Abstract
INTRODUCTION:
Rupture of the pectoralis major muscle appears to be increasing in athletes. However, the optimal treatment strategy has not yet been established.
OBJECTIVES:
To compare the isokinetic shoulder performance after surgical treatment to that after non-surgical treatment for pectoralis major muscle rupture.
METHODS:
We assessed 33 pectoralis major muscle ruptures (18 treated non-surgically and 15 treated surgically). Horizontal abduction and adduction as well as external and internal rotation at 60 and 120 degrees/s were tested in both upper limbs. Peak torque, total work, contralateral deficiency, and the peak torque agonist-to-antagonist ratio were measured.
RESULTS:
Contralateral muscular deficiency did not differ between the surgical and non-surgical treatment modalities. However, the surgical group presented twice the number of athletes with clinically acceptable contralateral deficiency (<20%) for internal rotators compared to the non-surgical group. The peak torque ratio between the external and internal rotator muscles revealed a similar deficit of the external rotation in both groups and on both sides (surgical, 61.60% and 57.80% and non-surgical, 62.06% and 54.06%, for the dominant and non-dominant sides, respectively). The peak torque ratio revealed that the horizontal adduction muscles on the injured side showed similar weakness in both groups (surgical, 86.27%; non-surgical, 98.61%).
CONCLUSIONS:
This study included the largest single series of athletes reported to date for this type of injury. A comparative analysis of muscular strength and balance showed no differences between the treatment modalities for pectoralis major muscle rupture. However, the number of significant clinical deficiencies was lower in the surgical group than in the non-surgical group, and both treatment modalities require greater attention to the rehabilitation process, especially for the recovery of muscle strength and balance.
Keywords: Isokinetic exercise, exercise, muscle imbalance, muscle rupture, orthopedics rehabilitation
INTRODUCTION
Rupture of the pectoralis major muscle is a rare injury with approximately 200 cases reported in the literature. It most commonly occurs among weight lifters and high-performance athletes, and to date, these injuries have been predominantly reported in men.1-3 The most common sport associated with this injury is weight lifting, particularly the “bench press” exercise.1 The prevalence of this injury appears to be increasing as the number of high-performance, recreational, and competitive athletes increases.4-7
Current treatment decisions are partly based on the classification of the injury. The classification of ruptures depends on the degree (complete vs. partial) and the location (enthesis, myotendinous junction, or intramuscular) of the injury.8,9 The rupture usually involves the distal part of the muscle region, particularly the myotendinous junction or insertion site, which usually requires surgical treatment.9 Most orthopedic surgeons choose non-surgical treatment for partial intramuscular tears.10-12 Surgical repair of complete tears at the enthesis and musculotendinous junction has been shown to provide superior cosmetic results and increased strength.1,4,7,9,10,13-16 However, previous studies that supported surgical repair did not employ consistent muscle assessment methodologies. Conservative treatment was evaluated in one case in which isokinetic strength testing11 produced favorable results, with a 40% increase in muscle force after treatment. The available series in previously published studies include a limited number of cases and employ inconsistent methods of pectoral major muscle strength evaluation.
Although it may be difficult in acute cases, muscle strength testing can be helpful in quantifying the pectoralis deficits and monitoring the progress of treatment. Some researchers have employed isokinetic strength testing in athletes who were diagnosed with pectoralis major ruptures and have concluded that isokinetic dynamometry is a useful, objective method of estimating loss of strength.5,17 This method of assessment can also compare the clinical aspects of non-surgical and surgical treatment.4,9,14,16,18
Hanna et al.14 described 21 athletes who underwent isokinetic assessment and showed that peak torque after surgical repair returned to 99% of that of the uninjured side, and total work performed returned to 97% of that of the uninjured side. For the non-surgically treated athletes, peak torque and total work performed returned to only 56% of that of the uninjured side.14 However, Komurcu et al.11 described a single case in which isokinetic testing was conducted before and after non-surgical treatment and found good results (contralateral deficiency reduced from 38% to 11%) from isokinetic assessment after treatment.11
Reported cases have included isokinetic dynamometer assessments in different positions, such as internal and external rotations in the scapular plane or 90 degrees of shoulder abduction. In these case studies, shoulder assessments were performed for different ranges of motions and in different planes,19,20 which prevents a solid comparative analysis of these shoulder evaluation studies. Knee assessments included extension and flexion movements that were consistently performed in the same position. Moreover, there are no published reports related to the agonist-to-antagonist ratio in cases of pectoralis major rupture; this is particularly important in pathological conditions. Although normalization should be a major focus of post-surgery rehabilitation, the ratio generally remains altered after surgery.19
Therefore, the purpose of the present study was to compare the isokinetic performance and the agonist-to-antagonist shoulder muscle ratio in a large single series of cases that involved surgical and non-surgical treatment of pectoralis major muscle ruptures.
MATERIALS AND METHODS
Subjects
Twenty-seven male athletes with pectoralis major muscle ruptures who were treated at the Department of Orthopedics and Traumatology of the Federal University of São Paulo were enrolled in this study. A total of 18 athletes from this group were initially treated non-surgically, and 6 of them were subsequently eligible for surgical treatment due to poor results. The mean age, height and weight of 27 athletes were 29.0 ± 4.8 years, 184.8 ± 6.6 cm and 92.7 ± 15.2 kg, respectively. All the athletes underwent magnetic resonance imaging to identify the specific location of the injury, and all of the athletes had experienced a partial or complete tear of the muscle, which was primarily located distal to the musculotendinous junction (4 lesions; 12%) or distal to the tendinous insertion (29 lesions; 88%). Because the vast majority of cases presented with the same lesion, both groups were similar in terms of the type of lesion. The most common cause of injury was bench pressing exercises (58%); the other 42% of the injuries occurred as a result of other sports activities (such as jiu-jitsu and water polo). To be eligible for the study, the athletes must have completed the rehabilitation procedures. The mean time between the injury and the isokinetic evaluation was 12 ± 10 months for non-surgical athletes, whereas the mean time between surgery and the isokinetic evaluation was 21±17 months for the surgical athletes. Despite this difference, there was no correlation between muscular deficiency and time after the injury.
Eighteen athletes were treated conservatively (the non-surgical group). For this reason, athletes underwent rehabilitation and stretching exercises as early as possible. Subsequently, resistance strengthening exercises were performed,12,21 which normalized the range of motion and resolved the pain.
Fifteen athletes were surgically treated (the surgical group) using the deltopectoral approach. Adhesions of the torn pectoralis muscle were freed from the surrounding soft tissues. Disinsertions were attached to the humerus using a screw and washer with non-absorbable sutures (Ethibond [Johnson & Johnson-Ethicon Inc., Somerville, New Jersey, USA] or Fiberwire [Arthrex, Naples, Florida, USA]). Bone scarification of the humeral cortex was created, into which the distal tendon border was reinserted. The sutured tendon was seated firmly back to its insertion site through the screw and washer.22
The Research Ethics Committee of the Federal University of São Paulo, São Paulo, Brazil approved this study, and all participants signed an informed consent form.
Procedures
Initially, all athletes provided the clinical history of the affected side, including the date and cause of injury, physical activity and level of satisfaction with the treatment.
After the clinical history was obtained, athletes underwent an isokinetic dynamometer evaluation (Cybex 6000, Cybex, Ronkonkoma, New York, USA) of both upper limbs, which was first performed on the non-injured side and was repeated on the injured side after a 3-minute rest. A pilot study was performed with two athletes to evaluate the loss of strength in all muscle groups on the injured side. These athletes underwent an isokinetic assessment for shoulder movements (adduction and abduction as well as internal and external rotation with the shoulder positioned in 90 degrees of abduction, flexion and extension movements). The pilot study showed greater contralateral strength deficits in internal rotation and horizontal adduction compared to the other shoulder movements.
Horizontal abduction and adduction as well as external and internal rotation in the scapular plane were tested. For horizontal abduction and adduction, athletes were placed in a supine position on an upper body testing table (UBXT, Cybex, Ronkonkoma, New York, USA) and were stabilized with bandages around the thorax and waist. Because of the position of the subjects during the evaluation, we performed gravity correction before testing, according to the manufacturer's specifications. For external and internal rotation, the athletes were placed in a standing position facing the machine and were stabilized with bandages around their upper limbs. The athletes performed a five-minute warm-up at 60W on an arm-cycle ergometer (Cybex), followed by specific stretching exercises for the shoulder. All muscle groups were tested concentrically at 60 and 120 degrees/s for both upper limbs. The sequence performed at each speed was comprised of three sub-maximum repetitions of the movement for athlete familiarization with the equipment, followed by five maximum repetitions at each speed, with a one-minute rest between sets.
Peak torque (in Nm) and total work (in J) are expressed as absolute values, whereas the contralateral deficiency and the strength ratio between external and internal rotation as well as horizontal abductors and adductors are expressed as percentages.
Statistical analysis
Qualitative variables are expressed as absolute and relative frequencies (%), and quantitative variables are expressed as mean ± standard deviation (SD). For each evaluated movement (external and internal rotation as well as horizontal abduction and adduction), an analysis of variance was used for comparisons between treatment type (surgical and non-surgical), side (injured and uninjured), and speed (60 and 120 degrees/s) to evaluate the significance of the differences in isokinetic values using the period of time between the lesion and the evaluation as the covariance.
In the analysis of the strength ratio between the external and internal rotators and between the horizontal abductors and adductors, Student's t-test was used for the comparison to normal values. Fisher's test was employed to analyze the association between the treatment and the frequency of athletes with muscular balance ratios and contralateral strength deficits that were greater than or less than standard values.
Statistical significance was established at p<0.05 for all tests.
RESULTS
Comparisons of the mean values of peak torque (Table 1) and total work (Table 2) registered by external and internal muscles as well as horizontal abductors and adductors from the surgical and non-surgical groups revealed no significant difference between the groups. In the assessment of shoulder movements, which did not require the action of the pectoralis major muscle (external rotation and horizontal abduction), a less-than-10% contralateral deficiency was found on average in both groups assessed. However, in the assessment of the internal rotation and horizontal adduction movements of the shoulder (movements that require action of the pectoralis major muscle), despite the non-significant difference between the groups, the deficiency found was between 10 and 20% (Table 3).
Table 1.
Peak torque for the internal and external rotator muscles and the horizontal abductor and adductor muscles of the shoulder at angular speeds of 60 and 120 degrees/s in athletes who had undergone surgical and non-surgical treatments.
| Muscles | Injured side | Uninjured side | ||
| 60 degrees/s | 120 degrees/s | 60 degrees/s | 120 degrees/s | |
| External rotators (Nm) | ||||
| Surgical (n = 15) | 31.7 ± 8.6 | 29.7 ± 8.5 | 34.3 ± 9.5 | 32.7 ± 8.2 |
| Non-surgical (n = 18) | 33.7 ± 9.5 | 30.6 ± 8.1 | 34.5 ± 5.2 | 34.6 ± 6.6 |
| Internal rotators (Nm) | ||||
| Surgical (n = 15) | 52.5 ± 14.5 | 49.7 ± 14.6 | 59.5 ± 12.4 | 57.0 ± 13.8 |
| Non-surgical (n = 18) | 56.8 ± 19.0 | 54.9 ± 21.6 | 65.3 ± 15.8 | 64.6 ± 17.1 |
| Abductors (Nm) | ||||
| Surgical (n = 15) | 75.9 ± 21.0 | 71.4 ± 22.5 | 82.4 ± 21.2 | 77.0 ± 24.3 |
| Non-surgical (n = 18) | 82.7 ± 24.0 | 84.1 ± 27.0 | 89.2 ± 21.1 | 88.6 ± 27.0 |
| Adductors (Nm) | ||||
| Surgical (n = 15) | 89. 7 ± 24.2 | 86.9 ± 21.6 | 111.5 ± 30.6 | 104.1 ± 27.2 |
| Non-surgical (n = 18) | 92.2 ± 30.7 | 95.3 ± 31.5 | 116.7 ± 23.8 | 114.7 ± 25.0 |
Data are presented as mean ± standard deviation.
There were no significant differences between the groups (surgical or non-surgical) and the angular velocities (60 and 120 degrees/s); p>0.05.
Table 2.
Total work for the internal and external rotator muscles and the horizontal abductor and adductor muscles of the shoulder at angular speeds of 60 and 120 degrees/s in athletes who had undergone surgical and non-surgical treatments.
| Muscles | Injured side | Uninjured side | ||
| 60 degrees/s | 120 degrees/s | 60 degrees/s | 120 degrees/s | |
| External rotators (J) | ||||
| Surgical (n = 15) | 42.2 ± 14,0 | 37.1 ± 14.6 | 45.5 ± 11.7 | 40.1 ± 12.8 |
| Non-surgical (n = 18) | 43.2 ± 10.9 | 37.2 ± 10.7 | 43.9 ± 7.6 | 40.2 ± 9.2 |
| Internal rotators (J) | ||||
| Surgical (n = 15) | 72.3 ± 21.8 | 67.0 ± 21,0 | 84.6 ± 20.6 | 79.2 ± 22.0 |
| Non-surgical (n = 18) | 75.7 ± 19.7 | 70.1 ± 22.7 | 86.6 ± 15.2 | 85.8 ± 19.3 |
| Abductors (J) | ||||
| Surgical (n = 15) | 74.9 ± 28.5 | 65.7 ± 31.0 | 84.5 ± 29.2 | 72.1 ± 32.8 |
| Non-surgical (n = 18) | 82.3 ± 24.8 | 74.0 ± 26.7 | 93.4 ± 27.3 | 82.0 ± 28.8 |
| Adductors (J) | ||||
| Surgical (n = 15) | 92.3 ± 28,0 | 80.3 ± 26.1 | 122.5 ± 39.6 | 104.8 ± 33.4 |
| Non-surgical (n = 18) | 93.4 ± 37.3 | 90.6 ± 37.6 | 130.3 ± 28.8 | 120.1 ± 32.7 |
Data are presented as mean ± standard deviation.
There were no significant differences between the groups (surgical or non-surgical) and the angular velocities (60 and 120 degrees/s); P>0.05.
Table 3.
Contralateral deficiency between the injured and uninjured sides in athletes who had undergone surgical and non-surgical treatments.
| 60 degrees/s | 120 degrees/s | |
| External rotators (%) | ||
| Surgical (n = 15) | -7.1 ± 20.3 | -7.5 ± 24.6 |
| Non-surgical (n = 18) | -2.3 ± 22.1 | -9.6 ± 26.7 |
| Internal rotators (%) | ||
| Surgical (n = 15) | -11.4 ± 17.6 | -12.3 ± 16.6 |
| Non-surgical (n = 18) | -14.0 ± 15.3 | -16.3 ± 18.9 |
| Abductors (%) | ||
| Surgical (n = 15) | -7.6 ± 10.8 | -5.3 ± 17.8 |
| Non-surgical (n = 18) | -7.6 ± 10.2 | -5.1 ± 9.7 |
| Adductors (%) | ||
| Surgical (n = 15) | -17.7 ± 17.3 | -14.1 ± 17.8 |
| Non-surgical (n = 18) | -20.8 ± 23,0 | -17.5 ± 20.6 |
Data are presented as mean ± standard deviation.
Negative values indicate a deficiency on the injured side.
There were no significant differences between the groups; P>0.05.
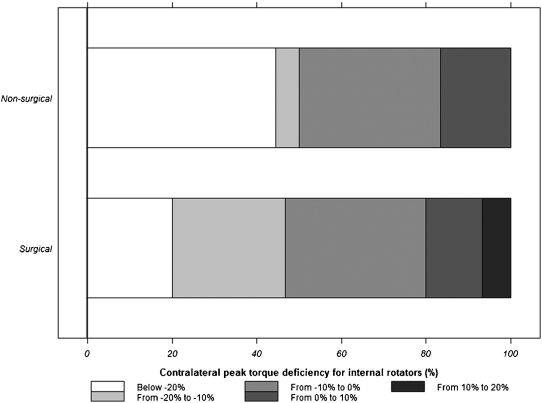
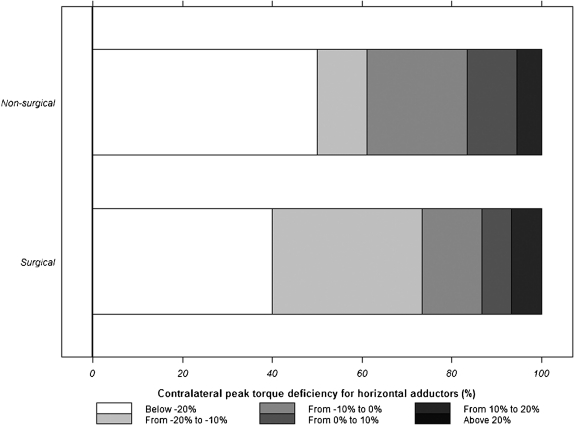
The number of athletes in the non-surgical group who presented with a greater-than-20% peak torque contralateral deficiency of the internal rotators of the shoulder was twice (8 athletes [44.4%]) the number of athletes who presented with the same deficit in the surgical group (3 athletes [20%]) (Figure 1). A greater-than-20% peak torque contralateral deficiency of the horizontal adductors was found in 9 (50%) of the athletes in the non-surgical group and 6 (40%) of the athletes in the surgical group (Figure 2).
Figure 1.
Range of athletes with contralateral deficiency of the internal rotator muscles (negative deficiency values indicate a deficiency on the injured side).
Figure 2.
Range of athletes with contralateral deficiency of the horizontal adductor muscles (negative deficiency values indicate a deficiency on the injured side).
Values of contralateral deficiency between 0 and 20% were found for the internal rotation movement in 9 (60%) of the athletes in the surgical group, and 7 (38.9%) of the athletes in the non-surgical group (Figure 1). In the horizontal adduction movement, this same range of contralateral deficiency was observed in 7 (46.6%) of the athletes in the surgical group and 6 (33.3%) of the athletes in the non-surgical group (Figure 2).
The contralateral deficiency found in our study had no significant correlation with age, mechanism, type or time of injury, type or time of treatment, or physical activity.
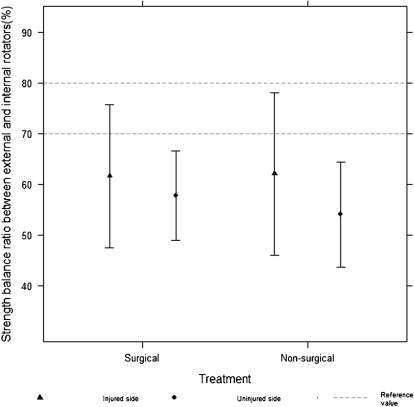
Figure 3 shows that 13 (86.7%) athletes who underwent surgical procedures and 13 (72.2%) who underwent non-surgical treatment presented with a muscular balance ratio between the concentric action of the external and internal rotator muscles of the shoulder that was less than the lower threshold of normality described in the literature (70 to 80%),23 which suggests weakness of the external rotator muscles. However, only one athlete (6.7%) in the surgical group and two (11.1%) in the non-surgical group presented with a balance ratio that was greater than the upper threshold of normality; these findings suggest a weakness of the internal rotator muscles. In terms of the ratio between the horizontal abduction and adduction movements of the shoulder in concentric action, seven (46.4%) athletes from the surgical group and eight (44.4%) athletes from the non-surgical group presented with values that were greater than the upper threshold of normality (73 to 81%, according to the literature), which suggests weakness of the horizontal adductor muscles.24 Five (33.3%) athletes from the surgical group and 5 (27.8%) athletes from the non-surgical group presented with values that were less than the reference value (Figure 4), which suggests weakness of the horizontal abductor muscles.
Figure 3.
Balance ratio between the external and internal rotator muscles of the shoulder for concentric action in athletes who underwent surgical and non-surgical treatment.
Figure 4.
Balance ratio between the horizontal abductor and adductor muscles of the shoulder for concentric action in athletes who underwent surgical and non-surgical treatment.
DISCUSSION
Rupture of the pectoralis major muscle is rare and occurs most commonly in young athletes.12 In our study, 58% of the athletes suffered this injury during bench press exercises, and 55% of the assessed athletes were weightlifters. Similarly, Aarimaa et al.10 and Bak et al.1 confirmed the prevalence of the lesion in athletes who performed strength training or weight lifting. This type of exercise is more often performed by men; therefore, there is a predominance of males in all of the cases described in the literature.
Only four of the lesions in this study occurred near the tendinous muscle junction (12%); of these, one was treated surgically. The remaining cases (88%) occurred through muscular disinsertion. There were no cases of osseous avulsion, which is considered to be the most serious complication of this injury.5 Some authors have found a relationship between athletic activity and the locations of the lesions; the tendinous muscle junction is the most frequent location.1,8,25 Kretzler et al.4 suggested that lesions close to the humeral insertion in the tendinous muscle junction are related to excessive tension associated with heavy weights and are typical of supine movement.
In our study, no correlation was observed between the level of contralateral strength deficiency and the elapsed time between the lesion and the treatment, which enabled us to compare both groups despite the different amounts of elapsed time between the lesion and the evaluation (a mean of 12 months in the surgical group and 21 months in the non-surgical group). Other aspects, such as age, type and mechanism of the injury, and level of physical activity, were also not statistically correlated with the magnitude of the contralateral deficiency of peak torque or total work, which supports the findings of Hanna et al.,14 Schepsis et al.,18 and Quilan et al.16 Aarimaa et al.10 also found that the best treatment outcome was correlated with the use of anabolic steroids, whereas the influence of factors such as time, treatment and age was small. In our study, approximately 60% of the athletes used anabolic steroids (60% of the surgical group and 61% of the non-surgical group).
No significant difference was seen between the isokinetic variables of the surgical and non-surgical groups, highlighting the efficacy of both treatments. Hanna et al.14 assessed the isokinetic muscular strength of 22 individuals with lesions of the pectoralis major muscle, 10 of whom were treated surgically and 12 of whom were treated non-surgically. In contrast to our results, the isokinetic variables of the injured side in the different groups showed that the recovery of strength occurred in 99% of the athletes from surgical group vs. 56% of the athletes from non-surgical group. Schepsis et al.18 also assessed the recovery of muscular strength after surgical and non-surgical treatment.18 They divided the athletes who underwent surgery into two subgroups: acute, for those who underwent surgery within a month after the lesion, and chronic, for those who underwent surgery longer than one month after the lesion. Their results showed that 74% recovery of peak torque occurred in the chronic group, 110% recovery occurred in the acute group, and 63% recovery occurred in the athletes who were non-surgically treated. Our study revealed similar findings on the analysis of some of our surgical group results. We divided the surgical athletes into two groups, as did Schepsis et al.18, but found no significant difference. It is possible that the positioning for the isokinetic assessment of the movements of the shoulder in our study differs from that used in other studies, and this may explain the different results.19 We assessed the strength of the pectoralis major muscle in movements of horizontal adduction and internal rotation in the scapular plane. Similarly, Schepsis et al.18 assessed the horizontal adduction movement, but did not perform the internal rotation movement, whereas Hanna et al.14 utilized the diagonal movement for the assessment of muscular strength on the isokinetic dynamometer. The diagonal movement pattern involves other muscle groups, and this may also explain the differences in the results. The non-surgical treatment of these lesions is scarcely described in the literature, and thus we cannot rule out the possibility that differences in the rehabilitation procedures might have also contributed to the differences between our results and those of other authors; in addition, differences in the surgical techniques may also be a factor.
Although there was no significant difference related to the contralateral deficiency between the surgical and non-surgical groups, according to clinical criteria, the surgical treatment seems to have produced better results compared to non-surgical treatment. Bak et al. (2000) considered a less-than-10% contralateral deficiency to be excellent, up to 20% as good and greater than 20% as bad or poor.1 Therefore, in clinical terms, we found that almost twice as many individuals from the non-surgical group (8 athletes or 44%) presented with greater-than-20% deficiencies for internal rotator peak torque, compared to the surgical group (3 athletes or 20%). This pattern was also observed in the analysis of the strength of the horizontal adductors of the shoulder. We found a higher number of athletes who had undergone surgical procedures to be within the clinically acceptable values of deficiency (<20%). Moreover, 60% (9 athletes) of athletes who were tested for internal rotators and 46.6% (7 athletes) tested for horizontal adductors showed acceptable results in the surgical group. Within the non-surgical group, acceptable values were identified in only 38.9% (7 athletes) of the athletes who were tested for internal rotation movement and in 33.3% (6 athletes) who were tested for horizontal adduction movement. Several authors have suggested that surgical intervention is the best treatment for lesions of the pectoralis major muscle.10,12,13 To confirm this, those authors considered muscular strength, which was measured manually or using isokinetic resistance, in addition to cosmetic aspects and overall satisfaction of the individual. However, further studies that involve larger athlete numbers and specific isokinetic testing movement patterns are required.
Because the shoulder is very unstable and the muscles play an essential role in the maintenance of stability, we studied not only the contralateral deficiency of muscular strength after pectoralis major muscle lesions but also the peak torque ratio between the antagonist muscles of the joint (the relationship between the horizontal abductors and adductors and the external and internal rotators). According to Codine et al. (2005), this ratio may remain affected after surgical treatment or may be the cause of the lesion.19 Ellenbecker (1989) suggested that extreme differences in muscular strength between the antagonist muscles of the shoulder are associated with the incidence of lesions of this joint, whereas rehabilitation should normalize this condition.20
Shklar and Dvir (1995) found that the values of normality for the ratio of muscular strengths acting on the movements of the shoulder corresponded to between 70 and 80% for the peak torque ratio between the external and internal rotators in concentric action.23 Several studies on different sports, such as swimming,26 baseball,27-30 and water polo,31 have presented values of normality for the ratios of muscular balance in the movements of internal and external rotation of the shoulder. Bak and Magnusson (1997) found that the internal rotators were stronger than the external rotators for swimming athletes.26 McMaster et al. (1991) found a 60% muscular balance ratio between the external and internal rotator muscles of the shoulder in concentric action in water polo athletes.31 Warner et al. (1990) found a 70% balance ratio in baseball athletes.29 Comparisons between the findings presented by Shklar and Dvir that involved non-athletic individuals23 with other studies cited above allowed us to conclude that the muscular balance ratio must be retained regardless of the sport. Therefore, the reference values found in these studies can be compared to our results. However, to our knowledge, there are no data in the literature on the balance ratio between rotator muscles of the shoulder after injuries to the pectoralis major muscle.
The muscular balance ratio between the external and internal rotators in concentric action assessed in this study (62% on the injured side and 55% on the uninjured side) was, on average, less than the values of normality,23 regardless of the side (injured or uninjured) or the treatment. This less-than-normal ratio indicates that the external rotator muscles of the shoulder present only 62% and 55% of the strength of the internal rotators of the injured and uninjured sides, respectively. The bilateral muscle weakness of the external rotator suggests that there is a significant imbalance of the muscular actions that involve the shoulders of these athletes. This imbalance, which favors the action of the internal rotator muscles of the shoulder, could be related to high volumes and intensity of training,10,32 which would explain why we did not find values within the normal range on the uninjured side.
It is possible that this imbalance is related to the causes of the lesions of the pectoralis major muscle. Moreover, we propose that the uninjured limb is exposed to a greater risk of injury because the balance ratio is also altered on that side.
Based on the muscular balance ratio between the horizontal abductor and adductor muscles of the shoulder in concentric action, the normality ratio found in the literature is between 73% and 81%.24 The ratio found in the present study was greater that the normality range only on the injured side, regardless of the procedure adopted (86.3% in the surgical group and 98.6% in the non-surgical group). The above-normal values of the muscular balance ratio between the antagonist groups indicate that the horizontal adductors of the shoulder were only 13.7% and 1.4% stronger than the horizontal abductor muscles in the surgical and non-surgical groups, respectively. This implies that, even after a certain period of time following treatment (surgical or otherwise), no significant increases in strength that enables the rebalance of the strength in the injured shoulder is observed in the pectoralis major muscle.
The analysis of muscle strength balance in the shoulder recovering from lesions of pectoralis major muscle showed that this muscle is stronger than its antagonists, but this is not sufficient to maintain the stability of the rotator cuffs.
CONCLUSION
Surgical treatment of injury to the pectoralis major muscle was associated with a lower incidence of significant strength deficits, although no difference was found in the magnitude of contralateral strength deficiency between the surgical and non-surgical treatments. Regardless of the type of treatment used, the subjects showed clinically significant strength imbalance of the shoulder muscles. Thus, shoulder muscle ratios warrant greater attention in preventive and rehabilitation programs. The findings of the present study also suggests that further studies that include additional clinical parameters should be conducted to determine the best treatment for pectoralis major muscle ruptures.
ACKNOWLEDGEMENTS
The authors thank all of the subjects who volunteered their time to participate in this study.
REFERENCES
- 1.Bak K, Cameron EA, Henderson IJ. Rupture of the pectoralis major: a meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc. 2000;8:113–9. doi: 10.1007/s001670050197. 10.1007/s001670050197 [DOI] [PubMed] [Google Scholar]
- 2.McEntire JE, Hess WE, Coleman SS. Rupture of the pectoralis major muscle. A report of eleven injuries and review of fifty-six. J Bone Joint Surg Am. 1972;54:1040–6. [PubMed] [Google Scholar]
- 3.Park JY, Espiniella JL. Rupture of pectoralis major muscle. A case report and review of literature, J Bone Joint Surg Am. 1970;52:577–81. [PubMed] [Google Scholar]
- 4.Kretzler HH, Jr, Richardson AB. Rupture of the pectoralis major muscle. Am J Sports Med. 1989;17:453–8. doi: 10.1177/036354658901700401. 10.1177/036354658901700401 [DOI] [PubMed] [Google Scholar]
- 5.Liu J, Wu JJ, Chang CY, Chou YH, Lo WH. Avulsion of the pectoralis major tendon. Am J Sports Med. 1992;20:366–8. doi: 10.1177/036354659202000324. 10.1177/036354659202000324 [DOI] [PubMed] [Google Scholar]
- 6.Roi GS, Respizzi S, Dworzak F. Partial rupture of the pectoralis major muscle in athletes. Int J Sports Med. 1990;11:85–7. doi: 10.1055/s-2007-1024768. 10.1055/s-2007-1024768 [DOI] [PubMed] [Google Scholar]
- 7.Zeman SC, Rosenfeld RT, Lipscomb PR. Tears of the pectoralis major muscle. Am J Sports Med. 1979;7:343–7. doi: 10.1177/036354657900700607. 10.1177/036354657900700607 [DOI] [PubMed] [Google Scholar]
- 8.Tietjen R. Closed injuries of the pectoralis major muscle. J Trauma. 1980;20:262–4. doi: 10.1097/00005373-198003000-00015. 10.1097/00005373-198003000-00015 [DOI] [PubMed] [Google Scholar]
- 9.Wolfe SW, Wickiewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle. An anatomic and clinical analysis. Am J Sports Med. 1992;20:587–93. doi: 10.1177/036354659202000517. 10.1177/036354659202000517 [DOI] [PubMed] [Google Scholar]
- 10.Aärimaa V, Rantanen J, Heikkilä J, Helttula I, Orava S. Rupture of the pectoralis major muscle. Am J Sports Med. 2004;32:1256–62. doi: 10.1177/0363546503261137. 10.1177/0363546503261137 [DOI] [PubMed] [Google Scholar]
- 11.Komurcu M, Yildiz Y, Ozdemir MT, Erler K. Rupture of the pectoralis major muscle in a paratrooper. Aviat Space Environ Med. 2004;75:81–4. [PubMed] [Google Scholar]
- 12.Petilon J, Carr DR, Sekiya JK, Unger DV. Pectoralis major muscle injuries: evaluation and management. J Am Acad Orthop Surg. 2005;13:59–68. doi: 10.5435/00124635-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Anbari A, Kelly JD, Moyer RA. Delayed repair of a ruptured pectoralis major muscle. A case report. Am J Sports Med. 2000;28:254–6. doi: 10.1177/03635465000280021901. [DOI] [PubMed] [Google Scholar]
- 14.Hanna CM, Glenny AB, Stanley SN, Caughey MA. Pectoralis major tears: comparison of surgical and conservative treatment. Br J Sports Med. 2001;35:202–6. doi: 10.1136/bjsm.35.3.202. 10.1136/bjsm.35.3.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kakwani RG, Matthews JJ, Kumar KM, Pimpalnerkar A, Mohtadi N. Rupture of the pectoralis major muscle, Surgical treatment in athletes. Int Orthop. 2007;31:159–63. doi: 10.1007/s00264-006-0171-2. 10.1007/s00264-006-0171-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quinlan JF, Molloy M, Hurson BJ. Pectoralis major tendon ruptures: when to operate. Br J Sports Med. 2002;36:226–8. doi: 10.1136/bjsm.36.3.226. 10.1136/bjsm.36.3.226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scott BW, Wallace WA, Barton MA. Diagnosis and assessment of pectoralis major rupture by dynamometry. J Bone Joint Surg Br. 1992;74:111–3. doi: 10.1302/0301-620X.74B1.1732236. [DOI] [PubMed] [Google Scholar]
- 18.Schepsis AA, Graf MW, Jones HP, Lemos MJ. Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med. 2000;28:9–15. doi: 10.1177/03635465000280012701. [DOI] [PubMed] [Google Scholar]
- 19.Codine P, Bernard PL, Pocholle M, Herisson C. Isokinetic strength measurement and training of the shoulder: methodology and results. Ann Readapt Med Phys. 2005;48:80–92. doi: 10.1016/j.annrmp.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Ellenbecker TS, Derscheid GL. Rehabilitation of overuse injuries of the shoulder. Clin Sports Med. 1989;8:583–604. [PubMed] [Google Scholar]
- 21.Dodds SD, Wolfe SW. Injuries to the pectoralis major. Sports Med. 2002;32:945–52. doi: 10.2165/00007256-200232140-00004. 10.2165/00007256-200232140-00004 [DOI] [PubMed] [Google Scholar]
- 22.Pochini AC, Ejnisman B, Andreoli CV, Monteiro GC, Fleury AM, Faloppa F, et al. Exact moment of tendon of pectoralis major muscle rupture captured on video. Br J Sports Med. 2007;41:618–19. doi: 10.1136/bjsm.2006.033563. 10.1136/bjsm.2006.033563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shklar A, Dvir Z. Isokinetic strength relationships in shoulder muscles, Clin Biomech (Bristol, Avon) 10 (1995):369–373. doi: 10.1016/0268-0033(95)00007-8. [DOI] [PubMed] [Google Scholar]
- 24.Silva RT, Gracitelli GC, Saccol MF, Laurino CF, Silva AC, Braga-Silva JL. Shoulder strength profile in elite junior tennis players: horizontal adduction and abduction isokinetic evaluation. Br J Sports Med. 2006;40:513–7. doi: 10.1136/bjsm.2005.023408. 10.1136/bjsm.2005.023408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zvijac JE, Schurhoff MR, Hechtman KS, Uribe JW. Pectoralis major tears: correlation of magnetic resonance imaging and treatment strategies. Am J Sports Med. 2006;34:289–94. doi: 10.1177/0363546505279573. 10.1177/0363546505279573 [DOI] [PubMed] [Google Scholar]
- 26.Bak K, Magnusson SP. Shoulder strength and range of motion in symptomatic and pain-free elite swimmers. Am J Sports Med. 1997;25:454–9. doi: 10.1177/036354659702500407. 10.1177/036354659702500407 [DOI] [PubMed] [Google Scholar]
- 27.Brown LP, Niehues SL, Harrah A, Yavorsky P, Hirshman HP. Upper extremity range of motion and isokinetic strength of the internal and external shoulder rotators in major league baseball players. Am J Sports Med. 1988;16:577–85. doi: 10.1177/036354658801600604. 10.1177/036354658801600604 [DOI] [PubMed] [Google Scholar]
- 28.Mikesky AE, Edwards JE, Wigglesworth JK, Kunkel S. Eccentric and concentric strength of the shoulder and arm musculature in collegiate baseball pitchers. Am J Sports Med. 1995;23:638–42. doi: 10.1177/036354659502300520. 10.1177/036354659502300520 [DOI] [PubMed] [Google Scholar]
- 29.Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Patterns of flexibility, laxity, and strength in normal shoulders and shoulders with instability and impingement. Am J Sports Med. 1990;18:366–75. doi: 10.1177/036354659001800406. 10.1177/036354659001800406 [DOI] [PubMed] [Google Scholar]
- 30.Wilk KE, Andrews JR, Arrigo CA. The physical examination of the glenohumeral joint: emphasis on the stabilizing structures. J Orthop Sports Phys Ther. 1997;25:380–9. doi: 10.2519/jospt.1997.25.6.380. [DOI] [PubMed] [Google Scholar]
- 31.McMaster WC, Long SC, Caiozzo VJ. Isokinetic torque imbalances in the rotator cuff of the elite water polo player. Am J Sports Med. 1991;19:72–5. doi: 10.1177/036354659101900112. 10.1177/036354659101900112 [DOI] [PubMed] [Google Scholar]
- 32.Almekinders LC. Anti-inflammatory treatment of muscular injuries in sport. An update of recent studies Sports Med. 1999;28:383–8. doi: 10.2165/00007256-199928060-00001. [DOI] [PubMed] [Google Scholar]