---|---|---|---|
| n = 35 | n = 38 | n = 73 | |
| n (%) | n (%) | n (%) | |
| Female | 15 (42.9) | 16 (42.1) | 31 (42.5) |
| Ethnicity | |||
| African American | 18 (51.4) | 17 (44.7) | 35 (47.9) |
| European American | 10 (28.6) | 15 (39.5) | 25 (34.2) |
| Latin American | 5 (14.3) | 4 (10.5) | 9 (12.3) |
| Native American | 2 (5.7) | 2 (5.2) | 4 (5.5) |
| Married or in stable relationship | 9 (25.7) | 7 (18.4) | 16 (21.9) |
| Employed, full or part time | 1 (20.0) | 10 (26.3) | 17 (23.3) |
| Completed high school education | 25 (71.4) | 15 (78.9) | 55 (75.4) |
| Primary substance use problem | |||
| Cocaine | 20 (57.1) | 23 (60.5) | 43 (58.9) |
| Alcohol | 8 (22.9) | 5 (13.2) | 13 (17.8) |
| Marijuana | 3 (8.6) | 2 (5.3) | 5 (6.8) |
| Opioids | 4 (11.4) | 8 (21.1) | 12 (16.4) |
| On probation or parole | 11 (31.4) | 16 (42.1) | 27 (37.0) |
| Referred through criminal justice system | 9 (25.7) | 11 (28.9) | 20 (27.4) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age | 40.6 (12.0) | 42.5 (8.4) | 41.6 (10.2) |
| Years primary substance used | 16.2 (11.3) | 17.1 (10.8) | 16.7 (11.0) |
| Days any substance use – past 28days | 9.6 (7.8) | 9.9 (8.4) | 9.7 (8.1) |
Treatments
All participants were offered standard treatment at the clinic, which typically consisted of weekly individual and group sessions. Those randomized to the CBT4CBT condition were provided access to the computer program in a small private room within the clinic. A research associate guided participants through their initial use of the CBT4CBT program and was available to answer questions and assist participants each time they used the program. Participants accessed the program through an identification/password system to protect confidentiality. As described in more detail in the report of the randomized trial (Carroll, et al., 2008), the CBT4CBT program was intended to be user-friendly, requiring no previous experience with computers and minimal use of text-based material. The program consisted of six lessons, or modules, the content of which was based closely on a NIDA-published CBT manual (Carroll, 1998) used in several previous randomized controlled trials in a range of substance-using populations (Carroll, et al., 2006; Carroll, et al., 2004; Carroll, et al., 1994). The six modules covered (1) functional analysis of substance use, (2) coping with craving, (3) problem solving skills, (4) refusing offers of drugs and alcohol, (5) managing and changing cognitions, and (6) decision-making skills. The program seeks to convey these specific skills using a range of strategies, including videotaped examples, interactive exercises, narrated instruction, and emphasis on behavioral practice (Carroll et al., 2008).
Of the 73 individuals who initiated treatment, 48 (66%) completed the study (22 in CBT4CBT, 26 in TAU, NS). Levels of exposure to the standard counseling services offered in the program was also comparable in both groups, with those assigned to CBT4CBT completing a mean of 39 days and those assigned to TAU completing 41 days of the 56 day protocol. Hence, analyses of the primary substance use outcomes were not constrained by differential rates of attrition nor data availability. Of those who initiated the CBT4CBT program, the mean number of computer sessions completed was 4.3 (SD = 2.4) of the six modules offered. Participants spent an average of 38.3 (SD = 8.2) minutes per session working with each module. Within CBT4CBT, participants completed an average of three homework assignments, and completion of homework was strongly associated with drug use outcomes in this sample (Carroll, et al., 2008). In terms of primary outcome measures, participants assigned to CBT4CBT as an adjunct to TAU submitted significantly fewer drug-positive urine samples during treatment and sustained longer periods of continuous abstinence during treatment (Carroll et al; 2008). These differences were sustained through a 6-month follow-up, in which participants assigned to TAU tended to increase their substance use over time, while those assigned to CBT4CBT continued to reduce their drug use (Carroll et al., 2009).
Assessments
Substance use
Participants were assessed before treatment, twice weekly during treatment, and at the 8-week treatment termination point by an independent clinical evaluator. Participants were administered the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1995) prior to randomization to establish substance use and psychiatric diagnoses. The Substance Abuse Calendar, similar to the Timeline Follow Back (Fals-Stewart, O'Farrell, Freitas, McFarlin, & Rutigliano, 2000; Hersh, Mulgrew, Van Kirk, & Kranzler, 1999), was administered weekly during treatment to collect detailed day-by-day self-reports of drug and alcohol use throughout the protocol.
Participant self-reports of illegal drug use were verified through urine toxicology screens that were obtained at every assessment visit. Of 578 urine specimens collected during the treatment phase of the study, the majority were consistent with participant self report in that only 58 (10%) were positive for drugs in cases where the participant had denied recent use during the period the drug’s metabolites are typically detectable in urine (3 days for cocaine and opioids, 7 days for marijuana). Breathalyzer samples were also collected at each assessment visit; none indicated recent alcohol use.
Coping strategies
Coping strategies were assessed using a modified version of the Coping Strategies Scale (CSS; Litt, Kadden, Cooney, & Kabela, 2003). The CSS is a self-report measure developed from the Process of Change Questionnaire (Prochaska, Velicer, DiClemente, & Fava, 1988) that was originally designed to assess alcohol-related coping strategies (Litt, et al., 2003; Petry, Litt, Kadden, & Ledgerwood, 2007) . In recent research, the CSS has been modified to assess coping strategies of marijuana users (Litt, et al., 2008) and pathological gamblers (Petry, et al., 2007). For the purposes of this study, we modified the wording of the Litt et al. (2008) 48-item version to generalize to alcohol and other drugs. In addition, we expanded the response scale from a 4-point to 5-point Likert scale. Thus, participants rated the frequency with which they used specific coping strategies during the past week (0 = never, 4 = all the time). The CSS was administered at pretreatment, week 4, and week 9 (post-treatment).
There were two previous evaluations of the factor structure of the CSS with CBT treatments. Litt and colleagues (2003) described developing rationally derived subscales (active-behavioral, active-cognitive, avoidant-behavioral, avoidant-cognitive), and found that the active and avoidant scales were highly correlated (r = .71), as were the behavioral and cognitive scales (r = .82). Results also indicated that type of coping, as measured by the subscales, was not as predictive of outcome as total coping score. Petry and colleagues (2007) conducted a principal components analysis and reported a 4-factor solution that accounted for 45.7% of variance in responses (general coping, emotional coping, remembering negative strategies, and social strategies). However, a composite score of ratings across all of the scale items was used in the analyses. Thus, neither study supported the use of subscale scores.
As a first step, we attempted to confirm the factor structure posited by Litt et al. (2003). We conducted a series of confirmatory factor analyses on the baseline CSS data including a four-factor model (active-cognitive, active-behavioral, avoidant-cognitive, and avoidant-behavioral), as well as both two factor models (active and avoidant, behavioral and cognitive) and a general one factor model. These analyses were conducted with the 50 participants that had complete data on the CSS at baseline. Although this sample size is underpowered for a CFA, we included these results to provide preliminary evidence of the structure of the measure. Neither of the two models indicated adequate fit using Hu and Bentler (1999) criteria. For example, for the 4-factor model, the fit statistics were not acceptable (GFI = .85, CFI = .82, IFI = .82, RMSEA = .08).
Next, we evaluated the CSS items in terms of whether they reflected content specifically covered in one of the CBT4CBT modules. Two of the authors (D.E.S and K.M.C) independently identified 17 items, which rationally corresponded to the content in each of the six modules (functional analysis, coping with craving, refusal skills, problem solving, cognitions, and decision making) and hence would be expected to change differentially with exposure to the CBT4CBT program. We then conducted a confirmatory factor analysis of baseline data including all of the 17 items as one construct, with correlated errors, which showed a good fit (GFI = .90, CFI = .99, IFI = .99, RMSEA = .04). Next, we examined a model with six subscales that reflect the six CBT4CBT modules as independent constructs driven by the construct of CBT skills and found a less acceptable level of fit (GFI = .66, CFI = .86, IFI = .87, RMSEA = .13). Thus, for subsequent analyses, we used the 17-item version as a single scale (CSS-17). The Cronbach’s alpha for the 17 items was .82.
Drug Risk Response Test (DRRT; Carroll, et al., 1999)
The DRRT is a role-play assessment of coping skills for high-risk situations associated with drug use. Participants listen to six high-risk situations on an audiotape. Participants are then asked to imagine themselves in the situation and indicate how they would respond to each situation if it were occurring at that moment. Participants record their response on audio tape and then each response is scored later by independent raters, blind to treatment condition and time (pre- versus post-treatment) using a detailed rating guide. Participants’ responses to each of the six situations were scored on the following variables: (1) latency – the number of seconds between completion of the audio-taped situation and initiation of the participant’s response; (2) number of coping responses provided – the number of plans articulated toward not using drugs or alcohol, or for solving a problem for each situation; (3) number of activities in each response – the number of articulated activities involved within each coping plan; (4) quality of best coping response – the quality of the best response provided in terms of likelihood of drug use. This was rated on a 7-point Likert scale ranging from 1-“would definitely use drugs or alcohol” to 7- “excellent response indicated complete confidence, no chance of using”; (5) quality of overall response – the overall quality of all responses given to each situation was scored according to same 7-point Likert scale. For these 5 dimensions, mean scores are used. Given that these were experienced raters who had participated in multiple previous trials using these instruments, intraclass correlation coefficient estimates for the reliability sample of four tapes, which were rated by all three raters were as follows: latency = .94, number of plans = .90, best response = .85, overall response = .86, and highest category (agreement of the best response category) = .97. For the analyses presented here we selected two variables from the DRRT, which we have demonstrated to be mediators of outcome for CBT4CBT (Kiluk et al, in press): quality of best coping response, and quality of overall coping response scores in these analyses. The DRRT was completed by participants at baseline and post-treatment. At pre-treatment, data were available from 51 participants who completed both the CSS and the DRRT; at post treatment, 44 participants completed both of these assessments.
Data analysis
Correlations were used to examine the association between the CSS-17 self-report scores and the two observer-rated subscores of the DRRT (quality of best coping response, and quality of overall coping response scores in these analyses) that have been shown in the literature to be related to substance use outcomes (Kiluk, et al., in press). Correlations between these two variables were examined at pre-treatment and post-treatment. Random effects regression models were run to evaluate change in CSS-17 scores over time (pre-post treatment) and by treatment condition.
The relationship between self-reported coping strategy score and drug use over time during the active treatment phase of CBT4CBT was evaluated using Aptitude Treatment Interaction (ATI) models. ATI examines the differential effectiveness of at least two treatments (CBT4CBT, TAU) for individuals who vary on at least one relevant aptitude or variable (coping strategy use) (Singer & Willett, 2003). ATI is ideal for these analyses because it allows us to assess the degree to which the two different treatments have different effects on drug use as a function of the individual’s coping strategy use. Participants receiving CBT4CBT are taught skills each week that relate to several of the coping strategies. Thus, we would expect implementation of coping strategies to vary by treatment.
To examine differential impact of self-reported coping strategies on outcome by treatment using ATI modeling, the rate of change in CSS-17 score during the active treatment phase was created using the individual slope estimates from the random effect regression model. Similarly, a random effect regression model was run to create the dependent variable, rate of change in weekly frequency of drug use during active treatment. Because both the independent and dependent variables are based on per-person change, cases with just one data point were excluded from the models, leaving a sample size of 32 participants. One multivariate outlier was determined and excluded from the analysis, leaving 31 cases. The ATI model included the predictor variables treatment condition, the rate of change in CSS-17 indicator, an interaction of the effect coded treatment variable and the rate of change indicator in coping strategies with the per-person rate of change in drug use frequency as the outcome.
Results
Self-reported coping strategies and observer-rated quality of coping skills
As shown in Table 2, pretreatment CSS-17 coping strategy use was significantly correlated with pretreatment DRRT ratings of quality of overall response and quality of best response. This same relationship was observed for correlations of post- treatment CSS-17 scores and post-treatment DRRT subscores. In addition, post-treatment CSS-17 score was significantly correlated with pretreatment quality of best response (r = .36).
Table 2.
Correlations between CSS-17 scores and DRRT scores at pre and post treatment
| Variable | 1 | 2 |
|---|---|---|
| Pre-Treatment (n = 51) | ||
| 1. CSS-17 | ||
| 2. DRRT quality of overall response | .43*** | |
| 3. DRRT quality of best response | .43*** | .99*** |
| Post-Treatment (n = 44) | ||
| 1. CSS-17 | ||
| 2. DRRT quality of overall response | .34* | |
| 3. DRRT quality of best response | .33* | .98*** |
Note. CSS-17 refers to the 17 items of the Coping Strategies Scale that was used in these analyses; DRRT refers to the Drug Risk Response Test.
p < .05
p < .001
Change across time by treatment condition
There were no significant differences in CSS-17 scores from baseline to week 8 using longitudinal analyses (group F[1, 127] =.28, p > .05), time F[1, 113] =.20, p > .05, group by time F[1, 113] =.96, p > .05).
Self-reported coping strategy use and substance use
Results revealed a significant effect of rate of change in CSS-17 scores overall (t = −3.78, p < .001), and a significant interaction of CSS-17 slope and treatment (t = −3.43, p < .01). These findings suggest that, overall, as coping strategies increase, frequency of drug use decreases (main effect of CSS-17 score). In addition, the interaction of treatment condition and CSS-17 slope indicates that the rate of reduction in drug use predicted by coping strategy scores is much greater for CBT4CBT participants compared to TAU. In other words, in the CBT condition, drug use outcomes are more highly correlated with change in coping strategies than in the TAU condition. Figure 1 depicts these findings graphically.
Figure 1.
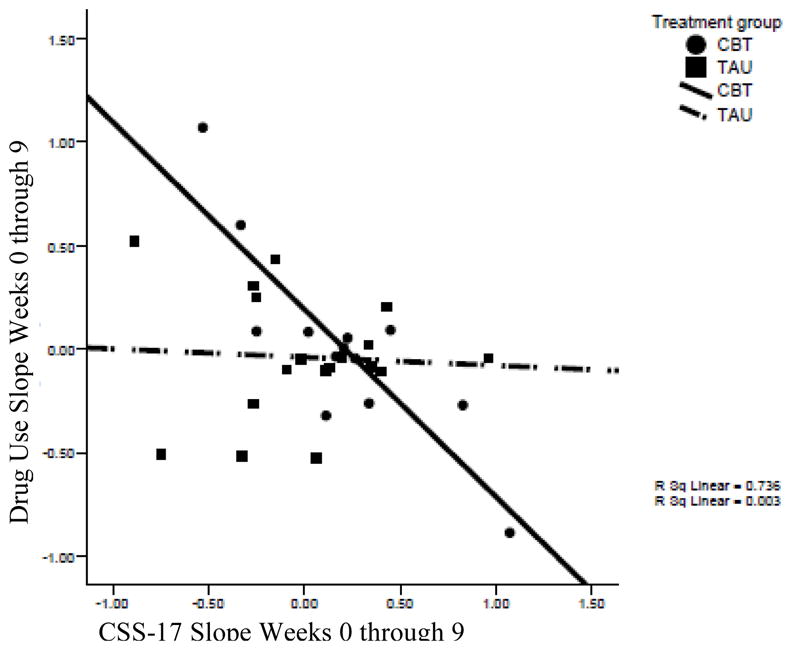
Correlation of change in CSS-17 slope from week 0 through 9 to change in drug use from week 0 through 9, by treatment group (n = 31)
Discussion
This evaluation of coping strategies using data from a randomized clinical trial of computerized CBT as an adjunct to substance abuse treatment suggests the following: (1) the CSS-17 is significantly associated with observer ratings of quality of coping skills both pre- and post-treatment; and (2) increases in coping strategy use during treatment, as measured by the CSS-17, are related to decreases in drug use in participants who engaged in computerized CBT. To date, this is the first study to show that self-reported strategy use is correlated with observer ratings of coping skills based on a role-play task. This finding suggests that the higher frequency of use is associated with higher skill quality ratings.
It was expected that participants in the CBT4CBT group would show increases in coping strategies compared to the TAU group. Surprisingly, there were no group differences in coping strategies across time. It is possible that both groups were using coping strategies at the same rate, but the CBT4CBT group might be using them more effectively. Evidence from the Aptitude Treatment Interaction modeling suggested that as coping strategies increased, frequency of drug use decreased. In particular, for participants in the CBT4CBT condition, drug use outcomes were more highly correlated with change in strategy use than in the TAU condition. These findings suggest that computerized CBT may affect coping strategy use more strongly than TAU, and this increase in coping strategy use is related to decreased drug use. One possibility is that that for the TAU group participants, their substance use may be affected by other behaviors that are emphasized in TAU (e.g. 12-step recovery). Although previous studies have found that coping skill use was predictive of improved treatment outcome, this study is unique in providing evidence that links computerized CBT specifically with a correlation of coping strategies with reduced drug use.
We acknowledge several limitations of this study. First, these were exploratory analyses derived from an existing data set. Second, as is common with substance abuse research, attrition reduced the sample size, and therefore power, for these analyses. Although we present data on the factor structure of the CSS, the small sample size decreases the stability of these analyses, and they should be interpreted cautiously. Third, the reliance on a self-report measure to assess coping strategies may have affected the results. Specifically, the majority of the items on the CSS are desirable behaviors and individuals in treatment may feel that they should being doing these behaviors, which could bias their responses. However, the analyses comparing the self-reported CSS-17 scores with the DRRT role-play measure show that participants’ self-report corresponds significantly to independent ratings of coping skills responses. Finally, due to missing data, the ATI analyses could only examine data from 31 participants. Replication of these findings is necessary with a larger sample.
Despite these limitations, this study has several strengths and important implications. This is the first study to examine treatment-related change in the use of coping strategies following a computerized, and hence highly standardized, version of CBT. Moreover, unlike previous research, this study utilized a clinically representative sample that was not limited to one specific substance use diagnosis. This study also identified a set of coping strategies directly related to the effects of CBT treatment on drug use. Thus, one fruitful area for future coping strategy research may be to more closely link self-reported coping strategy use to those specifically targeted and delivered in the treatment. Moreover, this study was the first to find a significant relationship between self-reported use of coping strategies with observer ratings of quality of coping skills on a role-play measure. Thus, this study extends the literature by suggesting that for individuals who receive the addition of computerized CBT to treatment-as-usual, their substance use is more strongly linked to their use of coping strategies. Future research should examine if this finding is specific to computerized CBT or to CBT in general.
Acknowledgments
Writing of this manuscript was supported by the National Institute on Drug Abuse grants P50-DA09241, R37-DA 015969, U10 DA13038, K05-DA00457, R25DA020515; the VISN 1 Mental Illness Educational, Research, and Clinical Center (MIRECC); and the Office of Academic Affiliations, Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ADB
References
- Carroll KM. A Cognitive-Behavioral Approach: Treating Cocaine Addiction. Rockville, Maryland: NIDA; 1998. [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio T, Gordon MA, et al. Computer-assisted cognitive-behavioral therapy for addiction. A randomized clinical trial of 'CBT4CBT'. American Journal of Psychiatry. Deposited in PMC 15 April 2008. 2008;165:881–888. doi: 10.1176/appi.ajp.2008.07111835. NIHMSID: NIHMS46416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive-behavioral therapy: A six-month follow-up of CBT4CBT. Drug and Alcohol Dependence. PMC journal in process. 2009;100:178–181. doi: 10.1016/j.drugalcdep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, et al. The use of contingency management and motivational/skills-building therapy to treat young adults with marijuana dependence. Journal of Consulting and Clinical Psychology. 2006;74:955–966. doi: 10.1037/0022-006X.74.5.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, et al. Efficacy of disulfiram and cognitive-behavioral therapy in cocaine-dependent outpatients: A randomized placebo controlled trial. Archives of General Psychiatry. 2004;64:264–272. doi: 10.1001/archpsyc.61.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Frankforter TL, Bisighini RM. Do patients change in the way we intend? Treatment-specific skill acquisition in cocaine-dependent patients using the Cocaine Risk Response Test. Psychological Assessment. 1999;11:77–85. [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. American Journal of Psychiatry. 2005;162:1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin FH. One year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: Delayed emergence of psychotherapy effects. Archives of General Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Chaney EF, O'Leary MR, Marlatt GA. Skill training with problem drinkers. Journal of Consulting and Clinical Psychology. 1978;46:1092–1104. doi: 10.1037//0022-006x.46.5.1092. [DOI] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV, Patient Edition. Washington, D.C: American Psychiatric Press; 1995. [Google Scholar]
- Gossop M, Stewart D, Browne N, Marsden J. Factors associated with abstinence, lapse or relapse to heroin use after residential treatment: Protective effect of coping responses. Addiction. 2002;97:1259–1267. doi: 10.1046/j.1360-0443.2002.00227.x. [DOI] [PubMed] [Google Scholar]
- Hersh D, Mulgrew CL, Van Kirk J, Kranzler HR. The validity of self-reported cocaine use in two groups of cocaine abusers. Journal of Consulting and Clinical Psychology. 1999;67:37–42. doi: 10.1037//0022-006x.67.1.37. [DOI] [PubMed] [Google Scholar]
- Hester RK, Squires DD, Delaney HD. The Drinker's Check-up: 12-month outcomes of a controlled clinical trial of a stand-alone software program for problem drinkers. Journal of Substance Abuse Treatment. 2005;28:159–169. doi: 10.1016/j.jsat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff fit criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Irvin JE, Bowers CA, Dunn ME, Wong MC. Efficacy of relapse prevention: A meta-analytic review. Journal of Consulting and Clinical Psychology. 1999;67:563–570. doi: 10.1037//0022-006x.67.4.563. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio TA, Carroll KM. Quantity versus quality: Acquisition of coping skills as a mediator of outcome in computer-assisted cognitive behavioral therapy for substance abuse. Addiction. doi: 10.1111/j.1360-0443.2010.03076.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MP, Tucker JA. Behavior change patterns and strategies distinguishing moderation drinking and abstinence during the natural resolution of alcohol problems without treatment. Psychology of Addictive Behaviors. 2000;14:48–55. doi: 10.1037//0893-164x.14.1.48. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive behavioral and interactional group therapy for alcoholism. Journal of Consulting and Clinical Psychology. 2003;71:118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Coping skills training and contingency management treatments for marijuana dependence: Exploring mechanisms of behavior change. Addiction. 2008;103:638–648. doi: 10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: Guilford; 1985. [Google Scholar]
- Merbaum M, Rosenbaum M. Self-control theory and technique in the modification of smoking, obesity, and alcohol abuse. Clinical Behavior Therapy Review. 1980;2:1–20. [Google Scholar]
- Monti PM, Rohsenow DJ, Colby SM, Abrams DB, Hester RK, Miller WR. Handbook of alcoholism treatment approaches: Effective alternatives. 2. Needham Heights, MA US: Allyn & Bacon; 1995. Coping and social skills training; pp. 221–241. [Google Scholar]
- Monti PM, Rohsenow DJ, Michalec E, Martin RA, Abrams DB. Brief coping skills treatment for cocaine abuse: Substance abuse outcomes at three months. Addiction. 1997;92:1717–1728. [PubMed] [Google Scholar]
- Monti PM, Rohsenow DJ, Swift RM, Gulliver SB, Colby SM, Mueller TI, et al. Naltrexone and cue exposure with coping and communication skills training for alcoholics: Treatment process and 1-year outcomes. Alcoholism: Clinical and Experimental Research. 2001;25:1634–1647. [PubMed] [Google Scholar]
- Moser AE, Annis HM. The role of coping in relapse crisis outcome: A prospective study of treated alcoholics. Addiction. 1996;91:1101–1114. doi: 10.1046/j.1360-0443.1996.91811013.x. [DOI] [PubMed] [Google Scholar]
- Petry NM, Litt MD, Kadden R, Ledgerwood DM. Do coping skills mediate the relationship between cognitive-behavioral therapy and reductions in gambling in pathological gamblers? Addiction. 2007;102:1280–1291. doi: 10.1111/j.1360-0443.2007.01907.x. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, DiClemente CC, Fava JS. Measuring the processes of change: applications to the cessation of smoking. Journal of Consulting and Clinical Psychology. 1988;56:520–528. doi: 10.1037//0022-006x.56.4.520. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Martin RA, Monti PM. Urge-specific and lifestyle coping strategies of cocaine abusers: Relationships to treatment outcomes. Drug and Alcohol Dependence. 2005;78:211–219. doi: 10.1016/j.drugalcdep.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Colby SM, Myers MG, Gulliver SB, et al. Motivational enhancement and coping skills training for cocaine abusers: Effects on substance use outcomes. Addiction. 2004;99:862–874. doi: 10.1111/j.1360-0443.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. Journal of Consulting and Clinical Psychology. 2000;68:515–520. doi: 10.1037//0022-006x.68.3.515. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Rubonis AV, Gulliver SB, Colby SM, Binkoff JA, et al. Cue exposure with coping skills training and communication skills training for alcohol dependence: 6- and 12-month outcomes. Addiction. 2001;96:1161–1174. doi: 10.1046/j.1360-0443.2001.96811619.x. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY US: Oxford University Press; 2003. [Google Scholar]
- Strecher VJ, Shiffman S, West R. Randomized controlled trial of a Web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction. 2005;100:682–688. doi: 10.1111/j.1360-0443.2005.01093.x. [DOI] [PubMed] [Google Scholar]
- Sugarman DE, Carey KB. The relationship between drinking control strategies and college student alcohol use. Psychology of Addictive Behaviors. 2007;21:338–345. doi: 10.1037/0893-164X.21.3.338. [DOI] [PMC free article] [PubMed] [Google Scholar]


