Abstract
In adaptive immunity, T helper-17 lymphocytes produce the IL-17 and IL-22 cytokines that stimulate mucosal antimicrobial defenses and tissue repair. Here, we observed that the TLR5 agonist flagellin induced swift and transient transcription genes encoding IL-17 and IL-22 in lymphoid, gut and lung tissues. This innate response also temporarily enhanced the expression of genes associated with the antimicrobial Th17 signature. The source of the Th17-related cytokines was identified as novel populations of CD3negCD127+ immune cells among which CD4-expressing cells resembling lymphoid tissue inducer cells. We also demonstrated that dendritic cells are essential for expression of Th17-related cytokines and so for stimulation of innate cells. These data define that TLR-induced activation of CD3negCD127+ cells and production of Th17-related cytokines may be crucial for the early defenses against pathogen invasion of host tissues.
Keywords: Toll-like receptor, innate immunity, mucosal immunity, dendritic cell
Keywords: Animals; Antigens, CD3; genetics; immunology; metabolism; Cells, Cultured; Dendritic Cells; drug effects; immunology; metabolism; Female; Flagellin; pharmacology; Flow Cytometry; Gene Expression; drug effects; immunology; Ileum; drug effects; immunology; metabolism; Interleukin-17; genetics; immunology; metabolism; Interleukin-7 Receptor alpha Subunit; genetics; immunology; metabolism; Interleukins; genetics; immunology; metabolism; Lymphoid Tissue; cytology; immunology; metabolism; Male; Mice; Mice, Inbred BALB C; Mice, Inbred C57BL; Mice, Knockout; Mice, SCID; Mice, Transgenic; Mucous Membrane; cytology; immunology; metabolism; Oligonucleotide Array Sequence Analysis; Signal Transduction; immunology; Spleen; cytology; immunology; metabolism; Toll-Like Receptor 5; genetics; immunology; metabolism
Introduction
Toll-like receptors (TLR) are key players in innate immunity and are essential for sensing microbial components and triggering the host defense (1). At the luminal interface, the TLR response is mediated by the epithelium and mainly consists of neutrophil recruitment and activation (2). After microbes cross the epithelium, sensing occurs within the lamina propria. However, the nature of the TLR-mediated innate cells and defense factors that are triggered by microbial desequestration has yet to be defined.
Recent studies highlighted the contribution of IL-17A, IL-17F and IL-22 to defensive reactions within the mucosa (3–6). These cytokines help orchestrate innate immunity by stimulating epithelial cells to produce defense molecules, matrix proteases and tissue repair molecules (7, 8). The source of IL-17A, IL-17F and IL-22 varies. During an adaptive response, the lymphocytes that differentiate into T helper 17 (Th17) cells are the main producers of cytokines (9). IL-17A can rapidly be produced during innate responses to bacteria or microbial molecular patterns by γδ T lymphocytes in a TLR4-dependent manner, natural killer T (NKT) cells activated with α-galactosylceramide or lymphoid tissue inducer (LTi)-like cells following stimulation with the TLR2/Dectin-1 agonist zymosan (10–12). NK-like and LTi-like innate lymphocytes expressing IL-7Rα, NKp46, the transcription factor RORγt and eventually CCR6 are sources of IL-22 and/or IL-17 in mucosa under steady-state conditions (13–18). Interestingly, microbial flora colonizing mucosa are required to switch on lasting IL-17 and IL-22 production (15, 17). In absence of these innate lymphocytes, infectious colitis is exacerbated, suggesting an operational role of IL-22 and IL-17 in the gut’s innate immunity (15, 17). However, the link between TLR-mediated signaling, Th17-related cytokine production by innate immune cells, and mucosal defenses has not been defined.
The ability of TLR5 signaling to induce mucosal production of IL-17 and IL-22 and thereby promote antimicrobial defense has never been investigated. TLR5 detects flagellins - the main protein of bacterial flagella (19). Flagellins are expressed by bacteria, particularly pathogenic bacteria, in the gut and the lung and activate epithelial TLR5 signaling (19–21). Flagellin expression is switched off as soon as bacteria translocate into the lamina propria (22). Detection of flagellin molecules represents therefore an alarm signal for subepithelial invasion and/or disruption of the epithelial barrier function. TLR5 signaling is rapidly induced in the lamina propria dendritic cells (DCs) of the small intestine (23). In the present study, we show that flagellin activates (via DCs) the splenic and mucosal production of IL-17 and IL-22 and the subsequent expression of target genes. This TLR5-mediated response was associated with a unique population of immune cells expressing CD127 but not CD3 that resembles LTi cells, LTi-like or NK-like innate lymphocytes. Our findings suggest that CD3negCD127+ innate immune cells may be instrumental to the host’s mucosal defense through the early production of Th17-related cytokines.
Materials and methods
Mice
Specific-pathogen free (SPF) mouse strains C57BL/6J, C57BL/6J-Ly5.1, BALB/c, and Tcrb−/−, Tcrd−/−, Tcrb−/−Tcrd−/−, Tlr5−/− (24), Myd88−/− (25), transgenic animals for pre-TCRα, Cd11c-DTR-EGFP (Itagx-DTR/EGFP) (26), Rag2−/−Il2rg−/− backcrossed on C57BL/6J mice, Cd1d−/− backcrossed on BALB/c background, and C.B-17 scid (SCID) mice were purchased from Charles River Laboratories, the Jackson laboratory, or Janvier (France) or bred in an accredited establishment (#A59107, Institut Pasteur de Lille; Transgenose Institute CNRS, Orleans; RCHCI at ETHZ; LICR Brussels and Lausanne branches). Animals (6–16 weeks old) were used according to national regulations and ethical guidelines.
For bone marrow (BM) chimera, recipient mice were irradiated (1000–1500 rads) and reconstituted 2-to-24h later with BM cells (4–20 × 106 cells i.v.). These mice were used at 10–16 weeks post-transplantation and the degree of chimerism was assessed by measuring CD45.1 and CD45.2 surface expression by leukocytes. The current protocol yielded 96.7% reconstitution for Cd11c-DTR/EGFP→C57BL/6 (WT) in spleen, 98.2% for Tlr5−/−→WT and 97.2% for WT→Tlr5−/− in lung. Depletion of CD11c+ cells was achieved by injecting i.p. diphteria toxin (DTX) as described (26). Depletion of γδ T cells (about 90% depletion) and NK cells cells (about 72% depletion) was performed by injecting i.p., 24h prior to flagellin treatment, 100μg mAb specific for TCRδ chain (GL3 clone) or NK1.1 (PK136) or irrelevant mAb HB152 as control.
Flagellin administration
LPS-depleted flagellin FliC from Salmonella typhimurium (5μg) produced as described (21), ultrapure LPS from Escherichia coli (serotype 0111:B4, 5μg, Invivogen), or phosphorothioate CpG oligonucleotide (TCCATGACGTTCCTGATGCT, 5μg, Eurogentec) diluted in PBS were injected i.v. or i.p to mice.
Flow cytometry and sorting
Spleens were digested with collagenase D (Roche, 0.5 mg/ml), DNase I (Sigma 40μg/ml) during 10 min at 37°C. Cells were stained for CD127-FITC, CD45.1-FITC, CD45.2-PE, PE-conjugated lineage-specific antibodies (CD3, B220, Gr1, CD11b, CD11c), MHCII-PE, NK1.1-PercP-Cy5.5, CD4-APC, CD11c-APC, and CD45.1-Pacific Blue (Becton Dickinson, BioLegend and eBioscience) and sorted on a BD FACSAria™.
Dendritic cell culture
DC were differentiated from bone marrow as described (25). On day 7 or 11, BMDCs were stimulated for 2h and analyzed.
Determination of cytokine production
CCL20 and IL-22 (R&D Systems) and IL-17A (eBioscience) levels were measured by ELISA in serum and tissue homogenates prepared with T-PER Reagent (Pierce) supplemented with protease inhibitors (Roche).
Gene expression
Total RNA was extracted with the Nucleospin RNA II kit (Macherey Nagel) and reverse-transcribed with the High-Capacity cDNA Archive Kit (Applied Biosystems). A pre-amplification of cDNA from sorted cells was performed prior to real time PCR using the PreAmp kit (Applied Biosystems). cDNA was amplified using SYBR Green-based real time PCR (Table S1) or commercial TaqMan assays (Applied Biosystems). For high throughput analysis, Taqman Low Density Arrays (Applied Biosystems) were used. Analysis was carried out using Real Time StatMiner software (Integromics). Relative mRNA levels (2−ΔΔCt) were determined by comparing (i) the cycle thresholds (Ct) for the gene of interest and Actb (ΔCt) and (ii) ΔCt values for treated and control groups (ΔΔCt). Ct upper limit was fixed to 33 cycles.
Microarrays
Total RNA (2μg) was processed on the Mouse Whole Genome Arrays v2.0 (Applied Biosystems) (27). Data were analyzed using the NeONORM method and heatmaps were created as described (27, 28). Gene Ontology was analyzed using the Panther Protein Classification System (http://www.pantherdb.org). Microarray data were deposited in the publicly available database: http://mace.ihes.fr with accession number: 2844328654.
Statistical analysis
The Mann-Whitney test and the Graphpad Prism software 5.0 were used in analyses. The Limma test with Benjamini-Hochberg FDR correction was used for high throughput PCR with Taqman Low Density Arrays. Results were considered significant for P < 0.05 indicated by “*”. Results are expressed as arithmetic means ± SD.
Results
Systemic TLR5 signaling enhances Il17a, Il17f and Il22 gene expression in lymphoid tissues
To establish whether or not TLR stimulation promotes the rapid expression of the Th17-related cytokines, mice were treated i.p. or i.v. with a TLR4 agonist (lipopolysaccharide or LPS), a TLR5 agonist (flagellin) or a TLR9 agonist (CpG). Gene expression in spleen and lymph nodes was then monitored (Fig. 1A–B). Flagellin administration triggered within 2h about 1,000-fold increase of Il22 mRNA levels. Similarly, Il17a and Il17f gene expression was upregulated. A TLR5-mediated, Th17-related innate response was also observed in the mediastinal and inguinal lymph nodes and, to a lesser extent in the liver (Fig. 1 and Fig. S1). LPS was initially shown to promote Il22 expression in many tissues (29). We found that LPS also enhanced the Th17-related innate response but to a lesser extent than flagellin did (Fig. 1A–B and Fig. S1). Although TLR9-mediated signaling activated the response in lymph nodes, it was devoid of any effect in the spleen.
Fig. 1. TLR5 signaling promotes a swift, transient, Th17-related response.
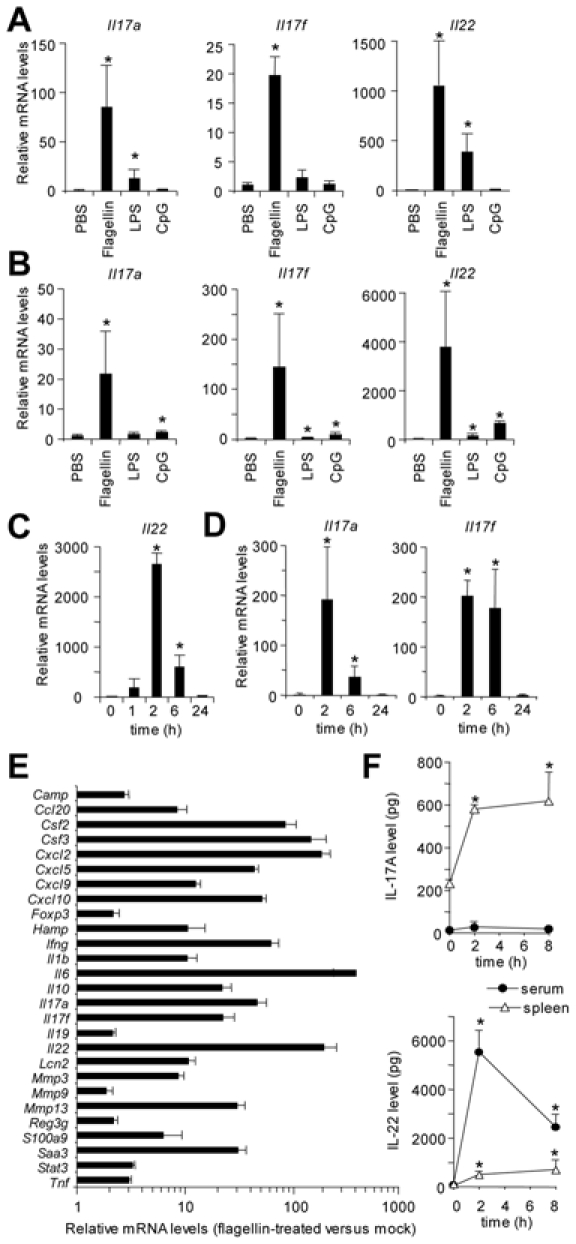
C57BL/6 mice (n=3–4) were treated i.p. or i.v. with PBS, flagellin, LPS or CpG. Tissues were assayed 2h later (or as indicated) for cytokine production or mRNA levels. (A) Spleen and (B) mesenteric lymph node gene expression in response to i.v. injection of TLR agonists. Kinetic analysis of transcription in mesenteric (C) and mediastinal (D) lymph nodes after i.v. flagellin injection. (E) Spleen transcriptional signature after i.p. flagellin injection. mRNA levels are expressed relative to the PBS group. (F) Cytokine production in spleen extract (per whole spleen) and serum (per ml) after i.p. flagellin injection. The results are representative of 2 to 4 experiments. Results are given as means ± SD. Asterisks indicate P<0.05 in Mann-Whitney test relative to PBS group. In panel E, all genes display P<0.05 in Limma test.
The flagellin-dependent response was transient and peaked at 2h; mRNA levels returned to baseline levels after 24h (Fig. 1C–D). Gene profiling showed that the expression of genes specific for TLR-, IL-17R- and IL-22R-mediated signaling was significantly enhanced in spleen (Fig. 1E). These genes encode pleiotropic and Th17-promoting cytokines (TNF-α, IL-1β, and IL-6), chemokines that are specific for neutrophils, monocytes and lymphocytes (CXCL-1, -2, -5, -9, and -10), antimicrobial molecules like CAMP and HAMP, lipocalin 2 (Lcn2), S100A9 and tissue remodeling proteases MMP-3 and -13. Strikingly, the expression of chemokine CCL20 which is specific for the recruitment of DC precursors, Th17 lymphocytes, LTi-like or NK-like cells (12, 14, 30, 31) was significantly upregulated. The transcription of IFN-γ encoding gene was also upregulated by flagellin treatment. However, we did not observe any change in the expression of genes coding for IL-21, RORγt or TGF-β (i.e. other factors involved in Th17 differentiation). As shown in Fig. 1F, IL-22 levels rose significantly in serum and spleen from flagellin-treated animals whereas IL-17A was hardly detectable in serum but rose 3-fold in the spleen. In conclusion, TLR5 signaling in lymphoid tissues promotes the rapid production of the innate cytokines IL-17A, IL-17F and IL-22 - a pattern which resembles a Th17-related innate response.
TLR5-mediated innate responses require γc chain-dependent immune cells
TLR5 is expressed by monocyte/macrophage/DC lineages, NK cells, CD4+ lymphocytes and radioresistant stromal cells but not B lymphocytes (25, 32–35). To define the cells involved in the early production of IL-17 and IL-22, we used bone marrow (BM) chimera expressing or not Tlr5 and tested their ability to respond to flagellin. As shown in Fig. 2A and 2E, TLR5-competent hematopoietic cells were required to trigger flagellin-mediated Il17 and Il22 gene expression. By using SCID, preTCRα animals harboring enhanced number of γδ lymphocytes, Tcrb−/− and Tcrd−/− mice, we demonstrated that neither B cells nor TCRαβ-/TCRγδ-expressing T lymphocytes were required for flagellin-mediated Il17 and Il22 expression (Fig. 2B and Fig. S2A–B and S2D). In contrast, the response was impaired in Rag2−/−Il2rg−/− mice that have almost normal DCs but lack B and T lymphocytes as well as NK, NKT, LTi, NK-like and LTi-like cells, all of which depend on the interleukin receptor γc chain encoded by Il2rg gene (Fig. 2C and 2E) (12, 15, 17, 36). The impairment was not a collapse of TLR5 signaling, since the liver was still responsive to flagellin (Fig. 2D). Our experiments using genetically deficient animals and depleting antibodies suggested that CD1d-restricted NKT cells or NK cells were not drivers of the TLR5-mediated response (Fig. S2C–D). Therefore, our data showed that the cells expressing Th17-related cytokines after flagellin stimulation require the interleukin receptor γc chain for differentiation or activation but are not NK, NKT or TCRγδ–expressing innate lymphocytes.
Fig. 2. The interleukin receptor γc chain is required for the TLR5-mediated, Th17-related innate response.
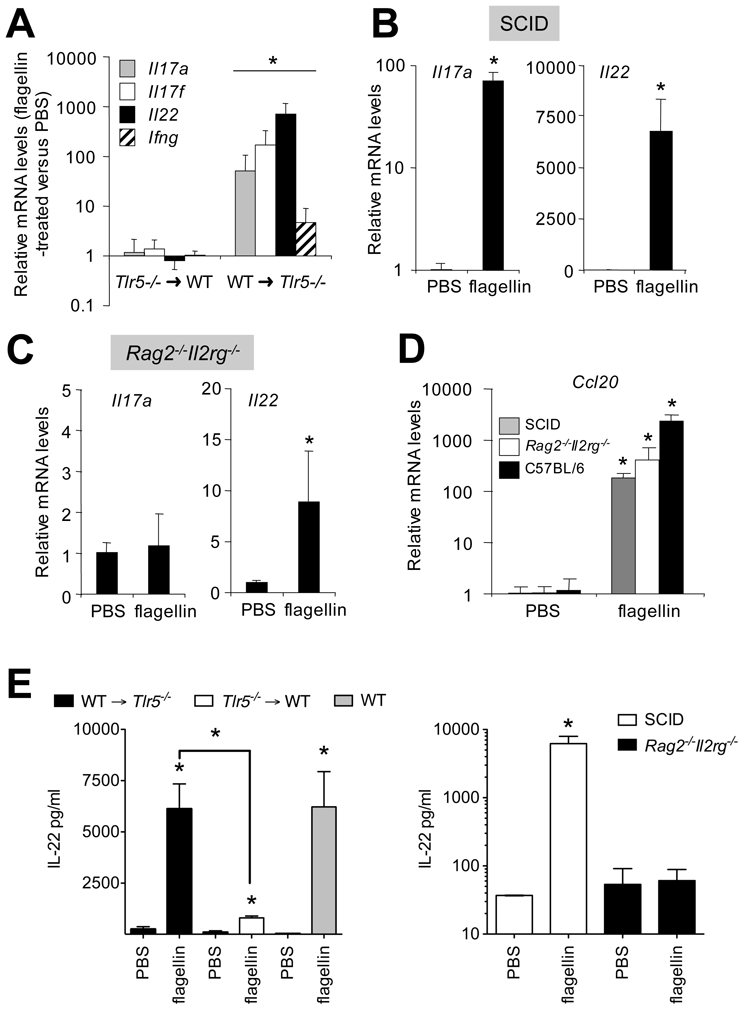
Mice (n=3–4) were treated i.p. with PBS or flagellin. Lymphoid tissues and serum were sampled 2h after injection for the quantification of mRNA levels and ELISA. (A) Response in mediastinal lymph nodes from C57BL/6 (WT) →Tlr5−/− and Tlr5−/− →WT bone marrow chimera. The spleen response in SCID (B) and Rag2−/−Il2rg−/− (C) mice. (D) The flagellin-mediated liver response. mRNA levels are expressed relative to the PBS group. (E) IL-22 production in serum. Results are given as means ± SD. Asterisks indicate P<0.05 in Mann-Whitney test relative to PBS group.
CD3negCD127+ LTi-like cells produce IL-17 and IL-22 in response to TLR5 signaling
We next sought to determine which γc chain-dependent innate immune cells are involved in TLR5-mediated response. Recent work has suggested that innate lymphocytes expressing IL-7R (i.e. the CD127 or IL-7Rα chain and the CD132 or γc chain) and LTi/NK cell markers are sources of IL-22 and IL-17 (12–17). To determine whether or not innate immune cells produce Th17-related cytokines, splenic cells from mock- and flagellin-treated animals were sorted on the basis of lineage (Lin) markers (CD11b, CD11c, Gr1, CD3, and B220), NK1.1, CD4 and CD127 (Fig. 3A). After TLR5 stimulation, LinnegNK1.1negCD127+CD4neg and LinnegNK1.1negCD127+CD4+ cells were found to strongly upregulate Il17f and Il22 expression about 80- and 500-fold, respectively (Fig. 3B). These subsets account for about 0.5–1% of LinnegNK1.1neg cells and 0.02–0.1% of splenocytes in a C57BL/6 mouse. Similar observations were done using CD3negCD127+CD4+ cells from SCID mice (Fig. 3D). Both subsets were found to express CD45, indicating an hematopoietic origin and their classification as immune cells (Fig. S3A). We also found that the CD3negCD127+CD4+ and CD3negCD127+CD4neg cells are mostly absent in the Rag2−/−Il2rg−/− mouse (Fig. S3D); This is consistent with previous observations (12, 17). In spleen, the frequency of LinnegNK1.1negCD127+CD4+ matched the number of LTi cells (12, 37). We also detected upregulation of Il22 transcript levels in CD4 lymphocytes (Lin+CD4+) and NK cells (Lin+NK1.1+) after flagellin administration. However, the LinnegNK1.1negCD127+CD4+ cells were the most potent producers, since Il17f and Il22 mRNA levels were 100- to 1,000-fold higher in this population than in LinnegNK1.1negCD127+CD4neg cells, CD4 or NK cells (Fig. 3C). Like the NK-like or LTi-like cells, LinnegNK1.1negCD127+CD4+ innate lymphocytes express Ccr6 but we were unable to detect any mRNA for Rorc or Ncr1 encoding RORγt and NKp46. In addition, we observed that, upon flagellin stimulation, Ifng expression was mainly upregulated in NK cells rather than LinnegCD127+ cells (data not shown). Finally, we observed that the LinnegCD127+ cells were absent in Rag2−/−Il2rg−/− animals (Fig. S3D). Our data provide evidence that LinnegCD127+ innate immune cells, and especially the CD4+ fraction which resembles LTi cells can rapidly produce IL-17 and IL-22 cytokines following TLR activation.
Fig. 3. LinnegCD127+ innate cells upregulate Il17 and Il22 expression following TLR5 stimulation.
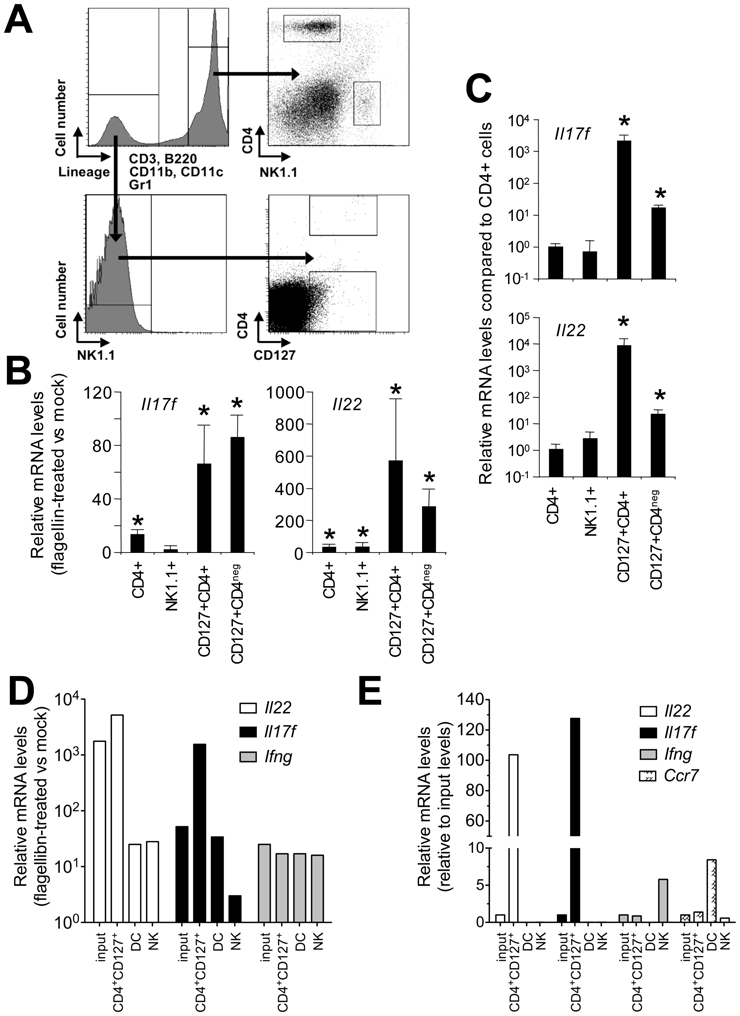
C57BL/6 (A–C) or SCID mice (D–E) mice (n=3–4) were treated i.p. with PBS or flagellin. Spleens were sampled after 2h for cell sorting and quantification of mRNA levels. (A) Sorting scheme. Cells were sorted as Lin+CD4+, Lin+NK1.1+, LinnegNK1.1negCD127+CD4+ cells and LinnegNK1.1negCD127+CD4neg cells. (B) Regulation of Il17f and Il22 expression following flagellin stimulation. mRNA levels and statistical significance are expressed relative to PBS. (C) Levels of transcripts in sorted cells following flagellin stimulation. mRNA levels levels and statistical significance are expressed relative to Lin+CD4+cells. The data correspond to the mean of 3 independent sorting. Results are given as means ± SD. Asterisks indicate P<0.05 in Mann-Whitney test. (D–E) Spleens cells were used such as (input) or sorted as CD3negCD4+CD127+, DC (CD11c+MHCII+) or NK (NKp46+). In D, mRNA levels in flagellin-treated animals are expressed relative to PBS. In E, mRNA levels levels are expressed relative to input cells.
TLR5-mediated activation of Th17-related innate responses requires dendritic cells
To determine whether the TLR5-mediated upregulation of Th17-related innate response is a direct innate lymphocyte activation process or requires DC stimulation, diphtheria toxin (DTX)-mediated ablation of CD11c+ cells was performed in a Cd11c-DTR-EGFP bone marrow chimera. The DTX treatment depleted 93.8±2.2% of CD11c+MHCIIhigh DCs (Fig. 4A). In addition, we found that DTX treatment did not eliminate the CD3negCD4+CD127+ cells in the spleen of a Cd11c-DTR-EGFP chimera and did not alter the the TLR5-mediated production of IL-22 (Fig. S3). As shown in Fig. 4B, systemic administration of flagellin to DC-depleted animals resulted in impaired Il17f or Il22 transcription, compared with controls. Thus, our experiments demonstrated that DCs are necessary for TLR5-mediated expression of Th17-related cytokines.
Fig. 4. Dendritic cells regulate TLR5-dependent, Th17-related innate responses.
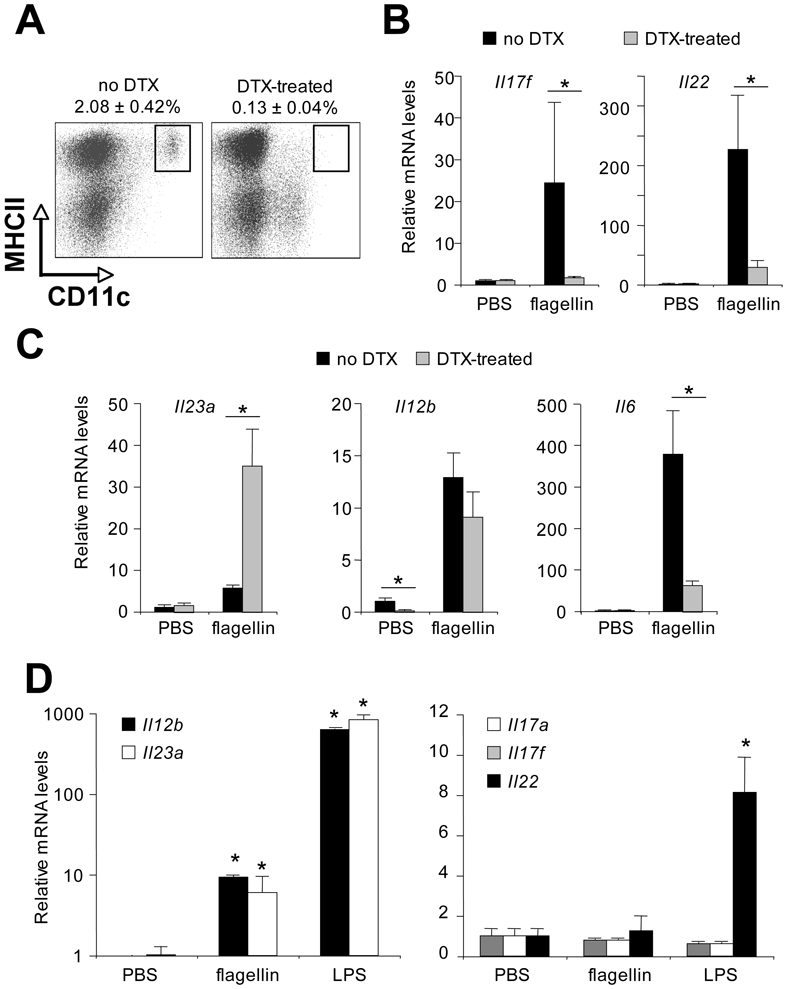
Cd11c-DTR-EGFP→C57BL/6 chimera mice (n=4) were injected i.p. with 100ng diphtheria toxin (DTX) or untreated (no DTX). (A) Depletion of splenic dendritic cells was assessed 24h later by flow cytometry. (B, C) The flagellin-specific transcriptional response. 24h after DTX injection, mice were treated i.p. with PBS or flagellin. Spleen was sampled after 2h for the quantification of transcripts specific for Th17-related cytokine genes (B) and DC-specific cytokine genes (C). mRNA levels are expressed relative to the no-DTX→PBS group. (D) Bone marrow-derived DCs from C57BL/6 mice were treated or not with LPS or flagellin (1μg/ml) for 2 h and mRNA levels were determined relative to mock DCs. Statistical significance was expressed relative to no-DTX (B, C) or relative to the mock DCs (D). Results are given as means ± SD. Asterisks indicate P<0.05 in Mann-Whitney test.
Th17 differentiation depends on tissue-derived TGFβ and IL-1β, and IL-6 produced by DCs and the maintenance of Th17 phenotype has been associated to DC-derived IL-23 (9). In vivo, DC cell ablation was found to attenuate the upregulation of Il6 transcription in response to flagellin (Fig. 4C). We did not observe any alteration in Il1b, Il12b coding for the p40 chain of IL-12 or IL-23, and Tgfb gene expression (data not shown). Intriguingly, Il23a (coding for the p19 chain of IL-23) transcription was enhanced by DTX treatment; it is possible that CD11clowMHCIIneg cells having infiltrated the spleen in DTX-treated mice support Il23a upregulation (Fig. 4A and 4C). Here, we found that flagellin promoted the expression of both Il12b and Il23a in BM-derived DCs (Fig. 4D). In response to flagellin, DCs can therefore produce both IL-6 and IL-23, with the subsequent expression of an innate, Th17-related signature. However, in vivo, IL-23 alone appears unable to induce gene activation. In response to flagellin, DC-mediated IL-6 production could therefore promote the Th17-related signature by LinnegCD127+ cells.
Previous studies suggested that DCs produce IL-22 (4, 38). Here, we found that flagellin promoted the expression of Il12b in BM-derived DCs but did not have any effect on Il17a, Il17f and Il22 transcription (Fig. 4D). Lipopolysaccharide which strongly increased Il12b and Il23a transcription did not upregulate expression of Il17a and Il17f in DCs but did enhance Il22 mRNA levels about 8-fold, compared with untreated cells. Analysis of transcription in splenic DC sorted from mice treated with flagellin also showed that DC were not potent source of IL-22 (Fig. 3D–E). Taken as a whole, our data suggested that DCs are not a major source of TLR5-mediated, Th17-related cytokine production but contribute to induction of the latter.
TLR5 signaling triggers an intestinal, Th17-related, innate response
Since Th17-related cytokines are important in the control of inflammation and infection in the mucosa (3–6, 38, 39), we next assessed the impact of flagellin administration on intestinal tissues. Flagellin strongly enhanced the production of IL-22 within 2h of administration from the duodenum to the proximal colon; the level then returned to the baseline at 8h (Fig. 5). CCL20 synthesis was also strongly induced in the small intestine (Fig. S4A). In contrast, gut IL-17A production changed moderately following flagellin treatment. In any intestine segments, TLR5 signaling strongly enhanced transcription of the Il17 and Il22 genes and those encoding antimicrobial peptides, neutrophil-specific chemokines and growth factors and tissue remodeling/repair molecules (Fig. 5C and Fig. S4B–E). A similar pattern was also observed in lung tissue, but regression to baseline levels was not observed at 8h, suggesting that the kinetic may be different in the respiratory tract (Fig. S5). In conclusion, systemic flagellin administration promotes mucosal Th17-related innate responses.
Fig. 5. TLR5 signaling promotes γc chain-dependent, Th17-related innate responses in the gut.
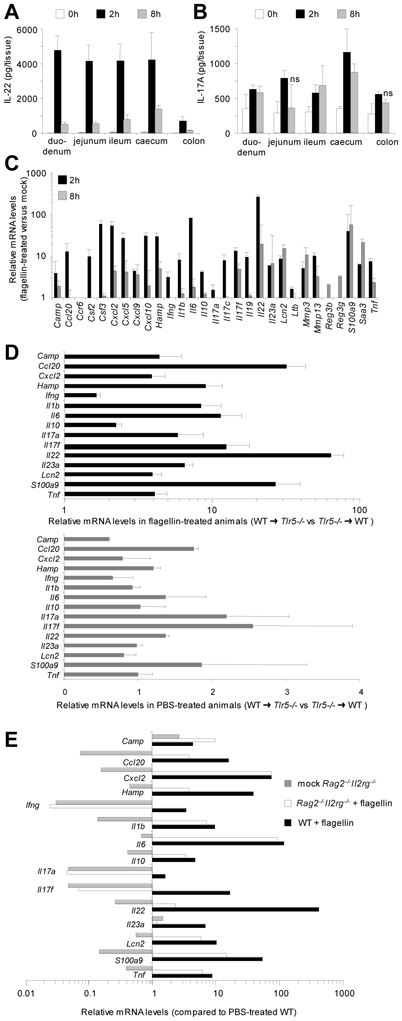
Mice (n=3–4) were treated i.p. with PBS or flagellin and gut segments (5 cm for proximal duodenum, jejunum, distal ileum, 3 cm for proximal colon and the whole cecum) were sampled at the indicated times for quantification of cytokine production and mRNA levels. (A, B) Cytokine production in C57BL/6 (WT) animals. Tissue segments were homogenized within 1 mL of lysis buffer. The results are representative of 2 experiments. (C) Time course analysis of the transcriptional response in WT distal ileum. (D) Contribution of TLR5 signaling in the hematopoietic compartment is essential for the Th17-related signature. mRNA levels 2h after flagellin treatment are expressed as WT→Tlr5−/− relative to Tlr5−/−→WT mice. (E) Contribution of the γc chain to intestinal response. mRNA levels are expressed relative to PBS-treated WT mice. In panels A, B, and D, all data displayed statistically significant changes, except where denoted as “ns” for “non-significant”. Results are given as means ± SD. Mann-Whitney test relative to PBS group was used in A and B. Limma test was used in C to E panels.
We used the same type of analysis than for the response in spleen and lymph nodes to investigate the effects of flagellin on mucosa. The gut and pulmonary flagellin-mediated Th17-like innate response was stronger in WT→Tlr5−/− than in Tlr5−/−→WT animals (Fig. 5D and Fig. S5). These findings indicated that TLR5-competent hematopoietic cells are also instrumental in the mucosal response. DC depletion impaired the upregulation of the intestinal Th17-related signature (Fig. S4F). Lastly, we compared Th17-related gene expression in Rag2−/−Il2rg−/− and WT animals (Fig. 5E). As previously reported, steady-state levels of Il22, Il17 and Ifng transcripts in the ileum were significantly lower in Rag2−/−Il2rg−/− than in WT animals (17). After TLR5 stimulation, transcription of these genes was not enhanced in the Rag2−/−Il2rg−/− intestine. Taken as a whole, our data suggest that TLR5 signaling elicits a mucosal Th17-related response by innate immune cells that require the γc chain and help from DCs.
Finally, the expression of many genes was upregulated in the gut of Rag2−/−Il2rg−/− animals, suggesting that TLR5 signaling promotes the activation of non-lymphoid cells (Fig. 5E). Experiments with the Tlr5−/− chimera reinforced these conclusions since radioresistant cells, likely structural/stromal cells, contributed to TLR5-mediated responses, especially in lung tissue (Fig. 5D and Fig. S5).
The flagellin-induced transcriptional signature has features of Th17- and TLR-mediated responses
To further characterize the response to flagellin, we performed a microarray time course analysis of gene expression in the distal ileum of treated mice. Biological processes including signaling and defense pathways, cytokine- and chemokine-mediated immunity, NF-κB signaling, granulocyte- and macrophage-mediated immunity, cell proliferation and differentiation and apoptosis were significantly modulated 2h-8h after flagellin administration (Fig. S6 and Table S2). On the basis of these data, we arbitrarily defined 5 groups of genes according to their potential role in the gut immune response (Table 1). The first group of genes encodes modulators of IL-17 an IL-22 production as well as differentiation of Th17, LTi, LTi-like, NK and NK-like cells. The second class was involved in the positive or negative transcriptional control of IL-17R (i.e. C/EBPβ and C/EBPδ), IL-22R (i.e. SOCS-1, SOCS-3 and STAT5A) and TLR (i.e. ATF3 and I-κBα) signaling. The third group includes TLR-, IL-17R- and IL-22R-signaling target genes coding for antimicrobial molecules or factors regulating epithelium barrier function. Interestingly, our analysis also identified antiviral genes. In contrast to previous studies of Th17 cytokine-mediated signaling, we did not find any transcriptional modulation of the mucin and β defensin genes. The fourth group corresponds to genes encoding factors involved in recruitment, development or function of various immune cells. Relative to controls, chemokines specific for innate immune cells like neutrophils, NK, NKT or LTi cells, T and B lymphocytes or monocytes were significantly enriched - suggesting that several cell types may enter the tissues and participate in the immune response. The last group includes genes required for TLR4 or TLR2 signaling (i.e. LBP, CD14 and MAL). In conclusion, intestinal gene expression profiling showed that flagellin promotes a transient immune response involving regulators and effectors of both TLR and Th17-mediated immunity.
Table I.
Flagellin-induced gene expression in the ileum displays signatures that are reminiscent of Th17- and TLR-mediated responses
| Expression | ||||
|---|---|---|---|---|
| Group | Genes | 2 h | 8 h | Contribution to |
| I | Ahrr | – | § | Transcriptional regulation of IL-22 gene |
| Arntl | o | – | Transcriptional regulation of IL-22 gene | |
| Batf | + | o | Master regulation of Th17 differentiation | |
| Il1b, Il6, Il1r1, Tnfsf15 | + | o | Activation of Th17 differentiation | |
| Il17f, Il22 | + | + | Th17 cell phenotype | |
| Nfil3 | + | + | Regulation of NK cell differentiation | |
| Pparg | o | – | Inhibition of Th17 differentiation | |
| Rorc | – | – | Master regulation of Th17, Treg, LTi, LTi-, and NK-like cell differentiation | |
| II | Atf3, Irf5, Map3k8, Nfkb1 | + | o | Activation of IL-17R and TLR signaling |
| Cebpb, Cebpd | + | + | Activation of IL-17R signaling | |
| Dusp1, Nfkbia, Nfkbie, Zfp36 | + | o | Repression of IL-17R and TLR signaling | |
| Irf4 | + | + | Activation of IL-17R and TLR signaling | |
| Socs1, Socs3 | + | + | Activation of IL-22R signaling | |
| Stat5a | + | o | Activation of IL-17R and IL-22R signaling | |
| III | Adm, Areg, Ereg, Nrg1, Sprr1a, Sprr2i, Tff2 | + | + | Epithelial barrier function |
| Bcl3, Birc3 | + | o | Inhibitor of apoptosis | |
| Hamp, lipocalin 2, S100a8, S100a9 | + | + | Antimicrobial activity | |
| Isg15, Isg20, Oas2, Oas3 | + | + | Antiviral activity | |
| Ncf1, Nox1, Sod2 | + | o | Antimicrobial activity via superoxides | |
| Retlna, Retlng | + | o | Inflammation control | |
| Rnase1,S100a11 | + | + | Antimicrobial activity? | |
| Saa2 | o | + | Acute phase protein | |
| Saa3 | + | + | Acute phase protein | |
| Serpine1, Serpina3g, Timp1 | + | + | Inflammation control | |
| IV | Adamts4, Adamts3, Adamts8 | + | o | Tissue remodeling |
| Ccl2, Ccl3, Ccl4 | + | + | Monocyte recruitment | |
| Ccl17, Ccl22 | + | o | T cell recruitment | |
| Cxcl1, Cxcl2, Cxcl5 | + | + | Granulocyte recruitment | |
| Ccl7, Cxcl9, Cxcl10, Cxcl11 | + | o | Immune cells recruitment | |
| Cxcl13 | o | + | B and LTi cell recruitment | |
| Ifng, Ifn-regulated genes | + | o | Activation of immunity | |
| Ltb | + | o | Lymphotoxin β receptor signaling in stromal cells | |
| Mmp3, Mmp13 | + | + | Tissue remodeling | |
| Tnfrsf1a, Tnfrsf1b | + | o | TNFRI and TNFRII signaling | |
| Vcam1 | + | + | LTi-mediated organization of lymphoid tissues | |
| V | Cd14 | + | + | LPS binding and TLR4 signaling |
| Lbp | o | + | LPS binding and TLR4 signaling | |
| Mal | o | + | Activation of TLR2 and TLR4 signaling | |
| Tlr2, Pglyprp1 | + | o | Bacterial cell wall signaling | |
• Microarray gene expression data from the distal ileal segments of mice (n = 3) treated i.p. with flagellin for 2 and 8 h were compared with data from mock animals in a time course analysis. All genes differentially expressed and the corresponding method and annotation are included as Supplemental Fig. 5 and Supplemental Table II.
• o, similar expression relative to mock animals; +, upregulation relative to mock animals; -, downregulation relative to mock animals; §, data from a comparison between mock and 2-h flagellin-treated animals.
Discussion
The way in which TLR signaling activates the host’s innate defenses during mucosal invasion by pathogens is subject to debate. In the present study, we showed that TLR5 signaling induces systemic and mucosal innate expression of the Th17-related IL-17 and IL-22 cytokines by stimulating LinnegCD127+ cells in a DC-dependent manner. Overall, our data suggest that LinnegCD127+ cells may play a major role as innate lymphocytes in the early orchestration of a TLR-dependent, protective response to mucosal invasion by pathogens.
Th17-related cytokines contribute to adaptive immunity in response to various inflammatory and infectious diseases (5, 6, 30, 39); however, their impact on the early phase of infection is poorly understood. The effect of TLR signaling on IL-17 and IL-22 was previously suggested since their synthesis was enhanced after administration of TLR2 and TLR4 agonists (12, 29). Very recently, TLR5 signaling was also associated to such response (40). Here, we analyzed the immune response to the TLR5 activator flagellin, with a focus on mucosa. Our rationale was that since flagellin expression is specifically restricted to luminal compartment, its desequestration is likely to be an alarm signal for mucosal invasion (22). We found that systemic flagellin administration promotes the swift, intense, transient production of IL-17A, IL-17F and IL-22 and factors controlling Th17 differentiation. For example, flagellin modulates expression of the genes coding for the aryl hydrogen receptor (AHR) repressor AHRR, the AHR nuclear translocator-like factor ARNTL and the ATF-like factor BATF - all of which are involved in Th17 differentiation (41, 42). Moreover, the flagellin-induced innate response and the Th17 adaptive response share many effectors, such as chemokines, antimicrobial peptides, anti-apoptotic factors and tissue remodeling factors. Therefore, we hypothesized that flagellin-mediated response enables the rapid and transient recruitment of systemic and mucosal defenses.
Our results suggest that the LinnegCD127+ cells, especially the CD4+ fraction, have a pivotal role in the TLR-mediated response via the production of IL-17 and IL-22. These cells are similar to LTi (CD3negCD127+CD4+), LTi-like (RORγt+LinnegCD127+CD4+) and NK-like (RORγt+NKp46+LinnegCD127+NK1.1+/neg) cells (12, 14–17). LTi-like/NK-like cells constitutively produce Th17-related cytokines in a process that depends on gut flora, γc chain and RORγt (15, 17). Moreover, the LTi-like cells were shown to upregulate the production of IL-17 and IL-22 in response to microbial products. The development of LinnegCD127+CD4+ and LinnegCD127+CD4neg cells identified in this study requires the γc chain. These subsets also express the CCR6 but not the NKp46 encoding gene, suggesting a common ontogeny with LTi and LTi-like cells. (12, 13). We were unable to detect any expression of RORγt in the LinnegCD127+ cells; expression below our assay’s detection threshold is one possible explanation for this failure. Furthermore, Rorc expression was downregulated in gut after flagellin injection. Interestingly, we noted enhanced intestinal expression of the gene encoding NFIL3 - a factor that is essential for NK cell development (43). Recent studies demonstrated that increased expression of IL-7 enhances the number of LTi cells (37) and that deficiency in IL-7 affects the number of NK-like IL-22 expressing population (44). Additional work will be needed to define the ontogeny and transcriptional factors involved in the differentiation of LinnegCD127+ cells.
Dendritic cells have an important role in integrating microbial signals and activating immune cells like Th17 lymphocytes (9). When DCs were depleted, the Th17-related innate response to flagellin was impaired, indicating that DCs are necessary for the activation of LinnegCD127+ cells. Similarly, transcription of Il6 was attenuated, which suggests that, in Th17 differentiation, DC-derived IL-6 like may contribute to LinnegCD127+ cell activation (9). Our findings suggested that IL-1β, IL-23 or TGF-β (or at least the amounts produced by DCs) are not required for LinnegCD127+ cell activation. However, IL-23 might be important for alternative activating pathway for production of IL-17 or IL-22 by LTi-like and NK-like cells because (i) cells are activated in vitro by supplementing the culture medium with IL-23 and (ii) CD3negCD4+ cells express IL-23R (12, 13, 15, 45). In the intestine, TLR5 signaling activates lamina propria DCs, which then promote Th17 differentiation (23). In contrast, intestinal DCs do not respond to TLR4 stimulation (23, 46). Flagellin treatment enhanced the transcription of the genes coding for CD14, LPB, MAL and TLR2 (Table 1 and S2). These findings suggest that responsiveness to TLR2 and TLR4 agonists may be re-activated or amplified after TLR5 stimulation, allowing the production of a second wave of effectors.
The relevance of TLR5 signaling in defense has recently been assessed. Flagellin-mediated protection of rodents and non-human primates against lethal irradiation was associated with CSF3-mediated granulopoiesis and the anti-apoptotic effect of SOD2 (47). Flagellin treatment has been linked to resistance against inflammatory colitis and gut infections (48) (40). The TLR5-induced circulating and local production of IL-17/IL-22 may be the main driving force behind these protective effects. The contribution of IL-22 was recently suggested as instrumental in the control of infection with enterococci (40). In response to IL-17R and IL-22R signaling, epithelial and stromal cells produce antimicrobial peptides (RegIII), CXC chemokines and growth factors (CSF3) for neutrophils all of which are involved in mucosal protection (3–7, 38). Flagellin treatment prompted the expression of similar factors. In addition, our study identified other potential effectors of the TLR/IL-17R/IL-22R axis, such as antiviral molecules (ISG15, ISG20, OAS2 and OAS3), acute phase proteins (SAA2, SAA3 and PTX3) and superoxide-mediated killing (NCF1, NOX1 and SOD2).
The LinnegCD127+CD4+ cells herein described resemble the LTi cells that are instrumental in the development of secondary/tertiary lymphoid tissues (such as Peyer’s patches or isolated lymphoid follicles) (13, 49). Intestinal LTi cells express lymphotoxin β (LTβ), and CCR6 and CXCR5, the receptors for CCL20 and CXCL13, respectively (13, 49). CXCL13 and CCL20 are produced by epithelial/stromal cells and are involved in the clustering of lymphocytes, DCs and LTi to form lymphoid follicles (50, 51). Ectopic epithelial expression of CXCL13 increases the number of LTi cells (which produce IL-22 constitutively) and isolated lymphoid follicles (13). Our work revealed that flagellin upregulated gut expression of genes coding for LTβ, CXCL13, and CCL20. We previously showed that flagellin triggers CCL20 production in intestinal epithelial cells (31). Hence, TLR5 signaling in both epithelial and hematopoeitic cells may increase the development of secondary/tertiary lymphoid tissues. Recent studies showed that TLR2, TLR4 and Nod1 are involved in the development of lymphoid follicles (50, 51). Pattern recognition receptors in general and TLRs in particular may have a pivotal role in simultaneously conditioning the antimicrobial environment and new ectopic sites for the development of mucosal adaptive immunity.
In conclusion, the present study found that LinnegCD127+ cells constitute a rapidly reacting, innate source of IL-17A, IL-17F and IL-22 in response to TLR signaling. We hypothesize that this immune reaction occurs during microbial penetration into the lamina propria and stimulates innate effectors to locally clear the infection. Similar cell populations have been identified in humans (14, 16) and so it remains to be seen whether TLR stimulation can promote activation of these innate immune cells.
Supplementary Material
Acknowledgments
We thank Michel Simonet and François Trottein for critical reading of the manuscript, Shizuo Akira for Tlr5−/− mice, David Dombrowicz for Rag2−/−Il2rg−/− mice, and Christelle Faveeuw and Laxmi Koodun for technical assistance.
Footnotes
CC, LVM, DC, and JCS are funded by INSERM, the Institut Pasteur de Lille, the Univ Lille Nord de France, the Région Nord Pas de Calais (ARCir Europe). WDH and JCS are funded by the European Community (INCO-CT-2006-032296).
References
- 1.Beutler B, Jiang Z, Georgel P, Crozat K, Croker B, Rutschmann S, Du X, Hoebe K. Genetic analysis of host resistance: Toll-like receptor signaling and immunity at large. Annu Rev Immunol. 2006;24:353–389. doi: 10.1146/annurev.immunol.24.021605.090552. [DOI] [PubMed] [Google Scholar]
- 2.Sansonetti PJ. War and peace at mucosal surfaces. Nat Rev Immunol. 2004;4:953–964. doi: 10.1038/nri1499. [DOI] [PubMed] [Google Scholar]
- 3.Aujla SJ, Chan YR, Zheng M, Fei M, Askew DJ, Pociask DA, Reinhart TA, McAllister F, Edeal J, Gaus K, Husain S, Kreindler JL, Dubin PJ, Pilewski JM, Myerburg MM, Mason CA, Iwakura Y, Kolls JK. IL-22 mediates mucosal host defense against Gram-negative bacterial pneumonia. Nat Med. 2008;14:275–281. doi: 10.1038/nm1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Y, Valdez PA, Danilenko DM, Hu Y, Sa SM, Gong Q, Abbas AR, Modrusan Z, Ghilardi N, de Sauvage FJ, Ouyang W. Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nat Med. 2008;14:282–289. doi: 10.1038/nm1720. [DOI] [PubMed] [Google Scholar]
- 5.Conti HR, Shen F, Nayyar N, Stocum E, Sun JN, Lindemann MJ, Ho AW, Hai JH, Yu JJ, Jung JW, Filler SG, Masso-Welch P, Edgerton M, Gaffen SL. Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. J Exp Med. 2009;206:299–311. doi: 10.1084/jem.20081463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ishigame H, Kakuta S, Nagai T, Kadoki M, Nambu A, Komiyama Y, Fujikado N, Tanahashi Y, Akitsu A, Kotaki H, Sudo K, Nakae S, Sasakawa C, Iwakura Y. Differential roles of interleukin-17A and -17F in host defense against mucoepithelial bacterial infection and allergic responses. Immunity. 2009;30:108–119. doi: 10.1016/j.immuni.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Gaffen SL. Structure and signalling in the IL-17 receptor family. Nat Rev Immunol. 2009;9:556–567. doi: 10.1038/nri2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kolls JK, McCray PB, Jr, Chan YR. Cytokine-mediated regulation of antimicrobial proteins. Nat Rev Immunol. 2008;8:829–835. doi: 10.1038/nri2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korn T, Bettelli E, Oukka M, Kuchroo VK. IL-17 and Th17 Cells. Annu Rev Immunol. 2009;27:485–517. doi: 10.1146/annurev.immunol.021908.132710. [DOI] [PubMed] [Google Scholar]
- 10.Shibata K, Yamada H, Hara H, Kishihara K, Yoshikai Y. Resident Vdelta1+ gammadelta T cells control early infiltration of neutrophils after Escherichia coli infection via IL-17 production. J Immunol. 2007;178:4466–4472. doi: 10.4049/jimmunol.178.7.4466. [DOI] [PubMed] [Google Scholar]
- 11.Michel ML, Keller AC, Paget C, Fujio M, Trottein F, Savage PB, Wong CH, Schneider E, Dy M, Leite-de-Moraes MC. Identification of an IL-17-producing NK1.1(neg) iNKT cell population involved in airway neutrophilia. J Exp Med. 2007;204:995–1001. doi: 10.1084/jem.20061551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Takatori H, Kanno Y, Watford WT, Tato CM, Weiss G, Ivanov, Littman DR, O’Shea JJ. Lymphoid tissue inducer-like cells are an innate source of IL-17 and IL-22. J Exp Med. 2009;206:35–41. doi: 10.1084/jem.20072713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marchesi F, Martin AP, Thirunarayanan N, Devany E, Mayer L, Grisotto MG, Furtado GC, Lira SA. CXCL13 expression in the gut promotes accumulation of IL-22-producing lymphoid tissue-inducer cells, and formation of isolated lymphoid follicles. Mucosal Immunol. 2009 doi: 10.1038/mi.2009.113. [DOI] [PubMed] [Google Scholar]
- 14.Cella M, Fuchs A, Vermi W, Facchetti F, Otero K, Lennerz JK, Doherty JM, Mills JC, Colonna M. A human natural killer cell subset provides an innate source of IL-22 for mucosal immunity. Nature. 2009;457:722–725. doi: 10.1038/nature07537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanos SL, V, Bui L, Mortha A, Oberle K, Heners C, Johner C, Diefenbach A. RORgammat and commensal microflora are required for the differentiation of mucosal interleukin 22-producing NKp46+ cells. Nat Immunol. 2009;10:83–91. doi: 10.1038/ni.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cupedo T, Crellin NK, Papazian N, Rombouts EJ, Weijer K, Grogan JL, Fibbe WE, Cornelissen JJ, Spits H. Human fetal lymphoid tissue-inducer cells are interleukin 17-producing precursors to RORC+ CD127+ natural killer-like cells. Nat Immunol. 2009;10:66–74. doi: 10.1038/ni.1668. [DOI] [PubMed] [Google Scholar]
- 17.Satoh-Takayama N, Vosshenrich CA, Lesjean-Pottier S, Sawa S, Lochner M, Rattis F, Mention JJ, Thiam K, Cerf-Bensussan N, Mandelboim O, Eberl G, Di Santo JP. Microbial flora drives interleukin 22 production in intestinal NKp46+ cells that provide innate mucosal immune defense. Immunity. 2008;29:958–970. doi: 10.1016/j.immuni.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Luci C, Reynders A, Ivanov, Cognet C, Chiche L, Chasson L, Hardwigsen J, Anguiano E, Banchereau J, Chaussabel D, Dalod M, Littman DR, Vivier E, Tomasello E. Influence of the transcription factor RORgammat on the development of NKp46+ cell populations in gut and skin. Nat Immunol. 2009;10:75–82. doi: 10.1038/ni.1681. [DOI] [PubMed] [Google Scholar]
- 19.Ramos HC, Rumbo M, Sirard JC. Bacterial flagellins: mediators of pathogenicity and host immune responses in mucosa. Trends Microbiol. 2004;12:509–517. doi: 10.1016/j.tim.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Bambou JC, Giraud A, Menard S, Begue B, Rakotobe S, Heyman M, Taddei F, Cerf-Bensussan N, Gaboriau-Routhiau V. In vitro and ex vivo activation of the TLR5 signaling pathway in intestinal epithelial cells by a commensal Escherichia coli strain. J Biol Chem. 2004;279:42984–42992. doi: 10.1074/jbc.M405410200. [DOI] [PubMed] [Google Scholar]
- 21.Didierlaurent A, Goulding J, Patel S, Snelgrove R, Low L, Bebien M, Lawrence T, van Rijt LS, Lambrecht BN, Sirard JC, Hussell T. Sustained desensitization to bacterial Toll-like receptor ligands after resolution of respiratory influenza infection. J Exp Med. 2008;205:323–329. doi: 10.1084/jem.20070891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes EA, Galan JE. Immune response to Salmonella: location, location, location? Immunity. 2002;16:325–328. doi: 10.1016/s1074-7613(02)00293-5. [DOI] [PubMed] [Google Scholar]
- 23.Uematsu S, Fujimoto K, Jang MH, Yang BG, Jung YJ, Nishiyama M, Sato S, Tsujimura T, Yamamoto M, Yokota Y, Kiyono H, Miyasaka M, Ishii KJ, Akira S. Regulation of humoral and cellular gut immunity by lamina propria dendritic cells expressing Toll-like receptor 5. Nat Immunol. 2008;9:769–776. doi: 10.1038/ni.1622. [DOI] [PubMed] [Google Scholar]
- 24.Uematsu S, Jang MH, Chevrier N, Guo Z, Kumagai Y, Yamamoto M, Kato H, Sougawa N, Matsui H, Kuwata H, Hemmi H, Coban C, Kawai T, Ishii KJ, Takeuchi O, Miyasaka M, Takeda K, Akira S. Detection of pathogenic intestinal bacteria by Toll-like receptor 5 on intestinal CD11c+ lamina propria cells. Nat Immunol. 2006;7:868–874. doi: 10.1038/ni1362. [DOI] [PubMed] [Google Scholar]
- 25.Didierlaurent A, Ferrero I, Otten LA, Dubois B, Reinhardt M, Carlsen H, Blomhoff R, Akira S, Kraehenbuhl JP, Sirard JC. Flagellin Promotes Myeloid Differentiation Factor 88-Dependent Development of Th2-Type Response. J Immunol. 2004;172:6922–6930. doi: 10.4049/jimmunol.172.11.6922. [DOI] [PubMed] [Google Scholar]
- 26.Hapfelmeier S, Muller AJ, Stecher B, Kaiser P, Barthel M, Endt K, Eberhard M, Robbiani R, Jacobi CA, Heikenwalder M, Kirschning C, Jung S, Stallmach T, Kremer M, Hardt WD. Microbe sampling by mucosal dendritic cells is a discrete, MyD88-independent step in DeltainvG S. Typhimurium colitis. J Exp Med. 2008;205:437–450. doi: 10.1084/jem.20070633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eilebrecht S, Pellay FX, Odenwalder P, Brysbaert G, Benecke BJ, Benecke A. EBER2 RNA-induced transcriptome changes identify cellular processes likely targeted during Epstein Barr Virus infection. BMC Res Notes. 2008;1:100. doi: 10.1186/1756-0500-1-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Noth S, Brysbaert G, Benecke A. Normalization using weighted negative second order exponential error functions (NeONORM) provides robustness against asymmetries in comparative transcriptome profiles and avoids false calls. Genomics Proteomics Bioinformatics. 2006;4:90–109. doi: 10.1016/S1672-0229(06)60021-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dumoutier L, Van Roost E, Colau D, Renauld JC. Human interleukin-10-related T cell-derived inducible factor: molecular cloning and functional characterization as an hepatocyte-stimulating factor. Proc Natl Acad Sci U S A. 2000;97:10144–10149. doi: 10.1073/pnas.170291697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirota K, Yoshitomi H, Hashimoto M, Maeda S, Teradaira S, Sugimoto N, Yamaguchi T, Nomura T, Ito H, Nakamura T, Sakaguchi N, Sakaguchi S. Preferential recruitment of CCR6-expressing Th17 cells to inflamed joints via CCL20 in rheumatoid arthritis and its animal model. J Exp Med. 2007;204:2803–2812. doi: 10.1084/jem.20071397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sierro F, Dubois B, Coste A, Kaiserlian D, Kraehenbuhl JP, Sirard JC. Flagellin stimulation of intestinal epithelial cells triggers CCL20-mediated migration of dendritic cells. Proc Natl Acad Sci U S A. 2001;98:13722–13727. doi: 10.1073/pnas.241308598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caron G, Duluc D, Fremaux I, Jeannin P, David C, Gascan H, Delneste Y. Direct Stimulation of Human T Cells via TLR5 and TLR7/8: Flagellin and R-848 Up-Regulate Proliferation and IFN-{gamma} Production by Memory CD4+ T Cells. J Immunol. 2005;175:1551–1557. doi: 10.4049/jimmunol.175.3.1551. [DOI] [PubMed] [Google Scholar]
- 33.Chalifour A, Jeannin P, Gauchat JF, Blaecke A, Malissard M, N’Guyen T, Thieblemont N, Delneste Y. Direct bacterial protein PAMP recognition by human NK cells involves TLRs and triggers alpha-defensin production. Blood. 2004;104:1778–1783. doi: 10.1182/blood-2003-08-2820. [DOI] [PubMed] [Google Scholar]
- 34.Sanders CJ, Moore DA, 3rd, Williams IR, Gewirtz AT. Both radioresistant and hemopoietic cells promote innate and adaptive immune responses to flagellin. J Immunol. 2008;180:7184–7192. doi: 10.4049/jimmunol.180.11.7184. [DOI] [PubMed] [Google Scholar]
- 35.Janot L, Sirard JC, Secher T, Noulin N, Fick L, Akira S, Uematsu S, Didierlaurent A, Hussell T, Ryffel B, Erard F. Radioresistant cells expressing TLR5 control the respiratory epithelium’s innate immune responses to flagellin. Eur J Immunol. 2009;39:1587–1596. doi: 10.1002/eji.200838907. [DOI] [PubMed] [Google Scholar]
- 36.Caminschi I, Ahmet F, Heger K, Brady J, Nutt SL, Vremec D, Pietersz S, Lahoud MH, Schofield L, Hansen DS, O’Keeffe M, Smyth MJ, Bedoui S, Davey GM, Villadangos JA, Heath WR, Shortman K. Putative IKDCs are functionally and developmentally similar to natural killer cells, but not to dendritic cells. J Exp Med. 2007;204:2579–2590. doi: 10.1084/jem.20071351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmutz S, Bosco N, Chappaz S, Boyman O, Acha-Orbea H, Ceredig R, Rolink AG, Finke D. Cutting Edge: IL-7 Regulates the Peripheral Pool of Adult ROR{gamma}+ Lymphoid Tissue Inducer Cells. J Immunol. 2009 doi: 10.4049/jimmunol.0802911. [DOI] [PubMed] [Google Scholar]
- 38.Pickert G, Neufert C, Leppkes M, Zheng Y, Wittkopf N, Warntjen M, Lehr HA, Hirth S, Weigmann B, Wirtz S, Ouyang W, Neurath MF, Becker C. STAT3 links IL-22 signaling in intestinal epithelial cells to mucosal wound healing. J Exp Med. 2009;206:1465–1472. doi: 10.1084/jem.20082683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zenewicz LA, Yancopoulos GD, Valenzuela DM, Murphy AJ, Stevens S, Flavell RA. Innate and adaptive interleukin-22 protects mice from inflammatory bowel disease. Immunity. 2008;29:947–957. doi: 10.1016/j.immuni.2008.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kinnebrew MA, Ubeda C, Zenewicz LA, Smith N, Flavell RA, Pamer EG. Bacterial flagellin stimulates Toll-like receptor 5-dependent defense against vancomycin-resistant Enterococcus infection. J Infect Dis. 2010;201:534–543. doi: 10.1086/650203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Veldhoen M, Hirota K, Christensen J, O’Garra A, Stockinger B. Natural agonists for aryl hydrocarbon receptor in culture medium are essential for optimal differentiation of Th17 T cells. J Exp Med. 2009;206:43–49. doi: 10.1084/jem.20081438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schraml BU, Hildner K, Ise W, Lee WL, Smith WA, Solomon B, Sahota G, Sim J, Mukasa R, Cemerski S, Hatton RD, Stormo GD, Weaver CT, Russell JH, Murphy TL, Murphy KM. The AP-1 transcription factor Batf controls T(H)17 differentiation. Nature. 2009;460:405–409. doi: 10.1038/nature08114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gascoyne DM, Long E, Veiga-Fernandes H, de Boer J, Williams O, Seddon B, Coles M, Kioussis D, Brady HJ. The basic leucine zipper transcription factor E4BP4 is essential for natural killer cell development. Nat Immunol. 2009;10:1118–1124. doi: 10.1038/ni.1787. [DOI] [PubMed] [Google Scholar]
- 44.Satoh-Takayama N, Lesjean-Pottier S, Vieira P, Sawa S, Eberl G, Vosshenrich CA, Di Santo JP. IL-7 and IL-15 independently program the differentiation of intestinal CD3-NKp46+ cell subsets from Id2-dependent precursors. J Exp Med. 2010;207:273–280. doi: 10.1084/jem.20092029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Awasthi A, Riol-Blanco L, Jager A, Korn T, Pot C, Galileos G, Bettelli E, Kuchroo VK, Oukka M. Cutting edge: IL-23 receptor gfp reporter mice reveal distinct populations of IL-17-producing cells. J Immunol. 2009;182:5904–5908. doi: 10.4049/jimmunol.0900732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cerovic V, Jenkins CD, Barnes AG, Milling SW, MacPherson GG, Klavinskis LS. Hyporesponsiveness of intestinal dendritic cells to TLR stimulation is limited to TLR4. J Immunol. 2009;182:2405–2415. doi: 10.4049/jimmunol.0802318. [DOI] [PubMed] [Google Scholar]
- 47.Burdelya LG, V, Krivokrysenko I, Tallant TC, Strom E, Gleiberman AS, Gupta D, Kurnasov OV, Fort FL, Osterman AL, Didonato JA, Feinstein E, Gudkov AV. An agonist of toll-like receptor 5 has radioprotective activity in mouse and primate models. Science. 2008;320:226–230. doi: 10.1126/science.1154986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vijay-Kumar M, Aitken JD, Sanders CJ, Frias A, Sloane VM, Xu J, Neish AS, Rojas M, Gewirtz AT. Flagellin treatment protects against chemicals, bacteria, viruses, and radiation. J Immunol. 2008;180:8280–8285. doi: 10.4049/jimmunol.180.12.8280. [DOI] [PubMed] [Google Scholar]
- 49.Meier D, Bornmann C, Chappaz S, Schmutz S, Otten LA, Ceredig R, Acha-Orbea H, Finke D. Ectopic lymphoid-organ development occurs through interleukin 7-mediated enhanced survival of lymphoid-tissue-inducer cells. Immunity. 2007;26:643–654. doi: 10.1016/j.immuni.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 50.Bouskra D, Brezillon C, Berard M, Werts C, Varona R, Boneca IG, Eberl G. Lymphoid tissue genesis induced by commensals through NOD1 regulates intestinal homeostasis. Nature. 2008;456:507–510. doi: 10.1038/nature07450. [DOI] [PubMed] [Google Scholar]
- 51.Tsuji M, Suzuki K, Kitamura H, Maruya M, Kinoshita K, Ivanov, Itoh K, Littman DR, Fagarasan S. Requirement for lymphoid tissue-inducer cells in isolated follicle formation and T cell-independent immunoglobulin A generation in the gut. Immunity. 2008;29:261–271. doi: 10.1016/j.immuni.2008.05.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


