Abstract
Tuberculosis remains a significant global health problem: one-third of the human population is infected with Mycobacterium tuberculosis (MTB) and 10% of those are at lifetime risk of developing tuberculosis. Although an important role of genetic variation of host in outcomes of tuberculosis infection is well documented, genetic determinants of susceptibility in immunocompetent individuals remain largely unknown due to complex multigenic control and significant impact of genes - environment interactions. Natural genetic variation of host resistance to MTB in immunocompetent inbred mice reflects heterogeneity among humans and allows stepwise dissection of the genetic control using a mouse model. Previously we characterized a mouse super-susceptibility locus (sst1) and mapped additional quantitative trait loci (QTLs) controlling anti-tuberculosis immunity, among which a QTL on chromosome 7 was most prominent. In this study we addressed a specific role of the chromosome 7 QTL and found that the chromosome 7 and sst1 loci independently control distinct mechanisms of host resistance to MTB, but the phenotypic expression of the chromosome 7 locus is significantly influenced by interactions with the sst1. While the sst1 locus is especially important in the lungs and the effect of the chromosome 7 locus is systemic, both loci affect macrophage-mediated control of virulent MTB in vivo. Their combined effect accounts for half of the dramatic difference in survival between the susceptible and resistant parental strains. Further genetic and functional dissection of the chromosome 7 locus to identify causal genetic variation will help untangle the genetic basis of tuberculosis susceptibility in immunocompetent hosts.
Keywords: Mycobacterium tuberculosis (MTB), sst1, Ipr1, chromosome 7, mouse infection model
Introduction
Tuberculosis (TB) remains a significant global health threat; approximately one third of the World's population is estimated to be infected with virulent Mycobacterium tuberculosis with almost 8 million new cases and nearly 2 million deaths annually (1). It is established that there is genetic heterogeneity in host population resistance to mycobacterial infection, this ranges from extreme susceptibility to avirulent mycobacteria to efficient control of fully virulent MTB. This heterogeneity is true of human populations, in which less than 10% of immunocompetent individuals develop clinical disease after infection with fully virulent MTB (21). Host genetic variation is also true of experimental mouse, guinea pig and rabbit models of infection (21), and without considering the contribution of host genetics the development of more efficient drug and vaccine interventions will be challenging.
In most immunocompetent patients, TB is controlled systemically, but the lung is destroyed leading to propagation and transmission to new hosts via the aerosol route (21). Host genetic variants that predispose immunocompetent hosts to TB by weakening their defenses enough to permit lung destruction and pathogen transmission remain to be elucidated. TB pathogenesis, a highly complex sequence of events, is multistage with many cell types participating during chronic infection. One would expect a hierarchy of genetic factors controlling a network of biological processes. Untangling complex genetic control of tuberculosis susceptibility in humans is inherently difficult. Thus, animal models are used to identify susceptibility genes under controlled experimental conditions in which route of infection, dose, strain, and virulence of M. tuberculosis, as well as environmental factors such as diet and stress, can be standardized (reviewed in (21). Natural variation in host genetic resistance to MTB can be addressed using forward genetic approaches, i.e., from phenotype to gene(s). The strengths of this approach are the ability to identify previously unknown mechanisms of anti-TB immunity and reveal their hierarchy, interactions and individual contributions to pathogenesis during host – pathogen interactions in vivo. Mouse models of MTB infection were used in three independent studies to map resistance/susceptibility genes (reviewed in (11). In each study, a different combination of inbred mice was used as resistant and susceptible partners for linkage analysis (21). Regardless of parental combinations, all groups reported complex multigenic control of host resistance to TB.
Previously, we investigated the genetic basis for extreme susceptibility of inbred mouse strain C3HeB/FeJ to MTB (19). These inbred mice are distinguished from most other strains because they form large necrotic lesions in their lungs after infection with virulent MTB (14) and M. bovis (our unpublished observations). C3HeB/FeJ mice are striking as they lack gross immunological abnormalities in known essential mechanisms of anti-TB immunity since their 1) dendritic cells produce IL-12 (our unpublished observations), 2) mycobacteria-specific CD4+ T cells differentiate along the Th1 pathway and 3) macrophages are capable of responding to IFN-γ (21). Nevertheless, C3HeB/FeJ mice exhibit survival time comparable to mice homozygous for knockouts in T-cell receptor α and β chains, IL-12 β chain, and shorter than that of the iNOS, CD4 and MHC class II knockouts (Kramnik, in press). We used forward genetics to reveal underlying defects in host resistance to TB. The sst1 (super susceptibility to tuberculosis 1) locus on chromosome 1 was mapped (19) and a candidate gene, Ipr1 (intracellular pathogen resistance 1) was identified by positional cloning (21). Two sst1 congenic strains, C3H.B6-sst1 and a reciprocal congenic strain B6.C3H-sst1 (Table 1) were generated to test the isolated effect of sst1 on C3HeBFe/J and C57BL/6J genetic backgrounds. Survival of both sst1 congenic strains fell intermediately between the parental strains indicating that non-sst1 loci had an effect on host survival. Four of those loci on chromosomes 7, 12, 15 and 17 were mapped using a cross between sst1 resistant (sst1R) strains C3H.B6-sst1 and C57BL/6J (18). Incomplete sst1 susceptible (sst1S) allele penetrance in the original cross and higher resistance of the B6.C3H-sst1 mice compared to C3HeB/FeJ (both sst1S) indicated that host resistance mechanisms, independent of the sst1 locus and capable of compensation for the sst1 deficiency, did exist.
Table 1. Genetic composition of congenic/consomic strains used in the study.
| Strain name | Parental background | sst1 allele | Chr7 allele | MST* |
|---|---|---|---|---|
| C3HeB/FeJ | S | S | 3,5 - 5.5 | |
| C3H-Chr7B6 | C3HeB/FeJ | S | R | 6 - 7 |
| C3H.B6-sst1 | C3HeB/FeJ | R | S | 9 -12 |
| C3H.B6-sst1,Chr7B6 | C3HeB/FeJ | R | R | 20 |
| Subcongenic A - D** | C3H.B6-sst1,Chr7B6 | R | to be determined | |
MST = median survival times. Range represents results obtained in several independent experiments after i.v. infections with 1 - 5 × 104 CFU of MTB Erdman.
see Fig.4 for details.
In the case of multigenic quantitative traits, identification of causal polymorphic genes encoded within each locus represents a significant challenge. Of the 2000 QTLs mapped by 2005, the underlying genetic polymorphisms have been identified for less than 1% (22). Factors that impede the progress from QTL to causal gene identification include broad candidate intervals, weak effects of individual loci on overall phenotype, unknown sub-phenotypes (i.e., specific functional effects) of each locus, a possibility of epistatic interactions among individual loci, and the potential complexity of each candidate region that may encode several functionally related genes (21). Thus, attempts to isolate and dissect individual loci following initial QTL mapping are often unsuccessful.
In this study we performed genetic and functional characterization of the second most powerful tuberculosis resistance locus in our model - a quantitative trait locus on mouse chromosome 7 and characterized its epistatic interactions with the sst1. Our data demonstrate that gene interactions play an important role in control of host resistance to TB in immunocompetent hosts and provide a basis for subsequent identification of novel TB resistance gene(s) within the chromosome 7 locus using positional cloning.
Results
I. The chromosome 7 locus is involved in the the sst1-independent genetic control of host resistance to tuberculosis infection
In our previous studies we observed a significant effect of the genetic background on phenotypic expression of the susceptible allele of the sst1 locus (sst1S) by comparing TB progression in two inbred strains homozygous for the sst1S - the C3HeB/FeJ parental inbred mice and the sst1S congenic mouse strain B6.C3H-sst1 (Table 1). The B6.C3H-sst1 congenic mice are genetically identical to the tuberculosis resistant parental strain C57BL/6J with the exception of a 12 cM segment of chromosome 1 (47 - 59 cM) encompassing the sst1 locus. Even though the sst1S strains (B6.C3H-sst1 and C3HeB/FeJ) were more susceptible to MTB than their sst1R counterparts (B6 and C3H.B6-sst1, respectively), tuberculosis progressed more rapidly in C3HeB/FeJ than in B6.C3H-sst1 mice. After i.v. infection with a standard dose of MTB Erdman (5 × 104 CFU per mouse), the B6.C3H-sst1 mice survived for 9 – 12 weeks, while the C3HeB/FeJ succumbed within 3.5 to 5.5 weeks. A low dose aerosol challenge with MTB resulted in a median survival time (MST) in B6.C3H-sst1 and C3HeB/FeJ mice of 225 days and 153 days, respectively (Table 1 and (18)). Using a cross of two sst1R strains C57BL/6J (B6) and C3H.B6-sst1, we have previously mapped four TB resistance loci on mouse chromosomes 7, 12, 15 and 17 (18). At that time it was impossible to determine whether the same or different loci contributed to host resistance in the sst1 susceptible B6.C3H-sst1 mice, because the population of the sst1S F2 hybrids (C3HeB/FeJ × B6.C3H-sst1) was much more susceptible to i.v. infection with a standard dose of MTB, as compared to the sst1R (C3H.B6-sst1 × B6)F2 hybrids (18).
In this study, we optimized the MTB infectious dose to increase phenotypic variation, used a backcross breeding strategy to reduce genetic variation and tested larger mouse populations to make statistical analyses more powerful. The sst1S (C3HeB/FeJ × B6.C3H-sst1)F1 hybrid males were backcrossed on C3HeB/FeJ or B6.C3H-sst1 backgrounds. A total of 220 backcross progeny on B6 and 160 progeny on C3H backgrounds were analyzed for survival after infection with 2 × 104 CFU of MTB i.v.. Backcrossed mice that represented 20% resistant and susceptible extremes in each backcross were selected for a whole genome scan, which was performed using a panel of 240 informative (polymorphic between the parental strains) SNP markers. In this analysis the chromosome 7 locus produced the highest linkage scores in both backcrosses on B6.C3H-sst1 and C3HeB/FeJ genetic backrounds (Z-scores 3.12 and 4.29, respectively). Mice carrying two copies of the B6-derived alleles on chromosome 7 were more resistant than heterozygotes in backcross on B6.C3H-sst1 background, while the heterozygous mice were more resistant than homozygous for the C3H-derived alleles in the backcross on the C3HeB/FeJ background. Thus, for the B6-derived resistance locus on chromosome 7 survival times were distributed as bb > bh > hh indicating that the B6-derived resistance allele was dominant with an additive mode of inheritance.
Next we performed high density genotyping using SNP markers that covered the entire chromosome 7 at 1 - 2 cM intervals in all mice that have been tested in four independent experiments, which included the (C3H.B6-sst1 × C57BL6J)F2 and (C3HeB/FeJ × B6.C3H-sst1)F2 intercross mice reported previously (18)and the backcross mice described above. As shown in Table 2, the Chr7 locus effect was prominent in the sst1R intercross progeny C3H-sst1RB6F2, but was of border-line significance in the sst1S progeny C3FeB6-sst1F2 after infection with the same dose of MTB. When a lower infectious dose of MTB was used to test the sst1S backcross progeny, the Chr7 locus effect was greater. Of note, the QTL candidate regions on chromosome 7 identified in each of four independent experiments were large, spanning 50 -70 Mb and only partially overlapping between 30 and 66 Mb of chromosome 7.
Table 2. Summary of independent replication of the tuberculosis resistance QTL on chromosome 7.
| Cross name | Abbreviated | Cross description | sst1 allele fixed | Chromosome 7 linkage results | |
|---|---|---|---|---|---|
| Z | p-value | ||||
| (C3H.B6-sst1 × C57BL6J)F2* | C3H-sst1RB6F2 | Intercross | R | 4.9 | 0.000006 |
| (C3HeB/FeJ × B6.C3H-sst1)F2 | C3FeB6-sst1F2 | Intercross | S | 2.2 | 0.05 |
| B6.C3H-sst1 × (C3HeB/FeJ × B6.C3H-sst1)F1 | B6-sst1(C3FeB6-st1F1) | Backcross to B6.C3H-sst1 | S | 4.8 | 0.000001 |
| C3HeB/FeJ × (C3HeB/FeJ × B6.C3H-sst1)F1 | C3Fe(C3FeB6-sst1F1) | Backcross to C3HeB/FeJ | S | 2.6 | 0.005 |
is original published cross (18), two-sided p-value; remaining confirmatory crosses are evaluated as one-sided tests of hypothesis of linkage developed in the C3H-sst1RB6F2 cross;
approximate 1 LOD CI around non-parametric mapping statistic from MAPMAKER/QTL
Thus, the tuberculosis resistance quantitative trait locus on chromosome 7 (Chr7 QTL) was replicated in a total of four independent crosses (Table 2). However, additional experiments neither allowed clearer delineation of the candidate region, nor excluded a presence of several resistance/susceptibility loci on this chromosome. Therefore, for further functional and genetic dissection of the Chr7 QTL, we generated a chromosome 7 consomic strain C3H-Chr7B6, which carried two copies of the entire B6-derived chromosome 7 on the C3HeB/FeJ genetic background.
II. Individual effect of the Chr7 locus on host resistance to TB infection and its synergy with the sst1 locus
An isolated effect of the Chr7 QTL on host TB resistance was tested by comparing survival of the parental C3HeB/FeJ and C3H-Chr7B6 consomic mouse strains after i.v. and aerosol infections with MTB. The Chr7 locus resistant allele produced a small increment in survival after i.v. infection with a standard dose of MTB - the C3HeB/FeJ mice had succumbed to infection by 42 days post i.v. challenge, while the C3H-Chr7B6 died within the next week (Fig.1A, left panel). After a low dose aerosol infection, however, the susceptible parental strain C3HeB/FeJ mice died much earlier with a MST of 75 days while the C3H-Chr7B6 mice survived for 120 - 150 days post infection (pi) (Fig 1A, right panel). Thus, the Chr7 locus significantly affected TB progression during chronic infection caused by a low dose aerosol infection with MTB.
Figure 1.

Effect of the Chr7 locus on the course of tuberculosis in C3HeB/FeJ genetic background mice. A: Left panel Survival of the parental C3HeB/FeJ and Chr7 consomic strain (C3H-Chr7B6) following systemic i.v. challenge with 4 × 104 CFU of M. tuberculosis Erdman. Right panel Survival of parental C3HeB/FeJ (C3H) and C3H-Chr7B6 consomic mice following aerosol challenge with 30 - 50 CFU of M. tuberculosis Erdman. Six to eight mice per group were used in each experiment. B: Interactions of the Chr7 and sst1 loci during the course of tuberculosis following i.v. challenge with M. tuberculosis Erdman. MTB burden (CFU) in the organs of the C3H–Chr7B6 (sst1S, S) and C3H.B6-sst1, Chr7B6 (sst1R, R) at 45 days post i.v. challenge with 5×104 CFU of MTB (four mice per group).C: Histopathology of representative tuberculosis lung lesions of the C3H-Chr7B6 left panel and C3H.B6-sst1,Chr7B6 right panel double congenic mice 45 days post i.v. challenge (H&E, original magnification 40×). H&E, original magnification 40×; inset acid fast fluorescent staining of MTB, original magnification 400×.
We hypothesized that the individual effect of the Chr7 resistance allele was suppressed due to the absence of other B6-derived resistance loci after infection with higher dose of MTB i.v.. To test interactions of the Chr7 and sst1 loci, the C3H-Chr7B6 consomic mice were crossed with the sst1R congenic strain C3H.B6-sst1 to produce F1 hybrids heterozygous at both loci. The (C3H.B6-sst1 × C3H-Chr7B6) F1 hybrids were backcrossed on C3H-Chr7B6 consomic strain to produce progeny that were homozygous for the Chr7 resistant allele, but segregated at the sst1 locus. The backcross mice were infected with a standard dose (5 × 104 CFU) of MTB i.v. and sacrificed 45 days pi to assess TB progression. Bacterial loads in the organs of mice grouped by their sst1 allele are presented in Fig.1B. Mice with the susceptible allele of the sst1 locus (S) developed necrotic lung lesions despite the presence of the resistant allele at the Chr7 locus (Fig.1C, left and middle panels). The backcross progeny carrying the sst1 resistant allele (R) had significantly fewer bacteria in their organs (Fig.1B), and did not develop lung necrosis (Fig.1C, right panel). Therefore, the resistant allele of the Chr7 locus failed to prevent the development of lung necrosis, which was controlled by the sst1 locus. However, the Chr7 resistant allele limited the extent of necrosis associated with tuberculosis lung lesions in the sst1 susceptible mice: in the Chr7 resistant C3H-Chr7B6 mice the areas of necrosis were found in the center of well-organized tubercles (Fig.1C, left panel), and advanced necrotic areas were separated from normal lung tissue by a wall of inflammatory cells (Fig.1C, middle panel). This is in contrast with the Chr7 susceptible parental C3HeB/FeJ mice (also sst1S), in which extensive inflammation resembling caseous pneumonia occurred within 25 - 35 days of infection and resulted in earlier death of these mice.
These data demonstrate that an individual effect of the resistant allele of the Chr7 QTL on TB progression can be detected in the susceptible C3HeB/FeJ genetic background. However an overall increase in host resistance due to the Chr7 QTL does not prevent formation of necrosis within tuberculosis lung lesions. The latter is specifically controlled by the sst1 locus. Therefore mechanistically, the Chr7 QTL phenotypic expression is sst1-independent, but its impact on tuberculosis progression at the whole organism level is limited in the presence of the sst1S allele.
III. The Chr7 locus mediates systemic control of TB at later stages of infection
To examine the effect of the Chr7 locus on TB resistance in the presence of the sst1R allele, the B6-derived Chr7 allele was introduced on the C3H.B6-sst1 background. Progeny, homozygous for the sst1R allele and segregated at the Chr7 locus, were produced by backcross-intercross breeding, and infected with MTB i.v., as described above. Survival curves of the intercross mice, grouped by their chromosome 7 allele, are presented in Fig.2A. The Chr7 locus exhibited a strong effect on survival in the presence of the sst1R allele: the MST for mice homozygous for the B6-derived resistant Chr7 allele (bb) was 131 days; the MST for C3H homozygotes (hh) was 56 days. Chr7 heterozygotes (bh) had an intermediate MST, which agrees with additive effects of this locus determined by linkage analyses (Table 2). Subsequently, detailed Chr7 locus studies were performed in the sst1R background using a double consomic/congenic strain C3H.B6-sst1,Chr7B6 carrying homozygous B6-derived Chr7 and sst1 alleles on the C3HeB/FeJ background (Table 1).
Figure 2.

The Chr7 effect on the course of tuberculosis in the sst1R genetic background following i.v. challenge with M. tuberculosis Erdman. A: Dose-dependent effect of the B6-derived resistance allele of the Chr7 locus on survival of the sst1R mice after systemic i.v. infection with 7 × 104 CFU of MTB. All mice in this experiment are homozygous for the susceptible allele of the Chr7 locus. The C3H.B6-sst1,chr7bh and C3H.B6-sst1,chr7bb carry one or two B6-derived resistant alleles of Chr7, respectively. Seven to twelve mice per group were used in the experiment. B: Tuberculosis lung lesion histopathology in the sst1R congenic mouse strains C3H.B6-sst1 and double congenic C3H.B6-sst1,Chr7B6 56 days post infection with MTB (H&E, original magnification 40×). C: Kinetic analysis of mycobacterial loads in spleens, lungs and livers of the parental C57BL/6 (B6), C3H.B6-sst1 and C3H.B6-sst1, chr7B6 mice 18, 38 and 56 days post i.v. challenge with5 × 104 CFU of MTB.
TB progression in two Chr7 disparate sst1R strains - C3H.B6-sst1 and C3H.B6-sst1,Chr7B6 and the resistant parental strain B6 were compared after i.v. infection with a standard dose of MTB. The initial growth of MTB up to 38 days pi was similar in C3H.B6-sst1 and C3H.B6-sst1,Chr7B6 mice (Fig. 2C), while a strong effect of the Chr7 locus occurred at eight weeks post infection: a 1.5 - 2 log increase in MTB burden was observed in all organs of the C3H.B6-sst1 mice carrying the Chr7 susceptible allele (Fig. 2C). The systemic effect of the Chr7 resistant allele was strongly protective: the bacterial load stabilized in the lungs and decreased significantly in spleens and livers of the C3H.B6-sst1,Chr7B6 congenic mouse (Fig. 2C). At 8 weeks post infection histopathology revealed greater lung inflammation, a decrease in airspaces and consolidation of the lung lesions in the Chr7 susceptible mice C3H.B6-sst1 (Fig. 2B, left panel). Meanwhile, the Chr7 resistant C3H.B6-sst1,Chr7B6 mice displayed moderate localized interstitial lung inflammation (Fig.2B, right panel), which at that time was similar to the parental resistant B6 mice (not shown).
To further examine the Chr7 effect in a physiologically more relevant tuberculosis model, the C3H.B6-sst1 and C3H.B6-sst1,Chr7B6 mice were infected with a low dose of MTB (30 - 50 CFU per animal) via aerosol. Four mice of each strain were sacrificed at 2, 6, 12 and 20 weeks pi to monitor TB progression (Fig.3A). Similar kinetics of the bacterial growth was observed until the 12th week pi. However, there was a 1.5 - 2 log increase in the MTB burden in the organs of C3H.B6-sst1 mice between the 12th and the 20th week pi, while bacterial loads remained stable in the Chr7 resistant consomic mice C3H.B6-sst1, Chr7B6.
Figure 3.

Effect of the Chr7 on the course of tuberculosis following low dose aerosol challenge with M. tuberculosis Erdman. A: Bacterial loads in organs of C3H.B6-sst1 and C3H.B6-sst1,Chr7B6 mice at 2, 6, 12 and 20 weeks post aerosol challenge with 30 -50 CFU of MTB strain Erdman. Four mice per strain were sacrificed at each time point. B: Tuberculosis lung lesion histopathology of the C3H.B6-sst1 and C3H.B6-sst1,Chr7B6 mice 20 weeks following low dose aerosol infection with MTB. Upper panels – H&E, original magnification 200×, lower panels – auramine-rhodamine staining of acid fast mycobacteria, original magnification 400×.
Histopathological examination at 20 weeks pi revealed that the Chr7 susceptible mouse lungs contained larger areas of inflammation and less airspace, as compared to those of the C3H.B6-sst1,Chr7B6 consomic mice (Fig.3B, upper left and right panels, respectively). No necrosis in lung lesions of either strain was found consistent with their sst1R genotype. In agreement with higher bacterial loads determined by plating organ homogenates, acid fast fluorescent staining of the lung sections revealed greater numbers of mycobacteria within the lung lesions of the Chr7 susceptible mice (Fig.3B, lower panels). The bacteria were intracellular in both strains. However, macrophages in the lung lesions of C3H.B6-sst1,Chr7B6 consomic mice contained 1-3 bacteria per cell while those in Chr7 susceptible C3H.B6-sst1 mice were loaded with 10 – 20 or more MTB per cell (Fig.3B, right and left lower panels, respectively). These data suggest that the Chr7 locus is involved in control of intracellular multiplication of MTB in vivo. Whether this genetic locus influences macrophage function directly or this is a secondary effect due to insufficient activation of macrophages by exogenous stimuli produced within tuberculosis lesions by other cell types remains to be determined.
To summarize, the Chr7 locus mediates control of intracellular multiplication of MTB in macrophages within tuberculosis granulomas in vivo, and its effect is displayed systemically at a later stage of the disease. The phenotypic expression of the Chr7 locus is significantly more pronounced in the presence of the sst1R allele, which prevents necrosis in tuberculosis lung lesions, extracellular multiplication of the pathogen and early lethality.
IV. Fine mapping of the Chr7 locus using sst1 resistant subcongenic strains
Since the difference in TB susceptibility between mice that carried the Chr7 resistant or susceptible alleles was maximal in the presence of the sst1R allele, for fine mapping of the Chr7 locus, we produced a set of subcongenic strains that carried recombinant chromosomes 7 on the C3H.B6-sst1 genetic background. Being derived from the same C3H.B6-sst1,Chr7B6 grandparent male after a second backcross on C3H.B6-sst1 female, each subcongenic strain was of C3HeB/FeJ genetic background, homozygous for the B6-derived sst1 resistant allele and carried a homozygous recombinant chromosome 7 with a single recombination event, such that a B6-derived segment in each subcongenic strain partially overlapped the candidate QTL region, as shown in Fig.4A.
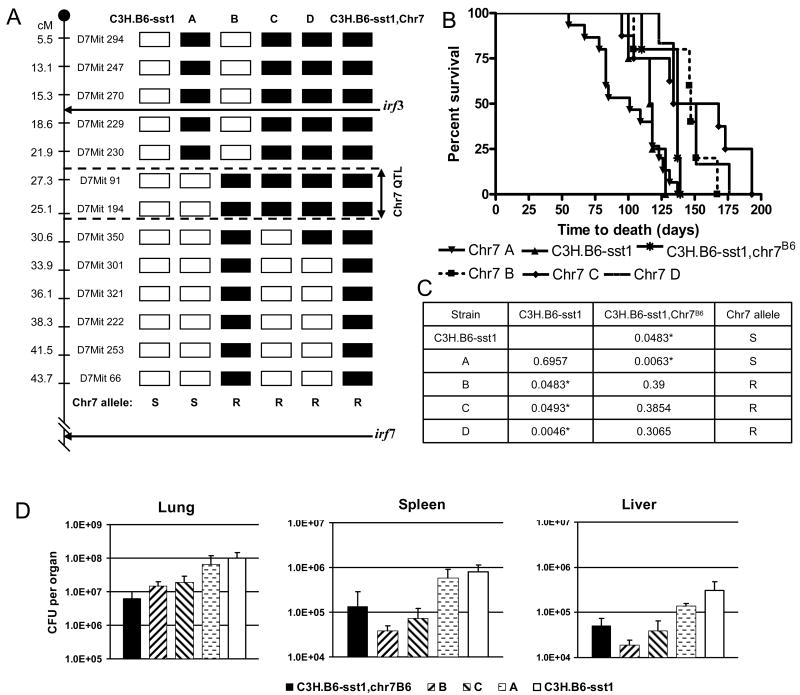
Figure 4.
The Chr7 locus mapping using Chr7 interval-specific subcongenic mouse strains.
A: Schematic diagram of the chromosome 7 interval-specific subcongenic mouse strains. Black and white boxes represent homozygous C57BL/6J and C3HeB/FeJ-derived alleles respectively. The chromosome 7 subcongenic strains mouse strains A, B, C, D are sst1R. The Chr7 allele is determined based on survival (panels B and C) and organ bacterial loads (panel D) after i.v. infection with MTB. B: Survival of four chromosome 7 subcongenic mouse strains A, B, C and D and the parental C3H.B6-sst1 and C3H.B6-sst1,Chr7B6 mice after i.v. infection with a standard dose of MTB Erdman. C: Pairwise comparisons of survival curves of each subcongenic strain with the parental strains to determine allele of the Chr7 locus. D: Bacterial burdens in the organs of the Chr7 subcongenic and parental mouse strains 10 weeks post infection with 5 × 104 CFU of MTB i.v.
Subcongenic strains A, B, C and D and the corresponding parental strains were tested for survival after i.v. challenge with a standard dose of MTB. Median survival time (MST) of the subcongenic strain A (101 days) was significantly shorter than in subcongenic strains B, C and D (MST = 147, 151 and 142.5, respectively, Fig. 4B). Pairwise comparisons of Kaplan - Mayer survival curves using log rank test demonstrated that survival of the subcongenic strain A was statistically indistinguishable from that of the Chr7 susceptible parental strain C3H.B6-sst1 and significantly shorter than that of the resistant consomic strain C3H.B6-sst1, Chr7B6 (Fig.4C). Subcongenic strain B, C and D survival curves were significantly different from those of C3H.B6-sst1 and subcongenic strain A, and these subcongenic strains were as resistant as the consomic parental strain C3H.B6-sst1,Chr7B6. These data indicate that subcongenic strains B,C and D carried the resistant and strain A the susceptible alleles of the Chr7 QTL and therefore, the Chr7 critical interval is delimited by microsatellite markers D7Mit230 and D7Mit350 (Fig.4A).
Since in addition to its effect on mouse survival, the Chr7 QTL had a clear systemic effect on the bacterial loads at late stages of the disease progression, in a second experiment we used both the survival and the bacterial burdens of spleen, liver and lung at 10 weeks post i.v. infection to differentiate the Chr7 resistant and susceptible alleles. As shown in Fig.4D, the bacterial burden in the lungs, spleens and livers of strains A and C3H.B6-sst1 were similar and significantly higher (p < 0.05) than in strains B, C and C3H.B6-sst1,chr7B6. In this experiment the MST of the susceptible strains A and C3H.B6-sst1 equaled 103 and 104 days, respectively, while the MST of strains B, C and C3H.B6-sst1,chr7B6 equaled 150, 163 and 143 days, respectively. Thus according to both criteria, the Chr7 subcongenic strains could be divided into two groups: resistant (strains B and C) and susceptible (strain A) indicating that the same chromosome 7 interval delimited by microsatellite markers D7Mit230 and D7Mit350 controls both mouse survival and the MTB organ burden. Because there were no statistically significant differences between the resistant subcongenic strains B, C and the resistant parental strain C3H.B6-sst1,Chr7B6 (P> 0.3) according to both criteria, we concluded that the entire effect of the Chr7 QTL on tuberculosis resistance was due to this 8.7 cM interval and confidently excluded the irf3 and irf7 genes from the Chr7 locus.
Discussion
Unusually severe lung pathology combined with early lethality that develops after infection with virulent MTB are characteristic for C3HeB/FeJ inbred mice. Because these mice fail to control TB progression in the lungs despite a functional immune system (21), a situation also typical in humans, a better understanding of pulmonary MTB pathogenesis may emerge by identifying causal genetic defects in these mice. Using a cross of these mice with a relatively resistant to tuberculosis inbred mouse strain B6, we have determined that the genetic control of tuberculosis resistance in our model is multigenic and mapped several tuberculosis resistance loci on mouse chromosomes 1 (sst1), 7, 12, 15 and 17.
In our previous mapping study the effect of the chromosome 7 locus was the strongest in a cross of two inbred strains that carried the sst1 resistant allele - B6 and the sst1 congenic C3H.B6-sst1. However, in a cross of two sst1 susceptible mouse strains, C3HeB/FeJ and the B6-derived sst1 susceptible congenic mouse strain B6.C3H-sst1, the chromosome 7 effect fell below the statistical threshold. This raised a possibility that the phenotypic expression of the Chr7 QTL, as well as of other non-sst1 loci identified previously, were dependent on the presence of the sst1 resistant allele. Several observations, however, suggested the existence of sst1-independent genetic factors capable of counteracting the devastating effect of the sst1S allele on TB progression. We repeated our attempt to map novel tuberculosis resistance loci in a cross of two sst1 susceptible parental strains using optimized infectious dose and backcross breeding strategy. Surprisingly, the highest linkage scores were obtained for loci on chromosomes 7, 15 and 17, which overlap with QTLs identified in our previous cross of the sst1R parents. These data demonstrate that, in principle, similar host resistance mechanisms may operate in the presence and in the absence of the sst1-dependent mechanism, although their effects are less pronounced in the sst1S genetic background.
Because of “genetic noise” produced by multiple unlinked loci in QTL analysis, candidate intervals are difficult to determine precisely. In each of our crosses the location of the Chr7 QTL peak varied. Therefore, a so-called consomic (chromosome substitution) mouse strain C3H-Chr7B6 was constructed by transferring the whole B6-derived chromosome 7 on the C3HeB/FeJ genetic background using a marker-assisted breeding strategy (25). Initially, the individual effect of the Chr7 locus on mouse survival was tested after i.v. infection. Although statistically significant, it was weak and hardly amenable to further dissection and gene identification. In isolation, the Chr7 locus resistant allele was unable to prevent necrosis within TB lung lesions in C3HeB/FeJ mice. On the sst1R genetic background, however, the B6-derived Chr7 locus produced much more pronounced chromosome dose-dependent phenotypic effect consistent with predicted dominant/additive pattern of inheritance.
At the whole organism level, the combined effect of the two loci, sst1 and Chr7, transformed an extremely TB-susceptible parental mouse C3HeB/FeJ that succumbs in 3.5 to 5 weeks to systemic MTB infection into a mouse with a relatively resistant phenotype that survives for 18 – 24 weeks, approximately a half of the difference between parental strain survival times. Each locus had a specific effect in vivo: the sst1R worked at an earlier time point and was responsible for preventing necrosis within forming TB granulomas specifically in the lungs. In the sst1 resistant setting, the Chr7 locus controlled intracellular MTB multiplication within tuberculosis inflammatory lesions. The effect of this locus was systemic i.e., observed in lungs, spleens and livers, and manifested at later time after infection. Differences in phenotypic expression of the sst1 and Chr7 loci suggest that each locus mediates a distinct molecular pathway. We propose the following explanation of the synergistic effect of the two loci: within the lung granulomas the sst1R locus ensures survival of the MTB-infected macrophages, while the resistant allele of the Chr7 locus limits a rate of the intracellular MTB multiplication in these cells. Because the sst1S macrophages are sensitized to necrotic cell death induced by virulent MTB (21), formation of necrotic microfoci within the lung lesions of the sst1S mice creates a favorable environment for rampant extracellular growth of the bacteria in the lungs (21) and, thus, limits the effect of the Chr7 locus explaining a hierarchical relationship between the two loci. Although the activities of the two TB resistance loci seemingly converge on macrophages, our ongoing studies will establish whether the effect of the Chr7 locus is macrophage cell autonomous or it is dependent on interactions of macrophages with other cell types within TB granulomas.
To date, linkage of tuberculosis resistance to chromosome 7 was identified in two independent studies. Mitsos et al. mapped the TB resistance locus on chromosome 7 (trl3) in a cross of B6 and DBA/2 mouse strains (21). Peak location of the trl3 on proximal chromosome 7 overlaps with the Chr7 QTL described here. Since C3H inbred mouse strain was derived from a cross of DBA and Bagg albino mice (26), the two susceptible strains are related and the Chr7 locus, may represent a common ancestral genetic polymorphism. On the contrary, the susceptible allele of the sst1 locus represents a recent mutation, which occurred in the C3HeB/FeJ, the only substrain of C3H that carries the sst1 susceptible allele. The interplay of the Chr7 and sst1 loci illustrates how effects of common ancestral polymorphisms may be modified, or even obscured, by less frequent recent mutations. Multigenic hierarchical genetic control of TB resistance presented in this study explains why previous attempts to attribute strain differences in tuberculosis susceptibility to a single known polymorphic candidate locus (21) were unsuccessful (28). Instead, identification of causal polymorphisms and physiological pathways whose interactions determine outcomes of tuberculosis infection is possible via systematic forward genetic analysis.
The reduced chromosome 7 region mapped here contains many attractive candidate genes. However, commenting on the role of individual genes would be highly speculative without further narrowing the critical interval. For example, analysis of interval-specific subcongenic strains in our studies excluded irf3 and irf7, which previously were considered top candidate genes, from the candidate region. It is important to note that the reduced candidate region is partially homologous to human chromosome 15q11-13, which has been previously identified as a tuberculosis susceptibility locus with suggestive evidence of linkage using genome-wide linkage analysis in humans by Cervino et al. (29). In a follow up study these authors found significant association of tuberculosis susceptibility with a 7 bp deletion in UBE3A gene encoded within the 15q11-13 region and concluded that UBE3A or a closely flanking gene may be a tuberculosis susceptibility locus. The reduced candidate region on mouse chromosome 7 also encompasses the Ube3a gene. UBE3A is a ubiquitin ligase known to function in the uniquitination and degradation of several proteins including p53 (30). The role of UBE3A in response to human papilloma virus (HPV) has been studied and this protein was shown to mediate the association of the E6 protein of HPV with p53 (30). However, this gene's role in control of bacterial infections remains unknown.
Further work to identify candidate genes and understand their function may reveal novel mechanisms of tuberculosis resistance common in mice and humans. Together with the analysis of the pathogen itself, this approach will permit more complete understanding of the pathogenesis of tuberculosis infection, as well as the evolutionary successful and sophisticated virulence strategy of MTB.
Experimental procedures
Animals
C3HeB/FeJ and C57BL/6J mice were purchased from The Jackson Laboratory (Bar Harbor, Maine, USA). C3H.B6-sst1 mice were generated by introgression of a B6-derived interval of Chr 1 (49 - 60 cM) encompassing the mouse TB susceptibility sst1 locus on the susceptible genetic background, C3HeB/FeJ, using marker-assisted breeding and 10 backcrosses (21). Chromosome 7 consomic mice, C3H-Chr7B6, were generated using a microsatellite marker assisted speed congenic breeding strategy (25). The entire B6-derived chromosome 7, which encompasses the QTL peak region identified by linkage analysis, was transferred to the C3HeB/FeJ parental strain yielding the C3H-chr7B6 consomic strain or to the C3H.B6-sst1 congenic strain yielding the C3H.B6-sst1,chr7B6 double congenic/consomic strain (Table 1). Chromosome 7 subconsomic strains A - D were derived from the C3H.B6-sst1,chr7B6 strain after backcross on to C3H.B6-sst1 background. Mice used in this study are presented in Table 1.
All sst1R strains carried the C3H-derived resistant allele of the Slc11a1 gene (formerly known as Nramp1) (21). Mice were housed under pathogen-free conditions in barrier animal facilities at the Harvard Medical School and were provided autoclaved chow and water ad libitum. Moribund mice were humanely killed. Time to death experiments were performed with the full knowledge and approval of the standing committee on animals at Harvard Medical School (protocol #03000).
Bacteria
Frozen stocks of M. tuberculosis (Erdman strain, Trudeau Institute, Saranac Lake, NY, USA) were prepared from lungs of B6 mice infected i.v. at least 6 months prior to harvest. Lung tissues were ground in a stomacher in 10 ml 1X PBS. To culture mycobacteria, 500 μL from neat and 10× diluted samples were plated on oleic albumin complex (OADC) -enriched 7H10 Middlebrook (Difco) agar plates. After 10 - 12 days of growth on solid media at 37°C, mycobacteria were collected by scraping the plates that produced visible growth of the bacteria, washed in PBS containing 0.05% Tween-80 and resuspended in 50 mL of OADC-enriched Middlebrook 7H9 medium. Clumps were removed by sedimentation at 1g and liquid cultures were grown in roller bottles to an O.D. of 0.4-0.6. Aliquots in 500 μL volumes were frozen and stored at -80°C. Viability of cultures was tested after one week by plating dilutions from a vial to determine colony forming units (cfu). The virulence of prepared stocks was tested by infecting susceptible C3H and resistant B6 female mice i.v.
Infection
An aliquot of M. tuberculosis was thawed, diluted 10× in phosphate buffered saline (1×) containing 0.05% Tween-80 and sonicated for 10 min in a cup horn sonicator. For i.v. infection, bacteria were diluted with PBS 1× containing 0.05% Tween-80. Mice were injected i.v. in the tail vein with 2-10 × 104 CFU live bacilli in 100 μL. Aerosol infections were performed using a Madison aerosol chamber (21). Aliquots of the bacterial suspension used for each infection were plated to determine actual infectious dose.
To enumerate bacterial loads, organs were harvested under aseptic conditions at the stated times, were homogenized individually in PBS 1× containing 0.05% Tween-80 and were plated on Middlebrook 7H10 agar enriched with 10% oleic acid/albumin/dextrose/catalase (OADC) (Difco, MI, USA) after serial 10-fold dilutions and 21-28 days of incubation at 37°C. Four to five animals per group were tested at each time point. Mice were sacrificed using isoflurane anesthesia.
Histopathology
Organs were fixed in 10% formalin for >24h, embedded in paraffin, sectioned (5 μm thickness) and stained with H&E by standard procedure at the Harvard Medical School Rodent Histopathology Core Facility.
Auramine/Rhodamine staining
Acid fast bacilli were identified in tissue sections using auramine/rhodamine dye (0.1% auramine O, 0.01% rhodamine B in H2O; Sigma, MO, USA). Sections were stained for 20 min at RT in the dark, destaining with 3% HCl in 70% EtOH (5 min, RT) and counterstained with Mayer's hematoxylin (VWR).
Linkage analysis
Survival phenotype linkage analyses to autosomal loci were performed using the Mapmaker/SURVIVOR extension of MAPMAKER (31). This software computes logarithm of odds (LOD) scores for the Cox proportional hazards model using a variant of the expectation maximization algorithm with Monte Carlo simulation. Mapmaker/SURVIVOR is available from MJD at mjdaly@genome.wi.mit.edu.
Statistical analysis
MTB loads were compared using a t-test (GraphPad Prizm, Version 4.0) and are presented as means ± s.d. Kaplan-Meier survival curves of mouse populations stratified by genotype were plotted using GraphPad Prizm and the log-rank tests were used to identify statistical differences between them.
Acknowledgments
We would like to thank Drs. Edward Jarroll and Angele Nalbandian for critical reading of this manuscript.
Abbreviations
- MTB
Mycobacterium tuberculosis
- sst1
super susceptibility to tuberculosis 1
- Ipr1
intracellular pathogen resistance protein 1
- QTL
quantitative trait locus
- Chr7
chromosome 7 locus
References
- 1.WHO Global tuberculosis control - surveillance, planning, financing. WHO Report 2006. 2006 [Google Scholar]
- 2.Schurr E. Is susceptibility to tuberculosis acquired or inherited? J Intern Med. 2007 Feb;261(2):106–11. doi: 10.1111/j.1365-2796.2006.01741.x. [DOI] [PubMed] [Google Scholar]
- 3.Britton WJ, Fernando SL, Saunders BM, Sluyter R, Wiley JS. The genetic control of susceptibility to Mycobacterium tuberculosis. Novartis Found Symp. 2007;281:79–89. doi: 10.1002/9780470062128.ch8. discussion -92, 208-9. [DOI] [PubMed] [Google Scholar]
- 4.Hill AV. Aspects of genetic susceptibility to human infectious diseases. Annu Rev Genet. 2006;40:469–86. doi: 10.1146/annurev.genet.40.110405.090546. [DOI] [PubMed] [Google Scholar]
- 5.Hill AV. The genomics and genetics of human infectious disease susceptibility. Annu Rev Genomics Hum Genet. 2001;2:373–400. doi: 10.1146/annurev.genom.2.1.373. [DOI] [PubMed] [Google Scholar]
- 6.Buschman E, Apt AS, Nickonenko BV, Moroz AM, Averbakh MH, Skamene E. Genetic aspects of innate resistance and acquired immunity to mycobacteria in inbred mice. Springer Semin Immunopathol. 1988;10(4):319–36. doi: 10.1007/BF02053844. [DOI] [PubMed] [Google Scholar]
- 7.Lurie MB, Zappasodi P, Dannenberg AM, Jr, Weiss GH. On the mechanism of genetic resistance to tuberculosis and its mode of inheritance. American Journal of Human Genetics. 1952;4:302–14. [PMC free article] [PubMed] [Google Scholar]
- 8.Lynch CJ, Pierce-Chase CH, Dubos R. A Genetic Study of Susceptibility to Experimental Tuberculosis in Mice Infected with Mammalian Tubercle Bacilli. J Exp Med. 1965 Jun 1;121:1051–70. doi: 10.1084/jem.121.6.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medina E, North RJ. Genetically susceptible mice remain proportionally more susceptible to tuberculosis after vaccination. Immunology. 1999 Jan;96(1):16–21. doi: 10.1046/j.1365-2567.1999.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ulrichs T, Kaufmann SH. New insights into the function of granulomas in human tuberculosis. J Pathol. 2006 Jan;208(2):261–9. doi: 10.1002/path.1906. [DOI] [PubMed] [Google Scholar]
- 11.Fortin A, Abel L, Casanova JL, Gros P. Host genetics of mycobacterial diseases in mice and men: forward genetic studies of BCG-osis and tuberculosis. Annu Rev Genomics Hum Genet. 2007;8:163–92. doi: 10.1146/annurev.genom.8.080706.092315. [DOI] [PubMed] [Google Scholar]
- 12.North RJ, Jung YJ. Immunity to tuberculosis. Annu Rev Immunol. 2004;22:599–623. doi: 10.1146/annurev.immunol.22.012703.104635. [DOI] [PubMed] [Google Scholar]
- 13.Sanchez F, Radaeva TV, Nikonenko BV, Persson AS, Sengul S, Schalling M, et al. Multigenic control of disease severity after virulent Mycobacterium tuberculosis infection in mice. Infect Immun. 2003 Jan;71(1):126–31. doi: 10.1128/IAI.71.1.126-131.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kramnik I, Demant P, Bloom BB. Susceptibility to tuberculosis as a complex genetic trait: analysis using recombinant congenic strains of mice. Novartis Found Symp. 1998;217:120–31. doi: 10.1002/0470846526.ch9. discussion 32-7. [DOI] [PubMed] [Google Scholar]
- 15.Lavebratt C, Apt AS, Nikonenko BV, Schalling M, Schurr E. Severity of tuberculosis in mice is linked to distal chromosome 3 and proximal chromosome 9. J Infect Dis. 1999 Jul;180(1):150–5. doi: 10.1086/314843. [DOI] [PubMed] [Google Scholar]
- 16.Mitsos LM, Cardon LR, Fortin A, Ryan L, LaCourse R, North RJ, et al. Genetic control of susceptibility to infection with Mycobacterium tuberculosis in mice. Genes Immun. 2000 Dec;1(8):467–77. doi: 10.1038/sj.gene.6363712. [DOI] [PubMed] [Google Scholar]
- 17.Mitsos LM, Cardon LR, Ryan L, LaCourse R, North RJ, Gros P. Susceptibility to tuberculosis: a locus on mouse chromosome 19 (Trl-4) regulates Mycobacterium tuberculosis replication in the lungs. Proc Natl Acad Sci U S A. 2003 May 27;100(11):6610–5. doi: 10.1073/pnas.1031727100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yan BS, Kirby A, Shebzukhov YV, Daly MJ, Kramnik I. Genetic architecture of tuberculosis resistance in a mouse model of infection. Genes Immun. 2006 Feb 2; doi: 10.1038/sj.gene.6364288. [DOI] [PubMed] [Google Scholar]
- 19.Kramnik I, Dietrich WF, Demant P, Bloom BR. Genetic control of resistance to experimental infection with virulent Mycobacterium tuberculosis. Proc Natl Acad Sci U S A. 2000 Jul 18;97(15):8560–5. doi: 10.1073/pnas.150227197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yan BS, Pichugin AV, Jobe O, Helming L, Eruslanov EB, Gutierrez-Pabello JA, et al. Progression of pulmonary tuberculosis and efficiency of bacillus Calmette-Guerin vaccination are genetically controlled via a common sst1-mediated mechanism of innate immunity. J Immunol. doi: 10.4049/jimmunol.179.10.6919. [DOI] [PubMed] [Google Scholar]