Abstract
We explore whether HIV stigma is associated with seeking to conceal testing interest. We examine 86,899 outpatient visits in a 1993–1997 national survey and compare HIV testing to four non-stigmatized tests: spirometry, allergy testing, mammography, and colonoscopy. We explore whether people testing for HIV, compared to people receiving control services, listed reasons for visit (RFV) less related to the test performed, listed their interest in testing more frequently as a non-primary RFV, and received more services unrelated to testing. A total of 48.7% of people tested for HIV listed a reason unrelated to testing as their primary RFV (spirometry: 8.9%; allergy testing: 29.3%), and 69.9% of people asking to test requested HIV testing as a secondary RFV (spirometry: 52%; allergy testing: 0%). People who tested for HIV received more services (M = 1.83 additional services) than non-testers (M = 0.95) on an index of seven services. We did not find this association for spirometry, allergy testing, colonoscopy, or mammography. We interpret these results to indicate that stigma may have behavioral correlates and that people may attempt to avoid HIV stigma by seeking a psychological cover for HIV testing. To our knowledge, this is the first study to attempt to use observational data on health service usage for assessing stigma and people’s attempts to deal with HIV testing stigma.
Keywords: HIV testing, stigma, health service usage, psychological cover, behavioral correlates of stigma
Introduction
Among the more than one million people who are living with HIV/AIDS in the USA, an estimated 25% are unaware that they are infected (Glynn & Rhodes, 2005; Kaiser Family Foundation, 2007). Despite campaigns to increase testing to raise awareness of HIV status, only 55% of US adults aged 18–64 report ever having tested for HIV (Kaiser Family Foundation, 2006).
Potential stigmatization is one of the most notable causes preventing individuals from testing and seeking care (Chesney & Smith, 1999; Fortenberry, McFarlane, Bleakley, & Bull, 2002; Garcia & Crocker, 2008; Myers, Orr, Locker, &Jackson, 1993; Phillips &Coates, 1995; Smith, Buzi, & Weinman, 2005; Young, Nussbaum, & Monin, 2007). People may be reluctant to test because the discovery of a positive HIV test result may lead to the loss of friendship, family ties, employment and housing, dismissal from school, and denial of health/ life insurance and health care (Folkman, Chesney, Cooke, Boccellari, & Collette, 1994). Apart from the consequences of a positive test result, the decision to test for HIV can lead to stigmatization (Young et al., 2007). The decision to avoid testing for HIV therefore allows people to prevent the stigmatization associated both with testing and a positive test result.
Individuals who wish to test for HIV may attempt “stigma management techniques” to avoid the potential stigmatization associated with testing (Goffman, 1963; Padilla et al., 2008). For example, people might mitigate the burden of stigma and increase willingness to test if they can seek a psychological cover to conceal their interest in HIV testing. A psychological cover allows people to engage in a behavior while concealing their desire to engage in that behavior (Holmes, Miller, & Lerner, 2002). In the case of HIV testing, people might be able to conceal their interest in testing for HIV by receiving other non-stigmatized services along with an HIV test. Evidence supports the possibility that people seek cover for HIV testing. For example, donating blood may provide a cover for HIV testing by allowing people to appear interested in performing the non-stigmatized service of blood donation (Chiavetta, Ennis, Gula, Baker, & Chambers, 2000; Korelitz, Busch, & Williams, 1996). People entering a clinic to test for HIV might employ similar strategies to avoid HIV stigma.
In this paper, we attempt to explore the behavioral correlates of HIV stigma by looking at health service usage in an outpatient population seeking HIV testing. We attempt to rule out alternative hypotheses to suggest the possibility that patients seek psychological cover for HIV testing by listing reasons for visits (RFV) that are unrelated to HIV testing, listing interest in HIV testing as a nonprimary RFV, and by receiving services unrelated to HIV testing.
Methods
Data
Data from the 1993–1997 National Hospital Ambulatory Medical Care Survey (NHAMCS) were combined to generate national estimates of health services usage. NHAMCS is a nationally representative probability sample of visits to hospital emergency and outpatient departments in non-federal hospitals conducted annually by the Centers for Disease Control and Prevention (CDC). Our analysis, focusing on HIV testing services, uses only the outpatient portion of the data from 1 January 1993 to 22 December 1997. This time period was chosen to allow analysis of behavioral correlates of HIV testing stigma during years of high stigma (Herek, 1999). Each observation is recorded based on a patient’s visit. Item non-response rates are typically under 0.05 each year. Imputations for missing outpatient data are performed for patient’s birth year, sex, and race. Details on the survey design and data are available online (CDC, 2008). We collected data on all individuals 18–65 years old at the time of the visit, including demographic characteristics, patients’ RFV, symptoms, physicians’ diagnoses, and services provided at the visit. Each patient provided up to three RFV the clinic, listed in order of self-reported reason. Health providers were instructed to record the RFV verbatim (CDC, 1995). Our analysis includes data on reported RFV and the diagnostic and therapeutic services performed.
Analysis
We aimed to determine the impact of HIV stigma on health service usage. The unit of analysis was the patient visit, and we examined HIV testing utilization patterns, making comparisons to control visits. We picked two non-stigmatized control services a priori (spirometry and allergy testing) from a list of nine frequently performed services. These were chosen as controls for HIV testing for three main reasons: their frequency in the sample was similar to HIV testing (less than 1% of sample visits); all were services where patients would be expected to receive additional tests and services; and the age distribution was similar. We used colonoscopy and mammography as two additional controls because HIV, colonoscopy, and mammography are screening tests where patients may receive the tests without symptom presentation. Colonoscopy and mammography were used as controls in the third analysis only because data on these services were unavailable to test the first two analyses. Data from 1993 to 1994 were available for these services.
We hypothesized that people attempt to evade HIV testing stigma by listing RFV that are unrelated to HIV testing, by expressing their interest in testing as a nonprimary RFV, or by receiving additional services that are unrelated to HIV testing. People who received control services should not adhere to the same predictions because there should be no stigma associated with requesting these services.
We looked at patients’ RFVs to test our first hypotheses that people receiving HIV tests may report reasons unrelated to HIV as their primary RFV. An infectious disease physician coded the RFVs according to their likelihood of signaling the need for an HIV test from extremely unlikely to trigger an HIV test (such as ankle sprain) to extremely likely to signal the need for an HIV test (such as genital discharge). The physician was blinded as to whether the patient received an HIV test. We analyzed the portion of HIV tests with RFVs that were unrelated to HIV compared to the total number of performed HIV tests. For the control services, the same physician coded the likelihood that people who received a spirometry or allergy test listed reasons related to these services. This preliminary analysis of descriptive statistics allowed us to determine the portion of people receiving HIV tests who listed reasons unrelated to HIV as their RFV. We predicted that people who received spirometry or allergy testing would be less likely than those testing for HIV to list a primary RFV that was unrelated to these services.
We also examined the hypothesis that people requesting an HIV test would be more likely to list testing as a secondary rather than primary RFV. We created two new variables, a patient’s primary and secondary RFV. To allow comparison between primary and secondary RFVs, we only included observations with all three RFV reported. We examined whether asking for an HIV test as a primary RFV (versus did not ask for the test) or secondary RFV (versus did not ask for the test) was associated with receiving an HIV test. We hypothesized that people who requested the non-stigmatized control services would be less likely to list these services as secondary rather than primary RFV.
Finally, we hypothesized people would try to avoid HIV stigma and conceal their interest in testing for HIV by requesting an HIV test as part of a large group of services that are unrelated to HIV. To assess this, we looked at the relationship between receiving an HIV test and receiving other services unrelated to HIV testing. We examined outcomes using services available for each year (excluding spirometry and allergy testing as they were used as controls). The list included seven services that were either possibly related or unlikely to be related to HIV testing (weight loss counseling, smoking cessation counseling, urinalysis, exercise counseling, blood pressure test, growth development counseling, and cholesterol counseling). We excluded services that were directly related to HIV testing such as HIV transmission counseling. Alogistic regression was used to test whether receiving an HIV test was associated with increased likelihood of receiving these services, controlling for age, race, and gender. We used Hochberg’s approach to correct for multiple testing comparisons (Hochberg, 1987; Hochberg & Benjamini, 2006). We also tested the hypothesis using an aggregate index of the seven services. For each patient visit, the index variable could have a value from zero to seven depending on the number of services that were performed. We hypothesized that people who tested for HIV would score higher on this index (receive more services) than people who did not test for HIV. To explore this hypothesis, we used linear regression analysis to determine whether HIV testing was associated with a higher value on this index, controlling for age, race, and gender. We predicted that compared to people who tested for HIV, those receiving a spirometry, allergy test, mammography, or colonoscopy should be less likely to receive additional services.
Results
The compiled sample from 1993 to 1997 included 86,899 visits. Table 1 shows baseline characteristics for the sample. Compared to visits for allergy and HIV tests, spirometry visits appeared to be from an older population. People whose RFV was an HIV test were on average 27.0 years old, similar to those visiting for allergy tests (M = 27.8) but younger than visits for spirometry (M = 38.1). Non-Whites were more likely to visit for an HIV test than spirometry or allergy test. Whites were more likely than non-Whites to visit for all three services.
Table 1.
Baseline characteristics (weighted) of patients who received an HIV test versus a spirometry or allergy test.
| HIV serology | Spirometry | Allergy test | |
|---|---|---|---|
| Age (mean, SE) | 27.0 (2.5) | 38.1 (.4.9) | 27.8 (5.8) |
| Gender | |||
| Male | 28.7% | 31.6% | 33.1% |
| Female | 71.3% | 68.4% | 66.9% |
| Race | |||
| White | 55.6% | 77.2% | 82.6% |
| Black | 41.4% | 21.6% | 8.6% |
| Asian | 2.6% | 0.7% | 6.3% |
| American Indian | 0.4% | 0.5% | 2.5% |
| Visiting hospital in urban area | |||
| Yes | 97.7% | 96.5% | 97.6% |
| No | 2.3% | 3.5% | 2.4% |
| Total number of patients tested in sample | 1131 | 171 | 58 |
| Most common primary reason for visit (% of cases) | Routine prenatal exam (36.9% of HIV visits) | Cough (12.1% of spirometry visits) | Allergies (9.3% of allergy testing visits) |
Figure 1 shows the weighted number of patients listing a reason unrelated to HIV testing as their RFV out of the total number of people receiving an HIV test. Whereas 48.7% (SE = 5.7%) of patients receiving an HIV test listed a RFV that was extremely unlikely to trigger an HIV test, 8.9% (SE = 2.9%) of patients receiving spirometries, and 29.3% (SE = 11.0) of patients receiving allergy tests listed RFVs that were extremely unlikely to trigger these services.
Figure 1. Total (weighted) number of allergy, spirometry, and HIV tests compared to tests performed on patients with reasons for visit that are unrelated to the test.
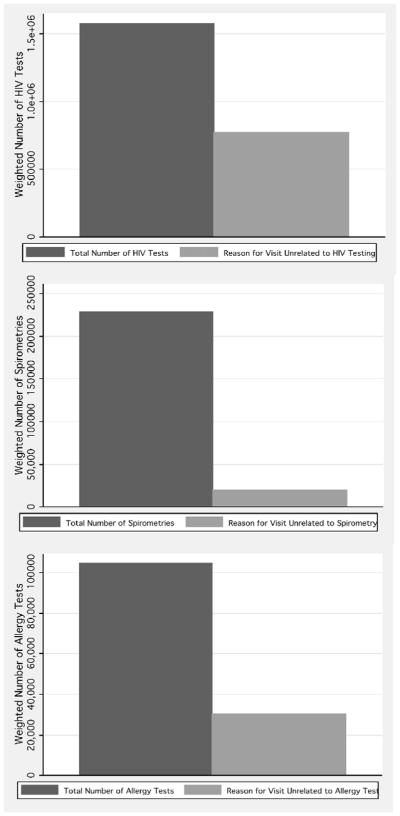
For 48.7% of performed HIV tests, patients listed reasons for visit that should be extremely unlikely to lead to an HIV test. Compared to HIV testing, a smaller portion of people receiving spirometries (8.9%) or allergy testing (29.3%) listed reasons for visit that are unrelated to these services.
Table 2 shows the number of HIV tests performed by requests for HIV testing as a primary or secondary RFV. There were 254 visits, where patients reporting three RFVs received an HIV test. Ninety-three percentage of these visitors (90% when applying the weights to generalize the sample to the general population) for HIV tests did not directly ask for the test. However, of the patients who asked for the test, 69.9% (SE = 17.0%) asked as a secondary RFV.
Table 2.
Requests for HIV/other related blood test, spirometry, and allergy test as a primary or second reason for visit.
| Asked for test as a primary reason for visit | Asked for test as a second or third reason for visit | Did not ask directly for test | Total tests with three reported reasons for visit | |
|---|---|---|---|---|
| HIV test | ||||
| Received HIV serology (unweighted) | 4 (1.6%) | 13 (5.1%) | 237 (93.3%) | 254 |
| Received HIV serology (weighted) | 2.8% | 6.5% | 90.7% | 100% |
| Spirometry | ||||
| Received spirometry (unweighted) | 21 (17.7%) | 21 (17.7%) | 77 (64.6%) | 119 |
| Received spirometry (weighted) | 20.9% | 22.4% | 56.7% | 100% |
| Allergy testing | ||||
| Received allergy test (unweighted) | 5 (7.9%) | 0 (0.0%) | 58 (92.1%) | 63 |
| Received allergy test (weighted) | 6.5% | 0.0% | 94.5% | 100% |
People were not significantly more likely to ask for non-stigmatized services as secondary rather than primary RFV; 52% (SE = 11.0%) of patients asking for a spirometry asked for the service as a secondary RFV; and all 57 patients asking for an allergy test asked for it as a primary RFV.
Table 3 shows the results of a logistic regression looking at the relationship between HIV testing and commonly performed services. Compared to visits where no HIV test was performed, receiving an HIV test predicted a greater likelihood of receiving five out of the seven services, controlling for age, race, and gender. HIV testers were more than six times more likely to receive smoking cessation counseling, more than three times more likely to receive a urinalysis, more than three times more likely to receive growth development counseling, almost 1.5 times more likely to receive a blood pressure test, and almost twice as likely to receive exercise counseling. These results were significant using Hochberg’s procedure (Hochberg, 1987; Hochberg & Benjamini, 2006) to control for multiple comparisons. No differences were found in weight reduction counseling or cholesterol education counseling. Receiving an HIV test was associated with an overall increase in service usage. While people not receiving HIV tests received on an average 0.95 of these seven services, those receiving an HIV test had on an average 1.83 additional services. This result was statistically significant, controlling for age, race, and gender, p <0.01.
Table 3.
Likelihood of receiving a diverse set of services, some of which are completely unrelated to HIV.
| Percentage (%) of HIV testers vs. non-HIV testers receiving service (weighted) | OR | SE | P | |
|---|---|---|---|---|
| Urinalysisa | ||||
| HIV | 51.4% vs. 14.2% | 4.84 | 0.79 | 0.00 |
| Exercise counselinga | ||||
| HIV | 13.0% vs. 6.4% | 2.24 | 0.49 | 0.00 |
| Cholesterol education | ||||
| HIV | 0.5% vs. 1.7% | 0.57 | 0.32 | 0.33 |
| Weight counseling | ||||
| HIV | 2.3% vs. 3.8% | 0.77 | 0.24 | 0.42 |
| Smoking cessation counselinga | ||||
| HIV | 13.4% vs. 2.4% | 6.03 | 2.3 | 0.00 |
| Growth development counselinga | ||||
| HIV | 6.9% vs. 1.8% | 2.72 | 0.57 | 0.02 |
| Blood pressurea | ||||
| HIV | 80.4% vs. 61.3% | 2.45 | 0.54 | 0.00 |
| Index of seven services | ||||
| Mean number of services for HIV testers (weighted) | 1.83 | |||
| Mean number of services for non-HIV testers (weighted) | 0.95 | |||
| HIV | 0.807 | 0.09 | 0.00 | |
Value is significant using Hochberg’s approach to correct for multiple comparisons.
Receiving the control services was not associated with receiving as many additional services (HIV testing: 93% increase in services, p <0.01; spirometry: 47% increase in services, p <0.01; allergy testing: 20% decrease in services, ns; colonoscopy: 5.3% decrease in services, ns; mammography: 14% increase in services, ns). We also entered both spirometry and allergy testing into the regression along with HIV testing. After correcting for multiple testing using Hochberg’s procedure (Hochberg, 1987; Hochberg & Benjamini, 2006) receiving a spirometry carried a stronger association than HIV testing of receiving a blood pressure test (spirometry Odds Ratio (OR)=6.54, p <0.01; HIV testing, OR=3.08, p <0.01; allergy testing, OR = 0.48, ns). Compared to spirometry and allergy testing, HIV had a greater association with receiving a urinalysis, growth development counseling, smoking cessation counseling, and exercise counseling. Receiving an HIV test was associated with receiving a greater number of services on the index of seven commonly performed services, controlling for age, race, and gender. To control for provider differences in prescribing services we looked across clinic types (general medicine, gynecology/obstetrics, surgery, substance abuse, and other type), and found that compared to patients not receiving an HIV test, those receiving an HIV test were significantly more likely to receive additional services in each clinic type, p <0.01.
Discussion
We present an analysis of survey data suggesting that people attempt to conceal their desire for HIV testing. Although people report that stigma has no effect on their HIV testing decision (Herek, Capitanio, & Widaman, 2003), one explanation of our data is that stigma affects testing decisions and behavior. Our analysis aims to suggest behavioral correlates of HIV stigma in terms of health service usage. Compared to people who received non-stigmatized services, people who tested for HIV were more likely to list RFV that were unrelated to HIV testing, more likely to list HIV testing as a secondary rather than primary RFV, and more likely to receive additional (possibly unrelated) health services. First, our results suggest that 49% of people who receive an HIV test enter a clinic listing reasons that are completely unrelated to HIV testing. Second, of those patients who can fight the potential stigmatization and ask directly for an HIV test, we found that 69.9% of these people ask for the test as a secondary rather than primary RFV. Finally, we found that, compared to visits where no HIV test is performed, patients receiving an HIV test have a higher likelihood of receiving possibly unrelated medical services, and on average receive more of these services. Taken together, one explanation of our data suggests that, compared to patients seeking non-stigmatized services, patients seeking an HIV test are more likely to seek cover to avoid potential stigmatization.
Although patients may be interested in testing for HIV, potential HIV stigmatization may decrease desire to request testing. Willingness to test for HIV may increase if people can report visiting the clinic for non-stigmatized reasons or by requesting other nonstigmatized services. For example in our data, we found that, compared to patients receiving controls services, those receiving an HIV test were more likely to receive additional, often unrelated, services. These additional services could possibly be a method of bundling stigmatized and non-stigmatized services to avoid the stigma associated with receiving a standalone HIV test. These additional services may sometimes be appropriate for patient’s health, but at other times might serve only to hide HIV stigma. Awareness of stigma and its effects might help to both increase willingness to request HIV testing, and to reduce unnecessary services performed to cover HIV stigma.
HIV researchers have requested innovative methods to measure HIV stigma. Stigma is typically measured through qualitative assessment and questionnaires where self-report and coding differences may cause inconsistent results (Nyblade, 2006; Swenderman, Rotheram-Borus, Comulada, Weiss, & Ramos, 2006). For example, although 56% of people in a randomized telephone survey reported that stigma does not affect their testing decision, researchers claim that additional measurements of HIV stigma will help to highlight how stigma reduces testing interest (Chesney & Smith, 1999; Fortenberry et al., 2002; Hereket al., 2003; Myers et al., 1993; Young et al., 2007).
The current study suggests that observational data can potentially be used as one method to assess how the stigma affects HIV testing decisions. To our knowledge, this is the first study to attempt to use observational data on health service usage for assessing stigma and people’s attempts to deal with HIV testing stigma.
This study has several limitations, mostly stemming from the observational study design. First, we cannot determine a causal link between stigma and increased health services usage. We attempted to rule out multiple alternative hypotheses, however, an experimental study is needed to test causation. Second, stigma and its effects may change over time, making our results based on 1993–1997 data unable to generalize to the current time period. We chose 1993–1997 a priori because it was a period of high HIV stigma (Herek& Capitanio, 1999) and allowed us to measure whether stigma may have behavioral correlates. Although the specific behavioral results might not generalize to the present day, our data suggest that HIV stigma may have behavioral correlates and we feel this is an important contribution. Third, it is possible that data in the NHAMCS dataset were not accurately coded: patients’ true RFVs may not have been recorded, RFVs might not have been recorded in the order the patient reported, or providers may have over or under-reported performing various services. However, the CDC has attempted to address this problem by training health providers on methods of reporting and stating that providers should report RFVs in patients’ own words. Fourth, the small sample and lack of formal statistical test in Hypothesis 2 may make that result less convincing. However, the small sample is the actual number of HIV tests performed based on a large sample of 86,899 patient visits. In addition, we think that the descriptive statistics presented display a convincing story for the stigma associated with HIV testing. That is, over 93% of HIV visitors never requested an HIV, and of the 7% of requests for the test, 69.9% asked as a secondary RFV. We did not find this same lack of willingness to request the control services. In fact, all patients asking for an allergy test asked for it as a primary RFV. Finally, other possible untested alternative hypotheses exist. For example, patients with unrelated RFVs might have been more likely to seek an HIV test because HIV receives substantial media attention, increasing the likelihood that patients might ask about their risk for HIV even if it was not their primary RFV. It is also possible that people seeking HIV tests received a greater number of overall tests because they are more responsive to aggressive public health awareness campaigns (such as exercise and smoking cessation counseling), or because providers recommended HIV testing to patients as part of a routine set of exams. Spirometry and allergy testing were used as controls because they were available in each year of the dataset. Colonoscopy and mammography were used as additional controls in the third hypothesis, although data on these services were limited to 1993–1994. Future work on this topic might explore alternative hypotheses using additional services.
In conclusion, findings suggest that people mask their desire to test for HIV because of the associated stigma, leading to suboptimal health service delivery. Total financial cost associated with this effect is still unknown but may lead to increased health care expenditures when patients receive unnecessary services. A sensitivity analysis can more accurately determine the most frequently provided requested and performed services, and the total bounded financial impact of these additional services. Although this paper has focused on the relationship between stigma and HIV testing, future research might explore outcomes for people seeking services for other stigmatized diseases, such as other sexually transmitted infections. Understanding the role that stigma plays in people’s testing and treatment decisions may improve interventions and reduce the social and economic consequences of stigma.
Acknowledgments
The authors wish to thank Jay Bhattacharya, Benn Eiffert, Kristin Cobb, Greg Szekeres, Sharif Sawires, and Thomas Coates for feed back on the studies.
References
- CDC. National hospital ambulatory medical care survey: 1995–1996 outpatient department patient record. 1995 Retrieved March 29, 2007, from http://www.cdc.gov/nchs/data/ahcd/odpr95-6.pdf. [PubMed]
- CDC. Ambulatory health care data. 2008 Retrieved September 25, 2008, from http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm.
- Chesney M, Smith AW. Critical delays in HIV testing and care: The potential role of stigma. American Behavioral Scientist. 1999;42(7):1162–1174. [Google Scholar]
- Chiavetta J, Ennis M, Gula CA, Baker AD, Chambers TL. Test-seeking as motivation in volunteer blood donors. Transfusion Medicine Reviews. 2000;14(3):205–215. doi: 10.1053/tm.2000.7353. [DOI] [PubMed] [Google Scholar]
- Folkman S, Chesney MA, Cooke M, Boccellari A, Collette L. Caregiver burden in HIV-positive and HIV-negative partners of men with AIDS. Journal of Consulting and Clinical Psychology. 1994;62(4):746–756. doi: 10.1037//0022-006x.62.4.746. [DOI] [PubMed] [Google Scholar]
- Fortenberry J, McFarlane M, Bleakley A, Bull S. Relationships of stigma and shame to gonorrhea and HIV screening. American Journal of Public Health. 2002;92(3):378–381. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia JA, Crocker J. Reasons for disclosing depression matter: The consequences of having egosystem and ecosystem goals. Social Science and Medicine. 2008;67:453–462. doi: 10.1016/j.socscimed.2008.03.016. [DOI] [PubMed] [Google Scholar]
- Glynn MK, Rhodes P. Estimated HIV prevalence in the United States at the end of 2003. Paper presented at the National HIV Prevention Conference; Atlanta, GA. 2005. Jun 12–15, Abstract No. T1-B1101. [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster; 1963. [Google Scholar]
- Herek GM. AIDS and stigma. American Behavioral Scientist. 1999;42(7):1106–1116. [Google Scholar]
- Herek GM, Capitanio JP. AIDS stigma and sexual prejudice. American Behavioral Scientist. 1999;42(7):1130–1147. [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. Stigma, social risk, and health policy: Public attitudes toward HIV surveillance policies and the social construction of illness. Health Psychology. 2003;22(5):533–540. doi: 10.1037/0278-6133.22.5.533. [DOI] [PubMed] [Google Scholar]
- Hochberg Y. Multiple comparison procedures. New York: John Wiley; 1987. [Google Scholar]
- Hochberg Y, Benjamini Y. More powerful procedures for multiple significance testing. Statistics in Medicine. 2006;9(7):811–818. doi: 10.1002/sim.4780090710. [DOI] [PubMed] [Google Scholar]
- Holmes JG, Miller DT, Lerner MJ. Committing altruism under the cloak of self-interest: The exchange fiction. Journal of Experimental Social Psychology. 2002;38(2):144–151. [Google Scholar]
- Kaiser Family Foundation. Survey of Americans on HIV/AIDS: Additional findings: HIV testing. 2006 Retrieved September 21, 2008, from http://www.kff.org/kaiserpolls/upload/7521.pdf.
- Kaiser Family Foundation. The HIV/AIDS epidemic in the United States. 2007 Retrieved September 21, 2008, from http://www.kff.org/hivaids/upload/3029-071.pdf.
- Korelitz JJ, Busch MP, Williams AE. Antigen testing for human immunodeficiency virus (HIV) and the magnet effect: Will the benefit of a new HIV test be offset by the numbers of higher-risk, test-seeking donors attracted to blood centers? Transfusion. 1996;36(3):203–208. doi: 10.1046/j.1537-2995.1996.36396182135.x. [DOI] [PubMed] [Google Scholar]
- Myers T, Orr K, Locker D, Jackson E. Factors affecting gay and bisexual men’s decisions and intentions to seek HIV testing. American Journal of Public Health. 1993;83:701–704. doi: 10.2105/ajph.83.5.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade L. Measuring HIV stigma: Existing knowledge and gaps. Psychology. Health & Medicine. 2006;11(3):335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- Padilla M, Castellanos D, Guilamo-Ramos V, Reyes AM, Marte LES, Soriano MA. Stigma, social inequality, and HIV risk disclosure among Dominican male sex workers. Social Science and Medicine. 2008;67:380–388. doi: 10.1016/j.socscimed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KA, Coates TJ. HIV counseling and testing: Research and policy issues. AIDS Care. 1995;7(2):115–124. doi: 10.1080/09540129550126623. [DOI] [PubMed] [Google Scholar]
- Smith PB, Buzi RS, Weinman ML. HIV testing and counseling among adolescents attending family planning clinics. AIDS Care. 2005;17(4):451–456. doi: 10.1080/09540120412331291788. [DOI] [PubMed] [Google Scholar]
- Swenderman D, Rotheram-Borus MJ, Comulada S, Weiss R, Ramos ME. Predictors of HIV related stigma among young people living with HIV. Health Psychology. 2006;25(4):501–509. doi: 10.1037/0278-6133.25.4.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S, Nussbaum D, Monin B. Potential moral stigma and reactions to sexually-transmitted diseases: Evidence for a disjunction fallacy. Personality and Social Psychology Bulletin. 2007;33(6):789–799. doi: 10.1177/0146167207301027. [DOI] [PubMed] [Google Scholar]


