Abstract
Perceived control and health are often closely linked in adulthood and old age. Little is known, however, about their time-ordered interplay at various phases of adult life. By applying dynamic models to four waves of data over 15.5 years from the Americans' Changing Lives study, we examined time-ordered relations between perceived control and health in midlife and old age. Results revealed that levels of perceived control predict subsequent changes in health over time in old age (aged 65+ years, n = 1,238), but not in midlife (aged 25–64 years; n = 2,364). No evidence was found for predictive effects of health for control changes in both age groups. These age-differential findings were corroborated using nested-model comparisons. Predictive effects of perceived control for health were attenuated to the null in models covarying for socio-demographic and psychosocial factors (physical activity, memory, emotional support, and depressive symptoms) suggesting that these variables play an important role in control-health relations. Our discussion focuses on the importance of perceived control for healthy living in old age and the differential implications of perceived control for health in midlife and old age.
Keywords: Control, Health, bivariate dual change score model, Midlife, Old Age, Americans' Changing Lives Study
Lifespan research has long been interested in intra-individual changes within and structural relations between domains of functioning (Baltes & Nesselroade, 1979; Brandtstädter & Lerner, 1999; Magnusson & Cairns, 1996). For example, rich conceptual frameworks highlight the importance of perceived control-health associations for development in midlife and old age (Krause, 2007; Lachman, 2006; Uchino, 2006) and for successful aging (Baltes & Baltes, 1990; Rowe & Kahn, 1987). Perceived control may act as an adaptive capacity to meet the challenges and experiences associated with age, including health that are likely to become more frequent and severe (Lachman, 2006; Rodin, 1986). Concomitantly, age-related declines in health can pose a problem for most individuals and put considerable strain on one's perceived control (Skaff, 2007). Less is known, however, about whether these constructs show dynamic (i.e., time-ordered) interrelations and what variables underlie such associations. It is theorized that control and health are interactive partners in the aging process (Skaff, 2007) and their relationship grows stronger with age (Heckhausen & Schulz, 1995; Rodin, 1986). Our objective in this study is to use data from the Americans' Changing Lives (ACL) study to examine whether dynamic links between perceived control and health exist in midlife and old age and to explore the role of socio-demographic and psychosocial factors for such time-lagged associations.
Perceived control is defined as the belief that changes in the environment are contingent upon one's actions, efforts, and choices (Fung et al., 1999). From a unidirectional perspective, it is argued that perceived control may impact health. For example, several longitudinal studies of older adults have shown that lower self-efficacy relates to stronger declines in physical functioning (Mendes de Leon et al., 1996; Seeman et al., 1999). This protective effect of perceived control was also seen in samples of the oldest old, where greater levels of mastery were protective of disability (Femia et al., 1997). Furthermore, Caplan and Schooler (2003) reported from a 20-year follow-up of adults in midlife and old age that a related construct, self-confidence, was protective of declines in physical functioning.
Health comprises the incidence of diseases that may undermine one's capacities for everyday living (Steinhagen-Thiessen & Borchelt, 1999). There is empirical evidence that health is predictive of perceived control. For example, cross-sectional findings from adult lifespan samples show that poor health and physical impairments relate to lower control beliefs (Lachman & Weaver, 1998; Mirowsky, 1995). In older adults, uncontrollable chronic diseases and poor physical functioning predicted both lower levels and stronger declines in facets of control (McAvay et al., 1996; Penninx et al., 1996). Finally, a 10-year study by Seeman and Lewis (1995) revealed that decreases in health were associated with increases in powerlessness (constraints), whereas 10-year improvements in health were associated with decreases in powerlessness.
Perceived control and health can also be conceptualized as reciprocally interacting domains that both directly and indirectly influence one another (Lachman, 2006; Skaff, 2007). For example, longitudinal data from the Midlife in the United States study found that perceived control predicted subsequent changes in health, and was also an outcome of better health (Gerstorf et al., 2010). Finally, to more thoroughly test whether control–health links were independent of or possibly mediated by a third variable, we included those demographic and psychosocial variables that have been suggested or empirically reported to possibly underlie such associations. A first candidate factor may be shared variances with years of education, which may partly account for sizable correlations between these constructs (Lachman & Weaver, 1998; Rodin, 1986). Similarly, greater support from social network members, namely family, friends, and spouse, is related to both perceived control and health (Antonucci, 2001). Furthermore, people who are more physically active and cognitively fitter typically feel greater control over changes in their environment and also report better health (Lachman, 2006; Mendes de Leon et al., 1996; Seeman et al., 1999). Finally, negative emotionality may also relate to lower levels of control and poorer health (McAvay et al., 1996).
In sum, both conceptual and empirical work suggests that cross-domain links between facets of control and health indeed exist, particularly in later phases of life. Our objective is to further explore questions about their developmental ordering and possible underlying variables. First, we apply a bivariate dual change score model (BDCSM; McArdle & Hamagami, 2001) to longitudinal data from the ACL study and examine dynamic links between perceived control and health in midlife and old age. Based on conceptual and empirical work, we hypothesize that perceived control and health show bi-directional associations such that perceived control predicts changes in health and is an outcome of better health. Additionally, perceived control-health links may differ between midlife and old age. For example, perceived control in midlife may not directly predict changes in health, but instead operate via underlying variables, whose effects typically take longer to accumulate. In contrast, increased risks for declines in health may contribute to control-health associations being stronger and more proximal in old age. Second, we explore whether such lead-lag associations remain independent of socio-demographic and psychosocial factors. We expect that socio-demographic and psychosocial factors will partially account for associations between perceived control and health.
Method
Participants and Procedure
We conducted a secondary data analysis of the ACL Study, a nationally representative stratified probability sample of people aged 25 years and older (House et al., 1990). As designated by the original investigators, the ACL study included an oversampling of African Americans and those aged 60 and older. The measures assessed cover a wide range of sociological, psychological, and physical health information. The ACL study encompasses four waves of data collected in 1986 (n = 3,617), 1989 (n = 2,867), 1994 (n = 2,653), and 2001/2 (n = 1,787) spanning a total of 15.5 years. Participants in the baseline ACL sample were, on average, 54 years of age (SD = 17.62, range 25 – 96) and attained 11 years of education (SD = 3.47), 63% were women, 64% Caucasian, and 55% were married. In this study, we included all participants with valid data on the measures of interest at T1 (N = 3,602). Relative to the remaining 3,617 ACL participants, our subsample did not differ in age (M = 54.03, SD = 17.62 vs. M = 58.14, SD = 18.66; F [1, 3616] = 0.76) and education (M = 11.47, SD = 3.47 vs. M = 9.93, SD = 4.41; F [1, 3616] = 2.77), but included more women (63% vs. 37%; χ2 [1, N = 3,617] = 4.29, p < .05).
Measures
Perceived control was assessed using six items from Pearlin and Schooler's (1978) Mastery and Self-Esteem scale that represent feelings of mastery (e.g., “I can do just about anything I really set my mind to do”). Participants were asked to rate the extent to which they feel their life is under their control using a 4-point Likert scale (1 = strongly agree to 4 = strongly disagree; α = .66). Negatively valenced items were reverse coded so that higher scores indicated greater feelings of control.
Health was assessed by self-reports of the number of health conditions participants were diagnosed with in the past year or currently have, out of a list of 10 health conditions: arthritis/rheumatism, lung disease, hypertension, heart attack and heart trouble, diabetes, cancer/malignant tumor, foot problems, stroke, fractures or broken bones, and loss of urine beyond one's control (see Shaw & Krause, 2001). We used the sum of all health conditions reported and reverse coded the score, with higher scores indicating better health.
Covariates
To examine whether control-health associations were independent of or possibly mediated by a third variable, we included covariates into our models. Physical activity was measured with three items assessing how often participants work in the garden, engage in active sports, and take walks (Parslow et al., 2006). Items were rated on a 4-point Likert scale (1 = often to 4 = never; α = .46) and reverse coded with higher scores indicating more physical activity. Memory was measured by serial 3's with participants being asked to subtract three from twenty and to stop when the answer is two or less (see also McArdle et al., 2007). Our sum score is based on the number of correct responses. Emotional support was measured using six items assessing the degree of support participants receive from children, spouse, and friends or relatives (see Fiori et al., 2006). Items were rated on a 5-point Likert scale (1 = not at all to 5 = a great deal; α = .64) with higher scores indexing greater support. Depressive symptoms were measured using 11 items from the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977; see Umberson et al., 1996), Participants rated how often they had experienced each feeling during the previous week using a 3-point Likert scale (1 = hardly ever to 3 = most of the time; α = .83). Positively valenced items were reverse coded, with higher scores indicating more depressive symptoms.
Data preparation
To ensure a common metric, we standardized perceived control and health to the T metric (M = 50, SD = 10) with the T1 ACL sample (N = 3,602) serving as the reference. We did not want to exclude any of the participants and thus divided the sample into two age groups based on their chronological age at T1, midlife (aged 25–64, n = 2,364) and old age (aged 65 + years, n = 1,238). However, substantively identical findings were obtained when we ran follow-up analyses with the midlife age group containing individuals aged 40-64 (n = 1,319). The descriptive statistics in Table 1 show that mean scores for perceived control remain relatively stable for both age groups, whereas health declines on average across waves. Table 1 also indicates that the midlife group was on average in the early 40s at T1 and approached old age by T4, whereas the old-age group was in their mid 70s and reached very old age over time.
Table 1. Age at Assessment and Descriptive Statistics for Measures Entered Into the Bivariate Dual Change Score Model.
| Measure | Midlife (aged 25 – 64) | Old Age (aged 65 + years) | ||||
|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | |
| Perceived Control | ||||||
| T1 | 2,364 | 50.02 | 9.94 | 1,238 | 49.96 | 10.13 |
| T2 | 1,933 | 50.75 | 9.86 | 915 | 49.28 | 10.31 |
| T3 | 1,801 | 51.31 | 9.27 | 588 | 49.40 | 10.15 |
| T4 | 1,451 | 51.98 | 9.11 | 236 | 49.61 | 9.94 |
| Health | ||||||
| T1 | 2,364 | 52.89 | 8.68 | 1,238 | 44.47 | 10.04 |
| T2 | 1,936 | 52.47 | 8.88 | 922 | 44.34 | 10.32 |
| T3 | 1,835 | 50.99 | 9.42 | 720 | 43.22 | 10.48 |
| T4 | 1,450 | 47.51 | 11.20 | 237 | 42.24 | 10.31 |
| Age | ||||||
| T1 | 2,364 | 43.93 | 12.45 | 1,238 | 73.29 | 6.44 |
| T2 | 1,936 | 47.22 | 12.39 | 922 | 75.63 | 6.01 |
| T3 | 1,835 | 51.81 | 12.24 | 720 | 79.90 | 5.55 |
| T4 | 1,484 | 58.26 | 11.91 | 300 | 85.26 | 4.38 |
| Emotional Support (1-5) | ||||||
| T1 | 2,364 | 4.01 | 0.74 | 1,238 | 4.12 | 0.76 |
| Physical Activity (1-4) | ||||||
| T1 | 2.364 | 2.80 | 0.77 | 1,238 | 2.45 | 0.88 |
| Memory (0-6) | ||||||
| T1 | 2,364 | 5.45 | 1.28 | 1,238 | 4.93 | 1.92 |
| Depressive Symptoms (1-3) | ||||||
| T1 | 2,353 | 1.44 | 0.37 | 1,224 | 1.42 | 0.36 |
| Education (0-17) | ||||||
| T1 | 2,364 | 12.23 | 3.05 | 1,238 | 10.02 | 3.75 |
| Gender (% Women) | ||||||
| T1 | 2,364 | 59% | 1,238 | 69% | ||
Note. Perceived control and Health standardized to the T metric with the Time 1 (T1) Americans' Changing Lives Study sample (N = 3,602) as the reference (M = 50, SD = 10). Baseline assessment or T1 in 1986, Time 2 (T2) in 1989, Time 3 (T3) in 1994, and Time 4 (T4) in 2001-2002.
To quantify longitudinal attrition, we calculated mean longitudinal selectivity for each age group with an effect-size metric indicating the degree to which participants who provided data over 15.5 years differed from the sample at T1 (Lindenberger et al., 2002). For midlife, total selectivity amounted to 0.06 SD for perceived control, 0.14 SD for health, −0.08 SD for age, and 0.18 SD for education, suggesting that selectivity effects were small. For old age, total selectivity amounted to 0.25 SD for perceived control, 0.36 SD for health, −0.53 SD for age, and 0.34 SD for education, suggesting that selectivity effects were relatively larger, with more control, better health, younger age, and more education at T1 relating to higher participation rates. We note that our models give implicitly more weight to information obtained from those positively selected individuals who provided the most change information.
Statistical Procedures
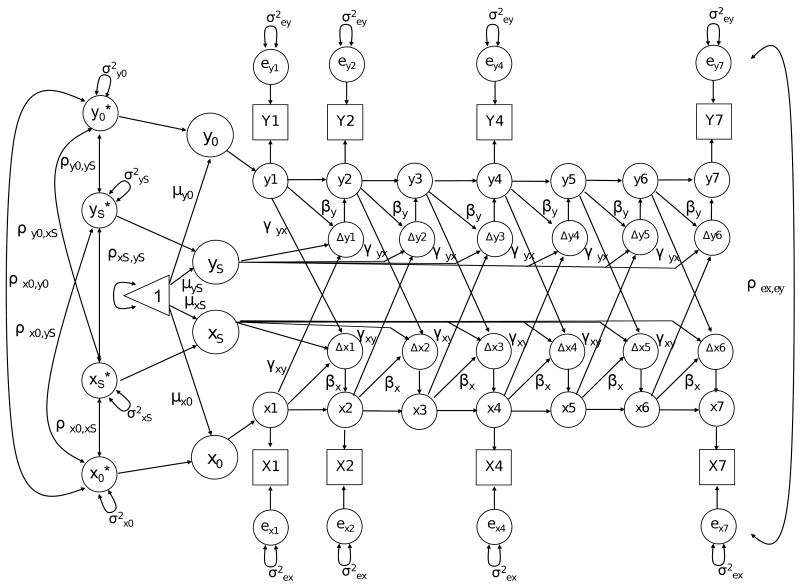
To examine our research questions, we use a BDCSM that is shown in Figure 1. Manifest variables are represented by squares, latent variables by circles, fixed model parameters as one-headed arrows, and random parameters as two-headed arrows; the triangle is used to allow the inclusion of means and intercepts (McArdle & Hamagami, 2001). Unlabeled paths are fixed to 1. The separately estimated error terms (ex; ey) are assumed to be normally distributed with a mean of zero, a time-invariant variance, and uncorrelated with all other components. The observed variables at T1, T2, T4, and T7 represent the assessments of control and health. Following usual practice (Gerstorf et al., 2007;McArdle, 2001), we accommodated the unbalanced design by adding unmeasured ‘node’ variables for occasions on which a given variable was not assessed, as was the case for the ACL study: T2 took place an average of 2.5 years, T3 7.5 years, and T4 15.5 years after T1, respectively. This procedure simplified the estimation and interpretation of model parameters and guaranteed an equal-interval, time-invariant scaling of approximately 2.5 years in-between occasions. The intercept and slope factors account for the time series information of both variables, are estimated at the population level and are allowed to vary and covary.
Figure 1.
Graphical representation of a Bivariate Dual Change Score Model. Observed variables are represented by squares, latent variables by circles, regression weights by one-headed arrows, and variances and covariance by two-headed arrows. The triangle represents a constant indicating means and intercepts. All unlabeled paths are set to 1.
Of particular interest are the latent difference scores, Δx[t] and Δy[t], which represent the reliable change score between adjacent waves. These difference scores are affected by three sets of influence: (i) the linear component of change within a given variable; (ii) the auto-proportion parameter β indicating the effect that level of functioning on one variable at [t] has on subsequent change at [t + 1] of this variable; and (iii) the inter-variable cross-lagged coupling parameter γ representing the effect of the other variable at [t] on subsequent change in the focus variable at [t + 1]. Both β's andγ's are assumed time-invariant. Our major focus is the inter-variable coupling parameters γ that allows for direct empirical testing of substantive hypotheses regarding dynamic links between perceived control and health. Specifically, we use an age-group BDCSM that simultaneously estimates separate models for individuals in midlife and old age and allow testing if parameter estimates differ across age groups. Analyses were conducted using MPlus (Muthén & Muthén, 1998-2007). We applied full information maximum likelihood estimation to all data points available, which allowed treating incomplete data as missing at random (Little & Rubin, 1987) and adjusting for unbalanced data structures (Singer, 1998).1
Results
Dynamic Links of Perceived Control and Health in Midlife and Old Age
The top portion of Table 2 presents results from a series of age-group BDCSM at the zero-order level. A model freely estimating both coupling parameters in each age group (Full Coupling) provided reasonably good fit to our data (e.g., CFI larger than 0.95). This model was the least parsimonious estimated and thus served as a reference to test several constrained versions of this model. Next, models that constrained the two coupling parameters to zero (No Coupling) or be invariant (Equal Couplings) both resulted in significant losses in the chi-square goodness of fit, suggesting that lead-lag associations between perceived control and health indeed exist and are of unequal size. To examine the directionality of associations, we next estimated unidirectional models that fixed either of the two coupling parameters to zero. Specifically, not allowing for health to predict changes in perceived control (Coupling γHealth→Perceived control = 0) was associated with a negligible loss in fit, whereas not allowing for perceived control to predict changes in health (Coupling γPerceived control→Health = 0) resulted in a highly significant and substantial loss in model fit. These nested model comparisons suggest that levels of perceived control predict subsequent changes in health, whereas there was no evidence for effects in the other direction.
Table 2. Goodness-of-Fit Model Comparison Among Alternative Bivariate Models of Perceived Control and Health, Using 15.5-Year Americans' Changing Lives Sample, With and Without Additionally Including Education, Gender, Physical Activities, Memory, Social Support, and Depressive Symptoms.
| Model | χ2 | df | Δ χ2/df | CFI | RMSEA |
|---|---|---|---|---|---|
| Zero-order model | |||||
| Bidirectional | |||||
| Full Coupling | 127.22 | 47 | – | 0.99 | 0.03 |
| Equal Coupling | 139.14 | 49 | 11.92 (2)* | 0.99 | 0.03 |
| No direction | |||||
| No Coupling | 136.39 | 51 | 9.17 (4)* | 0.99 | 0.03 |
| Unidirectional | |||||
| Coupling γperceived control → health = 0 | 135.29 | 49 | 8.07 (2)* | 0.99 | 0.03 |
| Coupling γhealth → perceived control = 0 | 128.66 | 49 | 1.44 (2) | 0.99 | 0.03 |
| Education, gender, memory, physical activities, memory, social support, and depressive symptoms included | |||||
| Bidirectional | |||||
| Full Coupling | 662.84 | 101 | – | 0.94 | 0.06 |
| Equal Coupling | 665.32 | 103 | 2.48 (2) | 0.94 | 0.06 |
| No direction | |||||
| No Coupling | 668.57 | 105 | 5.73 (4) | 0.94 | 0.06 |
| Unidirectional | |||||
| Coupling γperceived control → health = 0 | 667.16 | 103 | 4.32 (2) | 0.94 | 0.06 |
| Coupling γhealth → perceived control = 0 | 663.99 | 103 | 1.15 (2) | 0.94 | 0.06 |
Note. Midlife (aged 25 – 64, n = 2,364); Old Age (aged 65 + years, n = 1,238). CFI = Comparative Fit Index. RMSEA = Root Mean Square Error of Approximation.
p < .05 or below.
To examine whether lead-lag associations differ between midlife and old age, Table 3 shows parameter estimates separately for the two age groups. Of interest are the four dynamics parameters, of which only the γPerceived control→Health = 0.58, SE = 0.25, p < .05, for old age is reliably different from zero. To corroborate the statistical significance of the parameter differences, we tested a series of nested models that hierarchically set the variance, covariance, couplings, and means to be invariant across age groups. As shown in Table 4, setting each of these parameter sets to be invariant across midlife and old age revealed significant losses in model fit. Most importantly, setting the coupling parameters to be invariant resulted in a significant loss in model fit, Δχ2 = 19.31, df = 2, p < .05, corroborating that dynamics differ between midlife and old age. We conclude that levels of perceived control predict subsequent health changes in old age, but not in midlife, and no evidence was found for health predicting control changes.
Table 3. Bivariate Dual Change Score Model of Perceived Control and Health in the Americans' Changing Lives Study: Parameter Estimates for Nested Age-Group Zero-Order Model for Midlife and Old Age.
| Parameter | Midlife (aged 25 – 64) | Old Age (aged 65 + years) | Loss of Model Fit | ||
|---|---|---|---|---|---|
| Estimate | SE | Estimate | SE | Δ χ2/df | |
| Fixed effects | 762.50 (6)* | ||||
| Perceived control initial mean | 50.05* | 0.20 | 49.83* | 0.29 | |
| Perceived control slope mean | 25.15* | 4.96 | 13.86 | 7.14 | |
| Perceived control proportion | -0.47* | 0.09 | -0.21 | 0.18 | |
| Health initial mean | 52.89* | 0.18 | 44.40* | 0.28 | |
| Health slope mean | -8.25 | 4.47 | -27.90* | 9.62 | |
| Health proportion | 0.25* | 0.03 | -0.03 | 0.11 | |
| Random effects | 141.10 (4)* | ||||
| Perceived control initial variance | 59.06* | 2.92 | 50.10* | 3.80 | |
| Perceived control slope variance | 11.30 | 4.19 | 3.41 | 4.06 | |
| Health initial variance | 53.75* | 2.02 | 64.15* | 4.06 | |
| Health slope variance | 3.10* | 0.69 | 19.42 | 14.25 | |
| Covariance | 81.39 (6)* | ||||
| Perceived control initial ↔ slope | 19.84* | 4.24 | 11.43 | 8.15 | |
| Health initial ↔ slope | -10.85* | 2.37 | -8.01 | 5.31 | |
| Perceived control initial ↔ Health initial | 12.83* | 1.80 | 17.68* | 2.69 | |
| Perceived control initial ↔ Health slope | 2.06 | 3.86 | -29.45* | 11.47 | |
| Perceived control slope ↔ Health initial | 9.60* | 2.66 | 6.00 | 4.58 | |
| Perceived control slope ↔ Health slope | -0.30 | 1.86 | -7.06 | 5.23 | |
| Dynamics | 19.31 (2)* | ||||
| γperceived control → health | -0.10 | 0.08 | 0.58* | 0.25 | |
| γhealth → perceived control | -0.03 | 0.03 | -0.09 | 0.09 | |
| Residual variance | |||||
| Perceived control | 41.77* | 1.05 | 54.38* | 2.13 | |
| Health | 24.55* | 0.60 | 39.00* | 1.75 | |
Note. Midlife (aged 25 – 64, n = 2,364); Old Age (aged 65 + years, n = 1,238).
p < .05 or below.
Table 4. Dual Change Score Model: Nested Model Comparison Testing Age Group Differences in Parameter Estimates, and Couplings between Perceived Control, and Health.
| Model | χ2 | df | Δ χ2/df | CFI | RMSEA |
|---|---|---|---|---|---|
| Zero-order model | |||||
| Full Coupling Model | |||||
| Baseline | 127.22 | 47 | – | 0.99 | 0.03 |
| Variance invariance | 268.32 | 53 | 141.10 (6)* | 0.97 | 0.05 |
| Covariance invariance | 349.71 | 59 | 81.39 (6)* | 0.96 | 0.05 |
| Coupling invariance | 369.02 | 61 | 19.31 (2)* | 0.96 | 0.05 |
| Mean invariance | 1,131.52 | 67 | 762.50 (6)* | 0.85 | 0.09 |
Note. Midlife (aged 25 – 64, n = 2,364); Old Age (aged 65 + years, n = 1,238). Baseline model estimates a model that allows for group differences in all model parameters. Variance invariance, covariance invariance, coupling invariance, and mean invariance models constrain the variances in the intercepts and slopes, the random covariances, coupling parameters (i.e., gammas), and the intercepts and slopes (betas set invariant in mean invariance model) to be equal across groups, respectively. CFI = Comparative Fit Index. RMSEA = Root Mean Square Error of Approximation.
p < .05 or below.
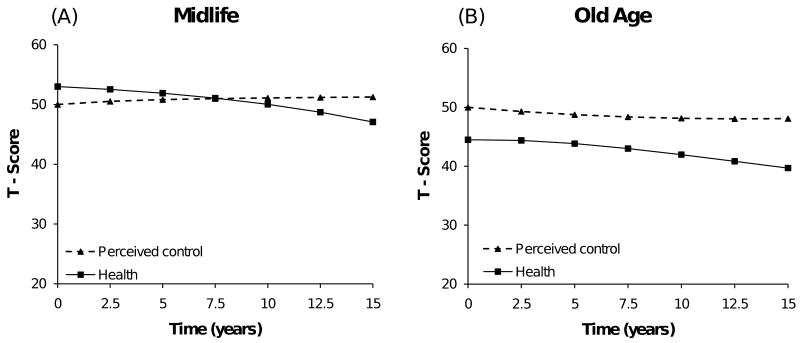
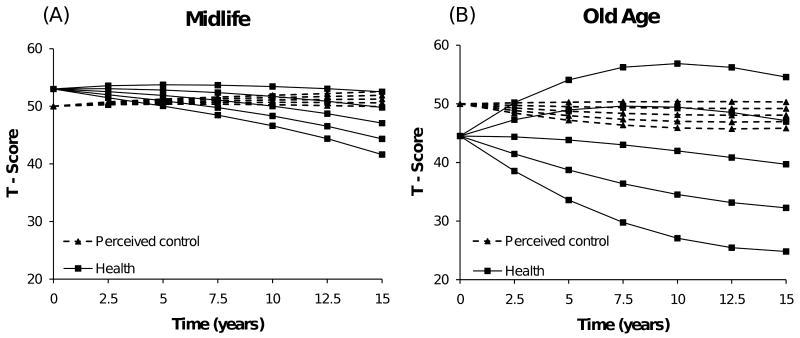
To better understand the differential magnitude and effects of the coupling parameters over time, we first graph the model-implied means for the Full Coupling model in Figure 2, indicating that both age groups remain relatively stable on perceived control, whereas health declines over time. 2 We then determine the differential coupling effects using a hypothetical scenario in which we vary the initial sample means for one variable by half a standard deviation while keeping the initial sample means for the other variable constant. Panel B of Figure 3 indicates that participants in old age with higher initial control show shallower health declines over time, whereas those with lower initial control show steeper health declines. Conversely, model-implied changes in control by altered initial health resulted in minimally different change trajectories. Similarly, Panel A of Figure 3 demonstrates the lack of couplings in midlife by showing that altering initial levels of either control or health did not result in major differences of change trajectories of the other variable.
Figure 2.
Model-implied mean longitudinal change trajectories over time for perceived control (dashed lines) and health (solid lines), for midlife (panel A) and old age (panel B), as revealed from the Bivariate Dual Change Score Model (Full Coupling).
Figure 3.
Graphical illustration of the differential magnitude of the coupling parameters and their effects over time for midlife and old age. Model-implied sample means from the Bivariate Dual Change Score Model (Full Coupling) for the hypothetical case that the initial sample means for one variable were varied by half a standard deviation (i.e., 5 T-score units), while the initial sample means for the other variable were kept constant. Panel B of Figure 3 indicates for this hypothetical scenario that participants in old age with higher initial perceived control show shallower health declines over time (solid lines), whereas those with lower initial perceived control show steeper health declines. Conversely, model-implied changes in perceived control as a function of different initial health resulted in minimal differences in perceived control changes (dashed lines). Similarly, Panel A of Figure 3 demonstrates the lack of couplings in midlife by showing that altering initial levels of either perceived control or health did not result in major differences of change trajectories of the other variable.
The Role of Socio-Demographic and Psychosocial Factors
In a final set of analyses, we tested whether education, gender, physical activity, memory, support, and depressive symptoms, implemented as time-invariant covariates at T1 into our models, account for dynamic perceived control-health links. In these models, the coupling parameters and all other parameters are statistically adjusted for differences in these covariates.
Controlling for the covariates substantially altered the dynamic structure reported above. More specifically, the bottom portion of Table 2 indicates a substantively different pattern. Compared to the Full Coupling model, the various constrained versions of this model do not significantly differ, suggesting that lead-lag associations between perceived control and health can be accounted for by socio-demographics and psychosocial factors. Including the covariates attenuated the predictive effect of perceived control for health changes in old age, γPerceived control→Health = −0.27, SE = 0.32, p > .05. In follow-up analyses, we targeted each covariate in separate models. Results indicated that the complete attenuation of control-health couplings was primarily driven by education, physical activity, and depressive symptoms, whereas gender, memory, and support did not alter the dynamics parameters. Taken together, our results suggest that dynamic control–health links may be mediated by education, physical activity, and depressive symptoms.
Discussion
Our objective was to examine whether perceived control and health are dynamically linked in midlife and old age. Applying an age-group BDCSM to longitudinal ACL data revealed that perceived control predicts health changes in old age, but not midlife. No evidence was found for health predicting ensuing changes in perceived control. We substantiated these age-differential findings in nested-model comparisons. Importantly, models covarying for socio-demographic and psychosocial factors completely attenuated the control-health dynamics suggesting that these variables play an important role in perceived control-health relations. Our discussion focuses on the importance of perceived control for healthy living in old age and the differential implications of control for health in midlife and old age.
Perceived Control and Health are Dynamically Interrelated in Old Age
Our predictive effects of perceived control for old-age changes in health replicate and extend previous reports from longitudinal studies of older adults that perceived control serves as both a protective and risk factor for health (Caplan & Schooler, 2003; Gerstorf et al., 2010; Kempen et al., 1999; Mendes de Leon et al., 1996). These results support and illustrate the role of perceived control for health and successful aging in old age. As a conceptual contribution, our age-differential results suggest that the implications of control for health may be different at various phases of life. In young adulthood and midlife, perceived control may serve more distal functions via operating on mechanisms such as health behaviors and social support, whose effects take longer to accumulate over time. For example, there is empirical evidence to suggest that greater locus of control in childhood predicts age-30 outcomes of not smoking, regular exercise, and a lower risk for obesity (Gale et al., 2008). Additionally, prospective studies reported that control-related constructs such as mature defenses and explanatory style in young adulthood predict later health behaviors and social relationships, which profoundly impact physical health in old age (Friedman et al., 1995; Vaillant & Mukamal, 2001). Conversely, in old age, such effects often have accumulated over a long period of time and may exert their effects more proximally. For example, the experience of irreversible health declines may substantially undermine one's sense of control (Rodin, 1986). A lower sense of control can then be expected to have more immediate and detrimental effects on health outcomes such as chronic disease, disability, and mortality (Fauth et al., 2007; Krause & Shaw, 2000; Penninx et al., 1997).
As a methodological contribution, our study made use of an advanced modeling technique that allowed directly testing competing substantive hypotheses regarding associations between perceived control and health in midlife and old age. However, we acknowledge that these results are contingent upon several strict statistical assumptions, including data missing-at-random and ergodocity. For example, to enable model identification, the dynamic couplings were allowed to differ between age groups but were assumed to be invariant across individuals within age groups. We also recognize that cross-domain interrelations are certainly not adequately depicted with a bivariate system. It is thus pivotal for future studies to replicate and extend upon our initial results.
The Role of Socio-Demographic and Psychosocial Factors
Including socio-demographic and psychosocial factors in our models of control-health associations substantively altered the dynamics reported. This pattern is partially consistent with reports documenting that socio-demographic and psychosocial variables such as education, health behaviors, and emotionality may act as mechanisms underlying control-health associations (Mendes de Leon et al., 1996; Seeman et al., 1999). To begin with, fewer years of education are often associated with fewer opportunities to influence the events that affect one's life, decreased autonomy on the job, and being confronted with more constraints in achieving goals and solving problems (Lachman & Weaver, 1998; Ross & Mirowsky, 2002). Second, individuals with greater perceived control may be more inclined to pursue health-promoting behaviors. For example, reports suggest that more control is associated with not smoking, pursuing regular exercise, eating a healthy diet, and reporting fewer acute and chronic health symptoms (Lachman & Firth, 2004). Third, facets of control are predictive of negative emotionality, including anxiety and depression. For example, more control may allow individuals to better regulate their affective and physiological states, which can promote well-being (Lachman & Firth, 2004; Lang & Heckhausen, 2001). Future studies need to examine these and other possible mechanisms (in earlier phases of adult life) in more detail.
Limitations and Outlook
We acknowledge several limitations of our study. First, we focused on only one aspect of the multidimensional constructs of control and health. Different cross-domain relations may emerge when using measures of domain-specific control (rather than generalized control; Krause & Shaw, 2000) or indices of physical functioning and subjective health (rather than health conditions; Steinhagen-Thiessen & Borchelt, 1999). Second, the observation period spanning 15.5 years led to considerable attrition of older adults over time and involved few measurement occasions spread widely apart. These factors may have limited our ability to adequately capture how change processes unfold over time and how people differ in this regard. As a third limitation, we note the larger residual variance in control relative to the health measure, which may have compromised our statistical power to detect leading effects of health for control.
To close, a number of studies have shown perceived control to be protective of health in midlife and old age (Caplan & Schooler, 2003; Gerstorf et al., 2010; Lachman & Weaver, 1998). Our study has shed some light on the nature of perceived control-health associations in midlife and old age and the variables underlying such relationships. Our findings illustrate the importance of maintaining a strong sense of control despite age-related changes and demonstrate that control is an important indicator of health and successful aging in old age. We also advocated the idea that control may have differential implications for health in midlife and old age. Our study thus provides further impetus to thoroughly examine processes involved in antecedent-consequent relations of perceived control and health.
Acknowledgments
The ACL study was conducted by Jim House and colleagues and was financially supported by grants from the National Institute on Aging (PO1 AG0551 and RO1 AG018418).
Footnotes
In total, this bivariate DCSM estimated 21 parameters, namely two times (one per age group) seven parameters within each of the two time series (means and variances for intercepts and slopes, one time-invariant residual, the auto-proportion parameter, and the intercorrelation between intercept and slope), plus four cross-variable intercorrelations, one covariance of time-invariant residuals between the time series, and two dynamics parameters between the time series. In the models including all covariates, a total of 72 parameters were estimated.
Model-implied means are produced by the formulas x[t] = 1 * Xs + (1 + βx) * x [t – 1] + γyx * y [t – 1] and y[t] = 1 * Ys + (1 + βy) * y [t – 1] + γxy * x [t – 1], which calculate the implied mean longitudinal trajectories from the BDCSM reported in Table 3. Results from the model are translated into change equations that represent change over 2.5 years on a given variable as a function of itself and all other components in the model. More details can be found in Ferrer & McArdle (2004) and Lövdén, Ghisletta, & Lindenberger, (2005).
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/dev
Contributor Information
Frank J. Infurna, Email: infurna@psu.edu.
Denis Gerstorf, Email: gerstorf@psu.edu.
Steven H. Zarit, Email: z67@psu.edu.
References
- Antonucci TC. Social relations: An examination of social networks, social support, and sense of control. In: Birren JE, Schaie KW, editors. Handbook of the psychology of aging. San Diego: Academic Press; 2001. pp. 427–453. [Google Scholar]
- Baltes PB, Baltes MM. Psychological perspectives on successful aging: The model of selective optimization with compensation. In: Baltes PB, Baltes MM, editors. Successful aging: Perspectives from the behavioral sciences. Cambridge, UK: Cambridge University Press; 1990. pp. 1–34. [Google Scholar]
- Baltes PB, Nesselroade JR. History and rationale of longitudinal research. In: Nesselroade JR, Baltes PB, editors. Longitudinal research in the study of behavior and development. New York: Academic Press; 1979. pp. 1–39. [Google Scholar]
- Brandtstädter J, Lerner RM. Action and self development: Theory and research through the lifespan. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- Caplan LJ, Schooler C. The roles of fatalism, self-confidence, and intellectual resources in the disablement process in older adults. Psychology and Aging. 2003;18:551–561. doi: 10.1037/0882-7974.18.3.551. [DOI] [PubMed] [Google Scholar]
- Fauth EB, Zarit SH, Malmberg B, Johansson B. Physical, cognitive, and psychosocial variables from the disablement process model predict patterns of independence and the transition into disability for the oldest-old. The Gerontologist. 2007;47:613–624. doi: 10.1093/geront/47.5.613. [DOI] [PubMed] [Google Scholar]
- Femia EE, Zarit SH, Johansson B. Predicting change in activities of daily living: A longitudinal study of the oldest old in Sweden. Journal of Gerontology: Psychological Sciences. 1997;52B:P294–P302. doi: 10.1093/geronb/52b.6.p294. [DOI] [PubMed] [Google Scholar]
- Ferrer E, McArdle JJ. An experimental analysis of dynamic hypotheses about cognitive abilities and achievement from childhood to early adulthood. Developmental Psychology. 2004;40:935–952. doi: 10.1037/0012-1649.40.6.935. [DOI] [PubMed] [Google Scholar]
- Fiori KL, Antonucci TC, Cortina KS. Social network typologies and mental health among older adults. Journal of Gerontology: Psychological Sciences. 2006;61B:P25–P32. doi: 10.1093/geronb/61.1.p25. [DOI] [PubMed] [Google Scholar]
- Friedman HS, Tucker JS, Schwartz JE, Tomlinson-Keasey C, Martin LR, Wingard DL, et al. Psychosocial and behavioral predictors of longevity: The aging and death of the “Termites”. American Psychologist. 1995;50:69–78. doi: 10.1037//0003-066x.50.2.69. [DOI] [PubMed] [Google Scholar]
- Fung HH, Abeles RP, Carstensen LL. Psychological control in later life: Implications for life-span development. In: Brandstädter J, Lerner RM, editors. Action & self-development: Theory and research through the lifespan. Thousand Oaks, CA: Sage; 1999. pp. 345–372. [Google Scholar]
- Gale CR, Batty GD, Deary IJ. Locus of control at age 10 years and health outcomes and behaviors at age 30 years: the 1970 British Cohort Study. Psychosomatic Medicine. 2008;70:397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Lövdén M, Röcke C, Smith J, Lindenberger U. Well-being affects changes in perceptual speed in advanced old age: Longitudinal evidence for a dynamic link. Developmental Psychology. 2007;43:705–718. doi: 10.1037/0012-1649.43.3.705. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Röcke C, Lachman ME. Antecedent-consequent relations of perceived control to health and social support: Longitudinal evidence for between-domain associations across adulthood. Manuscript submitted for publication. 2010 doi: 10.1093/geronb/gbq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckhausen J, Schulz R. A life-span theory of control. Psychological Review. 1995;102:284–304. doi: 10.1037/0033-295x.102.2.284. [DOI] [PubMed] [Google Scholar]
- House JS, Kessler RC, Herzog AR, Meto RP, Kinney AM, Breslow MJ. Age, socioeconomic status, and health. The Milbank Quarterly. 1990;68:383–411. [PubMed] [Google Scholar]
- Kempen GIJM, van Sonderen E, Ormel J. The impact of psychological attributes on changes in disability among low-functioning older persons. Journals of Gerontology: Psychological Sciences. 1999;54:P23–P29. doi: 10.1093/geronb/54b.1.p23. [DOI] [PubMed] [Google Scholar]
- Krause N. Age and decline in role-specific feelings of control. Journals of Gerontology: Social Sciences. 2007;62B:S28–S35. doi: 10.1093/geronb/62.1.s28. [DOI] [PubMed] [Google Scholar]
- Krause N, Shaw BA. Role-specific feelings of control and mortality. Psychology and Aging. 2000;15:617–626. doi: 10.1037//0882-7974.15.4.617. [DOI] [PubMed] [Google Scholar]
- Lachman ME. Perceived control over aging-related declines: Adaptive beliefs and behaviors. Current Directions in Psychological Science. 2006;15:282–286. [Google Scholar]
- Lachman ME, Firth KM. The adaptive value of feeling in control during midlife. In: Brim OG, Ryff CD, Kessler R, editors. How healthy are we? A national study of well-being at midlife. Chicago: University of Chicago Press; 2004. pp. 320–349. [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74:763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lang FR, Heckhausen J. Perceived control over development and subjective well-being: Differential benefits across adulthood. Journal of Personality and Social Psychology. 2001;81:509–523. doi: 10.1037//0022-3514.81.3.509. [DOI] [PubMed] [Google Scholar]
- Lindenberger U, Singer T, Baltes PB. Longitudinal selectivity in aging populations: Separating mortality-associated versus experimental components in the Berlin Aging Study (BASE) Journals of Gerontology Series B: Psychological Sciences. 2002;57B:P474–P482. doi: 10.1093/geronb/57.6.p474. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Lövdén M, Ghisletta P, Lindenberger U. Social participation attenuates decline in perceptual speed in old and very old age. Psychology and Aging. 2005;20:423–434. doi: 10.1037/0882-7974.20.3.423. [DOI] [PubMed] [Google Scholar]
- Magnusson D, Cairns RB. Developmental science: Toward a unified framework. In: Cairns RB, Elder GH, Costello EJ, editors. Developmental science. New York, NY: Cambridge University Press; 1996. pp. 7–30. [Google Scholar]
- McArdle JJ. A latent difference score approach to longitudinal dynamic structural analyses. In: Cudek R, du Toit S, Sorbom D, editors. Structural equation modeling: Present and future. Lincolnwood, IL: Scientific Software International; 2001. pp. 342–380. [Google Scholar]
- McArdle JJ, Fisher GG, Kadlec KM. Latent variable analyses of age trends of cognition in the Health and Retirement study, 1992-2004. Psychology and Aging. 2007;22:525–545. doi: 10.1037/0882-7974.22.3.525. [DOI] [PubMed] [Google Scholar]
- McArdle JJ, Hamagami F. Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In: Collins LM, Sayer AG, editors. New methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 137–176. [Google Scholar]
- McAvay GJ, Seeman TE, Rodin J. A longitudinal study of change in domain-specific self-efficacy among older adults. Journal of Gerontology: Psychological Sciences. 1996;51:P243–P253. doi: 10.1093/geronb/51b.5.p243. [DOI] [PubMed] [Google Scholar]
- Mendes de Leon CF, Seeman TE, Baker DI, Richardson ED, Tinetti ME. Self-efficacy, physical decline and change in functioning in community-living elders: A prospective study. Journal of Gerontology: Social Sciences. 1996;51B:S183–S190. doi: 10.1093/geronb/51b.4.s183. [DOI] [PubMed] [Google Scholar]
- Mirowsky J. Age and the sense of control. Social Psychology Quarterly. 1995;58:31–43. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 4th. Los Angeles, CA: Muthén & Muthén; 1998-2007. [Google Scholar]
- Parslow RA, Jorm AF, Christensen H, Mackinnon A. An instrument to measure engagement in life: Factor analysis and associations with sociodemographic, health and cognition measures. Gerontology. 2006;52:188–198. doi: 10.1159/000091829. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Penninx BW, Beekman JH, Aarjan TF, Ormel J, Kriegsman DMW, Boeke AJP, et al. Psychological status among elderly people with chronic diseases: Does type of disease play a part? Journal of Pschosomatic Research. 1996;40:521–534. doi: 10.1016/0022-3999(95)00620-6. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, van Tilburg T, Kriegsman DMW, deeg DJH, Boeke AJP, van Eijk JThM. Effects of social support and personal coping resources on mortality in older age: The Longitudinal Aging Study Amsterdam. American Journal of Epidemiology. 1997;146:510–519. doi: 10.1093/oxfordjournals.aje.a009305. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rodin J. Aging and health: Effects of the sense of control. Science. 1986;233:1271–1276. doi: 10.1126/science.3749877. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Age and the gender gap in the sense of personal control. Social Psychology Quarterly. 2002;65:125–145. [Google Scholar]
- Rowe JW, Kahn RL. Human aging: Usual and successful. Science. 1987;237:143–149. doi: 10.1126/science.3299702. [DOI] [PubMed] [Google Scholar]
- Seeman M, Lewis S. Powerlessness, health and mortality: A longitudinal study of older men and mature women. Social Science & Medicine. 1995;41:517–525. doi: 10.1016/0277-9536(94)00362-w. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Unger JB, McAvay G, Mendes de Leon CF. Self-efficacy beliefs and perceived declines in functional ability: MacArthur Studies of Successful Aging. Journals of Gerontology: Psychological Sciences. 1999;54B:P214–P222. doi: 10.1093/geronb/54b.4.p214. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Krause N. Exploring race variations in aging and personal control. Journal of Gerontology: Social Sciences. 2001;56B:S119–S124. doi: 10.1093/geronb/56.2.s119. [DOI] [PubMed] [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;23:323–355. [Google Scholar]
- Skaff MM. Sense of control and health: A dynamic duo in the aging process. In: Aldwin CM, Park CL, Spiro A, editors. Handbook of health psychology and aging. New York: Guilford Press; 2007. pp. 186–209. [Google Scholar]
- Steinhagen-Thiessen E, Borchelt M. Morbidity, medication, and functional limitations in very old age. In: Baltes PB, Mayer KU, editors. The Berlin Aging Study: Aging from 70 to 100. New York: Cambridge University Press; 1999. pp. 282–301. [Google Scholar]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Umberson D, Chen MD, House JS, Hopkins K, Slaten E. The effect of social relationships on psychological well-being: Are men and women really so different? American Sociological Review. 1996;61:837–857. [Google Scholar]
- Vaillant GE, Mukamal K. Successful aging. American Journal of Psychiatry. 2001;158:839–847. doi: 10.1176/appi.ajp.158.6.839. [DOI] [PubMed] [Google Scholar]